Short abstract
Blepharokeratoconjunctivitis secondary to ocular demodicosis in the pediatric population is often neglected and may result in a serious sight-threatening condition. In severe cases, it can lead to corneal perforation necessitating urgent corneal transplantation. However, the shortage and high cost of donor corneas is the foremost limitation of keratoplasty in developing countries. Small-incision lenticule extraction is an advanced flapless femtosecond laser refractive procedure in which an intrastromal corneal lenticule is detached and removed to correct myopia and myopic astigmatism. We herein describe a technique in which lenticules are used for the management of corneal perforation secondary to Demodex-induced blepharokeratoconjunctivitis. The lenticule was sutured over the site of the perforated cornea using 10-0 interrupted nylon sutures. The globe integrity was maintained with a good visual outcome. Thus, tectonic keratoplasty using small-incision lenticule extraction appears to be a safe, cost-effective, and reliable alternative method for the management of corneal perforation secondary to blepharokeratoconjunctivitis.
Keywords: Blepharokeratoconjunctivitis, corneal perforation, lenticule, tectonic keratoplasty, ocular demodicosis, pediatric patient
Introduction
Blepharokeratoconjunctivitis (BKC) in the pediatric age group is an under-recognized and poorly defined syndrome. BKC involves the cornea in severe cases, resulting in sight-threatening conditions.1 Among dermatological diseases, demodicosis has been found to be associated with various ocular disorders, including eyelash loss, meibomian gland dysfunction, chalazion formation, conjunctivitis, blepharitis, severe keratitis, and BKC.2–4 However, BKC in the pediatric population is often not considered and may result in vision-threatening problems such as amblyopia, scarring, corneal thinning, and corneal perforation.5–7
Corneal perforation may occur in severe cases of BKC and has been infrequently reported in the literature. Various treatment options are available, such as amniotic membrane transplantation and application of conjunctival flaps, silicone hydrogel contact lenses, and bandage contact lenses.8,9 In most cases, keratoplasty is the only suitable option for tectonic purposes. However, the shortage of donor corneas is an important limitation for corneal transplantation, especially in developing countries such as China, where the demand for grafts is very high.10 In this case report, we describe a surgical technique of tectonic keratoplasty using small-incision lenticule extraction (SMILE) to treat a corneal perforation secondary to BKC. This technique is a safe, feasible, and inexpensive alternative option that can be performed in countries with a huge corneal donor shortage, such as China.
Case presentation
Written informed consent was obtained from the patients for publication of this case report and all accompanying images. Ethical approval was not deemed necessary because this case report and review of the literature is meant for informational and educational purposes only.
The present case report provides an assessment of the treatment and outcome of two pediatric patients (two eyes) with corneal perforation secondary to BKC who were admitted to the Department of Ophthalmology, First Hospital of Jilin University and followed for 9 and 18 months, respectively.
Patient 1
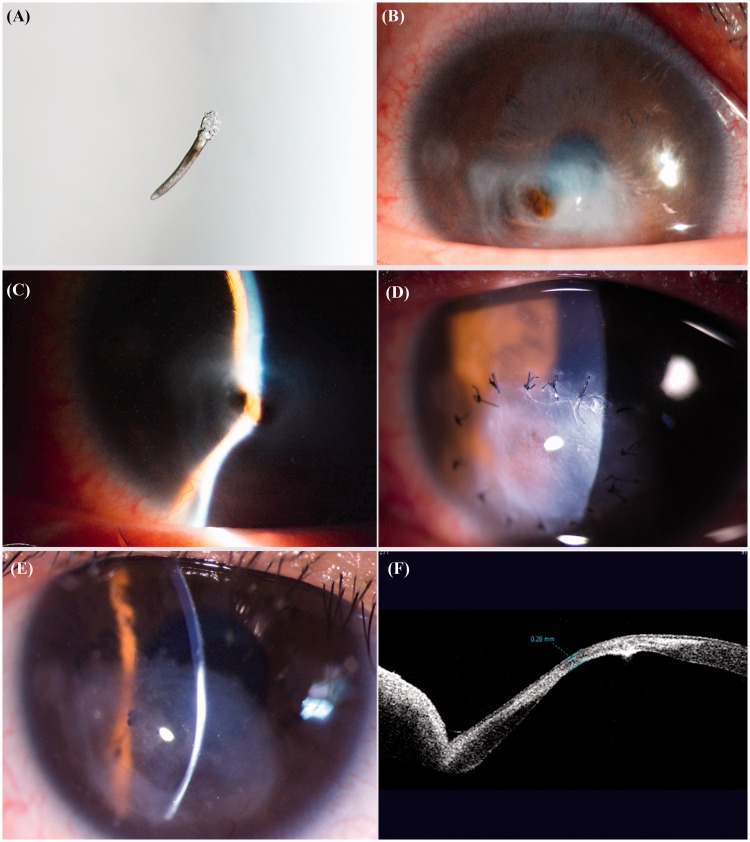
Patient 1 was 17-year-old male who presented with a 1-day history of blurring of vision and a foreign body sensation in the right eye (OD). He also reported bilateral recurrent red eye, eyelash loss, and ocular pain. On presentation, his best-corrected visual acuity (BCVA) was 20/80 OD and 20/20 in the left eye (OS). Four eyelashes were epilated from each eye (two from the upper lid and two from the lower lid). The specimens were then observed under a light microscope. More than three Demodex mites were observed in each eye, suggesting Demodex infection (Figure 1(a)). Slit-lamp biomicroscopy showed redness of the eyelids, crusts on the edges of the eyelids, conjunctival congestion, an irregular pupil, a shallow anterior chamber, and corneal perforation at the inferotemporal region with a prolapsed iris OD (Figure 1(b), (c)). Emergency tectonic keratoplasty using the SMILE technique was performed. No perioperative complications occurred. Postoperatively, the patient was prescribed topical 0.3% ofloxacin (Allergan, Irvine, CA, USA) four times a day for 2 months, topical 1% prednisolone (Allergan) four times a day for 1 month, and topical tacrolimus (Senju Pharmaceutical, Osaka, Japan) four times a day. After 1 month, the steroid was gradually tapered and the immunosuppressive drug was decreased to twice a day for 6 months. The patient was advised to scrub the eyelid with tea tree oil, maintain lid hygiene, and apply daily warm compression to treat the Demodex-associated BKC. The postoperative period was uneventful; the graft remained in position and the suture stayed intact (Figure 1(d)). The corneal suture was removed at 4 months postoperatively, and the patient’s BCVA was 20/60 OD (Figure 1(e)). Nine months after tectonic keratoplasty, the corneal thickness was maintained at 0.2 mm on anterior-segment optical coherence tomography (Visante; Carl Zeiss Meditec, Jena, Germany) (Figure 1(f)).
Figure 1.
Patient 1. (a) Microscopic picture showing Demodex in the epilated eyelashes. (b) Preoperative slit-lamp appearance of the right eye showing conjunctival congestion, corneal thinning, and corneal perforation in the inferotemporal region with iris prolapse as well as (c) a shallow anterior chamber. (d) Postoperative image showing the trimmed lenticule sutured with interrupted 10-0 nylon sutures and (e) the intact graft with no sign of graft rejection after suture removal. (f) Anterior-chamber optical coherence tomography showing a corneal thickness of 0.28 mm at the site of the perforation after the surgery.
Patient 2
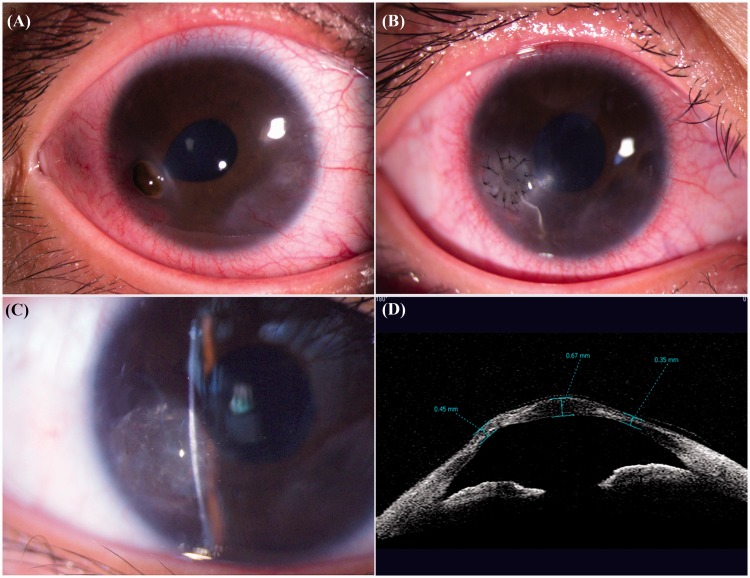
Patient 2 was 14-year-old female who presented with a 2-hour history of decreased vision in the right eye. Her BCVA on presentation was 20/200 OD and 20/20 OS. She had a history of a foreign body sensation and habitual rubbing of the eyes. A laboratory investigation was performed to rule out any systemic diseases. Demodex mites in her epilated eyelashes were confirmed by microscopic detection. Slit-lamp examination revealed crusts in the edges of the eyelids, ciliary injection, a distorted pupil, and a corneal perforation at the 7-o’clock position in the inferotemporal region with iris prolapse OD (Figure 2(a)). Topical corneal thinning was present in both eyes. Emergency surgery was performed. Postoperatively, she was prescribed the same medications as Patient 1. On the first postoperative day, the patient experienced a mild foreign body sensation, and slit-lamp examination showed a well-positioned graft with intact sutures (Figure 2(b)). Complete epithelialization was attained within the first week. Five months after surgery, the corneal sutures were removed and her BCVA was 20/40 with the graft in position (Figure 2(c)). The patient was then assessed every month. Twelve months after keratoplasty, her BCVA was 20/40 and anterior-segment optical coherence tomography revealed a corneal thickness of 0.45 mm at the site of the perforation (Figure 2(d)).
Figure 2.
Patient 2. (a) Preoperative slit-lamp appearance of the right eye showing ciliary injection, an irregular pupil, and perforated cornea in the inferior part of the temporal region with prolapse of the iris. (b) Postoperative image showing an intact suture with the graft in position. (c) Image after removal of the suture with a sealed corneal perforation and no sign of rejection. (d) Anterior-chamber optical coherence tomography showing a corneal thickness of 0.45 mm at the site of the perforation after the surgery.
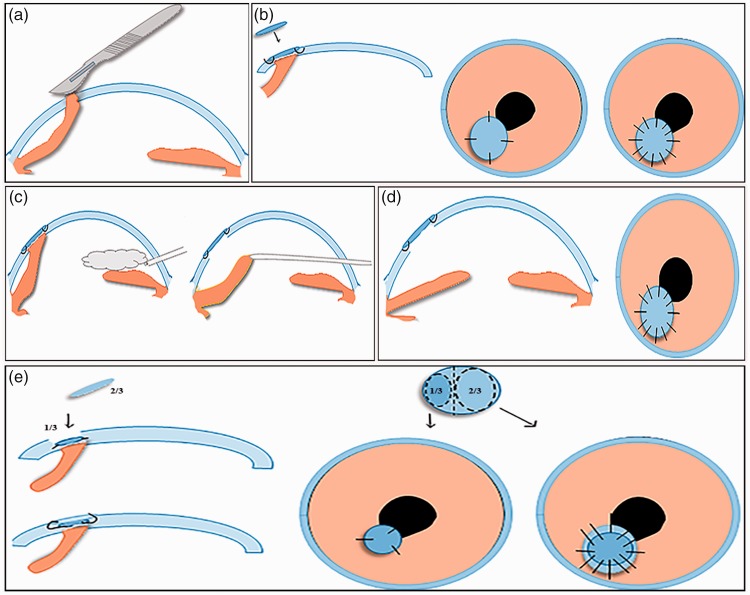
Surgical technique
After administration of a retrobulbar block, the epithelial tissue around the corneal perforation was debrided from the corneal surface using the surgical knife. The fibrous membrane covering the prolapsed iris was removed (Figure 3(a)). The size of the corneal defect was measured with a measuring caliper. In Patient 1, the lenticule for the SMILE procedure was obtained with a VisuMax femtosecond laser (Carl Zeiss Meditec) from a healthy myopic donor with a refractive correction spherical equivalent of −8.50 diopters and lenticular central thickness of ≥100 µm. The optical zone was 6.5 mm, and the cap thickness was 120 µm. The lenticule was then trimmed to a size slightly larger than the corneal defect. Synthetic monofilament nonabsorbable 10-0 nylon cardinal sutures (Ethicon, Somerville, NJ, USA) were placed at the 12-o’clock and 6-o’clock positions in the recipient; this was immediately followed by placement of 3-o’clock and 9-o’clock cardinal sutures. The remaining suture was then placed (Figure 3(b)).
Figure 3.
Tectonic keratoplasty procedure. (a) The fibrous membrane was removed using a scalpel. (b) The trimmed lenticule was placed over the corneal defect and sutured in a single layer using interrupted 10-0 nylon sutures in Patient 1. (c) The viscoelastic material was introduced and the iris was released from the perforation using an iris repository. (d) The graft was sutured with the iris in a normal anatomical position. (e) The lenticule was placed over the corneal defect and sutured in two layers in Patient 2.
For Patient 2, the lenticule was obtained as for Patient 1, from a healthy and serologically negative myopic donor. After the SMILE procedure, it was stored in glycerol media and cut into two pieces using Westcott scissors. Initially, the small piece of about one-third the total diameter of the lenticule was excised to a size slightly larger than the corneal defect, and three interrupted 10-0 nylon sutures were placed at the 1-o’clock, 4-o’clock, and 9-o’clock positions in the recipient’s eye to stabilize the graft. The larger piece of about two-thirds the total diameter was then trimmed to a size slightly larger than the defect and placed over the smaller piece. Both lenticule pieces were then sutured to the recipient using interrupted 10-0 nylon sutures (Figure 3(e)).
In both patients, viscoelastic material was then introduced into the anterior chamber from the site opposite the perforation to maintain the anterior chamber depth. The iris blocking the corneal perforation was then released using an iris repositor (Figure 3(c), (d)). After maintaining the anatomic integrity of the iris, the viscoelastic material was removed and the wound was tested for aqueous leaks. Finally, the cornea was enclosed with a therapeutic contact lens, and 0.3% tobramycin plus dexamethasone eye ointment (S.A. Alcon-Couvreur N.V., Puurs, Belgium) was applied in the conjunctival sac.
Outcome
This technique was performed by the same corneal surgeon in both cases. The corneal perforation healed, the globe integrity was maintained, and the visual outcome was good in both cases. At the follow-up examination, the patients had no signs of graft melting, graft rejection, corneal neovascularization, or infection.
Discussion
In this case report, we assessed the outcome of tectonic keratoplasty using a SMILE-derived lenticule as a graft for the management of corneal perforation secondary to BKC. Our cases indicate that this technique can be effectively performed in selected cases by an experienced corneal surgeon and that it is a safe, feasible, and effective alternative option for the management of corneal perforations. Possible early postoperative complications include primary graft failure, graft loss, wound leakage, increased intraocular pressure, and infection; late complications are graft rejection and infection. To reduce these risks, routine examination of the patient and proper monitoring of the drugs used is recommended. In case of primary graft failure and graft rejection, corneal transplantation is advised.
SMILE is an advanced flapless femtosecond laser refractive procedure to correct myopia and myopic astigmatism, in which an intrastromal corneal lenticule is detached and removed.11 Corneal lenticules obtained by this technique are reported to be transparent, high-quality grafts. Because these lenticules are extracted as a single piece, they can be re-implanted for the management of corneal defects and corneal perforations. Re-implantation of SMILE-extracted lenticules has been performed in animals12–14 and has been clinically applied in human patients.15 The first successful human implantation of a SMILE lenticule was reported by Pradhan et al.16 The lenticule was extracted from a myopic donor for the correction of hyperopia with no specific adverse effects at the 1-year follow-up. Moreover, various publications have described re-implantation of SMILE-extracted lenticules in human patients for the management of hyperopia,17,18 presbyopia,19 corneal thinning,20,21 corneal dystrophy,22 microperforations,23 bullous keratopathy,15 and corneal ulcers and perforations.24–27 To our knowledge, the use of SMILE-extracted lenticules for treatment of corneal perforation secondary to BKC has not been reported.
Preservation of the anatomical structure of the eyeball and visual rehabilitation are the main goals of corneal transplantation for corneal perforation secondary to BKC. However, a huge shortage and very high cost of donor corneas are the foremost limitations for keratoplasty in developing countries.10 In our cases, we used the SMILE-extracted lenticules as an alternative technique instead of the usual corneal grafts to both manage the perforation and maintain the structure of the eyeball. The layer of the lenticule used in each case depends upon the residual corneal thickness. In both cases, the anatomical structure of the eyeball was maintained with a good visual outcome. The surgical result was satisfactory, and both patients received these lenticules without additional financial cost.
A potential disadvantage of this technique is the low availability of donor lenticules in centers with no SMILE facility. However, these lenticules can be stored in glycerol media; thus, the lenticules may be supplied to other surgical facilities through the use of eye banks. Furthermore, the SMILE-extracted lenticule is not a mature graft, unlike other usual corneal tissues. Hence, in patients with severe infection, the corneal surfaces must be carefully observed and long-term follow-up is needed to assess the graft stability and rejection.
In conclusion, tectonic keratoplasty using a SMILE-derived intrastromal lenticule is a safe, efficient, and reasonable alternative approach for the management of corneal perforation secondary to BKC. Furthermore, these lenticules may solve the problem of the huge donor shortage coupled with the substantial monetary cost of donor corneas in developing countries such as China and result in better functional outcomes.
Declaration of conflicting interests
The authors declare that there is no conflict of interest.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
References
- 1.Farpour B, McClellan KA. Diagnosis and management of chronic blepharokeratoconjunctivitis in children. J Pediatr Ophthalmol Strabismus 2001; 38: 207–212. [DOI] [PubMed] [Google Scholar]
- 2.Kheirkhah A, Casas V, Li W, et al. Corneal manifestations of ocular demodex infestation. Am J Ophthalmol 2007; 143: 743–749. [DOI] [PubMed] [Google Scholar]
- 3.Lee SH, Chun YS, Kim JH, et al. The relationship between demodex and ocular discomfort. Invest Ophthalmol Vis Sci 2010; 51: 2906–2911. [DOI] [PubMed] [Google Scholar]
- 4.Liang L, Safran S, Gao Y, et al. Ocular demodicosis as a potential cause of pediatric blepharoconjunctivitis. Cornea 2010; 29: 1386–1391. [DOI] [PubMed] [Google Scholar]
- 5.Czepita D, Kuźna-Grygiel W, Kosik-Bogacka D. Investigations on the occurrence as well as the role of Demodex follicuforum and Demodex brevis in the pathogenesis of blepharitis. Klin Oczna 2005; 107: 80–82. [PubMed] [Google Scholar]
- 6.Jones SM, Weinstein JM, Cumberland P, et al. Visual outcome and corneal changes in children with chronic blephatokeratoconjunctivitis. Ophthalmology 2007; 114: 2271–2280. [DOI] [PubMed] [Google Scholar]
- 7.Culbertson WW, Huang AJ, Mandelbaum SH, et al. Effective treatment of phlyctenular keratoconjunctivitis with oral tetracycline. Ophthalmology 1993; 100: 1358–1366. [DOI] [PubMed] [Google Scholar]
- 8.Hick S, Demers PE, Brunette I, et al. Amniotic membrane transplantation and fibrin glue in the management of corneal ulcers and perforations: a review of 33 cases. Cornea 2005; 24: 369–377. [DOI] [PubMed] [Google Scholar]
- 9.Bendoriene J, Vogt U. Therapeutic use of silicone hydrogel contact lenses I children. Eye Contact Lens 2006; 32: 104–108. [DOI] [PubMed] [Google Scholar]
- 10.Hong J, Shi W, Liu Z, et al. Limitations of keratoplasty in China: a survey analysis. PLoS One 2015; 10: e0132268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sekundo W, Kunert KS, Blum M. Small incision corneal refractive surgery using the small incision lenticule extraction (SMILE) procedure for the correction of myopia and myopic astigmatism: results of a 6-month prospective study. Br J Ophthalmol 2011; 95: 335–339. [DOI] [PubMed] [Google Scholar]
- 12.Liu YC, Teo EPW, Ang HP, et al. Biological corneal inlay for presbyopia derived from small incision lenticule extraction (SMILE). Sci Rep. 2018; 8: 1831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Williams GP, Wu B, Liu YC, et al. Hyperopic refractive correction by LASIK, SMILE or lenticule reimplantation in a non-human primate model. PLoS One 2018; 13: e0194209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zhao J, Shen Y, Tian M, et al. Corneal lenticule allotransplantation after femtosecond laser small incision lenticule extraction in rabbits. Cornea 2017; 36: 222–228. [DOI] [PubMed] [Google Scholar]
- 15.Song YJ, Kim S, Yoon GJ. Case series: use of stromal lenticule as patch graft. Am J Ophthalmol Case Rep 2018; 12: 79–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pradhan KR, Reinstein DZ, Carp GI, et al. Femtosecond laser assisted keyhole endokeratophakia: correction of hyperopia by implantation of an allogeneic lenticule obtained by SMILE from a myopic donor. J Refract Surg 2013; 29: 777–782. [DOI] [PubMed] [Google Scholar]
- 17.Ganesh S, Brar S, Rao PA. Cryopreservation of extracted corneal lenticules after small incision lenticule extraction for potential use in human subjects. Cornea 2014; 33: 1355–1362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sun L, Yao P, Li M, et al. The safety and predictability of implanting autologous lenticule obtained by SMILE for hyperopia. J Refract Surg 2015; 31: 374–379. [DOI] [PubMed] [Google Scholar]
- 19.Jacob S, Kumar DA, Agarwal A, et al. Preliminary Evidence of Successful Near Vision Enhancement With a New Technique: PrEsbyopic Allogenic Refractive Lenticule (PEARL) corneal inlay using a SMILE lenticule. J Refract Surg 2017; 33: 224–229. [DOI] [PubMed] [Google Scholar]
- 20.Pant OP, Hao JL, Zhou DD, et al. A novel case using femtosecond laser-acquired lenticule for recurrent pterygium: case report and literature review. J Int Med Res 2018; 46: 2474–2480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pant OP, Hao JL, Zhou DD, et al. Lamellar keratoplasty using femtosecond laser intrastromal lenticule for limbal dermoid: case report and literature review. J Int Med Res 2018; 46: 4753–4759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zhao J, Sun L, Shen Y, et al. Using donor lenticules obtained through smile for anepikeratophakia technique combined with phototherapeutic keratectomy. J Refract Surg 2016; 32: 840–845. [DOI] [PubMed] [Google Scholar]
- 23.Bhandari V, Ganesh S, Brar S, et al. Application of the SMILE-derived glued lenticule patch graft in microperforations and partial-thickness corneal defects. Cornea 2016; 35: 408–412. [DOI] [PubMed] [Google Scholar]
- 24.Wu F, Jin X, Xu Y, et al. Treatment of corneal perforation with lenticules from small incision lenticule extraction surgery: a preliminary study of 6 patients. Cornea 2015; 34: 658–663. [DOI] [PubMed] [Google Scholar]
- 25.Jiang Y, Li Y, Liu XW, et al. A novel tectonic keratoplasty with femtosecond laser intrastromal lenticule for corneal ulcer and perforation. Chin Med J (Engl) 2016; 129: 1817–1821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Abd Elaziz MS, Zaky AG, et al. Stromal lenticule transplantation for management of corneal perforations; one year results. Graefes Arch Clin Exp Ophthalmol 2017; 255: 1179–1184. [DOI] [PubMed] [Google Scholar]
- 27.Xue C, Xia Y, Chen Y, et al. [Treatment of large corneal perforations with acellular multilayer of corneal stromal lenticules harvested from femtosecond laser lenticule extraction]. Zhonghua Yan Ke Za Zhi 2015; 51: 655–659. [PubMed] [Google Scholar]