Abstract
Telehealth interventions have the potential to deter repeated detoxification episodes and improve outcomes. Using a sample of 298 detoxification inpatients, this randomized controlled trial compared Enhanced Telephone Monitoring (ETM) to usual care (UC) on the primary outcome of reducing subsequent detoxification, and secondary outcomes of linking patients to addiction treatment and mutual-help, and patients’ experience of improved substance use and mental health outcomes. At the 3-month follow-up (i.e., at the end of the ETM intervention), compared to UC patients, ETM patients were significantly less likely to have received additional inpatient detoxification, but no more likely to have participated in 12-step groups or received outpatient addiction treatment. Even so, ETM patients had better alcohol, drug, and mental health outcomes. In contrast, at the 6-month follow-up, patients in ETM and UC generally did not differ on primary or secondary outcomes. Findings suggest that ETM deters additional detoxification episodes while the intervention is ongoing, but not after the intervention ends. Because telephone monitoring is low-intensity and low-cost, its extension over time may help reduce repeated detoxifications.
Keywords: detoxification, alcohol, opioids, telephone monitoring, treatment, mutual-help
1. Introduction
Detoxification services are likely to be ineffective for preventing relapse to substance use and repeated detoxifications if they are not followed by addiction treatment. However, many patients do not receive addiction treatment in the month or year following detoxification (Haley, Dugosh, & Lynch, 2011; Timko, Gupta, Schultz, & Harris, 2016). Telehealth interventions have the potential to deter (i.e., reduce the likelihood of) repeated detoxification episodes by facilitating use of treatment and 12-step groups to improve outcomes, but have not been evaluated with detoxification inpatients. The purpose of this study was to evaluate a telephone monitoring intervention with regard to reducing subsequent detoxification, linking patients to addiction treatment and mutual-help, and patients’ experience of improved substance use and mental health outcomes.
1.1. Treatment and outcomes among detoxification inpatients
Inpatient detoxification is one of the most expensive types of care in terms of costs per day, and is not considered addiction treatment (Haley et al., 2011; Spear, 2014). It accounts for 22% of yearly admissions to publicly-funded addiction treatment facilities and is frequently requested by Emergency Department patients (Substance Abuse and Mental Health Services Administration [SAMHSA], 2016). Inpatient detoxification delivers medically-supervised withdrawal from a substance of dependence to reduce the severity of withdrawal symptoms and serious medical complications. It is necessary because withdrawal from alcohol (and other sedative-hypnotics) that is not medically managed may lead to autonomic instability, seizures, delirium, or death. Opioid withdrawal syndrome poses nearly no mortality risk but can be protracted with intense symptoms, and the risk from overdose is significant for patients who relapse after withdrawal because of loss of opioid tolerance (VA/DoD, 2015).
Many individuals exhibit a pattern of repeated detoxifications with little intervening abstinence (Carroll, Triplett, & Mondimore, 2009). Studies of publicly-funded inpatient detoxification found that 20%−25% of patients were readmitted for detoxification within six months (Mark, Vandivort-Warren, & Montijano, 2006). However, patients who received treatment within one month of detoxification discharge were significantly less likely to be readmitted for detoxification and had a significantly longer time until a detoxification readmission (Mark et al., 2006). In the US, a survey of state Medicaid programs found that the average rate of readmission of Medicaid beneficiaries to detoxification within one year was 47%, with a range of 23%−93% across states (Stein, Kogan, & Sorbero, 2009). Similarly, in the Netherlands, 51% of a sample of detoxification inpatients were readmitted within one year (Van den Berg, Van den Brink, Kist, Hermes, & Kok, 2015).
Research literature reviews estimate that only 30%−35% of detoxification patients obtain some form of addiction treatment following detoxification (Haley et al., 2011), although rates vary widely (Timko, Below, Schultz, Brief, & Cucciare, 2015). For example, one study found that 41% of detoxification inpatients had entered treatment, and 33% had attended mutual-help, at a six-month follow-up (Chutuape, Jasinski, Fingerhood, & Stitzer, 2001). In California, only 11% of all opioid detoxification episodes were followed by admission to maintenance treatment within 14 days (Nosyk et al., 2014). In the Veterans Health Administration (VA), 50% of alcohol and opioid detoxification inpatients entered addiction treatment (outpatient and/or residential) within one month of discharge (Timko et al., 2016).
Substance use soon after detoxification is the norm when detoxification is not followed by treatment or mutual-help. Among people receiving detoxification who did not subsequently enter addiction treatment, between 73%−88% maintained abstinence for 1–3 days (Bailey, Herman, & Stein, 2013; Chutuape et al., 2001; Katz et al., 2004), 12%−45% maintained abstinence for one month (Bailey et al., 2013; Broers, Giner, Dumont, & Mino, 2000; Chutuape et al., 2001); 12%−23% maintained abstinence for six months (Broers et al., 2000; Day & Strang, 2011); and 10% maintained abstinence for one year (Bailey et al., 2013). Across five states in the US, detoxification patients who received addiction treatment within 14 days were less likely to be readmitted to detoxification in the same year than those who did not receive addiction treatment (for example, in Connecticut, 14% with treatment were readmitted, versus 24% without treatment; Lee et al., 2014). Indeed, patients who sustain prolonged abstinence and related positive outcomes after detoxification are distinguished by having been in treatment and/or mutual-help (Carroll et al., 2009; Chutuape et al., 2001; Ford & Zarate, 2010; Ivers et al., 2017).
Studies have examined how to engage detoxification patients in subsequent treatment to reduce the occurrence of repeated detoxification episodes and increase beneficial outcomes (Carroll et al., 2009). Strategies include detoxification staff familiarizing patients, during the detoxification episode, with the addiction treatment program patients will later enter (e.g., staff accompany patients on a shuttle bus to meet treatment counselors), and providing ongoing, in-person intensive case management (Chutuape et al., 2001; McLellan Weinstein, Shen, Kendig, & Levine, 2005; Zaller, Thurmond, Brett, Carleton, & Rich, 2006). Detoxification inpatients in an accompanied condition were more likely to enter treatment than those in usual care (76% vs. 24%; Chutuape et al., 2001). Compared to usual care, intensive case management of repeat detoxification inpatients showed a 70% increase in treatment entry and significantly longer treatment stays (McLellan et al., 2005; Zaller et al., 2006).
Unfortunately, these efficacious interventions are not feasible to implement routinely in many health care systems because they require substantial staff resources, and treatment program choice may be uncertain at the time of discharge or distant from the detoxification setting. In addition to often being infeasible, such resource-intensive approaches may not be necessary to reduce repeated detoxifications. With this in mind, we tested an approach with detoxification inpatients that delivered and evaluated a telehealth intervention, Enhanced Telephone Monitoring (ETM).
1.2. Telephone Monitoring
Telephone monitoring was designed to improve engagement in continuing care and outcomes for addiction patients who had attained abstinence in intensive treatment (Stout, Rubin, Zwick, Zywiak, & Bellino, 1999). It generally consists of one in-person session for orienting patients to the protocol, followed by regular, brief telephone contacts. It has been demonstrated as feasible (patients receive calls when assigned to do so), facilitating participation in addiction continuing care and 12-step programs (Hubbard et al., 2007; McKay et al., 2010b; Mensinger, Lynch, Tenhave, & McKay, 2007; Zanjani, Miller, Turiano, Ross, & Oslin, 2008), and a cost-effective approach to reduce substance use (McCollister, Yang, & McKay, 2016). In contrast to these robust findings, a randomized controlled trial in which addiction intensive outpatients were assigned to six months of telephone monitoring or usual in-person continuing care found that telephone-monitored patients achieved better substance use and psychiatric outcomes at 3-month, but not at 12-month, follow-up (McKellar et al., 2012).
Importantly, patients in the completed studies were already engaged in the addiction treatment system. In contrast, detoxification patients may not be fully aware of addiction treatment options or convinced that they can benefit from treatment. Detoxification patients, once the crisis that led them to detoxification has been alleviated, often believe that they are physically and psychologically ready to use alcohol and drugs again (Carroll et al., 2009). For patients seen outside of addiction treatment settings, an intervention to decrease repeated detoxification needs to explicitly target motivation and commitment to change substance use and engage with resources for help (Brown, Saunders, Bobula, Mundt, & Koch, 2007), and also prompt and reward desired behavior changes (Lash et al., 2007). Accordingly, the intervention evaluated in this study, ETM, added components of Motivational Interviewing (Miller & Rollnick, 2002) and Contracts, Prompts, and Reinforcements (Lash et al., 2007) to standard telephone monitoring.
Motivational Interviewing, a patient-centered, directive method for enhancing readiness for change (Miller & Rollnick, 2002), facilitates detoxification inpatients’ entry into and engagement with addiction treatment and mutual-help and better substance use and related outcomes (Kahler et al., 2004; Schilling, El-Bassel, Finch, Roman, & Hanson, 2002; Vederhus, Timko, Kristensen, & Clausen, 2014). Similarly, Contracts, Prompts, and Reinforcements has been shown to help patients in addiction residential treatment participate in continuing care and mutual-help after discharge, maintain abstinence, and reduce substance-related problems (Burden, Parker, Williams, & Lash, 2017). It uses continuing care contracts (between counselors and patients, outlining a commitment to treatment and mutual-help, and showing the better abstinence rates obtained with getting help), prompts (personal letters; telephone reminders to facilitate attendance at treatment sessions and mutual-help, and encourage returning after missed sessions), and social reinforcers (letters of congratulations, certificates, and medallions) (Lash et al., 2013). Altogether, findings for telephone monitoring, Motivational Interviewing, and Contracts, Prompts, and Reinforcements suggest the potential benefits of ETM for detoxification inpatients.
1.3. Present Study
The present randomized controlled trial was based on the premise that an inpatient detoxification episode should be a gateway to addiction treatment and mutual-help to reduce repeated detoxifications and improve outcomes. We expected that ETM, compared to usual care (UC), would help patients in inpatient detoxification reduce subsequent inpatient detoxifications, utilize addiction treatment and 12-step mutual-help groups following discharge, and improve outcomes at 3 and 6 months post-detoxification. Specifically, the primary outcome was whether additional inpatient detoxification services were received at follow-ups. To enhance the clinical usefulness of the findings, additional outcomes assessed participation in outpatient treatment and mutual-help groups, substance use and mental health outcomes, and self-efficacy to change substance use.
2. Material and methods
2.1. Sample and procedures
Patients entering one of two psychiatry units within the same health care system were included on the basis of (1) undergoing detoxification for alcohol and/or opioid dependence; and having (2) sufficient cognitive functioning to understand study procedures (i.e., able to answer the Montreal Cognitive Assessment’s section on Orientation; Nasreddine et al., 2005), (3) access to a cell or land line telephone when not hospitalized, and (4) at least one person who would know of their whereabouts after discharge, for whom contact information was available. After receiving an introduction to the study, participants signed an informed consent form. All study procedures were approved by the VA Central Institutional Review Board. Patients who provided informed consent completed the baseline interview during their second day on the unit. The 298 participants entered inpatient detoxification for withdrawal from alcohol (68%, n=202), opioids (11%, n=32), or both (21%, n=64). After the baseline interview, participants were randomly assigned to condition (ETM or UC) using random numbers generated by a computer program.
Regarding follow-ups, the research assistant, blinded to patients’ condition assignment, collected self-report data from patients by telephone at three months post-baseline (which was upon completion of the intervention for patients in the ETM condition) and at three months after the three-month follow-up (i.e., six months post-baseline). We used an intent-to-treat design and so followed all participants irrespective of participation in the intervention. Follow-up assessments were conducted by telephone because not all patients resided in close geographical proximity to the inpatient facility.
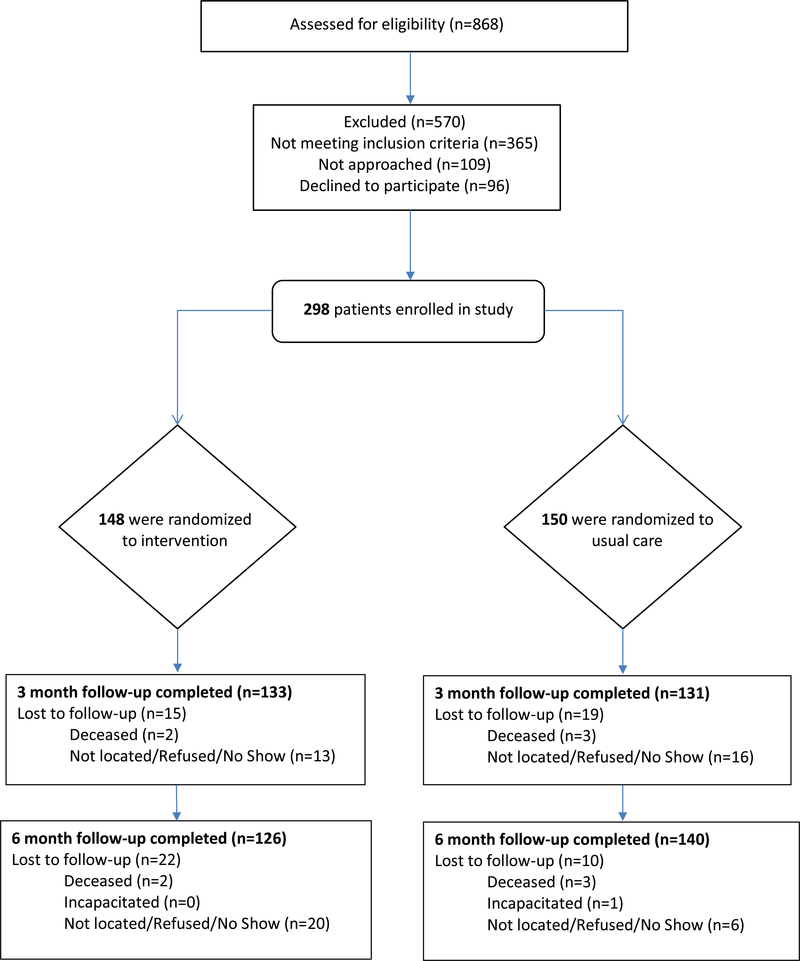
Figure 1 summarizes the flow of patients through the trial. Of the 868 patients who were assessed for eligibility, 298 were randomly assigned. Excluded were 570 patients because of refusal (n=96), ineligibility (n=365), or not having been approached about the study (e.g., were discharged before they could be approached; n=109). In all, 150 patients were randomly assigned to UC; of these, 131 (89.1% of those still alive) were followed at three months, and 140 (95.8% of those still alive and not incapacitated) were followed at six months. In addition, 148 patients were randomly assigned to the ETM condition; 133 (91.9% of those still alive) were followed at three months, and 126 (86.3% of those still alive) were followed at six months. Baseline comparisons on demographic characteristics of patients followed or not followed at 3 and 6 months post-baseline found no significant differences.
Fig. 1.
Flow of patients through the trial.
2.2. Conditions
UC
All patients, regardless of condition, received usual inpatient detoxification which consisted of medically supervised withdrawal. The health care system had available post-detoxification addiction outpatient and residential specialty care and pharmacotherapy. Study participants, as part of UC, were offered by detoxification staff a referral to or an appointment with addiction treatment services, if they chose to consider seeking treatment.
ETM
Patients assigned to the ETM condition received usual care plus the ETM intervention. ETM consisted of one 50-minute individual session during the inpatient stay and 12 weekly 15-minute telephone sessions from the same TeleCoach who conducted the in-person session.
The in-person session enhanced procedures in McKay, Van Horn, and Morrison’s (2010a) manual for implementing telephone monitoring with addiction patients transitioning from more to less intensive treatment. It provided an orientation to the telephone monitoring protocol, which was enhanced by Motivational Interviewing and Contracting. Motivational components included the TeleCoach’s empathy, conveying the patient’s responsibility for change, and supporting the patient’s self-efficacy to make changes, while addressing post-detoxification engagement in addiction treatment (i.e., behavioral treatments and/or medications in residential or individual or group outpatient settings), mutual-help, and their combination. Participants completed a contract containing two main elements: information that attending treatment and mutual-help increases the chances of remaining abstinent; and a stated intention to attend addiction treatment and/or mutual-help, with as much specificity as the patient could provide regarding these plans. Participants were informed of ETM’s reinforcers for beginning and participating in treatment and mutual-help, and given The Next Step Toward a Better Life (SAMHSA, 2014), which informs people completing detoxification what to expect physically and psychologically post-discharge, encourages use of treatment and mutual-help, and provides tools for remaining abstinent.
Telephone sessions also enhanced procedures in the McKay et al. (2010a) protocol. Patients were expected to complete one 15-minute telephone call per week for 12 weeks. When the patient failed to answer a call, the TeleCoach made at least two more attempts at that scheduled contact, and when successful, the initial non-response was discussed. Patients received reinforcements for completing 6 and then 12 phone calls (i.e., tote bags, key chains, collapsible cups, wristbands). During each telephone session, patients completed the Risk Assessment Worksheet (McKellar et al., 2012) about substance use and compliance with treatment and mutual-help since the last call. Telephone sessions were enhanced with prompts and reinforcements. The TeleCoach checked whether participants had attended planned treatment sessions and mutual-help meetings, and reminded them to return even if they had missed a session or meeting. Participants received social reinforcements for attending treatment and mutual-help, i.e., a personal congratulations letter from the TeleCoach for entering treatment and attending the first post-detoxification mutual-help meeting, certificates for abstinence milestones (2, 4, and 8 weeks), and a certificate plus medallion for abstinence through 12 weeks.
Of the 148 detoxification inpatients assigned to ETM, 95% (n=140) completed at least one telephone session. The mean number of completed calls was M=7.5 (SD=3.2). Two Masters-level TeleCoaches received regular supervision from doctoral-level, licensed clinicians that included review of sessions and feedback on adherence to the manualized content. TeleCoaches and the supervising clinicians had formal Motivational Interviewing training and experience. During the study, to assess ETM fidelity, all in-person and telephone sessions were audiotaped (with appropriate consent), the first 15 in-person and telephone sessions for each Coach were evaluated against a protocol checklist, and the Coach was provided corrective feedback. Then, eight sessions were reviewed at random each month to ensure ongoing fidelity of the intervention.
At the end of the study, for 20% of a random sample of participants’ intervention sessions, fidelity monitoring was conducted by two independent trained coders using the Motivational Interviewing Treatment Integrity Code (MITI 4; Moyers, Rowell, Manuel, Ernst, & Houck, 2016). Coders had excellent inter-rater agreement on global scores for Softening Sustain Talk (a technical component), Partnership (a relational component), and Empathy (relational) (intraclass correlation coefficients [ICC] = .82, .80, and .81 respectively), and fair agreement on Cultivating Change Talk (technical) (ICC =.53). On the 1 (low) to 5 (high) scale, TeleCoaches were rated as relatively high on each Motivational Interviewing component: Softening Sustain Talk (M=3.6, SD=0.6), Partnership (M=4.1, SD=0.5), Empathy (M=4.1, SD=0.2) and Cultivating Change Talk (M=4.3, SD=0.4). The same sessions were rated by the same coders for adherence to the intervention using the protocol checklist. Inter-rater agreement on the checklist was excellent (ICC = .82). Of 10 components on the checklist, 5 were provided to 100% of intervention participants, 4 were provided to 71%−91%, and 1 was provided to 64%. Thus, overall, the intervention was provided in a manner adherent to the protocol.
2.3. Measures
At baseline, patients were asked whether they had received previous inpatient detoxification (no or yes). At follow-ups, patients were asked whether they had received inpatient detoxification since the previous interview (in the past three months; no or yes). This was the primary outcome. All other outcomes assessed were secondary.
At baseline, patients were asked whether they had received previous outpatient treatment for alcohol and/or drugs in their lifetime and in the past 30 days (no or yes). At follow-ups, patients were asked whether they had received outpatient treatment for alcohol and/or drugs since the last interview (in the past three months; no or yes). At baseline and follow-ups, patients were asked whether they had attended a 12-step meeting in the past three months (no or yes) and if so, how many meetings.
At baseline and follow-ups, we used the Addiction Severity Index (ASI; McLellan, Cacciola, Alterman, Rikoon, & Carise, 2006) to assess alcohol use, drug use, and psychiatric severity. In each area, items measured the number, extent, and duration of symptoms in the past 30 days. ASI composite scores were produced from sets of items that were standardized and summed to provide internally consistent evaluations of patient status in the problem areas (McLellan et al., 2006). They range from 0 to 1, with higher scores indicating poorer outcomes. In addition, to ensure the clinical utility of findings, we report responses to the ASI items referring to the past 30 days that assessed number of days drank alcohol (0–30), number of days used opioids (0–30), experienced serious thoughts of suicide (that is, seriously considered a plan for taking own life; no or yes), and attempted suicide (no or yes).
We also used the Brief Addiction Monitor (required in VA for measurement based substance use disorder care) at baseline and follow-ups (Cacciola et al., 2013; CESATE, 2010), which yields two composite scores referring to the past 30 days. Substance use is the sum of three items, i.e., number of days drank alcohol, had at least 5 drinks (men) or at least 4 drinks (women), and used any illegal/street drugs or abused any prescription medications (for each, 0=0, to 4=16–30 days); scores range from 0 to 12. Risk factors for substance use is the sum of six items, e.g., physical health (0=excellent, 4=poor), number of nights having trouble falling or staying asleep (0=0, 4=16–30 days), in any situations or with any people that might increase risk for using alcohol or drugs (0=0, 4=16–30 days); scores range from 0 to 24.
At baseline and follow-ups self-efficacy was assessed with the Brief Situational Confidence Questionnaire (Breslin, Sobell, Sobell, & Agrawal, 2000). Eight items asked patients to rate their level of confidence in resisting drinking and using drugs as a response to different types of situations (e.g., unpleasant emotions, social pressure to drink/use), and then responses were averaged such that higher scores indicate more self-efficacy (Cronbach’s alpha = .91, .92, and .91 at baseline and 3 and 6 months, respectively; scores range from 0 to 100).
2.4. Analysis Plan
We first compared patients randomly assigned to ETM or UC on baseline demographic characteristics and primary and secondary outcomes. We then conducted logistic regressions (for dichotomous dependent variables assessing detoxification, treatment, and mutual-help) or analyses of covariance (ANCOVAs, for the remaining dependent variables) to compare the ETM and UC groups on primary and secondary outcomes at the 3- and 6-month follow-ups. Covariates were the baseline value of the outcome and the inpatient detoxification unit.
3. Results
Table 1 shows that in comparisons of patients randomly assigned to the ETM or UC condition, patients did not differ on characteristics assessed at baseline. Of the full sample, participants were mostly male (95.0%, n=283), white (76.0%, n=225), unmarried (81.9%, n=244), unemployed (66.1%, n=197), and housed (85.1%, n=245). The mean age was 50.1 years old (SD=13.2), and the mean years of education was 13.1 (SD=1.8). The majority of participants had previously received inpatient detoxification (98.0%, n=290) and outpatient addiction treatment (60.3%, n=179). Most had attended a 12-step meeting in the past three months (53.7%, n=160), but few had attended outpatient addiction treatment in the past 30 days (10.1%, n=30). In the past 30 days, participants had used alcohol a mean of 15.7 days (SD=10.8), and had used opioids a mean of 5.3 days (SD=11.3). Among those who used alcohol at least one day in the past 30 days, the mean number of days was 17.7 (SD=9.7). Among those who used opioids at least one day in the past 30 days, the mean number of days was 20.1 (SD=13.7). About one-third of participants reported having serious thoughts of suicide in the past 30 days (32.3%, n=96), and one-tenth reported having attempted suicide in the past 30 days (10.1%, n=30).
Table 1.
Baseline characteristics of Enhanced Telephone Monitoring (ETM; n=148) and Usual Care (UC; n=150) groups.
| Demographics | ETM | UC | X2/t | p |
|---|---|---|---|---|
| Male (%, n) | 95.3 (141) | 94.7 (142) | .06 | .812 |
| White (%, n) | 75.7 (112) | 76.4 (113) | .02 | .892 |
| Age (M, SD) | 51.4 (12.9) | 48.9 (13.5) | −1.68 | .095 |
| Married (%, n) | 18.9 (28) | 17.3 (26) | .13 | .722 |
| Years education (M, SD) | 13.0 (1.8) | 13.3 (1.9) | .98 | .329 |
| Employed (%, n) | 31.1 (46) | 36.7 (55) | 1.04 | .308 |
| Homeless (%, n) | 16.1 (23) | 13.8 (20) | .30 | .585 |
| Detoxification, mutual-help and treatment | ||||
| Detoxification, lifetime (%, n) | 98.0 (145) | 98.0 (145) | .00 | 1.00 |
| Attended 12-step meeting (%, n; past 3 months) | 54.7 (81) | 52.7 (79) | .13 | .721 |
| Number of meetings (M, SD) (past 3 months) | 7.0 (14.3) | 8.6 (15.8) | .62 | .533 |
| Treatment, lifetime (%, n) | 61.5 (91) | 59.1 (88) | .18 | .669 |
| Treatment, 30 days (%, n) | 10.8 (16) | 9.3 (14) | .18 | .672 |
| Addiction Severity Index composite | ||||
| Alcohol severity (M, SD) | .564 (.290) | .565 (.290) | .04 | .966 |
| Drugs severity (M, SD) | .134 (.151) | .125 (.157) | −.51 | .613 |
| Psychiatric (M, SD) | .479 (.226) | .490 (.236) | .40 | .692 |
| Addiction Severity Index items (past 30 days) | ||||
| Days used alcohol (M, SD) | 16.0 (10.7) | 15.3 (10.8) | −.507 | .612 |
| Days used opioids (M, SD) | 5.1 (11.0) | 5.6 (11.7) | .425 | .671 |
| Serious ideas suicide (%, n) | 32.8 (47) | 32.9 (49) | .04 | .835 |
| Attempted suicide (%, n) | 10.1 (15) | 10.1 (15) | .00 | .984 |
| Brief Addiction Monitor composite | ||||
| Alcohol and drug use (M, SD) | 7.2 (3.1) | 7.0 (2.9) | −.48 | .641 |
| Risk factors (M, SD) | 15.0 (4.6) | 15.6 (4.3) | 1.13 | .257 |
| Self-efficacy | ||||
| Confidence (M, SD) | 62.1 (29.0) | 58.4 (26.7) | −1.16 | .247 |
Table 2 shows comparisons of patients assigned to ETM or UC at the 3-month follow-up. Compared to patients in UC, patients in the ETM condition were significantly less likely to have received additional inpatient detoxification. However, they were no more likely to have participated in 12-step groups or to have received outpatient addiction treatment. Even so, patients in the ETM condition had better alcohol and drug use outcomes as assessed by the ASI composites of alcohol and drug use severity, the ASI items measuring number of days of alcohol and opioid use in the past 30 days, and the BAM composites tapping alcohol and drug use and risk factors for substance use. In addition, patients in the ETM condition had a better psychiatric outcome as assessed by the ASI composite. Further, patients in the ETM condition had more self-efficacy in terms of having more confidence to resist substance use.
Table 2.
Comparisons of ETM and UC groups on outcomes at 3- and 6-month follow-ups.
| 3-month follow-up | 6-month follow-up | |||||
|---|---|---|---|---|---|---|
| Primary outcome | ETM | UC | B/F (p) | ETM | UC | B/F(p) |
| Inpatient detoxification (%, n) | 24.43 (32) | 38.60 (51) | −.670 (.014) | 26.02 (33) | 33.33 (47) | −.357 (.197) |
| Secondary outcomes | ||||||
| Mutual-help and treatment | ||||||
| Attended a 12-step meeting (%, n) | 72.09 (96) | 66.41 (87) | −.372 (.218) | 53.28 (67) | 63.97 (90) | −.553 (.043) |
| Number 12-step meetings (M, SD) | 22.46 (24.48) | 17.93 (34.02) | 1.56 (.213) | 18.63 (32.36) | 20.81 (34.21) | 0.29 (.592) |
| Outpatient treatment (%, n) | 24.03 (32) | 34.65 (45) | −.528 (.062) | 30.08 (38) | 34.53 (48) | .414 (.137) |
| Addiction Severity Index composite | ||||||
| Alcohol severity (M, SD) | .195 (.199) | .247 (.232) | 3.94 (.048) | .212 (.223) | .217(.221) | 0.04 (.851) |
| Drug severity (M, SD) | .048 (.079) | .068 (.092) | 5.12 (.024) | .055 (.091) | .070 (.102) | 2.08 (.150) |
| Psychiatric severity (M, SD) | .347 (.228) | .405 (.239) | 4.74 (.030) | .383 (.232) | .369 (.229) | 0.27 (.606) |
| Addiction Severity Index items (past 30 days) | ||||||
| Days used alcohol (M, SD) | 3.60 (7.55) | 5.88 (9.39) | 4.85 (.029) | 4.96 (9.01) | 5.94 (9.16) | 0.78 (.377) |
| Days used opioids (M, SD) | 0.35 (2.96) | 1.62 (6.38) | 4.63 (.032) | 0.83 (4.69) | 1.25 (4.85) | 0.60 (.438) |
| Serious thoughts of suicide (%, n) | 11.60 (15) | 18.20 (24) | 2.46 (.118) | 20.80 (16) | 15.10 (21) | 1.47 (.226) |
| Attempted suicide (%, n) | 0.80 (1) | 3.20 (4) | 1.75 (.188) | 2.70 (2) | 0.90 (1) | 1.96 (.275) |
| Brief Addiction Monitor composite | ||||||
| Alcohol and drug use (M, SD) | 1.65 (2.77) | 2.68 (3.32) | 7.59 (.006) | 2.53 (3.51) | 2.86 (3.28) | 0.68 (.411) |
| Risk factors (M, SD) | 9.67 (4.60) | 11.07 (5.24) | 5.48 (.020) | 10.20 (4.67) | 11.01 (5.12) | 1.92 (.167) |
| Self-efficacy | ||||||
| Confidence (M, SD) | 75.84 (25.15) | 68.98 (28.91) | 3.97 (.048) | 72.94 (26.80) | 68.94 (26.82) | 1.31 (.253) |
Notes: Analyses conducted were logistic regressions or ANCOVAs controlling for inpatient detoxification unit and baseline value of the outcome.
Table 3 shows comparisons of patients assigned to ETM or UC at the 6-month follow-up, which occurred three months after the intervention ended for patients in the ETM group. Patients assigned to usual care were significantly more likely to have attended a 12-step meeting than were patients assigned to ETM, but no other differences were observed.
4. Discussion
In this randomized controlled trial with detoxification inpatients, a low-intensity telephone monitoring intervention enhanced with Motivational Interviewing and Contracts, Prompts, and Reinforcements was associated with better outcomes at 3-month follow-up. That is, patients who received ETM were less likely to receive repeated inpatient detoxification services and had lower substance use and psychiatric severity, while the intervention was active, than patients in UC. These benefits accrued even though ETM patients were no more likely than UC patients to obtain outpatient addiction treatment or attend mutual-help groups. However, the benefits of ETM did not hold at the 6-month follow-up. In fact, UC patients were more likely to have attended mutual-help between the 3- and 6-month follow-ups.
Relatedly, a study of patients with PTSD examined whether adding telephone care management (twice-per-month phone calls for three months) to usual outpatient mental health care improved treatment attendance and clinical outcomes (Rosen et al., 2017). Telephone-monitored patients completed more mental health visits during the intervention period than usual care patients did. However, telephone-monitored and usual care patients were comparable on treatment visits, substance use, and psychiatric symptoms at subsequent follow-ups. In both our and Rosen et al.’s (2017) studies, the lack of longer-term advantage for the telephone monitoring condition on outcomes occurred despite having successfully delivered the intervention. Specifically, in our study, 95% of patients assigned to ETM completed at least one phone call with the TeleCoach, with a mean of 8 (out of 12) phone calls completed. These telephone call “doses” are comparable to those in other trials of telephone interventions with mental health patients (Cook, Emiliozzi, Waters, & El Hajj, 2008; Rosen et al., 2013; Seal et al., 2012). However, other studies focused on patients with substance use disorders (Hilton et al., 2001; McKay et al., 2004; McKay, Lynch, Shepard, & Pettinati, 2005; McKay et al., 2010b) conducted telephone monitoring over a much longer period than used in our or others’ (Seal et al., 2012; Rosen et al., 2013; Rosen et al., 2017) research. For example, McKay et al.’s (2010b) telephone monitoring consisted of tapering telephone contacts for 18 months. In that study, the benefits of monitoring appeared to deteriorate over the final three months, when telephone contacts were least frequent. Together, our own and others’ (McKay et al., 2010; Rosen et al., 2017) studies suggest that benefits of telephone monitoring may not be sustained beyond the period of active intervention.
Whether sustaining ETM over a longer period than three months deters repeated inpatient detoxifications while improving outcomes, even without additional outpatient treatment, should be determined in future studies. Possibly, Telephone Monitoring, even over a longer period, would be both feasible and cost-saving. Indeed, telephone monitoring and counseling was found to be a cost-effective and potentially cost-saving continuing care intervention for individuals with substance use disorders (McCollister et al., 2016). The cost per additional day of abstinence was relatively low ($18.60), especially considering that abstinence is associated with positive outcomes such as better health, increased family stability and work productivity, and reductions in criminal activity and incarceration (Hagen et al., 2017; Kluk, Nich, Witkiewitz, Babuscio, & Carroll, 2014).
In our study, repeated inpatient detoxification between baseline and three months (24% and 39% of ETM and UC patients, respectively) and, separately, between three and six months (26% and 33%, respectively), of the initial detoxification episode was not uncommon; these findings are similar to those of other studies of publicly-funded inpatient detoxification (Mark et al., 2006). Repeated detoxifications may occur because patients view detoxification as quite desirable; it is accessed at a time of crisis, requires only a brief commitment, and has substantial palliative effects (Katz et al., 2004; Schultz, Martinez, Cucciare, & Timko, 2016). And, many detoxification patients are ambivalent about stopping use of substances (Katz et al., 2004; Schultz et al., 2016). Wait times for addiction treatment are another reason for repeated detoxifications (Timko et al., 2016). That is, patients who complete detoxification often have to wait weeks to be accepted by a treatment program and receive an admission date; they relapse while waiting and have to be “re-detoxed” to enter treatment.
In the current study, rates of outpatient addiction treatment following inpatient detoxification were about the same as those for another detoxification at 3-month follow-up (24% and 35% of ETM and UC patients, respectively) and 6-month follow-up (30% and 35%, respectively). Previous studies have also documented that even when patients successfully complete detoxification, relatively few engage in abstinence-oriented outpatient treatment (Davison et al., 2006), possibly precipitating high rates of emergency department visits (Constant, Le Gruyer, Le Lan, Riou, & Moirand, 2015). In contrast, in our study, higher proportions of patients attended 12-step groups during the 3-month (72% and 66%) and 6-month (53% and 64%) follow-up periods. Peer support, whether through 12-step group participation or from health care staff employed as peer support specialists, has been identified as critical to the recovery of detoxification patients because patients are likely to listen to peers who understand their experiences (Timko et al., 2016). As to why UC patients were more likely to have attended a 12-step group at the 6-month follow-up, we speculate that they sought support after experiencing relatively poorer outcomes in the immediate post-detoxification follow-up period than ETM patients. Previous research on detoxification inpatients found that they understood the potential benefits of 12-step group involvement, whether or not they had previous group exposure (Vederhus, Zemore, Rise, Clausen, & Hoie, 2015).
In the current study, one-third of patients reported having serious thoughts of suicide at baseline, and these thoughts continued at the 3-month (12% of ETM, and 18% of UC, patients) and 6-month (21% of ETM, and 15% of UC, patients) assessments. Likewise, of 253 detoxification inpatients, 37% had a lifetime history of attempted suicide or self-harm, and patients had high symptom levels of psychiatric disorders (Dore, Mills, Murray, Teesson, & Farrugia, 2012). Thus, together, the findings from the current study and from Dore et al. suggest that inpatient detoxification patients’ suicidality and mental health disorders such as depression and PTSD should be assessed. Because these conditions significantly impact the likelihood of recovery, they require developing patient-centered (reflecting the patient’s needs, preferences, and values) and individualized (coordinated, comprehensive, and continuous over time) long-term treatment strategies (Anderson, Hruska, Boros, Richardson, & Delahanty, 2018; Dore et al., 2012; Timko et al., 2016).
4.1. Limitations
This study had strengths (e.g., high retention rates among this difficult-to-follow patient population), but also limitations. Participants were mostly male and were from one health care system, the VA. Therefore, participants may not represent detoxification inpatients treated in community settings. However, VA is the largest US health care system and provider of addiction treatment services. Systematic reviews demonstrate that VA-provided health care is similar to care provided in non-VA health systems (Trivedi et al., 2011). An additional limitation was not having more comprehensive data to validate self-reports of substance use. Substance use was assessed by trained staff using valid and reliable procedures and instruments to minimize bias and help recall, and the veracity of substance use self-reports has been supported (Napper, Fisher, Johnson, & Wood, 2010; SAMSHA, 2010); nevertheless, future studies should consider requiring collateral reports or biological testing. This study is also limited in that reasons for ineligibility were not documented. Finally, in order to inform providers’ clinical practices, we conducted multiple comparisons on the secondary outcomes without adjustment, such that findings, although conceptually-sound, require replication. Specifically, we did not apply a Bonferroni correction because, although it would control for false positive associations of condition with outcomes, it would also increase the risk of generating false null associations.
4.2. Conclusions
Our findings suggest that detoxification inpatients benefit from receiving ETM while they are in contact with the TeleCoach, but that when these contacts end, the benefits fade. We also observed that many detoxification patients maintained a stable social network in the form of peers participating in 12-step mutual-help groups, which are free of charge and widely available. In light of mental health concerns such as suicidal ideation among detoxification patients, gaining a better understanding of how patients may more fully utilize mutual-help and treatment resources may be advantageous to their well-being. In addition, it will be important to test whether the extension over time of low-intensity, lost-cost approaches, such as telephone monitoring enhanced by empirically-supported practices, improve post-discharge outcomes among those receiving detoxification services.
Acknowledgments
This research was supported by the Department of Veterans Affairs (VA), Health Services Research and Development (HSR&D) Service (CRE 12-010 and RCS 00-001 to Dr. Timko). The views expressed are the authors’ and do not necessarily reflect those of the VA. No conflicts of interest are reported by any of the authors listed on this manuscript.
We gratefully acknowledge these contributors to the study: Uzma Ahmed, MD; Jessica Britt, MS; Matthew Palmisano, LCSW; Nicole Schultz, MA; Shannan Sonnicksen, LCSW, MPH; and Amanda Tjemsland, BS.
References
- Anderson RE, Hruska B, Boros AP, Richardson CJ, & Delahanty DL (2018). Patterns of co-occurring addictions, posttraumatic stress disorder, and major depressive disorder in detoxification treatment seekers: Implications for improving detoxification treatment outcomes. Journal of Substance Abuse Treatment, 86, 45–51. [DOI] [PubMed] [Google Scholar]
- Bailey GL, Herman DS, & Stein MD (2013). Perceived relapse risk and desire for medication assisted treatment among persons seeking inpatient opiate detoxification. Journal of Substance Abuse Treatment, 45, 201–305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breslin FC, Sobell LC, Sobell MB, & Agrawal S (2000). A comparison of a brief and long version of the Situational Confidence Questionnaire. Behaviour Research and Therapy, 38, 1211–1220. doi: 10.1016/S0005-7967(99)00152-7. [DOI] [PubMed] [Google Scholar]
- Broers B, Giner F, Dumont P, & Mino A (2000). Inpatient opiate detoxification in Geneva: follow-up at 1 and 6 months. Drug and Alcohol Dependence, 58, 85–92. doi: 10.1016/S0376-8716(99)00063-0. [DOI] [PubMed] [Google Scholar]
- Brown RL, Saunders LA, Bobula JA, Mundt MP, & Koch PE (2007). Randomized-controlled trial of a telephone and mail intervention for alcohol use disorders: Three-month drinking outcomes. Alcoholism: Clinical and Experimental Research, 31, 1372–1379. doi: 10.1111/j.1530-0277.2007.00430.x. [DOI] [PubMed] [Google Scholar]
- Burden JL, Parker JD, Williams DC, & Lash SJ (2017). Pre-implementation review of contracts, prompts, and reinforcement in SUD continuing care. Journal of Behavioral Health Services & Research, 44, 135–148. doi: 10.1007/s11414-016-9522-y. [DOI] [PubMed] [Google Scholar]
- Cacciola JS, Alterman AI, Dephilippis D, Drapkin ML, Valadez C Jr., Fala NC, Oslin D, & McKay JR (2013). Development and initial evaluation of the Brief Addiction Monitor (BAM). Journal of Substance Abuse Treatment, 44, 256–63. doi: 10.1016/j.jsat.2012.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carroll CP, Triplett PT, & Mondimore FM (2009). The intensive treatment unit: A brief inpatient detoxification facility demonstrating good postdetoxification treatment entry. Journal of Substance Abuse Treatment, 37, 111–119. doi: 10.1016/j.jsat.2008.11.003. [DOI] [PubMed] [Google Scholar]
- Center for Excellence in Substance Abuse Treatment and Education (CESATE). (2010). Brief Addiction Monitor: Manual of operations. Seattle, WA. [Google Scholar]
- Chutuape MA, Jasinski DR, Fingerhood MI, & Stitzer ML (2001). One-, three-, and six-month outcomes after brief inpatient opioid detoxification. American Journal of Drug and Alcohol Abuse, 27, 19–44. doi: 10.1081/ADA-100103117. [DOI] [PubMed] [Google Scholar]
- Constant A, Le Gruyer A, Le Lan C, Riou F, & Moirand R (2015). Postdetoxification factors predicting alcohol-related emergency room visits 12 to 24 months after discharge: Results from a prospective study of patients with alcohol dependence. Alcoholism: Clinical and Experimental Research, 39, 1236–1242. [DOI] [PubMed] [Google Scholar]
- Cook PF, Emiliozzi S, Waters C, & El Hajj D (2008). Effects of telephone counseling on antipsychotic adherence and emergency department utilization. American Journal of Managed Care, 14, 841–846. [PubMed] [Google Scholar]
- Davison JW, Sweeney ML, Bush KR, Davis Correale TM, Calsyn DA, Reoux JP, Sloan KL, & Kivlahan DR (2006). Outpatient treatment engagement and abstinence rates following inpatient opioid detoxification. Journal of Addictive Diseases, 25, 27–35. [DOI] [PubMed] [Google Scholar]
- Day E, & Strang J (2011). Outpatient versus inpatient opioid detoxification: A randomized controlled trial. Journal of Substance Abuse Treatment, 40, 56–66. doi: 10.1016/j.jsat.2010.08.007. [DOI] [PubMed] [Google Scholar]
- Dore G, Mills K, Murray R, Teesson M, & Farrugia P (2012). Post‐traumatic stress disorder, depression and suicidality in inpatients with substance use disorders. Drug and Alcohol Review, 31, 294–302. doi: 10.1111/j.1465-3362.2011.00314.x. [DOI] [PubMed] [Google Scholar]
- Ford LK, & Zarate P (2010). Closing the gaps: The impact of inpatient detoxification and continuity of care on client outcomes. Journal of Psychoactive Drugs, 42, 302–314. doi: 10.1080/02791072.2010.10400554. [DOI] [PubMed] [Google Scholar]
- Hagan E, Erga AH, Hagan KP, Nesvag SM, McKay JR, Lundervold AJ, & Walderhaug E (2017). One-year sobriety improves satisfaction with life, executive functions and psychological distress among patients with polysubstance use disorder. Journal of Substance Abuse Treatment, 76, 81–87. [DOI] [PubMed] [Google Scholar]
- Haley SJ, Dugosh KL, & Lynch KG (2011). Performance contracting to engage detoxification-only patients into continued rehabilitation. Journal of Substance Abuse Treatment, 40, 123–131. doi: 10.1016/j.jsat.2010.09.001. [DOI] [PubMed] [Google Scholar]
- Hilton ME, Maisto SA, Conigliaro J, McNiel M, Kraemer K, Kelley ME, Conigliaro R, Samet JH, Larson MJ, Savetsky J, Winter M, Sullivan LM, Saitz R, Weisner C, Mertens J, Parthasarathy S, Moore C, Hunkeler E, Hu TW, Selby J, Stout RL, Zywiak W, Rubin A, Zwick W, & Shepard D (2001). Improving alcoholism treatment across the spectrum of services. Alcoholism: Clinical and Experimental Research, 25, 128–35. [PubMed] [Google Scholar]
- Hubbard RL, Leimberger JD, Haynes L, Patkar AA, Holter J, Liepman MR, Lucas K, Tyson B, Day T, Thorpe EA, Faulkner B, & Hasson A (2007). Telephone enhancement of long-term engagement (TELE) in continuing care for substance abuse treatment: A NIDA clinical trials network (CTN) study. American Journal on Addictions, 16, 495–502 [DOI] [PubMed] [Google Scholar]
- Kiluk BD, Nich C, Wiitkiewitz K, Babuscio TA, & Carroll KM (2014). What happens in treatment doesn’t stay in treatment: Cocaine abstinence during treatment is associated with fewer problems at follow-up. Journal of Consulting and Clinical Psychology, 82, 619–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ivers JH, Zgaga L, Sweeney B, Keenan E, Darker C, Smyth BP, & Barry J (2017). A naturalistic longitudinal analysis of post-detoxification outcomes in opioid-dependent patients. Drug and Alcohol Review. doi: 10.1111/dar.12597. [DOI] [PubMed] [Google Scholar]
- Kahler CW, Read JP, Stuart GL, Ramsey SE, McCrady BS, & Brown RA (2004). Motivational enhancement for 12-step involvement among patients undergoing alcohol detoxification. Journal of Consulting and Clinical Psychology, 72, 736–741. doi: 10.1037/0022-006X.72.4.736. [DOI] [PubMed] [Google Scholar]
- Katz EC, Chutuape MA, Jones H, Jasinski D, Fingerhood M, & Sitzer M (2004). Abstinence incentive effects in a short-term outpatient detoxification program. Experimental and Clinical Psychopharmacology, 12, 262–268. doi: 10.1037/1064-1297.12.4.262. [DOI] [PubMed] [Google Scholar]
- Lash SJ, Stephens RS, Burden JL, Grambow SC, DeMarce JM, Jones ME, Lozano BE, Jeffreys AS, Fearer SA, & Horner RD (2007). Contracting, prompting, and reinforcing substance use disorder continuing care: A randomized clinical trial. Psychology of Addictive Behaviors, 21, 387–397. doi: 10.1037/0893-164X.21.3.387. [DOI] [PubMed] [Google Scholar]
- Lash SJ, Burden JL, Parker JD, Stephens RS, Budney AJ, Horner RD, Datta S, Jeffreys AS, & Grambow SC (2013). Contracting, prompting and reinforcing substance use disorder continuing care. Journal of Substance Abuse Treatment, 44, 449–56. doi: 10.1016/j.jsat.2012.09.008. [DOI] [PubMed] [Google Scholar]
- Lee MT, Horgan CM, Garnick DW, Acevedo A, Panas L, Ritter GA, Dunigan R, Babakhanlou-Chase H, Bidorini A, Campbell K, Habelin K, Huber A, Lambert-Wacey D, Leeper T, & Reynolds M (2014). A performance measure for continuity of care after detoxification: Relationship with outcomes. Journal of Substance Abuse Treatment, 47, 130–139. doi: 10.1016/j.jsat.2014.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mark TL, Vandivort-Warren R, & Montejano LB (2006). Factors affecting detoxification readmission: Analysis of public sector data from three states. Journal of Substance Abuse Treatment, 31, 439–445. doi: 10.1016/j.jsat.2006.05.019. [DOI] [PubMed] [Google Scholar]
- McCollister K, Yang X, & McKay JR (2016). Cost-effectiveness analysis of a continuing care intervention for cocaine-dependent adults. Drug & Alcohol Dependence, 158, 38–44. doi: 10.1016/j.drugalcdep.2015.10.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKay JR, Lynch KG, Shepard DS, Ratichek DS, Morrison S, Koppenhaver R, & Pettinati HM (2004). The effectiveness of telephone-based continuing care in the clinical management of alcohol and cocaine use disorders: 12-month outcomes. Journal of Consulting and Clinical Psychology; 72, 967–979. doi: 10.1037/0022-006X.72.6.967 [DOI] [PubMed] [Google Scholar]
- McKay JR, Lynch KG, Shepard DS, & Pettinati HM (2005). The effectiveness of telephone-based continuing care for alcohol and cocaine dependence: 24-month outcomes. Archives of General Psychiatry, 62, 199–207. doi: 10.1001/archpsyc.62.2.199. [DOI] [PubMed] [Google Scholar]
- McKay JR, Van Horn DH, & Morrison R (2010a). Telephone continuing care therapy for adults. Center City, MN: Hazelden. [Google Scholar]
- McKay JR, Van Horn DH, Oslin DW, Lynch KG, Ivey M, Ward K, Drapkin ML, Becher JR, & Coviello DM (2010b). A randomized trial of extended telephone-based continuing care for alcohol dependence: Within-treatment substance use outcomes. Journal of Consulting and Clinical Psychology, 78, 912–923. doi: 10.1037/a0020700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKellar J, Wagner T, Harris A, Oehlert M, Buckley S, & Moos R (2012). One-year outcomes of telephone case monitoring for patients with substance use disorder. Addictive Behaviors, 37, 1069–1074. doi: 10.1016/j.addbeh.2012.03.009. [DOI] [PubMed] [Google Scholar]
- McLellan AT, Weinstein RL, Shen Q, Kendig C, & Levine M (2005). Improving continuity of care in a public addiction treatment system with clinical case management. American Journal on Addictions,14, 426–440. doi: 10.1080/10550490500247099. [DOI] [PubMed] [Google Scholar]
- McLellan AT, Cacciola JC, Alterman AI, Rikoon SH, & Carise D (2006). The Addiction Severity Index at 25: Origins, contributions and transitions. American Journal on Addictions, 15, 113–124. doi: 10.1080/10550490500528316. [DOI] [PubMed] [Google Scholar]
- Mensinger JL, Lynch KG, Tenhave TR, & McKay JR (2007). Mediators of telephone-based continuing care for alcohol and cocaine dependence. Journal of Consulting and Clinical Psychology, 75, 775–784. doi: 10.1037/0022-006X.75.5.775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller WR, & Rollnick S (2002). Motivational Interviewing (2nd ed.). New York, NY: Guilford Press. [Google Scholar]
- Morgenstern J, Bux D, Labouvie E, Blanchard KA, & Thomas JM (2002). Examining mechanisms of action in 12-step treatment: The role of 12-step cognitions. Journal of Studies on Alcohol, 63, 665–672. doi: 10.15288/jsa.2002.63.665. [DOI] [PubMed] [Google Scholar]
- Moyers TB, Rowell LN, Manuel J, Ernst D, & Houck JM (2016). The Motivational Interviewing Treatment Integrity Code (MITIT 4): Rationale, preliminary reliability and validity. Journal of Substance Abuse Treatment, 65, 36–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Napper LE, Fisher DG, Johnson ME, & Wood MM (2010). The reliability and validity of drug users’ self reports of amphetamine use among primarily heroin and cocaine users. Addictive Behaviors, 35, 350–354. doi: 10.1016/j.addbeh.2009.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nasreddine ZS, Phillips NA, Bédirian V, Charbonneau S, Whitehead V, Collin I, Cummings JL, & Chertkow H (2005). The Montreal Cognitive Assessment, MoCA: A brief screening tool for mild cognitive impairment. Journal of the American Geriatric Society, 53, 695–699. doi: 10.1111/j.1532-5415.2005.53221.x. [DOI] [PubMed] [Google Scholar]
- Nosyk B, Li L, Evans E, Huang D, Min J, Kerr T, Brecht ML, & Hser YI (2014). Characterizing longitudinal health state transitions among heroin, cocaine, and methamphetamine users. Drug and Alcohol Dependence,140, 69–77. doi: 10.1016/j.drugalcdep.2014.03.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosen CS, Azevedo KJ, Tiet QQ, Greene CJ, Wood AE, Calhoun P, Bowe T, Capehart BP, Crawford EF, Greenbaum MA, Harris AH, Hertzberg M, Lindley SE, Smith BN, & Schnurr PP (2017). An RCT of effects of telephone care management on treatment adherence and clinical outcomes among veterans with PTSD. Psychiatric Services, 68, 151–158. [DOI] [PubMed] [Google Scholar]
- Rosen CS, Tiet QQ, Harris AH, Julian TF, McKay JR, Moore WM, Owen RR, Rogers S, Rosito O, Smith DE, Smith MW, & Schnurr PP (2013). Telephone monitoring and support after discharge from residential PTSD treatment: A randomized controlled trial. Psychiatric Services, 64, 13–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schilling RF, El-Bassel N, Finch JB, Roman RJ, & Hanson M (2002). Motivational interviewing to encourage self-help participation following alcohol detoxification. Research on Social Work Practice, 12, 711–730. doi: 10.1177/104973102237469. [DOI] [Google Scholar]
- Schultz NR, Martinez R, Cucciare MA, & Timko C (2016). Patient, program, and system barriers and facilitators to detoxification services in the US Veterans Health Administration: A qualitative study of provider perspectives. Substance Use & Misuse, 51, 1330–1341. [DOI] [PubMed] [Google Scholar]
- Seal KH, Abadian L, McCamish N, Shi Y, Tarasovsky G, & Weingardt K (2012). A randomized controlled trial of telephone motivational interviewing to enhance mental health treatment engagement in Iraq and Afghanistan veterans. General Hospital Psychiatry, 34, 450–459. [DOI] [PubMed] [Google Scholar]
- Spear SE (2014). Reducing readmissions to detoxification: An interorganizational network perspective. Drug and Alcohol Dependence, 137, 76–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stein BD, Kogan JN, & Sorbero M (2009). Substance abuse detoxification and residential treatment among Medicaid-enrolled adults: Rates and duration of subsequent treatment. Drug and Alcohol Dependence, 104, 100–106. doi: 10.1016/j.drugalcdep.2009.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stout RL, Rubin A, Zwick W, Zywiak W, & Bellino L (1999). Optimizing the cost-effectiveness of alcohol treatment: A rationale for extended case monitoring. Addictive Behaviors, 24, 17–35. doi: 10.1016/S0306-4603(98)00029-X. [DOI] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration. (2010). Reliability of key measures in the National Survey on Drug Use and Health (Office of Applied Studies, Methodology Series M-8, HHS Publication No. SMA 09–4425). Rockville, MD. [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration. (2014). The next step toward a better life (HHS Publication No. SMA 14–4474). Washington DC. [Google Scholar]
- Substance Abuse and Mental Health Services Administration, Center for Behavioral Health Statistics and Quality. (2016). Treatment Episode Data Set (TEDS) 2004–2014: National admissions to substance abuse treatment services (HHS Publication No. SMA 16–4986). Rockville, MD. [Google Scholar]
- Timko C, Below M, Schultz NR, Brief D, & Cucciare MA (2015). Patient and program factors that bridge the detoxification-treatment gap: A structured evidence review. Journal of Substance Abuse Treatment, 52, 31–39. doi: 10.1016/j.jsat.2014.11.009. [DOI] [PubMed] [Google Scholar]
- Timko C, Gupta S, Schultz N, & Harris AH (2016). Veterans’ service utilization patterns after alcohol and opioid detoxification in VHA care. Psychiatric Services, 67, 460–464. doi: 10.1176/appi.ps.201400579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trivedi AN, Matula S, Miake-Lye I, Glassman PA, Shekelle P, & Asch S (2011). Systematic review: Comparison of the quality of medical care in the Veterans Affairs and non-Veterans Affairs settings. Medical Care, 49, 76–88. [DOI] [PubMed] [Google Scholar]
- VA/DoD (Department of Veterans Affairs and Department of Defense) (2015). VA/DoD Clinical practice guideline for management of substance use disorders (SUD). Washington, DC: Department of Veterans Affairs. [Google Scholar]
- Van den Berg JE, Van den Brink W, Kist N, Hermes JS, & Kok RM (2015). Social factors and readmission after inpatient detoxification in older alcohol-dependent patients. American Journal on Addictions, 24, 661–666. doi: 10.1111/ajad.12287. [DOI] [PubMed] [Google Scholar]
- Vederhus J-K, Timko C, Kristensen O, & Clausen T (2014). Motivational intervention to enhance post-detoxification 12-step group affiliation: A randomized controlled trial. Addiction, 109(5), 766–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vederhus J-K, Zemore SE, Rise J, Clausen T, & Hoie M (2015). Predicting patient post-detoxification engagement in 12-step groups with an extended version of the theory of planned behavior. Addiction Science & Clinical Practice, 10, 15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zaller ND, Thurmond P, Brett J, Carleton JC, & Rich JD (2006). Linkage to methadone treatment from acute opiate detoxification treatment. Journal of Opioid Management, 2, 341–346. doi: 10.5055/jom.2006.0050. [DOI] [PubMed] [Google Scholar]
- Zanjani F, Miller B, Turiano N, Ross J, & Oslin D (2008). Effectiveness of telephone-based referral care management, a brief intervention to improve psychiatric treatment engagement. Psychiatric Services, 59, 776–781. doi: 10.1176/appi.ps.59.7.776. [DOI] [PubMed] [Google Scholar]