Short abstract
Objective
This study was designed to assess clinical predictors of hypoxemia and develop an artificial neural network (ANN) model for prediction of hypoxemia during sedation for gastrointestinal endoscopy examination.
Methods
A total of 220 patients were enrolled in this prospective observational study. Data on demographics, chronic concomitant disease information, neck circumference, thyromental distance and anaesthetic dose were collected and statistically analysed.
Results
Univariate analysis indicated that body mass index (BMI), habitual snoring and neck circumference were associated with hypoxemia. An ANN model was developed with three variables (BMI, habitual snoring and neck circumference). The area under the receiver operating characteristic curve for the ANN model was 0.80.
Conclusions
The ANN model developed here, comprising BMI, habitual snoring and neck circumference, was useful for prediction of hypoxemia during sedation for gastrointestinal endoscopy.
Keywords: Age, anaesthesia, endoscopic procedure, hypoxemia, risk factor, sedation, snoring
Introduction
Anaesthesiologist-directed propofol sedation in endoscopic procedures improves patient comfort and facilitates endoscopic performance. However, propofol may give rise to sedation-related complications by accentuating airway collapse and lowering the thresholds for upper airway obstruction and hypoxemia.1 Therefore, early identification of high-risk patients with hypoxemia before endoscopy may help physicians select those patients that would benefit most from aggressive interventions such as chin lifting, positive pressure ventilation and endotracheal intubation. Several studies have been conducted to develop bedside tests that can easily and quickly predict sedation-related complications.1,2 However, there is limited literature on specific clinical predictors of hypoxemia development during sedation for gastrointestinal endoscopic procedures.
Artificial neural network (ANN) analysis is a mathematical statistical technique that can successfully predict clinical outcomes when the relationship between predictors and prognosis is complex, multidimensional and non-linear.3 The aim of the present study was to assess the value of an ANN model in predicting the development of hypoxemia during gastrointestinal endoscopy examination.
Materials and methods
Inclusion and exclusion criteria
This prospective observational study was conducted between 5 July, 2017, and 31 July, 2017, in the First Affiliated Hospital of Wenzhou Medical University.4 Patients with American Society of Anesthesiologists (ASA) status I–III undergoing routine gastroscopy and/or colonoscopy examination were enrolled. Exclusion criteria were therapeutic endoscopy, prior gastric or colonic resection, inadequate bowel preparation, severe cardiopulmonary diseases before data collection, patients with ASA class of 4 or higher and lack of complete data availability.
Patient monitoring and data collection
Age, sex, body mass index (BMI), ASA class, neck circumference, thyromental distance, history of hypertension, diabetes mellitus, alcohol consumption, smoking and habitual snoring (yes or no) were recorded before the endoscopy.5 The category of endoscopy examination and the doses of propofol and etomidate were also recorded. Habitual snoring was defined as snoring on more than 3 nights a week.6
In the operating room, the patients received oxygen via a nasal cannula at 3 L/min and were positioned with pillows under the head. Electrocardiography, heart rate, pulse oximetry and intermittent blood pressure were continuously monitored. To induce anaesthesia, the anaesthesiologist used propofol alone or in combination with low-dose etomidate. Propofol dosage was adjusted to maintain deep sedation throughout the procedure.
Definition of outcome and ethics
The primary endpoint of this study was to develop an ANN model for prediction of hypoxemia. Hypoxemia was defined as a pulse oximetry reading <90% for any duration during the endoscopy procedure.1
This study protocol was approved by the ethics committee of the First Affiliated Hospital of Wenzhou Medical University and performed according to the principles articulated in the Declaration of Helsinki. Written informed consent was obtained from all subjects and data were anonymized before analysis.
Statistical analysis
This manuscript adheres to the Standards for Accurate Reporting of Diagnostic Tests (STARD) guidelines. Continuous values were expressed by mean ± standard deviation and compared using Student’s t-test. Categorical values were described using counts and proportions and compared using the χ2 test or Fisher’s exact test.
All variables that showed differences between patients with and those without hypoxemia in the univariate analysis were included in an ANN analysis. A three-layered ANN model with three hidden nodes and a back propagation circuit was constructed as described previously.3,7 A five-fold cross validation was performed to prevent overtraining. The ANN was trained with maximum iterations of 500 and 10 tours. The overfit penalty was set at 0.001 and a convergence criterion of 0.00001 was selected. The ANN output was transformed to the range 0–1; hypoxemia was predicted if the output was greater than or equal to 0.5.
A receiver operating characteristic (ROC) curve was constructed and the area under the receiver operating characteristic curve (AUC) was used to evaluate the performance of the ANN model and other predictions. A variable with an AUC above 0.8 was considered excellent.8 The sensitivity, specificity, positive likelihood ratio (+LR), negative likelihood ratio (−LR), positive predictive value, negative predictive value and diagnostic accuracy were calculated for the cutoff values.
Differences were considered statistically significant if the two-tailed P value was less than 0.05. All calculations were performed using JMP 6.0 (SAS Institute Inc., Cary, NC, USA) and STATA (StataCorp LP, College Station, TX, USA) software.
Results
Baseline characteristics
During the study period, 220 patients (mean age: 50 ± 12.0 years) were enrolled. Of these, 134 (60.9%) were males. In all, 25 (11.4%) patients underwent only gastroscopy and 41 (18.6%) received only colonoscopy; 154 (70.0%) received a combination of gastroscopy and colonoscopy examination. The incidence of hypoxemia was 10% (22/220). Interventions for hypoxemia were chin lift manoeuver (22 patients), modified mask airway (22 patients), positive pressure ventilation (also called bag-mask ventilation) (6 patients) and use of a nasopharyngeal airway (2 patients). Some patients received more than one manipulation. There were no cases of endotracheal intubation in the entire cohort.
Univariate analysis
Univariate analysis indicated that there was no significant statistical difference between patients with and without hypoxemia with respect to age, sex, ASA class, thyromental distance, hypertension, diabetes mellitus, alcohol consumption and smoking (Table 1). There was also no significant difference between patients with and without hypoxemia on type of endoscopy examination, dose of propofol and dose of etomidate used.
Table 1.
Baseline characteristics and clinical outcomes for 220 patients in the two study groups
| Variable | HypoxemiaN = 22 | Non-hypoxemiaN =198 | P value |
|---|---|---|---|
| Age, years | 54.7 ± 11.8 | 49.8 ± 11.8 | 0.07 |
| Male sex, N (%) | 15 (68.2) | 116 (60.1) | 0.46 |
| BMI, kg/m2 | 25.8 ± 3.6 | 23.1 ± 4.3 | 0.005 |
| ASA class I/II/III | 3/19/0 | 69/127/2 | 0.11 |
| Neck circumference (cm) | 37.5 ± 2.8 | 35.3 ± 4.0 | 0.014 |
| Thyromental distance (cm) | 6.5 ± 0.5 | 6.4 ± 0.9 | 0.57 |
| Hypertension, N (%) | 6 (27.3) | 35 (17.7) | 0.273 |
| Diabetes mellitus, N (%) | 2 (9.1) | 19 (9.6) | 0.94 |
| Alcohol consumption, N (%) | 7 (31.8) | 65 (32.8) | 0.924 |
| Smoking, N (%) | 4 (18.2) | 43 (21.7) | 0.701 |
| Habitual snoring, N (%) | 14 (63.6) | 67 (33.8) | 0.006 |
| Endoscopy | 0.932 | ||
| Gastroscopy only, N (%) | 2 (9.1) | 23 (11.6) | |
| Colonoscopy only, N (%) | 4 (18.2) | 37 (18.7) | |
| Gastroscopy and colonoscopy, N (%) | 16 (72.7) | 138 (69.7) | |
| Pharmacological data | |||
| Propofol induction dose | 119 ± 36 | 126 ± 25 | 0.251 |
| Total propofol dose | 185 ± 55 | 172 ± 44 | 0.227 |
| Etomidate, N (%) | 5 (22.7) | 33 (16.7) | 0.476 |
Data are shown with mean ± standard deviation or numbers and percentages as appropriate. BMI: body mass index; ASA: American Society of Anesthesiologists
However, BMI (P = 0.005), habitual snoring (P = 0.006) and neck circumference (P = 0.014) were significantly associated with hypoxemia.
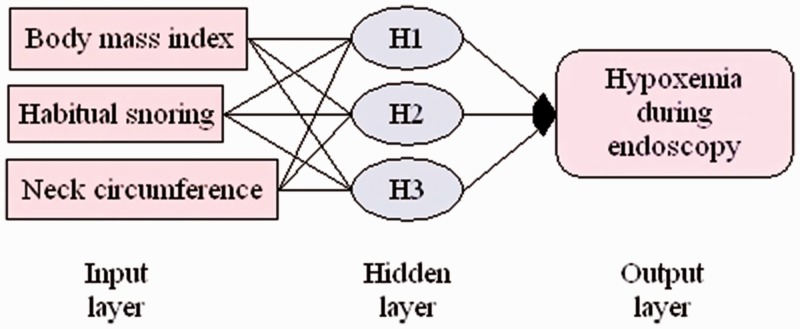
Construction and performance of ANN
Based on the univariate analysis results, three pre-endoscope measurement variables (BMI, habitual snoring and neck circumference) were used to develop and train a three-layer 3-3-1 feedforward backpropagation ANN model (Figure 1).
Figure 1.
An artificial neural network for the prediction of hypoxemia during endoscopy consisting of three input variables, a hidden layer with three nodes and one output variable
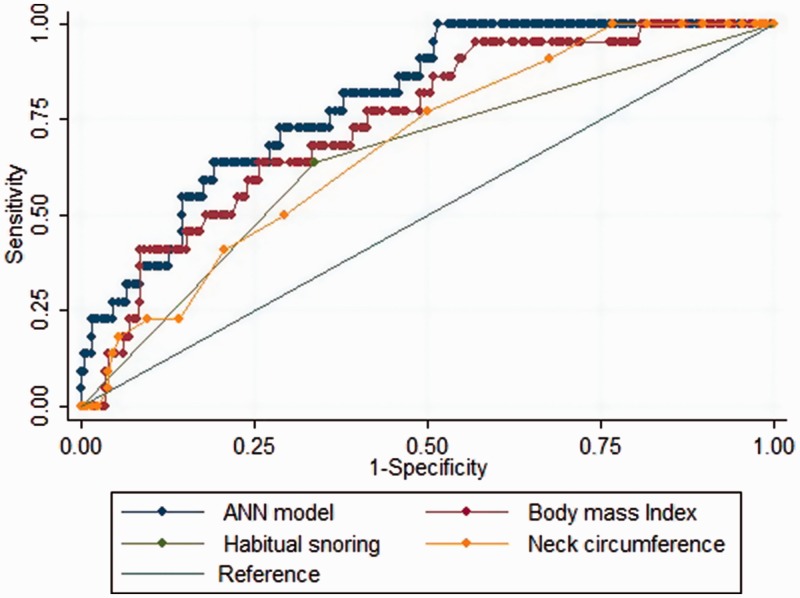
The ROC analysis (Figure 2) indicated that the AUC of the ANN model (0.80 ± 0.04) was significantly higher than that of BMI (0.74 ± 0.05, P < 0.001), habitual snoring (0.65 ± 0.06, P < 0.001) and neck circumference (0.68 ± 0.05, P < 0.001).
Figure 2.
Receiver operating characteristic curves for the artificial neural network (ANN) model, body mass index, habitual snoring and neck circumference. The ideal area under the receiver operating characteristic curve (AUC) was 1.00. The reference line represents an AUC of 0.50, based on chance alone
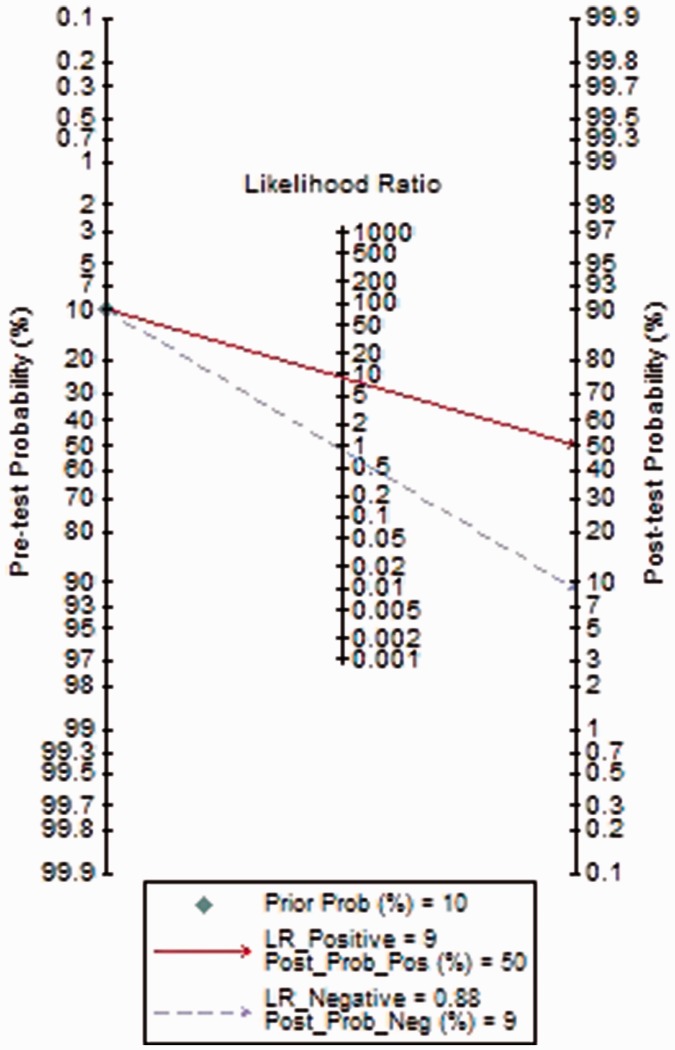
The sensitivity, specificity, +LR, −LR, positive predictive value, negative predictive value and diagnostic accuracy of the ANN model were 14%, 98%, 9.00, 0.88, 50%, 91% and 90%, respectively.
Using the prevalence value of hypoxemia (10% in this study) as the pre-test probability, a Fagan plot (Figure 3) indicated that the ANN model was clinically informative, as it increased the probability of hypoxemia classification up to 50% when positive and lowered the probability to 9% when negative.
Figure 3.
Fagan plot of ANN model for prediction of hypoxemia. ANN: artificial neural network; Prob: probability; LR Positive: positive likelihood ratio; LR Negative: negative likelihood ratio
Discussion
Jones and Nzekwu9 reported that lung volumes, particularly functional residual capacity and expiratory reserve volume, decrease as BMI increases. Kendale and Blitz10 observed that higher BMI was associated with the incidence of intraoperative hypoxemia. Wani et al.11 have suggested that BMI is an independent predictor of sedation-related complications during propofol-mediated sedation for advanced endoscopic procedures. Our study showed that patients with hypoxemia had higher BMI than patients without hypoxemia (25.8 vs. 23.1, P = 0.005) (Table 1).
Snoring is a major symptom of obstructive sleep apnoea–hypopnoea syndrome. Habitual snoring (snoring on more than 3 nights a week) is the best predictor of obstructive sleep apnoea.6 Cote et al.12 reported that the incidence of hypoxemia was more frequent in patients with obstructive sleep apnoea during advanced endoscopic procedures. Our study showed that hypoxemia occurred more frequently in patients who snored habitually than in patients who did not (63.6% vs. 33.8%, P = 0.006) (Table 1).
Fatty shorter necks and small thyromental distance have been used as simple, clinically useful predictors of difficult airway in some studies.13,14 However, the relationship among neck circumference, thyromental distance and hypoxemia during the endoscopy procedure has not been previously investigated. Our findings suggest that increased neck circumference, but not thyromental distance, was associated with risk of hypoxemia during endoscopy (Table 1).
An ANN model built on three variables (BMI, habitual snoring and neck circumference), with an AUC of 0.80, was a useful tool for prediction of hypoxemia during the endoscopy procedure (Figure 1). The ANN AUC was statistically superior to that of other single parameters, indicating that the ANN performed better than any other single parameter (Figure 2).
To the best of our knowledge, this is the first study to attempt to create an ANN to predict hypoxemia during sedation for endoscopic procedures. The ANN model successfully predicted hypoxemia better than did the individual variables in a univariate analysis. However, this study had several important limitations. First, the sample size was relatively small, which may have produced bias. Second, we did not investigate other potential predictors of hypoxemia, such as examination duration. However, results from a previous study suggest that procedure time is not associated with incidence of cardiopulmonary events using propofol sedation for routine oesophagogastroduodenoscopy or colonoscopy.2 Last, the sensitivity and positive predictive value of our ANN model were low, indicating that the ANN model could only identify a small portion of patients who developed hypoxemia during endoscopy. In other words, some patients who develop hypoxemia may have not high BMI, habitual snoring and large neck circumference. It would be interesting to carry out a large-sample prospective study to determine whether other variables such as age, ASA status and thyromental distance improve the sensitivity of our ANN model. However, the specificity and negative predictive values were high, indicating that our ANN model can correctly identify which patients will not develop hypoxemia during sedation for routine gastrointestinal endoscopy.
In conclusion, an ANN model comprising BMI, habitual snoring and neck circumference was useful for prediction of hypoxemia during sedation for routine gastrointestinal endoscopy.
Acknowledgements
This work was partly supported by the National Natural Science Foundation of China (81774109), Zhejiang Provincial Department of Education (Y201839270) and Wenzhou Science and Technology Plan Project (Y20180508).
Declaration of conflicting interest
The authors declare that there is no conflict of interest.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
References
- 1.Coté GA, Hovis RM, Ansstas MA, et al. Incidence of sedation-related complications with propofol use during advanced endoscopic procedures. Clin Gastroenterol Hepatol 2010; 8: 137–142. 2009/07/18. DOI: 10.1016/j.cgh.2009.07.008 S1542-3565(09)00656-9 [pii]. [DOI] [PubMed] [Google Scholar]
- 2.Mehta PP, Kochhar G, Kalra S, et al. Can a validated sleep apnea scoring system predict cardiopulmonary events using propofol sedation for routine EGD or colonoscopy? A prospective cohort study. Gastrointest Endosc 2014; 79: 436–444. 2013/11/14. DOI: 10.1016/j.gie.2013.09.022 S0016-5107(13)02407-3 [pii]. [DOI] [PubMed] [Google Scholar]
- 3.Hong WD, Chen XR, Jin SQ, et al. Use of an artificial neural network to predict persistent organ failure in patients with acute pancreatitis. Clinics (Sao Paulo) 2013; 68: 27–31. 2013/02/20. DOI: S1807-59322013000100005 [pii]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Geng W, Jia D, Wang Y, et al. A prediction model for hypoxemia during routine sedation for gastrointestinal endoscopy. Clinics (Sao Paulo) 2018; 73: e513. 2018/11/22. DOI: S1807-59322018000100285 [pii] 10.6061/clinics/2018/e513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Khan ZH, Mohammadi M, Rasouli MR, et al. The diagnostic value of the upper lip bite test combined with sternomental distance, thyromental distance, and interincisor distance for prediction of easy laryngoscopy and intubation: a prospective study. Anesth Analg 2009; 109: 822–824. 2009/08/20. DOI: 10.1213/ane.0b013e3181af7f0d 109/3/822 [pii]. [DOI] [PubMed] [Google Scholar]
- 6.Sharma SK, Kumpawat S, Banga A, et al. Prevalence and risk factors of obstructive sleep apnea syndrome in a population of Delhi, India. Chest 2006; 130: 149–156. 2006/07/15. DOI: S0012-3692(15)50965-3 [pii] 10.1378/chest.130.1.149. [DOI] [PubMed] [Google Scholar]
- 7.Hong WD, Ji YF, Wang D, et al. Use of artificial neural network to predict esophageal varices in patients with HBV related cirrhosis. Hepat Mon 2011; 11: 544–547. 2011/11/17. [PMC free article] [PubMed] [Google Scholar]
- 8.Hong WD, Zhu QH, Huang ZM, et al. Predictors of esophageal varices in patients with HBV-related cirrhosis: a retrospective study. BMC Gastroenterol 2009; 9: 11. 2009/02/07. DOI: 10.1186/1471-230X-9-11 1471-230X-9-11 [pii]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jones RL, Nzekwu MM. The effects of body mass index on lung volumes. Chest 2006; 130: 827–833. 2006/09/12. DOI: S0012-3692(15)52798-0 [pii] 10.1378/chest.130.3.827. [DOI] [PubMed] [Google Scholar]
- 10.Kendale SM, Blitz JD. Increasing body mass index and the incidence of intraoperative hypoxemia. J Clin Anesth 2016; 33: 97–104. 2016/08/25. DOI: 10.1016/j.jclinane.2016.03.020 S0952-8180(16)30033-2 [pii]. [DOI] [PubMed] [Google Scholar]
- 11.Wani S, Azar R, Hovis CE, et al. Obesity as a risk factor for sedation-related complications during propofol-mediated sedation for advanced endoscopic procedures. Gastrointest Endosc 2011; 74: 1238–1247. 2011/12/06. DOI: 10.1016/j.gie.2011.09.006 S0016-5107(11)02176-6 [pii]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cote GA, Hovis CE, Hovis RM, et al. A screening instrument for sleep apnea predicts airway maneuvers in patients undergoing advanced endoscopic procedures. Clin Gastroenterol Hepatol 2010; 8: 660–665.e1. 2010/06/29. DOI: 10.1016/j.cgh.2010.05.015 S1542-3565(10)00501-X [pii]. [DOI] [PubMed] [Google Scholar]
- 13.Tripathi M, Pandey M. Short thyromental distance: a predictor of difficult intubation or an indicator for small blade selection? Anesthesiology 2006; 104: 1131–1136. 2006/05/30. DOI: 00000542-200606000-00006 [pii]. [DOI] [PubMed] [Google Scholar]
- 14.Kim WH, Ahn HJ, Lee CJ, et al. Neck circumference to thyromental distance ratio: a new predictor of difficult intubation in obese patients. Br J Anaesth 2011; 106: 743–748. 2011/03/01. DOI: 10.1093/bja/aer024 S0007-0912(17)33227-0 [pii]. [DOI] [PubMed] [Google Scholar]