Abstract
Adrenal crisis is an acute life-threatening emergency contributing to the excess mortality that is reported in patients with adrenal insufficiency. The incidence of adrenal crisis is estimated to be 8 per 100 patient years in patients with adrenal insufficiency. Patients with adrenal crisis present systemically unwell with nonspecific signs and symptoms often leading to misdiagnosis and delayed treatment. An adrenal crisis may be the first presentation of adrenal insufficiency or can occur in patients who have been established on glucocorticoid replacement therapy. Infections are the major precipitating factor, but other causes include physical stress such as a surgical procedure or trauma, forgetting or discontinuing glucocorticoid therapy, pronounced physical activity, and psychological stress. The emergency treatment involves prompt recognition and administration of parenteral hydrocortisone, rehydration and management of electrolyte abnormalities. Prevention is centred around patient education. All patients should be educated on stress dosing and parenteral glucocorticoid administration. They should carry a steroid dependency alert card and wear a medical alert bracelet or similar identification. Despite many improvements in the management of patients with adrenal insufficiency, adrenal crisis continues to occur and represents a major source of morbidity, mortality and distress for patients. Improved patient and clinician education and measures to facilitate parenteral hydrocortisone self-administration in impending crisis are central to the management of this life-threatening event.
Keywords: Addison’s disease, adrenal crisis, adrenal insufficiency, cortisol, hydrocortisone
Introduction
Deficiency of the steroid hormones synthesized and secreted by the adrenal gland is associated with significant morbidity and mortality. Three classes of steroid hormone are produced by the adrenal cortex after uptake of precursor cholesterol from the plasma: mineralocorticoids, glucocorticoids and sex steroids. Mineralocorticoids (aldosterone and deoxycorticosterone) are secreted in low amounts (100–150 µg aldosterone/day) from the zona glomerulosa. Aldosterone secretion is principally under the control of the renin–angiotensin–aldosterone system and its action leads to enhanced uptake of sodium in the distal renal tubule following binding to the mineralocorticoid receptor. Glucocorticoids (cortisol and corticosterone) are secreted in larger amounts (10–15 mg cortisol/day)1,2 from the zona fasciculata in response to stimulation by adrenocorticotrophic hormone (ACTH) and have wide-ranging effects mediated by the glucocorticoid receptor.
Primary adrenal insufficiency (PAI) is caused by impairment of function of the adrenal gland itself, most commonly caused by autoimmune-mediated adrenalitis, infection or due to inborn disruption of adrenal cortisol production in congenital adrenal hyperplasia.3 Secondary adrenal insufficiency (SAI) is caused by disruption of the hypothalamic-pituitary-adrenal axis with insufficient stimulation of the adrenal gland due to inadequate secretion or synthesis of ACTH. This is often caused by pituitary diseases/tumours or their subsequent treatment including surgery and radiotherapy.4 However, chronic exogenous glucocorticoid treatment can also impair pituitary regulation of cortisol production, often termed tertiary adrenal insufficiency (Table 1). Conventional treatment of adrenal insufficiency (AI) involves lifelong glucocorticoid replacement therapy.
Table 1.
Causes of adrenal insufficiency.
| Causes | |
|---|---|
| Primary adrenal insufficiency | Autoimmune adrenalitis Infections (tuberculosis, systemic fungal infections, AIDS) Adrenal metastasis (from lung, breast, kidney) (rare), lymphoma involving the adrenals Congenital adrenal hyperplasia Adrenomyeloneuropathy/adrenoleukodystrophy Bilateral adrenal haemorrhage Bilateral adrenalectomy |
| Secondary adrenal insufficiency | Pituitary or metastatic tumour to the pituitary Other cranial tumours (craniopharyngioma, meningioma, germinoma) Central nervous system infection Pituitary surgery or radiation Primary and Secondary hypophysitis Head trauma Pituitary apoplexy/Sheehan’s syndrome Pituitary infiltration (sarcoidosis, histiocytosis) Empty-sella syndrome |
| Drug-induced adrenal insufficiency | Exogenous steroids (glucocorticoid therapy, megestrol acetate, medroxyprogesterone) |
The differentiation between PAI and SAI is crucial as it allows clinicians to target therapy to associated deficiencies. In PAI, all steroid hormones synthesised by the adrenal gland are deficient (aldosterone, cortisol and sex steroids) whereas in SAI only hormones that are predominantly controlled by ACTH (cortisol and sex steroids) are deficient, however, aldosterone replacement is not required as it is controlled by the renin–angiotensin–aldosterone system.
The principles of management of an adrenal crisis are similar in both children and adult patients, however different challenges exist for the paediatric population including higher rates of hypoglycaemia, weight-based dosing and difficult intravenous access. This review focuses on the management and prevention of adrenal crisis in adult patients.
Morbidity and mortality in AI
It has become increasingly evident that, even in patients with treated AI, there continues to be significant morbidity and reduced life expectancy.5–7 Recent data from the European Adrenal Insufficiency Registry8 (including both PAI and SAI patients) found the major causes of death in patients with AI were cardiovascular disease (35%) and infection (15%), supporting previous registry data for patients with PAI.9,10 The EU-AIRE study reported a mortality of 1.5% for patients with SAI. In those patients with SAI who died, 11.1 adrenal crisis per 100 patient years were reported, significantly higher than that has been reported in other cohorts of patients with SAI.11,12 In addition, patients with SAI who died were on higher mean daily doses of hydrocortisone (24.0 ± 7.6 versus 19.3 ± 5.7 mg, p = 0.002), which may reflect the physicians response to repeated adrenal crises, with increased doses of glucocorticoid therapy in an attempt to prevent recurrence of adrenal crisis.
An adrenal crisis is often the first presentation in undiagnosed AI. In a cross-sectional study of both PAI and SAI patients, only 50% of patients were diagnosed within the first 6 months after the onset of symptoms, with 20% of patients reporting symptoms for greater than 5 years before diagnosis.13 Similarly, in a large Norwegian study, approximately 40% of patients with Addison’s disease had a delay in diagnosis of greater than 6 months from the onset of their symptoms, with 64% of the patients diagnosed only after an acute hospital admission.14 This delay in establishment of the diagnosis, attributed to the relative rarity of the condition and the nonspecificity of the presenting symptoms, increases the risk of potentially lethal complications.
Epidemiology of adrenal crisis
Available literature reports a prevalence of adrenal crisis ranging from 5.2 to 8.3 per 100 patient years.12,15 The incidence of adrenal crisis appears to increase with age with one study reporting a rate of 24.3 admissions per million per year in patients aged 60–69 years.16 A postal survey of over 1000 patients with PAI from four countries reported an 8% annual frequency of adrenal crisis.17 A higher frequency was observed in those patients with concomitant health conditions such as type 1 and type 2 diabetes, asthma and premature ovarian failure.17 In a prospective study of more than 400 patients with AI, Hahner and colleagues reported 8.3 adrenal crises per 100 patient-years, with a mortality rate from adrenal crisis of 0.5/100 patient years.15
Definition
The range in prevalence of adrenal crisis reported in the literature is attributed not only to the heterogenous nature of the populations studied, but also complicated by the lack of a universally accepted definition of an adrenal crisis. Definitions differ between expert clinicians and research studies (Table 2). The Endocrine Society guidelines on the diagnosis and treatment of PAI defines an adrenal crisis as a medical emergency with hypotension, abdominal symptoms and laboratory abnormalities requiring emergency treatment.18 Allolio and colleagues describe an adrenal crisis as a major impairment of general health in addition to the demonstration of a clinical improvement following parenteral glucocorticoids.19 They also proposed a grading system using levels of hospitalization to denote adrenal crisis severity ranging from grade 1 (outpatient care only) to grade 4 (death from adrenal crisis), with or without parenteral glucocorticoid administration.19
Table 2.
Definitions of an adrenal crisis.
| Study | Definition and grading of adrenal crisis |
|---|---|
| Allolio et al. 19 | (A) Major impairment of general health with at least two of the following signs/symptoms: -Hypotension [systolic blood pressure (BP) <100 mmHg] -Nausea or vomiting -Severe fatigue -Fever -Somnolence -Hyponatraemia (⩽132 mmol/l) or hyperkalaemia -Hypoglycaemia (B) Parenteral glucocorticoid (hydrocortisone) administration followed by clinical improvement Grading: Grade 1: outpatient care only Grade 2: hospital care (general ward) Grade 3: admission to intensive care unit Grade 4: death from adrenal crisis (with or without parenteral glucocorticoid administration) |
| Bornstein et al. 18 | A medical emergency with hypotension, marked acute abdominal symptoms and marked laboratory abnormalities, requiring immediate treatment. |
| Paur et al. 20 | An acute deterioration in a patient with adrenal insufficiency. |
| Smans et al. 12 | An acute impairment of general health requiring hospital admission and administration of intravenous saline and glucocorticoids in patients with adrenal insufficiency. |
| Rushworth et al. 21 | An acute deterioration in health that is associated with absolute (systolic BP < 100 mmHg) or relative (systolic BP < 20 mmHg lower than the patients usual BP) hypotension, the features of which resolve following parenteral glucocorticoid administration (demonstrated by a marked resolution of hypotension within 1 h and improvement of clinical symptoms over 2 h) |
Definitions also differ among research studies. Puar et al.20 defined an adrenal crisis as an acute deterioration in a patient with AI, whereas Smans and colleagues defined adrenal crisis as an acute impairment of general health requiring hospitalization and administration of IV saline and glucocorticoids in patients with AI.12 More recently, Rushworth et al. proposed a definition that the authors feel will increase the likelihood that true adrenal crisis events are identified and that other, less-severe episodes of illness are not classified as an adrenal crisis but a milder form of illness.21 Their definition is outlined in Table 2. They also incorporated a list of clinical features such as acute abdominal symptoms, delirium/altered consciousness, pyrexia and hypoglycaemia, in the definition to assist the clinician in making the correct diagnosis.
Pathophysiology
The pathophysiology of adrenal crisis formation is not fully understood. In an adrenal crisis a mismatch occurs between the need and availability of cortisol. During the acute phase of an illness, serum cortisol concentrations correlate to the severity of the illness in patients with presumed normal hypothalamic–pituitary–adrenal (HPA) axis. Similarly in perioperative patients, serum cortisol levels often reflect the degree of surgical stress.22,23 Elevated cortisol concentrations in acute stress have traditionally been attributed to stress-induced activation of the HPA axis with ACTH-driven cortisol secretion, however studies have shown that critically ill patients have paradoxically low ACTH levels and exhibit impaired cortisol clearance which contributes to the observed hypercortisolism.24 Exposure to stressors cause the release of inflammatory cytokines such as tumour necrosis factor α (TNFα) and interleukins 1 and 6, which activate the HPA axis.25,26 The increased cortisol secretion subsequently exercises an anti-inflammatory effect by reducing leukocytic responses, and blocking cytokine production. Therefore, this cell-mediated immunity is diminished in situations of cortisol deficiency.
Another complicating factor is that cortisol is known to be important in the conversion of norepinephrine to epinephrine by phenylethanolamine N-methyltransferase (PNMT). In patients with AI, the decrease in intra-adrenal cortisol concentrations leads to a decrease in catecholamine synthesis (as a result of decrease PNMT activity).27 This was shown in a group of patients with CAH, where epinephrine levels were reduced at baseline and rose to only 20% of normal after exercise compared with sex- and body mass index (BMI)-matched healthy controls.28 Subsequent replacement glucocorticoid had little if any impact on circulating epinephrine levels in these patients.29 No replacement strategy for epinephrine deficiency is available, therefore it may be helpful for patients with AI to combine hydrocortisone with a small carbohydrate-rich meal before prolonged exercising.30
Aetiology and risk factors
An adrenal crisis may occur in a number of different settings. It may be the primary presentation in patients with undiagnosed AI or in patients with chronic AI, who are replaced with glucocorticoids, but experience an intercurrent infection or an acute, major stress, and there is a discrepancy in their glucocorticoid dose and their increased glucocorticoid requirements during these events. A recent systematic review of more than 2900 patients undergoing surgery revealed that the perioperative cortisol response is influenced by patient specific factors in addition to the type of surgery performed.31 It is important to consider these factors when deciding the perioperative steroid coverage in patients with AI.
As PAI patients are also deficient in mineralocorticoids, which are key regulators of blood pressure and electrolyte balance, PAI patients are often at a higher risk of adrenal crisis compared with patients with SAI and may develop more severe adrenal crisis.32 Another reason for potentially different rates of adrenal crisis in patients with AI is the relative degree of glucocorticoid deficiency. Many patients with PAI have negligible cortisol synthesis whereas some patients with SAI still have some cortisol synthesis (but insufficient amounts to maintain health and therefore require replacement therapy).
An adrenal crisis may occur in the setting of an acute insult to the adrenal or pituitary gland such as an infarction or haemorrhage.33–35 Unmasking of SAI may occur in patients who are abruptly withdrawn from supraphysiologic doses of glucocorticoid, which includes not only oral but also inhaled steroids.36 An adrenal crisis can occur in the setting of bilateral adrenal metastasis37,38 and secondary to immunomodulator anticancer agents.39 The addition of concomitant medication that alters cortisol metabolism could potentially precipitate an adrenal crisis.40 A well-recognized complication in clinical practice is the occurrence of an adrenal crisis following the initiation of thyroxine replacement in a patient with untreated AI as thyroxine increases corticosteroid metabolism.41 In patients with hypopituitarism, growth hormone replacement therapy can also unmask AI.42 Medications that induce the drug-metabolizing enzyme CYP3A4 including carbamazepine, Hypericum perforatum (St. John’s wort), mitotane and rifampicin also increase cortisol clearance, necessitating a higher replacement dose.40 It is important that this effect is anticipated prior to initiation and an appropriate daily glucocorticoid dose is given, and monitored thereafter to ensure adequate glucocorticoid replacement. Treatment of PAI with dexamethasone alone, without concurrent fludrocortisone, can also trigger an adrenal crisis as dexamethasone has no mineralocorti-coid activity.
In retrospective and prospective studies the most frequent precipitating causes of adrenal crisis are gastroenteritis (35–45%) and fever (17–24%),15,17,43 but other stressful events such as trauma,35 surgery,44 dental procedures45 and major psychological distress46 can cause adrenal crisis.
In their prospective study of PAI patients, Hahner et al. found that emotional stress was identified as a triggering factor in 30% of adrenal crisis, as frequently as gastrointestinal symptoms or infections (35% and 32%, respectively). The ability for psychological stress to trigger an adrenal crisis is under recognized and patients are often advised that this does not lead to adrenal crisis, which based on the above data is incorrect. Similarly, in a longitudinal study of patients across all ages with CAH, gastrointestinal and upper respiratory tract infections were the two most common precipitating events for adrenal crises and hospitalizations.47 A history of a previous adrenal crisis is the most important risk factor for further crises, with approximately threefold higher risk observed in the prospective study by Hahner et al.15
Clinical presentation and investigations
The predominant clinical features of adrenal crisis include hypotension and hypovolaemia (in patients with PAI due to concomitant mineralocorticoid deficiency), but patients often have nonspecific symptoms, such as anorexia, nausea, vomiting, abdominal pain, fatigue, lethargy, fever or altered consciousness (Table 3). The insidious onset of symptoms often results in a delay in diagnosis. One study of adrenal crisis admissions reported that 66.9% of adrenal crisis patients (n = 337) had visited the hospital within 90 days before the onset of the crisis.48 Hypotension (particularly postural hypotension) occurs secondary to hypovolemia, but also due to hypocortisolism hence, if AI is not suspected, it may be refractory to parenteral fluids and inotropes. In PAI, hyponatraemia and hyperkalaemia can occur as a consequence of mineralocorticoid deficiency. The principal mechanism of hyponatraemia in SAI is reduction in the osmolar threshold stimulating vasopressin secretion secondary to hypocortisolism and the inability to excrete a free water load.49 The hyponatraemia that occurs in SAI is indistinguishable clinically from the syndrome of inappropriate antidiuresis (SIAD). In a prospective cohort of patients with SIAD, the incidence of SAI was 2.4%.50 Other biochemical features that can present in an adrenal crisis include renal impairment secondary to hypovolaemia, hypoglycaemia and, rarely, hypercalcaemia, which is due to decreased renal excretion of calcium and increased bone resorption.
Table 3.
Clinical features and routine laboratory findings in adrenal crisis.
| Symptoms | Signs | Routine laboratory tests |
|---|---|---|
| Severe weakness | Hypotension | Hyponatraemia |
| Syncope | Abdominal tenderness/guarding | Hypoglycaemia |
| Nausea and vomiting | Fever | Hypercalcaemia |
| Abdominal pain | Hyperpigmentation (PAI) | Normocytic anaemia |
| Back pain | Altered GCS, delirium | Acute renal failure |
| Confusion | Hyperkalaemia (PAI) |
GCS, Glasgow Coma Scale; PAI, primary adrenal insufficiency.
Treatment
Emergency management
Expert consensus statements and guidelines exist on the management of AI and above all, emphasis is placed on the importance of prompt initiation of treatment in patients with suspected adrenal crisis.18,51,52 Diagnostic investigations should not delay treatment. A blood sample could be drawn immediately for serum cortisol and ACTH if suspected, but treatment should be started without waiting for assay results. In an acutely unwell patient, confirmation of diagnosis can be safely established once the patient has clinically recovered.
Emergency treatment includes immediate administration of parenteral hydrocortisone via a bolus injection of intravenous (IV) hydrocortisone 100 mg, or intramuscular (IM) hydrocortisone, pending IV access. This bolus should be followed by 200 mg of hydrocortisone per 24 h, either via continuous IV infusion or alternatively in doses of 50 mg of hydrocortisone per IV/IM injection every 6 h.18,51 A continuous infusion of hydrocortisone, produces a steady-state insert of cortisol concentration.53 Some authors including the Addison’s Disease Self-help Group (ADSHG) adrenal crisis guidelines recommend higher treatment doses of 100 mg of hydrocortisone every 6 h (after the first initial bolus) in the acute setting. However, several studies support that 50 mg q.d.s. IV/IM or 200 mg/24 h provides adequate cortisol concentrations to treat the acute cortisol deficiency. Jung et al. showed in healthy individuals, whose endogenous cortisol was suppressed by dexamethasone, that 50 mg of IV hydrocortisone achieved a mean 30 min total plasma cortisol of 2450 nmol/l.54 This level is greater than that reported in septic shock (mean, 880 nmol/l)55 or following major surgery such as coronary artery bypass surgery (median, 744 nmol/l).56 Similarly, recent data from Bancos et al.31 showed that patients undergoing grade III highly invasive surgery had a 3.5-fold higher cortisol output than healthy, unstressed individuals; however, the mean cortisol concentrations were not greater than 1000 nmol/l in the first 24 h.
In a patient with PAI, hydrocortisone doses of >50 mg/day have sufficient action at the mineralocorticoid receptor, therefore additional mineralocorticoid therapy is not required at this point.
Prompt rehydration should be initiated with isotonic saline; a rapid IV infusion of 1 litre of isotonic saline within the first hour or 5% glucose in isotonic saline, followed by continuous IV isotonic saline guided by individual patient needs (usually 4–6 litres in 24 hours, while monitoring for fluid overload in high-risk patients, i.e. in patients with heart failure, renal impairment and in elderly patients).51 The patients should be managed in a critical care environment with close monitoring of vital signs and regular assessment of serum electrolytes should be performed to avoid rapid over correction of hyponatraemia. Patients may also require parenteral glucose therapy if hypoglycaemic. Treatment for the precipitant of the adrenal crisis should be also be instigated, if necessary, as well as venous thromboembolism prophylaxis, and consideration of a short course of proton pump inhibitor therapy to prevent potential gastric stress ulceration.
Urgent review by the endocrinology team is recommended to guide safe tapering of hydrocortisone to maintenance doses, in addition to guiding further investigations in a patient with unknown AI. If the patient is clinically stable, tapering of hydrocortisone to replacement doses can be initiated usually within 24–72 h. In patients with PAI, mineralocorticoid administration should be started as soon as total daily hydrocortisone dose is lower than 50 mg/24 h. During an admission with an adrenal crisis, the physician should take the opportunity to address the context of the acute medical admission and attempt to identify any missed opportunities that could have prevented the adrenal crisis and educate the patient and fellow clinicians further.
Prevention strategies
Patient education
Patient education is the most important component in the prevention of adrenal crisis. After an acute presentation with an adrenal crisis, a regular review by an endocrinologist, in the months following diagnosis and then 6–12 months thereafter, is recommended. Patients need to be empowered to make relevant adjustments to their own medication, in the absence of their treating physician, and to adapt their dose according to individual needs. An additional dose of hydrocortisone may be considered in situations of severe and prolonged psychological stress, or prolonged physical exercise.11 Patients on shift work may need to adapt their hydrocortisone dose according to the time of wakefulness. In the case of a hot climate or strong perspiration, it is necessary to increase the fludrocortisone dose (0.1–0.2 mg/day) or the salt intake to compensate.
It is important that patients, caregivers and family members are aware of the symptoms of an impending crisis. It should be reinforced to patients to have a low threshold to administer a hydrocortisone emergency injection and seek urgent medical care if they develop these symptoms. Patients are encouraged to pack extra hydrocortisone when travelling abroad, including a letter from their endocrinologist to allow the emergency kit to go through customs.
Steroid alerts
Guidelines recommend that all patients should carry steroid emergency cards.18,51 An emergency steroid wallet card that is credit-card sized is available (Figure 1). It contains advice on the emergency treatment of an adrenal crisis and has been authored by expert endocrinologists in the field of adrenal disease and endorsed by the European Society of Endocrinology, the International Society of Endocrinology and a number of patient support groups. It is available in hard copy form and is sent free to members of certain patient support groups (including the ADSHG) upon sign up. The patient should keep the steroid emergency card with them at all times and show it to any healthcare professional they are attending. Medical alert identification wristbands/necklaces are also necessary to alert medical professionals of the need for immediate parenteral glucocorticoid treatment in the case of an adrenal crisis and reduced consciousness.
Figure 1.
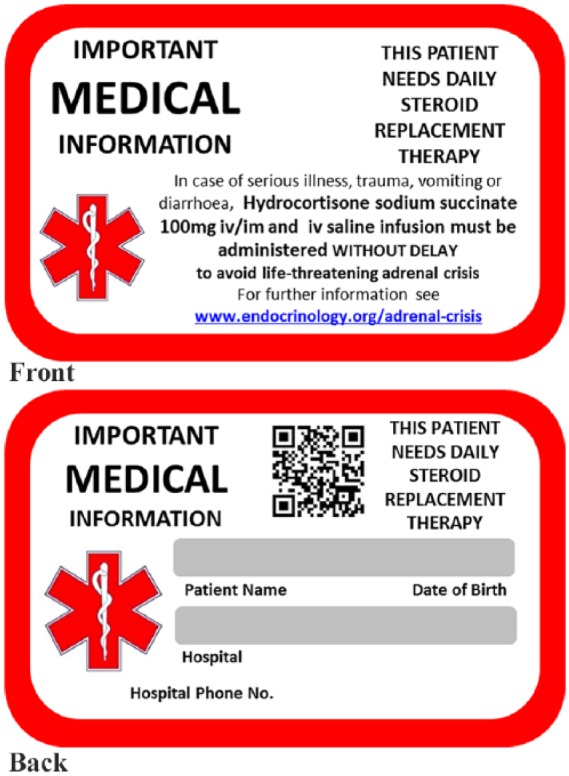
Adrenal emergency steroid card.
Permission to reprint granted by the Addisons Disease Self-Help Group, addisonsdisease.org.uk
Stress dosing advice: the ‘sick day’ rules
Education of patients and partner/family members regarding symptom awareness and the correct adjustment of glucocorticoid replacement dose is imperative. The following advice should be given.18
Sick day rule 1: need to double the routine oral glucocorticoid dose when the patient experiences fever or illness requiring bed rest; when requiring antibiotics for an infection; or before a small outpatient procedure (e.g. dental work). The patient should ensure that they have an additional supply of hydrocortisone tablets so that they can double their dose for at least 7 days if required.
Sick day rule 2: need to inject a glucocorticoid preparation IM/IV in the case of severe illness, trauma, persistent vomiting, when fasting for a procedure (colonoscopy) or during surgical intervention.
Inject 100 mg hydrocortisone IV, IM, or subcutaneously followed by 200 mg hydrocortisone per continuous IV infusion, alternatively repeated bolus doses of 50 mg of hydrocortisone (IV or IM) every 6 h.
There are no randomized controlled studies that have evaluated the dose to be given in cases where the requirement for hydrocortisone is increased. Published recommendations therefore rest largely on expert opinion. The Addison’s Clinical Advisory Panel (ACAP), a group of UK Endocrinologists who specialise in adrenal disease, give specific guidance to the ADSHG and physicians on glucocorticoid requirements and recommendations for adjustment for surgical procedures.57
Emergency hydrocortisone kit
Patients should have access to a vial of injectable hydrocortisone, e.g. 100 mg of hydrocortisone sodium succinate, with appropriate needles, syringes and water for injection for reconstitution, available at all times. The affected individual, their partner/spouse and their immediate family members should be trained in parenteral hydrocortisone administration and there are a number of online tutorials to support this education process. They should ensure that their kit is in date at all times and preferably kept with the patient, because a third of adrenal crises occur when the patient is away from home.11 It should be reinforced that this emergency injection does not obviate the necessity to attend for acute medical care and patients are recommended to still attend for emergency medical care.
In a recent prospective study of patients with chronic AI who presented to the emergency room, 62% of those who self-injected glucocorticoid were treated in the outpatient setting, compared with 27% of the patients who received parenteral glucocorticoid from a medical professional (p = 0.008), presumably due to the time interval between showing the emergency card and the injection by a medical professional. However, 84% of the patients in this study did indicate a need for an easier method of self-injection.32
Some patients are fearful of IM injections and subcutaneous administration of hydrocortisone may be more acceptable to patients than the IM approach. Research has demonstrated that while cortisol levels were slower to reach a peak level (greater than 1000 nmol/l) from a subcutaneous injection than following IM injection, it was deemed within an acceptable time limit among patients with a BMI of less than 27 kg/m2 who were not in shock.58 Unfortunately a preloaded syringe of hydrocortisone similar to an EpiPen® is not available but would provide greater potential to reduce the current barriers to hydrocortisone self-injection. Providing patients with emergency phone numbers and contact details for the patient self-help groups can also help ease patient and families anxiety regarding adrenal crisis.
Healthcare professional education
Emergency management of adrenal crisis is standardized, and patients respond well to the recommended therapy, with low mortality rates in hospitalized patients.16 Thus, it is the delay in timely and appropriate treatment that contributes to the mortality associated with adrenal crisis. Studies support the observation that there remains a significant time delay between the time from arrival of emergency medical care until glucocorticoid administration.59 There are also reports of patients having difficulties accessing appropriate and timely treatment.60 In a cross-sectional survey of AI patients, Chapman et al. found that more than 50% were dissatisfied with the level of information they received from their physician about their glucocorticoid medication.61 A German study investigated the knowledge of adrenal crisis across both medical and surgical disciplines in a large university hospital, and reported that only 20 physicians (9.6%) correctly identified all situations requiring hydrocortisone adjustment.62 In addition, internists, paediatricians and neurologists had more knowledge of AI treatment than anaesthesiologists or surgical doctors, who are potentially involved in the perioperative management of patients with AI.
Given the high prevalence of glucocorticoid use for the treatment of various inflammatory conditions, malignancies and after organ transplantation, it is of great clinical relevance to educate physicians about the risk of developing AI. Unfortunately, the risk of AI among patients receiving glucocorticoids is unpredictable. In a recent metanalysis, the percentage of patients with AI varied from 4.2% for nasal corticosteroids to 52.2% for intra-articular corticosteroids.63 The prevention of a potentially life-threatening adrenal crisis in these patients owing to relative cortisol insufficiency at times of minor or major ‘stress’ is of paramount importance. It is clear that improved education of physicians is a key target to reduce death from adrenal crisis in patients with known or suspected AI.
Future prevention and prediction strategies
Therapeutic patient education is recommended by two international consensus statements on the management of PAI.18,64 Therapeutic patient education is an element of nonpharmacological patient management and has been shown to be effective in chronic diseases.65 In the context of AI, it aims to provide more than just information but help patients to acquire and maintain competencies that help them to be more independent, to protect themselves from potentially life-threatening risks linked to their disease. A number of studies of therapeutic education for patients with AI have been published.66–68
One study investigated self-management in 246 patients receiving glucocorticoid replacement therapy (PAI and SAI) before and 6 months after an education group meeting. They found significantly more participants (p ⩽ 0.005) gave the correct answers to how to act in different situations. Moreover, the use of self-management tools, such as having a medicine passport (p = 0.007) or medical alert identifier (p = 0.0007), increased.68 However, no program has yet been able to demonstrate whether there is a consequent decrease in the incidence or severity of adrenal crises.
It is well established that patients with AI have impaired quality of life (QoL), with current replacement regimens failing to restore subjective health status in affected individuals.69 The Addison’s disease-specific quality of life questionnaire (AddiQoL) was established by the European consortium EURADRENAL to assess health-related QoL in patients with PAI.70
A recent prospective study investigated whether longitudinal AddiQoL scores could identify patents with PAI at higher risk of adrenal crisis.71 They included 110 patients with Addison’s disease who completed the disease-specific AddiQoL and another short questionnaire about adverse events once a month over a period of 10 months. The authors found that those with adrenal crisis (prevalence 10.9/100 patient years in this study) had a wider fluctuation in QoL over time. The subjective pre-crises phase, requiring an increased dose of hydrocortisone replacement, was associated with a lower QoL scores. Self-evaluation by regular identification of health-related QoL via patient diaries or mobile applications may provide a tool to help guide patients to assess their risk of adrenal crisis and indeed prompt physicians to alert patients who report fatigue with their replacement, to the warning signs of impending crisis.
Conclusion
Glucocorticoid replacement therapy has been available for more than 50 years, however adrenal crisis remains a significant cause of death in patients with AI. Improved patient education with an emphasis on stress dosing, medical alert identification and glucocorticoid emergency kits are pivotal in reducing the prevalence of this potentially life-threatening presentation.
Footnotes
Author contribution: All authors contributed to the writing of this manuscript.
Funding: MS has received funding for research from Shire Ltd. RD is funded by the Irish Research Council and the Meath Foundation, Ireland.
Conflict of interest statement: The authors declare that there is no conflict of interest.
ORCID iD: Mark Sherlock  https://orcid.org/0000-0003-4078-624X
https://orcid.org/0000-0003-4078-624X
Contributor Information
Rosemary Dineen, Academic Department of Endocrinology, Beaumont Hospital and the Royal College of Surgeons in Ireland, Dublin, Ireland.
Christopher J Thompson, Academic Department of Endocrinology, Beaumont Hospital and the Royal College of Surgeons in Ireland, Dublin, Ireland.
Mark Sherlock, Department of Endocrinology, Beaumont Hospital and the Royal College of Surgeons in Ireland, Dublin 9, Ireland.
References
- 1. Kerrigan JR, Veldhuis JD, Leyo SA, et al. Estimation of daily cortisol production and clearance rates in normal pubertal males by deconvolution analysis. J Clin Endocrinol Metab 1993; 76: 1505–1510. [DOI] [PubMed] [Google Scholar]
- 2. Esteban NV, Loughlin T, Yergey AL, et al. Daily cortisol production rate in man determined by stable isotope dilution/mass spectrometry. J Clin Endocrinol Metab 1991; 72: 39–45. [DOI] [PubMed] [Google Scholar]
- 3. Bancos I, Hahner S, Tomlinson J, et al. Diagnosis and management of adrenal insufficiency. Lancet Diabetes Endocrinol 2015; 3: 216–226. [DOI] [PubMed] [Google Scholar]
- 4. Grossman AB. Clinical Review#: the diagnosis and management of central hypoadrenalism. J Clin Endocrinol Metab 2010; 95: 4855–4863. [DOI] [PubMed] [Google Scholar]
- 5. Sherlock M, Ayuk J, Tomlinson JW, et al. Mortality in patients with pituitary disease. Endocr Rev 2010; 31: 301–342. [DOI] [PubMed] [Google Scholar]
- 6. Sherlock M, Reulen RC, Alonso AA, et al. ACTH deficiency, higher doses of hydrocortisone replacement, and radiotherapy are independent predictors of mortality in patients with acromegaly. J Clin Endocrinol Metab 2009; 94: 4216–4223. [DOI] [PubMed] [Google Scholar]
- 7. Johannsson G, Skrtic S, Lennernas H, et al. Improving outcomes in patients with adrenal insufficiency: a review of current and future treatments. Curr Med Res Opin 2014; 30: 1833–1847. [DOI] [PubMed] [Google Scholar]
- 8. Quinkler M, Ekman B, Zhang P, et al. Mortality data from the European Adrenal Insufficiency Registry-Patient characterization and associations. Clin Endocrinol (Oxf) 2018; 89: 30–35. [DOI] [PubMed] [Google Scholar]
- 9. Bergthorsdottir R, Leonsson-Zachrisson M, Oden A, et al. Premature mortality in patients with Addison’s disease: a population-based study. J Clin Endocrinol Metab 2006; 91: 4849–4853. [DOI] [PubMed] [Google Scholar]
- 10. Erichsen MM, Lovas K, Fougner KJ, et al. Normal overall mortality rate in Addison’s disease, but young patients are at risk of premature death. Eur J Endocrinol 2009; 160: 233–237. [DOI] [PubMed] [Google Scholar]
- 11. Hahner S, Loeffler M, Bleicken B, et al. Epidemiology of adrenal crisis in chronic adrenal insufficiency: the need for new prevention strategies. Eur J Endocrinol 2010; 162: 597–602. [DOI] [PubMed] [Google Scholar]
- 12. Smans LC, Van der Valk ES, Hermus AR, et al. Incidence of adrenal crisis in patients with adrenal insufficiency. Clin Endocrinol (Oxf) 2016; 84: 17–22. [DOI] [PubMed] [Google Scholar]
- 13. Bleicken B, Hahner S, Ventz M, et al. Delayed diagnosis of adrenal insufficiency is common: a cross-sectional study in 216 patients. Am J Med Sci 2010; 339: 525–531. [DOI] [PubMed] [Google Scholar]
- 14. Erichsen MM, Lovas K, Skinningsrud B, et al. Clinical, immunological, and genetic features of autoimmune primary adrenal insufficiency: observations from a Norwegian registry. J Clin Endocrinol Metab 2009; 94: 4882–4890. [DOI] [PubMed] [Google Scholar]
- 15. Hahner S, Spinnler C, Fassnacht M, et al. High incidence of adrenal crisis in educated patients with chronic adrenal insufficiency: a prospective study. J Clin Endocrinol Metab 2015; 100: 407–416. [DOI] [PubMed] [Google Scholar]
- 16. Rushworth RL, Torpy DJ. A descriptive study of adrenal crises in adults with adrenal insufficiency: increased risk with age and in those with bacterial infections. BMC Endocr Disord 2014; 14: 79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. White K, Arlt W. Adrenal crisis in treated Addison’s disease: a predictable but under-managed event. Eur J Endocrinol 2010; 162: 115–120. [DOI] [PubMed] [Google Scholar]
- 18. Bornstein SR, Allolio B, Arlt W, et al. Diagnosis and Treatment of Primary Adrenal Insufficiency: An Endocrine Society Clinical Practice Guideline. J Clin Endocrinol Metab 2016; 101: 364–389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Allolio B. Extensive expertise in endocrinology. Adrenal crisis. Eur J Endocrinol 2015; 172: R115–R124. [DOI] [PubMed] [Google Scholar]
- 20. Puar TH, Stikkelbroeck NM, Smans LC, et al. Adrenal crisis: still a deadly event in the 21st century. Am J Med 2016; 129: 339.e331–339. [DOI] [PubMed] [Google Scholar]
- 21. Rushworth RL, Torpy DJ, Falhammar H. Adrenal crises: perspectives and research directions. Endocrine 2017; 55: 336–345. [DOI] [PubMed] [Google Scholar]
- 22. Chernow B, Alexander HR, Smallridge RC, et al. Hormonal responses to graded surgical stress. Arch Intern Med 1987; 147: 1273–1278. [PubMed] [Google Scholar]
- 23. Mohler JL, Michael KA, Freedman AM, et al. The serum and urinary cortisol response to operative trauma. Surg Gynecol Obstet 1985; 161: 445–449. [PubMed] [Google Scholar]
- 24. Van den Berghe G, Boonen E, Walker BR. Reduced cortisol metabolism during critical illness. N Engl J Med 2013; 369: 481. [DOI] [PubMed] [Google Scholar]
- 25. Steensberg A, Fischer CP, Keller C, et al. IL-6 enhances plasma IL-1ra, IL-10, and cortisol in humans. Am J Physiol Endocrinol Metab 2003; 285: E433–E437. [DOI] [PubMed] [Google Scholar]
- 26. Turnbull AV, Rivier CL. Regulation of the hypothalamic-pituitary-adrenal axis by cytokines: actions and mechanisms of action. Physiol Rev 1999; 79: 1–71. [DOI] [PubMed] [Google Scholar]
- 27. Stewart PM. Adrenal replacement therapy: time for an inward look to the medulla? J Clin Endocrinol Metab 2004; 89: 3677–3678. [DOI] [PubMed] [Google Scholar]
- 28. Weise M, Mehlinger SL, Drinkard B, et al. Patients with classic congenital adrenal hyperplasia have decreased epinephrine reserve and defective glucose elevation in response to high-intensity exercise. J Clin Endocrinol Metab 2004; 89: 591–597. [DOI] [PubMed] [Google Scholar]
- 29. Weise M, Drinkard B, Mehlinger SL, et al. Stress dose of hydrocortisone is not beneficial in patients with classic congenital adrenal hyperplasia undergoing short-term, high-intensity exercise. J Clin Endocrinol Metab 2004; 89: 3679–3684. [DOI] [PubMed] [Google Scholar]
- 30. Klement J, Hubold C, Cords H, et al. High-calorie glucose-rich food attenuates neuroglycopenic symptoms in patients with Addison’s disease. J Clin Endocrinol Metab 2010; 95: 522–528. [DOI] [PubMed] [Google Scholar]
- 31. Prete A, Yan Q, Al-Tarrah K, et al. The cortisol stress response induced by surgery: a systematic review and meta-analysis. Clin Endocrinol (Oxf) 2018; 89: 554–567. [DOI] [PubMed] [Google Scholar]
- 32. Burger-Stritt S, Kardonski P, Pulzer A, et al. Management of adrenal emergencies in educated patients with adrenal insufficiency-A prospective study. Clin Endocrinol (Oxf) 2018; 89: 22–29. [DOI] [PubMed] [Google Scholar]
- 33. McGowan-Smyth S. Bilateral adrenal haemorrhage leading to adrenal crisis. BMJ Case Rep 2014; 2014 DOI: 10.1136/bcr-2014-204225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Sahin M, Oguz A, Tuzun D, et al. Primary adrenal failure due to antiphospholipid syndrome. Case Rep Endocrinol 2015; 2015: 161497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Ham PB, Cunningham AJ, Mentzer CJ, et al. Traumatic panhypopituitarism resulting in acute adrenal crisis. J Trauma Acute Care Surg 2015; 79: 484–489. [DOI] [PubMed] [Google Scholar]
- 36. Todd GR, Acerini CL, Ross-Russell R, et al. Survey of adrenal crisis associated with inhaled corticosteroids in the United Kingdom. Arch Dis Child 2002; 87: 457–461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Iqbal MS, Hardman J. Addisonian crisis secondary to bilateral adrenal metastases in rectal carcinoma: report of a rare case and literature review. J Gastrointest Cancer 2013; 44: 225–227. [DOI] [PubMed] [Google Scholar]
- 38. Akcay MN, Tekin SB, Akcay G. Addisonian crisis due to adrenal gland metastasis in Hodgkin’s disease. Int J Clin Pract 2003; 57: 840–841. [PubMed] [Google Scholar]
- 39. Trainer H, Hulse P, Higham CE, et al. Hyponatraemia secondary to nivolumab-induced primary adrenal failure. Endocrinol Diabetes Metab Case Rep 2016; 2016: 16-0108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Dineen R, Stewart PM, Sherlock M. Factors impacting on the action of glucocorticoids in patients receiving glucocorticoid therapy. Clin Endocrinol (Oxf). Epub ahead of print 24 September 2018. DOI: 10.1111/cen.13837. [DOI] [PubMed] [Google Scholar]
- 41. Iranmanesh A, Lizarralde G, Johnson ML, et al. Dynamics of 24-hour endogenous cortisol secretion and clearance in primary hypothyroidism assessed before and after partial thyroid hormone replacement. J Clin Endocrinol Metab 1990; 70: 155–161. [DOI] [PubMed] [Google Scholar]
- 42. Agha A, Monson JP. Modulation of glucocorticoid metabolism by the growth hormone - IGF-1 axis. Clin Endocrinol (Oxf) 2007; 66: 459–465. [DOI] [PubMed] [Google Scholar]
- 43. Reisch N, Willige M, Kohn D, et al. Frequency and causes of adrenal crises over lifetime in patients with 21-hydroxylase deficiency. Eur J Endocrinol 2012; 167: 35–42. [DOI] [PubMed] [Google Scholar]
- 44. Hernandez Padilla P. [Adrenal crisis in the surgical patient]. Cir Cir 1962; 30: 123–141. [PubMed] [Google Scholar]
- 45. Cawson RA, James J. Adrenal crisis in a dental patient having systemic corticosteroids. Br J Oral Surg 1973; 10: 305–309. [DOI] [PubMed] [Google Scholar]
- 46. Thomsen AF, Kvist TK, Andersen PK, et al. The risk of affective disorders in patients with adrenocortical insufficiency. Psychoneuroendocrinology 2006; 31: 614–622. [DOI] [PubMed] [Google Scholar]
- 47. El-Maouche D, Hargreaves CJ, Sinaii N, et al. Longitudinal assessment of illnesses, stress dosing, and illness sequelae in patients with congenital adrenal hyperplasia. J Clin Endocrinol Metab 2018; 103: 2336–2345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Iwasaku M, Shinzawa M, Tanaka S, et al. Clinical characteristics of adrenal crisis in adult population with and without predisposing chronic adrenal insufficiency: a retrospective cohort study. BMC Endocr Disord 2017; 17: 58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Yatagai T, Kusaka I, Nakamura T, et al. Close association of severe hyponatremia with exaggerated release of arginine vasopressin in elderly subjects with secondary adrenal insufficiency. Eur J Endocrinol 2003; 148: 221–226. [DOI] [PubMed] [Google Scholar]
- 50. Cuesta M, Garrahy A, Slattery D, et al. The contribution of undiagnosed adrenal insufficiency to euvolaemic hyponatraemia: results of a large prospective single-centre study. Clin Endocrinol (Oxf) 2016; 85: 836–844. [DOI] [PubMed] [Google Scholar]
- 51. Arlt W and Society for Endocrinology Clinical Committee. SOCIETY FOR ENDOCRINOLOGY ENDOCRINE EMERGENCY GUIDANCE: emergency management of acute adrenal insufficiency (adrenal crisis) in adult patients. Endocr Connect 2016; 5: G1–G3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Higham CE, Olsson-Brown A, Carroll P, et al. SOCIETY FOR ENDOCRINOLOGY ENDOCRINE EMERGENCY GUIDANCE: acute management of the endocrine complications of checkpoint inhibitor therapy. Endocr Connect 2018; 7: G1–G7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Gagliardi L, Nenke MA, Thynne TR, et al. Continuous subcutaneous hydrocortisone infusion therapy in Addison’s disease: a randomized, placebo-controlled clinical trial. J Clin Endocrinol Metab 2014; 99: 4149–4157. [DOI] [PubMed] [Google Scholar]
- 54. Jung C, Greco S, Nguyen HH, et al. Plasma, salivary and urinary cortisol levels following physiological and stress doses of hydrocortisone in normal volunteers. BMC Endocr Disord 2014; 14: 91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Ho JT, Al-Musalhi H, Chapman MJ, et al. Septic shock and sepsis: a comparison of total and free plasma cortisol levels. J Clin Endocrinol Metab 2006; 91: 105–114. [DOI] [PubMed] [Google Scholar]
- 56. Widmer IE, Puder JJ, Konig C, et al. Cortisol response in relation to the severity of stress and illness. J Clin Endocrinol Metab 2005; 90: 4579–4586. [DOI] [PubMed] [Google Scholar]
- 57. Addison’s Disease Self Help Group. ADSHG surgical guidelines, https://www.addisons.org.uk/files/file/4-adshg-surgical-guidelines/ (2015, accessed 14 September 2017).
- 58. Hahner S, Burger-Stritt S, Allolio B. Subcutaneous hydrocortisone administration for emergency use in adrenal insufficiency. Eur J Endocrinol 2013; 169: 147–154. [DOI] [PubMed] [Google Scholar]
- 59. Hahner S, Hemmelmann N, Quinkler M, et al. Timelines in the management of adrenal crisis - targets, limits and reality. Clin Endocrinol (Oxf) 2015; 82: 497–502. [DOI] [PubMed] [Google Scholar]
- 60. Gargya A, Chua E, Hetherington J, et al. Acute adrenal insufficiency: an aide-memoire of the critical importance of its recognition and prevention. Intern Med J 2016; 46: 356–359. [DOI] [PubMed] [Google Scholar]
- 61. Chapman SC, Llahana S, Carroll P, et al. Glucocorticoid therapy for adrenal insufficiency: nonadherence, concerns and dissatisfaction with information. Clin Endocrinol (Oxf) 2016; 84: 664–671. [DOI] [PubMed] [Google Scholar]
- 62. Kampmeyer D, Lehnert H, Moenig H, et al. A strong need for improving the education of physicians on glucocorticoid replacement treatment in adrenal insufficiency: an interdisciplinary and multicentre evaluation. Eur J Intern Med 2016; 33: e13–e15. [DOI] [PubMed] [Google Scholar]
- 63. Broersen LH, Pereira AM, Jorgensen JO, et al. Adrenal insufficiency in corticosteroids use: systematic review and meta-analysis. J Clin Endocrinol Metab 2015; 100: 2171–2180. [DOI] [PubMed] [Google Scholar]
- 64. Husebye ES, Allolio B, Arlt W, et al. Consensus statement on the diagnosis, treatment and follow-up of patients with primary adrenal insufficiency. J Intern Med 2014; 275: 104–115. [DOI] [PubMed] [Google Scholar]
- 65. Lagger G, Pataky Z, Golay A. Efficacy of therapeutic patient education in chronic diseases and obesity. Patient Educ Couns 2010; 79: 283–286. [DOI] [PubMed] [Google Scholar]
- 66. Vidmar AP, Weber JF, Monzavi R, et al. Improved medical-alert ID ownership and utilization in youth with congenital adrenal hyperplasia following a parent educational intervention. J Pediatr Endocrinol Metab 2018; 31: 213–219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Schad R, Schneider PJ, Nold EG. Reimbursable pharmacy teaching program for adrenalectomy patients. Am J Hosp Pharm 1979; 36: 1212–1214. [PubMed] [Google Scholar]
- 68. Repping-Wuts HJ, Stikkelbroeck NM, Noordzij A, et al. A glucocorticoid education group meeting: an effective strategy for improving self-management to prevent adrenal crisis. Eur J Endocrinol 2013; 169: 17–22. [DOI] [PubMed] [Google Scholar]
- 69. Hahner S, Loeffler M, Fassnacht M, et al. Impaired subjective health status in 256 patients with adrenal insufficiency on standard therapy based on cross-sectional analysis. J Clin Endocrinol Metab 2007; 92: 3912–3922. [DOI] [PubMed] [Google Scholar]
- 70. Oksnes M, Bensing S, Hulting AL, et al. Quality of life in European patients with Addison’s disease: validity of the disease-specific questionnaire AddiQoL. J Clin Endocrinol Metab 2012; 97: 568–576. [DOI] [PubMed] [Google Scholar]
- 71. Meyer G, Koch M, Herrmann E, et al. Longitudinal AddiQoL scores may identify higher risk for adrenal crises in Addison’s disease. Endocrine 2018; 60: 355–361. [DOI] [PubMed] [Google Scholar]


