Social scientists have long argued that power is a fundamental force behind human behavior.1–3 Power is not owned by one person; it is expressed in all relationships. Given its pervasive nature, every relationship in health care has a power dynamic.4
Learning how to navigate power dynamics is rarely part of medical training and has historically been a taboo topic of discussion. Residents are expected to demonstrate effective collaboration skills, according to the Accreditation Council for Graduate Medical Education5 and Royal College of Physicians and Surgeons of Canada6 competency frameworks. The intricacies of collaboration are difficult to master, because they are part of social relations where power flows unpredictably.7 How can we prepare residents to navigate the complex power dynamics embedded in health care settings?
Many social theories, including social network theories, can illuminate different aspects of power circulating in teams. In this editorial, we introduce a way of seeing power in interprofessional education (IPE) using social network theory. We demonstrate how this theory can usefully inform conversations about power in IPE and equip residents with (1) a sophisticated understanding of power, and (2) ways to manage power when working collaboratively with health professionals, patients, and families.
The Invisibility of Power in IPE
Research has established that positive collaborative relationships can promote efficacious teamwork, job satisfaction, team performance, and patient outcomes.8–13 However, when not managed or inadequately managed, power struggles can plague teams, resulting in team conflict, poor performance, low morale, and inferior decision-making.12–16 While the problems that arise with dysfunctional teams are widely recognized, and researchers have suggested techniques for resolving the dysfunction,17–20 poor collaborative team performance persists.12,21
One root cause that has yet to be robustly studied is the role of power in interprofessional collaboration. In a 2015 review of 2191 IPE-related articles, Paradis and Whitehead found that only 6 articles discussed issues and solutions related to sociological power.22 Paradis and Whitehead23 have argued that the predominant theory informing IPE initiatives has been contact theory.24,25 When applied to IPE, contact theory is premised on the notion that simply bringing different groups together will reduce prejudice and galvanize positive group relations.23 This approach to IPE is ineffective because coercing individuals into intergroup interactions can reinforce stereotypes, especially when power relations that traverse health care's professional hierarchy are obscured or ignored.23
Contact theory has been ritualized and sustained in IPE, and it has failed to capture important elements of teamwork, including power.23 Current approaches to IPE thus ill-prepare residents for the reality of practice where they must deliberately and effectively engage with power dynamics on teams to realize optimal patient care. We need a new approach.
What Is Social Network Theory?
Social network theory is an umbrella term for theories that focus on individuals, teams and organizations, and the web of interpersonal relationships that both constrain and enable human action in these social systems.26,27 Within social network theory there are several strands of theory, each using specific analytical approaches. Modern approaches developed in the field of relational sociology explore how network relations are interconnected with identity, power, meaning, and other socially constructed elements.26,28–31 These approaches emphasize culture, communication, and meaning making,26 and offer insights into the relational substance of teamwork—including power relations.32,33
Application to an Illustrative Case
To illustrate the value of employing social network theory to illuminate the pervasiveness of power on teams, we apply the theory to a clinical care situation. Even a routine interaction weaves a resident, attending physician, adolescent patient, and his parents into a social network permeated by power dynamics.
At an arthritis clinic, a senior resident informs an adolescent patient and his parents that the patient's arthritis symptoms have deteriorated and he should start taking medication. The patient and his parents are relieved when the resident explains that the medication's side effects will not be too severe. Afterward, the resident's attending physician interacts with the patient and his family and discovers signs of comorbidity. The attending decides that the patient needs to take a different medication with potentially serious side effects. The patient and family are disappointed with this news. They respond that the resident recommended a milder medication, and relay to the attending the information they can recall about the resident's initial plan. The attending calls a meeting with the resident, patient, and family for later that day to resolve the difference in opinions and discuss the plan. At the meeting, the resident explains and justifies the initial plan. The resident feels ashamed that she did not consider other comorbid conditions. The attending, burdened with time pressures and aware of the patient's and family's anxiety, harshly questions the resident's competence in front of the patient and family. The attending proclaims that the new recommendation embraces greater nuance in the patient's case. The attending does not elaborate on the decision-making process that led to the new recommendation. The attending asks the patient if he has any questions. Sensing the tension, the patient is not comfortable asking questions. The attending calls the meeting to a close. The patient and his parents leave and are upset that their concerns about side effects were not addressed. The resident goes to see the next patient while questioning her own clinical abilities and feeling unsure that she has what it takes to be a “good doctor.”
Applying social network theory to this vignette reveals the structural and sociocultural dynamics affecting this team's interactions. Using social network maps (ie, sociograms27) demonstrates how power dynamics shape the team's function by acting as static barriers and dynamic resources in collaborative practice. In this scenario, a sociogram (see the Figure) visually represents the network structure, connections and disconnections, and positions of influence on the team. Thin lines connecting nodes in this network represent weak relational ties. The unidirectional connections (eg, between the attending and the rest of team) emphasize how the resident, patient, and family lack open dialogue with the attending physician. The attending is in a position of power, and wields it from a disconnected and isolated position in the network structure. By discussing situations like the one in our scenario with residents, graduate medical educators can bring specific attention to power dynamics that shape clinical events. Educators can engage residents in an analysis of the power relations within teams, and identify possible solutions that minimize hierarchy and promote interconnectivity.
Figure.
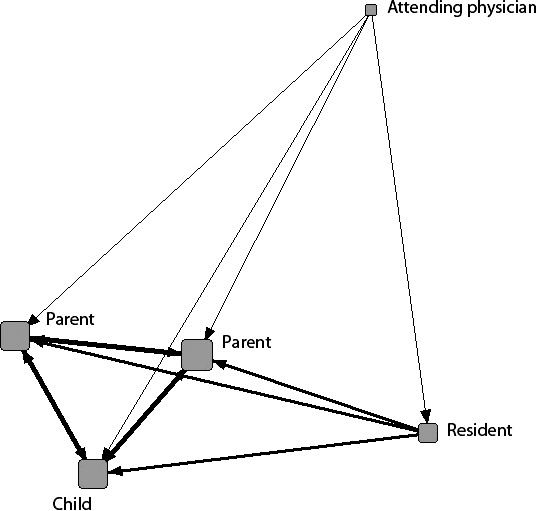
Sociogram of Team Structure
Power emerges through a subconscious internalization and acceptance of the positions of power held by team members.4,33 The flow of power is observable, for example, when the patient relays the resident's recommended medication to the attending. The patient acts as a “conduit of information” by representing the resident's goals and purposes to the attending. Later, when the attending has the final say in the medication decision, this authoritatively brings the potential for dialogue to a halt. The resident's, patient's, and family members' acceptance of this dominant communication style creates communication fracture in the network.32 After scrutinizing the power relations displayed in this example, faculty can ask residents to re-envision the scenario if power relations were not subordinate versus dominant, and to identify ways that they might shift the power in the situation to realize more egalitarian relations.
These are brief examples of the ways in which an implicit phenomenon like power can be rendered observable using a social network approach. There is vast potential for social network theory to highlight fragmenting and unproductive effects of particular power structures, as well as the choices residents have to navigate to negotiate power when engaging in collaborative practice.
Using Social Network Theory in IPE
Through visual network simulations, faculty can use social network theory to illuminate the complex social networks residents experience.32 For example, social network analysis software programs (eg, UCINET) can capture the way power flows productively or unproductively through the “capillaries”7 of network ties with drawing tools.34 Features like color, line width, and arrows enable sociograms to visually highlight connections between all team members, and to visually depict elements like dialogue, trust, and collaboration. Other more sophisticated network visualizations (eg, network movies)35 can be used to capture the fluid, unstable nature of teamwork, and the way power flows dynamically over time. These visualizations map out the dimensions of power within teams. Visualizations can stimulate reflection and creative problem solving between educators and residents about safely resisting hierarchies and transforming dominance in medical structures.36 Although social network approaches are underutilized in medical education,37 they hold great potential as a teaching or debriefing tool to reveal the function and outcome of power in collaborative practice.
A New Way of Seeing
We recognize that IPE interventions alone cannot foster collaborative practice and that broader systemic considerations (eg, political, organizational, governmental, legal, financial) must also be addressed.23,38 However, obscuring the social dimensions of teamwork fosters a culture of silence around power and ill-prepares residents for the interpersonal complexity of collaborative practice. Illuminating the multifaceted functions of power should be an integral part of IPE,12 and may be fostered by graduate medical educators' purposeful use of social network theory. Addressing the invisibility of power in IPE must be a high priority if we are to destabilize paternalistic approaches to teamwork,39 foster workplace innovation, and ultimately cultivate a more humane and democratic health care system.
References
- 1.Haugaard M. Power: A Reader. New York, NY: Manchester University Press; 2002. [Google Scholar]
- 2.Cartwright D. Power: a neglected variable in social psychology. In: Cartwright D, editor. Studies in Social Power. Ann Arbor, MI: University of Michigan Institute for Social Research;; 1959. pp. 1–14. [Google Scholar]
- 3.Russell B. Power: A New Social Analysis. New York, NY: W. W. Norton & Company;; 1938. [Google Scholar]
- 4.Nimmon L, Stenfors-Hayes T. The “handling” of power in the physician-patient encounter: perceptions from experienced physicians. BMC Med Educ. 2016;16(114):1–9. doi: 10.1186/s12909-016-0634-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Educational Commission for Foreign Medical Graduates. ACGME core competencies. 2019 http://www.ecfmg.org/echo/acgme-core-competencies.html Accessed April 10.
- 6.Frank JR. Ottawa, Canada: The Royal College of Physicians and Surgeons of Canada; 2005. 2019. The CanMEDS 2005 Physician Competency Framework. http://www.ub.edu/medicina_unitateducaciomedica/documentos/CanMeds.pdf Accessed April 10. [Google Scholar]
- 7.Bleakley A, Bligh J, Browne J. Medical Education for the Future: Identity, Power and Location. Dordrecht, Netherlands: Springe Science+Business Media;; 2011. [Google Scholar]
- 8.Kucukarslan SN, Peters M, Mlynarek M, Nafziger DA. Pharmacists on rounding teams reduce preventable adverse drug events in hospital general medicine units. Arch Intern Med. 2003;163(17):2014–2018. doi: 10.1001/archinte.163.17.2014. [DOI] [PubMed] [Google Scholar]
- 9.Gladstein DL. Groups in context: a model of task group effectiveness. Adm Sci Q. 1984;29(4):499–517. doi: 10.2307/2392936. [DOI] [Google Scholar]
- 10.Sundstrom E, de Meuse KP, Futrell D. Work teams: applications and effectiveness. Am Psychol. 1990;45(2):120–133. doi: 10.1037/0003-066X.45.2.120. [DOI] [Google Scholar]
- 11.Kash BA, Cheon O, Halzack NM, Miller TR. Measuring team effectiveness in the health care setting: an inventory of survey tools. Health Serv Insights. 2018;11:1–18. doi: 10.1177/1178632918796230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Janss R, Rispens S, Segers M, Jehn KA. What is happening under the surface? Power, conflict and the performance of medical teams. Med Educ. 2012;46(9):838–849. doi: 10.1111/j.1365-2923.2012.04322.x. [DOI] [PubMed] [Google Scholar]
- 13.On Teams. Boston, MA: Harvard Business School Publishing Corporation; 2013. Harvard Business Review. [Google Scholar]
- 14.Lee CT, Doran DM. The role of interpersonal relations in healthcare team communication and patient safety: a proposed model of interpersonal process in teamwork. Can J Nurs Res. 2017;49(2):75–93. doi: 10.1177/0844562117699349. [DOI] [PubMed] [Google Scholar]
- 15.Gittell JH, Weinberg D, Pfefferle S, Bishop C. Impact of relational coordination on job satisfaction and quality outcomes: a study of nursing homes. Hum Resource Manage J. 2008;18(2):154–170. doi: 10.1111/j.1748-8583.2007.00063.x. [DOI] [Google Scholar]
- 16.Mohammed S, Dumville BC. Team mental models in a team knowledge framework: expanding theory and measurement across disciplinary boundaries. J Organiz Behav. 2001;22(2):89–106. doi: 10.1002/job.86. [DOI] [Google Scholar]
- 17.Leonard M, Graham S, Bonacum D. The human factor: the critical importance of effective teamwork and communication in providing safe care. Qual Saf Health Care. 2004;13(suppl 1):85–90. doi: 10.1136/qhc.13.suppl_1.i85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Baker DP, Day R, Salas E. Teamwork as an essential component of high-reliability organizations. Health Serv Res. 2006;41(4, pt 2):1576–1598. doi: 10.1111/j.1475-6773.2006.00566.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Andersen PO, Jensen MK, Lippert A, Østergaard D. Identifying non-technical skills and barriers for improvement of teamwork in cardiac arrest teams. Resuscitation. 2010;81(6):695–702. doi: 10.1016/j.resuscitation.2010.01.024. [DOI] [PubMed] [Google Scholar]
- 20.Weller J, Boyd M, Cumin D. Teams, tribes and patient safety: overcoming barriers to effective teamwork in healthcare. Postgrad Med J. 2014;90(1061):149–154. doi: 10.1136/postgradmedj-2012-131168. [DOI] [PubMed] [Google Scholar]
- 21.Hackman JR. Tindale RS, Heath L, Edwards J, et al, eds. Theory and Research on Small Groups. New York, NY: Springer US;; 2002. Why teams don't work; pp. 245–267. [Google Scholar]
- 22.Paradis E, Whitehead CR. Louder than words: power and conflict in interprofessional education articles, 1954–2013. Med Educ. 2015;49:399–407. doi: 10.1111/medu.12668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Paradis E, Whitehead CR. Beyond the lamppost: a proposal for a fourth wave of education for collaboration. Acad Med. 2018;93(10):1457–1463. doi: 10.1097/ACM.0000000000002233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hean S, Dickinson C. The contact hypothesis: an exploration of its further potential in interprofessional education. J Interprof Care. 2005;19(5):480–491. doi: 10.1080/13561820500215202. [DOI] [PubMed] [Google Scholar]
- 25.Mohaupt J, van Soeren M, Andrusyszyn MA, Macmillan K, Devlin-Cop S, Reeves S. Understanding interprofessional relationships by the use of contact theory. J Interprof Care. 2012;26(5):370–375. doi: 10.3109/13561820.2012.673512. [DOI] [PubMed] [Google Scholar]
- 26.Fuhse JA. Theorizing social networks: the relational sociology of and around Harrison White. Int Rev Sociol. 2015;25(1):15–44. doi: 10.1080/03906701.2014.997968. [DOI] [Google Scholar]
- 27.Daly AJ. Social Network Theory and Educational Change. Cambridge, MA: Harvard Education Press;; 2010. [Google Scholar]
- 28.Bellotti E. Qualitative Networks: Mixed Methods in Sociological Research. New York, NY: Routledge;; 2015. [Google Scholar]
- 29.Mische A. Relational sociology, culture, and agency. In: Scott J, Carrington PJ, editors. The SAGE Handbook of Social Network Analysis. London, England: SAGE Publications Ltd;; 2011. pp. 80–98. [Google Scholar]
- 30.White HC. Identity and Control: A Structural Theory of Social Action. Princeton, NJ: Princeton University Press;; 1992. [Google Scholar]
- 31.DiMaggio P. Nadel's paradox revisited: relational and cultural aspects of organizational structure. In: Nohria N, Eccles RG, editors. Networks and Organizations: Structure, Form, and Action. Boston, MA: Harvard Business School Press;; 1992. pp. 118–142. [Google Scholar]
- 32.Nimmon L, Regehr G. The complexity of patients' health communication social networks: a broadening of physician communication. Teach Learn Med. 2017;30(4):352–366. doi: 10.1080/10401334.2017.1407656. [DOI] [PubMed] [Google Scholar]
- 33.Nimmon L, Cristancho S. When I say networks and systems. Med Educ. 2018;53:331–333. doi: 10.1111/medu.13673. [DOI] [PubMed] [Google Scholar]
- 34.Borgatti SP, Everett MG, Freeman LC. UCINET for Windows: software for social network analysis. Harvard, MA: Analytic Technologies;; 2002. [Google Scholar]
- 35.Bender-deMoll S, McFarland DA. The art and science of dynamic network visualization. J Soc Struct. 2006;7(2):1–38. [Google Scholar]
- 36.Shaw MK, Rees CE, Andersen NB, Black LF, Monrouxe LV. Professionalism lapses and hierarchies: a qualitative analysis of medical students' narrated acts of resistance. Soc Sci Med. 2018;219:45–53. doi: 10.1016/j.socscimed.2018.10.009. [DOI] [PubMed] [Google Scholar]
- 37.Isba R, Woolf K, Hanneman R. Social network analysis in medical education. Med Educ. 2017;51(1):81–88. doi: 10.1111/medu.13152. [DOI] [PubMed] [Google Scholar]
- 38.Thistlewaite J. Power and conflict in health care: everyone's responsibility. Med Educ. 2015;49(8):847. doi: 10.1111/medu.12757. [DOI] [PubMed] [Google Scholar]
- 39.Lingard L, Sue-Chue-Lam C, Tait GR, Bates J, Shadd J, Schulz V. Pulling together and pulling apart: influences of convergence and divergence on distributed healthcare teams. Adv Health Sci Educ Theory Pract. 2017;22(5):1085–1099. doi: 10.1007/s10459-016-9741-2. [DOI] [PMC free article] [PubMed] [Google Scholar]


