Abstract
Objective
Perfluoroalkyl and polyfluoroalkyl substances (PFASs) are persistent pollutants and have endocrine disruptive and neurotoxic effects. The association between maternal PFAS concentrations and neuropsychological development in children is inconclusive. The present study aimed to examine the effect of maternal PFAS concentrations on neuropsychological development in 4-years-old children.
Methods
We used data from Shanghai-Minhang Birth Cohort, which recruited pregnant women at 12–16 gestational weeks. Among 981 women having PFAS measurement, 533 mother-child pairs were included in the study. A total of eight PFASs were measured, including perfluorooctane sulfonate (PFOS), perfluorooctanoic acid (PFOA), perfluorohexane sulfonate (PFHxS), perfluorononanoic acid (PFNA), perfluorodecanoic acid (PFDA), perfluoroundecanoic acid (PFUdA), perfluorododecanoic acid (PFDoA), and perfluorotridecanoic acid (PFTrDA). When infants turned 4 years old, mothers were asked to complete the Ages and Stages Questionnaires® (ASQ) to assess neuropsychological development of their children. Poisson regression model with robust variance estimates was used to examine the association between maternal PFAS concentrations and each developmental subscale of the ASQ.
Results
Prenatal plasma concentrations of most PFASs tended to be associated with increased risk of development problem in personal-social skills, including PFHxS, PFOS, PFOA, PFNA, PFDA, and PDUdA, and the associations for PFNA and PFDA were significant (per natural log unit increase: RRPFNA = 1.92, 95% CI: 1.21, 3.05; RR PFDA = 1.66, 95% CI: 1.17, 2.37). In stratified analyses by child’ sex, the consistent pattern of higher risk of developmental problems in personal-social skills associated with most PFASs was mainly observed among girls (RRPFOS = 2.56, 95% CI: 1.20, 5.45; RRPFOA = 9.00, 95% CI: 3.82, 21.21; RRPFNA = 3.11, 95% CI: 1.36, 7.13; RRPFDA = 2.20, 95% CI: 1.21, 4.00; RRPFUdA = 2.44, 95% CI: 1.14, 5.20; RRPFDoA = 1.62, 95% CI: 1.04, 2.54). Boys with higher maternal PFOA concentrations had a decreased risk of developmental problems in gross motor skills (RR = 0.47, 95% CI: 0.25, 0.89).
Conclusion
Prenatal plasma PFAS concentrations were associated with neuropsychological development in girls at 4 years of age, mainly in the subset of personal-social skills.
Electronic supplementary material
The online version of this article (10.1186/s12940-019-0493-3) contains supplementary material, which is available to authorized users.
Keywords: Perfluoroalkyl and polyfluoroalkyl substances, Neuropsychology, Age and stage questionnaire, Prenatal concentrations
Introduction
Perfluoroalkyl and polyfluoroalkyl substances (PFASs), a group of synthetic chemicals with hydrophobic (water-repelling) and oleophobic (oil-repelling) properties, have been extensively used in many consumer products, including oil, stain, grease, and water-repellent coatings on carpet, textiles, leather, and paper [1]. PFASs are bio-accumulative and have a long elimination half-life of 2–9 years [2]. Thus, they have been detected in wildlife and humans worldwide [3]. Concerns about the health/toxic effects of PFASs, particularly for in-utero exposure, have been raised for decades [4].
In animal studies, maternal PFAS exposure during pregnancy was associated with somatic growth, e.g., birth weight and size [5]. Moreover, maternal PFAS exposure can induce alteration in neuropsychological development of fetuses and neonates. Deranged spontaneous behavior was observed in adult mice following perfluorooctane sulfonate (PFOS) and perfluorooctanoic acid (PFOA) exposure during neonatal period, manifesting in hyperactivity and irreversibly reduced habituation [6]. In addition, maternal PFOS or PFOA exposure during pregnancy can lead to decreased motor function and delayed learning in rat offspring [7].
The associations between maternal PFAS exposure and neuropsychological development in children have also been examined in human studies, but the findings are inconsistent [8–11]. A prospective birth cohort study in Japan showed an association between prenatal PFOA exposure and mental developmental in girls aged 6 months, but not in those aged 18 months [12]. The biopersistent organochlorines in diet and human fertility (INUENDO) cohort study reported that prenatal exposure to PFOS and PFOA may have adverse effects on children’s neurobehavioral development, specifically in terms of hyperactive behavior [13]. However, in the Danish National Birth Cohort (DNBC) established between 1996 and 2002, maternal serum levels of PFOA and PFOS were not associated with behavioral and motor coordination problems in 7-year old children [10]. A nested case-control study from the DNBC suggested that prenatal PFAS exposure did not increase the risk of attention-deficit/hyperactivity disorder (ADHD) or autism in children [11]. In a 2005–2006 cohort study in the Mid-Ohio Valley, children in the highest quartile of maternal PFOA concentrations had higher intelligence quotient scores and decreased ADHD scores at ages 6–12 years compared with those in the lowest quartile [8].
Previous studies examining the associations between maternal PFAS exposure and child neurodevelopment focused on PFOS and PFOA. However, other commonly used PFAS compounds, such as perfluorohexane sulfonate (PFHxS), perfluorononanoic acid (PFNA), and perfluorodecanoic acid (PFDA), can be detected in more than 85% of individuals in China and in France [14, 15] and 50% of individuals in USA [16] and are less studied. Maternal concentrations of PFASs, including PFOS, PFOA PFHxS, PFNA, and PFDA, are much higher in the Shanghai area than in the United States, Europe and Asian countries [14]. In the present study, we used data from the Shanghai-Minhang Birth Cohort Study (S-MBCS) to examine associations between maternal concentrations of eight PFASs and the neurodevelopment of 4-year-old children assessed by the Ages and Stages Questionnaires, 3rd edition® (ASQ − 3).
Methods
Participants
The Shanghai-Minhang Birth Cohort was established between April and December 2012 [14, 17]. While attending routine antenatal examinations at the Maternal and Child Health Hospital of Minhang district in Shanghai, all pregnant women at 12–16 weeks of gestation was invited to participate in the study. Inclusion criteria included: being registered residents of Shanghai, having no history of chronic disease of the liver, kidney, or other organs, planning to deliver in this study hospital, and willingness to participate in specified interviews during pregnancy and after delivery.
In total, 1292 eligible pregnant women completed a structured questionnaire, among them, 981 provided a fasting blood sample at enrollment. Sixty-seven eligible pregnant women were excluded due to referral to other hospitals (n = 28), twin pregnancy (n = 8), and abortion or stillbirth (n = 31). The remaining 1225 women delivered singleton live births. Structured questionnaires were administered postnatally during home visits at 4 years of age to collect information on the child’s physical and neuropsychological development. ASQ-3 included in the structured questionnaire was used to identify children at a risk for neuropsychological developmental delay. We obtained complete ASQ-3 assessment data from 661 participants at 4 years of age. The present study included 533 mother-infant pairs who had measurements of prenatal PFAS concentration and child neuropsychological development at 4 years of age.
Exposure assessment
Maternal blood samples were collected at enrollment. After separating plasma from whole blood, the plasma samples were stored at − 80 °C until shipment using dry ice to the Center for Disease Control and Prevention in Hubei Province for quantitative analyses of 11 PFASs.
Eleven PFASs in each plasma sample were measured using high-performance liquid chromatography coupled with tandem mass spectrometry (Agilent Technologies Inc., USA). Detailed information on sample preparation, separation, quantification, quality control, and limit of detection (LOD) has been described previously [14]. The following eight PFASs with detection rates ≥90% were included in the present study for statistical analyses: PFHxS, PFOS, PFOA, PFNA, PFDA, perfluoroundecanoic acid (PFUdA), perfluorododecanoic acid (PFDoA), and perfluorotridecanoic acid (PFTrDA).
Assessment of children’s neuropsychological development
ASQ-3, contains 30 items designed to assess infant neuropsychological development in children aged 1–60 months. It covers five developmental subscales: communication, gross motor function, fine motor function, problem-solving ability, and personal-social skills [18]. A detailed description of Chinese translation, training, and process of validation of ASQ-3 has been described elsewhere [19]. The Simplified Chinese version of ASQ-3 has good internal consistency (Cronbach’s α = 0.80), high test-retest reliability (correlation coefficient = 0.8), and high validity (sensitivity = 87.50%, specificity = 84.48%) [19].
At home visits, parents or other caregivers were asked whether the child performs the described behavior based on three alternatives: “yes” (10 points), “sometimes” (5 points) and “not yet” (0 points). The score of each ASQ-3 subscale was highly skewed, with few children scoring lower than 2 standard deviations (SDs) below the standardized mean. Thus, the 10th percentile score of each subscale was used to identify children at a potential risk of developmental problem/delay, i.e., if scores on any subscale were less than or equal to the 10th percentile, the child was classified as having a developmental problem/delay. Additional file 1: Table S1 presents the rates of potential developmental problem assessed at 4 years of age in the study.
Covariates and potential confounders
Trained interviewers used a structured questionnaire at enrollment to collect information on maternal age, education, height, pre-pregnancy weight, parity, health status, per capita household income, and lifestyle. Body mass index (BMI) was calculated as body weight in kilograms divided by squared body height in meters. The information on child’s sex and gestational age was extracted from the study hospital’s medical records. Potential confounders were identified based on previous literature of potential determinants of early childhood development, available data in the present study, and results of bivariate analyses examining the relationship with neuropsychological problems (P < 0.20). Maternal age at enrollment (years), pre-pregnancy BMI (kg/m2), parity, per capita household income (< 4000, 4000–8000, and > 8000 CNY/month), passive smoker (yes/no), gestational age (weeks), and child’s sex (Boy/Girl) were included as covariates in the final model.
Statistical analysis
We first described and compared the demographic characteristics of included and excluded mother-infant pairs. The distributions of prenatal plasma concentrations of PFASs were presented by geometric means (GMs), SD, and percentiles. Risk ratios (RRs) and associated 95% confidence intervals (CIs) were estimated for the association between each PFAS and each developmental subscale of ASQ using Poisson regression analysis with robust variance estimates [20]. Prenatal PFAS concentrations were natural log (ln) transformed to approximate a normal distribution for regression analysis and were treated as continuous independent variables in all models. Values below the LOD were replaced with LOD/√2.
Considering that a previous study reported the sex-specific effect of PFASs on neurobehavioral problems [21], we introduced a cross product term for child’s sex with each individual PFAS to evaluate potential interaction effects. As several interaction items showed statistical significance (P < 0.10), we performed stratified analyses by child’s sex. PFAS concentrations were also categorized into tertiles according to its distribution in the subjects and were analyzed using Poisson regression. The lowest tertile was used as the reference group.
Additionally, we fit generalized additive models to investigate a potential nonlinear relationships between maternal PFAS concentration and neurobehavioral problems, and visually inspected plots of the smoothed data. Several associations between ln-transformed PFASs and children’s neuropsychological development showed nonlinear (Additional file 1: Figure S1-S5). In order to make our results comparable to other studies and considering that the aim of our study was inference rather than prediction, we still primarily presented the results of linear models (PFAS concentrations as continuous and categorical variables, respectively),
The Statistical Analysis System (SAS, version 9.3; SAS Institute, Inc., Cary, NC, USA) was used for statistical analysis. P values < 0.05 from two-tailed tests were considered statistically significant.
Results
Table 1 presents characteristics of mother-child pairs included and excluded in the study. The mean age of the included mothers at recruitment was 27.9 years, and 18.7 and 5.9% of them were underweight and overweight, respectively. Included parents tended to have high educational attainment, with 78.0% having college or above degrees. Among included mothers, the majority were nulliparous and had household income per capita > 4000 CNY/month, and over 40% of them were exposed to secondhand smoke during pregnancy, while only 0.87% of them reported alcohol consumption during pregnancy. About 18.6% of included mothers had depressive symptoms during pregnancy. The mean gestational weeks of included mothers at birth of children was 39.5 weeks and 55.7% of children were boys. The characteristics of excluded mother-pairs were comparable with those included, except that the proportion of nulliparous women was slightly higher among the included than those excluded (86.9% vs. 82.7%).
Table 1.
Characteristics of included and excluded mother-child pairs
| Characteristics | Included (N = 533) n (%) / Mean ± SD |
Excluded (N = 692) n (%) / Mean ± SD |
P-value of Student’s t-test or Chi-square test |
|---|---|---|---|
| Maternal age at enrollment (years) | |||
| Mean ± SD | 27.9 ± 3.4 | 27.8 ± 3.4 | 0.7451 |
| < 25 | 81 (15.2) | 103 (14.9) | 0.7900 |
| 25–30 | 299 (56.1) | 404 (58.4) | |
| ≥ 30 | 153 (28.7) | 185 (26.7) | |
| Maternal pre-pregnancy BMI (kg/m2) | |||
| Mean ± SD | 20.6 ± 2.4 | 20.4 ± 2.4 | 0.1905 |
| < 18.5 | 98 (18.7) | 146 (21.5) | 0.2112 |
| 18.5–24.9 | 395 (75.4) | 506 (74.4) | |
| ≥ 25 | 31 (5.9) | 28 (4.1) | |
| Maternal education | |||
| Blow high school | 41 (7.7) | 78 (11.3) | 0.1064 |
| High School | 76 (14.3) | 99 (14.3) | |
| College or above | 415 (78.0) | 514 (74.4) | |
| Paternal education | |||
| Blow high school | 28 (5.25) | 57 (8.28) | 0.9430 |
| High School | 76 (14.26) | 119 (17.3) | |
| College or above | 429 (80.49) | 512 (74.42) | |
| Per capita household income (CNY) | |||
| < 4000 | 113 (21.3) | 140 (20.6) | 0.0282 |
| 4000–8000 | 212 (40.0) | 277 (40.8) | |
| > 8000 | 205 (38.7) | 262 (38.6) | |
| Parity | |||
| Nulliparous | 459 (86.9) | 569 (82.7) | 0.0432 |
| Multiparous | 69 (13.1) | 119 (17.3) | |
| Maternal alcohol consumption during pregnancy | |||
| No | 454 (99.13) | 508 (98.64) | 0.4743 |
| Yes | 4 (0.87) | 7 (1.36) | |
| Maternal passive smoking before conception | |||
| No | 307 (57.8) | 420 (60.9) | 0.2811 |
| Yes | 224 (42.2) | 270 (39.1) | |
| Maternal prenatal depressive symptoms | |||
| No | 434 (81.43) | 551 (79.62) | 0.4309 |
| Yes | 99 (18.57) | 141 (20.38) | |
| Sex of child | |||
| Boy | 297 (55.7) | 370 (53.7) | 0.4816 |
| Girl | 236 (44.3) | 319 (46.3) | |
| Gestational age (weeks) | |||
| Mean ± SD | 39.5 ± 1.3 | 39.51 ± 1.5 | 0.6182 |
| < 37 | 19 (3.6) | 26 (3.8) | 0.8640 |
| ≥ 37 | 513 (96.4) | 666 (96.2) | |
Missing data: Included: pre-pregnancy BMI (n = 9), maternal education (n = 1), per capita household income (n = 3), parity (n = 5), maternal alcohol consumption during pregnancy (n = 75) and maternal passive smoking before conception (n = 2); Excluded: pre-pregnancy BMI (n = 12), maternal education (n = 1), paternal education (n = 4), per capita household income (n = 13), parity (n = 4), maternal alcohol consumption during pregnancy (n = 177), maternal passive smoking before conception (n = 2), and maternal prenatal depressive symptoms (n = 1)
PFHxS, PFOS, PFOA, PFNA, PFDA, PFUdA, and PFDoA were detected in all maternal plasma samples, while PFTrDA was detected in 90.6% of samples. PFOA had the highest exposure levels (GM = 20.0 ng/ml), followed by PFOS (GM = 10.8 ng/ml). The concentrations of PFHxS, PFDA, PFNA, and PFUdA were one order of magnitude lower than those of PFOA and PFOS, while those of PFDoA and PFTrDA were two orders of magnitude lower (Table 2). Prenatal PFAS concentrations were similarly distributed in girls and boys (Additional file 1: Table S2).
Table 2.
Maternal PFASs concentrations (ng/mL) at 12–16 gestational weeks (N = 533) in Shanghai, China
| PFAS | LOD | >LOD (N %) | GM (GSD) | Percentiles | ||||
|---|---|---|---|---|---|---|---|---|
| 5th | 25th | 50th | 75th | 95th | ||||
| PFHxS | 0.015 | 533 (100) | 2.7 (1.6) | 1.4 | 2.1 | 2.8 | 3.5 | 5.7 |
| PFOS | 0.02 | 533 (100) | 10.8 (1.8) | 4.5 | 7.6 | 10.8 | 15.8 | 25.2 |
| PFOA | 0.01 | 533 (100) | 20.0 (1.6) | 9.3 | 15.3 | 19.9 | 27.4 | 38.9 |
| PFNA | 0.02 | 533 (100) | 1.8 (1.6) | 0.8 | 1.3 | 1.8 | 2.5 | 3.9 |
| PFDA | 0.01 | 533 (100) | 2.1 (1.9) | 0.7 | 1.4 | 2.1 | 3.2 | 6.3 |
| PFUdA | 0.01 | 533 (100) | 1.6 (1.9) | 0.5 | 1.0 | 1.6 | 2.5 | 4.4 |
| PFDoA | 0.015 | 533 (100) | 0.1 (2.9) | LOD | 0.1 | 0.1 | 0.2 | 0.4 |
| PFTrDA | 0.02 | 483 (90.6) | 0.1 (2.9) | LOD | 0.1 | 0.1 | 0.2 | 0.4 |
LOD Limit of detection, GM Geometric mean, GSD Geometric standard deviation
Table 3 and Fig. 1 present associations between maternal ln-transformed PFAS concentrations (as continuous variables) and children’s neurodevelopmental problems at 4 years of age. There was a pattern of higher risks of developmental problem in personal-social skills associated with higher prenatal plasma concentrations of PFHxS, PFOS, PFOA, PFNA, PFDA, and PDUdA, with significant associations for PFNA and PFDA (per natural log unit increase: RRPFNA = 1.92, 95% CI: 1.21, 3.05; RR PFDA = 1.66, 95% CI: 1.17, 2.37). Children with higher prenatal PFTrDA concentrations tended to have a slightly higher risk of developmental problem in communication, with borderline significance (RR = 1.16 for per natural log unit increase, 95% CI: 0.99, 1.36), but the association was not observed for other PFASs. No statistically significant association was observed between maternal PFAS concentrations and developmental problems in gross motor, fine motor, and problem solving skills.
Table 3.
Associations between maternal PFAS concentrations (ln-transformed) and neuropsychological problems of ASQ scales at 4 years of age in Poisson regression with robust variance estimates
| PFAS | Communication | Gross motor | Fine motor | Problem solving | Personal–social skills | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| CRR (95% CI) | ARR (95% CI) | CRR (95% CI) | ARR (95% CI) | CRR (95% CI) | ARR (95% CI) | CRR (95% CI) | ARR (95% CI) | CRR (95% CI) | ARR (95% CI) | |
| PFHxS | 1.15 (0.84, 1.58) | 1.10 (0.78, 1.54) | 1.07 (0.56, 2.03) | 1.00 (0.53, 1.88) | 0.80 (0.44, 1.49) | 0.79 (0.45, 1.37) | 0.88 (0.57, 1.35) | 0.85 (0.54, 1.36) | 1.49 (0.82, 2.71) | 1.60 (0.92, 2.80)# |
| PFOS | 0.99 (0.76, 1.28) | 1.01 (0.77, 1.34) | 1.16 (0.76, 1.76) | 1.22 (0.79, 1.89) | 1.20 (0.82, 1.77) | 1.25 (0.79, 1.96) | 1.05 (0.76, 1.44) | 1.02 (0.71, 1.47) | 1.23 (0.83, 1.82) | 1.34 (0.91, 1.96) |
| PFOA | 0.83 (0.59, 1.15) | 0.84 (0.59, 1.19) | 0.85 (0.46, 1.55) | 0.86 (0.47, 1.58) | 0.93 (0.51, 1.70) | 0.99 (0.53, 1.84) | 1.22 (0.73, 2.03) | 1.26 (0.73, 2.15) | 1.43 (0.77, 2.64) | 1.67 (0.89, 3.14) |
| PFNA | 0.83 (0.61, 1.13) | 0.85 (0.61, 1.17) | 1.03 (0.62, 1.72) | 1.07 (0.63, 1.82) | 0.97 (0.55, 1.70) | 1.04 (0.58, 1.86) | 0.94 (0.63, 1.38) | 0.92 (0.60, 1.39) | 1.50 (0.93, 2.40) | 1.92 (1.21, 3.05)* |
| PFDA | 0.97 (0.77, 1.21) | 0.99 (0.78, 1.26) | 1.17 (0.78, 1.74) | 1.18 (0.78, 1.78) | 1.03 (0.72, 1.47) | 1.08 (0.72, 1.62) | 1.05 (0.77, 1.45) | 1.00 (0.71, 1.43) | 1.42 (1.00, 2.01)* | 1.66 (1.17, 2.37)* |
| PFUdA | 0.96 (0.77, 1.18) | 0.97 (0.77, 1.21) | 1.07 (0.71, 1.60) | 1.06 (0.70, 1.60) | 0.92 (0.61, 1.39) | 0.94 (0.61, 1.44) | 1.00 (0.73, 1.36) | 0.97 (0.70, 1.36) | 1.28 (0.89, 1.82) | 1.44 (0.99, 2.09) |
| PFDoA | 1.04 (0.91, 1.2) | 1.08 (0.93, 1.25) | 1.09 (0.85, 1.41) | 1.07 (0.83, 1.38) | 0.88 (0.70, 1.11) | 0.89 (0.71, 1.13) | 1.11 (0.90, 1.37) | 1.08 (0.87, 1.34) | 1.15 (0.92, 1.43) | 1.17 (0.93, 1.47) |
| PFTrDA | 1.10 (0.95, 1.27) | 1.16 (0.99, 1.36)# | 1.13 (0.91, 1.41) | 1.13 (0.89, 1.43) | 1.03 (0.82, 1.29) | 1.05 (0.81, 1.36) | 0.89 (0.74, 1.08) | 0.89 (0.73, 1.10) | 1.07 (0.86, 1.35) | 1.11 (0.88, 1.38) |
Models were adjusted for maternal age at enrollment (age), pre-pregnancy BMI (kg/m2), maternal education, paternal education, parity, per capita household income (< 4000, 4000–8000, and > 8000 CNY), maternal passive smoking (yes or no), maternal prenatal depressive symptoms (yes or no), gestational age (weeks), and child’s sex
CRR Crude risk ratio, ARR Adjusted risk ratio, CI Confidence interval
# Marginally significant differences (0.05 < p < 0.10)
* Statistically significant differences (p < 0.05)
Fig. 1.
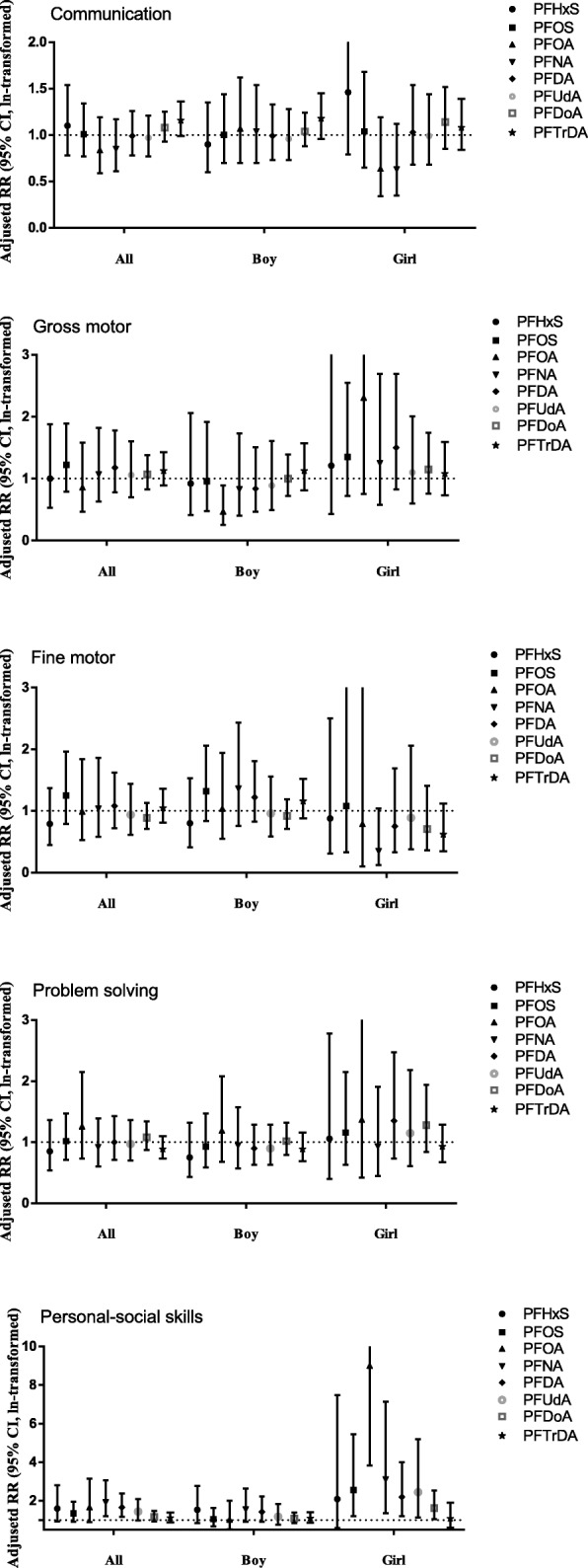
Associations between maternal PFAS concentrations (ln-transformed) and neuropsychological problems of ASQ scales at 4 years of age in Poisson regression with robust variance estimates
When evaluating the potential effect modifications by child’s sex, some interaction items of maternal PFAS concentrations and child’s sex were statistically significant (p < 0.10) in the models examining PFOA and gross motor, PFNA and fine motor, and PFOS/PFOA and personal-social skills (Additional file 1: Table S3). The consistent pattern of higher risk of developmental problems in personal-social skills associated with most PFASs shown in Table 3 was mainly observed among girls (Table 4). Among these associations, those for PFOS, PFOA, PFNA, PFDA, PFUdA, and PFDoA concentrations were statistically significant (per natural log unit increase of PFAS concentrations: RRPFOS = 2.56, 95% CI: 1.20, 5.45; RRPFOA = 9.00, 95% CI: 3.82, 21.21; RRPFNA = 3.11, 95% CI: 1.36, 7.13; RRPFDA = 2.20, 95% CI: 1.21, 4.00; RRPFUdA = 2.44, 95% CI: 1.14, 5.20; RRPFDoA = 1.62, 95% CI: 1.04, 2.54). There were no significant associations between PFAS concentrations and problems in other subscales in girls (Table 4). No clear association between PFAS concentrations and problems in each subscale was observed in boys (Table 4). Only boys with higher prenatal PFOA concentrations had a decreased risk of developmental problems in gross motor skills (per natural log unit increase: RR = 0.47, 95% CI: 0.25, 0.89) (Table 4).
Table 4.
Associations between maternal PFAS concentrations (ln-transformed) and neuropsychological problems of ASQ scales at 4 years of age among boys and girls in Poisson regression with robust variance estimates
| PFAS | Communication ARR (95% CI) | Gross motor ARR (95% CI) | Fine motor ARR (95% CI) | Problem solving ARR (95% CI) | Personal–social skills ARR (95% CI) | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| Girl (N = 236) | Boy (N = 297) | Girl (N = 236) | Boy (N = 297) | Girl (N = 236) | Boy (N = 297) | Girl (N = 236) | Boy (N = 297) | Girl (N = 236) | Boy (N = 297) | |
| PFHxS | 1.46 (0.79, 2.70) | 0.90 (0.60, 1.35) | 1.21 (0.43, 3.41) | 0.92 (0.41, 2.06) | 0.88 (0.31, 2.50) | 0.80 (0.41, 1.53) | 1.06 (0.40, 2.78) | 0.75 (0.43, 1.32) | 2.09 (0.58, 7.49) | 1.53 (0.84, 2.78) |
| PFOS | 1.04 (0.65, 1.68) | 1.00 (0.70, 1.44) | 1.35 (0.72, 2.55) | 0.96 (0.48, 1.92) | 1.08 (0.33, 3.59) | 1.32 (0.84, 2.06) | 1.16 (0.63, 2.15) | 0.93 (0.59, 1.47) | 2.56 (1.20, 5.45)* | 1.05 (0.67, 1.64) |
| PFOA | 0.64 (0.34, 1.19) | 1.07 (0.70, 1.62) | 2.31 (0.75, 7.10) | 0.47 (0.25, 0.89)* | 0.79 (0.10, 6.29) | 1.04 (0.55, 1.94) | 1.37 (0.42, 4.47) | 1.19 (0.68, 2.08) | 9.00 (3.82, 21.21)*a | 1.03 (0.53, 2.01) |
| PFNA | 0.63 (0.35, 1.12) | 1.04 (0.70, 1.54) | 1.25 (0.58, 2.69) | 0.83 (0.40, 1.73) | 0.35 (0.12, 1.04) | 1.36 (0.76, 2.43) | 0.93 (0.45, 1.91) | 0.95 (0.57, 1.57) | 3.11 (1.36, 7.13)* | 1.55 (0.91, 2.64) |
| PFDA | 1.03 (0.68, 1.54) | 0.99 (0.73, 1.33) | 1.50 (0.83, 2.69) | 0.84 (0.47, 1.51) | 0.75 (0.33, 1.69) | 1.22 (0.83, 1.81) | 1.35 (0.73, 2.47) | 0.84 (0.55, 1.27) | 2.20 (1.21, 4.00)* | 1.42 (0.91, 2.22) |
| PFUdA | 0.99 (0.68, 1.44) | 0.96 (0.73, 1.28) | 1.10 (0.60, 2.01) | 0.89 (0.49, 1.61) | 0.89 (0.38, 2.06) | 0.96 (0.59, 1.56) | 1.15 (0.61, 2.18) | 0.90 (0.63, 1.29) | 2.44 (1.14, 5.20)* | 1.18 (0.75, 1.84) |
| PFDoA | 1.14 (0.85, 1.52) | 1.04 (0.88, 1.24) | 1.15 (0.76, 1.74) | 1.00 (0.72, 1.39) | 0.71 (0.36, 1.41) | 0.92 (0.71, 1.19) | 1.28 (0.84, 1.94) | 1.02 (0.79, 1.32) | 1.62 (1.04, 2.54) * | 1.08 (0.84, 1.38) |
| PFTrDA | 1.08 (0.84, 1.39) | 1.18 (0.96, 1.45) | 1.08 (0.73, 1.59) | 1.13 (0.81, 1.57) | 0.62 (0.35, 1.12) | 1.16 (0.88, 1.52) | 0.93 (0.67, 1.29) | 0.89 (0.69, 1.16) | 1.08 (0.61, 1.90) | 1.10 (0.86, 1.41) |
Models were adjusted for maternal age at enrollment (ages), pre-pregnancy BMI (kg/m2), maternal education, paternal education, parity, per capita household income (< 4000, 4000–8000, and > 8000 CNY), maternal passive smoking (yes or no), maternal prenatal depressive symptoms (yes or no), and gestational age (weeks)
aThe strong association may be caused by statistical imprecision mainly due to the imbalanced distribution of numbers of children having potential problems by PFOA concentrations. As shown in Table 5, there was no cases in the lowest tertile group of PFOA concentrations among girls, which potentially influenced the estimation in Poisson regression model
ARR Adjusted risk ratio, CI Confidence interval
* Statistically significant differences (p < 0.05)
We further examined the associations between maternal PFAS concentration as categorical variables and developmental problems by child’s sex (Table 5). Generally, the models using categorized PFAS variables showed similar results as reported in the main analyses. In girls, there was a consistent pattern of increased risk of problems in personal-social skills associated with higher maternal PFAS concentrations except PFTrDA, although the estimates became imprecise. For PFOA, the regression model did not converge because there was no child with developmental problem in the lowest tertile group. A linear trend was observed between tertiles of PFOS, PFNA, PFDA, and PFDoA and problems in the subscale (P for trend =0.0027, 0.0417, 0.0110, and 0.0159, respectively, Table 5). In addition, prenatal PFNA concentrations were associated with a decreased risk of communication problems; adjusted RRs were 0.73 (95%CI: 0.41, 1.32) for the middle tertile and 0.50 (95% CI: 0.26, 0.94) for the highest tertile (P for trend =0.0292). There were no clear associations between maternal PFAS concentrations and problems in each subscale among boys. However, boys with higher maternal PFTrDA concentrations were more likely to have communication problem; the adjusted RRs was 1.53 (95%CI: 0.92, 2.55) for middle tertile and 1.83 (95%CI: 1.08, 3.12) for the highest tertile (P for trend = 0.0218). Boys in the middle tertile of maternal PFUdA concentrations had more problems in fine motor scale (RR = 2.19, 95%CI: 1.16, 4.17) (Table 5).
Table 5.
Associations between maternal PFAS concentrations (divided by tertiles) and neuropsychological problems of ASQ scales at 4 years of age among boys and girls in Poisson regression with robust variance estimates
| PFAS | Communication ARR (95% CI) | Gross motor ARR (95% CI) | Fine motor ARR (95% CI) | Problem solving ARR (95% CI) | Personal–social skills ARR (95% CI) | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| Girl (N = 236) | Boy (N = 297) | Girl (N = 236) | Boy (N = 297) | Girl (N = 236) | Boy (N = 297) | Girl (N = 236) | Boy (N = 297) | Girl (N = 236) | Boy (N = 297) | |
| PFHxS | ||||||||||
| Low tertile | Ref | Ref | Ref | Ref | Ref | Ref | Ref | Ref | Ref | Ref☆ |
| Middle tertile | 0.99 (0.53, 1.83) | 0.64 (0.39, 1.05) | 1.55 (0.68, 3.55) | 0.76 (0.35, 1.67) | 1.46 (0.35, 6.10) | 0.55 (0.27, 1.13) | 0.81 (0.35, 1.89) | 0.85 (0.44, 1.64) | 1.62 (0.43, 6.08) | 0.68 (0.30, 1.55) |
| High tertile | 1.24 (0.65, 2.36) | 0.90 (0.59, 1.36) | 1.43 (0.55, 3.68) | 0.57 (0.26, 1.24) | 0.50 (0.05, 5.00) | 0.73 (0.40, 1.36) | 1.24 (0.48, 3.21) | 0.61 (0.32, 1.18) | 2.56 (0.73, 9.03) | 1.77 (0.94, 3.34) |
| PFOS | ||||||||||
| Low tertile | Ref | Ref | Ref | Ref | Ref | Ref | Ref | Ref | Ref☆ | Ref |
| Middle tertile | 0.52 (0.26, 1.04)# | 1.16 (0.76, 1.77) | 0.81 (0.27, 2.43) | 0.94 (0.43, 2.07) | 0.79 (0.13, 4.91) | 1.87 (0.92, 3.80)# | 0.55 (0.15, 2.07) | 1.21 (0.65, 2.28) | 0.32 (0.04, 2.77) | 1.47 (0.76, 2.84) |
| High tertile | 1.10 (0.63, 1.92) | 0.89 (0.53, 1.51) | 1.61 (0.62, 4.16) | 0.91 (0.37, 2.24) | 1.98 (0.34, 11.53) | 1.19 (0.52, 2.71) | 2.00 (0.77, 5.17) | 0.66 (0.29, 1.48) | 2.97 (0.90, 9.84)# | 1.18 (0.57, 2.44) |
| PFOA | ||||||||||
| Low tertile | Ref☆ | Ref | Ref | Ref☆ | Ref | Ref | Ref | Ref | Ref | Ref |
| Middle tertile | 0.86 (0.49, 1.50) | 1.02 (0.65, 1.6) | 1.08 (0.33, 3.57) | 0.51 (0.23, 1.11)# | 0.50 (0.13, 1.93) | 0.88 (0.43, 1.80) | 0.93 (0.35, 2.46) | 1.09 (0.56, 2.12) | not converge | 1.60 (0.80, 3.19) |
| High tertile | 0.55 (0.28, 1.10)# | 0.96 (0.61, 1.52) | 1.90 (0.66, 5.44) | 0.45 (0.19, 1.04)# | 1.32 (0.29, 5.93) | 0.91 (0.47, 1.78) | 0.90 (0.36, 2.26) | 1.10 (0.58, 2.06) | not converge | 1.50 (0.77, 2.93) |
| PFNA | ||||||||||
| Low tertile | Ref★ | Ref | Ref | Ref | Ref | Ref | Ref | Ref | Ref★ | Ref |
| Middle tertile | 0.73 (0.41, 1.32) | 1.19 (0.76, 1.88) | 0.96 (0.29, 3.20) | 0.91 (0.39, 2.08) | 1.15 (0.25, 5.24) | 1.72 (0.82, 3.62) | 0.56 (0.20, 1.55) | 1.24 (0.64, 2.43) | 2.87 (0.37, 22.20) | 1.23 (0.62, 2.47) |
| High tertile | 0.50 (0.26, 0.94)* | 1.17 (0.72, 1.91) | 1.50 (0.54, 4.21) | 1.06 (0.48, 2.35) | 0.46 (0.10, 2.11) | 1.72 (0.82, 3.59) | 0.93 (0.4, 2.17) | 1.08 (0.52, 2.25) | 5.68 (0.82, 39.34) | 1.70 (0.86, 3.36) |
| PFDA | ||||||||||
| Low tertile | Ref | Ref | Ref | Ref | Ref | Ref | Ref | Ref | Ref★ | Ref |
| Middle tertile | 0.61 (0.31, 1.20) | 1.01 (0.66, 1.55) | 1.16 (0.36, 3.71) | 0.87 (0.42, 1.81) | 2.04 (0.43, 9.66) | 1.65 (0.87, 3.13) | 0.50 (0.14, 1.74) | 1.27 (0.69, 2.33) | 2.16 (0.26, 17.69) | 1.14 (0.57, 2.28) |
| High tertile | 1.02 (0.54, 1.91) | 0.88 (0.55, 1.42) | 1.83 (0.62, 5.39) | 0.53 (0.21, 1.32) | 0.40 (0.03, 4.74) | 0.80 (0.37, 1.76) | 1.71 (0.70, 4.15) | 0.65 (0.31, 1.36) | 8.68 (1.41, 53.43)* | 1.52 (0.74, 3.09) |
| PFUdA | ||||||||||
| Low tertile | Ref | Ref | Ref | Ref | Ref | Ref | Ref | Ref | Ref☆ | Ref |
| Middle tertile | 0.64 (0.32, 1.25) | 1.18 (0.78, 1.80) | 0.44 (0.12, 1.53) | 1.14 (0.54, 2.43) | 2.10 (0.43, 10.41) | 2.19 (1.16, 4.17)* | 0.27 (0.05, 1.33) | 1.57 (0.81, 3.03) | 0.79 (0.11, 5.56) | 1.77 (0.90, 3.47)# |
| High tertile | 0.93 (0.52, 1.66) | 0.83 (0.50, 1.38) | 1.29 (0.53, 3.16) | 0.77 (0.31, 1.92) | 1.35 (0.18, 10.02) | 0.64 (0.26, 1.56) | 1.35 (0.62, 2.94) | 0.88 (0.40, 1.90) | 3.72 (0.79, 17.62)# | 1.12 (0.48, 2.63) |
| PFDoA | ||||||||||
| Low tertile | Ref | Ref | Ref | Ref | Ref | Ref | Ref | Ref | Ref★ | Ref |
| Middle tertile | 0.78 (0.38, 1.58) | 1.29 (0.82, 2.04) | 0.81 (0.27, 2.38) | 0.88 (0.41, 1.91) | 0.48 (0.11, 2.06) | 1.34 (0.70, 2.56) | 1.25 (0.35, 4.41) | 1.06 (0.54, 2.06) | 3.99 (0.46, 34.3) | 0.91 (0.47, 1.77) |
| High tertile | 1.33 (0.72, 2.46) | 1.14 (0.72, 1.82) | 1.27 (0.51, 3.19) | 0.93 (0.41, 2.09) | 0.40 (0.07, 2.37) | 0.84 (0.41, 1.75) | 1.78 (0.61, 5.23) | 1.13 (0.58, 2.18) | 6.89 (0.97, 48.67)# | 0.91 (0.46, 1.79) |
| PFTrDA | ||||||||||
| Low tertile | Ref | Ref’ | Ref | Ref | Ref | Ref | Ref | Ref | Ref | Ref |
| Middle tertile | 1.19 (0.60, 2.36) | 1.53 (0.92, 2.55) | 0.94 (0.33, 2.66) | 2.25 (0.82, 6.14) | 0.44 (0.10, 1.98) | 1.90 (0.86, 4.20) | 1.69 (0.64, 4.47) | 1.46 (0.75, 2.84) | 0.79 (0.21, 2.96) | 1.70 (0.85, 3.4) |
| High tertile | 1.36 (0.69, 2.69) | 1.83 (1.08, 3.12)* | 0.85 (0.31, 2.29) | 1.68 (0.56, 5.1) | 0.28 (0.05, 1.61) | 1.81 (0.78, 4.19) | 0.88 (0.31, 2.52) | 0.71 (0.29, 1.73) | 0.84 (0.23, 3.03) | 1.29 (0.61, 2.75) |
Models were adjusted for maternal age at enrollment (ages), pre-pregnancy BMI (kg/m2), maternal education, paternal education, parity, per capita household income (< 4000, 4000–8000, and > 8000 CNY), maternal passive smoking (yes or no), maternal prenatal depressive symptoms (yes or no), and gestational age (weeks)
ARR Adjusted risk ratio, CI Confidence interval
# Marginally significant differences (0.05 < p < 0.10)
* Statistically significant differences (p < 0.05)
★p-trend < 0.05
☆0.05 < p-trend < 0.10
Discussion
We found that girls with higher maternal concentrations of PFHxS, PFOS, PFOA, PFNA, PFDA, PFUdA, and PFDoA tended to have more problems in personal-social skills, while there was little evidence for consistent associations in boys.
In the study, median concentrations for maternal PFOS and PFOA were 10.8 and 19.9 ng/ml, respectively, which are one of the highest levels reported among pregnant women during the similar period (around 2012) compared to those of the studies conducted in the US (2.4 and 1.1 ng/ml) [16], Canada (4.6 and 1.7 ng/ml) [22], Denmark (8.23 and 2.0 ng/ml) [23], Australia (1.99 ad 0.86 ng/ml) [24], and Japan (3.52 and 1.27 ng/ml) [25], especially for PFOA. However, compared to the studies on prenatal PFAS concentrations and child’s neurodevelopment where the samples were collected mainly around 2000, PFOS concentrations were lower than most of the studies (ranged from 13.2 to 34.4 ng/ml) [10, 26] except the Hokkaido study in Japan [12, 27], while PFOA concentrations were much higher (ranged from 1.2 to 5.6 ng/ml in previous studies) [12, 28]. Different from other studies where PFOS has the highest concentrations, PFOA was the most predominant compound in the present study, which was also observed in another cohort study in Shanghai [29]. This may be explained by the findings that PFOA is the most prevalent compound in the surface water of Shanghai, accounting for 51–86% of total PFAS concentrations [30].
Results from epidemiological studies on neurodevelopmental impact of in utero PFAS exposure are inconsistent [10, 28, 31, 32]. A cohort study from Taiwan showed that prenatal exposure to PFOS might affect child neurodevelopment, especially gross motor development at 2 years of age [32]. Among 432 mother-daughter pairs from the Avon Longitudinal cohort, a 1 ng/mL increase in PFOS was associated with a 3.82-point (95% CI: − 6.18, − 1.47) lower vocabulary score at 15 months and a 0.80-point (95% CI: − 1.74, 0.14) lower language score at 38 months in daughters of mothers aged < 25 years [33]. A birth cohort study between 2002 and 2005 suggested an association between prenatal PFOA exposure and neurodevelopmental delay in 6-month-old females, as measured by mental scales of the second edition of the Bayley Scales of Infant Development [12]. In Oulhote et al.’s study, cross-sectional analyses at 7 years of age showed possible sex-dimorphic associations between PFAS concentrations and the Strengths and Difficulties Questionnaire (SDQ) scores; girls had consistently positive associations with SDQ scores, whereas boys exhibited a pattern of negative or null associations [9]. However, in a prospective study from the DNBC, maternal plasma levels of PFOA or PFOS were neither associated with mental developmental nor fine and gross motor developmental milestones in infants [28], and there was no association between PFAS concentration and behavioral and motor coordination problems at 7 years of age [10]. In a Norwegian birth cohort study, PFOA or PFOS measured in breast milk was not associated with child neuropsychological development assessed by ASQ at 12 and 24 months [31]. Moreover, behavioral development assessed by the Infant-Toddler Symptom Checklist (ITSC) found no consistent increase in behavioral problems at 12 and 24 months [31]. The inconsistent findings between the current study and previous studies may be due to differences in screening tools, children’s ages at assessment, and PFAS compounds measured and their concentrations [10, 28, 31].
The mechanism of the effect of PFASs on neurobehavioral development remains unclear. In animal studies, some PFASs may affect the cholinergic or dopaminergic system, resulting in altered responses to nicotine or imbalanced expression of the acetylcholine/dopamine phenotype [6]. PFASs also affect synaptogenesis and functional protein levels during neuron growth [34]. PFOA and PFOS significantly increased the levels of synaptophysin and tau in the cerebral cortex and hippocampus. Because these proteins are important for normal brain development, altered levels during a critical period of brain growth spurts could be one of the mechanisms of behavioral defects [34]. Other possible mechanisms include the endocrine-disrupting properties of PFASs in glucocorticoid, sex hormone [27] and thyroid hormone balance [35, 36]. Prenatal and postnatal exposure to PFASs interferes with thyroid hormone balance in humans, resulting in higher thyroid-stimulating hormone, decreased total/free triiodothyronine, and decreased total/free thyroxine levels [37–39], which may play a role in how PFASs affect human neurodevelopment.
Additionally, we found a consistent pattern of adverse effects on personal-social skills in girls but not in boys following prenatal PFAS exposure. Although chance findings may be incompletely excluded, mechanism investigations are warranted to understand the sex-specific association. In previous studies, prenatal PFOA exposure was associated with decreased Mental Developmental indices scores of female infants at 6 months of age [12], and PFOS exposure was associated with poorer metacognition scores only among school-aged girls [26]. These findings are in line with our results on personal-social skills which evaluate children’s abilities of self-helping and interacting with others. Human studies suggested that prenatal PFOA/PFOS exposure was significantly associated with testosterone/estradiol in male infants, progesterone levels, glucocorticoid levels, and DHEA levels in cord blood samples of both sexes [27, 40]. In addition, effects of PFAS exposure on thyroid hormone homeostasis may differ across sexes [41]. The hormonal effects of PFAS may differently affect the neurobehavioral development of males or females. However, whether the sex-specific difference is inherited due to sex or due to hormonal effects of PFAS exposure warrants further investigation.
One strength of our study is that the prospective design provides strong causality between PFAS exposure levels and child neurodevelopment. We measured two of the most frequently detected PFASs, PFOS and PFOA, as well as other PFAS compounds to provide a profile of the effects of commonly detected PFAS compounds. However, some potential limitations of the current study should be mentioned. First, there was considerable loss to follow-up for neurodevelopmental assessment during the study period, which increased the potential for selection bias. However, the characteristics of subjects in the original cohort were similar to those in the final sample in terms of maternal age, pre-pregnancy BMI, parity, and gestational age. Thus, the loss to follow-up was less likely to lead to substantial bias. Second, parental intelligence quotient (IQ) may affect the children’s ASQ score, however, the information about parental IQ has not been collected in the study. We adjusted for parental education in the models, which may partially control for the confounding effects of parental IQ. In addition, the relationship between PFASs and ASQ measures may have been confounded by postnatal environmental risk factors [42, 43]. The confounding effect of uncollected factors, e.g., child sleepiness and maternal self-regulation, cannot be adjusted for. Third, multiple comparisons may also be of concern because we examined the associations between eight PFASs and five subscales. However, for our main findings on the associations between PFAS concentrations and personal-social skills among girls, patterns were consistent across PFAS compounds, which were less likely to be due to chance alone.
Conclusions
Maternal PFAS concentrations during pregnancy were inversely associated with neuropsychological development assessed by ASQ in 4-year-old children. Further investigation of the underlying mechanism of the effect of prenatal PFAS exposure on neuropsychological development is needed.
Additional file
Table S1. The rates of potential developmental problem assessed at 4 years of age by the Age and Stage Questionnaire (ASQ). Table S2. Maternal PFASs concentrations (ng/mL) at 12–16 gestational weeks stratified by child sex. Table S3. P-values of interaction item (PFASs*child sex) in the associations between maternal PFASs concentrations and child’s neurobehavioral problems assessed by ASQ at 4 years of age*. Figure S1. Adjusted generalized additive model plots of ln-transformed PFAS concentrations with developmental problems in communication among offspring. Figure S2. Adjusted generalized additive model plots of ln-transformed PFAS concentrations with offspring developmental problems in Gross motor among offspring. Figure S3. Adjusted generalized additive model plots of ln-transformed PFAS concentrations with developmental problems in Fine motor among offspring. Figure S4. Adjusted generalized additive model plots of ln-transformed PFAS concentrations with developmental problems in Problem solving among offspring. Figure S5. Adjusted generalized additive model plots of ln-transformed PFAS concentrations with developmental problems in Personal-social skills among offspring. (DOCX 15944 kb)
Acknowledgements
This work was supported by grants from the National Key Research and Development Program of China (2018YFC1002801, 2016YFC1000505, 2017YFC1600500); the Science and Technology Commission of Shanghai Municipality (16ZR1430100); the National Natural Science Foundation of China (21628701); Shanghai municipal health commission (201840184); Health Commission of Zhejiang Province (2018KY812), Health Commission of Jiaxing City (2016BY58088, 2016A05), and Innovation-oriented Science and Technology Grant from NHC Key Laboratory of Reproduction Regulation (CX2017-06).
Authors’ contributions
WY, HL and MM conceived and designed the study. JN, YT and HL performed data analysis and drafted the article. WY, MM, YR, HX, XSu, HH, XSo, LY and SW revised the manuscript and critically discussed the results. All authors were involved in interpreting the data and approved the final article.
Funding
None.
Availability of data and materials
The datasets used in the current study are available from the corresponding authors on reasonable request.
Ethics approval and consent to participate
The study was approved by the ethical review committee of Shanghai Institute of Planned Parenthood Research (SIPPR). The study was conducted according to the Declaration of Helsinki. All mothers gave their written informed consent for themselves and their children before enrollment and at each follow-up.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Jinbo Niu and Hong Liang contributed equally to this work.
References
- 1.Post GB, Cohn PD, Cooper KR. Perfluorooctanoic acid (PFOA), an emerging drinking water contaminant: a critical review of recent literature. Environ Res. 2012;116:93–117. doi: 10.1016/j.envres.2012.03.007. [DOI] [PubMed] [Google Scholar]
- 2.Olsen GW, Burris JM, Ehresman DJ, Froehlich JW, Seacat AM, Butenhoff JL, Zobel LR. Half-life of serum elimination of perfluorooctanesulfonate, perfluorohexanesulfonate, and perfluorooctanoate in retired fluorochemical production workers. Environ Health Perspect. 2007;115(9):1298–1305. doi: 10.1289/ehp.10009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Houde M, Martin JW, Letcher RJ, Solomon KR, Muir DC. Biological monitoring of polyfluoroalkyl substances: a review. Environ Sci Technol. 2006;40(11):3463–3473. doi: 10.1021/es052580b. [DOI] [PubMed] [Google Scholar]
- 4.Lau C, Anitole K, Hodes C, Lai D, Pfahles-Hutchens A, Seed J. Perfluoroalkyl acids: a review of monitoring and toxicological findings. Toxicol Sci. 2007;99(2):366–394. doi: 10.1093/toxsci/kfm128. [DOI] [PubMed] [Google Scholar]
- 5.Apelberg BJ, Witter FR, Herbstman JB, Calafat AM, Halden RU, Needham LL, Goldman LR. Cord serum concentrations of perfluorooctane sulfonate (PFOS) and perfluorooctanoate (PFOA) in relation to weight and size at birth. Environ Health Perspect. 2007;115(11):1670–1676. doi: 10.1289/ehp.10334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Johansson N, Fredriksson A, Eriksson P. Neonatal exposure to perfluorooctane sulfonate (PFOS) and perfluorooctanoic acid (PFOA) causes neurobehavioural defects in adult mice. Neurotoxicology. 2008;29(1):160–169. doi: 10.1016/j.neuro.2007.10.008. [DOI] [PubMed] [Google Scholar]
- 7.Butenhoff JL, Ehresman DJ, Chang SC, Parker GA, Stump DG. Gestational and lactational exposure to potassium perfluorooctanesulfonate (K+PFOS) in rats: developmental neurotoxicity. Reprod Toxicol (Elmsford, NY) 2009;27(3–4):319–330. doi: 10.1016/j.reprotox.2008.12.010. [DOI] [PubMed] [Google Scholar]
- 8.Stein CR, Savitz DA, Bellinger DC. Perfluorooctanoate and neuropsychological outcomes in children. Epidemiology (Cambridge, Mass) 2013;24(4):590–599. doi: 10.1097/EDE.0b013e3182944432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Oulhote Y, Steuerwald U, Debes F, Weihe P, Grandjean P. Behavioral difficulties in 7-year old children in relation to developmental exposure to perfluorinated alkyl substances. Environ Int. 2016;97:237–245. doi: 10.1016/j.envint.2016.09.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fei C, Olsen J. Prenatal exposure to perfluorinated chemicals and behavioral or coordination problems at age 7 years. Environ Health Perspect. 2011;119(4):573–578. doi: 10.1289/ehp.1002026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Liew Z, Ritz B, von Ehrenstein OS, Bech BH, Nohr EA, Fei C, Bossi R, Henriksen TB, Bonefeld-Jorgensen EC, Olsen J. Attention deficit/hyperactivity disorder and childhood autism in association with prenatal exposure to perfluoroalkyl substances: a nested case-control study in the Danish National Birth Cohort. Environ Health Perspect. 2015;123(4):367–373. doi: 10.1289/ehp.1408412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Goudarzi H, Nakajima S, Ikeno T, Sasaki S, Kobayashi S, Miyashita C, Ito S, Araki A, Nakazawa H, Kishi R. Prenatal exposure to perfluorinated chemicals and neurodevelopment in early infancy: the Hokkaido study. Sci Total Environ. 2016;541:1002–1010. doi: 10.1016/j.scitotenv.2015.10.017. [DOI] [PubMed] [Google Scholar]
- 13.Hoyer BB, Ramlau-Hansen CH, Obel C, Pedersen HS, Hernik A, Ogniev V, Jonsson BA, Lindh CH, Rylander L, Rignell-Hydbom A, et al. Pregnancy serum concentrations of perfluorinated alkyl substances and offspring behaviour and motor development at age 5–9 years--a prospective study. Environ Health. 2015;14:2. doi: 10.1186/1476-069X-14-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tian Y, Zhou Y, Miao M, Wang Z, Yuan W, Liu X, Wang X, Wang Z, Wen S, Liang H. Determinants of plasma concentrations of perfluoroalkyl and polyfluoroalkyl substances in pregnant women from a birth cohort in Shanghai, China. Environ Int. 2018;119:165–173. doi: 10.1016/j.envint.2018.06.015. [DOI] [PubMed] [Google Scholar]
- 15.Cariou R, Veyrand B, Yamada A, Berrebi A, Zalko D, Durand S, Pollono C, Marchand P, Leblanc JC, Antignac JP, et al. Perfluoroalkyl acid (PFAA) levels and profiles in breast milk, maternal and cord serum of French women and their newborns. Environ Int. 2015;84:71–81. doi: 10.1016/j.envint.2015.07.014. [DOI] [PubMed] [Google Scholar]
- 16.Starling AP, Adgate JL, Hamman RF, Kechris K, Calafat AM, Ye X, Dabelea D. Perfluoroalkyl substances during pregnancy and offspring weight and adiposity at birth: examining mediation by maternal fasting glucose in the healthy start study. Environ Health Perspect. 2017;125(6):067016. doi: 10.1289/EHP641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Xia R, Jin L, Li D, Liang H, Yang F, Chen J, Yuan W, Miao M. Association between paternal alcohol consumption before conception and Anogenital distance of offspring. Alcohol Clin Exp Res. 2018;42(4):735–742. doi: 10.1111/acer.13595. [DOI] [PubMed] [Google Scholar]
- 18.Squires JBD. Ages & Stages Questionnaires[R], Third Edition (ASQ-3[TM]): A Parent-Completed Child-Monitoring System. Baltimore: Brookes Publishing Company; 2009.
- 19.Wei M, Bian X, Squires J, Yao G, Wang X, Xie H, Song W, Lu J, Zhu C, Yue H, et al. Studies of the norm and psychometrical properties of the ages and stages questionnaires, third edition, with a Chinese national sample. Zhonghua Er Ke Za Zhi. 2015;53(12):913–918. [PubMed] [Google Scholar]
- 20.Zou G. A modified poisson regression approach to prospective studies with binary data. Am J Epidemiol. 2004;159(7):702–706. doi: 10.1093/aje/kwh090. [DOI] [PubMed] [Google Scholar]
- 21.Stein CR, Savitz DA, Bellinger DC. Perfluorooctanoate exposure in a highly exposed community and parent and teacher reports of behaviour in 6-12-year-old children. Paediatr Perinat Epidemiol. 2014;28(2):146–156. doi: 10.1111/ppe.12097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Fisher M, Arbuckle TE, Liang CL, LeBlanc A, Gaudreau E, Foster WG, Haines D, Davis K, Fraser WD. Concentrations of persistent organic pollutants in maternal and cord blood from the maternal-infant research on environmental chemicals (MIREC) cohort study. Environ Health. 2016;15(1):59. doi: 10.1186/s12940-016-0143-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bjerregaard-Olesen C, Bach CC, Long M, Ghisari M, Bech BH, Nohr EA, Henriksen TB, Olsen J, Bonefeld-Jorgensen EC. Determinants of serum levels of perfluorinated alkyl acids in Danish pregnant women. Int J Hyg Environ Health. 2016;219(8):867–875. doi: 10.1016/j.ijheh.2016.07.008. [DOI] [PubMed] [Google Scholar]
- 24.Callan AC, Rotander A, Thompson K, Heyworth J, Mueller JF, Odland JO, Hinwood AL. Maternal exposure to perfluoroalkyl acids measured in whole blood and birth outcomes in offspring. Sci Total Environ. 2016;569-570:1107–1113. doi: 10.1016/j.scitotenv.2016.06.177. [DOI] [PubMed] [Google Scholar]
- 25.Okada E, Kashino I, Matsuura H, Sasaki S, Miyashita C, Yamamoto J, Ikeno T, Ito YM, Matsumura T, Tamakoshi A, et al. Temporal trends of perfluoroalkyl acids in plasma samples of pregnant women in Hokkaido, Japan, 2003-2011. Environ Int. 2013;60:89–96. doi: 10.1016/j.envint.2013.07.013. [DOI] [PubMed] [Google Scholar]
- 26.Vuong AM, Yolton K, Webster GM, Sjodin A, Calafat AM, Braun JM, Dietrich KN, Lanphear BP, Chen A. Prenatal polybrominated diphenyl ether and perfluoroalkyl substance exposures and executive function in school-age children. Environ Res. 2016;147:556–564. doi: 10.1016/j.envres.2016.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Goudarzi H, Araki A, Itoh S, Sasaki S, Miyashita C, Mitsui T, Nakazawa H, Nonomura K, Kishi R. The Association of Prenatal Exposure to Perfluorinated chemicals with glucocorticoid and androgenic hormones in cord blood samples: the Hokkaido study. Environ Health Perspect. 2017;125(1):111–118. doi: 10.1289/EHP142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Fei C, McLaughlin JK, Lipworth L, Olsen J. Prenatal exposure to perfluorooctanoate (PFOA) and perfluorooctanesulfonate (PFOS) and maternally reported developmental milestones in infancy. Environ Health Perspect. 2008;116(10):1391–1395. doi: 10.1289/ehp.11277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bjerregaard-Olesen C, Bossi R, Liew Z, Long M, Bech BH, Olsen J, Henriksen TB, Berg V, Nost TH, Zhang JJ, et al. Maternal serum concentrations of perfluoroalkyl acids in five international birth cohorts. Int J Hyg Environ Health. 2017;220(2 Pt A):86–93. doi: 10.1016/j.ijheh.2016.12.005. [DOI] [PubMed] [Google Scholar]
- 30.Lu Z, Song L, Zhao Z, Ma Y, Wang J, Yang H, Ma H, Cai M, Codling G, Ebinghaus R, et al. Occurrence and trends in concentrations of perfluoroalkyl substances (PFASs) in surface waters of eastern China. Chemosphere. 2015;119:820–827. doi: 10.1016/j.chemosphere.2014.08.045. [DOI] [PubMed] [Google Scholar]
- 31.Forns J, Iszatt N, White RA, Mandal S, Sabaredzovic A, Lamoree M, Thomsen C, Haug LS, Stigum H, Eggesbo M. Perfluoroalkyl substances measured in breast milk and child neuropsychological development in a Norwegian birth cohort study. Environ Int. 2015;83:176–182. doi: 10.1016/j.envint.2015.06.013. [DOI] [PubMed] [Google Scholar]
- 32.Chen MH, Ha EH, Liao HF, Jeng SF, Su YN, Wen TW, Lien GW, Chen CY, Hsieh WS, Chen PC. Perfluorinated compound levels in cord blood and neurodevelopment at 2 years of age. Epidemiology (Cambridge, Mass) 2013;24(6):800–808. doi: 10.1097/EDE.0b013e3182a6dd46. [DOI] [PubMed] [Google Scholar]
- 33.Jeddy Z, Hartman TJ, Taylor EV, Poteete C, Kordas K. Prenatal concentrations of Perfluoroalkyl substances and early communication development in British girls. Early Hum Dev. 2017;109:15–20. doi: 10.1016/j.earlhumdev.2017.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Johansson N, Eriksson P, Viberg H. Neonatal exposure to PFOS and PFOA in mice results in changes in proteins which are important for neuronal growth and synaptogenesis in the developing brain. Toxicol Sci. 2009;108(2):412–418. doi: 10.1093/toxsci/kfp029. [DOI] [PubMed] [Google Scholar]
- 35.Vested A, Ramlau-Hansen CH, Olsen SF, Bonde JP, Kristensen SL, Halldorsson TI, Becher G, Haug LS, Ernst EH, Toft G. Associations of in utero exposure to perfluorinated alkyl acids with human semen quality and reproductive hormones in adult men. Environ Health Perspect. 2013;121(4):453–458. doi: 10.1289/ehp.1205118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Thibodeaux JR, Hanson RG, Rogers JM, Grey BE, Barbee BD, Richards JH, Butenhoff JL, Stevenson LA, Lau C. Exposure to perfluorooctane sulfonate during pregnancy in rat and mouse. I: maternal and prenatal evaluations. Toxicol Sci. 2003;74(2):369–381. doi: 10.1093/toxsci/kfg121. [DOI] [PubMed] [Google Scholar]
- 37.Ji K, Kim S, Kho Y, Paek D, Sakong J, Ha J, Kim S, Choi K. Serum concentrations of major perfluorinated compounds among the general population in Korea: dietary sources and potential impact on thyroid hormones. Environ Int. 2012;45:78–85. doi: 10.1016/j.envint.2012.03.007. [DOI] [PubMed] [Google Scholar]
- 38.Berg V, Nost TH, Hansen S, Elverland A, Veyhe AS, Jorde R, Odland JO, Sandanger TM. Assessing the relationship between perfluoroalkyl substances, thyroid hormones and binding proteins in pregnant women; a longitudinal mixed effects approach. Environ Int. 2015;77:63–69. doi: 10.1016/j.envint.2015.01.007. [DOI] [PubMed] [Google Scholar]
- 39.Wang Y, Rogan WJ, Chen PC, Lien GW, Chen HY, Tseng YC, Longnecker MP, Wang SL. Association between maternal serum perfluoroalkyl substances during pregnancy and maternal and cord thyroid hormones: Taiwan maternal and infant cohort study. Environ Health Perspect. 2014;122(5):529–534. doi: 10.1289/ehp.1306925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Itoh S, Araki A, Mitsui T, Miyashita C, Goudarzi H, Sasaki S, Cho K, Nakazawa H, Iwasaki Y, Shinohara N, et al. Association of perfluoroalkyl substances exposure in utero with reproductive hormone levels in cord blood in the Hokkaido study on environment and Children's health. Environ Int. 2016;94:51–59. doi: 10.1016/j.envint.2016.05.011. [DOI] [PubMed] [Google Scholar]
- 41.Byrne SC, Miller P, Seguinot-Medina S, Waghiyi V, Buck CL, von Hippel FA, Carpenter DO. Exposure to perfluoroalkyl substances and associations with serum thyroid hormones in a remote population of Alaska natives. Environ Res. 2018;166:537–543. doi: 10.1016/j.envres.2018.06.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Quach J, Hiscock H, Canterford L, Wake M. Outcomes of child sleep problems over the school-transition period: Australian population longitudinal study. Pediatrics. 2009;123(5):1287–1292. doi: 10.1542/peds.2008-1860. [DOI] [PubMed] [Google Scholar]
- 43.Bridgett DJ, Burt NM, Laake LM, Oddi KB. Maternal self-regulation, relationship adjustment, and home chaos: contributions to infant negative emotionality. Infant Behav Dev. 2013;36(4):534–547. doi: 10.1016/j.infbeh.2013.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. The rates of potential developmental problem assessed at 4 years of age by the Age and Stage Questionnaire (ASQ). Table S2. Maternal PFASs concentrations (ng/mL) at 12–16 gestational weeks stratified by child sex. Table S3. P-values of interaction item (PFASs*child sex) in the associations between maternal PFASs concentrations and child’s neurobehavioral problems assessed by ASQ at 4 years of age*. Figure S1. Adjusted generalized additive model plots of ln-transformed PFAS concentrations with developmental problems in communication among offspring. Figure S2. Adjusted generalized additive model plots of ln-transformed PFAS concentrations with offspring developmental problems in Gross motor among offspring. Figure S3. Adjusted generalized additive model plots of ln-transformed PFAS concentrations with developmental problems in Fine motor among offspring. Figure S4. Adjusted generalized additive model plots of ln-transformed PFAS concentrations with developmental problems in Problem solving among offspring. Figure S5. Adjusted generalized additive model plots of ln-transformed PFAS concentrations with developmental problems in Personal-social skills among offspring. (DOCX 15944 kb)
Data Availability Statement
The datasets used in the current study are available from the corresponding authors on reasonable request.


