Abstract
Objective
To determine the effects of a structured team-based learning approach to quality improvement (QI) on the performance 12 months later of two teams caring for patients with dementia.
Design
Before and after prospective study.
Setting
Staff working in two inpatient services in National Health Service Trusts in England, one providing orthopaedic surgery (Team A) and one caring for elderly people with mental health conditions, including dementia (Team B). Team A consisted of nurses; Team B included doctors, nurses, therapists, mental health support workers and administrators.
Methods
QI training and support, assessment of the performance of teams and team coaching were provided to the two teams. QI training integrated tools for teamworking and a structured approach to QI. Team members completed the Aston Team Performance Inventory, a validated tool for assessing team performance, at the start of the QI work (time 1) and 1 year later (time 2).
Results
A year after the QI training and team QI project, Team A members perceived themselves as a high-performing team, reflected in improvement in 24 of 52 components measured in the Inventory; Team B was initially a poorly performing team and had improvements in 42 of 52 components a year later.
Conclusion
This study demonstrates that a structured team-based learning approach to QI has effects a year later on the performance of teams in clinical settings, as measured by a validated team performance tool.
Keywords: teamwork, team training, quality improvement methodologies, quality improvement
Introduction
Healthcare systems throughout the world are focused on achieving improvements in the quality of patient care using the concept of quality improvement (QI).1–3 A number of strategies and approaches, for example, Plan-Do-Study-Act (PDSA), lean, value stream analysis, six sigma, re-engineering, have been applied in healthcare organisations.4
The importance of teams and skilled facilitation of teamwork on a QI project has been recognised.5–10 These studies have limitations, particularly the lack of evidence on the attributes of successful and unsuccessful team QI initiatives, how to establish and implement QI teams and the contribution of selected QI interventions.11 It has also been unclear if teamwork demonstrated in the completion of a QI project is sustained over time and can be generalised to other teamwork functions other than QI.
QI Fellowships have been established in some National Health Service (NHS) organisations in England to teach and support for individual clinicians interested in carrying out a QI project. In recognition of the evidence on teams and QI, a QI Team Fellowship was offered to clinical teams working in a Region in the English NHS. The QI Team Fellowship provided face-to-face learning on QI, skilled QI facilitation and team coaching for teams of staff interested in carrying out a QI project. Staff teams applied and were selected to participate in the QI Team Fellowship.
This paper reports on the experience of two teams that participated in this QI Team Fellowship and the effects of participation on their performance as teams in clinical settings 1 year later. Evidence of the specific improvements in quality of care achieved by the teams for patients with dementia has been previously reported elsewhere.12 13
Setting
Two inpatient services in NHS Trusts in England, one an 88-bedded inpatient orthopaedic surgery unit (Team A), and one an 18-bedded inpatient ward caring for elderly people with mental health conditions, in particular, dementia (Team B). Team A consisted of nurses; Team B included doctors, nurses, therapists, mental health support workers and administrators. A senior nurse served as coordinator of the QI work in each team.
Methods
QI interventions
A structured package of QI interventions was provided for both teams, consisting of standardised workshops and facilitation as needed. The workshops included content on: the QI process; tools to reach consensus on decisions within the team; and how to design the QI project; involve key stakeholders; carry out baseline measurement of the effects of current performance; analyse findings; and plan and implement change interventions. For purposes of the QI training, a simple model for QI was derived from the major approaches to QI (lean, six sigma, and so on). To emphasise the need for teamwork on a QI project, stages in the QI model were explained using an acronym, A–TEAM. The stages are described in table 1.
Table 1.
Stages and tools in the A-TEAM model
| Stage | Meaning—the team uses QI tools to: | Tools |
| Agree on care or service to improve, the objective/s of the QI project and stakeholders to involve | Agree by consensus as a team the subject, objective/s and stakeholders for a QI project | Structured brainstorming Consensus-building tools including nominal group process, Delphi process and multivoting Affinity diagram |
| Test the team’s and stakeholders’ commitment to the QI project | Identify the benefits and barriers the team may experience in carrying out the QI project, and ensure they—and key stakeholders—are committed to it | Stakeholder analysis Force-field analysis |
| Establish a baseline by describing or measuring the way things work now and the effects of current practice | Learn exactly how patient care is delivered now and quantitatively or qualitatively measure the effects of current practice on patients, staff or others | Clinical audits of current practice, using evidence-based practice (timing and nature of staff interventions with patients) Run charts of incidents and complaints Surveys of staff and carers Process maps of current practice Analysis of data on length of stay and number of sedatives administered by Team B |
| Analyse how things can be improved and act to change practice | Identify the problems impeding quality care and their root causes, and implement changes to address the problems and achieve desired improvements | Root cause analysis of problems identified by baseline measurement, including fishbone diagram and asking why five times Tree or driver diagram Setting priorities for change interventions Project planning and management |
| Measure again to compare the way things work after change and demonstrate benefits to patients or others | Repeat measurement of the way things work and compare the findings with baseline measurement to see if intended improvements have been achieved | Repeat clinical audits and surveys Continuous run charts of incidents and complaints Continuous capture of data on length of stay and sedatives administered for Team B |
QI, quality improvement.
In the first workshop, teams completed the Agree and Test commitment stages and decided how to establish a baseline for their projects. All staff in Team A participated in the workshop. Because of the size of Team B, a multidisciplinary Steering Group consisting of representatives of all staff groups participated in the first workshop. The workshop was repeated twice for Team B in order to involve all members of staff, particularly in reaching consensus on and testing commitment to the QI project.
In subsequent workshops, held approximately 6–8 weeks apart, teams designed the measurement of current practice, analysed problems and planned change. The workshops also reviewed teams’ progress, provided technical guidance and contributed to resolving problems encountered by the teams. Team B’s Steering Group requested an additional workshop 3 months after the implementation of changes in practice, to share the data gathered from repeat measurement with as many staff as possible, celebrate the team’s success and learn what further actions were needed to sustain the improvements.
The same teacher, an experienced QI facilitator (ND), presented all the workshops and attended all QI meetings with teams. The same teaching materials were used for both teams.
Team performance assessments
The Aston Team Performance Inventory (ATPI) was used to measure team performance of the two teams. The ATPI is a validated comprehensive measure of team performance, which has been used to evaluate the functioning of teams in clinical settings in healthcare organisations.14–18 Team members categorise their performance as a team in 18 dimensions, grouped under team inputs, processes, leadership processes and outputs, by completing online 100 questionnaire items consisting of rating scales. The dimensions in the ATPI are summarised in table 2.
Table 2.
Summary of Aston Team Performance Inventory (ATPI) scales
| Element | Dimension | Items, n | Component description |
| Team inputs | Task design | 11 | Autonomy, task relevance, complete task, feedback, task interdependence |
| Team effort and skills | 8 | Team member motivation, appropriateness of skills, team potency | |
| Organisational support | 11 | Information and communication, training for teamworking, climate for teamworking | |
| Resources | 4 | Resources provided to the team | |
| Team processes | Objectives | 3 | Clarity of, commitment to and agreement about team objectives |
| Reflexivity | 4 | Reflection on performance | |
| Participation | 7 | Decision-making processes, communication, regular meetings, trust, safety and support | |
| Task focus | 6 | Concern with quality, service user focus, constructive debate about task performance and error management | |
| Team conflict | 5 | Task-related and interpersonal conflict | |
| Creativity and innovation | 3 | Practical support for new and improved products and services, and climate for creativity and innovation | |
| Leadership processes | Leading | 4 | Extent to which the team leader sets direction, acquires resources and supports innovation |
| Managing | 8 | Extent to which team leader guides teams towards effective processes, monitors performance, gives helpful feedback, encourages interteam working, and recognises and rewards performance | |
| Coaching | 5 | Availability, concern for individual team members, encouragement and support, and encourages learning from error | |
| Team outputs | Team member satisfaction | 6 | Team member satisfaction with recognition for contribution, responsibility, team member support, influence over decisions, team openness and how conflicts are resolved |
| Attachment | 3 | Feeling of attachment to team and its members | |
| Team effectiveness | 3 | Managerial praise, goal achievement | |
| Interteam relationships | 5 | Cooperation, and lack of conflict, with other teams | |
| Team innovation | 4 | Development of new products, services and ways of working |
Both teams volunteered to complete the ATPI and staff in each team who were willing and available completed the questionnaire approximately 3 months after the start of the QI Team Fellowship. An ATPI accredited facilitator (LW) administered, analysed and interpreted the results for both teams.
Team members’ answers on the ATPI were collated and a mean score for each component was calculated. These scores were compared with scores from a representative sample of comparable teams (norm groups). The analysis involves comparison of scores to the norm group scores to determine the position of the team’s scores: well below average is defined as in the bottom 9% of team scores; below average in the next 24% of team scores; average in the middle 34% of team scores; above average in the next 24% of team scores; or well above average in the top 9% of team scores. The dimension of team conflict is scored in reverse. The analysis also considers the extent to which team members agree in their views on each dimension.
Team coaching
On completion of the team performance assessment at time 1, the ATPI accredited facilitator (LW) met individually with each team leader to discuss the report. The ATPI facilitator and each team leader then presented the findings to the members of each team and discussed the implications with the team members. The ATPI facilitator also provided a team coaching session for each team, and participated in the QI ‘feedback’ workshop that was requested by Team B. No specific method was used to develop team leadership, apart from use of the QI tools to build the team and feedback from the ATPI assessments.
The teams’ QI project proposals were reviewed and approved by their NHS Trusts. The provider of the QI interventions screened the teams’ proposals for any ethical issues prior to the start of the work, using a checklist derived from the literature,19 and determined that there were none. All staff who responded to the ATPI volunteered to complete the questionnaire. The teams both consented to the anonymous presentation of their performance on the ATPI. Thus, it was deemed by the funding organisation that there were no ethical issues associated with the evaluation.
Results
Team A
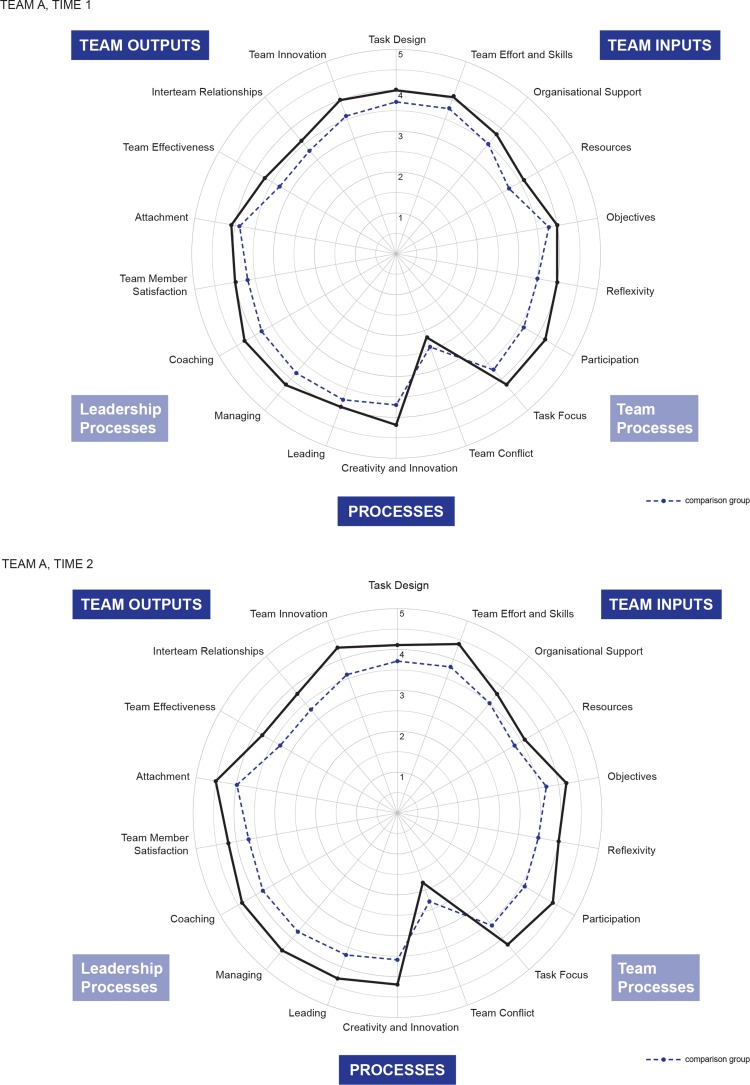
Eight staff in Team A completed the initial ATPI (time 1) and six completed the repeat ATPI (time 2). The spider diagrams in figure 1 show how Team A’s performance compares with the performance of comparable healthcare teams.
Figure 1.
Spider diagrams showing comparison of Team A’s performance with the performance of comparable healthcare Teams.
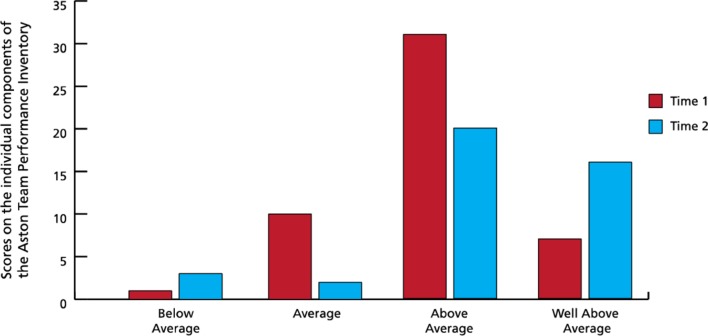
The repeat ATPI scores for Team A showed improvement from the original scores, with a wide gap between Team A’s scores and those of the comparison group for Team A. There was an improvement in scores in 24 of the 52 components of the ATPI. Figure 2 illustrates the shift the team made from average to above and well above average. The increase in below average is due to two ‘reverse’ scores relating to team conflict moving from average to below average, a positive move.
Figure 2.
Bar chart showing improvement in Team A’s performance before and after completion of the quality improvement project. Scores on the individual components of the Aston Team Performance Inventory. Performance of the team in comparison to similar teams before and after participation in the quality improvement project.
On the first measurement, team members reported that they did not need to work interdependently, which changed on the repeat measurement. At the repeat measurement, team members also perceived that the team had clear and shared objectives, and that there was an increased level of commitment to the team’s objectives. At time 2, they reported fewer conflicts about how the team’s tasks should be performed and interpersonal conflicts between team members were reported as infrequent or minor in nature.
The team also had an increased focus on the needs of the patient as well as an increased concern for quality. The team climate improved to be very supportive of creativity and innovation with team members continuing to offer practical support to each other to develop new ideas or ways of working. The team leader was seen as effective in acquiring the resources needed by the team and for the QI project and being more available to the team.
In addition, there was improved satisfaction with the recognition the team members received from colleagues for their contribution to the team and with the way in which conflicts are resolved. Team members reported a stronger level of attachment to the team and team member colleagues. They reported that they were now much more encouraged to work collaboratively with other teams, the biggest area of improvement for Team A. The team had improved levels of cooperation with other relevant teams within the organisation.
On the repeat assessment, Team A was perceived to be a high-performing team by its members, an improvement from the initial ATPI assessment. The largest increases in scores were for working interdependently (from below average to above average) and the team leader’s encouragement of interteam working (from average to well above average). The team scored lower on only four components between the two times of measurement, which included a reduction in the level of challenge to the team due to completing the QI project.
Team A’s performance changes as a team need to be placed in context: Shortly after the start of the QI project, major changes were made in allocation of inpatient beds for the orthopaedic service in the hospital and the roles of some members of the team were under threat for several weeks. In addition, in the same time period, team members were getting ready for and going through a major inspection by the health and social care regulator.
Team B
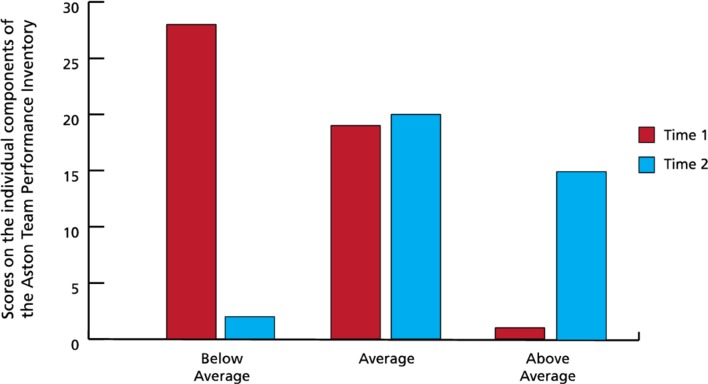
At time 1, 39 of 57 staff in Team B completed the ATPI and 39 of 54 staff completed the repeat ATPI at time 2. The spider diagrams in figure 3 show how Team B’s performance compared with scores by individual subgroups of staff and overall for the team as a whole. Team B’s initial scores on the ATPI were poor; the team generally performed worse than the comparison group. When the results were fed back to the team, team members agreed that the scores reflected how team members felt.
Figure 3.
Spider diagrams showing comparison of Team B’s performance with the performance of comparable healthcare teams.
Figure 4 shows the distribution of scores on individual components of the ATPI, illustrating the shift the team made, removing almost all the below average scores and achieving a significant number of above average ratings. On the repeat ATPI assessment at time 2, Team B generally performed better than the comparable clinical service teams. There was a large improvement in overall team effectiveness. The team members developed greater clarity about their task and established shared objectives. The team’s scores on all aspects of participation, including decision-making, communication and regular meetings, improved. Team conflict also reduced.
Figure 4.
Bar chart showing improvement in Team B’s performance before and after completion of the quality improvement project. Scores on the individual components of the Aston Team Performance Inventory. Performance of the team in comparison to similar teams before and after participation in the quality improvement project.
The team became more patient focused with an increased concern for quality. The team climate was reported to be more supportive of creativity and innovation with team members sometimes offering practical support to each other in developing new ways of working, and being much more supportive of teamworking.
The team leader was seen as being more effective in acquiring the resources needed by the team and providing clear direction in relation to expected team performance. There was improvement in the team leader’s management of the team’s processes, monitoring of performance, encouragement of interteam working and recognition and reward. There was a striking improvement in the ratings for team satisfaction, with team members above average on all measures of satisfaction. Also, team members reported a stronger level of attachment to the team and team member colleagues.
In subgroup analysis, the ratings for trained staff (nurses and therapists) moved from well below average to well above average, when compared with norm groups. The multidisciplinary Steering Group members’ ratings also rose to above average from average; however, the one component on which Steering Group members scored below average indicates that they feel they no longer have a challenging task to perform now that the QI project has been completed. Administrative staff members’ ratings moved from below average to average. Ratings stayed at similar levels for night staff and mental health support workers.
Again, the context for Team B’s performance is relevant: the unit in which the QI project was based was under continuous scrutiny concerning a potential reduction in the number of patients cared for. A few of the mental health support workers who were part of the team when the QI project began left the team to take advantage of better economic opportunities. It is possible that replacement staff did not take part in the QI or team-related workshops or meetings.
Both teams
For both teams, the data from before and after assessments on the ATPI present a compelling picture of significant overall improvement in team-based working. Team A became a high-performing team by the completion of the team’s QI project. Team B, comprising more than 50 staff many of whom are support workers, began as a poorly performing team. Following participation in the QI experience, they reported above average satisfaction, a high positive profile in their organisation and a large overall improvement in team effectiveness.
Both teams reported that they perceived they no longer have a challenging task to work on because they achieved the improvements they intended in their QI projects.
Discussion
Involvement of a multidisciplinary team and skilled facilitation of teamwork on a QI project have been recognised as key factors in the success of QI in healthcare organisations. If teamwork is key to achieving improvements in patient care, some questions emerge for healthcare organisations. Can an assumption be made that professionals working in clinical settings function effectively as teams? What are the processes that produce successful teamworking in clinical environments? How does participation in a QI project work to change the way a team performs?
In a large-scale study of team-based working in NHS Trusts using findings from a national NHS staff survey, Carter and colleagues16 reported that nearly 90% of NHS staff said they worked in a team. When West’s20 definition of a team (clear shared team objectives; role interdependence and clarity; meeting regularly to review and improve performance) was applied through survey questions, only 56% of staff respondents could be classified as working in a well-structured ‘real team.’ The research team concluded that comparatively large numbers of staff in NHS Trusts work in poorly functioning ‘pseudo’ teams, that is, groups where there is no attention to collective performance.21
A number of processes that underpin teamworking have been identified from synthesis of the literature.17 These processes include: a shared sense of purpose; pooling of resources; collaboration and coordination; efficient, open and equitable communication; shared responsibility and influence; support and value; critically reviewing performance and decisions; generating and implementing new ideas; individual learning; leadership; tactical communication; role blurring; and team behavioural norms. A group of staff working together to achieve a well-defined improvement in the quality of patient care is likely to experience many if not all of the processes identified.
Healthcare organisations are routinely expecting individual members of staff or small teams to work on QI projects, using one of the well-established approaches to QI including the PDSA cycle, lean, six sigma or re-engineering. Some teams are successful in achieving intended improvements; some are not and no one approach to QI is more effective than any other approach.4 A question is, therefore, what made the approach to QI used with Team A and Team B effective both in improving teamwork and in achieving important improvements in patient care.
Traditional approaches to QI all begin with a problem to solve, a service to improve or a change to implement. They do not begin with the team doing the work or do not explicitly recognise the need for a functional team to carry out the work. An assumption is often made that a group of individuals will be motivated to carry out the QI-related work. What is unique about the QI model used with Team A and Team B is that the QI process started with the team itself. The first stages in the A-TEAM model taught the team members how to work together to reach consensus as a team on the improvement subject and objective. The second stage taught the team members to test their own commitment and the commitment of their key stakeholders to the team’s QI project.
We believe that this investment in developing teamworking skills within the team itself contributed significantly to the way the teams worked on their QI projects. West’s characteristics of a team became embedded in the QI process through the A-TEAM model: the team members learnt how to develop a shared objective; that they could not achieve the objective without working interdependently; that they needed to have clear roles within the team, including for the leader; and how to use meetings to review and advance their progress on achieving the objective.
Both teams achieved their improvement objectives with both quantitative and qualitative evidence of the effects of the changes in practice they made. Examples included: significantly improved compliance with evidence-based practice relating to patients with dementia; reduction in behaviour-related incidents involving patients with dementia; improved staff and carer satisfaction with services provided; and for Team B, reduction in total length of stay and use of sedative medications. In addition, the measures of team performance of the two teams at different points in time show that the QI process itself the teams experienced influenced positively how they perform as teams. The study indicates the need for more research on the relationship between team development as part of the QI process itself and the longer term functioning of teams in clinical settings.22
Limitations
This study has a number of limitations. It involved only two teams in two NHS Trusts. The work extended over only 12 months, and data were not available to confirm if the improvements in the quality of care were sustained over a longer time. It is unknown what the effects would be with substantial turnover in staff or leaders of the teams.
Although the two teams were focusing on care for the same type of patients, that is, patients with dementia, the nature of the services provided by the teams was substantially different: Team A provided care for patients having orthopaedic surgery on an acute orthopaedic surgical ward; Team B provided care for female elderly patients with a range of mental health conditions, including dementia. The NHS Trusts where the services are located are in different cities and have somewhat different population profiles.
The QI Team Fellowship was funded for 1 year only; therefore, it was not possible to follow the teams over a longer time period to confirm whether or not the improvements achieved both in care and in teamwork were sustained over time. Both teams received awards from their Trusts months after completion of the study, based on the evidence of improvements the teams achieved; however, it is not known if the improvements have been sustained long term. Also, the staff who make up teams in a workplace change, and the effect of staff turnover on team performance is unknown.
Because the study is limited to two teams providing care to patients with dementia, the findings cannot be generalised to other teams providing care to other types of patients in other care settings.
Conclusion
This study demonstrates that a structured team-based learning approach to QI that emphasises development of the team as part of the process can have effects over at least 1 year on the performance of two teams in their clinical settings, as measured by the ATPI validated team performance tool. It is notable that on repeat measurement, both teams perceived a reduction in the level of challenge to the team due to completing their QI projects. It is unknown if the findings can be generalised to other teams or other settings, or if other approaches to QI would have the same effect.
The study indicates the need for more research on the relationship between team development as part of the QI process itself and the longer term performance of teams in clinical settings.
Acknowledgments
Fleur Kitsell, PhD, Health Dean, and Siobhan O’Donnell, LLB and MA, Patient Safety and Quality Improvement Lead, Health Education England, Wessex reviewed a draft of the paper and made valuable suggestions and comments.
Footnotes
Contributors: ND provided the QI interventions with the teams and drafted this paper. LW worked with the teams to complete the ATPI assessments and provided team coaching for both teams, prepared a report on the team’s pre/post-QI intervention performance on the ATPI and provided comments on the draft of this paper.
Funding: The quality improvement interventions and the team assessment work with the teams described was supported by Health Education England, Wessex.
Competing interests: The authors are employed by commercial entities that provide consultancy and training on quality improvement and teamworking.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: Teams agreed for the data to be presented as long as the teams are anonymous.
Patient consent for publication: Not required.
References
- 1.Australian Safety and Quality Framework for Health Care. Putting the framework into action: Getting started. Australian Commission on Safety and Quality in Healthcare. https://www.safetyandquality.gov.au/wp-content/uploads/2011/01/ASQFHC-Guide-Healthcare-team.pdf (accessed 16 Jan 2019).
- 2.Shared commitment to quality from the National Quality Board. Five year forward view. https://www.england.nhs.uk/wp-content/uploads/2016/12/nqb-shared-commitment-frmwrk.pdf (accessed 16 Jan 2019).
- 3.Department of Health and Human Services. The patient safety and quality improvement act of 2005. https://www.hhs.gov/hipaa/for-professionals/patient-safety/patient-safety-quality-improvement-act-2005/index.html?language=es (accessed 16 Jan 2019).
- 4.Babich LP, Charns MP, McIntosh N, et al. Building systemwide improvement capability: does an organization’s strategy for quality improvement matter? Qual Manag Health Care 2016;25:92–101. 10.1097/QMH.0000000000000089 [DOI] [PubMed] [Google Scholar]
- 5.Hughes RG. Tools and strategies for quality improvement and patient safety. Section 6, Chapter 44 in Hughes RG, editor. Patient Safety and Quality: An Evidence-Based Handbook for Nurses: Vol. 3. AHRQ Publication No. 08-0043. Rockville, MD: Agency for Healthcare Research and Quality, US Department of Health and Human Services, 2008. [Google Scholar]
- 6.Brandrud AS, Schreiner A, Hjortdahl P, et al. Three success factors for continual improvement in healthcare: an analysis of the reports of improvement team members. BMJ Qual Saf 2011;20:251–9. 10.1136/bmjqs.2009.038604 [DOI] [PubMed] [Google Scholar]
- 7.Mills PD, Weeks WB. Characteristics of successful quality improvement teams: lessons from five collaborative projects in the VHA. Jt Comm J Qual Saf 2004;30:152–62. 10.1016/S1549-3741(04)30017-1 [DOI] [PubMed] [Google Scholar]
- 8.Santana C, Curry LA, Nembhard IM, et al. Behaviors of successful interdisciplinary hospital quality improvement teams. J Hosp Med 2011;6:501–6. 10.1002/jhm.927 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Stetler CB, Legro MW, Rycroft-Malone J, et al. Role of "external facilitation" in implementation of research findings: a qualitative evaluation of facilitation experiences in the Veterans Health Administration. Implement Sci 2006;1:23 10.1186/1748-5908-1-23 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Thor J, Wittlöv K, Herrlin B, et al. Learning helpers: how they facilitated improvement and improved facilitation — lessons from a hospital-wide quality improvement initiative. Qual Man Health Care 2004;13:60–74. [DOI] [PubMed] [Google Scholar]
- 11.White DE, Straus SE, Stelfox HT, et al. What is the value and impact of quality and safety teams? A scoping review. Implement Sci 2011;6:97 10.1186/1748-5908-6-97 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sherrington R, Baldwin G, Cheesman A, et al. What matters most for those living with dementia during their stay on an orthopaedic unit: a quality improvement programme. Poster session presented at: The 27th Annual National Forum on Quality Improvement in Health Care. Orlando, FL, 2015. [Google Scholar]
- 13.Clarke C, West J. Improving patient safety through increased therapeutic activity and person centered care. Poster session presented at: The International Forum on Quality and Safety in Health Care. London, UK, 2017. [Google Scholar]
- 14.The Aston Team Performance Inventory. https://www.affinaod.com/wp-content/uploads/2015/01/ATPI-sample-report.pdf/(accessed 16 Jan 2019).
- 15.Borrill CS, Carletta J, Caret AJ, et al. The effectiveness of health care teams in the National Health Service Report. Birmingham: University of Aston, 2000. [Google Scholar]
- 16.Carter M, West M, Dawson J, et al. Developing team-based working in NHS Trusts. Summary Report, June 2009. Birmingham: Aston University. [Google Scholar]
- 17.Harris R, Sims S, Hewitt G, et al. Interprofessional teamwork across stroke care pathways: outcomes and patient and carer experience. National Institute for Health Research Service Delivery and Organisation Programme, February 2013. http://eprints.kingston.ac.uk/id/eprint/25627 (accessed 16 Jan 2019).
- 18.West M, Baker R, Dawson J, et al. Quality and safety in the NHS: evaluating progress, problems and promise. https://www.lancaster.ac.uk/media/lancaster-university/content-assets/documents/lums/cphr/quality-safety-nhs-e.pdf (accessed 16 Jan 2019).
- 19.Dixon N. Guide to managing ethical issues in quality improvement and clinical audit, February 2017, Healthcare Quality Improvement Partnership. https://www.hqip.org.uk/resource/guide-to-managing-ethical-issues-in-quality-improvement-or-clinical-audit-projects/#.XD8CR_zgoyk (accessed 16 Jan 2019).
- 20.West M. Effective teamwork: practical lessons from organizational research. Oxford: Blackwell/British Psychological Society, 2004. [Google Scholar]
- 21.Katsenbach JR, Smith DK. The Wisdom of teams. creating the high-performance organization. Boston: Harvard Business School Press, 1993. [Google Scholar]
- 22.Rowland P, Lising D, Sinclair L, et al. Team dynamics within quality improvement teams: a scoping review. Int J Qual Health Care 2018;30:416–22. 10.1093/intqhc/mzy045 [DOI] [PubMed] [Google Scholar]