Abstract
Ethanol is one of the most commonly abused drugs. Although environmental and genetic factors contribute to the etiology of alcohol use disorders, it is ethanol’s actions in the brain that explain (1) acute ethanol-related behavioral changes, such as stimulant followed by depressant effects, and (2) chronic changes in behavior, including escalated use, tolerance, compulsive seeking, and dependence. Our knowledge of ethanol use and abuse thus relies on understanding its effects on the brain. Scientists have employed both bottom-up and top-down approaches, building from molecular targets to behavioral analyses and vice versa, respectively. This review highlights current progress in the field, focusing on recent and emerging molecular, cellular, and circuit effects of the drug that impact ethanol-related behaviors. The focus of the field is now on pinpointing which molecular effects in specific neurons within a brain region contribute to behavioral changes across the course of acute and chronic ethanol exposure.
Humans consume and abuse ethanol, and thus understanding ethanol’s effects on the nervous system necessarily involves knowing the pharmacology of the drug. This two-carbon molecule is only able to interact with other biomolecules via hydrogen bonding and weak hydrophobic interactions, limiting its potency. Thus, it is no surprise that ethanol has a reputation as a nonspecific drug. Indeed, ethanol’s effects on brain function mainly occur across a range from the low millimolar range to 100 mM in naive and occasional users. Ethanol’s effects at doses that produce blood ethanol concentrations (BECs) of ~28 mg/dL (~6 mM) can be reliably distinguished in humans and animals (Ando, 1975; Schechter, 1980). Acute intoxication grows progressively stronger as BECs rise to higher levels associated with anxiolytic and euphoric effects (~12 mM) and legal intoxication (~18 mM), where slowed reaction times, motor incoordination, and cognitive impairment occur. At concentrations up to 50 mM, locomotor disruption, cognitive impairment, and sedation escalate. Above this level, strong sedation and respiratory depression can lead to coma or death (Alifimoff et al., 1989). According to the 2015 National Survey on Drug Use and Health (NSDUH), injuries and fatalities due to acute intoxication (including toxicity due to respiratory depression), accidents, violence, and traffic fatalities affect tens of thousands of people (Bose et al., 2016; Mokdad et al., 2004).
Chronic ethanol exposure and alcohol use disorder (AUD) have an even greater negative impact on society, including failed relationships, loss of employment, psychiatric symptoms, overt neurotoxicity, liver failure, and severe cognitive disruption (Bose et al., 2016). These chronic problems consume considerable resources for psychiatric care, organ transplants, and long-term medical treatment. As tolerance to the acute effects of ethanol develops, humans can survive with BECs up to 8 times those that would kill an ethanol-naive person. Indeed, awake individuals with blood concentrations near 300 mM have been reported (Johnson et al., 1982). Overall, the global consequences of AUD include 3.3 million annual deaths (5.9% of all deaths) and 5.1% of the burden of disease and injury, with an economic burden of ~$250 billion annually in the United States (WHO, 2014; Sacks et al., 2015). Given this huge societal impact, the US Surgeon General recently issued a first of its kind report, “Facing Addiction in America: The Surgeon General’s Report on Alcohol, Drugs, and Health,” highlighting alcoholism and addiction (US DHHS, 2016). Thus, a review of the current state of knowledge about ethanol effects on the brain is warranted.
In light of this large societal impact, the field seeks to understand how ethanol alters brain function across a range of concentrations and time frames/phases of drinking. Indeed, several phenotypic phases of ethanol consumption and AUD that occur over weeks to years have been proposed (Koob and Volkow, 2016). We will focus on the latest findings from neurobiological studies examining acute and chronic ethanol effects on the brain, with emphasis on neuronal molecules, synapses, and brain circuits with important roles in behavioral effects of the drug. The entire scope of the neural actions of ethanol cannot be covered in this limited format (unfortunately including topics such as fetal alcohol effects, ethanol effects on glia, neuroinflammatory mechanisms, and extracellular matrix), but references for some topics are provided to allow the reader to gain a deeper understanding of the field.
A Multi-level, Integrative Analysis of Ethanol’s Effects on the Nervous System: Bottom-Up and Top-Down Approaches to Finding Ethanol Targets
Ethanol distribution in the body and brain is similar to water, with equilibration throughout organs and cells within a few minutes of drinking. This property contributed to the idea that many of ethanol’s effects involve its occupation of water-filled cavities in proteins and subsequent alteration of function. Considering the ubiquity of distribution and low drug potency, ethanol acts on numerous molecular targets in neurons and synapses throughout the brain. This lack of specificity can be daunting to those who study potent and specific drugs, including drugs of abuse with circumscribed primary molecular targets (e.g., opiates). However, even these target-specific drugs produce complex secondary neuroadaptations that contribute to drug use disorders. It is worth noting that the function of many molecules in mammalian neurons appears to be remarkably insensitive to ethanol (Yamakura et al., 2001). Thus, earlier ideas about ubiquitous molecular effects due to changes in membrane fluidity are not helpful in understanding how ethanol alters neuronal function (Peoples et al., 1996). Even if fluidity changes occur, these changes lead to altered neuronal function, and thus, we must examine the proteins that dictate neuronal function. Thankfully, the tools available to modern neuroscientists have enabled examination of ethanol effects at multiple levels. We can now determine how a given molecular effect on a specific neuronal or synaptic subtype contributes to ethanol-induced behavioral changes. Both bottom-up and top-down approaches are being used in such studies.
The bottom-up approach builds from the identification of an ethanol-sensitive molecule followed by determination of its role in acute and chronic ethanol changes in physiology and behavior. On the other hand, top-down approaches begin with ethanol-related physiological or behavioral changes leading to the study of specific molecular mechanisms and brain circuits contributing to these effects.
Molecular Targets
Recent theories have posited specific ethanol-binding sites on several proteins that may act directly or indirectly to produce a biological effect (Figure 1). To understand how ethanol affects the brain and behavior using a bottom-up approach, it is important to first distinguish between the direct and indirect effects of ethanol. To that end, the following criteria have been proposed to classify direct ethanol targets (Harris et al., 2008; Trudell et al., 2014):
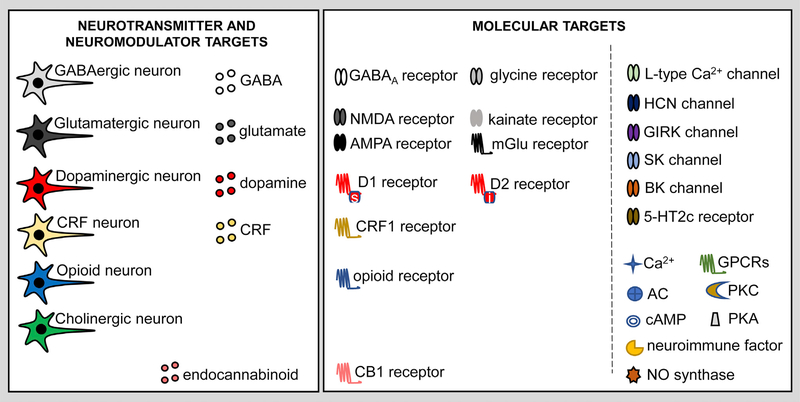
Figure 1. Neurotransmitter/Modulator Systems and Molecular Targets of Ethanol.
The symbols and definitions shown here are used in Figures 2 and 3.
The putative target protein should be affected by ethanol at both low and high concentrations.
The molecular binding site and ethanol interaction should be characterized biochemically or modeled. Manipulation of the amino acids making up the putative binding site should alter the ethanol interaction and, consequently, the biological effect of ethanol.
Structural biological evidence should indicate that ethanol inhabits the putative binding site.
Genetic alteration of the target protein (e.g., knockout) should result in a readily discernable ethanol-related phenotype.
These criteria allow for the clear identification of direct ethanol targets. However, the low-affinity and transient molecular interactions of ethanol make fulfillment of all four criteria challenging. Thus, some of the molecular targets we discuss will be referred to as “putative” direct targets to indicate only partial fulfillment of the preceding criteria. Targets that do not meet any of the criteria above or that do not have any molecular structures indicative of an ethanol-binding site are referred to as indirect targets.
Direct Molecular Targets
Low concentrations of ethanol can directly interact with several molecules (Cui and Koob, 2017). The best example of a direct ethanol target (though not brain exclusive) is alcohol dehydrogenase (ADH). Ethanol has been shown to interact with ADH at low millimolar concentrations, the binding site is well characterized, and manipulation of ADH results in biological effects (Goto et al., 2015).
Ethanol has rapid acute effects on the function of proteins involved in excitatory and inhibitory synaptic transmission (Figures 1 and 2). Ethanol generally potentiates cys-loop ligand-gated ion channels (LGICs) (e.g., GABAA and glycine receptors [GlyRs]) but inhibits ionotropic glutamate receptors (reviewed in Lovinger and Roberto, 2013; Söderpalm et al., 2017). The different ligand-binding and transmembrane domains of these proteins likely underlie this difference. The current thinking is that ethanol interacts with membrane-spanning domains within these proteins and the subsequent allosteric changes in conformation produced differ for the different LGIC subtypes (Möykkynen and Korpi, 2012; Olsen et al., 2014). However, more work is needed to understand the structural basis of these differences. Ethanol also modulates nicotinic acetylcholine receptor (nAChR) function in a subunit-specific manner (Davis and de Fiebre, 2006; Hendrickson et al., 2013; Rahman et al., 2016) and potentiates 5HT3Rs (McBride et al., 2004).
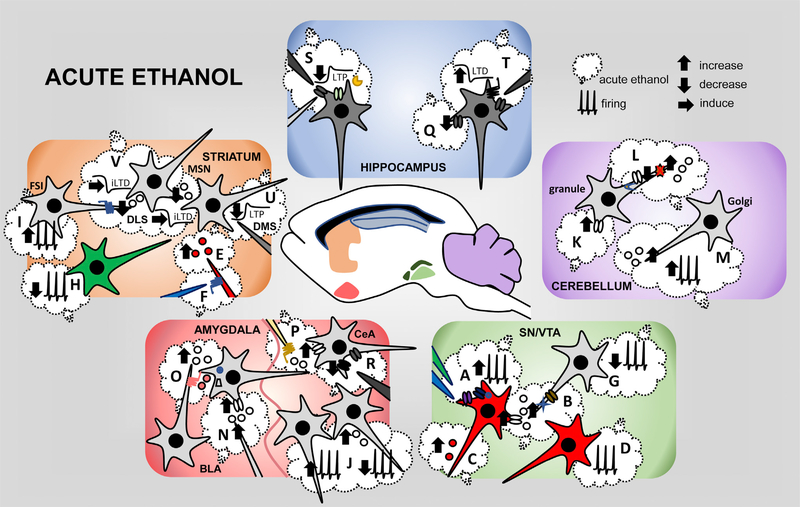
Figure 2. Acute Effects of Ethanol on the Hippocampus, Striatum, Cerebellum, Amygdala, and Midbrain.
BLA, basolateral amygdala; CeA, central amygdala; DLS, dorsolateral striatum; DMS, dorsomedial striatum; FSI, fast-spiking interneuron; iLTD, Inhibitory long-term depression; LTP, long-term potentiation; LTD, long-term depression; MSN, medium spiny neuron; SN/VTA, substantia nigra/ventral tegmental area. See text and Figure S1 for references related to each letter and highlighted effect.
Primary ethanol-binding sites that fulfill the four criteria have yet to be identified for all of these LGICs, but there is evidence of direct interactions with several of the cys-loop LGICs (Howard et al., 2014). For example, the structural basis for a direct interaction of ethanol with the prototypic G. violaceus LGIC has been determined and is thought to be a transmembrane cavity between two membrane-spanning domains (Sauguet et al., 2013). Identifying the expression sites and cellular actions of the subunits of these ethanol-sensitive channels is an important next step in understanding how the molecular effect of ethanol translates into altered neuronal and circuit function.
Studies of ethanol interactions with GlyRs are a good example of the bottom-up approach. These studies initially focused on the molecular mechanisms of ethanol’s potentiation of GlyRs (Burgos et al., 2015; Mascia et al., 1996; Mihic, 1999; Perkins et al., 2010) and moved to studies of how ethanol’s effects on GlyRs contribute to changes in circuit function and behavior (Aguayo et al., 2014; Blednov et al., 2012, 2015). Ethanol’s effects on GlyR function have been identified in several brain regions (Badanich et al., 2013; Förstera et al., 2017; McCracken et al., 2017). There is also evidence for a glycinergic “tone” or steady-state receptor activation that can be potentiated by ethanol (Salling and Harrison, 2014; Zhang et al., 2008), but the site and basic mechanisms of glycine release remain unclear. The use of genetically engineered mice with alterations in receptor subunit expression or structure (knockouts and knockins) allow investigators to exploit the bottom-up approach and analyze the behavioral consequences of ethanol’s effects on specific targets. Mice lacking the GlyR alpha 2 subunit show reduced ethanol intake, but GlyR alpha 3 knockout mice show increased intake (Mayfield et al., 2016). More evidence of the cellular and brain region location of the GlyRs involved in these behaviors is needed. For example, glycine transporter blockade in the ventral medial prefrontal cortex (PFC) contributes to increased motor impulsivity during protracted abstinence from long-term ethanol exposure (Irimia et al., 2017). Targeted conditional knockout mice may help us to better understand the contribution of GlyRs to ethanol intoxication, consumption, and AUD.
Ethanol inhibition of NMDA receptor (NMDAR) function has been studied in depth, but the details of the ethanol-receptor interaction are poorly understood (Bell et al., 2016). Interactions appear to involve the N-terminal and transmembrane 3 (TM3) domains of receptor subunits, as mutation of these sites alters ethanol inhibition of NMDARs (Smothers et al., 2013). Based on this work, a bottom-up approach using an ethanol-resistant TM3 domain mutation (Ronald et al., 2001; Smothers and Woodward, 2006, 2016) found altered ethanol-associated behaviors (den Hartog et al., 2013). Further investigation is needed to fully understand how this mutation and other alterations in NMDAR function can affect pharmacological and behavioral effects of ethanol.
The putative direct interaction of ethanol with the large-conductance Ca2+-activated K+ channel (BK channel) has spurred research on a molecular target that affects neurons and circuit function using both bottom-up and top-down approaches. Early studies showed that acute ethanol enhances BK channel function (Dopico et al., 2014). More recently, Bukiya et al. (2014) characterized an ethanol-sensing site in the channel-forming α subunit. Bottom-up studies have examined how changes in ethanol’s effects on BK channels alter behavior. For example, ethanol potentiates α and αβ4 BK channel open probability, but the potentiation of an α-only-containing BK channel shows rapid tolerance (Martin et al., 2008; Velázquez-Marrero et al., 2014), which could be related to behavioral tolerance (Treistman and Martin, 2009). Studies using genetic manipulation of BK channels have identified a role for these channels in ethanol-induced depressive behavior in C. elegans, tolerance in Drosophila, and several behavioral responses in rodents (reviewed in Bettinger and Davies, 2014). A top-down approach revealed molecular mechanisms responsible for these behavioral effects. Blocking BK channel transport to the presynaptic plasma membrane alters ethanol-induced locomotor depression in C. elegans (Oh et al., 2017), while Wnt/β-catenin-signaling-dependent trafficking of BK channels out of the membrane contributes to ethanol tolerance at the cellular level (Palacio et al., 2015; Pietrzykowski et al., 2004; Velázquez-Marrero et al., 2016). However, no data have associated these molecular events with ethanol-induced behaviors, including tolerance.
Another ion channel with notable ethanol sensitivity is the G-protein-coupled inwardly rectifying K+ channel (GIRK). Ethanol enhances GIRK channel function (Bodhinathan and Slesinger, 2013; Glaaser and Slesinger, 2017), and genetic studies have identified a 43-amino-acid C-terminal region that is crucial for this action of ethanol (Lewohl et al., 1999). Mice carrying a missense mutation in the GIRK channel showed a loss of ethanol-induced analgesia (Kobayashi et al., 1999), and GIRK3 subunit knockout mice showed ethanol conditioned place preference, which was absent in controls (Tipps et al., 2016). Using a crystal structure of a mouse inward rectifier containing a bound ethanol molecule and structure-based mutagenesis, investigators probed a putative hydrophobic ethanol-binding pocket in the cytoplasmic domains of GIRK channels (Aryal et al., 2009).
Ethanol can also interact directly with non-ion-channel targets, including intracellular signaling molecules such as protein kinase C (PKC) (Pany and Das, 2015; Ron and Barak, 2016) and adenylate cyclase (AC) (Yoshimura et al., 2006). The physiological consequences of these effects of ethanol are not fully clear, but roles in the effects of drugs on synaptic transmission are emerging, as discussed later in this review.
Indirect Molecular Targets
Indirect ethanol targets include ion channel subunits, intracellular signaling proteins, growth factors, transcription factors, proteins involved in epigenetic regulation of gene expression, and even membrane lipids. In most cases, there is no clear evidence of an ethanol-binding site or that acute ethanol alters the expression or function of these molecules, but they show prominent alterations following chronic ethanol exposure and intake. Examples of indirect targets are highlighted in this and later sections of the review.
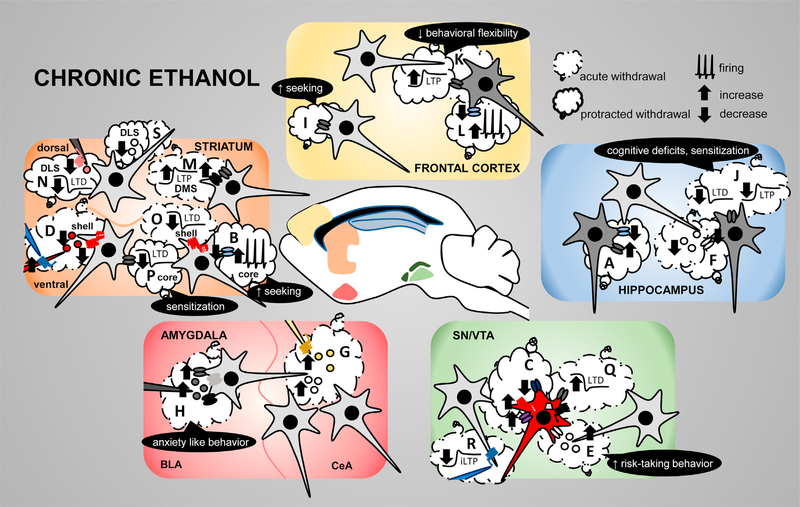
An intriguing example that has been the subject of recent study is the small-conductance Ca2+-dependent K+ (SK) channel. Ethanol inhibits SK2 channel currents in a heterologous expression system (Dreixler et al., 2000), but there is no evidence of direct ethanol interactions with this channel. However, a number of studies indicate that chronic ethanol exposure and withdrawal reduce SK channel function in the ventral tegmental area (VTA) dopamine, hippocampal CA1 (Figure 3A), and cortical neurons (reviewed in Mulholland et al., 2009, 2011; Nimitvilai et al., 2016a; Korkotian et al., 2013). Furthermore, decreased SK channel expression and function were observed in the nucleus accumbens (NAc) core after ethanol self-administration. This effect was associated with greater ethanol seeking and was blocked by administration of an SK channel activator into the NAc after abstinence (Hopf et al., 2010). Similarly, NAc SK channel inhibition increases ethanol intake in mice (Padula et al., 2015), supporting the association between SK channels and ethanol intake (Figure 3B). Clearly, the SK channel has important roles in neuroadaptations that alter ethanol-related behaviors.
Figure 3. Chronic Effects of Ethanol on the Frontal Cortex, Striatum, Hippocampus, Amygdala, and Midbrain.
BLA, basolateral amygdala; CeA, central amygdala; core, nucleus accumbens core; DLS, dorsolateral striatum; DMS, dorsomedial striatum; iLTP, inhibitory long-term potentiation; LTP, long-term potentiation; LTD, long-term depression; shell, nucleus accumbens shell; SN/VTA, substantia nigra/ventral tegmental area. See text and Figure S2 for explanation and references related to each letter and highlighted effect.
In the following sections, we will consider the neurophysiological and behavioral effects of ethanol. The emphasis will be on the effects of ethanol in particular brain circuits and their ramifications for ethanol-related behaviors.
Ethanol Effects on Intrinsic Excitability, Synaptic Transmission, and Plasticity
Effects on Neuronal Firing
Ethanol has well-known locomotor and reinforcing effects, and certainly the latter contribute to drinking in some capacity. Thus, top-down approaches based on these behavioral outcomes led scientists to study ethanol’s effects on midbrain dopamine neurons that have prominent roles in locomotion and reward (Melis et al., 2007; Samson et al., 1992). Although findings suggest that lesions of the mesolimbic dopamine system do not change ethanol self-administration (Rassnick et al., 1993), rodents do self-administer ethanol into the VTA (Gatto et al., 1994; Rodd et al., 2004), and dopamine is clearly implicated in ethanol-induced increases in locomotion and sensitization (Phillips and Shen, 1996). Ethanol facilitates action potential firing of midbrain dopamine neurons (Figure 2A) and increases extracellular dopamine levels in the VTA (Deehan et al., 2016) (Figure 2C). The physiological mechanisms thought to underlie this ethanol potentiation were reviewed by Morikawa and Mornsett (2010) and include reductions of a barium-sensitive potassium and M-type currents. Furthermore, GIRK channels (Herman et al., 2015) and the hyperpolarization-activated and cyclic nucleotide-gated (HCN) channel current (Ih) (Appel et al., 2003; McDaid et al., 2008; Nimitvilai et al., 2016b) may also be involved in ethanol stimulation of dopamine neuron firing. Synaptic mechanisms also contribute to this stimulatory ethanol effect. Opioid (Xiao and Ye, 2008; Xiao et al., 2007), GABA, cholinergic, and serotoninergic transmission modulate ethanol excitation of VTA dopamine neurons (Adermark et al., 2014; Theile et al., 2009, 2011; Xiao and Ye, 2008; Xiao et al., 2007; but see Nimitvilai et al., 2016b) (Figures 2A and 2B). It is now clear that dopamine neurons are heterogeneous, and recent reports have identified a subset of VTA dopamine neurons with greater sensitivity to ethanol’s effects (Avegno et al., 2016; Mrejeru et al., 2015; Tateno and Robinson, 2011) (Figures 2A and 2D). The chronic and withdrawal effects of ethanol on dopamine neuron firing are mixed, with decreases observed in anesthetized rats (Diana et al., 1996) but no change (Okamoto et al., 2006; Perra et al., 2011) or increases (Didone et al., 2016) detected in slices. Repeated in vivo ethanol downregulates Ih density in dopamine neurons (Okamoto et al., 2006) and induces adaptations in the dopamine D2 receptor and GIRK channels (Perra et al., 2011) (Figure 3C). Thus, while changes in dopamine neuron firing are among the most consistent effects of ethanol, more work is needed to pin down the mechanisms underlying this effect.
The acute ethanol-induced increase in dopamine neuron firing is associated with increased NAc dopamine levels in rodents (Ericson et al., 1998; Yoshimoto et al., 1992) and humans (Aalto et al., 2015; Boileau et al., 2003) (Figure 2E). Interestingly, active and passive ethanol administration produces similar increases in NAc dopamine levels (Bassareo et al., 2017) that may be dependent on taurine (Ericson et al., 2011), GlyRs (Adermark et al., 2011a), and opiate receptors (Benjamin et al., 1993; Zapata and Shippenberg, 2006) (Figure 2F). In contrast, high concentrations of ethanol dampen dopamine release from terminals measured with fast-scan cyclic voltammetry in the striatum (Budygin et al., 2001; Schilaty et al., 2014). These seemingly contradictory effects of ethanol on the striatal dopamine depend on the ethanol dose, with lower doses increasing dopamine via actions in midbrain and higher doses inhibiting release. Chronic ethanol exposure produces adaptations in dopamine release, and the opioid system may play a role (reviewed in Barbaccia et al., 1980). A nonspecific opioid receptor antagonist blocks dopamine release induced by ethanol drinking in the NAc (Gonzales and Weiss, 1998). Recent work has also shown that the ethanol-induced dopamine increase switches to a decrease after short-term withdrawal, which could be associated with a supersensitivity of kappa opiate receptors (Karkhanis et al., 2016; Rose et al., 2016; Siciliano et al., 2015) (Figure 3D). Interestingly, decreased availability of striatal D2 dopamine receptors is associated with AUD (Volkow et al., 2002; Volkow et al., 2017) (Figure 3D), indicating less dopamine responsiveness after short-term withdrawal from chronic ethanol exposure. Hirth et al. (2016), however, found that while dopamine levels were decreased during acute ethanol withdrawal, protracted withdrawal was accompanied by increased dopamine in rodents. Thus, while the overall trend is a decrease in dopaminergic transmission after chronic ethanol and withdrawal, this may depend on the withdrawal duration.
Neurons that fire spontaneously set a rhythm of tonic activity in many brain areas. Ethanol alters activity of distinct types of these “tonically active” neurons. Although ethanol potentiates the firing of dopamine neurons, it inhibits the firing of midbrain GABAergic neurons (Adermark et al., 2014; Burkhardt and Adermark, 2014; Stobbs et al., 2004) (Figure 2G). Interneurons of the striatum are also differentially affected by acute ethanol (Blomeley et al., 2011; Clarke and Adermark, 2015). Ethanol decreases the tonic firing frequency of cholinergic interneurons in the striatum, which then affects the activity of medium spiny neurons (MSNs) (Adermark et al., 2011b; Blomeley et al., 2011) (Figure 2H). These findings indicate that ethanol’s effects on intrinsic excitability are region and cell-type specific. Indeed, in the globus pallidus external segment, acute ethanol decreases the firing of low-frequency, but not high-frequency, firing neurons. The ethanol-induced inhibition of low-frequency firing neurons is attributable to ethanol activation of the BK channel (Abrahao et al., 2017). Thus, this is one neuronal subtype in which the bottom-up approach can be used to assess the circuit and behavioral effects of BK activation by ethanol.
Ethanol also differentially affects the excitability of neurons that are not tonically active. For example, low-threshold spiking striatal interneurons show acute ethanol-induced hyperpolarization, but fast-spiking interneurons (FSIs) show a significant ethanol-induced membrane depolarization (Blomeley et al., 2011). Indeed, in vivo electrophysiological recordings show that acute ethanol increases the firing rate of FSIs in the NAc that may be related to the depolarization observed in vitro (Burkhardt and Adermark, 2014) (Figure 2I). In the central amygdala (CeA), acute ethanol can increase or decrease the firing of different neurons (Herman and Roberto, 2016) (Figure 2J).
Specific groups of neurons express one or more channels that are direct or indirect ethanol targets, allowing for neuron-specific ethanol modulation of activity. In the case of neurons whose intrinsic activity is ethanol insensitive, it remains to be determined whether they lack ethanol target channels or whether the factors that control sensitivity to ethanol (e.g., post-translational modifications) differ between ethanol-sensitive and insensitive neurons. Future studies should use both top-down and bottom-up approaches to examine how acute and chronic ethanol exposure affects excitability and firing in different neuronal populations in brain regions with key roles in the behavioral actions of ethanol and in which ethanol-sensitive molecules contribute to these changes.
Fast Inhibitory Synaptic Transmission
Ethanol’s interactions with GABA-mimetic drugs have long been known, and the synergism of ethanol and barbiturates was studied extensively before it was clear that both of these drugs act on GABAA receptors (Mihic and Harris, 2011). Thus, a top-down analysis indicated that ethanol’s effect on GABAA-mediated fast synaptic transmission was likely to be a fruitful area of study to better understand intoxication and high-dose ethanol actions. Accordingly, it was natural to assume that ethanol would act on GABAA receptors in a manner similar to other sedative drugs. Indeed, ethanol potentiates GABAA receptors in some neurons and heterologous expression systems (Harris et al., 1997; Mihic, 1999). Examination of “tonic” GABAA currents consistently revealed increases in postsynaptic GABA responses in the cerebellum (Diaz and Valenzuela, 2016) (Figure 2K), hippocampus (Liang et al., 2006), and thalamus (Jia et al., 2008). These actions of ethanol often involve the GABAA δ subunit (Choi et al., 2008). However, there has been debate about the mechanisms involved in this tonic current effect. In the cerebellum, there is evidence that ethanol’s enhancement of interneuron firing is a key factor underlying increased tonic current (Valenzuela and Jotty, 2015), but this may not be the case in other brain regions.
Analysis of intact synapses indicated that while acute ethanol enhanced GABAergic transmission at synapses in several brain regions (Siggins et al., 2005; Weiner et al., 1997; Zhu and Lovinger, 2006), these effects often involved unexpected presynaptic potentiation (Ariwodola and Weiner, 2004; Carta et al., 2004; Nie et al., 2004; Roberto et al., 2003). The clearest evidence for enhanced GABA release at individual synapses comes from studies of isolated neurons from the cerebellum (Figures 2L and 2M) and basolateral amygdala (BLA) (Figures 2N and 2O) that include pinched-off, functional synaptic boutons that spontaneously release GABA. Ethanol potentiates this spontaneous release at concentrations relevant to intoxication. Indices of postsynaptic changes are not observed in the presence of ethanol (Kelm et al., 2007; Zhu and Lovinger, 2006), and this potentiation cannot result from activity of interneurons, as the boutons are no longer connected to somata. This type of experiment provides clear evidence of an increase in GABA release at central synapses.
The mechanisms underlying ethanol potentiation of GABA release are not well-understood. Examination of mice lacking protein kinase A (PKA) or PKC epsilon indicate loss of the presynaptic actions of ethanol (Bajo et al., 2008; Proctor et al., 2003) and inhibition of AC has been shown to prevent this ethanol effect at some synapses (Talani and Lovinger, 2015) (Figure 2O). Activation of a variety of Gi/o-coupled G-protein coupled receptors (GPCRs) counteracts ethanol’s potentiation of GABA release at synapses in several brain regions (Ariwodola and Weiner, 2004; Kelm et al., 2011; Roberto et al., 2010; Talani and Lovinger, 2015). These findings reinforce the idea that signaling through AC and PKA is involved in ethanol’s actions and are in accord with findings from invertebrate models (Moore et al., 1998). In cerebellar granule neurons, although ethanol inhibits the function of GABAA receptors through a mechanism involving postsynaptic PKC, ethanol also enhances GABA release via inhibition of nitric oxide synthase (Kaplan et al., 2013) (Figure 2L).
Presynaptic ethanol effects at some synapses are secondary to release of neuromodulators that are themselves the direct mediators of increased vesicle fusion. The CeA, for example, expresses a number of neuropeptides (including corticotropin-releasing factor [CRF]) affected by ethanol, and peptides in this region are implicated in the processing of aversive stimuli and emotional salience. As such, CeA is critically involved in the negative affective states accompanying drug and alcohol abuse and addiction (Koob, 2015). CRF enhances GABAergic transmission in the CeA via presynaptic CRF1 receptors (Bajo et al., 2008; Cruz et al., 2012; Roberto et al., 2010). Acute ethanol also enhances this transmission (Kang-Park et al., 2013; Nie et al., 2004; Roberto et al., 2003; Roberto et al., 2004a), and this effect is CRF1 dependent, suggesting that ethanol acts indirectly to increase GABA release by facilitating local CRF release (Bajo et al., 2008; Nie et al., 2004) (Figure 2P). However, in some CeA neurons, the ethanol and CRF effects on GABA transmission are additive, suggesting distinct mechanisms of action. In the dorsolateral striatum, however, ethanol inhibits GABA release by enhancing enkephalin release and presynaptic delta opiate receptor activation (Patton et al., 2016). Thus, ethanol-induced neuropeptide release modulates GABA release in a synapse-specific manner. Neuropeptide release is certainly not involved in ethanol’s actions on GABA release at all synapses, as evidenced by potentiation in isolated neuron preparations (Criswell et al., 2008; Zhu and Lovinger, 2006).
Chronic ethanol exposure and intake also alter GABAergic transmission via pre- and postsynaptic mechanisms. These effects were covered in a recent review (Roberto and Varodayan, 2017) and will not be discussed in detail here. Both increases and decreases in GABA release are observed in several brain regions and they appear to be synapse specific (Cuzon Carlson et al., 2011; Herman et al., 2016a; Schindler et al., 2016; Tremwel et al., 1994; Wanat et al., 2009; Wilcox et al., 2014) (Figures 3E–3G). In the CeA, for example, CRF levels and GABA transmission are increased and remain so during acute withdrawal. Interestingly, acute ethanol exposure following chronic ethanol treatment has the same effect as acute ethanol in naive animals, suggesting that acute ethanol-induced facilitation of GABA transmission does not undergo tolerance (Roberto et al., 2004a) (Figure 3G).
Fast Excitatory Synaptic Transmission
Ethanol has several effects on glutamatergic transmission (Bell et al., 2016; Hwa et al., 2017; Roberto and Varodayan, 2017). Acute ethanol inhibits all glutamate receptors. These effects occur in the hippocampus (Lovinger et al., 1990) (Figure 2Q), frontal cortex (Weitlauf and Woodward, 2008), and CeA (Kirson et al., 2017; Roberto et al., 2004b, 2006; Zhu et al., 2007) (Figure 2R), among other brain regions. The acute effects of ethanol on glutamate release vary, with some reports showing presynaptic potentiation (Herman et al., 2016b; Silberman et al., 2015; Xiao et al., 2009) and others showing inhibitory effects (Basavarajappa et al., 2008; Hendricson et al., 2004; Herman et al., 2016b; Maldve et al., 2004; Zhu et al., 2007).
Chronic ethanol exposure can affect NMDARs (Abrahao et al., 2013; den Hartog et al., 2017; Hendricson et al., 2007), kainate receptors (Carta et al., 2003; Läck et al., 2009), AMPA receptors (AMPARs) (Läck et al., 2007), and metabotropic glutamate receptors (mGluRs) (Ding et al., 2016; Mihov and Hasler, 2016). These ethanol effects in specific brain regions have been linked to different ethanol-related phenotypes. For example, increased glutamatergic transmission in the BLA induced by chronic ethanol is associated with withdrawal anxiety-like behavior (Christian et al., 2013; Läck et al., 2007) (Figure 3H). In addition, selective deletion of the GluN2B NMDAR subunit in cortical interneurons reduces ethanol seeking (Radke et al., 2017a, 2017b) (Figure 3I). Analysis of the role of glutamate and glutamate receptors in ethanol-related behaviors should be extended to additional synapses and brain regions. Chronic ethanol exposure elevates extracellular glutamate levels in several brain regions, inducing a “hyperglutamatergic” state thought to contribute to AUDs (Gass and Olive, 2008; Spanagel, 2009). For example, this increased glutamatergic drive may lead to excessive activation at key synapses in circuits involved in ethanol seeking, including the corticostriatal synapses examined by Meinhardt et al. (2013). Indeed, increased extracellular NAc glutamate, induced by chronic ethanol or glutamate reuptake inhibition, promoted ethanol consumption in mice (Griffin et al., 2014). Based on this line of work, glutamate uptake has been targeted to treat AUD (Rao et al., 2015).
Synaptic Plasticity
Ethanol alters learning and memory (Oslin and Cary, 2003; White, 2003), and this may involve effects on synaptic plasticity, including long-term depression (LTD) and long-term potentiation (LTP) (reviewed in Zorumski et al., 2014). Most of the data on ethanol effects on synaptic plasticity come from studies in the hippocampus. Acute ethanol inhibits LTP in hippocampal slices (Blitzer et al., 1990; Morrisett and Swartzwelder, 1993), but these results are not consistent (Fujii et al., 2008; Swartzwelder et al., 1995). This variability may be due to many factors, including age, subregion, and stimulus strength. Acute ethanol blocks LTP in apical dendrites but only reduces LTP in basal dendrites (Ramachandran et al., 2015). These effects may be due to NMDAR inhibition (Chandler et al., 1998; Izumi et al., 2005), but recent work posits a role for neurosteroids (Izumi et al., 2015; Tokuda et al., 2013). In contrast to LTP, hippocampal LTD is enhanced by acute ethanol in the CA1 region (Hendricson et al., 2002), and this effect involves NMDARs and mGluR type 5 (mGluR5) (Izumi and Zorumski, 2012; Overstreet et al., 1997) (Figure 2T).
Chronic ethanol exposure reversibly inhibits LTP (Durand and Carlen, 1984; Roberto et al., 2002) and dampens LTD in hippocampal neurons (Thinschmidt et al., 2003) (Figure 3J). Indeed, high-dose ethanol treatment can transiently abolish NMDA-dependent LTD in hippocampal neurons and elicit cognitive deficits in rats (Silvestre de Ferron et al., 2015). Impairment of mGluR5-LTD in hippocampal slices following ethanol vapor exposure (Wills et al., 2017) indicates that other types of plasticity may be affected by chronic ethanol. Relevant to the role of plasticity in ethanol-related behaviors, mice susceptible to the development of locomotor sensitization to ethanol show normal hippocampal LTD, whereas mice resistant to ethanol sensitization lack LTD (Coune et al., 2017). We still have an incomplete understanding of how changes in synaptic plasticity are associated with behavioral adaptations produced by chronic ethanol treatment.
The PFC is involved in the cognitive symptoms of AUD. Although studies have investigated the acute effects of ethanol on PFC NMDARs (Weitlauf and Woodward, 2008), few have investigated the effect on synaptic plasticity in this area. Chronic ethanol exposure induces an increase in the NMDA/AMPA current ratio in the PFC and enhances expression of NMDAR-mediated spike-timing-dependent LTP, a neuroadaptation likely associated with reduced behavioral flexibility (Kroener et al., 2012; Nimitvilai et al., 2016a) Figures 3K–3L). It will be interesting to determine how these plasticity changes contribute to ethanol-induced cognitive impairment.
Ethanol can also affect striatal plasticity (Lovinger and Kash, 2015). For example, acute ethanol application blocks LTP (Figure 2U) and has diverse effects on LTD (Clarke and Adermark, 2010; McCool, 2011; Yin et al., 2007). In contrast, chronic ethanol facilitates corticostriatal LTP (Wang et al., 2012; Xia et al., 2006) (Figure 3M) and impairs endocannabinoid-mediated disinhibition in the dorsolateral striatum (Adermark et al., 2011c). Furthermore, chronic ethanol dampens striatal LTD at excitatory synapses (Adermark et al., 2011c; Cui et al., 2011; DePoy et al., 2013) (Figure 3N). With novel optogenetic and transgenic tools, scientists can now study pathway-specific ethanol effects. For example, excessive ethanol intake potentiates AMPA- and NMDA-mediated transmission at the medial prefrontal cortex (mPFC) input and increases glutamate release from BLA afferents to the dorsomedial striatum (DMS). These changes could explain the effect of chronic ethanol exposure on striatal LTP, as paired activation of the mPFC and BLA inputs induces robust LTP of the corticostriatal input to the DMS (Ma et al., 2017).
Acute and chronic ethanol-induced changes in plasticity have also been extensively studied in the NAc, a region implicated in the rewarding effects of ethanol (reviewed in Renteria et al., 2016), and will only be briefly summarized here. Acute ethanol inhibits NMDAR-dependent LTD in the NAc shell in an MSN-sub-type-specific manner (Jeanes et al., 2014). In the NAc core, acute ethanol impairs LTP via effects on mGluRs (Mishra et al., 2012). Following chronic ethanol exposure, LTD is altered such that D1-negative MSNs show LTD while D1-positive MSNs lose LTD, and sometimes show LTP (Jeanes et al., 2014; Renteria et al., 2017) (Figure 3O). These effects were lost after 2 weeks of withdrawal. Another study found impaired expression of NMDAR-LTD in the NAc core, but not shell, of mice that showed robust locomotor sensitization to ethanol after 2 weeks of withdrawal from chronic ethanol treatment (Abrahao et al., 2013) (Figure 3P). Thus, plasticity deficits in the NAc and hippocampus may contribute to behavioral adaptations to chronic ethanol (Coune et al., 2017).
Much less is known about ethanol’s effects on plasticity in other areas. A single in vivo ethanol administration impairs LTP in VTA dopamine neurons in DBA mice, with no effect in C57 mice (Wanat et al., 2009), but unlike other regions, chronic ethanol treatment enhances NMDA-dependent LTD in VTA dopamine neurons (Bernier et al., 2011) (Figure 3Q). Ethanol exposure also inhibits LTP in VTA neuron GABAergic synapses (Guan and Ye, 2010) (Figure 3R). Further study is required to understand the effect of ethanol on midbrain dopamine neurons, especially in light of recent findings on the anatomical and biochemical diversity of dopamine neurons (Lammel et al., 2008; Poulin et al., 2014).
Circuitry
While much of the past focus has been on ethanol effects on molecules and synapses, there has been increasing realization that these targets must be considered in the context of micro- and larger circuits. This concept has arisen from the findings that ethanol effects on cellular targets vary across brain regions due to differences in the molecular complement of different neurons and differences in ethanol sensitivity. For example, ethanol potentiates GIRK channel function in cerebellar granule neurons, but striatal MSNs do not express GIRK channels (Kobayashi et al., 1995), and thus, this mechanism would not be viable in these neurons. The variability in ethanol potentiation of delta-subunit-containing GABAA subunits (e.g., thalamus and hippocampus) also reinforces this point. In addition, there is increasing recognition of how different brain circuits contribute to behavior, and thus, we must understand ethanol’s effects on circuitry to fully appreciate the factors underlying the range of behavioral effects of the drug. The increasing appreciation of the larger circuitry in which individual brain regions participate has stimulated systems-level neuroscience in general and spurred increasing work at this level in the alcohol research field.
Microcircuitry
The acute and chronic effects of ethanol on microcircuits can help reveal changes in local control of synapses that alter the output of key brain regions. As the majority of synapses in microcircuits are GABAergic, this research has focused mostly on changes in the effects of GABA. Some of the ethanol-induced changes in interneuron function and synaptic transmission were mentioned earlier in this review, and we will now focus on recent data from striatum and cerebellum.
In the dorsal striatum, local GABAergic connections include synapses between FSIs and MSNs, as well as collateral MSN-MSN connections (Wilson, 2007). Effects of both acute and chronic ethanol on these GABAergic synapses have been characterized in rodents (Patton et al., 2016; Wilcox et al., 2014) (Figure 2V) and non-human primates (Cuzon Carlson et al., 2011). One theme that has emerged from these studies is that ethanol has opposing actions on GABAergic synapses in two subregions of the striatum. In the “associative” or DMS, ethanol potentiates GABAergic transmission via a presynaptic mechanism, while ethanol inhibits GABAergic transmission in the “sensorimotor” or dorsolateral striatum, with the aforementioned opiate receptor-dependent presynaptic mechanism implicated in this action (Wilcox et al., 2014). Ethanol also inhibits MSN-MSN synapses via a mechanism that is not as well characterized (Patton et al., 2016). Thus, the net effect of acute ethanol is to inhibit MSN output from associative striatum while disinhibiting output from sensorimotor striatum. These striatal subregions are part of larger circuits that control goal-directed, conscious actions (the associative circuit) and habitual, unconscious actions (the sensorimotor circuit). The combination of associative circuit inhibition and sensorimotor circuit activation could help to promote the learning and performance of habitual actions. Short- and long-term ethanol consumption reduces GABAergic synaptic responses in sensorimotor regions and exacerbates the imbalance in the output of associative and sensorimotor circuits (Cuzon Carlson et al., 2011; Wilcox et al., 2014) (Figure 3S).
Recent work has focused on how differences in genetics and intracellular signaling impact ethanol’s actions on microcircuits and the relationship between these effects and alcohol intoxication, reward, and drinking. It is well known that C57Bl6J mice differ from DBA mice in ethanol-related behaviors (Belknap et al., 1993), likely due to differences in genes governing the neural mechanisms underlying reward and aversion (Cunningham et al., 1992). A top-down examination of ethanol’s effects on GABAA-receptor-mediated transmission in cerebellar microcircuitry revealed differences between these strains that may account for the behavioral differences. Rossi and colleagues observed a differential balance between the GABA-potentiating and inhibiting effects of ethanol in C57Bl6J and DBA mouse strains (Kaplan et al., 2013) that correlate with differences in ethanol intake. More recent studies indicate that enhancing GABAergic transmission in the cerebellum of C57Bl6J mice decreases ethanol drinking to levels seen in DBA mice (Kaplan et al., 2016).
Projections and Large-Scale Circuits
Ultimately, the scope of alcohol research will have to expand to examine effects on large-scale brain circuitry and how circuits control alcohol-related behaviors. In animal models, this work will be bolstered by techniques allowing for more precise control of neuronal projections (e.g., opto- and chemogenetics), as well as new techniques for widespread measurement of neuronal activity. While these approaches are just beginning to be applied within the field, there are some intriguing findings.
Rinker et al. (2017) reported that reducing the function of CRF-expressing bed nucleus of the stria terminalis (BNST)-VTA projections reduces ethanol intake in a mouse model of binge drinking. This effect was mimicked by blockade of CRF1. Both the BNST and CRF are implicated in ethanol drinking and relapse driven by stress and negative affect (Koob, 2015), and there is evidence that BNST-VTA projection neurons regulate the expression of ethanol conditioned place preference (Pina et al., 2015; Pina and Cunningham, 2017).
The limbic corticostriatal circuitry has long been implicated in drug use disorders (Koob and Volkow, 2016). Recent work on inputs from the mPFC and insula to the NAc is illuminating the role of specific synapses and molecules mediating excessive ethanol drinking. These glutamatergic corticostriatal inputs drive the activity of MSNs, and the NMDAR is key for synaptic function and plasticity at these synapses (Lovinger, 2010). Ethanol drinking alters the NMDAR subtypes by insertion of the NR2C subunit at mPFC and insula synapses onto MSNs in the NAc core, but it leaves these receptors unchanged at glutamatergic inputs from amygdala (Seif et al., 2013). The mPFC and insula synapses appear to drive drinking in the face of aversive consequences, and the NR2C subunit is implicated in the loss of this control (Seif et al., 2013). In addition, projections from the ventral subiculum to the NAc shell are also important for ethanol seeking in the face of aversive consequences, as selective inhibition of this pathway by chemogenetic techniques decreased context-induced relapse (Marchant et al., 2016). These findings show how synapse-specific molecular changes alter the ability of limbic circuits to control ethanol drinking in relation to negative environmental events that would normally curtail drinking.
mGluR2 has also been implicated in the control of excessive ethanol intake by dampening corticostriatal input. Chronic ethanol exposure reduces mGluR2 expression in infralimbic NAc shell projection neurons (Meinhardt et al., 2013). This down-regulation contributes to a hyperglutamatergic state within the NAc shell. In an ethanol self-administration paradigm, cues associated with ethanol elicit responding that is especially strong in ethanol-dependent rats and involves limbic corticostriatal circuitry (Meinhardt et al., 2013). Increasing mGluR2 expression in infralimbic projections to the NAc shell attenuates this responding to levels seen in non-dependent rats. Thus, mGluR2 appears to provide a feedback brake on mPFC-drive for excessive ethanol seeking. Interestingly, the alcohol-preferring P rat is a functional mGluR2 knockout, and enhanced ethanol intake is observed in both this rat and mGluR2 knockout mice (Zhou et al., 2013). Inputs to the DMS are also altered by chronic ethanol exposure. Excessive ethanol consumption potentiates glutamatergic transmission via a postsynaptic mechanism at the corticostriatal input and involves a presynaptic mechanism at the amygdalostriatal input (Ma et al., 2017). Chronic ethanol consumption strengthens glutamatergic input to D1-, but not D2-, receptor-expressing DMS MSNs, and GABAergic synaptic strength is enhanced specifically onto D2 MSNs (Cheng et al., 2017; Wang et al., 2015). Interestingly, a bottom-up-approach study following from these findings demonstrated that chemo-genetic excitation of DMS D1 MSNs or inhibition of D2 MSNs promotes ethanol consumption in mice (Cheng et al., 2017).
This circuit-centered work, aided by new technologies, can help to show how specific neuronal pathways and neurotransmitters are implicated in ethanol-specific phenotypes, including reinforcing, appetitive, and consummatory behaviors.
Conclusions
As this review indicates, the effects of ethanol at the molecular, cellular, and circuit levels are myriad and may appear daunting to those outside the field, especially when compared to drugs that act through one predominant molecular target. However, the number of direct and indirect targets of ethanol’s action, while numerous, are still limited enough to allow appreciation of many drug actions that strongly influence circuits and behavior. Furthermore, some targets (e.g., GlyRs, GABA release, NMDARs, GIRK, BK, and SK) mediate ethanol effects on several neurons and synapses throughout the brain. By abandoning a “single-target” view of ethanol’s actions and instead examining which molecules are altered by ethanol in which cells, investigators are beginning to piece together the intoxicating, abuse-promoting, and toxic actions of the drug. With the adoption of new techniques for cellular and circuit manipulation, along with sophisticated measures of neuronal function in vivo and in reduced preparations, researchers can link ethanol’s effects at all levels to behavioral changes brought about by this widely used and abused drug. This rapidly evolving field is providing information that will be valuable in addressing the large public health problem created by this small drug.
Supplementary Material
ACKNOWLEDGMENTS
This work was supported by the Division of Intramural Clinical and Biological Research of the National Institute on Alcohol Abuse and Alcoholism (ZIA AA000407).
Footnotes
SUPPLEMENTAL INFORMATION
Supplemental Information includes two figures and can be found with this article online at https://doi.org/10.1016/j.neuron.2017.10.032.
REFERENCES
- Aalto S, Ingman K, Alakurtti K, Kaasinen V, Virkkala J, Någren K, Rinne JO, and Scheinin H (2015). Intravenous ethanol increases dopamine release in the ventral striatum in humans: PET study using bolus-plus-infusion administration of [(11)C]raclopride. J. Cereb. Blood Flow Metab 35, 424–431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Abrahao KP, Ariwodola OJ, Butler TR, Rau AR, Skelly MJ, Carter E, Alexander NP, McCool BA, Souza-Formigoni ML, and Weiner JL (2013). Locomotor sensitization to ethanol impairs NMDA receptor-dependent synaptic plasticity in the nucleus accumbens and increases ethanol self-administration. J. Neurosci 33, 4834–4842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Abrahao KP, Chancey JH, Chan CS, and Lovinger DM (2017). Ethanolsensitive pacemaker neurons in the mouse external globus pallidus. Neuropsychopharmacology 42, 1070–1081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adermark L, Clarke RB, Ericson M, and Söderpalm B (2011a). Subregion-specific modulation of excitatory input and dopaminergic output in the striatum by tonically activated glycine and GABA(A) receptors. Front. Syst. Neurosci 5, 85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adermark L, Clarke RB, Söderpalm B, and Ericson M (2011b). Ethanol-induced modulation of synaptic output from the dorsolateral striatum in rat is regulated by cholinergic interneurons. Neurochem. Int. 58, 693–699. [DOI] [PubMed] [Google Scholar]
- Adermark L, Jonsson S, Ericson M, and Söderpalm B (2011c). Intermittent ethanol consumption depresses endocannabinoid-signaling in the dorsolateral striatum of rat. Neuropharmacology 61, 1160–1165. [DOI] [PubMed] [Google Scholar]
- Adermark L, Söderpalm B, and Burkhardt JM (2014). Brain region specific modulation of ethanol-induced depression of GABAergic neurons in the brain reward system by the nicotine receptor antagonist mecamylamine. Alcohol 48, 455–461. [DOI] [PubMed] [Google Scholar]
- Aguayo LG, Castro P, Mariqueo T, Muñoz B, Xiong W, Zhang L, Lovinger DM, and Homanics GE (2014). Altered sedative effects of ethanol in mice with α1 glycine receptor subunits that are insensitive to Gβγ modulation. Neuropsychopharmacology 39, 2538–2548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alifimoff JK, Firestone LL, and Miller KW (1989). Anaesthetic potencies of primary alkanols: implications for the molecular dimensions of the anaesthetic site. Br. J. Pharmacol 96, 9–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ando K (1975). The discriminative control of operant behavior by intravenous administration of drugs in rats. Psychopharmacologia 45, 47–50. [Google Scholar]
- Appel SB, Liu Z, McElvain MA, and Brodie MS (2003). Ethanol excitation of dopaminergic ventral tegmental area neurons is blocked by quinidine. J. Pharmacol. Exp. Ther 306, 437–446. [DOI] [PubMed] [Google Scholar]
- Ariwodola OJ, and Weiner JL (2004). Ethanol potentiation of GABAergic synaptic transmission may be self-limiting: role of presynaptic GABA(B) receptors. J. Neurosci 24, 10679–10686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aryal P, Dvir H, Choe S, and Slesinger PA (2009). A discrete alcohol pocket involved in GIRK channel activation. Nat. Neurosci 12, 988–995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Avegno EM, Salling MC, Borgkvist A, Mrejeru A, Whitebirch AC, Margolis EB, Sulzer D, and Harrison NL (2016). Voluntary adolescent drinking enhances excitation by low levels of alcohol in a subset of dopaminergic neurons in the ventral tegmental area. Neuropharmacology 110 (Pt A), 386–395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Badanich KA, Mulholland PJ, Beckley JT, Trantham-Davidson H, and Woodward JJ (2013). Ethanol reduces neuronal excitability of lateral orbito-frontal cortex neurons via a glycine receptor dependent mechanism. Neuropsychopharmacology 38, 1176–1188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bajo M, Cruz MT, Siggins GR, Messing R, and Roberto M (2008). Protein kinase C epsilon mediation of CRF- and ethanol-induced GABA release in central amygdala. Proc. Natl. Acad. Sci. USA 105, 8410–8415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barbaccia ML, Reggiani A, Spano PF, and Trabucchi M (1980). Ethanol effects on dopaminergic function: modulation by the endogenous opioid system. Pharmacol. Biochem. Behav 13 (Suppl 1), 303–306. [DOI] [PubMed] [Google Scholar]
- Basavarajappa BS, Ninan I, and Arancio O (2008). Acute ethanol suppresses glutamatergic neurotransmission through endocannabinoids in hippocampal neurons. J. Neurochem 107, 1001–1013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bassareo V, Cucca F, Frau R, and Di Chiara G (2017). Changes in dopamine transmission in the nucleus accumbens shell and core during ethanol and sucrose self-administration. Front. Behav. Neurosci 11, 71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Belknap JK, Crabbe JC, and Young ER (1993). Voluntary consumption of ethanol in 15 inbred mouse strains. Psychopharmacology (Berl.) 112, 503–510. [DOI] [PubMed] [Google Scholar]
- Bell RL, Hauser SR, McClintick J, Rahman S, Edenberg HJ, Szumlinski KK, and McBride WJ (2016). Ethanol-associated changes in glutamate reward neurocircuitry: a minireview of clinical and preclinical genetic findings. Prog. Mol. Biol. Transl. Sci 137, 41–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benjamin D, Grant ER, and Pohorecky LA (1993). Naltrexone reverses ethanol-induced dopamine release in the nucleus accumbens in awake, freely moving rats. Brain Res. 621, 137–140. [DOI] [PubMed] [Google Scholar]
- Bernier BE, Whitaker LR, and Morikawa H (2011). Previous ethanol experience enhances synaptic plasticity of NMDA receptors in the ventral tegmental area. J. Neurosci 31, 5205–5212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bettinger JC, and Davies AG (2014). The role of the BK channel in ethanol response behaviors: evidence from model organism and human studies. Front. Physiol 5, 346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blednov YA, Benavidez JM, Homanics GE, and Harris RA (2012). Behavioral characterization of knockin mice with mutations M287L and Q266I in the glycine receptor α1 subunit. J. Pharmacol. Exp. Ther 340, 317–329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blednov YA, Benavidez JM, Black M, Leiter CR, Osterndorff-Kahanek E, and Harris RA (2015). Glycine receptors containing α2 or α3 subunits regulate specific ethanol-mediated behaviors. J. Pharmacol. Exp. Ther 353, 181–191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blitzer RD, Gil O, and Landau EM (1990). Long-term potentiation in rat hippocampus is inhibited by low concentrations of ethanol. Brain Res. 537, 203–208. [DOI] [PubMed] [Google Scholar]
- Blomeley CP, Cains S, Smith R, and Bracci E (2011). Ethanol affects striatal interneurons directly and projection neurons through a reduction in cholinergic tone. Neuropsychopharmacology 36, 1033–1046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bodhinathan K, and Slesinger PA (2013). Molecular mechanism underlying ethanol activation of G-protein-gated inwardly rectifying potassium channels. Proc. Natl. Acad. Sci. USA 110, 18309–18314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boileau I, Assaad JM, Pihl RO, Benkelfat C, Leyton M, Diksic M, Tremblay RE, and Dagher A (2003). Alcohol promotes dopamine release in the human nucleus accumbens. Synapse 49, 226–231. [DOI] [PubMed] [Google Scholar]
- Bose J, Hedden SL, Lipari RN, Park-Lee E, Porter J, and Pemberton M (2016). Key substance use and mental health indicators in the United States: results from the 2015 National Survey on Drug Use and Health. Report of the Substance Abuse and Mental Health Services Administration; https://www.samhsa.gov/data/sites/default/files/NSDUH-FFR1-2015/NSDUH-FFR1-2015/NSDUH-FFR1-2015.pdf. [Google Scholar]
- Budygin EA, Phillips PE, Wightman RM, and Jones SR (2001). Terminal effects of ethanol on dopamine dynamics in rat nucleus accumbens: an in vitro voltammetric study. Synapse 42, 77–79. [DOI] [PubMed] [Google Scholar]
- Bukiya AN, Kuntamallappanavar G, Edwards J, Singh AK, Shivakumar B, and Dopico AM (2014). An alcohol-sensing site in the calcium- and voltage-gated, large conductance potassium (BK) channel. Proc. Natl. Acad. Sci. USA 111, 9313–9318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burgos CF, Castro PA, Mariqueo T, Bunster M, Guzmán L, and Aguayo LG (2015). Evidence for α-helices in the large intracellular domain mediating modulation of the α1-glycine receptor by ethanol and Gβγ. J. Pharmacol. Exp. Ther 352, 148–155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burkhardt JM, and Adermark L (2014). Locus of onset and subpopulation specificity of in vivo ethanol effect in the reciprocal ventral tegmental area-nucleus accumbens circuit. Neurochem. Int 76, 122–130. [DOI] [PubMed] [Google Scholar]
- Carta M, Partridge LD, Savage DD, and Valenzuela CF (2003). Neurosteroid modulation of glutamate release in hippocampal neurons: lack of an effect of a chronic prenatal ethanol exposure paradigm. Alcohol. Clin. Exp. Res 27, 1194–1198. [DOI] [PubMed] [Google Scholar]
- Carta M, Mameli M, and Valenzuela CF (2004). Alcohol enhances GABAergic transmission to cerebellar granule cells via an increase in Golgi cell excitability. J. Neurosci 24, 3746–3751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chandler LJ, Harris RA, and Crews FT (1998). Ethanol tolerance and synaptic plasticity. Trends Pharmacol. Sci 19, 491–495. [DOI] [PubMed] [Google Scholar]
- Cheng Y, Huang CCY, Ma T, Wei X, Wang X, Lu J, and Wang J (2017). Distinct synaptic strengthening of the striatal direct and indirect pathways drives alcohol consumption. Biol. Psychiatry 81, 918–929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choi DS, Wei W, Deitchman JK, Kharazia VN, Lesscher HM, McMahon T, Wang D, Qi ZH, Sieghart W, Zhang C, et al. (2008). Protein kinase Cdelta regulates ethanol intoxication and enhancement of GABA-stimulated tonic current. J. Neurosci 28, 11890–11899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Christian DT, Alexander NJ, Diaz MR, and McCool BA (2013). Thalamic glutamatergic afferents into the rat basolateral amygdala exhibit increased presynaptic glutamate function following withdrawal from chronic intermittent ethanol. Neuropharmacology 65, 134–142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clarke RB, and Adermark L (2010). Acute ethanol treatment prevents endo-cannabinoid-mediated long-lasting disinhibition of striatal output. Neuropharmacology 58, 799–805. [DOI] [PubMed] [Google Scholar]
- Clarke R, and Adermark L (2015). Dopaminergic regulation of striatal interneurons in reward and addiction: focus on alcohol. Neural Plast. 2015, 814567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coune F, Silvestre de Ferron B, González-Marín MC, Antol J, Naassila M, and Pierrefiche O (2017). Resistance to ethanol sensitization is associated with a loss of synaptic plasticity in the hippocampus. Synapse 71, 2. [DOI] [PubMed] [Google Scholar]
- Criswell HE, Ming Z, Kelm MK, and Breese GR (2008). Brain regional differences in the effect of ethanol on GABA release from presynaptic terminals. J. Pharmacol. Exp. Ther 326, 596–603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cruz MT, Herman MA, Kallupi M, and Roberto M (2012). Nociceptin/orphanin FQ blockade of corticotropin-releasing factor-induced gamma-aminobutyric acid release in central amygdala is enhanced after chronic ethanol exposure. Biol. Psychiatry 71, 666–676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cui C, and Koob GF (2017). Titrating tipsy targets: the neurobiology of low-dose alcohol. Trends Pharmacol. Sci 38, 556–568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cui SZ, Wang SJ, Li J, Xie GQ, Zhou R, Chen L, and Yuan XR (2011). Alteration of synaptic plasticity in rat dorsal striatum induced by chronic ethanol intake and withdrawal via ERK pathway. Acta Pharmacol. Sin 32, 175–181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cunningham CL, Niehus DR, Malott DH, and Prather LK (1992). Genetic differences in the rewarding and activating effects of morphine and ethanol. Psychopharmacology (Berl.) 107, 385–393. [DOI] [PubMed] [Google Scholar]
- Cuzon Carlson VC, Seabold GK, Helms CM, Garg N, Odagiri M, Rau AR, Daunais J, Alvarez VA, Lovinger DM, and Grant KA (2011). Synaptic and morphological neuroadaptations in the putamen associated with longterm, relapsing alcohol drinking in primates. Neuropsychopharmacology 36, 2513–2528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis TJ, and de Fiebre CM (2006). Alcohol’s actions on neuronal nicotinic acetylcholine receptors. Alcohol Res. Health 29, 179–185. [PMC free article] [PubMed] [Google Scholar]
- Deehan GA Jr., Knight CP, Waeiss RA, Engleman EA, Toalston JE, McBride WJ, Hauser SR, and Rodd ZA (2016). Peripheral administration of ethanol results in a correlated increase in dopamine and serotonin within the posterior ventral tegmental area. Alcohol Alcohol. 51, 535–540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- den Hartog CR, Beckley JT, Smothers TC, Lench DH, Holseberg ZL, Fedarovich H, Gilstrap MJ, Homanics GE, and Woodward JJ (2013). Alterations in ethanol-induced behaviors and consumption in knock-in mice expressing ethanol-resistant NMDA receptors. PLoS ONE 8, e80541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- den Hartog CR, Gilstrap M, Eaton B, Lench DH, Mulholland PJ, Homanics GE, and Woodward JJ (2017). Effects of repeated ethanol exposures on NMDA receptor expression and locomotor sensitization in mice expressing ethanol resistant NMDA receptors. Front. Neurosci 11, 84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DePoy L, Daut R, Brigman JL, MacPherson K, Crowley N, Gunduz-Cinar O, Pickens CL, Cinar R, Saksida LM, Kunos G, et al. (2013). Chronic alcohol produces neuroadaptations to prime dorsal striatal learning. Proc. Natl. Acad. Sci. USA 110, 14783–14788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diana M, Pistis M, Muntoni A, and Gessa G (1996). Mesolimbic dopaminergic reduction outlasts ethanol withdrawal syndrome: evidence of protracted abstinence. Neuroscience 71, 411–415. [DOI] [PubMed] [Google Scholar]
- Diaz MR, and Valenzuela CF (2016). Sensitivity of GABAergic tonic currents to acute ethanol in cerebellar granule neurons is not age- or δ subunit- dependent in developing rats. Alcohol. Clin. Exp. Res 40, 83–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Didone V, Masson S, Quoilin C, Seutin V, and Quertemont E (2016). Correlation between ethanol behavioral sensitization and midbrain dopamine neuron reactivity to ethanol. Addict. Biol 21, 387–396. [DOI] [PubMed] [Google Scholar]
- Ding ZM, Ingraham CM, Rodd ZA, and McBride WJ (2016). Alcohol drinking increases the dopamine-stimulating effects of ethanol and reduces D2 auto-receptor and group II metabotropic glutamate receptor function within the posterior ventral tegmental area of alcohol preferring (P) rats. Neuropharmacology 109, 41–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dopico AM, Bukiya AN, and Martin GE (2014). Ethanol modulation of mammalian BK channels in excitable tissues: molecular targets and their possible contribution to alcohol-induced altered behavior. Front. Physiol 5, 466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dreixler JC, Jenkins A, Cao YJ, Roizen JD, and Houamed KM (2000). Patch-clamp analysis of anesthetic interactions with recombinant SK2 subtype neuronal calcium-activated potassium channels. Anesth. Analg. 90, 727–732. [DOI] [PubMed] [Google Scholar]
- Durand D, and Carlen PL (1984). Impairment of long-term potentiation in rat hippocampus following chronic ethanol treatment. Brain Res. 308, 325–332. [DOI] [PubMed] [Google Scholar]
- Ericson M, Blomqvist O, Engel JA, and Söderpalm B (1998). Voluntary ethanol intake in the rat and the associated accumbal dopamine overflow are blocked by ventral tegmental mecamylamine. Eur. J. Pharmacol 358, 189–196. [DOI] [PubMed] [Google Scholar]
- Ericson M, Chau P, Clarke RB, Adermark L, and Söderpalm B (2011). Rising taurine and ethanol concentrations in nucleus accumbens interact to produce dopamine release after ethanol administration. Addict. Biol 16, 377–385. [DOI] [PubMed] [Google Scholar]
- Förstera B, Muñoz B, Lobo MK, Chandra R, Lovinger DM, and Aguayo LG (2017). Presence of ethanol-sensitive glycine receptors in medium spiny neurons in the mouse nucleus accumbens. J. Physiol 595, 5285–5300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fujii S, Yamazaki Y, Sugihara T, and Wakabayashi I (2008). Acute and chronic ethanol exposure differentially affect induction of hippocampal LTP. Brain Res. 1211, 13–21. [DOI] [PubMed] [Google Scholar]
- Gass JT, and Olive MF (2008). Glutamatergic substrates of drug addiction and alcoholism. Biochem. Pharmacol 75, 218–265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gatto GJ, McBride WJ, Murphy JM, Lumeng L, and Li TK (1994). Ethanol self-infusion into the ventral tegmental area by alcohol-preferring rats. Alcohol 11, 557–564. [DOI] [PubMed] [Google Scholar]
- Glaaser IW, and Slesinger PA (2017). Dual activation of neuronal G proteingated inwardly rectifying potassium (GIRK) channels by cholesterol and alcohol. Sci. Rep. 7, 4592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gonzales RA, and Weiss F (1998). Suppression of ethanol-reinforced behavior by naltrexone is associated with attenuation of the ethanol-induced increase in dialysate dopamine levels in the nucleus accumbens. J. Neurosci 18, 10663–10671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goto M, Kitamura H, Alam MM, Ota N, Haseba T, Akimoto T, Shimizu A, Takano-Yamamoto T, Yamamoto M, and Motohashi H (2015). Alcohol dehydrogenase 3 contributes to the protection of liver from nonalcoholic steatohepatitis. Genes Cells 20, 464–480. [DOI] [PubMed] [Google Scholar]
- Griffin WC 3rd, Haun HL, Hazelbaker CL, Ramachandra VS, and Becker HC (2014). Increased extracellular glutamate in the nucleus accumbens promotes excessive ethanol drinking in ethanol dependent mice. Neuropsychopharmacology 39, 707–717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guan YZ, and Ye JH (2010). Ethanol blocks long-term potentiation of GABAergic synapses in the ventral tegmental area involving mu-opioid receptors. Neuropsychopharmacology 35, 1841–1849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris RA, Mihic SJ, Brozowski S, Hadingham K, and Whiting PJ (1997). Ethanol, flunitrazepam, and pentobarbital modulation of GABAA receptors expressed in mammalian cells and Xenopus oocytes. Alcohol. Clin. Exp. Res 21, 444–451. [DOI] [PubMed] [Google Scholar]
- Harris RA, Trudell JR, and Mihic SJ (2008). Ethanol’s molecular targets. Sci. Signal 1, re7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hendrickson LM, Guildford MJ, and Tapper AR (2013). Neuronal nicotinic acetylcholine receptors: common molecular substrates of nicotine and alcohol dependence. Front. Psychiatry 4, 29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hendricson AW, Miao CL, Lippmann MJ, and Morrisett RA (2002). Ifenprodil and ethanol enhance NMDA receptor-dependent long-term depression. J. Pharmacol. Exp. Ther 301, 938–944. [DOI] [PubMed] [Google Scholar]
- Hendricson AW, Sibbald JR, and Morrisett RA (2004). Ethanol alters the frequency, amplitude, and decay kinetics of Sr2+-supported, asynchronous NMDAR mEPSCs in rat hippocampal slices. J. Neurophysiol 91, 2568–2577. [DOI] [PubMed] [Google Scholar]
- Hendricson AW, Maldve RE, Salinas AG, Theile JW, Zhang TA, Diaz LM, and Morrisett RA (2007). Aberrant synaptic activation of N-methyl-D-aspartate receptors underlies ethanol withdrawal hyperexcitability. J. Pharmacol. Exp. Ther. 321, 60–72. [DOI] [PubMed] [Google Scholar]
- Herman MA, and Roberto M (2016). Cell-type-specific tonic GABA signaling in the rat central amygdala is selectively altered by acute and chronic ethanol. Addict. Biol 21, 72–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herman MA, Sidhu H, Stouffer DG, Kreifeldt M, Le D, Cates-Gatto C, Munoz MB, Roberts AJ, Parsons LH, Roberto M, et al. (2015). GIRK3 gates activation of the mesolimbic dopaminergic pathway by ethanol. Proc. Natl. Acad. Sci. USA 112, 7091–7096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herman MA, Contet C, and Roberto M (2016a). A functional switch in tonic GABA currents alters the output of central amygdala corticotropin releasing factor receptor-1 neurons following chronic ethanol exposure. J. Neurosci. 36, 10729–10741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herman MA, Varodayan FP, Oleata CS, Luu G, Kirson D, Heilig M, Ciccocioppo R, and Roberto M (2016b). Glutamatergic transmission in the central nucleus of the amygdala is selectively altered in Marchigian Sardinian alcohol-preferring rats: alcohol and CRF effects. Neuropharmacology 102, 21–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hirth N, Meinhardt MW, Noori HR, Salgado H, Torres-Ramirez O, Uhrig S, Broccoli L, Vengeliene V, RoBmanith M, Perreau-Lenz S, et al. (2016). Convergent evidence from alcohol-dependent humans and rats for a hyperdopaminergic state in protracted abstinence. Proc. Natl. Acad. Sci. USA 113, 3024–3029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hopf FW, Bowers MS, Chang SJ, Chen BT, Martin M, Seif T, Cho SL, Tye K, and Bonci A (2010). Reduced nucleus accumbens SK channel activity enhances alcohol seeking during abstinence. Neuron 65, 682–694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Howard RJ, Trudell JR, and Harris RA (2014). Seeking structural specificity: direct modulation of pentameric ligand-gated ion channels by alcohols and general anesthetics. Pharmacol. Rev 66, 396–412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hwa L, Besheer J, and Kash T (2017). Glutamate plasticity woven through the progression to alcohol use disorder: a multi-circuit perspective. F1000Res. 6, 298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Irimia C, Buczynski MW, Natividad LA, Laredo SA, Avalos N, and Parsons LH (2017). Dysregulated glycine signaling contributes to increased impulsivity during protracted alcohol abstinence. J. Neurosci 37, 1853–1861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Izumi Y, and Zorumski CF (2012). NMDA receptors, mGluR5, and endocannabinoids are involved in a cascade leading to hippocampal long-term depression. Neuropsychopharmacology 37, 609–617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Izumi Y, Kitabayashi R, Funatsu M, Izumi M, Yuede C, Hartman RE, Wozniak DF, and Zorumski CF (2005). A single day of ethanol exposure during development has persistent effects on bi-directional plasticity, N-methyl-D-aspartate receptor function and ethanol sensitivity. Neuroscience 136, 269–279. [DOI] [PubMed] [Google Scholar]
- Izumi Y, O’Dell KA, and Zorumski CF (2015). Corticosterone enhances the potency of ethanol against hippocampal long-term potentiation via local neurosteroid synthesis. Front. Cell. Neurosci. 9, 254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jeanes ZM, Buske TR, and Morrisett RA (2014). Cell type-specific synaptic encoding of ethanol exposure in the nucleus accumbens shell. Neuroscience 277, 184–195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jia F, Chandra D, Homanics GE, and Harrison NL (2008). Ethanol modulates synaptic and extrasynaptic GABAA receptors in the thalamus. J. Pharmacol. Exp. Ther 326, 475–482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson RA, Noll EC, and Rodney WM (1982). Survival after a serum ethanol concentration of 1 ½%. Lancet 2, 1394. [DOI] [PubMed] [Google Scholar]
- Kang-Park M, Kieffer BL, Roberts AJ, Siggins GR, and Moore SD (2013). κ-Opioid receptors in the central amygdala regulate ethanol actions at presynaptic GABAergic sites. J. Pharmacol. Exp. Ther 346, 130–137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaplan JS, Mohr C, and Rossi DJ (2013). Opposite actions of alcohol on tonic GABA(A) receptor currents mediated by nNOS and PKC activity. Nat. Neurosci 16, 1783–1793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaplan JS, Nipper MA, Richardson BD, Jensen J, Helms M, Finn DA, and Rossi DJ (2016). Pharmacologically counteracting a phenotypic difference in cerebellar GABAA receptor response to alcohol prevents excessive alcohol consumption in a high alcohol-consuming rodent genotype. J. Neurosci. 36, 9019–9025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karkhanis AN, Huggins KN, Rose JH, and Jones SR (2016). Switch from excitatory to inhibitory actions of ethanol on dopamine levels after chronic exposure: Role of kappa opioid receptors. Neuropharmacology 110 (Pt A), 190–197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelm MK, Criswell HE, and Breese GR (2007). Calcium release from presynaptic internal stores is required for ethanol to increase spontaneous gamma-aminobutyric acid release onto cerebellum Purkinje neurons. J. Pharmacol. Exp. Ther 323, 356–364. [DOI] [PubMed] [Google Scholar]
- Kelm MK, Criswell HE, and Breese GR (2011). Ethanol-enhanced GABA release: a focus on G protein-coupled receptors. Brain Res. Brain Res. Rev 65, 113–123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirson D, Oleata CS, Parsons LH, Ciccocioppo R, and Roberto M (2017). CB1 and ethanol effects on glutamatergic transmission in the central amygdala of male and female msP and Wistar rats. Addict. Biol Published online June 28, 2017. 10.1111/adb.12525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kobayashi T, Ikeda K, Ichikawa T, Abe S, Togashi S, and Kumanishi T (1995). Molecular cloning of a mouse G-protein-activated K+ channel (mGlRK1) and distinct distributions of three GIRK (GIRK1, 2 and 3) mRNAs in mouse brain. Biochem. Biophys. Res. Commun 208, 1166–1173. [DOI] [PubMed] [Google Scholar]
- Kobayashi T, Ikeda K, Kojima H, Niki H, Yano R, Yoshioka T, and Kumanishi T (1999). Ethanol opens G-protein-activated inwardly rectifying K+ channels. Nat. Neurosci 2, 1091–1097. [DOI] [PubMed] [Google Scholar]
- Koob GF (2015). The dark side of emotion: the addiction perspective. Eur. J. Pharmacol 753, 73–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koob GF, and Volkow ND (2016). Neurobiology of addiction: a neurocircuitry analysis. Lancet Psychiatry 3, 760–773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Korkotian E, Bombela T, Odegova T, Zubov P, and Segal M (2013). Ethanol affects network activity in cultured rat hippocampus: mediation by potassium channels. PLoS ONE 8, e75988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroener S, Mulholland PJ, New NN, Gass JT, Becker HC, and Chandler LJ (2012). Chronic alcohol exposure alters behavioral and synaptic plasticity of the rodent prefrontal cortex. PLoS ONE 7, e37541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Läck AK, Diaz MR, Chappell A, DuBois DW, and McCool BA (2007). Chronic ethanol and withdrawal differentially modulate pre- and postsynaptic function at glutamatergic synapses in rat basolateral amygdala. J. Neurophysiol 98, 3185–3196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Läck AK, Christian DT, Diaz MR, and McCool BA (2009). Chronic ethanol and withdrawal effects on kainate receptor-mediated excitatory neurotransmission in the rat basolateral amygdala. Alcohol 43, 25–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lammel S, Hetzel A, Häckel O, Jones I, Liss B, and Roeper J (2008). Unique properties of mesoprefrontal neurons within a dual mesocorticolimbic dopamine system. Neuron 57, 760–773. [DOI] [PubMed] [Google Scholar]
- Lewohl JM, Wilson WR, Mayfield RD, Brozowski SJ, Morrisett RA, and Harris RA (1999). G-protein-coupled inwardly rectifying potassium channels are targets of alcohol action. Nat. Neurosci 2, 1084–1090. [DOI] [PubMed] [Google Scholar]
- Liang J, Zhang N, Cagetti E, Houser CR, Olsen RW, and Spigelman I (2006). Chronic intermittent ethanol-induced switch of ethanol actions from extrasynaptic to synaptic hippocampal GABAA receptors. J. Neurosci 26, 1749–1758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lovinger DM (2010). Neurotransmitter roles in synaptic modulation, plasticity and learning in the dorsal striatum. Neuropharmacology 58, 951–961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lovinger DM, and Kash TL (2015). Mechanisms of neuroplasticity and ethanol’s effects on plasticity in the striatum and bed nucleus of the stria terminalis. Alcohol Res. 37, 109–124. [PMC free article] [PubMed] [Google Scholar]
- Lovinger DM, and Roberto M (2013). Synaptic effects induced by alcohol. Curr. Top. Behav. Neurosci 13, 31–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lovinger DM, White G, and Weight FF (1990). NMDA receptor-mediated synaptic excitation selectively inhibited by ethanol in hippocampal slice from adult rat. J. Neurosci 10, 1372–1379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ma T, Barbee B, Wang X, and Wang J (2017). Alcohol induces input-specific aberrant synaptic plasticity in the rat dorsomedial striatum. Neuropharmacology 123, 46–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maldve RE, Chen X, Zhang TA, and Morrisett RA (2004). Ethanol selectively inhibits enhanced vesicular release at excitatory synapses: real-time visualization in intact hippocampal slices. Alcohol. Clin. Exp. Res 28, 143–152. [DOI] [PubMed] [Google Scholar]
- Marchant NJ, Campbell EJ, Whitaker LR, Harvey BK, Kaganovsky K, Adhikary S, Hope BT, Heins RC, Prisinzano TE, Vardy E, et al. (2016). Role of ventral subiculum in context-induced relapse to alcohol seeking after punishment-imposed abstinence. J. Neurosci 36, 3281–3294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin GE, Hendrickson LM, Penta KL, Friesen RM, Pietrzykowski AZ, Tapper AR, and Treistman SN (2008). Identification of a BK channel auxiliary protein controlling molecular and behavioral tolerance to alcohol. Proc. Natl. Acad. Sci. USA 105, 17543–17548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mascia MP, Machu TK, and Harris RA (1996). Enhancement of homomeric glycine receptor function by long-chain alcohols and anaesthetics. Br. J. Pharmacol 119, 1331–1336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mayfield J, Arends MA, Harris RA, and Blednov YA (2016). Genes and alcohol consumption: studies with mutant mice. Int. Rev. Neurobiol 126, 293–355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McBride WJ, Lovinger DM, Machu T, Thielen RJ, Rodd ZA, Murphy JM, Roache JD, and Johnson BA (2004). Serotonin-3 receptors in the actions of alcohol, alcohol reinforcement, and alcoholism. Alcohol. Clin. Exp. Res 28, 257–267. [DOI] [PubMed] [Google Scholar]
- McCool BA (2011). Ethanol modulation of synaptic plasticity. Neuropharmacology 61, 1097–1108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCracken LM, Lowes DC, Salling MC, Carreau-Vollmer C, Odean NN, Blednov YA, Betz H, Harris RA, and Harrison NL (2017). Glycine receptor α3 and α2 subunits mediate tonic and exogenous agonist-induced currents in forebrain. Proc. Natl. Acad. Sci. USA 114, E7179–E7186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McDaid J, McElvain MA, and Brodie MS (2008). Ethanol effects on dopaminergic ventral tegmental area neurons during block of Ih: involvement of barium-sensitive potassium currents. J. Neurophysiol 100, 1202–1210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meinhardt MW, Hansson AC, Perreau-Lenz S, Bauder-Wenz C, Stählin O, Heilig M, Harper C, Drescher KU, Spanagel R, and Sommer WH (2013). Rescue of infralimbic mGluR2 deficit restores control over drug-seeking behavior in alcohol dependence. J. Neurosci 33, 2794–2806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Melis M, Enrico P, Peana AT, and Diana M (2007). Acetaldehyde mediates alcohol activation of the mesolimbic dopamine system. Eur. J. Neurosci 26, 2824–2833. [DOI] [PubMed] [Google Scholar]
- Mihic SJ (1999). Acute effects of ethanol on GABAA and glycine receptor function. Neurochem. Int. 35, 115–123. [DOI] [PubMed] [Google Scholar]
- Mihic SJ, and Harris RA (2011). Hypnotics and sedatives. In Goodman & Gilman’s the Pharmacological Basis of Therapeutics, Brunton LL, Chabner BA, and Knollmann BC, eds. (McGraw Hill and Company; ), pp. 457–480. [Google Scholar]
- Mihov Y, and Hasler G (2016). Negative allosteric modulators of metabotropic glutamate receptors subtype 5 in addiction: a therapeutic window. Int. J. Neuropsychopharmacol 19, pyw002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mishra D, Zhang X, and Chergui K (2012). Ethanol disrupts the mechanisms of induction of long-term potentiation in the mouse nucleus accumbens. Alcohol. Clin. Exp. Res 36, 2117–2125. [DOI] [PubMed] [Google Scholar]
- Mokdad AH, Marks JS, Stroup DF, and Gerberding JL (2004). Actual causes of death in the United States, 2000. JAMA 291, 1238–1245. [DOI] [PubMed] [Google Scholar]
- Moore MS, DeZazzo J, Luk AY, Tully T, Singh CM, and Heberlein U (1998). Ethanol intoxication in Drosophila: genetic and pharmacological evidence for regulation by the cAMP signaling pathway. Cell 93, 997–1007. [DOI] [PubMed] [Google Scholar]
- Morikawa H, and Morrisett RA (2010). Ethanol action on dopaminergic neurons in the ventral tegmental area: interaction with intrinsic ion channels and neurotransmitter inputs. Int. Rev. Neurobiol 91, 235–288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morrisett RA, and Swartzwelder HS (1993). Attenuation of hippocampal long-term potentiation by ethanol: a patch-clamp analysis of glutamatergic and GABAergic mechanisms. J. Neurosci 13, 2264–2272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Möykkynen T, and Korpi ER (2012). Acute effects of ethanol on glutamate receptors. Basic Clin. Pharmacol. Toxicol 111, 4–13. [DOI] [PubMed] [Google Scholar]
- Mrejeru A, Martí-Prats L,Avegno EM, Harrison NL, and Sulzer D (2015). A subset of ventral tegmental area dopamine neurons responds to acute ethanol. Neuroscience 290, 649–658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mulholland PJ, Hopf FW, Bukiya AN, Martin GE, Liu J, Dopico AM, Bonci A, Treistman SN, and Chandler LJ (2009). Sizing up ethanol-induced plasticity: the role of small and large conductance calcium-activated potassium channels. Alcohol. Clin. Exp. Res 33, 1125–1135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mulholland PJ, Becker HC, Woodward JJ, and Chandler LJ (2011). Small conductance calcium-activated potassium type 2 channels regulate alcohol-associated plasticity of glutamatergic synapses. Biol. Psychiatry 69, 625–632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nie Z, Schweitzer P, Roberts AJ, Madamba SG, Moore SD, and Siggins GR (2004). Ethanol augments GABAergic transmission in the central amygdala via CRF1 receptors. Science 303, 1512–1514. [DOI] [PubMed] [Google Scholar]
- Nimitvilai S, Lopez MF, Mulholland PJ, and Woodward JJ (2016a). Chronic intermittent ethanol exposure enhances the excitability and synaptic plasticity of lateral orbitofrontal cortex neurons and induces a tolerance to the acute inhibitory actions of ethanol. Neuropsychopharmacology 41, 1112–1127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nimitvilai S, You C, Arora DS, McElvain MA, Vandegrift BJ, Brodie MS, and Woodward JJ (2016b). Differential effects of toluene and ethanol on dopaminergic neurons of the ventral tegmental area. Front. Neurosci. 10, 434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oh KH, Haney JJ, Wang X, Chuang CF, Richmond JE, and Kim H (2017). ERG-28 controls BK channel trafficking in the ER to regulate synaptic function and alcohol response in C. elegans. eLife 6, e24733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Okamoto T, Harnett MT, and Morikawa H (2006). Hyperpolarization-activated cation current (Ih) is an ethanol target in midbrain dopamine neurons of mice. J. Neurophysiol 95, 619–626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olsen RW, Li GD, Wallner M, Trudell JR, Bertaccini EJ, Lindahl E, Miller KW, Alkana RL, and Davies DL (2014). Structural models of ligand-gated ion channels: sites of action for anesthetics and ethanol. Alcohol. Clin. Exp. Res 38, 595–603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oslin DW, and Cary MS (2003). Alcohol-related dementia: validation of diagnostic criteria. Am. J. Geriatr. Psychiatry 11, 441–447. [PubMed] [Google Scholar]
- Overstreet LS, Pasternak JF, Colley PA, Slater NT, and Trommer BL (1997). Metabotropic glutamate receptor mediated long-term depression in developing hippocampus. Neuropharmacology 36, 831–844. [DOI] [PubMed] [Google Scholar]
- Padula AE, Griffin WC 3rd, Lopez MF, Nimitvilai S, Cannady R, McGuier NS, Chesler EJ, Miles MF, Williams RW, Randall PK, et al. (2015). KCNN genes that encode small-conductance Ca2+-activated K+ channels influence alcohol and drug addiction. Neuropsychopharmacology 40, 1928–1939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palacio S, Velázquez-Marrero C, Marrero HG, Seale GE, Yudowski GA, and Treistman SN (2015). Time-dependent effects of ethanol on BK channel expression and trafficking in hippocampal neurons. Alcohol. Clin. Exp. Res 39, 1619–1631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pany S, and Das J (2015). Alcohol binding in the C1 (C1A+C1B) domain of protein kinase C epsilon. Biochim. Biophys. Acta 1850, 2368–2376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patton MH, Roberts BM, Lovinger DM, and Mathur BN (2016). Ethanol disinhibits dorsolateral striatal medium spiny neurons through activation of a presynaptic delta opioid receptor. Neuropsychopharmacology 41, 1831–1840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peoples RW, Li C, and Weight FF (1996). Lipid vs protein theories of alcohol action in the nervous system. Annu. Rev. Pharmacol. Toxicol 36, 185–201. [DOI] [PubMed] [Google Scholar]
- Perkins DI, Trudell JR, Crawford DK, Alkana RL, and Davies DL (2010). Molecular targets and mechanisms for ethanol action in glycine receptors. Pharmacol. Ther 127, 53–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perra S, Clements MA, Bernier BE, and Morikawa H (2011). In vivo ethanol experience increases D(2) autoinhibition in the ventral tegmental area. Neuropsychopharmacology 36, 993–1002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phillips TJ, and Shen EH (1996). Neurochemical bases of locomotion and ethanol stimulant effects. Int. Rev. Neurobiol 39, 243–282. [DOI] [PubMed] [Google Scholar]
- Pietrzykowski AZ, Martin GE, Puig SI, Knott TK, Lemos JR, and Treistman SN (2004). Alcohol tolerance in large-conductance, calcium-activated potassium channels of CNS terminals is intrinsic and includes two components: decreased ethanol potentiation and decreased channel density. J. Neurosci 24, 8322–8332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pina MM, and Cunningham CL (2017). Ethanol-seeking behavior is expressed directly through an extended amygdala to midbrain neural circuit. Neurobiol. Learn. Mem 137, 83–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pina MM, Young EA, Ryabinin AE, and Cunningham CL (2015).The bed nucleus of the stria terminalis regulates ethanol-seeking behavior in mice. Neuropharmacology 99, 627–638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Poulin JF, Zou J, Drouin-Ouellet J, Kim KY, Cicchetti F, and Awatramani RB (2014). Defining midbrain dopaminergic neuron diversity by single-cell gene expression profiling. Cell Rep. 9, 930–943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Proctor WR, Poelchen W, Bowers BJ, Wehner JM, Messing RO, and Dunwiddie TV (2003). Ethanol differentially enhances hippocampal GABA A receptor-mediated responses in protein kinase C gamma (PKC gamma) and PKC epsilon null mice. J. Pharmacol. Exp. Ther 305, 264–270. [DOI] [PubMed] [Google Scholar]
- Radke AK, Jury NJ, Delpire E, Nakazawa K, and Holmes A (2017a). Reduced ethanol drinking following selective cortical interneuron deletion of the GluN2B NMDA receptors subunit. Alcohol 58, 47–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radke AK, Jury NJ, Kocharian A, Marcinkiewcz CA, Lowery-Gionta EG, Pleil KE, McElligott ZA, McKlveen JM, Kash TL, and Holmes A (2017b). Chronic EtOH effects on putative measures of compulsive behavior in mice. Addict. Biol 22, 423–434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rahman S, Engleman EA, and Bell RL (2016). Recent advances in nicotinic receptor signaling in alcohol abuse and alcoholism. Prog. Mol. Biol. Transl. Sci 137, 183–201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramachandran B, Ahmed S, Zafar N, and Dean C (2015). Ethanol inhibits long-term potentiation in hippocampal CA1 neurons, irrespective of lamina and stimulus strength, through neurosteroidogenesis. Hippocampus 25, 106–118. [DOI] [PubMed] [Google Scholar]
- Rao PS, Bell RL, Engleman EA, and Sari Y (2015). Targeting glutamate uptake to treat alcohol use disorders. Front. Neurosci. 9, 144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rassnick S, Stinus L, and Koob GF (1993). The effects of 6-hydroxydop-amine lesions of the nucleus accumbens and the mesolimbic dopamine system on oral self-administration of ethanol in the rat. Brain Res. 623, 16–24. [DOI] [PubMed] [Google Scholar]
- Renteria R, Jeanes ZM, Mangieri RA, Maier EY, Kircher DM, Buske TR, and Morrisett RA (2016). Using in vitro electrophysiology to screen medications: accumbal plasticity as an engram of alcohol dependence. Int. Rev. Neurobiol 126, 441–465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Renteria R, Buske TR, and Morrisett RA (2017). Long-term subregion-specific encoding of enhanced ethanol intake by D1DR medium spiny neurons of the nucleus accumbens. Addict. Biol. Published online June 28, 2017. 10.1111/adb.12526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rinker JA, Marshall SA, Mazzone CM, Lowery-Gionta EG, Gulati V, Pleil KE, Kash TL, Navarro M, and Thiele TE (2017). Extended amygdala to ventral tegmental area corticotropin-releasing factor circuit controls binge ethanol intake. Biol. Psychiatry 81, 930–940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberto M, and Varodayan FP (2017). Synaptic targets: dhronic alcohol actions. Neuropharmacology 122, 85–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberto M, Nelson TE, Ur CL, and Gruol DL (2002). Long-term potentiation in the rat hippocampus is reversibly depressed by chronic intermittent ethanol exposure. J. Neurophysiol 87, 2385–2397. [DOI] [PubMed] [Google Scholar]
- Roberto M, Madamba SG, Moore SD, Tallent MK, and Siggins GR (2003). Ethanol increases GABAergic transmission at both pre- and postsynaptic sites in rat central amygdala neurons. Proc. Natl. Acad. Sci. USA 100, 2053–2058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberto M, Madamba SG, Stouffer DG, Parsons LH, and Siggins GR (2004a). Increased GABA release in the central amygdala of ethanol-dependent rats. J. Neurosci. 24, 10159–10166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberto M, Schweitzer P, Madamba SG, Stouffer DG, Parsons LH, and Siggins GR (2004b). Acute and chronic ethanol alter glutamatergic transmission in rat central amygdala: an in vitro and in vivo analysis. J. Neurosci. 24, 1594–1603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberto M, Bajo M, Crawford E, Madamba SG, and Siggins GR (2006). Chronic ethanol exposure and protracted abstinence alter NMDA receptors in central amygdala. Neuropsychopharmacology 31, 988–996. [DOI] [PubMed] [Google Scholar]
- Roberto M, Cruz M, Bajo M, Siggins GR, Parsons LH, and Schweitzer P (2010). The endocannabinoid system tonically regulates inhibitory transmission and depresses the effect of ethanol in central amygdala. Neuropsychopharmacology 35, 1962–1972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodd ZA, Melendez RI, Bell RL, Kuc KA, Zhang Y, Murphy JM, and McBride WJ (2004). Intracranial self-administration of ethanol within the ventral tegmental area of male Wistar rats: evidence for involvement of dopamine neurons. J. Neurosci 24, 1050–1057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ron D, and Barak S (2016). Molecular mechanisms underlying alcohol-drinking behaviours. Nat. Rev. Neurosci 17, 576–591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ronald KM, Mirshahi T, and Woodward JJ (2001). Ethanol inhibition of N-methyl-D-aspartate receptors is reduced by site-directed mutagenesis of a transmembrane domain phenylalanine residue. J. Biol. Chem 276, 44729–44735. [DOI] [PubMed] [Google Scholar]
- Rose JH, Karkhanis AN, Chen R, Gioia D, Lopez MF, Becker HC, McCool BA, and Jones SR (2016). Supersensitive kappa opioid receptors promotes ethanol withdrawal-related behaviors and reduce dopamine signaling in the nucleus accumbens. Int. J. Neuropsychopharmacol 19, pyv127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sacks JJ, Gonzales KR, Bouchery EE, Tomedi LE, and Brewer RD (2015). 2010 national and state costs of excessive alcohol consumption. Am. J. Prev. Med 49, e73–e79. [DOI] [PubMed] [Google Scholar]
- Salling MC, and Harrison NL (2014). Strychnine-sensitive glycine receptors on pyramidal neurons in layers II/III of the mouse prefrontal cortex are tonically activated. J. Neurophysiol 112, 1169–1178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Samson HH, Tolliver GA, Haraguchi M, and Hodge CW (1992). Alcohol self-administration: role of mesolimbic dopamine. Ann. N Y Acad. Sci 654, 242–253. [DOI] [PubMed] [Google Scholar]
- Sauguet L, Howard RJ, Malherbe L, Lee US, Corringer PJ, Harris RA, and Delarue M (2013). Structural basis for potentiation by alcohols and anaesthetics in a ligand-gated ion channel. Nat. Commun 4, 1697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schechter MD (1980). Ability of 3-carboxysalsolinol to produce ethanol-like discrimination in rats. Psychopharmacology (Berl.) 68, 277–281. [DOI] [PubMed] [Google Scholar]
- Schilaty ND, Hedges DM, Jang EY, Folsom RJ, Yorgason JT, McIntosh JM, and Steffensen SC (2014). Acute ethanol inhibits dopamine release in the nucleus accumbens via α6 nicotinic acetylcholine receptors. J. Pharmacol. Exp. Ther 349, 559–567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schindler AG, Soden ME, Zweifel LS, and Clark JJ (2016). Reversal of alcohol-induced dysregulation in dopamine network dynamics may rescue maladaptive decision-making. J. Neurosci 36, 3698–3708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seif T, Chang SJ, Simms JA, Gibb SL, Dadgar J, Chen BT, Harvey BK, Ron D, Messing RO, Bonci A, and Hopf FW (2013). Cortical activation of accumbens hyperpolarization-active NMDARs mediates aversion-resistant alcohol intake. Nat. Neurosci 16, 1094–1100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siciliano CA, Calipari ES, Cuzon Carlson VC, Helms CM, Lovinger DM, Grant KA, and Jones SR (2015). Voluntary ethanol intake predicts κ-opioid receptor supersensitivity and regionally distinct dopaminergic adaptations in macaques. J. Neurosci 35, 5959–5968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siggins GR, Roberto M, and Nie Z (2005). The tipsy terminal: presynaptic effects of ethanol. Pharmacol. Ther 107, 80–98. [DOI] [PubMed] [Google Scholar]
- Silberman Y, Fetterly TL, Awad EK, Milano EJ, Usdin TB, and Winder DG (2015). Ethanol produces corticotropin-releasing factor receptor-dependent enhancement of spontaneous glutamatergic transmission in the mouse central amygdala. Alcohol. Clin. Exp. Res 39, 2154–2162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silvestre de Ferron B, Bennouar KE, Kervern M, Alaux-Cantin S, Robert A, Rabiant K, Antol J, Naassila M, and Pierrefiche O (2015). Two binges of ethanol a day keep the memory away in adolescent rats: key role for GLUN2B subunit. Int. J. Neuropsychopharmacol 19, pyv087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smothers CT, and Woodward JJ (2006). Effects of amino acid substitutions in transmembrane domains of the NR1 subunit on the ethanol inhibition of recombinant N-methyl-D-aspartate receptors. Alcohol. Clin. Exp. Res 30, 523–530. [DOI] [PubMed] [Google Scholar]
- Smothers CT, and Woodward JJ (2016). Differential effects of TM4 tryptophan mutations on inhibition of N-methyl-d-aspartate receptors by ethanol and toluene. Alcohol 56, 15–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smothers CT, Jin C, and Woodward JJ (2013). Deletion of the N-terminal domain alters the ethanol inhibition of N-methyl-D-aspartate receptors in a subunit-dependent manner. Alcohol. Clin. Exp. Res 37, 1882–1890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Söderpalm B, Lidö HH, and Ericson M (2017). The glycine receptor: a functionally important primary brain target of ethanol. Alcohol. Clin. Exp. Res 41, 1816–1830. [DOI] [PubMed] [Google Scholar]
- Spanagel R (2009). Alcoholism: a systems approach from molecular physiology to addictive behavior. Physiol. Rev 89, 649–705. [DOI] [PubMed] [Google Scholar]
- Stobbs SH, Ohran AJ, Lassen MB, Allison DW, Brown JE, and Steffensen SC (2004). Ethanol suppression of ventral tegmental area GABA neuron electrical transmission involves N-methyl-D-aspartate receptors. J. Pharmacol. Exp. Ther 311, 282–289. [DOI] [PubMed] [Google Scholar]
- Swartzwelder HS, Wilson WA, and Tayyeb MI (1995). Age-dependent inhibition of long-term potentiation by ethanol in immature versus mature hippocampus. Alcohol. Clin. Exp. Res 19, 1480–1485. [DOI] [PubMed] [Google Scholar]
- Talani G, and Lovinger DM (2015). Interactions between ethanol and the endocannabinoid system at GABAergic synapses on basolateral amygdala principal neurons. Alcohol 49, 781–794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tateno T, and Robinson HP (2011). The mechanism of ethanol action on midbrain dopaminergic neuron firing: a dynamic-clamp study of the role of I(h) and GABAergic synaptic integration. J. Neurophysiol 106, 1901–1922. [DOI] [PubMed] [Google Scholar]
- Theile JW, Morikawa H, Gonzales RA, and Morrisett RA (2009). Role of 5-hydroxytryptamine2C receptors in Ca2+-dependent ethanol potentiation of GABA release onto ventral tegmental area dopamine neurons. J. Pharmacol. Exp. Ther 329, 625–633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Theile JW, Morikawa H, Gonzales RA, and Morrisett RA (2011). GABAergic transmission modulates ethanol excitation of ventral tegmental area dopamine neurons. Neuroscience 172, 94–103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thinschmidt JS, Walker DW, and King MA (2003). Chronic ethanol treatment reduces the magnitude of hippocampal LTD in the adult rat. Synapse 48, 189–197. [DOI] [PubMed] [Google Scholar]
- Tipps ME, Raybuck JD, Kozell LB, Lattal KM, and Buck KJ (2016). G protein-gated inwardly rectifying potassium channel subunit 3 knock-out mice show enhanced ethanol reward. Alcohol. Clin. Exp. Res 40, 857–864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tokuda K, Izumi Y, and Zorumski CF (2013). Locally-generated acetaldehyde contributes to the effects of ethanol on neurosteroids and LTP in the hippocampus. Neurol. Clin. Neurosci 1, 138–147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Treistman SN, and Martin GE (2009). BK Channels: mediators and models for alcohol tolerance. Trends Neurosci 32, 629–637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tremwel MF, Hunter BE, and Peris J (1994). Chronic ethanol exposure enhances [3H]GABA release and does not affect GABAA receptor mediated 36Cl uptake. Synapse 17, 149–154. [DOI] [PubMed] [Google Scholar]
- Trudell JR, Messing RO, Mayfield J, and Harris RA (2014). Alcohol dependence: molecular and behavioral evidence. Trends Pharmacol. Sci 35, 317–323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services (HHS) (2016). Facing addiction in America: the surgeon general’s report on alcohol, drugs, and health. Office of the Surgeon General, November, 2016. https://addiction.surgeongeneral.gov. [PubMed] [Google Scholar]
- Valenzuela CF, and Jotty K (2015). Mini-Review: effects of ethanol on gabaa receptor-mediated neurotransmission in the cerebellar cortex-recent advances. Cerebellum 14, 438–446. [DOI] [PubMed] [Google Scholar]
- Velázquez-Marrero C, Seale GE, Treistman SN, and Martin GE (2014). Large conductance voltage- and Ca2+-gated potassium (BK) channel β4 subunit influences sensitivity and tolerance to alcohol by altering its response to kinases. J. Biol. Chem 289, 29261–29272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Velázquez-Marrero C, Burgos A, García JO, Palacio S, Marrero HG, Bernardo A, Pérez-Laspiur J, Rivera-Oliver M, Seale G, and Treistman SN (2016). Alcohol regulates BK surface expression via Wnt/β-catenin signaling. J. Neurosci 36, 10625–10639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Volkow ND, Wang GJ, Maynard L, Fowler JS, Jayne B, Telang F, Logan J, Ding YS, Gatley SJ, Hitzemann R, et al. (2002). Effects of alcohol detoxification on dopamine D2 receptors in alcoholics: a preliminary study. Psychiatry Res. 116, 163–172. [DOI] [PubMed] [Google Scholar]
- Volkow ND, Wiers CE, Shokri-Kojori E, Tomasi D, Wang GJ, and Baler R (2017). Neurochemical and metabolic effects of acute and chronic alcohol in the human brain: studies with positron emission tomography. Neuropharmacology 122, 175–188. [DOI] [PubMed] [Google Scholar]
- Wanat MJ, Sparta DR, Hopf FW, Bowers MS, Melis M, and Bonci A (2009). Strain specific synaptic modifications on ventral tegmental area dopamine neurons after ethanol exposure. Biol. Psychiatry 65, 646–653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang J, Ben Hamida S, Darcq E, Zhu W, Gibb SL, Lanfranco MF, Carnicella S, and Ron D (2012). Ethanol-mediated facilitation of AMPA receptor function in the dorsomedial striatum: implications for alcohol drinking behavior. J. Neurosci 32, 15124–15132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang J, Cheng Y, Wang X, Roltsch Hellard E, Ma T, Gil H, Ben Hamida S, and Ron D (2015). Alcohol elicits functional and structural plasticity selectively in dopamine D1 receptor-expressing neurons of the dorsomedial striatum. J. Neurosci 35, 11634–11643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiner JL, Gu C, and Dunwiddie TV (1997). Differential ethanol sensitivity of subpopulations of GABAA synapses onto rat hippocampal CA1 pyramidal neurons. J. Neurophysiol 77, 1306–1312. [DOI] [PubMed] [Google Scholar]
- Weitlauf C, and Woodward JJ (2008). Ethanol selectively attenuates NMDAR-mediated synaptic transmission in the prefrontal cortex. Alcohol. Clin. Exp. Res. 32, 690–698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- White AM (2003). What happened? Alcohol, memory blackouts, and the brain. Alcohol Res. Health 27, 186–196. [PMC free article] [PubMed] [Google Scholar]
- WHO (2014). Global Status Report on Alcohol and Health, 2014 (World Health Organization; ). [Google Scholar]
- Wilcox MV, Cuzon Carlson VC, Sherazee N, Sprow GM, Bock R, Thiele TE, Lovinger DM, and Alvarez VA (2014). Repeated binge-like ethanol drinking alters ethanol drinking patterns and depresses striatal GABAergic transmission. Neuropsychopharmacology 39, 579–594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wills TA, Baucum AJ 2nd, Holleran KM, Chen Y, Pasek JG, Delpire E, Tabb DL, Colbran RJ, and Winder DG (2017). Chronic intermittent alcohol disrupts the GluN2B-associated proteome and specifically regulates group I mGlu receptor-dependent long-term depression. Addict. Biol 22, 275–290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson CJ (2007). GABAergic inhibition in the neostriatum. Prog. Brain Res 760, 91–110. [DOI] [PubMed] [Google Scholar]
- Xia JX, Li J, Zhou R, Zhang XH, Ge YB, and Ru Yuan X (2006). Alterations of rat corticostriatal synaptic plasticity after chronic ethanol exposure and withdrawal. Alcohol. Clin. Exp. Res 30, 819–824. [DOI] [PubMed] [Google Scholar]
- Xiao C, and Ye JH (2008). Ethanol dually modulates GABAergic synaptic transmission onto dopaminergic neurons in ventral tegmental area: role of mu-opioid receptors. Neuroscience 153, 240–248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiao C, Zhang J, Krnjević K, and Ye JH (2007). Effects of ethanol on midbrain neurons: role of opioid receptors. Alcohol. Clin. Exp. Res 31, 1106–1113. [DOI] [PubMed] [Google Scholar]
- Xiao C, Shao XM, Olive MF, Griffin WC 3rd, Li KY, Krnjević K, Zhou C, and Ye JH (2009). Ethanol facilitates glutamatergic transmission to dopamine neurons in the ventral tegmental area. Neuropsychopharmacology 34, 307–318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yamakura T, Lewohl JM, and Harris RA (2001). Differential effects of general anesthetics on G protein-coupled inwardly rectifying and other potassium channels. Anesthesiology 95, 144–153. [DOI] [PubMed] [Google Scholar]
- Yin HH, Park BS, Adermark L, and Lovinger DM (2007). Ethanol reverses the direction of long-term synaptic plasticity in the dorsomedial striatum. Eur. J. Neurosci 25, 3226–3232. [DOI] [PubMed] [Google Scholar]
- Yoshimoto K, McBride WJ, Lumeng L, and Li TK (1992). Alcohol stimulates the release of dopamine and serotonin in the nucleus accumbens. Alcohol 9, 17–22. [DOI] [PubMed] [Google Scholar]
- Yoshimura M, Pearson S, Kadota Y, and Gonzalez CE (2006). Identification of ethanol responsive domains of adenylyl cyclase. Alcohol. Clin. Exp. Res 30, 1824–1832. [DOI] [PubMed] [Google Scholar]
- Zapata A, and Shippenberg TS (2006). Endogenous kappa opioid receptor systems modulate the responsiveness of mesoaccumbal dopamine neurons to ethanol. Alcohol. Clin. Exp. Res 30, 592–597. [DOI] [PubMed] [Google Scholar]
- Zhang LH, Gong N, Fei D, Xu L, and Xu TL (2008). Glycine uptake regulates hippocampal network activity via glycine receptor-mediated tonic inhibition. Neuropsychopharmacology 33, 701–711. [DOI] [PubMed] [Google Scholar]
- Zhou Z, Karlsson C, Liang T, Xiong W, Kimura M, Tapocik JD, Yuan Q, Barbier E, Feng A, Flanigan M, et al. (2013). Loss of metabotropic glutamate receptor 2 escalates alcohol consumption. Proc. Natl. Acad. Sci. USA 110, 16963–16968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu PJ, and Lovinger DM (2006). Ethanol potentiates GABAergic synaptic transmission in a postsynaptic neuron/synaptic bouton preparation from basolateral amygdala. J. Neurophysiol 96, 433–441. [DOI] [PubMed] [Google Scholar]
- Zhu W, Bie B, and Pan ZZ (2007). Involvement of non-NMDA glutamate receptors in central amygdala in synaptic actions of ethanol and ethanol-induced reward behavior. J. Neurosci 27, 289–298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zorumski CF, Mennerick S, and Izumi Y (2014). Acute and chronic effects of ethanol on learning-related synaptic plasticity. Alcohol 48, 1–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.