Abstract
Objectives
To estimate the prevalence of lifetime traumatic experiences, describe related symptoms of traumatic stress, and examine their association with perceived social support and physical and mental health among older American Indians.
Method
Analyses of existing interview data from the Native Elder Care Study, a random age-stratified sample of 505 tribal members ≥55 years of age conducted in partnership with a large Southeastern tribe. Interviews assessed trauma exposure, traumatic stress, measures of social support, and physical and mental health status.
Results
Overall, 31% of participants had experienced a traumatic event; of these, 43% reported traumatic stress at the time of the interview. Higher perceived social support was associated with a reduced prevalence of traumatic stress. Compared to their counterparts without traumatic stress, women participants reporting traumatic stress reported more symptoms of depression, and both symptomatic men and women had a higher prevalence of cardiovascular disease and chronic pain.
Discussion
Traumatic stress was associated with less perceived social support and poorer health. Social support was not found to moderate the relationship between traumatic stress and physical and mental health.
Keywords: American Indians, Health, Native Americans, Social Support, Trauma
The majority of American Indians, age 55 years or younger, have experienced at least one traumatic event in their lifetime (Beals et al., 2013; Robin, Chester, Rasmussen, Jaranson, & Goldman, 1997). Up to 81% of American Indians report experiencing a wide array of traumatic events including assault, domestic violence, Indian boarding school abuse, combat, motor vehicle crashes, and natural disasters (Robin et al., 1997). Traumatic experiences may also include witnessing traumatic events or hearing that a family member or close friend experienced an event such as rape/sexual abuse or suicide (Beals et al., 2013, Manson, Beals, Klein, & Croy, 2005).
The landmark American Indian Service Utilization, Psychiatric Epidemiology, Risk and Protective Factors Project (AI-SUPERPFP; Beals et al., 2005) examined traumatic experiences among several of the largest reservation-based populations in the country. A total of 3,084 tribal members between the ages of 15–54 years from two reservations were interviewed; 1,967 (64%) had been exposed to at least one traumatic event during their lifetime (Beals et al., 2013). These events fell into four categories: interpersonal (e.g., assault, rape, domestic violence, and combat), non-interpersonal (e.g., accidents and natural disasters), witnessing traumatic events, and trauma to someone close. American Indian women experienced more interpersonal trauma than did men and American Indian men experienced more non-interpersonal trauma within each tribe than did women (Beals et al., 2013). Within interpersonal traumas, men were more likely to report combat exposure, and women were more likely to report rape and domestic violence (Beals et al., 2013). The probability of trauma exposure increased with age, but by virtue of the study’s design, this finding truncated at age 55. Another study of American Indians from a Southwest tribe reported an even higher prevalence (81.4%) of having experienced a traumatic event (Robin et al., 1997).
Neither study addressed the nature and extent of trauma among older American Indians, who may experience unique risks in this regard, such as forced Indian boarding school education. From the 1880s to the 1970s, the U.S. government removed hundreds of thousands of American Indian children from their families, often forcibly, in the early years of their lives. Children were placed in government or church-run boarding schools established to “civilize” students by distancing them from their culture and immersing them in an “Americanized” system (Colmant et al., 2004). In addition, many children in Indian boarding schools were victims of physical and sexual abuse (Lefler & Belt, 2009). Disconnection from culture and family left many American Indians with a loss of language, customs, and traditional relationships (Lefler & Belt, 2009; Wesley-Esquimaux & Smolewski, 2004; Whitesell, Beals, Crow, Mitchell, & Novins, 2012). Within the context of modern psychopathology, the kind of cultural trauma experienced by American Indians during the boarding school era is difficult to conceptualize.
As a consequence of exposure to a traumatic event, symptoms of traumatic stress may develop which include emotional numbing, hyper-arousal, flashbacks, and avoidance behaviors. An estimated 40% of American Indians exposed to a traumatic event will develop one or more symptoms of traumatic stress (Bassett, Nelson, Rhoades, Krantz, & Omidpanah, 2014). In sufficient number, combination, and duration, these symptoms can lead to post-traumatic stress disorder (PTSD), a chronic, debilitating condition that portends impaired function in many aspects of one’s life (American Psychiatric Association, 2013). Lifetime prevalence of PTSD ranges from 6.6% (Bassett, Buchwald, & Manson, 2014) to 7.4% (Roberts, Gilman, Breslau, Breslau, & Koenen, 2011) for the general U.S. population. In comparison, American Indians in the AI-SUPERPFP study exhibited higher prevalence of PTSD than the general population (Women: >20 vs. 9.1%; Men: >11.5 vs. 4.3%; Beals et al., 2005). On average, prevalence of PTSD for women is double that of men among both the general population (Ditlevsen & Elklit, 2010; Kessler, Sonnega, Bromet, Hughes, & Nelson, 1995; McPherson-Sexton, 2006) and American Indians (Bassett, Buchwald, et al., 2014; Beals et al., 2013). American Indians are twice as likely to develop full PTSD compared to the general U.S. population (Bassett, Buchwald, et al., 2014), due in part to the high prevalence of exposure to traumatic events (Beals et al., 2013). Although studies have reported the prevalence of lifetime trauma exposure and development of symptoms of traumatic stress for American Indians from childhood through middle-age, this relation among older American Indians is unknown.
Trauma exposure and the resulting stress are associated with increased likelihood of depression and substance use in the general U.S. population (Schnurr & Green, 2004) as well as among American Indians (Bassett, Buchwald et al., 2014). Among the general population, women are more likely to report co-occurring internalizing disorders like anxiety and depression, and men are more likely to report externalizing disorders, like substance abuse (Kessler et al., 2005; Tolin & Foa, 2006). Traumatic exposure is also related to poorer self-reported health and chronic health conditions, namely chronic pain, hypertension, cardiovascular disease, obesity, and hyperlipidemia in both the population at large (McFarlane, 2010) and among American Indians (Bassett, Buchwald et al., 2014). The combination of high prevalence of trauma (Manson et al., 2005) and symptomological consequences (Bassett, Buchwald et al., 2014; Beals et al., 2013) may compromise the health and well-being of American Indians across the lifespan.
Social support can buffer traumatic stress and forestall the onset of related symptoms among the general population (Brewin, Andrews, & Valentine, 2000; McPherson-Sexton, 2006). The specific mechanisms are frequently discussed in terms of emotional, informational, and tangible support, positive social interaction, and affection (Sherbourne & Stewart, 1991). Emotional and informational supports include empathetic understanding, encouragement, and guidance. Tangible support includes material aid and behavioral assistance. Positive social interaction consists of social companionship and having someone to engage in social activities. Affectionate support consists of physical expressions of love and caring (Sherbourne & Stewart, 1991). This four-factor model of perceived social support was supported for all three major indigenous groups in Canada (Richmond, Ross, & Bernier, 2007).
The salutary effect of social support on psychological well-being in general, and specifically regarding traumatic stress is less clear with respect to older adults. Forming and maintaining close relationships can be difficult for older individuals exposed to trauma (Colman & Widom, 2004), often due to the disengagement that accompanies emotional numbing and withdrawal (Galovski & Lyons, 2004). Then, too, older individuals are at risk for less social support due to decreased mobility and greater morbidity and mortality of people in their interpersonal networks (McPherson-Sexton, 2006).
The literature is silent with respect to how social support may buffer traumatic stress among older American Indians. There is a prevailing belief that social support is alive and well among American Indians (Limb, Shafer, & Sandoval, 2014). American Indians tend to value interdependence and rely more on social support from and have more frequent contact with extended kin networks than other ethnic groups (MacPhee, Fritz, & Miller-Heyl, 1996). They also report feeling closer to those in their networks and support systems than other ethnic groups (MacPhee et al., 1996; D. Martin & Yurkovich, 2014). Similar themes emerge regarding caregiving for older American Indians. Informal caregivers tend to see their role as an interdependent exchange, benefitting all involved, and respecting elders as a core cultural value (Jervis, Boland, & Fickenscher, 2010). Consequently, social support may play a crucial protective role, especially among older adults, who often endorse such cultural ideals. Despite these values, some rural and reservation communities experience an outward migration of younger members, often in search of educational or economic opportunities, resulting in fewer available caregivers (Garrett et al., 2010).
Clear evidence exists that social support can protect against adverse health outcomes (Holt-Lunstad, Smith, & Layton, 2010). Low levels of social support may increase the risk of mortality among older adults (Mazzella et al., 2010), while higher levels of social support are associated with lower levels of loneliness and better mental health (Isaacowitz, Smith, & Carstensen, 2003). Among American Indians, less social support has been linked to poor perceived health (Bassett, Nelson, et al., 2014). This relation of social support as the most important dimension of health has been corroborated in two studies with Indigenous Canadians that examined health status and types of social support among 31,625 Inuit, Metis, and First Nations peoples (Richmond, Ross, & Bernier, 2007; Richmond, Ross, & Egeland, 2007). Women who reported better health status reported higher levels of emotional support, tangible support, and positive social interactions (Richmond, Ross, & Egeland, 2007). Men who reported better health status reported higher levels of emotional support (Richmond, Ross, & Egeland, 2007).
The number of older American Indians is growing rapidly and expected to triple in the next 30 years (Ortman, Velkoff, & Hogan, 2014). Yet, no studies of trauma among American Indians have considered the experiences of adults over 55 years of age (Bassett, Buchwald et al., 2014; Manson et al., 2005). Nor does the relevant literature offer insight into the factors that may moderate the resulting stress and subsequent impairment or disability. Given opportunities for future intervention, and an increasing emphasis on emotional well-being and resilience, this line of inquiry is particularly timely and important (Community Translational Science Team, 2016).
The analyses reported here address this knowledge gap by drawing upon data derived from the Native Elder Care Study (Goins, Garroutte, Fox, Geiger, & Manson, 2011). We first sought to describe the prevalence of lifetime exposures to traumatic events and current symptoms of traumatic stress. We then hypothesized that current symptoms of traumatic stress would be negatively associated with perceived social support. We also hypothesized that current traumatic stress symptoms would be related to poorer health, but that this relation would be moderated by perceived social support. We postulated that of those with current symptoms of traumatic stress, women would express more depressive symptomology then men, and men would report higher consumption of alcohol than women.
Design and Method
The Native Elder Care Study was developed through a collaborative process of tribal participatory research (Goins et al., 2011). It is a cross-sectional study of 505 older members of a rural, Southeastern, federally recognized tribe living within their tribe’s service region (Goins et al., 2011).
Study Population and Procedures
The Native Elder Care Study entailed identifying all individuals ≥55 years of age living within the tribe’s service area through tribal rolls, followed by selection of a random, age-stratified sample for participation in the study protocol. Individuals in an institutional setting (nursing home, hospital, prison) and those aged ≥65 years who failed a brief dementia screening were deemed ineligible to participant in the study (14 possible participants were in a nursing home, 14 did not pass the dementia screener, none were excluded for being in the hospital or a prison at the time of the study; Goins, Innes, & Dong, 2012).
Five hundred and five participants completed a baseline interview and examination between 2006 and 2008. Tribal leaders consulted in choosing instruments. The interview included measures of physical and mental health, daily functioning, service use, sociodemographics, and environmental characteristics. The reliability and validity of all measures were considered, with specific attention to those measures previously used with American Indians.
For these analyses, we excluded 19 participants who did not answer items about trauma experience or related symptoms. The mean age of the remaining participants was 70.7 years of age; 65% were female. The face-to-face interview lasted from 60 to 90 minutes, either in the participant’s home or at a local tribal building. In line with tribal participatory research, over half of the interviewers were tribal members and the others resided in the community. The appropriate Tribal and university institutional review boards reviewed and approved the original Native Elder Care Study as well as this secondary data analysis.
Measures
Sociodemographic characteristics—participant age, gender, education (less than high school degree, high school degree or general education diploma, or at least some college), current annual income (less than $15,000, $15,000–$24,999, ≥$25,000), and marital status (single, married or current life partner, divorced, or widowed)—were included in our analyses.
Lifetime trauma exposure and related symptoms were elicited using the PTSD questions from the National Anxiety Disorder Screening Day instrument (Olfson et al., 2000; Ritsher, Struening, Hellman, & Guardino, 2002). This measure has been successfully used in prior large-scale studies with American Indians (Jacob et al., 2013; Ritsher et al., 2002). We operationalized “lifetime trauma exposure” as a binary, categorical variable based on the participant’s answer to the question “Sometimes bad things happen to us that can affect our health. Have you ever had an extremely frightening, traumatic, or horrible experience? Here we mean something like being a victim of a violent crime or domestic violence, being in a disaster like a flood or fire, or being in combat. Other examples are being seriously injured in an accident or being sexually assaulted. It could also mean seeing someone seriously injured or killed.” Participants endorsing the item of lifetime trauma exposure were then asked about their possible experience of traumatic symptoms, organized in terms of the four major categories, over the 30 days prior to the interview: (1) re-experiencing the traumatic event; (2) emotional numbing; (3) hyper-arousal, and (4) avoidance behaviors. Each category of symptoms was recorded as present or absent. We then created a binary measure of traumatic symptoms, with the value of 0 indicating either no traumatic experience or a traumatic experience but no current symptoms of trauma, and a value of 1 indicating the experience of a traumatic event and endorsement of at least one symptom category attributed to that experience.
Social support was measured with the Medical Outcomes Study Social Support Survey (Sherbourne & Stewart, 1991). This scale consists of 19 items, employing a five-point response scale that ranges from none of the time (0) to all of the time (4), with higher scores indicating more perceived social support. It assesses perceived availability of four types of support: tangible support; affectionate support; positive social interaction; emotional support. Overall social support is computed by combining the scores of the four subscales. This measure exhibits good psychometric properties across diverse populations (López & Cooper, 2011). Overall social support and its four subtypes have good construct validity, demonstrated through multi-trait scaling and factor analysis with a sample of 2,987 participants with one or more chronic diseases residing in three large cities (Sherbourne & Stewart, 1991). High internal reliability has also been demonstrated (Cronbach’s alpha coefficients > 0.90) for each subscale and overall social support (Sherbourne & Stewart, 1991).
The performance characteristics of the Medical Outcomes Study Social Support Survey were previously evaluated using data from the Native Elder Care Study (Conte, Schure, & Goins, 2015). Cronbach’s alpha scores ranged from 0.89 to 0.95 (Conte et al., 2015) and construct validity was replicated. A principal component factor analysis revealed a single factor of overall social support and every item had a high factor loading (≥0.65) with the single dimension of social support (Conte et al., 2015). A confirmatory factor analysis supported the four subscale factor structure (Conte et al., 2015).
Depression was measured using the Center for Epidemiologic Studies Depression Scale (CES-D; Radloff, 1977) which assesses how often common symptoms of depression were experienced in the past week. It consists of 20 items with a four-point response scale ranging from rarely or none of the time to most or all of the time. The scale is reliable and valid in diverse populations (Radloff, 1977) and demonstrates good internal consistency with both American Indian youth (Manson, Ackerson, Dick, Baron, & Fleming, 1990) and adults (Somervell et al., 1993). The Cronbach’s alpha for the Elder Care Study sample is 0.87 and showed good convergent and divergent validity (Schure & Goins, 2017). The cut-point score most commonly used to indicate those at risk for clinically significant depression is ≥16, but a lower cut-point of 12 may be more appropriate for older adults (Lewinsohn, Seeley, Roberts, & Allen, 1997).
Current alcohol drinkers were queried about how frequently they consumed alcohol (daily, 3–6 times a week, 1–2 times a week, 1–3 times a month, less than once a month) and how many drinks per day on average they consumed when drinking. Commercial tobacco (not ceremonial) use was assessed by asking if participants currently smoked cigarettes or chewed tobacco. Endorsement of either type of tobacco use constituted an affirmative answer to this question.
Participants were asked if they had been diagnosed since turning 55 years old with hypertension, diabetes, chronic pain (a composite of items chronic pain syndrome, back pain, and/or arthritis), or cardiovascular disease (a composite of items on heart attack, stroke, congestive heart failure, angina, or heart disease). These items expanded a previous version of a survey designed to assess common conditions across eight medical domains in the general population (Rigler, Studenski, Wallace, Reker, & Duncan, 2002). The test–retest reliability of the original version has kappa scores between 0.78 and 1.00 for all domains except musculoskeletal pain (Rigler et al., 2002). Although the accuracy of self-report varies widely by type of condition (L. M. Martin, Leff, Calonge, Garrett, & Nelson, 2000), many of the self-reported health conditions in our analyses correlated well with medical records, including hypertension (L. M. Martin et al., 2000; Okura, Urban, Mahoney, Jacobsen, & Rodeheffer, 2004), diabetes (L. M. Martin et al., 2000; Okura et al., 2004), heart attack (Okura et al., 2004), and stroke (Okura et al., 2004).
Data Analysis
We calculated summary statistics for sociodemographic, clinical, and health-related characteristics of this sample. We used logistic regression to estimate the association between lifetime trauma exposure, related symptoms, and current social support. Linear and logistic regression analyses estimated the relation between current traumatic symptoms and mental and physical health measures. We further assessed these associations for effect modification by social support. All models adjusted for age, gender, education, and Indian boarding school attendance. We assessed marital status and income as possible confounders (a 10% or greater change in estimated effects); though, as late-life exposures, these are suspect to be caused by traumatic exposure and related symptoms. We assessed possible effect modification by gender in all models by adjusting for a product term and conducting statistical testing at the 0.10 level. Marginal standardization was used to transform odds ratios to prevalence ratios in logistic models (Muller & MacLehose, 2014). We present model coefficients and prevalence ratios from linear and logistic regression models along with 95% robust confidence intervals and Wald tests using robust standard errors. The overall prevalence of missingness was low and did not follow any discernable patterns. We used complete cases in all analyses. All analyses were conducted using R version 3.3.3 (R Core Team, 2017) and the packages sandwich (Zeileis, 2004) and epitools (Aragon, 2017).
Results
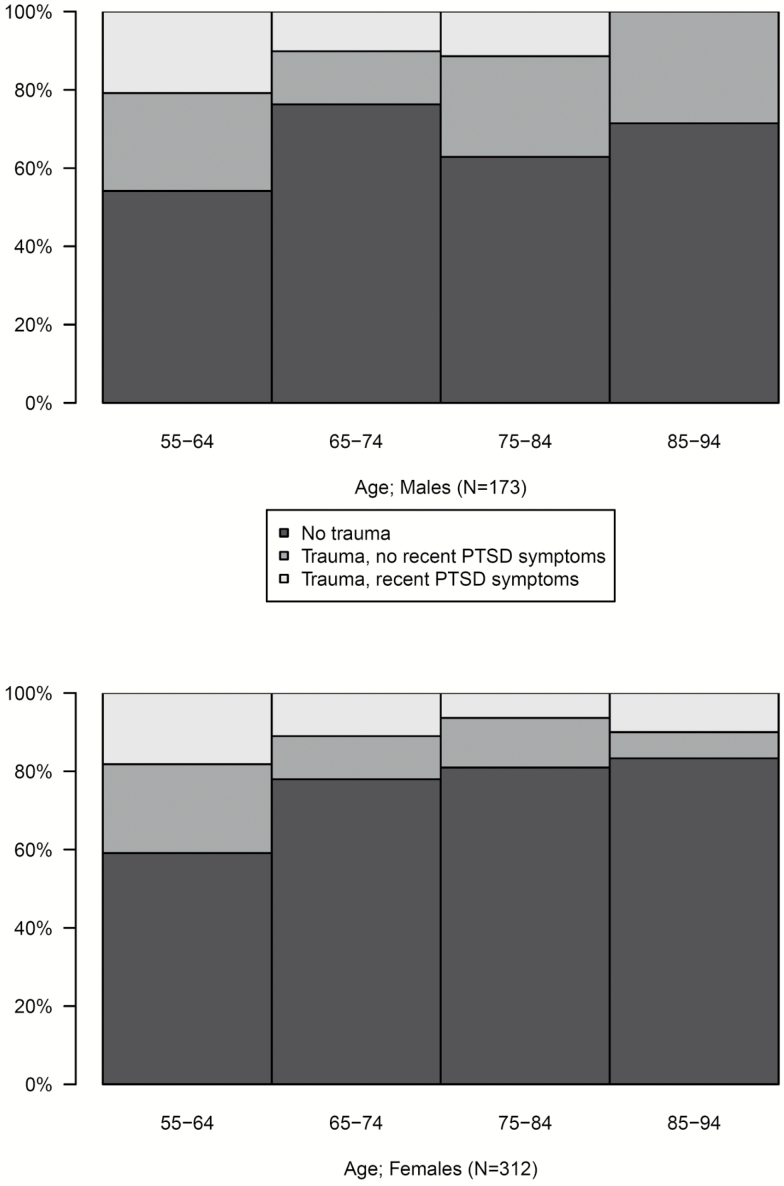
Table 1 summarizes the results of the sociodemographic, clinical, and psychosocial measures for the study sample. One hundred and forty-nine participants (31%) reported experiencing a traumatic event during their lifetime. Of these individuals, 64 (43%) reported current symptoms. Among symptomatic participants, the majority endorsed symptoms in one category (41%); an approximately equal number endorsed symptoms in 2–4 categories (2: 22%, 3: 19%, 4: 19%). The most frequently experienced symptom was re-experiencing the traumatic event (67%) followed by hyper-arousal (55%), avoidance (50%), and emotional numbing (44%). Overall, 40% reported symptoms persisting for longer than a month at time of interview. Figure 1 shows the prevalence of trauma exposure and current traumatic stress symptoms by age groups and gender.
Table 1.
Sociodemographic, Psychosocial, and Clinical Characteristics of the Native Elder Care Study participants
| No Trauma (n = 337) | Trauma, No Symptoms (n = 85) | Trauma, Current Symptoms (n = 64) | |
|---|---|---|---|
| Mean (SD) or count (%) | |||
| Age (years) | 70.7 (9.4) | 68.3 (9.8) | 66.5 (9.1) |
| Gender | |||
| Male | 111 (32%) | 37 (43%) | 25 (39%) |
| Female | 226 (67%) | 48 (56%) | 39 (60%) |
| Marital status | |||
| Single | 13 (3%) | 2 (2%) | 2 (3%) |
| Married/life partner | 139 (41%) | 51 (60%) | 36 (56%) |
| Divorced/widowed | 183 (54%) | 32 (37%) | 24 (37%) |
| Attended Indian Boarding School | |||
| No | 201 (59%) | 61 (71%) | 40 (62%) |
| Yes | 131 (38%) | 24 (28%) | 24 (37%) |
| Education | |||
| <High school | 132 (39%) | 24 (28%) | 25 (39%) |
| High school graduate or equivalent | 112 (33%) | 24 (28%) | 19 (29%) |
| Some college or more | 92 (27%) | 37 (43%) | 20 (31%) |
| Income | |||
| <$15,000 | 72 (21%) | 9 (10%) | 16 (25%) |
| $15,000 to $24,999 | 81 (24%) | 17 (20%) | 18 (28%) |
| ≥$25,000 | 92 (27%) | 37 (44%) | 17 (26%) |
| Physical health | |||
| Cardiovascular disease | 90 (27%) | 21 (25%) | 24 (38%) |
| Chronic pain | 189 (56%) | 48 (57%) | 50 (78%) |
| Hypertension | 197 (59%) | 54 (64%) | 43 (67%) |
| Diabetes | 142 (42%) | 35 (41%) | 29 (45%) |
| Mental health | |||
| Depressive symptomatology (CESD) | 5.9 (7.5) | 5.5 (6.7) | 13.6 (12.2) |
| Current alcohol user | 30 (9%) | 16 (19%) | 5 (8%) |
| Current tobacco user | 69 (21%) | 20 (24%) | 13 (20%) |
| Social support | |||
| Overall support | 3.2 (0.7) | 3.3 (0.7) | 3.0 (0.9) |
| Emotional support | 3.0 (0.9) | 3.2 (0.8) | 2.7 (0.9) |
| Tangible support | 3.4 (0.8) | 3.4 (0.9) | 3.2 (0.9) |
| Affectionate support | 3.5 (0.8) | 3.5 (0.8) | 3.1 (1.1) |
| Positive social interaction | 3.3 (1.0) | 3.5 (0.8) | 3.0 (1.1) |
CESD, Center for Epidemiologic Studies Depression Scale.
Figure 1.
Prevalence of trauma exposure and current traumatic stress symptoms by age groups.
As shown in Table 2, exposure to traumatic events was not associated with overall social support or with any social support subscale. Conversely, we found a significant association between traumatic stress and overall social support and all subscales except tangible support. Each additional unit of social support was associated with a 27% lower probability of traumatic stress, adjusting for age, gender, education, and boarding school attendance. We observed similar directions and magnitudes of effects for all social support subscales except for tangible support, which was not statistically significant. Additional models further adjusting for marital status and income resulted in similar results (change in estimated prevalence ratios <10%). Effect modification by gender was not statistically significant (Trauma exposure p-interaction = .30; Traumatic stress symptoms p-interaction = .77).
Table 2.
Associations of Trauma Exposure and Current Traumatic Stress Symptoms with Perceived Social Support Total and Subscales among Older American Indians
| Trauma Exposurea | Traumatic Stress Symptomsa, b | |||||
|---|---|---|---|---|---|---|
| Prevalence Ratio | 95% CI | p-value | Prevalence Ratio | 95% CI | p-value | |
| Overall | 0.91 | (0.77, 1.06) | .215 | 0.73 | (0.58, 0.93) | .011 |
| Emotional support | 0.95 | (0.83, 1.10) | .516 | 0.77 | (0.63, 0.96) | .017 |
| Tangible support | 0.88 | (0.77, 1.00) | .061 | 0.89 | (0.70, 1.13) | .328 |
| Affectionate support | 0.89 | (0.78, 1.03) | .123 | 0.75 | (0.61, 0.92) | .006 |
| Positive social interaction | 0.96 | (0.84, 1.10) | .586 | 0.78 | (0.65, 0.94) | .008 |
Estimated from logistic regression model using marginal standardization, controlling for age, gender, education, and attendance at Indian boarding school.
Traumatic stress symptoms defined as having one or more self-reported traumatic symptoms.
Table 3 reveals that traumatic stress was significantly related to cardiovascular disease and chronic pain, but not hypertension or diabetes. Those with traumatic stress had a 7.6 mean increase in depression symptoms as measured by the CESD. Symptomatic participants also consumed 0.70 fewer alcoholic beverages per week. The analyses did not support effect modification by social support. Further adjustment for marital status and income did not lead to a 10% or greater change in estimated effect measures.
Table 3.
Association Between Current Traumatic Stress Symptoms and Self-Reported Mental and Physical Health Among Older American Indians
| Prevalence Ratioa | 95% CI | p-Value | p-Interactionc | |
|---|---|---|---|---|
| Cardiovascular disease | 1.640 | (1.204, 2.234) | .002 | .378 |
| Chronic pain | 1.314 | (1.158, 1.492) | <.001 | .672 |
| Hypertension | 1.177 | (0.993, 1.394) | .060 | .644 |
| Diabetes | 1.008 | (0.753, 1.348) | .959 | .378 |
| Smoking | 0.776 | (0.473, 1.274) | .316 | .480 |
| Mean Differenceb | 95% CI | p-value | p-interactionc | |
|---|---|---|---|---|
| Alcoholic drinks per week | −0.698 | (−1.174, −0.223) | .004 | .319 |
| CESD (Depression symptomology) | 7.600 | (4.127, 11.074) | <.001 | .909 |
Models estimated using estimated from log-binomial generalized estimating equations adjusting for age, gender, education, and Indian boarding school attendance.
Models estimated using estimated from linear generalized estimating equations adjusting for age, gender, education, and Indian boarding school attendance.
p-value from the test of effect modification in a model additionally adjusting for social support and its interaction with traumatic stress symptoms.
Table 4 presents coefficients for product terms assessing modification of effects in the previous analyses by gender. We found strong effect modification by gender in the CESD analyses. The gender-difference in CESD mean was 7.9 (95% CI: 4.1, 11.1). Adjustment of this product term negated the previously evident association in men to a mean difference of 2.6 (95% CI: −1.2, 6.4). A borderline significant result was found relating gender to chronic pain suggesting that men had a greater prevalence ratio of chronic pain for traumatic symptoms than women, with the effect for women being 0.8 that of men (95% CI: 0.7, 1.0). We did not find any other gender interactions.
Table 4.
Interaction between Gender and Current Traumatic Stress Symptoms for Self-Reported Mental and Physical Health Among Older American Indians
| Prevalence Ratioa | 95% CI | p-Interaction | |
|---|---|---|---|
| Cardiovascular disease | 0.913 | (0.493, 1.693) | .773 |
| Chronic pain | 0.835 | (0.677, 1.031) | .094 |
| Hypertension | 1.076 | (0.727, 1.594) | .713 |
| Diabetes | 0.963 | (0.530, 1.752) | .903 |
| Smoking | 3.032 | (0.719, 12.785) | .131 |
| Mean Differenceb | 95% CI | p-Interaction | |
|---|---|---|---|
| Alcoholic drinks per week | 0.398 | (−0.562, 1.358) | .417 |
| CESD (Depression symptomology) | 7.890 | (1.518, 14.262) | .015 |
Models estimated using estimated from log-binomial generalized estimating equations adjusting for age, gender, education, and Indian boarding school attendance.
Models estimated using estimated from linear generalized estimating equations adjusting for age, gender, education, and Indian boarding school attendance.
Discussion
This is the first study to investigate the prevalence of trauma exposure, related symptoms, and their association with social support and health among older American Indians. Our results suggest that lifetime trauma exposure is lower compared to younger American Indians and that individuals reporting traumatic stress perceive less social support, do not drink as much, yet report worse health than absent traumatic stress. Specifically, the risk of traumatic stress decreases as social support increases, including emotional support, affectionate support, and positive social interactions. In addition, symptomatic participants had greater prevalence of cardiovascular disease and chronic pain. Symptomatic women reported more symptoms of depression.
The prevalence of traumatic experience was much lower than expected (31% in our study compared to 64–81% in previous studies with younger American Indians). One explanation for this might be that the probing question was not detailed enough to elicit all possible traumatic events that participants had experienced during their lifetime. A second possible explanation relates to the interviewers living within the community of the participants. While this provides many benefits, including an added level of trust and understanding in general, there is the potential of response bias related to the personal nature and possibly perceived stigma with reporting traumatic experiences. A third explanation may be that participants’ perceptions of the nature of trauma changed over time. As people accumulate more life experiences and survive, they may not consider earlier events to have been traumatic (Owens, Baker, Kasckow, Ciesla, & Mohamed, 2005). Lastly, it is possible that the sample reflected a survivorship bias. Given the association of traumatic stress with poorer health, participants who experienced trauma and related stress symptoms may not have lived long enough to be part of this study (Owens et al., 2005). A nationally representative sample found the prevalence rate of lifetime PTSD was significantly lower at 2.5% in those 60 years of age and older compared to 9.2% in the 45–59 age group (Kessler et al., 2005). Moreover, the exclusion criteria may have screened out participants who had experienced traumatic events, such as those in nursing homes or those with dementia, though those excluded for these reasons were minimal.
This study extends our knowledge of trauma, related symptoms, their health consequences, and the buffering effects of social support among older American Indians. Consistent with previous research among younger American Indians (Bassett, Buchwald et al., 2014), approximately 40% of the older American Indians in this study who reported experiencing a traumatic event endorsed current traumatic stress symptoms. In this study, symptomatic participants perceived less social support available to them, but the cross-sectional nature of the data collection does not permit us to determine the directionality of this relationship.
Consistent with prior research (Green & Kimerling, 2004), traumatic stress related to adverse health outcomes, including cardiovascular disease, chronic pain, and depression. As hypothesized, the increase in depressive symptomology was attributable to women with current traumatic stress. There was no statistically significant difference between men with and without current traumatic stress. Contrary to our hypothesis, we did not find higher alcohol consumption for men with current traumatic stress symptoms. We did not find gender related to alcohol consumption and yet we found those with current traumatic stress consumed less alcohol than those without traumatic stress.
One explanation for those experiencing traumatic stress consuming fewer alcoholic beverages per week may relate to the symptoms experienced. While increased alcohol use is frequently discussed as a means of self-medicating traumatic stress symptoms, that relation is strongest with symptoms of emotional numbing (Jakupcak et al., 2010). Hyper-arousal tends to relate to activation of the sympathetic nervous system to allow the individual to be constantly “on guard” (Sherin & Nemeroff, 2011). Multiple alcoholic drinks are associated with inhibition of the sympathetic nervous system and include slowed thinking and reaction times, which can be counterintuitive for someone “desiring” hyper-arousal. Another possible explanation is that participants reported less alcohol consumption due to response bias in favor of perceived social desirability to drink less or not at all. A third explanation is related to the smaller number of men in our sample, as men in the general population who experience PTSD are at risk for substance abuse (Kessler et al., 2005; Tolin & Foa, 2006). This finding may be related to lack of survivorship for males with traumatic stress and higher drinking.
Social support related to experiencing symptoms associated with exposure to a traumatic event. We found a relation between traumatic symptoms and social support as well as between traumatic symptoms and adverse health outcomes. However, the association between traumatic symptoms and health did not appear to be moderated by social support. Future research should consider how social support might be activated earlier in this process as a protective factor prior to symptom onset or if social support could aid in traumatic stress symptom recovery.
This large sample of Native elders, a difficult-to-reach population, was assembled through a collaborative process of tribal participatory research (Goins et al., 2011). Sampling randomly from the tribal rolls minimized selection bias and allowed for more confidence in the findings than typically is the case in studies within American Indian populations. Nonetheless, the data are cross-sectional, precluding causal inference. Many of the self-reported health conditions in our analyses have been shown to correlate well with medical records (L. M. Martin et al., 2000; Okura et al., 2004), although the accuracy of self-report varies by the type of condition (L. M. Martin et al., 2000). Important data related to trauma were not collected; notably, the number of exposures, type(s) of trauma, and year(s) of occurrence, thus not allowing for more nuanced analyses incorporating these characteristics. In this sample, 37% of older American Indians attended Indian boarding school, but this was not predictive of current traumatic stress. In addition, historical or inter-generational traumas are hard to conceptualize and quantify and are not captured within our results.
Older American Indians are rapidly growing in number and will triple in the next 30 years (Ortman et al., 2014) We can no longer neglect the circumstances that affect the quality of their lives, nor the forces with which they struggle to overcome adversities that threaten to compromise their health. Trauma and its consequences are a part of the discourse in Native communities and among older adults generally. It is time to bring these conversations together.
Funding
This work was supported by the National Institute on Aging at the National Institutes of Health (P30AG015297 to S. Manson and K01AG022336 to R. T. G.).
Acknowledgements
M.T. conceptualized and designed study, drafted manuscript, interpreted results, and managed submission process. D.B. conceptualized and designed study and assisted with drafting and revisions of the manuscript. C.B.-L. conceptualized and designed study and assisted with drafting and revisions of manuscript. A.O. conceptualized and designed study, provided statistical expertise, analyzed, and interpreted data. S.M.M. refined research conceptualization and provided critical revision of the manuscript. R.T.G. conceptualized and designed study, provided data and managed Tribal IRB process.
References
- American Psychiatric Association.(2013). Diagnostic and statistical manual of mental disorders (5th ed.). Washington, DC: American Psychiatric Association. [Google Scholar]
- Aragon T. J. (2017). Epitools: Epidemiology Tools. R package version 0.5–9 Retrieved from https://CRAN.R-project.org/package=epitools.
- Bassett D. Buchwald D. & Manson S (2014). Posttraumatic stress disorder and symptoms among American Indians and Alaska Natives: A review of the literature. Social Psychiatry and Psychiatric Epidemiology, 49, 417–433. doi:10.1007/s00127-013-0759-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bassett D. R., Nelson L., Rhoades D. A., Krantz E. M., & Omidpanah A (2014). A national study of social networks and perceptions of health among urban American Indian/Alaska Natives and non-Hispanic Whites. Journal of Biosocial Science, 46, 556–559. doi:10.1017/S0021932013000679 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beals J., Belcourt-Dittloff A., Garroutte E. M., Croy C., Jervis L. L., Whitesell N. R.,… AI-SUPERFP Team. (2013). Trauma and conditional risk of posttraumatic stress disorder in two American Indian reservation communities. Social Psychiatry and Psychiatric Epidemiology, 48, 895–905. doi:10.1007/s00127-012-0615-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beals J. Novins D. K. Whitesell N. R. Spicer P. Mitchell C. M. & Manson S. M (2005). Prevalence of mental disorders and utilization of mental health services in two American Indian reservation populations: mental health disparities in a national context. The American Journal of Psychiatry, 162, 1723–1732. doi:10.1176/appi.ajp.162.9.1723 [DOI] [PubMed] [Google Scholar]
- Brewin C. R. Andrews B. & Valentine J. D (2000). Meta-analysis of risk factors for posttraumatic stress disorder in trauma-exposed adults. Journal of Consulting and Clinical Psychology, 68, 748–766. doi:10.1037/0022-006X.68.5.748 [DOI] [PubMed] [Google Scholar]
- Colman R. A. & Widom C. S (2004). Childhood abuse and neglect and adult intimate relationships: a prospective study. Child Abuse & Neglect, 28, 1133–1151. doi:10.1016/j.chiabu.2004.02.005 [DOI] [PubMed] [Google Scholar]
- Colmant S., Schultz L., Robbins R., Ciali P., Dorton J., & Rivera-Colmant Y (2004). Constructing meaning to the Indian boarding school experience. Journal of American Indian Education, 43(3), 22–40. [Google Scholar]
- Community Translational Science Team.(2016). Building a Public Health Model for Promoting Emotional Well-Being. (Policy Report). Los Angeles, CA: University of California Los Angeles. [Google Scholar]
- Conte K. P. Schure M. B. & Goins R. T (2015). Correlates of social support in older American Indians: The Native Elder Care Study. Aging & Mental Health, 19, 835–843. doi:10.1080/13607863.2014.967171 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ditlevsen D. N. & Elklit A (2010). The combined effect of gender and age on post traumatic stress disorder: Do men and women show differences in the lifespan distribution of the disorder?Annals of General Psychiatry, 9, 32 doi:10.1186/1744-859X-9-32 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galovski T., & Lyons J. A (2004). Psychological sequelae of combat violence: A review of the impact of PTSD on the veteran’s family and possible interventions. Aggression and Violent Behavior, 9, 477–501. doi:10.1016/S1359-1789(03)00045-4 [Google Scholar]
- Garrett M. D., Baldridge D., Muus K., Baker-Demaray T., Benson W. F., & McGuire L. C (2010). Native migration: In search of the missing cohorts. American Indian and Alaska Native migration and the loss of caregivers in Native communities. Pimatisiwin: A Journal of Aboriginal & Indigenous Community Health, 8, 1–18. [Google Scholar]
- Goins R. T. Garroutte E. M. Fox S. L. Dee Geiger S. & Manson S. M (2011). Theory and practice in participatory research: Lessons from the Native Elder Care Study. The Gerontologist, 51, 285–294. doi:10.1093/geront/gnq130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goins R. T. Innes K. & Dong L (2012). Lower body functioning prevalence and correlates in older American Indians in a southeastern tribe: The Native Elder Care Study. Journal of the American Geriatrics Society, 60, 577–582. doi:10.1111/j.1532-5415.2011.03869.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Green B. L., & Kimerling R (2004). Trauma, posttraumatic stress disorder, and health status. In Schnurr P. P. & Green B. L. (Eds.), Trauma and health: Physical health consequences of exposure to extreme stress (pp. 13–42). Washington, DC: American Psychological Association. [Google Scholar]
- Holt-Lunstad J. Smith T. B. & Layton J. B (2010). Social relationships and mortality risk: A meta-analytic review. PLoS Medicine, 7, e1000316 doi:10.1371/journal.pmed.1000316 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Isaacowitz D. M., Smith T. B., & Carstensen L. L (2003). Socioemotional selectivity and mental health among trauma survivors in old age. Ageing International, 28, 181–199. doi:10.1007/s12126-003-1023-7 [Google Scholar]
- Jacob M. M., Gonzales K. L., Calhoun D., Beals J., Muller C. J., Goldberg J., …, Howard B. V. (2013). Psychological trauma symptoms and Type 2 diabetes prevalence, glucose control, and treatment modality among American Indians in the Strong Heart Family Study. Journal of Diabetes and Its Complications, 27, 553–557. doi:10.1016/j.jdiacomp.2013.07.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jakupcak M. Tull M. T. McDermott M. J. Kaysen D. Hunt S. & Simpson T (2010). PTSD symptom clusters in relationship to alcohol misuse among Iraq and Afghanistan war veterans seeking post-deployment VA health care. Addictive Behaviors, 35, 840–843. doi:10.1016/j.addbeh.2010.03.023 [DOI] [PubMed] [Google Scholar]
- Jervis L. L. Boland M. E. & Fickenscher A (2010). American Indian family caregivers’ experiences with helping elders. Journal of Cross-Cultural Gerontology, 25, 355–369. doi:10.1007/s10823-010-9131-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler R. C., Berglund P., Demler O., Jin R., Merikangas K. R., & Walters E. E (2005). Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey replication. Archives of General Psychiatry, 62, 593–602. doi:10.1001/archpsyc.62.6.593 [DOI] [PubMed] [Google Scholar]
- Kessler R. C. Sonnega A. Bromet E. Hughes M. & Nelson C. B (1995). Posttraumatic stress disorder in the National Comorbidity Survey. Archives of General Psychiatry, 52, 1048–1060. doi:10.1001/archpsyc1995.03950240066012 [DOI] [PubMed] [Google Scholar]
- Lefler L. J., & Belt R (2009). Historical trauma, stress, and diabetes. In Lefler L. J. (Ed.), Under the Rattlesnake: Cherokee Health and Resiliency (pp. 61–78). Tuscaloosa, AL: University of Alabama Press. [Google Scholar]
- Lewinsohn P. M. Seeley J. R. Roberts R. E. & Allen N. B (1997). Center for Epidemiologic Studies Depression Scale (CES-D) as a screening instrument for depression among community-residing older adults. Psychology and Aging, 12, 277–287. doi:10.1037/0882-7974.12.2.277 [DOI] [PubMed] [Google Scholar]
- Limb G. E., Shafer K., & Sandoval K (2014). The impact of kin support on urban American Indian families. Child & Family Social Work, 19, 432–442. doi:10.1111/cfs.12041 [Google Scholar]
- López M. L., & Cooper L (2011). Social support measures review (pp. 1–115). Retrieved from http://www.first5la.org/files/SSMS_LopezCooper_LiteratureReviewandTable_02212011.pdf
- MacPhee D., Fritz J., & Miller-Heyl J (1996). Ethnic variations in personal social networks and parenting. Child Development, 67, 3278–3295. doi:10.1111/j.1467–8624.1996.tb01914.x [Google Scholar]
- Manson S. M., Ackerson L. M., Dick R. W., Baron A. E., & Fleming C. M (1990). Depressive symptoms among American Indian adolescents: Psychometric characteristics of the Center for Epidemiologic Studies Depression Scale (CES-D). Psychological Assessment: A Journal of Consulting and Clinical Psychology, 2, 231 doi:10.1037/1040-3590.2.3.231 [Google Scholar]
- Manson S. M. Beals J. Klein S. A. & Croy C. D;AI-SUPERPFP Team. (2005). Social epidemiology of trauma among 2 American Indian reservation populations. American Journal of Public Health, 95, 851–859. doi:10.2105/AJPH.2004.054171 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin D. & Yurkovich E (2014). “Close-knit” defines a healthy Native American Indian family. Journal of Family Nursing, 20, 51–72. doi:10.1177/1074840713508604 [DOI] [PubMed] [Google Scholar]
- Martin L. M. Leff M. Calonge N. Garrett C. & Nelson D. E (2000). Validation of self-reported chronic conditions and health services in a managed care population. American Journal of Preventive Medicine, 18, 215–218. doi:10.1016/S0749-3797(99)00158-0 [DOI] [PubMed] [Google Scholar]
- Mazzella F., Cacciatore F., Galizia G., Della-Morte D., Rossetti M., Abbruzzese R.,…, Abete P. (2010). Social support and long-term mortality in the elderly: Role of comorbidity. Archives of Gerontology and Geriatrics, 51, 323–328. doi:10.1016/j.archger.2010.01.011 [DOI] [PubMed] [Google Scholar]
- McFarlane A. C. (2010). The long-term costs of traumatic stress: Intertwined physical and psychological consequences. World Psychiatry: official journal of the World Psychiatric Association (WPA), 9, 3–10. doi:10.1002/j.2051-5545.2010.tb00254.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- McPherson-Sexton S. A. (2006). A comprehensive view of post-traumatic stress disorder: Populations, etiology, treatments, and more. Journal of Police Crisis Negotiations, 6, 93–124. doi:10.1300/J173v06n01_06 [Google Scholar]
- Muller C. J. & MacLehose R. F (2014). Estimating predicted probabilities from logistic regression: different methods correspond to different target populations. International Journal of Epidemiology, 43, 962–970. doi:10.1093/ije/dyu029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Okura Y. Urban L. H. Mahoney D. W. Jacobsen S. J. & Rodeheffer R. J (2004). Agreement between self-report questionnaires and medical record data was substantial for diabetes, hypertension, myocardial infarction and stroke but not for heart failure. Journal of Clinical Epidemiology, 57, 1096–1103. doi:10.1016/j.jclinepi.2004.04.005 [DOI] [PubMed] [Google Scholar]
- Olfson M. Guardino M. Struening E. Schneier F. R. Hellman F. & Klein D. F (2000). Barriers to the treatment of social anxiety. The American journal of psychiatry, 157, 521–527. doi:10.1176/appi.ajp.157.4.521 [DOI] [PubMed] [Google Scholar]
- Ortman J. M., Velkoff V. A., & Hogan H (2014). An aging nation: The older population in the United States (pp. 1–28). Retrieved from https://www.census.gov/prod/2014pubs/p25-1140.pdf
- Owens G. P. Baker D. G. Kasckow J. Ciesla J. A. & Mohamed S (2005). Review of assessment and treatment of PTSD among elderly American armed forces veterans. International Journal of Geriatric Psychiatry, 20, 1118–1130. doi:10.1002/gps.1408 [DOI] [PubMed] [Google Scholar]
- R Core Team.(2017). R: A language and environment for statistical computing. In R Foundation for Statistical Computing; Vienna, Austria: Retrieved from https://www.R-project.org/ [Google Scholar]
- Radloff L. S. (1977). The CES-D Scale: A self-report depression scale for research in the general population. Applied Psychological Measurement, 1, 385–401. doi:10.1177/014662167700100306 [Google Scholar]
- Richmond C. A. M., Ross N. A., & Bernier J (2007). Exploring Indigenous concepts of health: The dimensions of Métis and Inuit health. Aboriginal Policy Research: Directions and Outcomes, 4, 3–13. [Google Scholar]
- Richmond C. A. Ross N. A. & Egeland G. M (2007). Social support and thriving health: A new approach to understanding the health of indigenous Canadians. American Journal of Public Health, 97, 1827–1833. doi:10.2105/AJPH.2006.096917 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rigler S. K. Studenski S. Wallace D. Reker D. M. & Duncan P. W (2002). Co-morbidity adjustment for functional outcomes in community-dwelling older adults. Clinical Rehabilitation, 16, 420–428. doi:10.1191/0269215502cr515oa [DOI] [PubMed] [Google Scholar]
- Ritsher J. B., Struening E. L., Hellman F., & Guardino M (2002). Internal validity of an anxiety disorder screening instrument across five ethnic groups. Psychiatry Research, 111, 199–213. doi:10.1016/S0165-1781(02)00135-X [DOI] [PubMed] [Google Scholar]
- Roberts A. L. Gilman S. E. Breslau J. Breslau N. & Koenen K. C (2011). Race/ethnic differences in exposure to traumatic events, development of post-traumatic stress disorder, and treatment-seeking for post-traumatic stress disorder in the United States. Psychological Medicine, 41, 71–83. doi:10.1017/S0033291710000401 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robin R. W. Chester B. Rasmussen J. K. Jaranson J. M. & Goldman D (1997). Prevalence and characteristics of trauma and posttraumatic stress disorder in a southwestern American Indian community. The American Journal of Psychiatry, 154, 1582–1588. doi:10.1176/ajp.154.11.1582 [DOI] [PubMed] [Google Scholar]
- Schnurr P. P., & Green B. L (2004). A context for understanding the physical health consequences of exposure to extreme stress. In Schnurr P. P. & Green B. L. (Eds.), Trauma and health: Physical health consequences of exposure to extreme stress (pp. 3–10). Washington, DC: American Psychological Association. [Google Scholar]
- Schure M. B., & Goins R. T.(2017). Psychometric examination of the Center for Epidemiologic Studies Depression scale with older American Indians: The Native Elder Care Study. American Indian and Alaska Native Mental Health Research, 24(3), 1–13. doi:10.5820/aian.2402.2017.1 [DOI] [PubMed] [Google Scholar]
- Sherbourne C. D., & Stewart A. L (1991). The MOS social support survey. Social Science & Medicine, 32, 705–714. doi:10.1016/0277-9536(91)90150-B [DOI] [PubMed] [Google Scholar]
- Sherin J. E. & Nemeroff C. B (2011). Post-traumatic stress disorder: the neurobiological impact of psychological trauma. Dialogues in Clinical Neuroscience, 13, 263–278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Somervell P. D. Beals J. Kinzie J. D. Boehnlein J. Leung P. & Manson S. M (1993). Criterion validity of the Center for Epidemiologic Studies Depression Scale in a population sample from an American Indian village. Psychiatry Research, 47, 255–266. doi:10.1016/0165-1781(93)90083-S [DOI] [PubMed] [Google Scholar]
- Tolin D. F. & Foa E. B (2006). Sex differences in trauma and posttraumatic stress disorder: a quantitative review of 25 years of research. Psychological Bulletin, 132, 959–992. doi:10.1037/0033-2909.132.6.959 [DOI] [PubMed] [Google Scholar]
- Wesley-Esquimaux C. C., & Smolewski M (2004). Historic trauma and aboriginal healing. Ottawa, ON: Aboriginal Healing Foundation. [Google Scholar]
- Whitesell N. R., Beals J., Crow C. B., Mitchell C. M., & Novins D. K (2012). Epidemiology and etiology of substance use among American Indians and Alaska natives: Risk, protection, and implications for prevention. The American Journal of Drug and Alcohol Abuse, 38, 376–382. doi:10.3109/00952990.2012.694527 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zeileis A. (2004). Econometric computing with HC and HAC covariance matrix estimators, Journal of Statistical Software, 11(10), 1–17. doi:https://doi.org/ttps://doi.org/10.18637/jss.v011.i10 [Google Scholar]