Abstract
Healthcare providers make time-sensitive care decisions based on EHR data. As systems of record, the EHR is often not configured to optimally surface timely information. For patients awaiting admission, infection control concerns that potentially require private rooms can prolong stays in the Emergency Department. We aim to determine if an event-based notification platform connected with a commercial EHR can help prioritize timely information and improve patient flow in the emergency department.
We undertook a pre-post analysis for patients being admitted from the emergency room who were tested for influenza. We used a primary outcome of mean time from negative test result to inpatient transfer. The median time decreased by 27%, from 4.1 hours to 3.0 hours. The distribution of transfer times pre and post-intervention were significantly different with a p-value of <0.001. Our findings support the use of event-based notification systems to improve patient flow in the emergency department.
Introduction
Widespread adoption of electronic health records (EHRs) has increased the availability of real-time information for frontline healthcare providers [1]. Though promising, electronic access to patient data poses its own challenges of data overload and challenging workflow changes [2–4]. EHRs are systems of record, displaying all available patient information. However, EHRs often require the user to identify time-sensitive patient data amidst hundreds of data elements. Providers typically access the record in a “pull” mode in which users seek out data elements of interest by occasionally reviewing the chart for new updates. Physicians spend as much as half of their time interacting with the EHR, and 12% of their time reviewing test results alone [5,6]. These are two of many challenges that limit the otherwise promising potential for digitalization to improve the quality and efficiency of care [7–9].
Real-time notifications help turn a “pull” mode of data review into a “push” mode in which specified data is actively presented to individuals for time-sensitive decision making. A large literature has examined the impacts of such notifications, particularly for critical laboratory results [10–12]. Critical result notifications create their own challenge of “alert fatigue”, although there is evidence that alert-based decision support systems can meaningfully improve patient care [8,13]. Push notifications of troponin results to emergency department (ED) physicians, for example, have reduced the time to discharge among patients presenting with chest pain [14].
A complement to the “pull” mode inherent in a system of record is a customizable notification system. We previously implemented a general notification platform for clinical data using software offered by a commercial vendor (Herald Health, Cambridge, MA) and have been used for alerts about critical lab results, radiology results, home care needs, and care pathways. During the winter and early spring of 2018, operational leadership at the hospital became interested in using Herald for improving patient flow within the hospital. A severe influenza season created a high volume of patients who could need single-occupancy rooms. Before transferring to an inpatient bed, patients with suspected flu would stay in the ED until an influenza test revealed whether the patient was appropriate for single or double occupancy. Given the high hospital census during influenza season, more timely communication of negative flu to the operations personnel responsible for bed assignment could improve patient care and efficiency.
Our objective in this study is to evaluate the impact of real-time notifications beyond the traditional focus on critical lab results. We hypothesize that a customizable notification platform such as Herald can significantly improve patient care by accelerating decisions made by frontline staff. Here, we examine the impact of a protocol for influenza test results on transfer times from the ED to an assigned bed.
Methods
In this retrospective observational study, we used a pre-post methodology to analyze data about patients admitted to the Brigham and Women’s Hospital (BWH) through the emergency department (ED). Specifically, we focused only on patients for whom a rapid Influenza test (known as a “flu swab”) was collected while they were in the ED, and the result of the swab was negative for Influenza A and Influenza B. These patients are automatically put on droplet precautions when the flu swab is ordered. If they require an admission to the inpatient units, they will need to be admitted to a single-occupancy room because of the droplet precautions. However, if the result of the flu swab is negative, assuming the patient does not have any other conditions requiring isolation, the patient can be admitted to a shared room (most rooms in the hospital units are shared rooms with two patient beds). Because the negative result is not an “abnormal” result requiring immediate medical intervention, it is not communicated to the providers. Consequently, many patients remain on “droplet isolation” status in the ED and are ineligible for a shared room, delaying their admission and transfer to inpatient units.
The Herald Health notification platform connects to a variety of real-time clinical data sources and monitors those data sources according to a set of protocols defined by frontline users or hospital administrators. Protocols can be simple rules—for example, a final imaging report is available—or contain complex logic, requiring a variety of patient data elements to be met before triggering (e.g. a physical therapy consult has been ordered for a patient on Medicare that lives within 5 miles of the hospital). If the conditions for a protocol are met, the software sends a notification to a frontline staff member according to their preferred communication channel, such as a pager, email, or web-based feed of events. The software had previously been deployed at Brigham and Women’s Hospital for alerts about critical lab results, radiology results, home care needs (notifying care coordinators that an order was placed for home physical therapy), and care pathways (identifying patients eligible for a home hospital program).
For the protocol we study here—alerting operations staff when flu test results are available for a patient waiting to be admitted to the hospital—the Herald software receives the lab test results via HL7 v2 message and patient location and bed status information available via additional application programming interfaces (APIs). The software processes these data in real time and checks whether the protocol logic is satisfied for each set of flu tests received. If the protocol is satisfied, the software automatically sends a page with the test result and patient information to the designated operations associate in charge of bed assignment via the hospital’s in-house paging system.
We collected data about patients with negative flu swab results who visited the BWH ED from three months before the software was deployed until three months after its implementation. We identified the timestamps associated with the flu swab order, flu swab result, droplet isolation order start and end time, and the date and time of patient’s transfer from the ED to an inpatient unit.
The primary outcome of our study was time from when the flu swab negative result was available until the patient was transferred to an inpatient unit. We excluded patients who were not admitted to an inpatient unit, patients whose flu swab result was only available after their transfer to an inpatient unit, and patients who remained on droplet isolation for more than 48 hours (i.e. had other indications for droplet precautions). Secondary outcomes included time from flu swab result until the time the precautionary droplet isolation order was discontinued and ED length of stay (LOS). ED LOS was defined as time from arrival at the ED until the patient arrived at their assigned bed in the inpatient unit. Therefore, it included the actual stay in the ED plus the “boarding time” for those patients who did not get directly transferred from the ED to their inpatient bed.
We anticipated that all outcome measures would be continuous variables with a significant skew, therefore we compared them using the Mann-Whitney U test for comparison of means. All analyses were done using R version 3.4.3 [15] and the study was approved by the Institutional Review Board of Partners Healthcare.
Results
A total of 917 cases with negative flu swab results were considered for this study, and 814 were included in the final analysis (the rest were excluded because their isolation status lasted more than 48 hours after the flu swab was resulted). Table 1 summarizes the key demographic features of the two study arms. Overall, no significant difference was observed between the two study arms with respect to these demographic characteristics.
Table 1.
Distribution of patient characteristics across the two study arms. The last row shows the p-value for the Mann-Whitney U test.
| Before | After | ||
|---|---|---|---|
| Number of encounters | 404 | 410 | |
| Number of patients | 392 | 401 | |
| Sex = female (%) | 225 (56%) | 211 (51%) | |
| Age (mean ± SD in years) | 64.1 ± 17.2 | 61.1 ± 16.9 | |
| Race (%) | White | 260 (64.4%) | 261 (63.7%) |
| Black | 68 (16.8%) | 77 (18.8%) | |
| Hispanic | 24 (5.9%) | 24 (5.9%) | |
| Asian | 21 (5.2%) | 22 (5.4%) | |
| Other/Unknown | 31 (7.7%) | 26 (6.2%) | |
| Primary Insurance (%) | Medicare | 215 (53.2%) | 204 (49.8%) |
| Medicaid | 42 (10.4%) | 36 (8.8%) | |
| Commercial | 135 (33.4%) | 157 (38.3%) | |
| Other | 12 (3.0%) | 13 (3.1%) | |
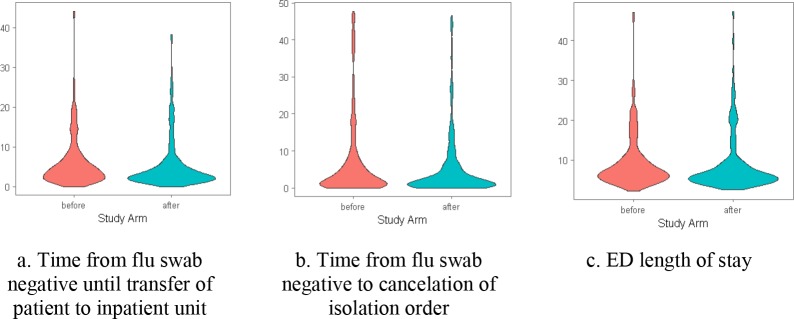
Figure 1 shows the distribution of the three main outcomes before and after the implementation of the flu test result notification protocol. The distribution of all three outcome variables shifted to shorter time intervals after implementation of the notification protocol.
Figure 1.
Distribution of the main outcome variables across the two study arms. All outcome measures are reported in hours. See text for explanation regarding the outlier values.
Table 2 compares the mean, standard deviation, median, and interquartile range of each outcome across the two periods. The time from flu swab negative result was available until the patient was transferred to the inpatient unit was statistically significantly shorter after the notifications were implemented (decreasing from a median of 4.1 hours to 3.0). The time from flu swab negative result was available until the isolation order was discontinued decreased by a similar amount (from 2.8 hours to 2.0). Similarly, the ED LOS was shorter in patients with negative flu swabs after the notifications were implemented compared to the historical control (from a median of 7.1 to 6.2). The distribution for each outcome was significantly different pre versus post-implementation of the protocol (with p-values of < 0.001, 0.006, and <0.001 respectively). For all three outcome measures, outliers existed in both arms of the study. However, removing those outliers did not change the directionality or statistical significance of the results.
Table 2.
Distribution of the main outcome variables across the two study arms. All outcome measures are reported in hours.
| Time from flu swab negative until transfer of patient to inpatient unit | Time from flu swab negative to cancelation of isolation order | ED length of stay | ||||
|---|---|---|---|---|---|---|
| Before | After | Before | After | Before | After | |
| Mean (SD) | 6.2 (6.7) | 5.4 (6.3) | 7.2 (10.8) | 5.3 (8.5) | 9.5 (6.8) | 8.9 (7.1) |
| Median (IQR) | 4.1 (5.2) | 3.0 (3.9) | 2.8 (6.4) | 2.0 (5.3) | 7.1 (5.2) | 6.2 (4.2) |
| P-value | < 0.001 | 0.006 | < 0.001 | |||
Discussion
We observed that a push notification of negative flu test results for patients admitted from the ED with suspected influenza awaiting inpatient bed resulted in approximately one-hour median declines for time to cancellation of isolation order, time to transfer to inpatient unit, and ED length of stay. These results are both clinically and statistically significant.
Increased boarding hours in the ED are associated with worse patient outcomes. Creation of new more available bed- hours in an ED during peak demand periods will increase more timely evaluations for other patients waiting for care. Scarce inpatient isolation rooms are also preserved for the most appropriate patients. More broadly, our results demonstrate that a tailored push notification system can have impact not just in clinical care, but also in hospital operations. While the study did not formally assess patient satisfaction, prolonged ED length of stay is known to negatively affect patient experience.
Both critical lab result notifications and adverse drug interaction alerts have received significant attention for their potential impacts on physician behavior and patient safety [16–18]. The opportunity to use real-time data from EHRs to improve the quality and efficiency of care may be broader [19]. A variety of frontline providers—from physicians and nurses to care coordinators and operations associates—make daily decisions that depend upon real- time data. That patient data can take many forms, including laboratory results, location, drug administration, demographics, and imaging studies. The typical “pull” mode of reviewing the system of record for updates can create delays in decision making, or worse, risk overlooking important changes to patient status. Data overload and poor EHR usability impede quick action.
Our study has limitations. A pre-post design is not ideal to assess causal relationships, and it is likely that unmeasured or unmeasurable factors external to this study may have contributed to the change observed in the outcome measures. Of note, the implementation of the notification system for flu negative patients was part of an operational decision on improving the flow of such patients, and it is likely that this operational push itself may have contributed to the outcome. Also, ED volume is affected by other seasonal factors, and a pre-post design cannot account for such factors. Nevertheless, the fact that our secondary outcome (time to discontinue isolation order), which is not impacted by temporal trends in hospital capacity, also declined in the same period suggests that these results are not exclusively due to seasonal trends. We also did not specifically study the potential for alert fatigue, which is a concern with all electronic notifications. However, we believe the potential for alert fatigue was minimal, because the notifications were purposefully designed in collaboration with the designated operations associates in charge of bed assignment, and because of the small number of cases that would qualify for these notifications (less than 5 a day, on average). Lastly, our analysis is limited to influenza testing only, and this may limit its generalizability. However, there are other use cases for infection control (such as resistant bacteria) that may present much larger opportunities, without seasonality. All in all, our findings support our original hypothesis that such a customizable notification system can play a significant role in facilitating hospital operations.
Conclusion
We demonstrated that a customizable, real-time notification system can significantly impact the efficiency of patient flow in the emergency department when tailored to the workflows of operations personnel responsible for bed assignment.
Acknowledgements
We thank Bradford Diephuis, MD, Craig Monsen, MD MS, and Andrew Hillis, PhD from Herald Health for working closely with us to design the flu test notification protocol. They did not participate in the study design, data collection, or analysis of the results, but reviewed an earlier version of this manuscript. Brigham and Women’s Hospital holds shares in Herald Health; none of the authors of this publication have shares with Herald Health. We also thank Sheila Harris, Executive Director for Patient Access Services at BWH, for her leadership in this project.
Figures & Table
References
- 1.Henry J, Pylypchuk Y, Searcy T, Patel V. Adoption of electronic health record systems among U.S. non-federal acute care hospitals: 2008–2015. ONC Data Br. 2016;35 [Google Scholar]
- 2.Boonstra A, Broekhuis M. Barriers to the acceptance of electronic medical records by physicians from systematic review to taxonomy and interventions. BMC Health Serv Res. 2010;10 doi: 10.1186/1472-6963-10-231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ajami S, Bagheri-Tadi T. Barriers for adopting electronic health records (EHRs) by physicians. Acta Inform Medica. 2013;21(2):129–34. doi: 10.5455/aim.2013.21.129-134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hall A, Walton G. Information overload within the health care system: a literature review. Heal Inf Libr J. 2004;21(2):102–8. doi: 10.1111/j.1471-1842.2004.00506.x. [DOI] [PubMed] [Google Scholar]
- 5.Hill RG, Sears LM, Melanson SW. 4000 clicks: a productivity analysis of electronic medical records in a community hospital ED. Am J Emerg Med. 2013;31(11):1591–4. doi: 10.1016/j.ajem.2013.06.028. [DOI] [PubMed] [Google Scholar]
- 6.Sinsky C, Colligan L, Li L, Prgomet M, Reynolds S, Goeders L, et al. Allocation of physician time in ambulatory practice: A time and motion study in 4 specialties. Ann Intern Med. 2016;165(11):753–60. doi: 10.7326/M16-0961. [DOI] [PubMed] [Google Scholar]
- 7.Hillestad R, Bigelow J, Bower A, Girosi F, Meili R, Scoville R, et al. Can electronic medical record systems transform health care? Potential health benefits, savings, and costs. Health Aff. 2005;24(5):1103–17. doi: 10.1377/hlthaff.24.5.1103. [DOI] [PubMed] [Google Scholar]
- 8.Chaudhry B, Wang J, Wu S, Maglione M, Mojica W, Roth E, et al. Systematic review: impact of health information technology on quality, efficiency, and costs of medical care. Ann Intern Med. 2014;144(10):742–52. doi: 10.7326/0003-4819-144-10-200605160-00125. [DOI] [PubMed] [Google Scholar]
- 9.Buntin MMB, Burke MMF, Hoaglin MCM, Blumenthal D. The benefits of health information technology: A review of the recent literature shows predominantly positive results. Health Aff. 2011;30(3):464–71. doi: 10.1377/hlthaff.2011.0178. [DOI] [PubMed] [Google Scholar]
- 10.Slovis BH, Nahass TA, Salmasian H, Kuperman G, Vawdrey DK. Asynchronous automated electronic laboratory result notifications: a systematic review. J Am Med Informatics Assoc. 2017;24(May):1173–83. doi: 10.1093/jamia/ocx047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kuperman GJ, Teich JM, Tanasijevic MJ, Ma’Luf N, Rittenberg E, Jha A, et al. Improving response to critical laboratory results with automation. J Am Med Informatics Assoc. 1999;6(6):512–22. doi: 10.1136/jamia.1999.0060512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kuperman GJ, Teich JM, Bates DW, Hiltz FL, Hurley JM, Lee RY, et al. Proceedings of the AMIA Annual Fall Symposium. American Medical Informatics Association; 1996. Detecting alerts, notifying the physician, and offering action items: a comprehensive alerting system; pp. 704–8. [PMC free article] [PubMed] [Google Scholar]
- 13.Bright T, Wong A, Dhurjati R, Bristow E, Bastian L, Coeytaux R, et al. Effect of clinical decision-support systems: a systematic review. Ann Intern Med. 2012;157(1):29–43. doi: 10.7326/0003-4819-157-1-201207030-00450. [DOI] [PubMed] [Google Scholar]
- 14.Verma A, Wang AS, Feldman MJ, Hefferon DA, Kiss A, Lee JS. Push-alert notification of troponin results to physician smartphones reduces the time to discharge emergency department patients: a randomized controlled trial. Ann Emerg Med. 2017;70(3):348–56. doi: 10.1016/j.annemergmed.2017.03.021. [DOI] [PubMed] [Google Scholar]
- 15.R Core Team. R: A language and environment for statistical computing. 2017 [Google Scholar]
- 16.Bates DW, Leape LL, Cullen DJ, Laird N, Petersen LA, Teich JM, et al. Effect of computerized physician order entry and a team intervention on prevention of serious medication errors. Jama. 1998;280(15):1311–6. doi: 10.1001/jama.280.15.1311. [DOI] [PubMed] [Google Scholar]
- 17.Bates David W, Teich Jonathan M, Lee Joshua, Kuperman Diane Seger Gilad J, Ma’Luf Nell, Boyle Deborah, LL The impact of computerized physician order entry on medication error prevention. J Am Med Inform Assoc. 1999;6(4):313–21. doi: 10.1136/jamia.1999.00660313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kaushal R, Shojania K, Bates D. Effects of computerized physician order entry and clinical decision support systems on medication safety: a systematic review. Arch Intern Med. 2003;163(12):1409–16. doi: 10.1001/archinte.163.12.1409. [DOI] [PubMed] [Google Scholar]
- 19.Choi K, Gitelman Y, Asch DA. Subscribing to your patients - reimagining the future of electronic health records. N Engl J Med. 2018;378(21):1960–2. doi: 10.1056/NEJMp1800874. [DOI] [PubMed] [Google Scholar]