Abstract
Background
Identification of surrogate decision makers (SDMs) is an important part of advance care planning for hospitalized patients. Despite its importance, the best methods for engaging residents to sustainably improve SDM documentation have not been identified.
Objective
We implemented a hospital-wide quality improvement initiative to increase identification and documentation of SDMs in the electronic health record (EHR) for hospitalized patients, utilizing a Housestaff Quality and Safety Council (HQSC).
Methods
EHR documentation of SDMs for all adult patients admitted to a tertiary academic hospital, excluding psychiatry, were tracked and grouped by specialty in a weekly run chart during the intervention period (July 2015 through April 2016). This also continued postintervention. Interventions included educational outreach for residents, monthly plan-do-study-act cycles based on performance feedback, and a financial incentive of a one-time payment of 0.75% of a resident's salary put into the retirement account of each resident, contingent on meeting an SDM documentation target. Comparisons were made using statistical process control and chi-square tests.
Results
At baseline, SDMs were documented for 11.1% of hospitalized adults. The intervention period included 9146 eligible admissions. Hospital-wide SDM documentation increased significantly and peaked near the financial incentive deadline at 48% (196 of 407 admissions, P < 001). Postintervention, hospital-wide SDM documentation declined to 30% (134 of 446 admissions, P < .001), but remained stable.
Conclusions
This resident-led intervention sustainably increased documentation of SDMs, despite a decline from peak rates after the financial incentive period and notable differences in performance patterns by specialty admitting service.
What was known and gap
Documenting surrogate decision makers (SDMs) is an important part of advance care planning, but there is no standard method for engaging residents to document SDMs, which creates variability regarding whether the information is available and accessible.
What is new
A hospital-wide, resident-led quality improvement initiative, with financial incentive, to increase identification and documentation of SDMs in the electronic health record for hospitalized patients.
Limitations
The initiative only targeted residents and did not include other health care professionals. The initiative occurred in a single institution without a comparison group.
Bottom line
A resident-led quality improvement initiative with a multifaceted intervention that included a financial incentive improved documentation of SDMs for hospitalized adults.
Introduction
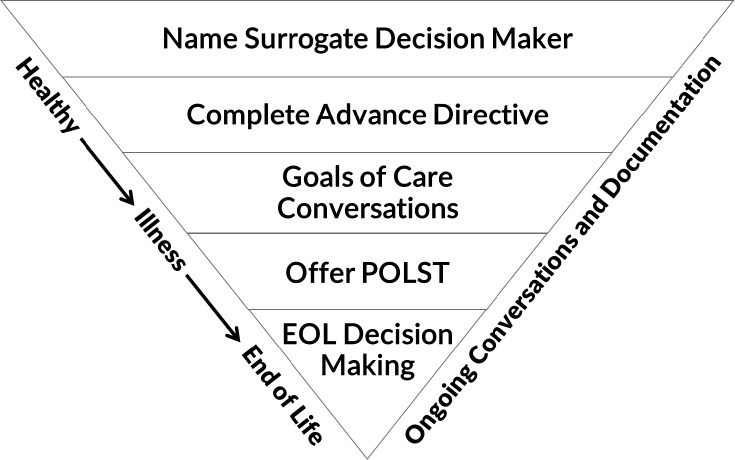
Early advance care planning (ACP) has been shown to increase goal-concordant care and reduce unwanted interventions near the end of life.1,2 While there is increasing awareness of the importance of early ACP,3 its routine implementation in inpatient settings remains limited.4 Documentation of surrogate decision makers (SDMs) is a first step in ACP5 and applicable to the broadest number of patients, who may lack or are at risk of losing their decision-making capacity during hospitalization (Figure 1). At our institution, there was no standard for documenting SDMs for adult hospitalized patients, resulting in variability in the presence and accessibility of SDM information when needed. Prior efforts to engage residents in early ACP for hospitalized patients at other institutions have shown transient improvements in ACP documentation following use of performance feedback, electronic health record (EHR) templates, and a financial incentive,6 although the mechanisms for achieving sustainable ACP documentation are unknown. Therefore, the aim of this resident-led initiative was to build on these methods to sustainably increase documentation of SDMs into a newly created ACP navigator of the EHR.
Figure 1.
Advance Care Planning Model5
Abbreviations: POLST, physician order for life-sustaining treatment; EOL, end of life.
Methods
This initiative was conducted at Oregon Health & Science University Hospital (OHSU), a 428-bed public academic medical center in Portland, Oregon. Prior to the start of the initiative, standard workflow for identifying a patient's SDM and documenting this information in the ACP navigator of the EHR was limited to the palliative care consult service and was not widely known or used outside of this service.
This intervention was led by a Housestaff Quality and Safety Council (HQSC), with its structure and function similar to groups described at other academic medical centers.7–9 HQSC members were resident volunteers, with at least one representative resident from each of the 20 core graduate medical education (GME) programs (provided as online supplemental material) assigned to the committee. Starting in July 2015, the HQSC sought to increase documentation of SDMs for inpatients within the ACP navigator of the EHR. The hospital administration offered an incentive of 0.75% of an individual's salary for each resident's retirement account if hospital-wide documentation of SDMs within the EHR reached 40% by the end of April 2016. This incentive was all-or-nothing—either every resident received the incentive or none of the residents did.
HQSC members were provided with educational material in customizable presentation slide decks with standard content (descriptions of the HQSC initiative and the rationale for implementing it, the goal, the financial incentive and deadline, and instructions on proper documentation). HQSC members were asked to customize these slides and deliver 10- to 30-minute presentations to their co-residents in their specialty during scheduled lectures such as grand rounds. Additionally, a 40-minute online training module was distributed to all residents as part of the required training. Created by the palliative care service, the module covered complementary vital topics such as descriptions of ACP, useful language for asking patients about SDMs,10 and instructions for appropriately documenting SDM in the ACP navigator using various clinical scenarios.
During monthly HQSC meetings, members participated in plan-do-study-act (PDSA) cycles, discussing different ACP processes, comparing their own specialty's performance to others, gathering feedback from other residents regarding SDM documentation practice, and brainstorming improvement strategies for subsequent cycles. HQSC resident leadership and faculty advisors also coordinated with palliative care expert advisors, EHR programmers, and administration officials to problem-solve complex systematic barriers identified during successive PDSA cycles.
The target population was adult patients admitted to OHSU from December 1, 2015, through June 30, 2016, with a length of stay greater than 24 hours, including non-teaching service patients and excluding patients admitted to the psychiatry service. SDM information documented in the ACP navigator of the EHR was extracted into a spreadsheet that characterized SDM documentation as complete if text was present or incomplete if text was absent. Reports were generated 3 days after each weekly reporting period, allowing time for documentation of an SDM for that patient. SDM documentation rates per eligible admissions were calculated hospital-wide, as well as for selected admitting service specialties (available as online supplemental material), using a run chart with weekly intervals. Performance data were discussed at monthly HQSC meetings, distributed via e-mail to HQSC members, and during the final month of the intervention period, updates on performance were sent weekly via e-mail to HQSC members and service department leadership. Statistical process control11 was used to assess stability of the process in the postintervention time period. Comparisons between percentages of SDM documentation at various time points during and after the intervention period were made using chi-square analysis with SPSS Statistics 25 (IBM Corp, Armonk, NY). A post-hoc chart review of documented SDMs from a convenience sample of 100 patients admitted after the initial intervention period was performed for quality control.
This project was reviewed by the OHSU Institutional Review Board and declared exempt as quality improvement not involving human subjects research.
Results
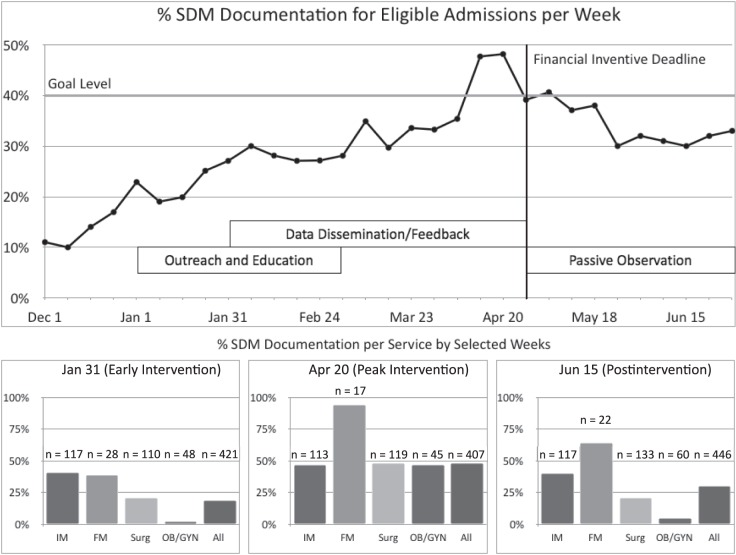
The completion rate of the SDM online training module by March 2016 was 87% (732 of 840 residents). During the intervention period (December 2015 to April 2016), documentation of SDMs for adult admissions (n = 9146) increased from a preintervention level of 11% (56 of 508 admissions) to a peak of 48% on April 20, 2016 (196 of 407 admissions, P < .001; Figure 2). For data collected during an additional 2 months postintervention (n = 3712 admissions), there was a significant decline in overall SDM documentation to 30% (134 of 446 admissions) measured on June 15, 2016 (postintervention) when compared to the peak intervention rate (P < .001). This postintervention rate was stable without evidence of significant variation an additional 3 months after the postintervention period, from June 16, 2016 to September 16, 2016 (Figure 3). Chart review of 100 random patients admitted after the intervention period, for whom the SDM field was populated, demonstrated appropriate data entry for 100% of patients sampled. A 0.75% of salary payment was awarded, ranging from $430 to $580 per resident, totaling approximately $400,000.
Figure 2.
Percentage of Documented Surrogate Decision Makers by Week and by Service Department for Selected Weeks: Early, Peak Intervention, and Postintervention
Abbreviations: SDM, surrogate decision maker; IM, internal medicine; FM, family medicine; Surg, surgery; ob-gyn, obstetrics and gynecology.
Figure 3.
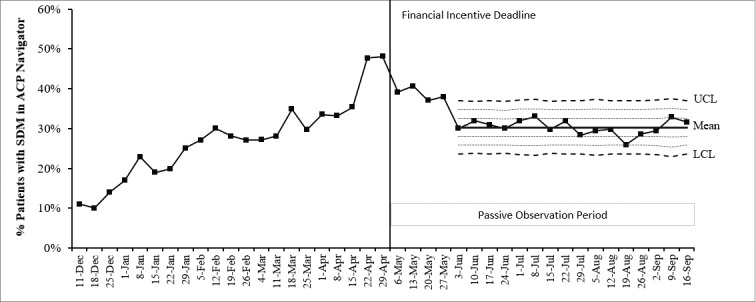
P Type Statistical Process Control Chart Demonstrating Stable Documentation Following Intervention Period
Abbreviations: SDM, surrogate decision maker; ACP, advance care planning; UCL, upper control limit; LCL, lower control limit.
SDM documentation rates varied over time by admitting service specialty. Internal medicine (IM) and family medicine (FM) demonstrated faster adoption rates and approached the goal level within the first 2 months of the intervention, with rates of 41% (48 of 117 admissions) and 39% (11 of 28 admissions), respectively. At peak hospital-wide SDM documentation, FM reached a documentation rate of 94% (16 of 17 admissions), whereas IM sustained rates achieved early in the intervention period at 47% (53 of 113 admissions). FM and IM maintained higher rates of SDM documentation in the postintervention period of 64% (14 of 22 admissions) and 40% (47 of 117 admissions), respectively. Neurology and neurological surgery had performance patterns similar to those of FM and IM (data not shown). Surgery and obstetrics and gynecology (ob-gyn) improved their rates to 48% (57 of 119 admissions) and 47% (21 of 45 admissions) immediately before the deadline for incentive, but dropped to lower levels, 21% (28 of 133 admissions) and 5% (3 of 60 admissions), respectively, by the postintervention analysis time point. Orthopedic surgery and urology had a similar transient higher performance patterns around the incentive deadline (data not shown).
Discussion
This resident-led initiative to improve SDM documentation was successful at meeting the target documentation rate of 40% by the financial incentive deadline. Additionally, increased SDM documentation was sustained at a stable rate beyond the intervention period, with varying documentation rates by admitting service specialty.
Our initiative benefited from several factors. First, our work strategically aligned with a major institutional priority, making key resources available such as EHR analysts who facilitated changes to the ACP navigator workflow and weekly extraction of hospital-wide SDM documentation data. Additionally, the HQSC structure allowed for rapid identification and triage of implementation barriers. In general, these consisted of macro-level barriers, which were addressed by HQSC leadership and faculty advisors (eg, changes to the ACP navigator within the EHR) and micro-level barriers, for which resident members of those services were best equipped to address directly with their respective specialty peers (eg, incorporation of SDM documentation into standardized admission workflows; Table). Frequent distribution of performance data by admitting service specialty during the intervention period provided necessary benchmarking for improvement cycles. Finally, the financial incentive deadline appears to correlate with a spike in SDM documentation, although this effect likely only contributed to the transient improvement seen in the admitting service specialties during the incentive period, after which SDM documentation in nearly every service specialty declined.
Table.
Examples of Barriers Encountered and Interventions Undertaken for SDM Documentation Initiative
| Barrier | Intervention |
Obtaining buy-in
|
Reframe SDM as part of a larger ACP continuum
|
Legal concerns
|
Allow for flexibility with documentation
|
Integration into workflow
|
ACP education and EHR changes
|
Abbreviations: SDM, surrogate decision maker; ACP, advance care planning; EHR, electronic health record.
We propose that sustained postintervention SDM documentation rates are suggestive of lasting changes in resident attitudes and behaviors despite the absence of a continued financial incentive. In general, the sustained high-performing specialties had representatives who frequently participated in HQSC meetings, surfaced barriers to implementation, and actively worked on solutions. Anecdotally, HQSC members from high-performing specialties also reported high levels of interest in the initiative and understanding of importance, with one HQSC member commenting during a meeting that SDM documentation for all of her patients was “the right thing to do.” In comparison, members of the lower-performing specialties, with only transient higher performance near the incentive deadline, had infrequent attendance to HQSC meetings, and anecdotally remarked on the potential non-relevance of SDM documentation for younger, healthier patients or those undergoing elective surgery, or reported persistent workflow barriers (eg, history and physical examination documentation occurring in the outpatient setting before planned admissions for surgery). We theorize that perceived relevance of SDM documentation to daily work and incorporation into clinical workflows were the primary factors driving sustained SDM documentation in high-performing specialties, with the financial incentive resulting in transient performance improvement near the incentive deadline. A similar intervention among IM residents to increase ACP discussion documentation for inpatients that included a financial incentive, EHR template, and performance feedback concluded that consistent performance feedback was the key element,6 though their analysis lacked postintervention follow-up data. The specific reasons for high-sustained SDM documentation postintervention versus transient high performance around the incentive deadline are unknown and may be confounded by our lack of comparison groups. Despite this limitation, our results call into question the sustainability of the interventions used, particularly the role of target-based financial incentives to drive improvement, which warrants further study.
Our initiative had several limitations. First, although the HQSC engaged residents across multiple specialties, we did not directly work with nurses or other health care professionals who often aid in identifying SDMs and facilitating ACP. Similarly, nonteaching attending patients were included in this data, but the intervention did not target these attending physicians, nor was nonteaching attending performance tracked as a comparison group, due to limitations with the data extraction process. Although a chart audit identified high rates of identification of those named as SDMs, the validity or accuracy of this information was not independently verified. This was also a single institution initiative without a comparison group, so changes in SDM documentation due to confounding factors or secular trends cannot be excluded. A high salary payment of approximately $400,000 was awarded to residents, limiting generalizability to institutions without these financial resources.
Future work will focus on PDSA cycles to identify and spread enabling workflow improvements, inclusion of other multiprofessional health care team members in the ACP process, extending identification of SDMs to other elements of ACP (such as documenting advance directives and goals of care conversations within the EHR), and will evaluate the effect on resident- and patient-centered outcomes. While completion of the ACP educational module will remain a requirement for all residents at OHSU, our institution has transitioned from a retirement bonus contingent on meeting performance targets to one based instead on continual engagement of residents in health system priority-aligned improvement work through the HQSC.
Conclusion
Our experience demonstrates that a resident-led quality improvement initiative utilizing a multifaceted intervention consisting of an educational module, periodic performance feedback via a HQSC, and a goal-contingent financial incentive improved documentation of SDMs for hospitalized adults. This increased documentation rate was sustained following the financial incentive period, suggesting durable changes in resident attitudes and behaviors surrounding ACP occurred as a result of the intervention.
Supplementary Material
References
- 1.Abarshi E, Onwuteaka-Philipsen B, Donker G, Echteld M, Van den Block L, Deliens L. General practitioner awareness of preferred place of death and correlates of dying in a preferred place: a nationwide mortality follow-back study in the Netherlands. J Pain Symptom Manage. 2009;38(4):568–577. doi: 10.1016/j.jpainsymman.2008.12.007. [DOI] [PubMed] [Google Scholar]
- 2.Gieniusz M, Nunes R, Saha V, Renson A, Schubert FD, Carey J. Earlier goals of care discussions in hospitalized terminally ill patients and the quality of end-of-life care: a retrospective study. Am J Hosp Palliat Care. 2018;35(1):21–27. doi: 10.1177/1049909116682470. [DOI] [PubMed] [Google Scholar]
- 3.Institute of Medicine. Dying in America: Improving Quality and Honoring Individual Preferences Near the End of Life. Washington, DC: The National Academy Press;; 2014. [PubMed] [Google Scholar]
- 4.Heyland DK, Barwich D, Pichora D, Dodek P, Lamontagne F, You JJ, et al. Failure to engage hospitalized elderly patients and their families in advance care planning. JAMA Intern Med. 2013;173(9):778–787. doi: 10.1001/jamainternmed.2013.180. [DOI] [PubMed] [Google Scholar]
- 5.Izumi S, Fromme EK. A model to promote clinicians' understanding of the continuum of advance care planning. J Palliat Med. 2017;20(3):220–221. doi: 10.1089/jpm.2016.0516. [DOI] [PubMed] [Google Scholar]
- 6.Lakin JR, Le W, Mourad M, Hollander H, Anderson WG. Incentivizing residents to document inpatient advance care planning. JAMA Intern Med. 2013;173(17):1652–1654. doi: 10.1001/jamainternmed.2013.8158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fleischut PM, Evans AS, Nugent WC, Faggiani SL, Lazar EJ, Liebowitz RS, et al. Ten years after the IOM report: engaging residents in quality and patient safety by creating a house staff quality council. Am J Med Qual. 2011;26(2):89–94. doi: 10.1177/1062860610380731. [DOI] [PubMed] [Google Scholar]
- 8.Tevis SE, Ravi S, Buel LB, Clough B, Goelzer S. Blueprint for a successful resident quality and safety council. J Grad Med Educ. 2016;8(3):328–331. doi: 10.4300/JGME-D-15-00250.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Iams W, Heck J, Kapp M, Leverenz D, Vella M, Szentirmai E, et al. A multidisciplinary housestaff-led initiative to safely reduce daily laboratory testing. Acad Med. 2016;91(6):813–820. doi: 10.1097/ACM.0000000000001149. [DOI] [PubMed] [Google Scholar]
- 10.White J, Fromme EK. “In the beginning...”: tools for talking about resuscitation and goals of care early in the admission. Am J Hosp Palliat Care. 2013;30(7):676–682. doi: 10.1177/1049909112468609. [DOI] [PubMed] [Google Scholar]
- 11.Benneyan JC, Lloyd RC, Plsek PE. Statistical process control as a tool for research and healthcare improvement. Qual Saf Health Care. 2003;12(6):458–464. doi: 10.1136/qhc.12.6.458. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.