Abstract
Growing scientific evidence has unveiled increased incidences of obesity in domestic animals and its influence on a plethora of associated disorders. Leptin, an adipokine regulating body fat mass, represents a key molecule in obesity, able to modulate immune responses and foster chronic inflammatory response in peripheral tissues. High levels of cytokines and inflammatory markers suggest an association between inflammatory state and obesity in dogs, highlighting the parallelism with humans. Canine obesity is a relevant disease always accompanied with several health conditions such as inflammation, immune-dysregulation, insulin resistance, pancreatitis, orthopaedic disorders, cardiovascular disease, and neoplasia. However, leptin involvement in many disease processes in veterinary medicine is poorly understood. Moreover, hyperleptinemia as well as leptin resistance occur with cardiac dysfunction as a consequence of altered cardiac mitochondrial metabolism in obese dogs. Similarly, leptin dysregulation seems to be involved in the pancreatitis pathophysiology. This review aims to examine literature concerning leptin and immunological status in obese dogs, in particular for the aspects related to obesity-associated diseases.
Keywords: leptin, dog, obesity, immune function, physiology, human
1. Introduction
Obesity is a metabolic disorder arising due to abnormal and frequently ectopic white adipose tissue deposition, as a consequence of an altered balance between energy intake and consumption, usually dependent on the body’s inefficiency to convert caloric intake in energy. Literature has been focused on the role of leptin in determining obesity and related diseases in humans. The economic impact of obesity on the world health care system stimulated research interest [1] on the underlying molecular and biochemical mechanisms of obesity-associated comorbidities such as diabetes mellitus, metabolic disorders [2], orthopaedic disease [3], respiratory dysfunction [4], and altered renal function [5]. Growing incidences of obesity highlighted its relevance in domestic animals and, in particular, in dogs [6].
From its first characterization in 1994 to today, the relationship between leptin and its involvement in supporting inflammatory processes becomes increasingly relevant also in the determinism of autoimmunity [7,8].
In this regard, white adipose tissue has been considered not only a fat storage compartment able to regulate energy homeostasis, but also a key provider of several biomolecules able to deeply modulate tissue physiology in individuals [9,10,11,12]. Leptin production is mainly based on adipocytes secretion, the level of such a hormone correlates with white adipose tissue mass and contributes to an inflammatory state in overweight and obese humans [12]. In addition to the control of the biological processes involved in energy homeostasis, leptin has systemic effects that include the regulation of endocrine function, the immune response, and haematopoiesis [13,14,15]. Therefore, obesity can be considered as a chronic and complex pathological state associated with multiple systemic and tissue-specific alterations. This review intends to examine the physiological role of leptin, the possible relationship between leptin, immune function, and metabolism in dogs, and to highlight possible perspectives for human studies.
2. Physiological Role of Leptin and Its Relationship with Obesity
Leptin is a hormone secreted by white adipocytes [16,17]. Through the blood-brain barrier, such a hormone reaches the hypothalamus to decrease food intake and to increase metabolism [16]. Leptin receptors, encoded by the LEPR gene [18,19], are expressed by hypothalamic satiety centres and are widely disseminated throughout the body—this occurrence reflects the pleiotropic nature of leptin that is involved in the control of many physiologic processes [20]. Ob-Rb, the ‘long’ isoform of the receptor, is predominantly expressed in the hypothalamus [21,22,23], while the short isoforms (Ob-Ra, Ob-Rc, Ob-Rd, and Ob-Rf) are expressed in the peripheral tissues [24,25]. Leptin receptor (LEPR) needs the activation of receptor associated kinases of Janus family (JAKs), which in turn induce downstream signalling involving different members of signal transducers and activators of transcription (STAT) family [26]. Leptin receptors activate a complex neural circuit involving anorexigenic (i.e., appetite-diminishing) and orexigenic (i.e., appetite-stimulating) neuropeptides to control food intake.
Moreover, leptin also stimulates the sympathetic nervous system inducing an increase in plasma norepinephrine and epinephrine concentrations via the ventromedial hypothalamus [27].
In addition to its pivotal role in the regulation of energy metabolism [28], leptin possesses other important physiological activities as the control of neuroendocrine and immune functions, and haematopoiesis [29,30]. The strict association between obesity and hematopoietic disruption evidenced the role of leptin on bone organization. The direct role for leptin in haematopoiesis has been demonstrated by the presence of Ob-R on bone marrow CD34+ cells as well as on lympho-haematopoietic and megakaryocytic cell lines [31,32]. Recently, Claycombe et al. [33] demonstrated that myelopoiesis recover after treatment with leptin in obese mice (ob/ob). Aberrant leptin levels in patients with haematological malignancies have been described, suggesting that leptin signalling is involved in the progression of haematological malignancies and could represent a useful prognostic value [34].
Relationship between leptin and obesity could be considered as a part of metabolic syndrome (MS), the pathological condition comprising of also dyslipidaemia, hyperglycaemia, and high blood pressure. It is noteworthy that obesity is related to the leptin receptor resistance mechanisms [35], including several aspects such as: (i) Interruption of leptin signalling in hypothalamic and other central nervous system (CNS) neurons; (ii) alteration of leptin transport across blood-brain barrier; (iii) hypothalamic inflammation, autophagy, and endoplasmic reticulum stress [36,37]. The development of leptin resistance and of hyperleptinemia have been widely demonstrated in humans and in domestic animals [38].
In the course of obesity and hyperleptinemia condition, an accumulation of epicardial adipose tissue has been demonstrated [39], suggesting its involvement in cardiovascular system damage. Chronic inflammation and the accumulation of epicardial fat is strongly concomitant with coronary artery disease, independent of visceral adiposity [39]. Furthermore, high circulating levels of leptin appeared to induce significant impairment of the haemostatic balance in cardiovascular diseases [40].
Moreover, leptin has been associated to hypertension and congestive heart failure (HF) in humans, dogs, and cats [38,41]. In addition, leptin accelerates atherosclerosis spreading [42].
The role of leptin and adipokines on the cardiovascular system have been largely described to be dependent on two mechanisms involving the heart or the central nervous system [43,44,45]. Leptin acts by stimulating the migration and proliferation of vascular smooth muscle cells (VSMCs) [46]. Such hormones block the vasoconstrictor action of angiotensin II and inhibits the angiotensin II-induced increase in intracellular Ca2+ in VSMCs through Ob-Rb [47]. Leptin shows angiogenetic effects dependent on both proliferation and migration of vascular smooth muscle cells by promoting the upregulation of vascular endothelial growth factor (VEGF) expression [48] and the cytoskeleton reorganization [49].
Acute pancreatitis is associated with high levels of leptin in serum and pancreas [50,51], suggesting the role for such a hormone as a marker for adipose tissue necrosis [52]. Intriguingly, the pancreas could secrete leptin and its protective role in pancreatitis has been described [53,54]. In agreement with this hypothesis, beneficial effects of leptin on acute pancreatitis have been evidenced in ischemia/reperfusion [54,55].
3. Role of Leptin in the Relationship between Obesity and Immune-Modulation.
An interesting scenario on obesity is that immune response greedily needs “energy” to be implemented. In a pathophysiological perspective, this energy can be in excess or in deficit. In this regard, food opulence is frequently associated with autoimmune diseases [7,56,57], while hyponutrition induces susceptibility to infectious diseases [58,59,60,61]. Therefore, an excess of nutrients could drive the immune system towards self-reactivity, while a defect can determine insufficient anti-infectious immune responses. In this regard, the relationship between obesity and immune modulation appears of great relevance in both human and veterinary medicine [7,56,57,62,63,64,65,66,67].
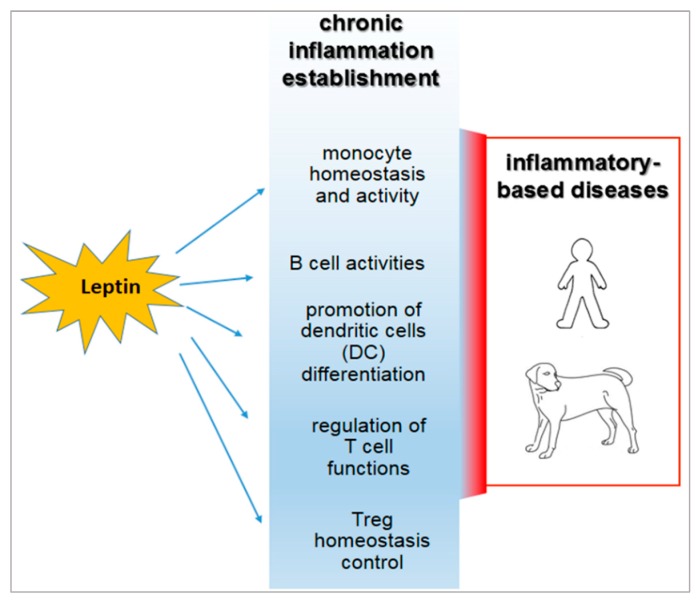
In human and animal obesity, the secretion of leptin and other hormones from the adipose tissue appears to determine the dysregulation of the immune response [7,68,69] (Figure 1).
Figure 1.
Inflammatory roles of leptin in the course of obesity and their relevance in both human and veterinary medicine.
Moreover, leptin and its receptors are integral components of a complex physiological system evolved to regulate fuel stores and energy balance at an optimum level in mammals [70].
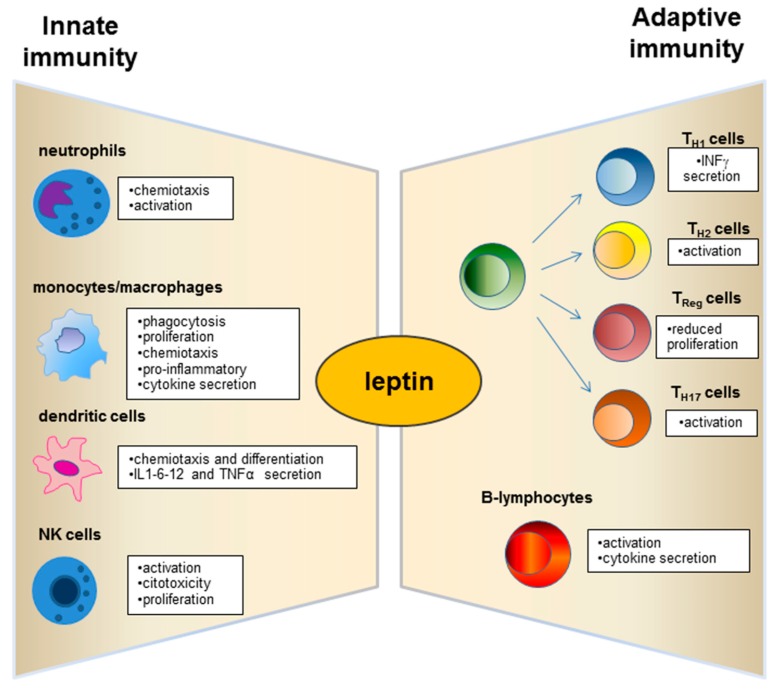
Leptin has structural similarities with the alpha-helix family of cytokines and its receptor (ObR) belongs to the superfamily of class I cytokine receptors [71]. Leptin receptors are expressed by immune system cells [72,73,74], and leptin possesses modulatory effects on both innate and adaptive immunity [75,76] (Figure 2). Such a hormone is currently considered a pro-inflammatory adipokine [7,8,12]. In this regard, leptin acts as an acute phase inflammatory cytokine like interleukin (IL)-1, IL-6, and tumour necrosis factor (TNF)-α [29] and is necessary for phagocytosis of bacteria by polymorph nuclear cells [77].
Figure 2.
Physiological role of leptin on innate and adaptive immunity.
Several studies evidenced the involvement of leptin in activation of macrophages [78] and in their recruitment in adipose tissue [79] (Figure 2). Leptin fosters pro-inflammatory activity by monocyte [80] and promotes their production of reactive oxygen species (ROS) [81,82] (Figure 2). Furthermore, such a hormone plays an anti-apoptotic role in serum-deprived monocytes demonstrating that this adipokine could act as a growth factor for these cells [83]. Leptin also exerts chemotactic activity on neutrophils [84] and promotes their production of intracellular hydrogen peroxide [85] (Figure 2).
Neutrophils express the short form of the leptin receptor [86] that can stimulate the expression of CD11b and prevent apoptosis.
Dendritic cells (DC), a specialized cell population for antigen uptake in body tissues, express leptin receptors (Ob-R) on their surface [87]. Leptin acts on these cells, favouring their differentiation, maturation, recruitment, and survival [87,88] and modulating the signalling pathways involved in these biological processes as observed in db/db mice lacking leptin receptors (Ob-R) [88]. Furthermore, an important role of leptin is exercised by the activation and recruitment of the DC (Figure 2).
Deficits of leptin receptors in Natural Killer (NK) cells correlate with decreased NK number and functions [89,90].
Moreover, LEPR-deficient (db/db) mice evidenced a decrease of NK function [91].
The role of leptin in adaptive immunity has been largely demonstrated from early studies on db/db mice that showed high level of thymocyte apoptosis [92].
A great research interest has moved to explore the leptin role on the T and B cell population (Figure 2). Leptin acts with several mechanisms on T lymphocytes and induces the expression of the long isoform of LEPR in CD4+ T cells [93]. Such adipokine promotes activation and proliferation of T lymphocytes and enhances their cytokine production [94,95]. In addition, the leptin supplementation to a mixed lymphocyte reaction has been observed to induce a proliferation of CD4+ T cells [95].
Leptin regulates the adaptive immunity, also influencing activities of T Helper (Th) 1 and 2 lymphocytes [7,8,58,96]. In particular, the hormone stimulates the Th1 production of cytokines such as IL-2, interferon (IFN)-γ, TNF-α, and IL-18, and drives the differentiation of the Th17 cells mainly involved in chronic inflammation establishment [97,98].
In addition, leptin influences B-cell activities, regulating and promoting cell cycle by Bcl-2 and cyclin D activation [99].
It is of note that leptin acts on the homeostasis of a specific CD4+CD25highFoxp3+ T immune regulatory cell population, usually referred to as Treg [7,100,101,102,103,104]. Such cells avoid the auto reactivity of the immune system against the “self” molecular components that belong to the individual itself [7,100,101,102]. Human Treg cells display heterogeneous gene expression, phenotype, and suppressive functions [105]. This occurrence strongly correlates with the different splicing variants of the transcriptional factor FoxP3 [106]—the full-length isoform (FoxP3fl), which contains the sequences involved in the interaction with retinoic acid-related orphan receptors α and γt (RORα and RORγt), is associated with Treg function in humans [107]. In contrast, the expression of the isoform lacking exon 2 (FoxP3Δ2) correlates with dysfunction of Treg cells, since it appears to be unable to interact with RORα and RORγt [108]. FoxP3Δ2 expression has been correlated with multiple sclerosis in humans [109]. Expression of the different FOXP3 isoforms is conditioned by metabolic aspects [110] and by the exposure of Treg to the pro-inflammatory micro-environment [111]. No data over this potential functional dichotomy are available from canine or feline models.
Nutrient availability is essential for the maintenance of tissue homeostasis. In this context, the intracellular “sensor” of nutrients [112] is represented by the mammalian target of rapamycin, the mTOR molecule [113]. This serine–threonine kinase “senses” the extracellular bioavailability of amino acids, glucose, growth factors, and hormones [101,112,113,114], promotes cell metabolism and growth when the conditions are favourable; or catabolic processes when conditions are not favourable. In this context, mTOR is strongly correlated with Treg homeostasis and functions [115]. High levels of leptin correlate with a reduced number and with decreased functions of Treg cells in human autoimmune diseases [7,56]. The relationship between metabolism and cell plasticity is of great relevance, particularly for the homeostasis of immune system cells that are highly “sensitive” to bioavailable nutrients [116,117,118,119]. In this context, T effectors and Treg cells [114,120] are significantly influenced by metabolism—such an occurrence may explain why caloric excess correlates with autoimmune diseases [7,57], while hyponutrition increases susceptibility to infections [58,59,60,61]. In this negatively virtuous interplay, the high levels of leptin secreted by the adipose tissue are able to dysregulate the Treg cells and determine an increased risk of developing autoimmune diseases in obese patients [121,122,123].
Reduced Treg cells have been observed in visceral adipose tissue of obese mice and humans. However, it is unknown whether human obesity affects circulating Treg cells and whether Treg number is associated with markers of systemic inflammation or glucose intolerance. The effect of human obesity to reduce Treg levels has been addressed [124,125]. Circulating Treg cells are inversely correlated with body weight and plasma leptin levels [125].
Reduction of circulating Treg cells in obesity may be caused by their recruitment into an active inflammation site. In this regard, an upregulated expression of homing receptors—including the chemokine receptors CXCR3 and CCR7—on the surface of Treg cells and an increased accumulation of Treg cells in the spleen of obese mice have been reported [126]. Increased serum levels of adipose tissue-derived cytokines may impair Treg cell maturation and/or survival in obesity. Interestingly, the receptor of the adipokine leptin is expressed on T lymphocytes [95], including Treg cells, and leptin neutralization promotes their proliferative capacity [101]. Moreover, hypercholesteraemic LDL-R mice with defective leptin signalling exhibited improved Treg cell functions [127].
Adiposity has been associated with increased concentrations of leptin and other proinflammatory adipokines, cytokines, and acute-phase proteins [128]. The role of adiponectin in dogs still appears controversial and few data are available in the veterinary literature on the possible impact of obesity on the immune response. The effects of weight loss on canine adipokines and cytokines have been reported [2,3,129,130,131]. Several studies showed that plasma leptin concentrations correlate with body fat content in experimentally induced obese beagles [132,133]. In this regard, Sagawa et al. highlighted that the positive relationship between plasma leptin concentration and body fat content in dogs is similar to correlations reported for humans and rodents [132]. Ishioka et al. [134] showed that plasma leptin represents an index of adiposity in dogs regardless of their age, gender, and breed variations. It is well known that plasma leptin concentrations increase with weight gain and decrease with weight loss in dogs. In this regard, Jeusette et al. [135] described a decrease in ghrelin and an increase in leptin and insulin concentrations in obese beagle dogs. The same authors [135] suggested that ghrelin and leptin could play a role in dogs in the adaptation to a positive or negative energy balance, as observed in humans. Proinflammatory state directly influences glucose metabolism, resulting in decreased insulin sensitivity [128]. In fact, high-plasma leptin concentrations have been correlated to insulin resistance in humans [136] and in insulin-resistant dogs [135]. Serum leptin concentrations correlated with percentage of body fat and decreased with weight loss, whereas the involvement of other inflammatory markers in canine obesity and weight loss is still less understood. Induction of canine obesity has been shown to increase concentrations of TNF-α [137] which decreases after a weight loss program in obese dogs [2]. However, acute phase proteins appeared to be unaltered after the weight loss program [129], while the production of C-reactive protein decreased in obese dogs [2,129,130,131,138].
Van de Velde et al. [139] investigated the effect of a short-term increase in body weight on immunological variables in adult healthy beagle dogs in which weight gain and increased body condition score (BCS) were accompanied by a significantly higher leptin concentration. Subsequently, the same authors [140] described that T-cell proliferation is affected after weight gain in Beagle dogs.
Recently, concentrations of IL-6 and monocyte chemoattractant protein 1, but not IL-8, were found to be increased in overweight dogs [141], whereas other authors described decreasing concentrations of IL-8 and other interleukins with weight loss in dogs [131]. Piantedosi et al. [142] revealed no significant differences in serum TNF-α and IL-6 concentrations between obese and normal weight dogs.
Several studies have reported that the systemic circulating leptin deficiency in malnutrition is also correlated to infectious diseases [61,77,81,143,144,145] including leishmaniasis [146,147] due to defective cytokine production [84,148]. Leptin can augment host protective immune response during experimental visceral leishmaniasis (VL) [146,147]. Indeed, leptin induces the phagocytic activity of human macrophages against L. donovani infection by enhancing the phagolysosome formation and oxidative killing of the parasite via intracellular reactive oxygen species (ROS) generation [147].
Palatucci et al. [65] reported that obese Labrador Retrievers are characterized by the inverse correlation between leptin serum concentration and circulating Treg levels. Moreover, an increased number of cytotoxic T cell effectors and a higher IFN-γ production by cytotoxic T lymphocytes have been observed in obese dogs [65]. However, the relationship between obesity, leptin, and circulating Treg level, as well as the occurrence of systemic inflammation in dogs and in other domestic mammalians are still poorly understood.
Increased inflammatory response has been correlated with clinical exacerbation, and the immunotherapeutic role of Tregs appears to be relevant in leishmaniosis [149].
Tregs function, macrophage activation, and the proinflammatory state appear to be involved in the pathogenesis of canine leishmaniasis. Naturally L. infantum infected dogs expressed alteration in leptin gene transcription and low levels of circulating Treg [150]. In the same model, ineffective immune response to parasites appeared to be associated with high Treg levels [151]. Di Loria et al. [152] showed an increase in leptin mRNA expression in dogs naturally infected by L. infantum.
4. Leptin and Associated Diseases in Humans and Dogs
High body mass index represents a risk factor in both human and canine mammary inflammatory carcinomas [153,154,155,156]. How obesity can influence the development and prognosis of human breast cancer remains unknown, although several factors secreted by adipocytes including aromatase, leptin, adiponectin, oestrogens, and insulin-like growth factor-1 have been implicated [157]. Leptin may promote carcinogenesis of the mammary tissue through its interaction with the leptin receptor Ob-R [158,159,160,161,162]. Such a hormone could affect breast cancer by stimulating growth of normal mammary epithelial cells and tumour cells, tumour invasion, angiogenesis, and aromatase activity [157,162]. Obesity is considered a pro-inflammatory state and is associated with increasing circulating levels of TNF-α and IL-6 [163]. Chronic inflammation promotes tumour development [164], macrophage recruitment in mammary gland in human and murine obese subjects [165,166] and metastasis of breast tumours [167]. Notably, obesity-related macrophage infiltration of murine mammary gland reversed with caloric restriction [168].
Obesity affects progression, and metastasis in canine mammary carcinoma (MC) by recruitment of macrophages [156] (Figure 2). In this regard, macrophage infiltration of tumour areas appears to be higher in overweight or obese subjects than in lean subjects. In addition, decreased adiponectin expression and increased macrophage numbers in overweight or obese subjects associate with poor prognosis, high histological grade, and lymphatic invasion [156]. Leptin and Ob-R expression correlates with oestrogen receptor status MC [156].
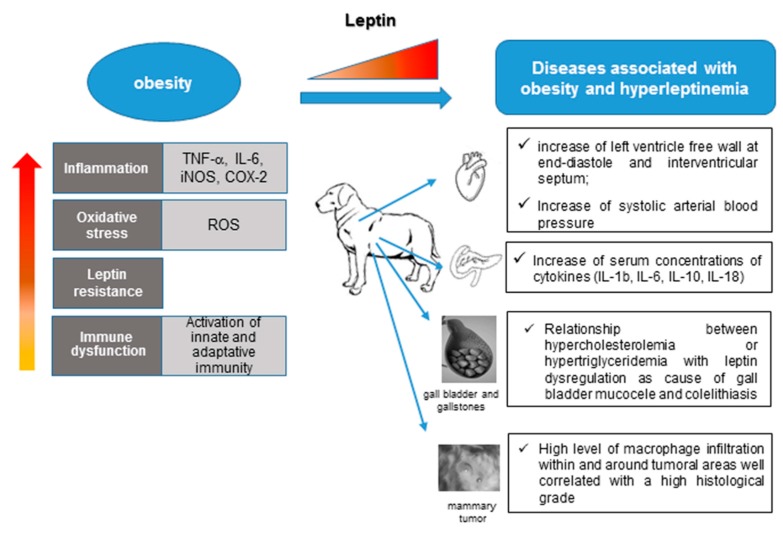
Canine obesity has been associated with cardiac dysfunction [142,169,170,171]. Leptin has been observed in canine cardiovascular disease [172,173] (Figure 3). Varied morphologies of human obesity-related cardiac structural changes have been described and many include symmetric or asymmetric left ventricle hypertrophy (LVH) with or without left ventricular chamber dilatation [174,175]. In canine model, Adolphe et al. [170] described alterations in glucose, adipokines (leptin and adiponectin) and heart during obesity (Figure 3). Weight loss reversed these alterations. Piantedosi et al. [142] suggested the presence of myocardial concentric hypertrophy in obese dogs.
Figure 3.
Obesity in dogs and diseases associated with hyperleptinemia.
Systolic arterial blood pressure appeared to be higher in obese than in normal weight dogs (Figure 3). Similar cardiovascular findings and increased systolic blood pressure have been reported by Mehlman et al. [169]. In contrast, hypertension has not been related to canine obesity [176].
Obese dogs express alterations in cardiac function, insulin resistance, dyslipidaemia, hypo-adiponectinaemia and increased concentrations of inflammatory markers and leptin [171]. However, only few studies investigated the role of leptin in canine cardiac diseases [169,177,178]. In the heart, cardiomyocytes and endothelial cells produce leptin and express its receptor. In addition to changes in blood concentrations, functional auto- and paracrine effects may occur [179,180,181,182]. Leptin regulates the baseline physiology of the heart including myocyte contractility, hypertrophy, apoptosis, and metabolism [181,183,184]. Localized depots of epicardial or perivascular fat might also play physiological or pathological roles [183,185,186]. In cardiac disease (CDi) and in congestive heart failure (CHF), leptin significantly increased, suggesting that an increased metabolic rate is associated with high concentrations of catecholamines and proinflammatory cytokines present in CHF [187,188]. Furthermore, because of elicited central sympathoexcitatory effects, leptin participates in the neuro-humoral activation in heart failure [189]. Increased leptin has been associated with increased oxygen consumption and intracellular calcium release and decreased cardiac efficiency in vivo [179,186,190]. In CDi, leptin is involved in cardiac remodelling, characterized by cardiomyocyte hypertrophy and disruption of the extracellular matrix resulting in increased collagen deposition [185,186,191], which might contribute to cardiac dysfunction. Such a hormone protects cardiomyocytes from apoptosis, which plays an important role in the development of CHF [192]. Leptin might decrease cardiac hypertrophy, apoptosis, and inflammation in deficient leptin receptor mice [193]. Therefore, leptin can impact cardiovascular function by direct heart effects or by central nervous system responses and may represent a predictor of cardiovascular morbidity [179,185]. However, the role of leptin in development and progression of canine CDi and CHF is still poorly understood [172,173].
The role of leptin as a pathophysiological modulator has been described in other canine pathological conditions [194,195], besides cardiovascular diseases. Adipokines, especially resistin and visfatin, have been implicated in the development of acute pancreatitis (AP) in humans [196,197,198,199] and in experimental animal models [200,201,202]. However, little information is available about the circulating adipokine concentrations during the pathogenesis of AP in dogs. Recently, Paek et al. [203] described that leptin, resistin, and visfatin were significantly higher in the dogs with AP than in healthy dogs, whereas adiponectin concentration was significantly lower in AP than in healthy dogs. IL-1b, IL-6, IL-10, and IL-18 also increased in AP dogs [203]. These results suggest a potential role for adipokines in the development and modulation of AP in dogs (Figure 3).
In addition, leptin and its receptor play several physiological roles in the canine gallbladder (Figure 3). Gallbladder is not only a source of leptin, but it is also affected by autocrine/paracrine mechanisms [204]. Lee et al. [205] revealed an increased expression of leptin and leptin receptors in dogs with gallbladder mucocele (GBM), suggesting that such a hormone plays a role as a causative factor in GBM.
The relationship between serum triglyceride/cholesterol and leptin is still controversial [206,207]. Leptin may correlate with serum lipids in dogs [208,209]. A positive association between human hyperlipidaemia and gallstones has been described [210,211]. Recently, Lee et al. [212] described an increase in serum leptin during hyperlipidaemia and cholelithiasis occurrence in dogs.
Finally, leptin is known for its involvement in the regulation of reproductive functions. Such a hormone is important for uterine receptivity, implantation, placental growth, and maternal energy homeostasis in several species [213,214]. The uterus and placenta are also sources of leptin and targets of its actions during gestation in canine species. Leptin and leptin receptors are expressed both in the foetal and maternal sides of the placenta, thus, a role in placental physiology seems likely. The leptin signalling system may be one of the pathways involved in the establishment and maintenance of pregnancy and may also play a regulatory role in parturition in the bitch [215].
5. Conclusions
Leptin constitutes a relevant hormonal “actor” in obesity, immune-system homeostasis and in several associated metabolic-related as well as immune-mediated diseases [8]. Recent clinical studies on autoimmune disease patients demonstrated that high serum leptin levels may play a causal role in the disease progression and could represent a diagnostic marker for clinical application. It remains to be established if leptin could be a potential therapeutic target in treating human autoimmune diseases [30,216].
Circulating leptin correlates with fat mass and is considered a useful marker of adiposity in veterinary settings. However, no studies are available concerning other clinical applications of such a hormone, and about the involvement of leptin in canine immune-mediated diseases.
The growing worldwide scientific attention for obesity and leptin—in consideration of the important implications for quality of life in humans and animals—must motivate further studies, able to generate information on the molecular mechanism exerted by leptin in the course of the disease, and to therefore identify possible therapeutic targets for obesity as well as other associated diseases. Furthermore, the most recent interest in the study of obesity and related diseases in animal species appears to be intriguingly “translational” to better understand the human etiopathology of the metabolic syndrome. In fact, domestic animals, particularly the dog, represent the natural biological indicators of the habits of life in, correlating with human aspects. Therefore, the need for studies to understand the pro-inflammatory role of leptin and weight gain in canine diseases seems to be of great importance, not only for veterinary medicine, but also to protect human health and to contain health-related expenditure generated by many widespread chronic metabolic diseases.
Abbreviations
| apoE | Apolipoprotein E |
| AP | Acute pancreatitis |
| BCS | Body condition score |
| CDi | Cardiac disease |
| CHF | Congestive heart failure |
| CNS | Central nervous system |
| CRP | C-reactive protein |
| DC | Dendritic cells |
| GBM | Gallbladder mucocele |
| HF | Heart failure |
| IFN | Interferon |
| IL | Interleukin |
| JAK | Janus kinase |
| LEPR | Leptin receptor |
| LVH | Left ventricle hypertrophy |
| MAPK | Mitogen-activated protein kinases |
| MC | Mammary carcinoma |
| MCP-1 | Monocyte chemoattractant protein-1 |
| MS | Metabolic Syndrome |
| VEGF | Vascular growth factor |
| VL | Visceral Leishmaniasis |
| ROR | Retinoic acid-related orphan receptor |
| ROS | Reactive oxygen species |
| NK | Natural Killer |
| STAT | Signal transducer and activator of transcription |
| TNF | Tumour necrosis factor |
| Treg cells | Regulatory T cells |
| VSMCs | Vascular smooth muscle cells |
Funding
This research received no external funding.
Conflicts of Interest
The authors declare no conflict of interest.
References
- 1.Tremmel M., Gerdtham U.G., Nilsson P.M., Saha S. Economic burden of obesity: A systematic literature review. Int. J. Environ. Res. Public Health. 2017;14:435. doi: 10.3390/ijerph14040435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pradhan A. Obesity, metabolic syndrome, and type 2 diabetes: Inflammatory basis of glucose metabolic disorders. Nutr. Rev. 2007;65:S152–S156. doi: 10.1301/nr.2007.dec.S152-S156. [DOI] [PubMed] [Google Scholar]
- 3.Mihalko W.M., Bergin P.F., Kelly F.B., Canale S.T. Obesity, orthopaedics, and outcomes. J. Am. Acad. Orthop. Surg. 2014;22:683–690. doi: 10.5435/JAAOS-22-11-683. [DOI] [PubMed] [Google Scholar]
- 4.Zammit C., Liddicoat H., Moonsie I., Makker H. Obesity and respiratory diseases. Int. J. Gen. Med. 2010;3:335–343. doi: 10.2147/IJGM.S11926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Câmara N.O., Iseki K., Kramer H., Liu Z.H., Sharma K. Kidney disease and obesity: Epidemiology, mechanisms and treatment. Nat. Rev. Nephrol. 2017;13:181–190. doi: 10.1038/nrneph.2016.191. [DOI] [PubMed] [Google Scholar]
- 6.German A.J. The growing problem of obesity in dogs and cats. J. Nutr. 2006;136:1940S–1946S. doi: 10.1093/jn/136.7.1940S. [DOI] [PubMed] [Google Scholar]
- 7.La Cava A. Leptin in inflammation and autoimmunity. Cytokine. 2017;98:51–58. doi: 10.1016/j.cyto.2016.10.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Abella V., Scotece M., Conde J., Pino J., Gonzalez-Gay M.A., Gómez-Reino J.J., Mera A., Lago F., Gómez R., Gualillo O. Leptin in the interplay of inflammation, metabolism and immune system disorders. Nat. Rev. Rheumatol. 2017;13:100–109. doi: 10.1038/nrrheum.2016.209. [DOI] [PubMed] [Google Scholar]
- 9.Fantuzzi G. Adipose tissue, adipokines, and inflammation. J. Allergy Clin. Immunol. 2005;115:911–919. doi: 10.1016/j.jaci.2005.02.023. [DOI] [PubMed] [Google Scholar]
- 10.Lago F., Dieguez C., Gómez-Reino J., Gualillo O. Adipokines as emerging mediators of immune response and inflammation. Nat. Clin. Pract. Rheumatol. 2007;3:716–724. doi: 10.1038/ncprheum0674. [DOI] [PubMed] [Google Scholar]
- 11.Lago F., Dieguez C., Gómez-Reino J., Gualillo O. The emerging role of adipokines as mediators of inflammation and immune responses. Cytokine Growth Factor Rev. 2007;18:313–325. doi: 10.1016/j.cytogfr.2007.04.007. [DOI] [PubMed] [Google Scholar]
- 12.Lago F., Gómez R., Gómez-Reino J.J., Dieguez C., Gualillo O. Adipokines as novel modulators of lipid metabolism. Trends Biochem. Sci. 2009;34:500–510. doi: 10.1016/j.tibs.2009.06.008. [DOI] [PubMed] [Google Scholar]
- 13.Ahima R.S., Flier J.S. Leptin. Annu. Rev. Physiol. 2000;62:413–437. doi: 10.1146/annurev.physiol.62.1.413. [DOI] [PubMed] [Google Scholar]
- 14.Park H.K., Ahima R.S. Physiology of leptin: Energy homeostasis, neuroendocrine function and metabolism. Metabolism. 2015;64:24–34. doi: 10.1016/j.metabol.2014.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Friedman J. The long road to leptin. J. Clin. Investig. 2016;126:4727–4734. doi: 10.1172/JCI91578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zhang Y., Proenca R., Maffei M., Barone M., Leopold L., Friedman J.M. Positional cloning of the mouse obese gene and its human homologue. Nature. 1994;372:425–432. doi: 10.1038/372425a0. [DOI] [PubMed] [Google Scholar]
- 17.Havel P.J. Role of adipose tissue in body-weight regulation: Mechanisms regulating leptin production and energy balance. Proc. Nutr. Soc. 2000;59:359–371. doi: 10.1017/S0029665100000410. [DOI] [PubMed] [Google Scholar]
- 18.Lee G.H., Proenca R., Montez J.M., Carroll K.M., Darvishzadeh J.G., Lee J.I., Friedman J.M. Abnormal splicing of the leptin receptor in diabetic mice. Nature. 1996;379:632–635. doi: 10.1038/379632a0. [DOI] [PubMed] [Google Scholar]
- 19.Armağan C., Yılmaz C., Koç A., Abac A., Ülgenalp A., Böber E., Erçal D., Demir K. A toddler with a novel LEPR mutation. Hormones. 2019 doi: 10.1007/s42000-019-00097-6. [DOI] [PubMed] [Google Scholar]
- 20.Wasim M., Awan F.R., Najam S.S., Khan A.R., Khan H.N. Role of Leptin Deficiency, Inefficiency, and Leptin Receptors in Obesity. Biochem. Genet. 2016;54:565–572. doi: 10.1007/s10528-016-9751-z. [DOI] [PubMed] [Google Scholar]
- 21.Tartaglia L.A. The leptin receptor. J. Biol. Chem. 1997;272:6093–6096. doi: 10.1074/jbc.272.10.6093. [DOI] [PubMed] [Google Scholar]
- 22.Gorska E., Popko K., Stelmaszczyk-Emmel A., Ciepiela O., Kucharska A., Wasik M. Leptin receptors. Eur. J. Med. Res. 2010;15:50–54. doi: 10.1186/2047-783X-15-S2-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Fei H., Okano H.J., Li C., Lee G.H., Zhao C., Darnell R., Friedman J.M. Anatomic localization of alternatively spliced leptin receptors (Ob-R) in mouse brain and other tissues. Proc. Natl. Acad. Sci. USA. 1997;94:7001–7005. doi: 10.1073/pnas.94.13.7001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Yamashita T., Murakami T., Otani S., Kuwajima M., Shima K. Leptin receptor signal transduction: OBRa and OBRb of fa type. Biochem. Biophys. Res. Commun. 1998;246:752. doi: 10.1006/bbrc.1998.8689. [DOI] [PubMed] [Google Scholar]
- 25.Margetic S., Gazzola C., Pegg G.G., Hill R.A. Leptin: A review of its peripheral actions and interactions. Int. J. Obes. Relat. Metab. Disord. 2002;26:1407–1433. doi: 10.1038/sj.ijo.0802142. [DOI] [PubMed] [Google Scholar]
- 26.Frühbeck G. Intracellular signalling pathways activated by leptin. Biochem. J. 2006;393:7–20. doi: 10.1042/BJ20051578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Satoh N., Ogawa Y., Katsuura G., Numata Y., Tsuji T., Hayase M., Ebihara K., Masuzaki H., Hosoda K., Yoshimasa Y., et al. Sympathetic activation of leptin via the ventromedial hypothalamus: Leptin-induced increase in catecholamine secretion. Diabetes. 1999;48:1787–1793. doi: 10.2337/diabetes.48.9.1787. [DOI] [PubMed] [Google Scholar]
- 28.Dalamaga M., Chou S.H., Shields K., Papageorgiou P., Polyzos S.A., Mantzoros C.S. Leptin at the intersection of neuroendocrinology and metabolism: Current evidence and therapeutic perspectives. Cell Metabol. 2013;18:29–42. doi: 10.1016/j.cmet.2013.05.010. [DOI] [PubMed] [Google Scholar]
- 29.Fantuzzi G., Faggioni R. Leptin in the regulation of immunity, inflammation, and hematopoiesis. J. Leukoc. Biol. 2000;68:437–446. [PubMed] [Google Scholar]
- 30.Pérez-Pérez A., Vilariño-García T., Fernández-Riejos P., Martín-González J., Segura-Egea J.J., Sánchez-Margalet V. Role of leptin as a link between metabolism and the immune system. Cytokine Growth Factor Rev. 2017;35:71–84. doi: 10.1016/j.cytogfr.2017.03.001. [DOI] [PubMed] [Google Scholar]
- 31.Gainsford T., Willson T.A., Metcalf D., Handman E., McFarlane C., Nq A., Nicola N.A., Alexander W.S., Hilton D.J. Leptin can induce proliferation, differentiation, and functional activation of hemopoietic cells. Proc. Natl. Acad. Sci. USA. 1996;93:14564–14568. doi: 10.1073/pnas.93.25.14564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bennett B.D., Solar G.P., Yuan J.Q., Mathias J., Thomas G.R., Matthews W. A role for leptin and its cognate receptor in hematopoiesis. Curr. Biol. 1996;6:1170–1180. doi: 10.1016/S0960-9822(02)70684-2. [DOI] [PubMed] [Google Scholar]
- 33.Claycombe K., King L.E., Fraker P.J. A role for leptin in sustaining lymphopoiesis and myelopoiesis. Proc. Natl. Acad. Sci. USA. 2008;105:2017–2021. doi: 10.1073/pnas.0712053105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Han T.J., Wang X. Leptin and its receptor in hematologic malignancies. Int. J. Clin. Exp. Med. 2015;8:19840–19849. [PMC free article] [PubMed] [Google Scholar]
- 35.Ahima R.S., Prabakaran D., Mantzoros C., Qu D., Lowell B., Maratos-Flier E., Flier J.S. Role of leptin in the neuroendocrine response to fasting. Nature. 1996;382:250–252. doi: 10.1038/382250a0. [DOI] [PubMed] [Google Scholar]
- 36.Myers M.G., Jr., Heymsfield S.B., Haft C., Kahn B.B., Laughlin M., Leibel R.L., Tschöp M.H., Yanovski J.A. Challenges and opportunities of defining clinical leptin resistance. Cell Metabol. 2012;15:150–156. doi: 10.1016/j.cmet.2012.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Jung C.H., Kim M.S. Molecular mechanisms of central leptin resistance in obesity. Arch. Pharm. Res. 2013;36:201–207. doi: 10.1007/s12272-013-0020-y. [DOI] [PubMed] [Google Scholar]
- 38.Zoran D.L. Obesity in dogs and cats: A metabolic and endocrine disorder. Vet. Clin. North Am. Small Anim. Pract. 2010;40:221–239. doi: 10.1016/j.cvsm.2009.10.009. [DOI] [PubMed] [Google Scholar]
- 39.Packer M. Epicardial adipose tissue may mediate deleterious effects of obesity and inflammation on the myocardium. J. Am. Coll. Cardiol. 2018;71:2360–2372. doi: 10.1016/j.jacc.2018.03.509. [DOI] [PubMed] [Google Scholar]
- 40.Russo I. The prothrombotic tendency in metabolic syndrome: Focus on the potential mechanisms involved in impaired haemostasis and fibrinolytic balance. Scientifica. 2012;2012:525374. doi: 10.6064/2012/525374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Barbosa-Ferreira J.M., Fernandes F., Dabarian A., Mady C. Leptin in heart failure. Expert. Opin. Med. Diagn. 2013;7:113–117. doi: 10.1517/17530059.2013.735229. [DOI] [PubMed] [Google Scholar]
- 42.Chiba T., Shinozaki S., Nakazawa T., Kawakami A., Ai M., Kaneko E., Kitagawa M., Kondo K., Chait A., Shimokado K. Leptin deficiency suppresses progression of atherosclerosis in apoE-deficient mice. Atherosclerosis. 2008;196:68–75. doi: 10.1016/j.atherosclerosis.2007.01.040. [DOI] [PubMed] [Google Scholar]
- 43.Lopaschuk G.D., Folmes C.D., Stanley W.C. Cardiac energy metabolism in obesity. Circ. Res. 2007;101:335–347. doi: 10.1161/CIRCRESAHA.107.150417. [DOI] [PubMed] [Google Scholar]
- 44.Tune J.D., Considine R.V. Effects of leptin on cardiovascular physiology. J. Am. Soc. Hypertens. 2007;1:231–241. doi: 10.1016/j.jash.2007.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Balasubramanian P., Hall D., Subramanian M. Sympathetic nervous system as a target for aging and obesity-related cardiovascular diseases. Geroscience. 2019;41:13–24. doi: 10.1007/s11357-018-0048-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Oda A., Taniguchi T., Yokoyama M. Leptin stimulates rat aortic smooth muscle cell proliferation and migration. Kobe J. Med. Sci. 2001;47:141–150. doi: 10.1016/S0021-9150(97)89646-3. [DOI] [PubMed] [Google Scholar]
- 47.Fortuño A., Rodríguez A., Gómez-Ambrosi J., Muñiz P., Salvador J., Díez J., Frühbeck G. Leptin inhibits angiotensin II-induced intracellular calcium increase and vasoconstriction in the rat aorta. Endocrinology. 2002;143:3555–3560. doi: 10.1210/en.2002-220075. [DOI] [PubMed] [Google Scholar]
- 48.Suganami T., Mukoyama M., Mori K., Yokoi H., Koshikawa M., Sawai K., Hidaka S., Ebihara K., Tanaka T., Sugawara A., et al. Prevention and reversal of renal injury by leptin in a new mouse model of diabetic nephropathy. FASEB J. 2005;19:127–129. doi: 10.1096/fj.04-2183fje. [DOI] [PubMed] [Google Scholar]
- 49.Morales-Ruiz M., Fulton D., Sowa G., Languino L.R., Fujio Y., Walsh K., Sessa W.C. Vascular endothelial growth factor-stimulated actin reorganization and migration of endothelial cells is regulated via the serine/threonine kinase Akt. Circ. Res. 2000;86:892–896. doi: 10.1161/01.RES.86.8.892. [DOI] [PubMed] [Google Scholar]
- 50.Konturek P.C., Jaworek J., Maniatoglou A., Bonior J., Meixner H., Konturek S.J., Hahn E.G. Leptin modulates the inflammatory response in acute pancreatitis. Digestion. 2002;65:149–160. doi: 10.1159/000064935. [DOI] [PubMed] [Google Scholar]
- 51.Frossard J.L., Lescuyer P., Pastor C.M. Experimental evidence of obesity as a risk factor for severe acute pancreatitis. World J. Gastroenterol. 2009;15:5260–5265. doi: 10.3748/wjg.15.5260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Karpavicius A., Dambrauskas Z., Sileikis A., Vitkus D., Strupas K. Value of adipokines in predicting the severity of acute pancreatitis: Comprehensive review. World J. Gastroenterol. 2012;18:6620–6627. doi: 10.3748/wjg.v18.i45.6620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Konturek P.C., Konturek S.J., Brzozowski T., Jaworek J., Hahn E.G. Role of leptin in the stomach and the pancreas. J. Physiol. 2001;95:345–354. doi: 10.1016/S0928-4257(01)00047-X. [DOI] [PubMed] [Google Scholar]
- 54.Warzecha Z., Dembiński A., Ceranowicz P., Jaworek J., Konturek P.C., Dembiński M., Bilskl J., Konturek S.J. Influence of leptin administration on the course of acute ischemic pancreatitis. J. Physiol. Pharmacol. 2002;53:775–790. [PubMed] [Google Scholar]
- 55.Gultekin F.A., Kerem M., Tatlicioglu E., Aricioglu A., Unsal C., Bukan N. Leptin treatment ameliorates acute lung injury in rats with cerulein-induced acute pancreatitis. World J. Gastroenterol. 2007;13:2932–2938. doi: 10.3748/wjg.v13.i21.2932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Carbone F., La Rocca C., De Candia P., Procaccini C., Colamatteo A., Micillo T., De Rosa V., Matarese G. Metabolic control of immune tolerance in health and autoimmunity. Semin. Immunol. 2016;28:491–504. doi: 10.1016/j.smim.2016.09.006. [DOI] [PubMed] [Google Scholar]
- 57.Medina G., Vera-Lastra O., Peralta-Amaro A.L., Jiménez-Arellano M.P., Saavedra M.A., Cruz-Domínguez M.P., Jara L.J. Metabolic syndrome, autoimmunity and rheumatic diseases. Pharmacol. Res. 2018;133:277–288. doi: 10.1016/j.phrs.2018.01.009. [DOI] [PubMed] [Google Scholar]
- 58.Katona P., Katona-Apte J. The interaction between nutrition and infection. Clin. Infect. Dis. 2008;46:1582–1588. doi: 10.1086/587658. [DOI] [PubMed] [Google Scholar]
- 59.Farhadi S., Ovchinnikov R.S. The relationship between nutrition and infectious diseases: A review. Biomed. Biotechnol. Res. J. 2018;2:168–172. [Google Scholar]
- 60.Hennig B., Petriello M.C., Gamble M.V., Surh Y.J., Kresty L.A., Frank N., Rangkadilok N., Ruchirawat M., Suk W.A. The role of nutrition in influencing mechanisms involved in environmentally mediated diseases. Rev. Environ. Health. 2018;33:87–97. doi: 10.1515/reveh-2017-0038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Maurya R., Bhattacharya P., Dey R., Nakhasi H.L. Leptin Functions in Infectious Diseases. Front. Immunol. 2018;9:2741. doi: 10.3389/fimmu.2018.02741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Naylor C., Petri W.A., Jr. Leptin regulation of immune responses. Trends Mol. Med. 2016;22:88–98. doi: 10.1016/j.molmed.2015.12.001. [DOI] [PubMed] [Google Scholar]
- 63.Maldonado-Ruiz R., Fuentes-Mera L., Camacho A. Central modulation of neuroinflammation by neuropeptides and energy-sensing hormones during obesity. Biomed. Res. Int. 2017;2017:7949582. doi: 10.1155/2017/7949582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Lourenço E.V., Liu A., Matarese G., La Cava A. Leptin promotes systemic lupus erythematosus by increasing autoantibody production and inhibiting immune regulation. Proc. Natl. Acad. Sci. USA. 2016;113:10637–10642. doi: 10.1073/pnas.1607101113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Palatucci A.T., Piantedosi D., Rubino V., Giovazzino A., Guccione J., Pernice V., Ruggiero G., Cortese L., Terrazzano G. Circulating regulatory T cells (Treg), leptin and induction of proinflammatory activity in obese Labrador Retriever dogs. Vet. Immunol. Immunopathol. 2018;202:122–129. doi: 10.1016/j.vetimm.2018.07.004. [DOI] [PubMed] [Google Scholar]
- 66.Kawauchi I.M., Jeremias J.T., Takeara P., de Souza D.F., Balieiro J.C.C., Pfrimer K., Brunetto M.A., Pontieri C.F.F. Effect of dietary protein intake on the body composition and metabolic parameters of neutered dogs. J. Nutr. Sci. 2017;6:e40. doi: 10.1017/jns.2017.41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Kim A.Y., Kim H.S., Kang J.H., Yang M.P. Serum adipokine concentrations in dogs with diabetes mellitus: A pilot study. J. Vet. Sci. 2015;16:333–340. doi: 10.4142/jvs.2015.16.3.333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Lam Q.L., Lu L. Role of leptin in immunity. Cell. Mol. Immunol. 2007;4:1–13. [PubMed] [Google Scholar]
- 69.Francisco V., Pino J., Campos-Cabaleiro V., Ruiz-Fernández C., Mera A., Gonzalez-Gay M.A., Gómez R., Gualillo O. Obesity, fat mass and immune system: Role for leptin. Front. Physiol. 2018;9:640. doi: 10.3389/fphys.2018.00640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Friedman J.M., Halaas J.L. Leptin and the regulation of body weight in mammals. Nature. 1998;395:763–770. doi: 10.1038/27376. [DOI] [PubMed] [Google Scholar]
- 71.Tartaglia L.A., Dembski M., Weng X., Deng N., Culpepper J., Devos R., Richards G.J., Campfield L.A., Clark F.T., Deeds J., et al. Identification and expression cloning of a leptin receptor, OB-R. Cell. 1995;83:1263–1271. doi: 10.1016/0092-8674(95)90151-5. [DOI] [PubMed] [Google Scholar]
- 72.Matarese G., La Cava A. The intricate interface between immune system and metabolism. Trends Immunol. 2004;25:193–200. doi: 10.1016/j.it.2004.02.009. [DOI] [PubMed] [Google Scholar]
- 73.Chan J.L., Matarese G., Shetty G.K., Raciti P., Kelesidis I., Aufiero D., De Rosa V., Perna F., Fontana S., Mantzoros C.S. Differential regulation of metabolic, neuroendocrine, and immune function by leptin in humans. Proc. Natl. Acad. Sci. USA. 2006;103:8481–8486. doi: 10.1073/pnas.0505429103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Procaccini C., Jirillo E., Matarese G. Leptin as an immunomodulator. Mol. Aspects Med. 2012;33:35–45. doi: 10.1016/j.mam.2011.10.012. [DOI] [PubMed] [Google Scholar]
- 75.La Cava A., Matarese G. The weight of leptin in immunity. Nat. Rev. Immunol. 2004;4:371–379. doi: 10.1038/nri1350. [DOI] [PubMed] [Google Scholar]
- 76.Bernotiene E., Palmer G., Gabay C. The role of leptin in innate and adaptive immune responses. Arthritis. Res. Ther. 2006;8:217. doi: 10.1186/ar2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Hsu A., Aronoff D.M., Phipps J., Goel D., Mancuso P. Leptin improves pulmonary bacterial clearance and survival in ob/ob mice during pneumococcal pneumonia. Clin. Exp. Immunol. 2007;150:332–339. doi: 10.1111/j.1365-2249.2007.03491.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Gruen M.L., Hao M., Piston D.W., Hasty A.H. Leptin requires canonical migratory signaling pathways for induction of monocyte and macrophage chemotaxis. Am. J. Physiol. Cell Physiol. 2007;293:C1481–C1488. doi: 10.1152/ajpcell.00062.2007. [DOI] [PubMed] [Google Scholar]
- 79.Dib L.H., Ortega M.T., Fleming S.D., Chapes S.K., Melgarejo T. Bone marrow leptin signaling mediates obesity-associated adipose tissue inflammation in male mice. Endocrinology. 2014;155:40–46. doi: 10.1210/en.2013-1607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Conde J., Scotece M., Gómez R., Gómez-Reino J.J., Lago F., Gualillo O. At the crossroad between immunity and metabolism: Focus on leptin. Expert. Rev. Clin. Immunol. 2010;6:801–808. doi: 10.1586/eci.10.48. [DOI] [PubMed] [Google Scholar]
- 81.Sánchez-Pozo C., Rodriguez-Baño J., Domínguez-Castellano A., Muniain M.A., Goberna R., Sánchez-Margalet V. Leptin stimulates the oxidative burst in control monocytes but attenuates the oxidative burst in monocytes from HIV-infected patients. Clin. Exp. Immunol. 2003;134:464–469. doi: 10.1111/j.1365-2249.2003.02321.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Kohchi C., Inagawa H., Nishizawa T., Soma G. ROS and innate immunity. Anticancer Res. 2009;29:817–821. [PubMed] [Google Scholar]
- 83.Najib S., Sánchez-Margalet V. Human leptin promotes survival of human circulating blood monocytes prone to apoptosis by activation of p42/44 MAPK pathway. Cell Immunol. 2002;220:143–149. doi: 10.1016/S0008-8749(03)00027-3. [DOI] [PubMed] [Google Scholar]
- 84.Faggioni R., Feingold K.R., Grunfeld C. Leptin regulation of the immune response and the immunodeficiency of malnutrition. FASEB J. 2001;15:2565–2571. doi: 10.1096/fj.01-0431rev. [DOI] [PubMed] [Google Scholar]
- 85.Bruno A., Conus S., Schmid I., Simon H.U. Apoptotic pathways are inhibited by leptin receptor activation in neutrophils. J. Immunol. 2005;174:8090–8096. doi: 10.4049/jimmunol.174.12.8090. [DOI] [PubMed] [Google Scholar]
- 86.Zarkesh-Esfahani H., Pockley A.G., Wu Z., Hellewell P.G., Weetman A.P., Ross R.J. Leptin indirectly activates human neutrophils via induction of TNF-alpha. J. Immunol. 2004;172:1809–1814. doi: 10.4049/jimmunol.172.3.1809. [DOI] [PubMed] [Google Scholar]
- 87.Mattioli B., Straface E., Quaranta M.G., Giordani L., Viora M. Leptin promotes differentiation and survival of human dendritic cells and licenses them for Th1 priming. J. Immunol. 2005;174:6820–6828. doi: 10.4049/jimmunol.174.11.6820. [DOI] [PubMed] [Google Scholar]
- 88.Lam Q.L.K., Liu S., Cao X., Lu L. Involvement of leptin signaling in the survival and maturation of bone marrow-derived dendritic cells. Eur. J. Immunol. 2006;36:3118–3130. doi: 10.1002/eji.200636602. [DOI] [PubMed] [Google Scholar]
- 89.Laue T., Wrann C.D., Hoffmann-Castendiek B., Pietsch D., Hübner L., Kielstein H. Altered NK cell function in obese healthy humans. BMC Obes. 2015;2:1. doi: 10.1186/s40608-014-0033-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Jahn J., Spielau M., Brandsch C., Stangl G.I., Delank K.S., Bähr I., Berreis T., Wrann C.D., Kielstein H. Decreased NK cell functions in obesity can be reactivated by fat mass reduction. Obesity. 2015;23:2233–2241. doi: 10.1002/oby.21229. [DOI] [PubMed] [Google Scholar]
- 91.Tian Z., Sun R., Wei H., Gao B. Impaired natural killer (NK) cell activity in leptin receptor deficient mice: Leptin as a critical regulator in NK cell development and activation. Biochem. Biophys. Res. Commun. 2002;298:297–302. doi: 10.1016/S0006-291X(02)02462-2. [DOI] [PubMed] [Google Scholar]
- 92.Howard J.K., Lord G.M., Matarese G., Vendetti S., Ghatei M.A., Ritter M.A., Lechler R.I., Bloom S.R. Leptin protects mice from starvation-induced lymphoid atrophy and increases thymic cellularity in ob/ob mice. J. Clin. Investig. 1999;104:1051–1059. doi: 10.1172/JCI6762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Sánchez-Margalet V., Martín-Romero C., González-Yanes C., Goberna R., Rodríguez-Baño J., Muniain M.A. Leptin receptor (Ob-R) expression is induced in peripheral blood mononuclear cells by in vitro activation and in vivo in HIV-infected patients. Clin. Exp. Immunol. 2002;129:119–124. doi: 10.1046/j.1365-2249.2002.01900.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Martín-Romero C., Santos-Alvarez J., Goberna R., Sánchez-Margalet V. Human leptin enhances activation and proliferation of human circulating T lymphocytes. Cell Immunol. 2000;199:15–24. doi: 10.1006/cimm.1999.1594. [DOI] [PubMed] [Google Scholar]
- 95.Lord G.M., Matarese G., Howard J.K., Baker R.J., Bloom S.R., Lechler R.I. Leptin modulates the T-cell immune response and reverses starvation-induced immunosuppression. Nature. 1998;394:897–901. doi: 10.1038/29795. [DOI] [PubMed] [Google Scholar]
- 96.Batra A., Okur B., Glauben R., Erben U., Ihbe J., Stroh T., Fedke I., Chang H.D., Zeitz M., Siegmund B. Leptin: A critical regulator of CD4+ T-cell polarization in vitro and in vivo. Endocrinology. 2010;151:56–62. doi: 10.1210/en.2009-0565. [DOI] [PubMed] [Google Scholar]
- 97.Deng J., Liu Y., Yang M., Wang S., Zhang M., Wang X., Ko K.H., Hua Z., Sun L., Cao X., et al. Leptin exacerbates collagen-induced arthritis via enhancement of Th17 cell response. Arthritis Rheum. 2012;64:3564–3573. doi: 10.1002/art.34637. [DOI] [PubMed] [Google Scholar]
- 98.Reis B.S., Lee K., Fanok M.H., Mascaraque C., Amoury M., Cohn L.B., Rogoz A., Dallner O.S., Moraes-Vieira P.M., Domingos A.I., et al. Leptin receptor signaling in T cells is required for Th17 differentiation. J. Immunol. 2015;194:5253–5260. doi: 10.4049/jimmunol.1402996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Lam Q.L.K., Wang S., Ko O.K.H., Kincade P.W., Lu L. Leptin signaling maintains B-cell homeostasis via induction of Bcl-2 and Cyclin D1. Proc. Natl Acad. Sci. USA. 2010;107:13812–13817. doi: 10.1073/pnas.1004185107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Sakaguchi S. The origin of FOXP3-expressing CD4+ regulatory T cells: Thymus or periphery. J. Clin. Investig. 2003;112:1310–1312. doi: 10.1172/JCI200320274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.De Rosa V., Procaccini C., Calì G., Pirozzi G., Fontana S., Zappacosta S., La Cava A., Matarese G. A key role of leptin in the control of regulatory T cell proliferation. Immunity. 2007;26:241–245. doi: 10.1016/j.immuni.2007.01.011. [DOI] [PubMed] [Google Scholar]
- 102.Silva Morales M., Mueller D. Anergy into T regulatory cells: An integration of metabolic cues and epigenetic changes at the Foxp3 conserved non-coding sequence 2. F1000Research. 2018;7:1938. doi: 10.12688/f1000research.16551.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Kumar P., Bhattacharya P., Prabhakar B.S. A comprehensive review on the role of co-signaling receptors and Treg homeostasis in autoimmunity and tumor immunity. J. Autoimmun. 2018;95:77–99. doi: 10.1016/j.jaut.2018.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Matarese G., Procaccini C., De Rosa V., Horvath T.L. La Cava, A. Regulatory T cells in obesity: The leptin connection. Trends Mol. Med. 2010;16:247–256. doi: 10.1016/j.molmed.2010.04.002. [DOI] [PubMed] [Google Scholar]
- 105.Lopes J.E., Torgerson T.R., Schubert L.A., Anover S.D., Ocheltree E.L., Ochs H.D., Ziegler S.F. Analysis of FOXP3 reveals multiple domains required for its function as a transcriptional repressor. J. Immunol. 2006;177:3133–3142. doi: 10.4049/jimmunol.177.5.3133. [DOI] [PubMed] [Google Scholar]
- 106.Ito T., Hanabuchi S., Wang Y.H., Park W.R., Arima K., Bover L., Qin F.X., Gilliet M., Liu Y.J. Two functional subsets of FOXP3+ regulatory T cells in human thymus and periphery. Immunity. 2008;28:870–880. doi: 10.1016/j.immuni.2008.03.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Du J., Huang C., Zhou B., Ziegler S.F. Isoform-specific inhibition of ROR alpha-mediated transcriptional activation by human FOXP3. J. Immunol. 2008;180:4785–4792. doi: 10.4049/jimmunol.180.7.4785. [DOI] [PubMed] [Google Scholar]
- 108.Zhou L., Lopes J.E., Chong M.M., Ivanov I.I., Min R., Victora G.D., Shen Y., Du J., Rubtsov Y.P., Rudensky A.Y., et al. TGF-beta-induced Foxp3 inhibits T(H)17 cell differentiation by antagonizing RORgammat function. Nature. 2008;453:236–240. doi: 10.1038/nature06878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Sambucci M., Gargano F., De Rosa V., De Bardi M., Picozza M., Placido R., Ruggieri S., Capone A., Gasperini C., Matarese G., et al. FoxP3 isoforms and PD-1 expression by T regulatory cells in multiple sclerosis. Sci. Rep. 2018;8:3674. doi: 10.1038/s41598-018-21861-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.De Rosa V., Galgani M., Porcellini A., Colamatteo A., Santopaolo M., Zuchegna C., Romano A., De Simone S., Procaccini C., La Rocca C., et al. Glycolysis controls the induction of human regulatory T cells by modulating the expression of FOXP3 exon 2 splicing variants. Nat. Immunol. 2015;16:1174–1184. doi: 10.1038/ni.3269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Mailer R.K., Joly A.L., Liu S., Elias S., Tegner J., Andersson J. IL-1β promotes Th17 differentiation by inducing alternative splicing of FOXP3. Sci. Rep. 2015;5:14674. doi: 10.1038/srep14674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.McLeod L.E., Proud C.G. ATP depletion increases phosphorylation of elongation factor eEF2 in adult cardiomyocytes independently of inhibition of mTOR signalling. FEBS Lett. 2002;531:448–452. doi: 10.1016/S0014-5793(02)03582-2. [DOI] [PubMed] [Google Scholar]
- 113.Laplante M., Sabatini D.M. mTOR signaling at a glance. J. Cell. Sci. 2009;122:3589–3594. doi: 10.1242/jcs.051011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Galgani M., Procaccini C., De Rosa V., Carbone F., Chieffi P., La Cava A., Matarese G. Leptin modulates the survival of autoreactive CD4+ T cells through the nutrient/energy-sensing mammalian target of rapamycin signaling pathway. J. Immunol. 2010;185:7474–7479. doi: 10.4049/jimmunol.1001674. [DOI] [PubMed] [Google Scholar]
- 115.Zeng H., Yang K., Cloer C., Neale G., Vogel P., Chi H. mTORC1 couples immune signals and metabolic programming to establish T(reg)-cell function. Nature. 2013;499:485–490. doi: 10.1038/nature12297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Wang R., Dillon C.P., Shi L.Z., Milasta S., Carter R., Finkelstein D., McCormick L.L., Fitzgerald P., Chi H., Munger J., et al. The transcription factor Myc controls metabolic reprogramming upon T lymphocyte activation. Immunity. 2011;35:871–882. doi: 10.1016/j.immuni.2011.09.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Donnelly R.P., Finlay D.K. Glucose, glycolysis and lymphocyte responses. Mol. Immunol. 2015;68:513–519. doi: 10.1016/j.molimm.2015.07.034. [DOI] [PubMed] [Google Scholar]
- 118.Blagih J., Coulombe F., Vincent E.E., Dupuy F., Galicia-Vázquez G., Yurchenko E., Raissi T.C., van der Windt G.J., Viollet B., Pearce E.L., et al. The energy sensor AMPK regulates T cell metabolic adaptation and effector responses in vivo. Immunity. 2015;42:41–54. doi: 10.1016/j.immuni.2014.12.030. [DOI] [PubMed] [Google Scholar]
- 119.Loftus R.M., Finlay D.K. Immunometabolism: Cellular metabolism turns immune regulator. J. Biol. Chem. 2016;291:1–10. doi: 10.1074/jbc.R115.693903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Gerriets V.A., Rathmell J.C. Metabolic pathways in T cell fate and function. Trends Immunol. 2012;33:168–173. doi: 10.1016/j.it.2012.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Procaccini C., Carbone F., Galgani M., La Rocca C., De Rosa V., Cassano S., Matarese G. Obesity and susceptibility to autoimmune diseases. Expert. Rev. Clin. Immunol. 2011;7:287–294. doi: 10.1586/eci.11.18. [DOI] [PubMed] [Google Scholar]
- 122.Lee B.C., Lee J. Cellular and molecular players in adipose tissue inflammation in the development of obesity-induced insulin resistance. Biochim. Biophys Acta. 2014;1842:446–462. doi: 10.1016/j.bbadis.2013.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Wang M., Chen F., Wang J., Zeng Z., Yang Q., Shao S. Th17 and Treg lymphocytes in obesity and Type 2 diabetic patients. Clin. Immunol. 2018;197:77–78. doi: 10.1016/j.clim.2018.09.005. [DOI] [PubMed] [Google Scholar]
- 124.Yun J.M., Jialal I., Devaraj S. Effects of epigallocatechin gallate on regulatory T cell number and function in obese v. lean volunteers. Br. J. Nutr. 2010;103:1771–1777. doi: 10.1017/S000711451000005X. [DOI] [PubMed] [Google Scholar]
- 125.Wagner N.M., Brandhorst G., Czepluch F., Lankeit M., Eberle C., Herzberg S., Faustin V., Riggert J., Oellerich M., Hasenfuss G., et al. Circulating regulatory T cells are reduced in obesity and may identify iubjects at increased metabolic and cardiovascular risk. Obesity. 2013;2:461–468. doi: 10.1002/oby.20087. [DOI] [PubMed] [Google Scholar]
- 126.Deiuliis J., Shah Z., Shah N., Needleman B., Mikami D., Narula V., Perry K., Hazey J., Kampfrath T., Kollengode M., et al. Visceral adipose inflammation in obesity is associated with critical alterations in T regulatory cell numbers. PLoS ONE. 2011;6:e16376. doi: 10.1371/journal.pone.0016376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Taleb S., Herbin O., Ait-Oufella H., Verreth W., Gourdy P., Barateau V., Merval R., Esposito B., Clément K., Holvoet P., et al. Defective leptin/leptin receptor signaling improves regulatory T cell immune response and protects mice from atherosclerosis. Arterioscler. Thromb. Vasc. Biol. 2007;27:2691–2698. doi: 10.1161/ATVBAHA.107.149567. [DOI] [PubMed] [Google Scholar]
- 128.Antuna-Puente B., Feve B., Fellahi S., Bastard J.P. Adipokines: The missing link between insulin resistance and obesity. Diabetes Metab. 2008;34:2–11. doi: 10.1016/j.diabet.2007.09.004. [DOI] [PubMed] [Google Scholar]
- 129.Tvarijonaviciute A., Tecles F., Martinez-Subiela S., Ceron J.J. Effect of weight loss on inflammatory biomarkers in obese dogs. Vet. J. 2012;193:570–572. doi: 10.1016/j.tvjl.2012.02.015. [DOI] [PubMed] [Google Scholar]
- 130.Wakshlag J.J., Struble A.M., Levine C.B., Bushey J.J., Laflamme D.P., Long G.M. The effects of weight loss on adipokines and markers of inflammation in dogs. Br. J. Nutr. 2011;106:S11–S14. doi: 10.1017/S0007114511000560. [DOI] [PubMed] [Google Scholar]
- 131.Bastien B.C., Patil A., Satyaraj E. The impact of weight loss on circulating cytokines in Beagle dogs. Vet. Immunol. Immunopathol. 2015;163:174–182. doi: 10.1016/j.vetimm.2014.12.003. [DOI] [PubMed] [Google Scholar]
- 132.Sagawa M.M., Nakadomo F., Honjoh T., Ishioka K., Saito M. Correlation between plasma leptin concentration and body fat content in dogs. Am. J. Vet. Res. 2002;63:7–10. doi: 10.2460/AJVR.2002.63.7. [DOI] [PubMed] [Google Scholar]
- 133.Ishioka K., Soliman M.M., Sagawa M., Nakadomo F., Shibata H., Honjoh T., Hashimoto A., Kitamura H., Kimura K., Saito M. Experimental and clinical studies on plasma leptin in obese dogs. J. Vet. Med. Sci. 2002;64:349–353. doi: 10.1292/jvms.64.349. [DOI] [PubMed] [Google Scholar]
- 134.Ishioka K., Hosoya K., Kitagawa H., Shibata H., Honjoh T., Kimura K., Saito M. Plasma leptin concentration in dogs: Effects of body condition score, age, gender and breeds. Res. Vet. Sci. 2007;82:11–15. doi: 10.1016/j.rvsc.2006.06.002. [DOI] [PubMed] [Google Scholar]
- 135.Jeusette I.C., Detilleux J., Shibata H., Saito M., Honjoh T., Delobel A., Istasse L., Diez M. Effects of chronic obesity and weight loss on plasma ghrelin and leptin concentrations in dogs. Res. Vet. Sci. 2005;79:169–175. doi: 10.1016/j.rvsc.2004.11.012. [DOI] [PubMed] [Google Scholar]
- 136.Segal K.R., Landt M., Klein S. Relationship between insulin sensitivity and plasma leptin concentration in lean and obese men. Diabetes. 1996;45:988–991. doi: 10.2337/diab.45.7.988. [DOI] [PubMed] [Google Scholar]
- 137.Gayet C., Bailhache E., Dumon H., Martin L., Siliart B., Nguyen P. Insulin resistance and changes in plasma concentration of TNFalpha, IGF1, and NEFA in dogs during weight gain and obesity. J. Anim. Physiol. Anim. Nutr. 2004;88:157–165. doi: 10.1111/j.1439-0396.2003.00473.x. [DOI] [PubMed] [Google Scholar]
- 138.Veiga A.P.M., Price C.A., de Oliveira S.T., dos Santos A.P., Campos R., Barbosa P.R., Gonzalez F.H.D. Association of canine obesity with reduced serum levels of C-reactive protein. J. Vet. Diagn. Investig. 2008;20:224–228. doi: 10.1177/104063870802000214. [DOI] [PubMed] [Google Scholar]
- 139.Van de Velde H., Janssens G.P., Stuyven E., Cox E., Buyse J., Hesta M. Short-term increase of body weight triggers immunological variables in dogs. Vet. Immunol. Immunopathol. 2012;145:431–437. doi: 10.1016/j.vetimm.2011.12.021. [DOI] [PubMed] [Google Scholar]
- 140.Van de Velde H., Janssens G.P., Rochus K., Duchateau L., Scharek-Tedin L., Zentek J., Nguyen P., Cox E., Buyse J., Biourge V., et al. Proliferation capacity of T-lymphocytes is affected transiently after a long-term weight gain in Beagle dogs. Vet. Immunol. Immunopathol. 2013;152:237–244. doi: 10.1016/j.vetimm.2012.12.011. [DOI] [PubMed] [Google Scholar]
- 141.Frank L., Mann S., Levine C.B., Cummings B.P., Wakshlag J.J. Increasing body condition score is positively associated interleukin-6 and monocyte chemoattractant protein-1 in Labrador retrievers. Vet. Immunol. Immunopathol. 2015;167:104–109. doi: 10.1016/j.vetimm.2015.07.010. [DOI] [PubMed] [Google Scholar]
- 142.Piantedosi D., Di Loria A., Guccione J., De Rosa A., Fabbri S., Cortese L., Carta S., Ciaramella P. Serum biochemistry profile, inflammatory cytokines, adipokines and cardiovascular findings in obese dogs. Vet. J. 2016;216:72–78. doi: 10.1016/j.tvjl.2016.07.002. [DOI] [PubMed] [Google Scholar]
- 143.Wieland C.W., Florquin S., Chan E.D., Leemans J.C., Weijer S., Verbon A., Fantuzzi G., van der Poll T. Pulmonary Mycobacterium tuberculosis infection in leptin deficient ob/ob mice. Int. Immunol. 2005;17:1399–1408. doi: 10.1093/intimm/dxh317. [DOI] [PubMed] [Google Scholar]
- 144.Vedantama G., Viswanathana V.K. Leptin signaling protects the gut from Entamoeba histolytica infection. Gut Microbes. 2012;3:1. doi: 10.4161/gmic.19424. [DOI] [PubMed] [Google Scholar]
- 145.Madan R., Guo X., Naylor C., Buonomo E.L., Mackay D., Noor Z., Concannon P., Scully K.W., Pramoonjago P., Kolling G.L., et al. Role of leptin-mediated colonic inflammation in defense against Clostridium difficile Colitis. Infect. Immun. 2014;82:341–349. doi: 10.1128/IAI.00972-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Shivahare R., Ali W., Vishwakarma P., Natu S.M., Puri S.K., Gupta S. Leptin augments protective immune responses in murine macrophages and enhances potential of miltefosine against experimental visceral leishmaniasis. Acta. Tropica. 2015;150:35–41. doi: 10.1016/j.actatropica.2015.06.024. [DOI] [PubMed] [Google Scholar]
- 147.Dayakar A., Chandrasekaran S., Veronica J. Maurya, R.S. Leptin induces the phagocytosis and protective immune response in Leishmania donovani infected THP-1 cell line and human PBMCs. Exp. Parasitol. 2016;160:54–59. doi: 10.1016/j.exppara.2015.12.002. [DOI] [PubMed] [Google Scholar]
- 148.Rodríguez L., Graniel J., Ortiz R. Effect of leptin on activation and cytokine synthesis in peripheral blood lymphocytes of malnourished infected children. Clin. Exp. Immunol. 2007;148:478–485. doi: 10.1111/j.1365-2249.2007.03361.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Ehrlich A., Moreno Castilho T., Goldsmith-Pestana K., Chae W.J., Bothwell A.L., Sparwasser T., McMahon-Pratt D. The immunotherapeutic role of regulatory T cells in Leishmania (Viannia) panamensis infection. J. Immunol. 2014;193:2961–2970. doi: 10.4049/jimmunol.1400728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Cortese L., Annunziatella M., Palatucci A.T., Rubino V., Piantedosi D., Di Loria A., Ruggiero G., Ciaramella P., Terrazzano G. Regulatory T cells, Cytotoxic T lymphocytes and a T(H)1 cytokine profile in dogs naturally infected by Leishmania infantum. Res. Vet. Sci. 2013;95:942–949. doi: 10.1016/j.rvsc.2013.08.005. [DOI] [PubMed] [Google Scholar]
- 151.Adalid-Peralta L., Fragoso G., Fleury A., Sciutto E. Mechanisms underlying the induction of regulatory T cells and its relevance in the adaptive immune response in parasitic infections. Int. J. Biol. Sci. 2011;7:1412–1426. doi: 10.7150/ijbs.7.1412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Di Loria A., Squillacioti C., De Luca A., Veneziano V., Mirabella N., Guccione J., Santoro D. Increased leptin mRNA expression in the blood of dogs naturally infected by Leishmania infantum. Vet. J. 2014;202:634–636. doi: 10.1016/j.tvjl.2014.10.010. [DOI] [PubMed] [Google Scholar]
- 153.Chang S., Buzdar A.U., Hursting S.D. Inflammatory breast cancer and body mass index. J. Clin. Oncol. 1998;16:3731–3735. doi: 10.1200/JCO.1998.16.12.3731. [DOI] [PubMed] [Google Scholar]
- 154.Marconato L., Romanelli G., Stefanello D., Giacoboni C., Bonfanti U., Bettini G., Finotello R., Verganti S., Valenti P., Ciaramella L. Prognostic factors for dogs with mammary inflammatory carcinoma: 43 cases (2003–2008) J. Am. Vet. Med. Assoc. 2009;235:967–972. doi: 10.2460/javma.235.8.967. [DOI] [PubMed] [Google Scholar]
- 155.Chan D.S., Vieira A.R., Aune D., Bandera E.V., Greenwood D.C., McTiernan A., Navarro Rosenblatt D., Thune I., Vieira R., Norat T. Body mass index and survival in women with breast cancer-systematic literature review and meta-analysis of 82 follow-up studies. Ann. Oncol. 2014;25:1901–1914. doi: 10.1093/annonc/mdu042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Lim H.Y., Im K.S., Kim N.H., Kim H.W., Shin J.I., Yhee J.Y., Sur J.H. Effects of obesity and obesity-related molecules on canine mammary gland tumors. Vet. Pathol. 2015;52:1045–1051. doi: 10.1177/0300985815579994. [DOI] [PubMed] [Google Scholar]
- 157.Lorincz A.M., Sukumar S. Molecular links between obesity and breast cancer. Endocr. Relat. Cancer. 2006;13:279–292. doi: 10.1677/erc.1.00729. [DOI] [PubMed] [Google Scholar]
- 158.Laud K., Gourdou I., Pessemesse L., Peyrat J., Djiane J. Identification of leptin receptors in human breast cancer: Functional activity in the T47-D breast cancer cell line. Mol. Cell. Endocrinol. 2002;188:219–226. doi: 10.1016/S0303-7207(01)00678-5. [DOI] [PubMed] [Google Scholar]
- 159.Jardé T., Caldefie-Chezet F., Damez M., Mishellany F., Penault-Llorca F., Guillot J., Vasson M.P. Leptin and leptin receptor involvement in cancer development: A study on human primary breast carcinoma. Oncol. Rep. 2008;19:905–912. doi: 10.3892/or.19.4.905. [DOI] [PubMed] [Google Scholar]
- 160.Jardé T., Perrier S., Vasson M.P., Caldefie-Chézet F. Molecular mechanisms of leptin and adiponectin in breast cancer. Eur. J. Cancer. 2011;47:33–43. doi: 10.1016/j.ejca.2010.09.005. [DOI] [PubMed] [Google Scholar]
- 161.Ray A. Cancer and comorbidity: The role of leptin in breast cancer and associated pathologies. World J. Clin. Cases. 2018;6:483–492. doi: 10.12998/wjcc.v6.i12.483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Rose D.P., Gilhooly E.M., Nixon D.W. Adverse effects of obesity on breast cancer prognosis, and the biological actions of leptin. Int. J. Oncol. 2002;21:1285. doi: 10.3892/ijo.21.6.1285. [DOI] [PubMed] [Google Scholar]
- 163.Ghanim H., Aljada A., Hofmeyer D., Syed T., Mohanty P., Dandona P. Circulating mononuclear cells in the obese are in a proinflammatory state. Circulation. 2004;110:1564–1571. doi: 10.1161/01.CIR.0000142055.53122.FA. [DOI] [PubMed] [Google Scholar]
- 164.Nicolini A., Carpi A., Rossi G. Cytokines in breast cancer. Cytokine Growth Factor Rev. 2006;17:325–337. doi: 10.1016/j.cytogfr.2006.07.002. [DOI] [PubMed] [Google Scholar]
- 165.Morris P.G., Hudis C.A., Giri D., Morrow M., Falcone D.J., Zhou X.K., Du B., Brogi E., Crawford C.B., Kopelovich L. Inflammation and increased aromatase expression occur in the breast tissue of obese women with breast cancer. Cancer Prev. Res. 2011;4:1021–1029. doi: 10.1158/1940-6207.CAPR-11-0110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Arendt L.M., McCready J., Keller P.J., Baker D.D., Naber S.P., Seewaldt V., Kuperwasser C. Obesity promotes breast cancer by CCL2-mediated macrophage recruitment and angiogenesis. Cancer Res. 2013;73:6080–6093. doi: 10.1158/0008-5472.CAN-13-0926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Qian B.Z., Li J., Zhang H., Kitamura T., Zhang J., Campion L.R., Kaiser E.A., Snyder L.A., Pollard J.W. CCL2 recruits inflammatory monocytes to facilitate breast-tumour metastasis. Nature. 2011;475:222–225. doi: 10.1038/nature10138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Bhardwaj P., Du B., Zhou X.K., Sue E., Harbus M.D., Falcone D.J., Giri D., Hudis C.A., Kopelovich L., Subbaramaiah K. Caloric restriction reverses obesity- induced mammary gland inflammation in mice. Cancer Prev. Res. 2013;6:282–289. doi: 10.1158/1940-6207.CAPR-12-0467. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 169.Mehlman E., Bright J.M., Jeckel K., Porsche C., Veeramachaneni D.N., Frye M. Echocardiographic evidence of left ventricular hypertrophy in obese dogs. J. Vet. Intern. Med. 2013;27:62–68. doi: 10.1111/jvim.12018. [DOI] [PubMed] [Google Scholar]
- 170.Adolphe J.L., Silver T.I., Childs H., Drew M.D., Weber L.P. Short-term obesity results in detrimental metabolic and cardiovascular changes that may not be reversed with weight loss in an obese dog model. Br. J. Nutr. 2014;112:647–656. doi: 10.1017/S0007114514001214. [DOI] [PubMed] [Google Scholar]
- 171.Tropf M., Nelson O.L., Lee P.M., Weng H.Y. Cardiac and metabolic variables in obese dogs. J. Vet. Intern. Med. 2017;31:1000–1007. doi: 10.1111/jvim.14775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Fonfara S., Hetzel U., Tew S.R., Dukes-McEwan J., Cripps P., Clegg P.D. Leptin expression in dogs with cardiac disease and congestive heart failure. J. Vet. Intern. Med. 2011;25:1017–1024. doi: 10.1111/j.1939-1676.2011.00782.x. [DOI] [PubMed] [Google Scholar]
- 173.Kim H.S., Kang J.H., Jeung E.B., Yang M.P. Serum concentrations of leptin and adiponectin in dogs with myxomatous mitral valve disease. J. Vet. Intern. Med. 2016;30:1589–1600. doi: 10.1111/jvim.14570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Cuspidi C., Rescaldani M., Sala C., Grassi G. Left-ventricular hypertrophy and obesity: A systematic review and meta-analysis of echocardiographic studies. J. Hypertens. 2014;32:16–25. doi: 10.1097/HJH.0b013e328364fb58. [DOI] [PubMed] [Google Scholar]
- 175.Murdolo G., Angeli F., Reboldi G., Di Giacomo L., Aita A., Bartolini C., Vedecchia P. Left ventricular hypertrophy and obesity: Only a matter of fat? High Blood Press. Cardiovasc. Prev. 2015;22:29–41. doi: 10.1007/s40292-014-0068-x. [DOI] [PubMed] [Google Scholar]
- 176.Pérez-Sánchez A.P., Del-Angel-Caraza J., Quijano-Hernández I.A., Barbosa-Mireles M.A. Obesity-hypertension and its relation to other diseases in dogs. Vet. Res. Commun. 2015;39:45–51. doi: 10.1007/s11259-015-9630-9. [DOI] [PubMed] [Google Scholar]
- 177.Verwaerde P., Sénard J.M., Galinier M., Rougé P., Massabuau P., Galitzky J., Berlan M., Lafontan M., Montastruc J.L. Changes in short-term variability of blood pressure and heart rate during the development of obesity-associated hypertension in high-fat fed dogs. J. Hypertens. 1999;17:1135–1143. doi: 10.1097/00004872-199917080-00013. [DOI] [PubMed] [Google Scholar]
- 178.Montoya J.A., Morris P.J., Bautista I., Juste M.C., Suarez L., Peña C., Hackett R.M., Rawlings J. Hypertension: A risk factor associated with weight status in dogs. J. Nutr. 2006;136:2011S–2013S. doi: 10.1093/jn/136.7.2011S. [DOI] [PubMed] [Google Scholar]
- 179.Schulze P.C., Kratzsch J. Leptin as a new diagnostic tool in chronic heart failure. Clin. Chim. Acta. 2005;362:1–11. doi: 10.1016/j.cccn.2005.05.019. [DOI] [PubMed] [Google Scholar]
- 180.Purdham D.M., Zou M.X., Rajapurohitam V. Rat heart is a site of leptin production and action. Am. J. Physiol. Heart. Circ. Physiol. 2004;287:H2877–H2884. doi: 10.1152/ajpheart.00499.2004. [DOI] [PubMed] [Google Scholar]
- 181.Karmazyn M., Purdham D.M., Rajapurohitam V., Zeidan A. Leptin as a cardiac hypertrophic factor: A potential target for therapeutics. Trends Cardiovasc. Med. 2007;17:206–211. doi: 10.1016/j.tcm.2007.06.001. [DOI] [PubMed] [Google Scholar]
- 182.Sierra-Honigmann M.R., Nath A.K., Murakami C., García-Cardeña G., Papapetropoulos A., Sessa W.C., Madge L.A., Schechner J.S., Schwabb M.B., Polverini P.J., et al. Biological action of leptin as an angiogenic factor. Science. 1998;281:1683–1686. doi: 10.1126/science.281.5383.1683. [DOI] [PubMed] [Google Scholar]
- 183.Sweeney G. Cardiovascular effects of leptin. Nat. Rev. Cardiol. 2010;7:22–29. doi: 10.1038/nrcardio.2009.224. [DOI] [PubMed] [Google Scholar]
- 184.Sharma V., McNeill J.H. The emerging roles of leptin and ghrelin in cardiovascular physiology and pathophysiology. Curr. Vasc. Pharmacol. 2005;3:169–180. doi: 10.2174/1570161053586868. [DOI] [PubMed] [Google Scholar]
- 185.Cheng K.H., Chu C.S., Lee K.T., Lin T.H., Hsieh C.C., Chiu C.C., Voon W.C., Sheu S.H., Lai W.T. Adipocytokines and proinflammatory mediators from abdominal and epicardial adipose tissue in patients with coronary artery disease. Int. J. Obes. 2008;32:268–274. doi: 10.1038/sj.ijo.0803726. [DOI] [PubMed] [Google Scholar]
- 186.Knudson J.D., Payne G.A., Borbouse L., Tune J.D. Leptin and mechanisms of endothelial dysfunction and cardiovascular disease. Curr. Hypertens. Rep. 2008;10:434–439. doi: 10.1007/s11906-008-0082-2. [DOI] [PubMed] [Google Scholar]
- 187.Anker S.D., Chua T.P., Ponikowski P., Hrrington D., Swan J.W., Kox W.J., Poole-Wilson P.A., Coats A.J. Hormonal changes and catabolic/anabolic imbalance in chronic heart failure and their importance for cardiac cachexia. Circulation. 1997;96:526–534. doi: 10.1161/01.CIR.96.2.526. [DOI] [PubMed] [Google Scholar]
- 188.Doehner W., Pflaum C.D., Rauchhaus M., Godsland I.F., Egerer K., Cicoira M., Florea V.G., Sharma R., Bolger A.P., Coats A.J., et al. Leptin, insulin sensitivity and growth hormone binding protein in chronic heart failure with and without cardiac cachexia. Eur. J. Endocrinol. 2001;145:727–735. doi: 10.1530/eje.0.1450727. [DOI] [PubMed] [Google Scholar]
- 189.Haynes W.G., Morgan D.A., Walsh S.A., Mark A.L., Sivitz W.I. Receptor- mediated regional sympathetic nerve activation by leptin. J. Clin. Investig. 1997;100:270–278. doi: 10.1172/JCI119532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Atkinson L.L., Fischer M.A., Lopaschuk G.D. Leptin activates cardiac fatty acid oxidation independent of changes in the AMP-activated protein kinase-acetyl-CoA carboxylase-malonyl- CoA axis. J. Biol. Chem. 2002;277:29424–29430. doi: 10.1074/jbc.M203813200. [DOI] [PubMed] [Google Scholar]
- 191.Schram K., De Girolamo S., Madani S., Munoz D., Thong F., Sweeney G. Leptin regulates MMP-2, TIMP-1 and collagen synthesis via p38 MAPK in HL-1 murine cardiomyocytes. Cell Mol. Biol. Lett. 2010;15:551–563. doi: 10.2478/s11658-010-0027-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Barouch L.A., Gao D., Chen L., Miller K.L., Xu W., Phan A.C., Kittleson M.M., Minhas K.M., Berkowitz D.E., Wei C., et al. Cardiac myocyte apoptosis is associated with increased DNA damage and decreased survival in murine models of obesity. Circ. Res. 2006;98:119–124. doi: 10.1161/01.RES.0000199348.10580.1d. [DOI] [PubMed] [Google Scholar]
- 193.McGaffin K.R., Witham W.G., Yester K.A., Romano L.C., O’Doherty R.M., McTiernan C.F., O’Donnell C.P. Cardiac-specific leptin receptor deletion exacerbates ischaemic heart failure in mice. Cardiovasc. Res. 2011;89:60–71. doi: 10.1093/cvr/cvq288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Mazaki-Tovi M., Feuermann Y., Segev G., Klement E., Yas-Natan E., Farkas A., Kol A., Shamay A. Increased serum leptin and insulin concentrations in canine hypothyroidism. Vet. J. 2010;183:109–114. doi: 10.1016/j.tvjl.2008.08.017. [DOI] [PubMed] [Google Scholar]
- 195.Greene V.R., Wilson H., Pfent C., Roethele J., Carwile J., Qin Y., Grimm E., Ellerhorst J.A. Expression of leptin and iNOS in oral melanomas in dogs. J. Vet. Intern. Med. 2013;27:1278–1282. doi: 10.1111/jvim.12169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Schaffler A., Landfried K., Volk M., Fürst A., Büchler C., Schölmerich J., Herfarth H. Potential of adipocytokines in predicting peripancreatic necrosis and severity in acute pancreatitis: Pilot study. J. Gastroenterol. Hepatol. 2007;22:326–334. doi: 10.1111/j.1440-1746.2006.04364.x. [DOI] [PubMed] [Google Scholar]
- 197.Sharma A., Muddana V., Lamb J., Greer J., Papachristou G.I., Whitcomb D.C. Low serum adiponectin levels are associated with systemic organ failure in acute pancreatitis. Pancreas. 2009;38:907–912. doi: 10.1097/MPA.0b013e3181b65bbe. [DOI] [PubMed] [Google Scholar]
- 198.Schaffler A., Hamer O., Dickopf J., Goetz A., Landfried K., Voelk M., Herfarth H., Kopp A., Büchler C., Schölmerich J., et al. Admission resistin levels predict peripancreatic necrosis and clinical severity in acute pancreatitis. Am. J. Gastroenterol. 2010;105:2474–2484. doi: 10.1038/ajg.2010.278. [DOI] [PubMed] [Google Scholar]
- 199.Schaffler A., Hamer O.W., Dickopf J., Goetz A., Landfried K., Voelk M., Herfarth H., Kopp A., Buechler C., Schölmerich J., et al. Admission visfatin levels predict pancreatic and peripancreatic necrosis in acute pancreatitis and correlate with clinical severity. Am. J. Gastroenterol. 2011;106:957–967. doi: 10.1038/ajg.2010.503. [DOI] [PubMed] [Google Scholar]
- 200.Kerem M., Bedirli A., Pasaoglu H., Unsal C., Yilmaz T.U., Ofluoglu E., Sahin T.T. Role of ghrelin and leptin in predicting the severity of acute pancreatitis. Dig. Dis. Sci. 2007;52:950–955. doi: 10.1007/s10620-006-9150-0. [DOI] [PubMed] [Google Scholar]
- 201.Zyromski N.J., Mathur A., Pitt H.A., Lu D., Gripe J.T., Walker J.J., Yancey K., Wade T.E., Swartz-Basile D.A. A murine model of obesity implicates the adipokine milieu in the pathogenesis of severe acute pancreatitis. Am. J. Physiol. Gastrointest. Liver Physiol. 2008;295:G552–G558. doi: 10.1152/ajpgi.90278.2008. [DOI] [PubMed] [Google Scholar]
- 202.Franco-Pons N., Gea-Sorlì S., Closa D. Release of inflammatory mediators by adipose tissue during acute pancreatitis. J. Pathol. 2010;221:175–182. doi: 10.1002/path.2691. [DOI] [PubMed] [Google Scholar]
- 203.Paek J., Kang J.H., Kim H.S., Lee I., Seo K.W., Yang M.P. Serum adipokine concentrations in dogs with acute pancreatitis. J. Vet. Intern. Med. 2014;28:1760–1769. doi: 10.1111/jvim.12437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Lee S., Lee A., Kweon O.K., Kim W.H. Presence and distribution of leptin and leptin receptor in the canine gallbladder. Acta Histochem. 2016;118:674–678. doi: 10.1016/j.acthis.2016.09.002. [DOI] [PubMed] [Google Scholar]
- 205.Lee S., Kweon O.K., Kim W.H. Increased leptin and leptin receptor expression in dogs with gallbladder mucocele. J. Vet. Intern. Med. 2017;31:36–42. doi: 10.1111/jvim.14612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Haluzík M., Fiedler J., Nedvidkova J., Ceska R. Serum leptin concentrations in patients with combined hyperlipidemia: Relationship to serum lipids and lipoproteins. Physiol. Res. 1998;48:363–368. [PubMed] [Google Scholar]
- 207.Haluzík M., Fiedler J., Nedvídkova J., Ceska R. Serum leptin levels in patients with hyperlipidemias. Nutrition. 2000;16:429–433. doi: 10.1016/S0899-9007(00)00288-4. [DOI] [PubMed] [Google Scholar]
- 208.Park H.J., Lee S.E., Oh J.H., Seo K.W., Song K.H. Leptin, adiponectin and serotonin levels in lean and obese dogs. BMC Vet. Res. 2014;10:113. doi: 10.1186/1746-6148-10-113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209.Gonzaga N.C., Medeiros C.C., de Carvalho D.F., Alves J.G. Leptin and cardiometabolic risk factors in obese children and adolescents. J. Paediatr. Child Health. 2014;50:707–712. doi: 10.1111/jpc.12610. [DOI] [PubMed] [Google Scholar]
- 210.Cuevas A., Miquel J.F., Reyes M.S., Zanlungo S., Nervi F. Diet as a risk factor for cholesterol gallstone disease. J. Am. Coll. Nutr. 2004;23:187–196. doi: 10.1080/07315724.2004.10719360. [DOI] [PubMed] [Google Scholar]
- 211.Kim J.M., Lee H.L., Moon W., Koh D.H., Lee O.Y., Yoon B.C., Choi H.S., Hahm J.S., Lee M.H., Lee D.H., et al. Association between insulin, insulin resistance, and gallstone disease in Korean general population. Korean J. Gastroenterol. 2007;50:183–187. [PubMed] [Google Scholar]
- 212.Lee S., Kweon O.K., Kim W.H. Associations between serum leptin levels, hyperlipidemia, and cholelithiasis in dogs. PLoS ONE. 2017;12:e0187315. doi: 10.1371/journal.pone.0187315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213.Hardie L., Trayhurn P., Abramovich D., Fowler P. Circulating leptin in women: A longitudinal study in the menstrual cycle and during pregnancy. Clin. Endocrinol. 1997;47:101–106. doi: 10.1046/j.1365-2265.1997.2441017.x. [DOI] [PubMed] [Google Scholar]
- 214.Amico J.A., Thomas A., Crowley R.S., Burmeister L.A. Concentrations of leptin in the serum of pregnant, lactating, and cycling rats and of leptin messenger ribonucleic acid in rat placental tissue. Life Sci. 1998;63:1387–1395. doi: 10.1016/S0024-3205(98)00405-6. [DOI] [PubMed] [Google Scholar]
- 215.Balogh O., Staub L.P., Gram A., Boos A., Kowalewski M.P., Reichler I.M. Leptin in the canine uterus and placenta: Possible implications in pregnancy. Reprod. Biol. Endocrinol. 2015;13:13. doi: 10.1186/s12958-015-0003-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216.Cojocaru M., Cojocaru I.M., Silosi I., Rogoz S. Role of Leptin in Autoimmune Diseases. Maedica J. Clin. Med. 2013;8:75–79. [PMC free article] [PubMed] [Google Scholar]