Abstract
Oncogenic potential of Blastocystis species have been predicted on reporting the enhanced proliferation of human colorectal cancer cells by the parasite solubilized antigen in vitro, and the enhanced drug-induced carcinogenesis by infection in vivo. The present study is the first to investigate some phenotypic characters, namely the surface ultrastructure, protein profiles and protease activity of Blastocystis sp. isolated from three different clinical groups: colorectal carcinoma (CRC) patients, symptomatic and asymptomatic infected persons. Under SEM, all CRC Blastocystis sp. isolates had a very rough intensely folded surface in comparison to the less rough and completely smooth surface of all symptomatic and asymptomatic Blastocystis sp. Non-CRC isolates, respectively. Under reducing conditions, the sodium dodecyl sulfate–polyacrylamide gel electrophoresis had shown a significant presence of 2 protein bands of 230 and 32 KDa in 42.9% of Blastocystis sp. CRC isolates with their complete absence from Non-CRC isolates. While using non-reducing condition with the incorporation of gelatin in the gel to study the protease activity of the parasite, no significant difference existed between isolates of the three groups. In conclusion, the significant difference in surface ultrastructure and in protein profiles exists between Blastocystis sp. of CRC and Non-CRC isolates. These differences might be either secondary to the altered gut environment in the presence of CRC or are indicators of a different pathogenic potential of the parasite isolates inducing malignancy.
Keywords: Blastocystis sp., Colorectal carcinoma, Surface ultrastructure, Protein profiles, Zymography
Introduction
Recognized since the early 1900s as a harmless yeast (Tan 2008), Blastocystis species is nowadays identified as a protist (Silberman et al. 1996) belonging to the Stramenopiles line of eukaryotic organisms (Ho et al. 2000; Arisue et al. 2002). Blastocystis infection has been associated with several gastrointestinal symptoms such as diarrhea, abdominal pain, constipation, flatulence, fatigue, urticaria and skin rash (Parija and Jeremiah 2013) even though most cases are asymptomatic (Yason and Tan 2018). Blastocystis sp. is, also, known to play a significant role in some chronic gastrointestinal illnesses such as irritable bowel syndrome (IBS) (Abaza et al. 2014; Abu El-Fetouh et al. 2015). Furthermore, the parasite was identified with the significantly higher incidence in patients with colorectal carcinoma than with normal colonic epithelium (Steer 2007). More recently, El-Gayar and Mahmoud (2014), Mohamed et al. (2017) and Kumarasamy et al. (2017) speculated potential carcinogenic effect of Blastocystis sp. as the parasite affected the growth of colorectal cancer cells in vitro (Chandramathi et al. 2010) and induced precancerous polyp formation in vivo in rats (Kumarasamy et al. 2017).
Based mainly on small-subunit ribosomal RNA (SSU-rRNA) gene sequences, Blastocystis was found to be a species complex composed of 17 subtypes (STs) (Stensvold et al. 2007a, b) with biological and morphological differences (Yason and Tan 2018). Among the 17 STs recognized, ST1–8 could colonize both humans as well as non-human hosts (Stensvold 2013), with Blastocystis ST1 to ST4 diagnosed in most surveys in human populations (Alfellani et al. 2013; Ramírez et al. 2016; Yason and Tan 2018), ST9 was found to colonize human intestine only and ST10-17 are limited to non-human hosts (Stensvold 2013). Blastocystis ST7 hardly occurs, but in vitro and drug susceptibility studies pointed out that this subtype could possess a greater pathogenic potential (Wu et al. 2014a, b). Although some studies determining the subtype pathogenicity described a significant correlation between STs and the associated clinical presentation (Tan et al. 2008; AbdelHameed and Hassanin 2011), intra subtype variations in pathogenicity has also been detected, that is, not all the strains of a particular subtype are pathogenic with no significant differences in distribution of the STs between the symptomatic, asymptomatic (El-Wakil and Talaat 2009; Scanlan 2012; Abu EL-Fetouh et al. 2015) and irritable bowel syndrome (Abaza et al. 2014) groups. These observations illustrated that subtyping alone does not predict the pathogenicity of the isolate (Nagel et al. 2012).
Currently, the phenomenon of intra subtype variation in pathogenicity is explained by the phenotypic differences between the pathogenic and non-pathogenic members. The most studied phenotypic disparities of the pathogenic members are the predominance of amoeboid forms (Tan and Suresh 2006), the secretion of proteases and other hydrolytic enzymes (Tan and Suresh 2006; AbdelHameed and Hassanin 2011), the protein profiles (AbouGamra et al. 2011; Fadl et al. 2016), the growth kinetics (Parija and Jeremiah 2013), and the surface ultrastructure (Ragavan et al. 2014).
The present work aims to recognize the surface ultrastructure characters, the protein profiles and the protease activity of Blastocystis sp. isolated from colorectal carcinoma patients.
Materials and methods
Study design
The present work is a cross-sectional observational study conducted from September 2015 to October 2017, at the Parasitological Research and Diagnostic Laboratory unit of Parasitology Department, Faculty of Medicine, Ain-Shams University.
Collection and recruitment of Blastocystis isolates
Seven Blastocystis sp. isolates were recruited from stools collected from patients with early diagnosed colorectal carcinoma (CRC) attending the outpatient clinics (Oncology and Surgery) and Colonoscopy unit of El Demerdash Hospitals of Faculty of Medicine, and was referred to as Group I (GI),12 isolates were obtained from infected persons not diagnosed to have CRC (Non-CRC), 6 of them were infected symptomatic patients and were referred to as Group II (GII) and 6 were infected non-symptomatic carriers and were referred to as Group III (GIII), all of the Non-CRC patients were attending the Parasitological Research and Diagnostic Laboratory of Parasitology Department, Faculty of Medicine, Ain Shams University for stool examination.
Persons providing stool samples were subjected to a thorough medical history questionnaire covering the personal data, the presence of GIT symptoms related to Blastocystis sp. infection (diarrhea, abdominal pain, constipation, flatulence), parasitic infections, malignancy, and drug intake. Stool specimens were examined microscopically (Garcia 2015) using normal saline and iodine to detect parasites. Modified Ziehl–Neelsen and modified trichrome stains of fixed permanent smears were done to exclude coccidian parasites. Blastocystis positive stool samples were excluded from the study if they contained other parasites or if they were taken from patients with a history of anti-parasitic or chemotherapeutic drug intake.
Blastocystis sp. isolates were established in culture from human positive stool samples by culturing on the biphasic egg-slant medium overlaid with Locke’s solution and 20% inactivated horse serum (Clark and Diamond 2002).
After repeated subcultures, organisms of each Blastocystis sp. isolate were harvested from tubes containing peak growth by centrifugation (500×g, 5 min) and washed twice with sterile phosphate buffered saline (PBS; pH 7.4). Subsequently, parasites were purified using a density gradient centrifugation technique (Upcroft et al. 1989) to reduce bacterial contamination and to concentrate Blastocystis organisms from culture supernatants. Briefly, washed organisms suspended in 3 ml PBS (PH 7.4) were layered onto 10 ml of Ficoll-Hypaque separating media (Pharmacia Biotech Inc., Piscataway, NJ, USA) in a 12-ml centrifuge tube and were concentrated by centrifugation (2000×g for 20 min). Blastocystis sp. cells banded approximately 1 cm from the top of the Ficoll-Hypaque solution, while bacteria pelleted at the bottom of the tube. Purified parasites were removed by aspirating the band, washed in sterile PBS, and pelleted by centrifugation (500×g for 5 min). This was repeated for five times, then a portion of the final pellet was examined under bright field microscopy at the magnification of 1000× to ensure the purity of the sample, and the pellet was stored at − 70 °C until processed to be further fixed and examined under scanning electron microscopy and to prepare Blastocystis sp. solubilized antigen for protein profiling and zymography by SDS–polyacrylamide electrophoresis.
Scanning electron microscopy (SEM) (Zaman et al. 1999)
The specimen for SEM was prepared by fixing overnight in 4% (v/v) glutaraldehyde in 0.1 M sodium cacodylate buffer (pH 7.3) and, postfixed for 30 min in 1% osmium tetroxide in cacodylate buffer. After osmication, specimens were mounted on glass cover-slips previously coated with poly-I-lysine (Sigma Chemical Company, St. Louis) for 0.5 h in a moist chamber and then dehydrated in graded ethanols. After critical point drying in CO2, the cover glass was placed on adhesive-coated stubs, gold coated by SPI-Module and examined by Environmental SEM (Inspect S; FEI Company, Holland) at the Electron Microscopy Unit of Theodor Bilharz Research Institute (TBRI).
Sodium dodecyl sulfate–polyacrylamide gel electrophoresis (SDS–PAGE)
Blastocystis sp. isolates solubilized antigen preparation (Gericke et al. 1997)
Harvested parasites, stored at − 70 °C, were subjected to successive cycles of freezing at − 20 °C and thawing at 37 °C in a water bath. Completion of lysis was achieved by adding few drops of sterile distilled water followed by ultrasonication at 30 s for six cycles with 30-s intervals. The homogenates were centrifuged at 11,000×g for 10 min at 4 °C and the supernatants containing the crude extract of the parasites were collected, and their protein contents were estimated by the Bradford technique (Bradford 1976). The antigens were kept at − 20 °C till use.
SDS–PAGE protein profiles analysis (Laemmli 1970)
Cell lysate containing 40 μg protein from each isolate was denatured by boiling for 4 min with 1× sample buffer (10% SDS, 128 mM 2-β mercaptoethanol, 20% glycerol, 1% bromophenol blue, 500 mM TrisHCl pH 6.8) and loaded into SDS–discontinuous polyacrylamide gel for electrophoresis (PAGE) in a Mini-Protean II Electrophoresis Unit (BioRad). Two acrylamide concentrations, 12% and 5% in resolving and stacking gels, respectively, were used. Electrophoresis was started at a voltage of 35 V for 20 min (for stacking gel), then, the voltage was increased to 150 V for 90 min (for resolving gel). Pre-stained molecular weight markers were used (Bio-Rad Laboratories, Hercules, Calif., USA). The protein bands were visualized by staining in 0.25% Coomassie Brilliant blue R-250 for 30 min. The gel was imaged using gel imaging instrument, and the molecular weights of proteins were determined by computerized analysis of SDS–PAGE gels using Gel pro-documentation software.
Gelatin SDS–PAGE protease activity (zymography)
Electrophoretic analysis of proteolytic activity contained in Blastocystis sp. isolates was carried out as described by Toth and Fridman (2001) in the SDS-discontinuous buffer system of Laemmli (1970) as previously described with 0.2% (w/v) gelatin (Sigma) copolymerized into the resolving gel. Samples (20 μg/well) were loaded in Laemmli’s buffer devoid of reducing agents (β-mercaptoethanol) without boiling so that enzymatic activity of the proteases would be regained upon renaturation. Electrophoresis was run for 90 min at 140 V at 4 °C in resolving gel. To develop and visualize proteolytic activity, gels were then incubated with continuous shaking on an orbital shaker in a 0.25% (v/v) Triton X-100 solution (Washing buffer) for 1 h at room temperature to remove the SDS and to allow the proteases to become active, soaked 3 times in distilled water for 5 min each, and transferred to incubation buffer containing 1 mM DTT (dithiothreitol, Sigma) for overnight at 37 °C. The bands were visualized by staining in 0.12% (w/v) Coomassie brilliant blue R-250 in 40% [v/v] methanol-10% [v/v] acetic acid solution for 4 h. Molecular weight determination was done with reference to prestained markers (BioRad) by computerized analysis of gels using Gel pro-documentation software.
Statistical analysis
The data were analyzed using the Statistical Package for Social Science (SPSS 15.0.1 for Windows; SPSS Inc., Chicago, IL, 2001). A one-way analysis of variance (ANOVA) test was used to assess the statistical significance of the difference between more than two study group means. A P value ≥ 0.05 was considered statistically significant.
Results
According to the clinical history and stool examination, nineteen Blastocystis species isolates were obtained and grouped into 3 groups: 7 isolates in group I (GI) from early diagnosed colorectal carcinoma (CRC) patients (CRC isolates), 6 isolates in group II (GII) from Non-CRC patients with symptoms suggestive of blastocystosis such as diarrhea, abdominal pain, vomiting, and flatulence as abdominal pain, bloating and diarrhea (Non-CRC symptomatic isolates), and, 6 isolates in group III (GIII) from Non-CRC patients without any gastrointestinal symptoms (Non-CRC asymptomatic isolates).
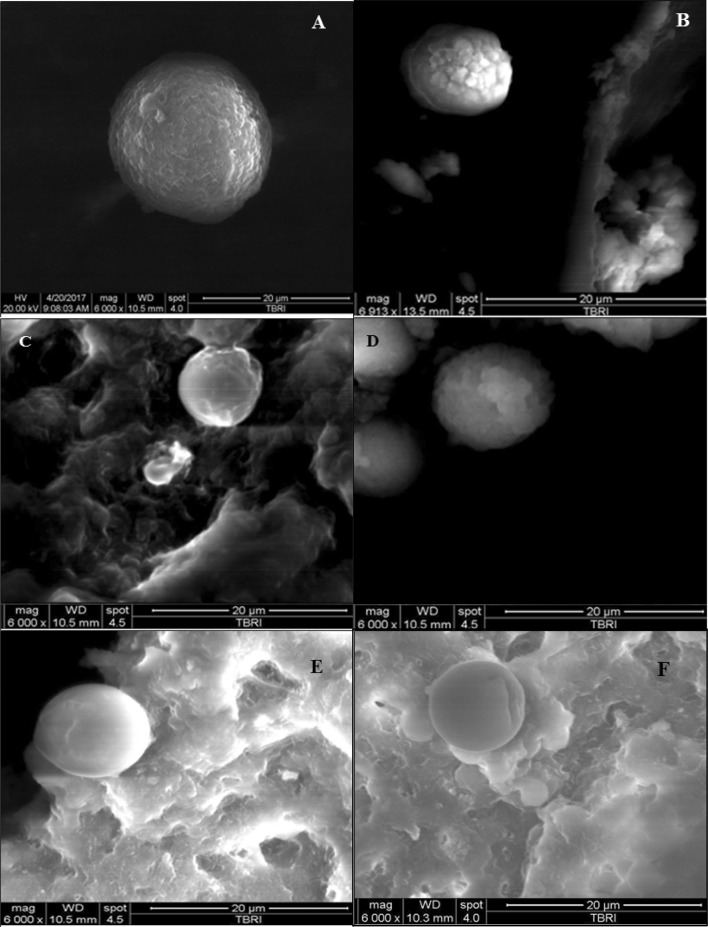
Under SEM, Blastocystis organisms from cultures of the isolates from the three groups appeared round, oval, and sometimes, irregular in shape, with sizes ranging from 5 to 20 μm. No size differences was detected between the three groups. No surface coat was detected in any isolates in culture. All Blastocystis organisms of CRC isolates possess extremely rough and intensely folded surface while isolates from Non-CRC symptomatic isolates possess less rough with tiny pores, and Blastocystis asymptomatic isolates have a very smooth surface as shown in Fig. 1 and Table 1.
Fig. 1.
Scanning electron micrographs of Blastocystis sp. isolates from GI: colorectal carcinoma patients (a, b) with extremely folded rough surface, GII: non-colorectal carcinoma symptomatic patients (c, d) with slightly rough surface, and GIII: non-colorectal carcinoma asymptomatic carriers (e, f) with smooth surface
Table 1.
Surface structure of Blastocystis sp. isolates of GI (CRC group), GII (Non-CRC symptomatic sub-group) and GIII (Non-CRC asymptomatic sub-group) under SEM examination
| SEM | GI (N = 7) | GII (N = 6) | GIII (N = 6) | P value |
|---|---|---|---|---|
| Description | Organisms with a coarse and intensely folded surface with marked surface irregularity in organisms of all seven isolates | Organisms with slightly rough surface with tiny pores in organisms of all six isolates | Organisms with smooth surface in organisms of all six isolates of the group | P < 0.001 |
N = number of isolates in the group. Comparison by One-way ANOVA test, where: P value = Probability value, where: P < 0.01 = highly significant difference
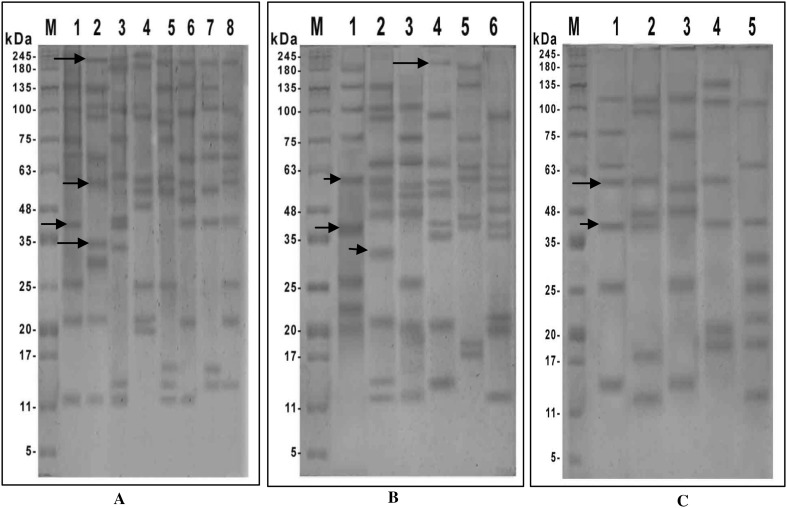
The protein profiles of Blastocystis sp. isolates analyzed by SDS–page showed the presence of a total of 30 bands, of both high and low molecular weights (MW) ranging from 12 to 230 kDa. Statistical analysis of protein profiles of the three groups revealed significant differences in one high MW (230 kDa) and some low MW (56, 38, 32 kDa) bands. Analysis showed a significant presence of 2 protein bands of 230 and 32 kDa in 42.9% of Blastocystis sp. of CRC isolates with their complete absence from Non-CRC isolates. The protein band of 56 kDa was detected in 2 (28.6%) isolates of GI, and in 4 isolates (66.7%) in GIII and significantly not detected in any isolates of GII. No common protein band was detected in all isolates of the three groups (Table 2, Fig. 2).
Table 2.
Molecular weight and frequency of protein bands of Blastocystis isolates in GI (CRC group), GII (Non-CRC symptomatic sub-group) and GIII (Non-CRC asymptomatic sub-group), analyzed by SDS–PAGE
| MW of bands (kDa) | Group | P value | |||||
|---|---|---|---|---|---|---|---|
| GI | GII | GIII | |||||
| Count | % | Count | % | Count | % | ||
| 230 | 3 | 42.9 | 0 | 0 | 0 | 0 | 0.047 |
| 200 | 3 | 42.9 | 3 | 50 | 1 | 16.7 | 0.448 |
| 180 | 0 | 0 | 1 | 16.7 | 0 | 0 | 0.319 |
| 135 | 2 | 28.6 | 4 | 66.7 | 1 | 16.7 | 0.169 |
| 130 | 0 | 0 | 1 | 16.7 | 0 | 0 | 0.319 |
| 127 | 0 | 0 | 0 | 0 | 1 | 16.7 | 0.319 |
| 112 | 0 | 0 | 0 | 0 | 1 | 16.7 | 0.319 |
| 100 | 5 | 71.4 | 3 | 50 | 3 | 50 | 0.659 |
| 95 | 1 | 14.3 | 1 | 16.7 | 0 | 0 | 0.591 |
| 90 | 3 | 42.9 | 2 | 33.3 | 2 | 33.3 | 0.917 |
| 75 | 4 | 57.1 | 3 | 50 | 3 | 50 | 0.956 |
| 65 | 1 | 14.3 | 1 | 16.7 | 0 | 0 | 0.519 |
| 64 | 3 | 42.9 | 4 | 66.7 | 3 | 50 | 0.648 |
| 58 | 6 | 85.7 | 3 | 50 | 2 | 33.3 | 0.095 |
| 56 | 2 | 28.6 | 0 | 0 | 4 | 66.7 | 0.045 |
| 50 | 1 | 14.3 | 1 | 16.7 | 2 | 33.3 | 0.668 |
| 48 | 1 | 14.3 | 3 | 50 | 1 | 16.7 | 0.331 |
| 47 | 2 | 28.6 | 1 | 16.7 | 0 | 0 | 0.370 |
| 45 | 1 | 14.3 | 1 | 16.7 | 1 | 16.7 | 0.990 |
| 40 | 3 | 42.9 | 1 | 16.7 | 1 | 16.7 | 0.458 |
| 38 | 2 | 28.6 | 3 | 50 | 6 | 100 | 0.030 |
| 32 | 3 | 42.9 | 0 | 0 | 0 | 0 | 0.047 |
| 30 | 0 | 0 | 2 | 33.3 | 0 | 0 | 0.088 |
| 25 | 3 | 42.9 | 3 | 50 | 4 | 66.7 | 0.684 |
| 22 | 2 | 28.6 | 4 | 66.7 | 1 | 16.7 | 0.169 |
| 20 | 2 | 28.6 | 0 | 0 | 1 | 16.7 | 0.370 |
| 18 | 1 | 14.3 | 3 | 50 | 1 | 16.7 | 0.280 |
| 17 | 2 | 28.6 | 1 | 16.7 | 1 | 16.7 | 0.828 |
| 14 | 2 | 28.6 | 3 | 50 | 3 | 50 | 0.659 |
| 12 | 3 | 42.9 | 4 | 66.7 | 2 | 33.3 | 0.489 |
The cells in italics show bands of statistical significance in the studied groups
Fig. 2.
SDS–PAGE protein profiles of the 19 Blastocystis isolates separated in 12% polyacrylamide gel and stained by Coomassie blue stain. Lane M, broad range molecular weight standard. Lanes 1–4 in a, lanes 3–5 in b: represent isolates from GI (CRC group). Lanes 5–7 in a, lanes 1–2 in b, and lane 5 in c: isolates from GII (Non-CRC symptomatic group). Lane 8 in a, lane 6 in b and lanes: 1–4 in c: isolates from the GIII (Non-CRC asymptomatic group)
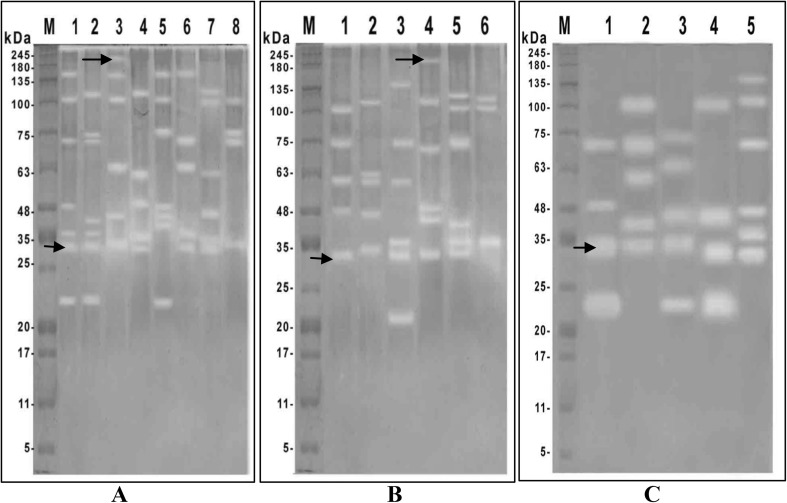
Using gelatin-SDS–PAGE analysis, protease bands were seen as clear bands against a stained dark background (Fig. 3). Blastocystis sp. isolates showed a total of 17 protease bands ranging between 22 and 215 kDa. Both high (215, 143, 140, 120, 100, 74, 70, 63 and 60 kDa) and low (48, 45, 39, 35, 33, 32 and 22 kDa) molecular weights proteins were detected. Statistical analysis of SDS–PAGE protease profiles revealed that there is no significant difference (P > 0.05) between the three studied groups (Table 3).
Fig. 3.
Gelatin-SDS–PAGE showing the protease profiles of different Blastocystis isolates. Protease bands can be seen as clear bands against blue background. Lanes 1–4 in a, lanes 3–5 in b represent isolates in GI (CRC group). Lanes 5–7 in a, lanes 1–2 in b and lane 5 in c represent isolates in GII (Non-CRC symptomatic group). Lane 8 in a, lane 6 in b and lanes 1–4 in c represent isolates in GIII (Non-CRC asymptomatic group) (color figure online)
Table 3.
Molecular weight and frequency of protease bands of different groups of Blastocystis isolates separated by SDS–PAGE
| MW of bands (kDa) | Group | P value | |||||
|---|---|---|---|---|---|---|---|
| GI | GII | GIII | |||||
| Count | % | Count | % | Count | % | ||
| 215 | 2 | 28.6 | 0 | 0 | 0 | 0 | 0.147 |
| 143 | 0 | 0 | 1 | 16.7 | 0 | 0 | 0.319 |
| 140 | 4 | 57.1 | 2 | 33.3 | 0 | 0 | 0.087 |
| 120 | 3 | 42.9 | 3 | 50 | 1 | 16.7 | 0.448 |
| 100 | 3 | 42.9 | 3 | 50 | 4 | 66.7 | 0.684 |
| 74 | 3 | 42.9 | 2 | 33.3 | 2 | 33.3 | 0.917 |
| 70 | 3 | 42.9 | 2 | 33.3 | 3 | 50 | 0.842 |
| 63 | 1 | 14.3 | 2 | 33.3 | 1 | 16.7 | 0.668 |
| 60 | 2 | 28.6 | 2 | 33.3 | 1 | 16.7 | 0.795 |
| 48 | 3 | 42.9 | 3 | 50 | 1 | 16.7 | 0.448 |
| 45 | 2 | 28.6 | 2 | 33.3 | 2 | 33.3 | 0.977 |
| 39 | 2 | 28.6 | 1 | 16.7 | 1 | 16.7 | 0.828 |
| 35 | 4 | 57.1 | 2 | 33.3 | 1 | 16.7 | 0.313 |
| 33 | 3 | 42.9 | 2 | 33.3 | 0 | 0 | 0.194 |
| 32 | 5 | 71.4 | 4 | 66.7 | 4 | 66.7 | 0.977 |
| 30 | 0 | 0 | 0 | 0 | 1 | 16.7 | 0.319 |
| 22 | 3 | 42.9 | 1 | 16.7 | 3 | 50 | 0.531 |
% = Percent. Using Chi square test: P ≤ 0.5, P ≤ 0.001 = highly significant
Discussion
During the last two decades, the pathogenic potential of Blastocystis sp. was widely debated in literature because the parasite has been found in both symptomatic and asymptomatic patients (Souppart et al. 2009). Various reports showed that Blastocystis sp. may be associated with some intestinal disorders such as IBS (Eida and Eida 2008) and CRC (Chan et al. 2012).
Discrimination between symptomatic and asymptomatic isolates of Blastocystis sp. has been attempted based on phenotypic characteristics such as protein profiles (Lanuza et al. 1999), serogroups (Müller 1994) and isoenzyme patterns (Gericke et al. 1997) or genotypic characteristics such as molecular profiles and subtype signatures (Stensvold et al. 2007a, b).
The aim of the present work was to study the surface ultrastructure, protein profile and protease activity of Blastocystis isolates from patients having colorectal carcinoma in comparison with those isolated from infected individuals without colorectal carcinoma.
SEM is used to study the surface structural feature of cells while viewing the general morphology. Under SEM, in the present study, Blastocystis organisms from culture showed variation in shape being round, oval, and irregular in shape as was previously reported by Tan et al. (2008), Zhang et al. (2012) and Ragavan et al. (2014). The size range of the organisms in the three groups was similar to that recorded by Zhang et al. (2012) ranging from 5 to 20 μm. Several studies have examined the surface morphology of Blastocystis sp. by SEM (Dunn et al. 1989; Boreham and Stenzel 1993; Suresh et al. 1994; Cassidy et al. 1994; Zaman et al. 1999; Tan et al. 2008; Zhang et al. 2012; Ragavan et al. 2014). In the present study, the smooth surface of Blastocystis sp. in asymptomatic isolates was similarly described previously by Suresh et al. (1994), Tan et al. (2008) and Ragavan et al. (2014) under SEM examination of cultured Blastocystis sp. isolated from asymptomatic carriers. The rougher surface topography of organisms of symptomatic isolates in the present study was first reported in Boreham and Stenzel (1993) who observed rough topography of cells of an isolate from a patient suffering from diarrhea in which Blastocystis sp. was the only parasite seen during detailed stool examination. Tan et al. (2008) and Ragavan et al. (2014) confirmed the presence of differences in the surface ultrastructure of organisms derived from symptomatic and asymptomatic infected persons; organisms of symptomatic isolates have rougher topography while asymptomatic isolates have a smooth surface. More rough with excessive convolutions was the surface described of isolates derived from patients suffering from IBS. In the present study, a very rough surface with excessive convolutions was the characteristic appearance of isolates derived from patients with CRC.
Hence, the current observations, together with the previously reported surface topography of the clinically different isolates, add further weight to a possible relationship between the surface morphology and the pathogenic potential of Blastocystis sp.; however, its significance remains to be elucidated. On the other hand, the different topography of organisms from different clinical conditions may be a consequence to the various intestinal environmental conditions in the different clinical presentation.
Besides morphologic heterogeneity of Blastocystis sp., antigenic heterogeneity was also reported, both between and within geographical regions (Tan 2008; Fadl et al. 2016). In the present study, analysis of the protein profile of Blastocystis isolates was done by SDS–PAGE to investigate the degree of heterogeneity of the parasite and its correlation with clinical conditions of infected patients.
The presence of similar and distinctive antigenic bands in the protein extracts of isolates in the three groups involved in the current study indicated different phenotypes of the isolates. A total of 30 bands were resolved in the protein profiles of the isolates of the three groups. Nearly similar number of bands (31 bands) was previously reported by Lanuza et al. (1999) while only a total of 22 bands were reported in symptomatic and asymptomatic isolates in the study of AbouGamra et al. (2011) and Fadl et al. (2016).
Statistical analysis of protein profiles of isolates in the present study revealed significant differences in one high MW (230 kDa) and few low MW (56, 38, 32 kDa) bands between isolates of the three groups. Protein bands in GII (symptomatic Non-CRC isolates), and GIII (asymptomatic Non-CRC) ranged from 12 to 200 kDa. The same range of protein profile of symptomatic and asymptomatic isolates was reported by Init et al. (2003) and Fadl et al. (2016). The narrower range was reported by Hegazy et al. (2008) and AbouGamra et al. (2011); they reported protein profile ranging between 24 and 130 kDa, and 12–125.5 kDa, respectively.
The present study is the first to investigate the protein profile of CRC-patients-derived Blastocystis isolates. Protein profile of Blastocystis isolates from GI, CRC-patients, ranged from 12 to 230 kDa, with two bands of 230 and 32 kDa significantly present in 42.9% of CRC isolates and completely absent from both groups in GII and GIII (Non-CRC). These two bands could be considered characterizing isolates from CRC patients.
In the present study, a common band with molecular weight of 38 kDa was detected significantly in all isolates (100%) in GIII (Non-CRC asymptomatic) while present in 50% only in GII (Non-CRC symptomatic) and 28.6% in GI (CRC group). This is in contrast to the work of AbouGamra et al. (2011), where this band was found significantly in 80% in symptomatic and only 40% of asymptomatic patients. While in the studies, of Init et al. (2003) and Fadl et al. (2016) the band was reported in all Blastocystis isolates whether symptomatic and asymptomatic.
In the present study, the band 56 kDa was significantly absent completely from GII (Non-CRC symptomatic), while present in 66.7% in GIII (Non-CRC asymptomatic) and in 28.6% of GI (CRC). In the work of AbouGamra et al. (2011), this protein band was present in both symptomatic (100%) and asymptomatic (80%) isolates.
The protein band of 29 kDa that was previously reported in AbouGamra et al. (2011) to be present in all their symptomatic and asymptomatic isolates and could be used by the authors to discriminate between asymptomatic and symptomatic isolates by immunoblotting assay, could not be detected in any isolate in the present study. It is worth mentioning that this band could not be detected, also, in the study of Fadl et al. (2016) in symptomatic and asymptomatic isolates. Instead, a band of 30 kDa was detected, insignificantly, in the present work, only in 33.3% of the Non-CRC symptomatic isolates and also, insignificantly in 9.5% of symptomatic isolates in the study of Fadl et al. (2016). The band of 30 kDa was not detected in asymptomatic isolates in both studies and in the present study could not be detected in GI (CRC group). From this observation, it could be deduced that the band of 29 kDa in AbouGamra et al. (2011)‘s work could be considered replaced by the 30 kDa band in both studies, but of no significance, it could be further investigated for more diagnostic significance. Discrepancies in the protein bands resolved in different studies may be due to differences in concentration of polyacrylamide used in the SDS–PAGE gels as suggested by Lanuza et al. (1999) and Hegazy et al. (2008) or due to the geographical differences between Blastocystis sp. isolates (Chen et al. 1999). Although the four studies carried by Hegazy et al. (2008), AbouGamra et al. (2011) and Fadl et al.(2016) and the present study on the protein profiles of Blastocystis sp. were carried on isolates from Egyptian patients using 12% concentration of polyacrylamide gel, differences in the protein bandings of isolates were reported. This may be due to the genetic diversity of isolates from symptomatic and asymptomatic Egyptian patients.
Marked inter- and intra-subtype variation in cysteine protease production/expression by Blastocystis STs proved that cysteine proteases are essential virulence factors responsible for variation in disease symptoms observed among carriers (Poirier et al. 2012). Based on these data, zymography was performed to compare protease activities in Blastocystis isolates in the three groups in the present study. No significant differences were present between different protease activities in the isolates in the three groups of the study. This may be due to small numbers of isolates in each group. A smaller number of protease activity bands (13 bands), ranging from 22 to 120 kDa, were detected in GIII (Non-CRC asymptomatic) isolates, in contrast to 15 bands detected in isolates of GI (CRC group) and GII (Non-CRC symptomatic). Bands of isolates in GI ranged from 22 to 215 kDa with the 215 kDa band appearing only in this group, while bands of isolates in GII ranged from 22 to 143 kDa. The smaller number of bands in GIII, might be related to the lower virulence of the asymptomatic group isolates. Protease activity at 32 kDa band, which was previously detected by AbdelHameed and Hassanin (2011), and reported by the authors to be of significant value in differentiating between symptomatic and asymptomatic isolates being detected in 61.1% of symptomatic and 12.5% of asymptomatic isolates, was the most frequently detected band in the present study but of no significant difference in existence between GI (CRC group) being present in 71.4%, GII (Non-CRC symptomatic) 66.7% and GIII (Non-CRC asymptomatic) 66.7%.
Conclusion
In conclusion, this work is a preliminary study demonstrating the presence of a significant difference in surface ultrastructure and in protein profiles between Blastocystis sp. of CRC and Non-CRC isolates. It is not known whether these differences develop secondary to the altered gut environment in the presence of CRC or are indicators of the different pathogenic potential of the parasite isolates inducing malignancy. Further work needs to be done to analyze molecular characterization and phylogenetic analysis of zymograms of organisms from CRC isolates.
Acknowledgements
The present work was supported by Ain Shams Faculty of Medicine Grants Office, Grant No. 2016/31.
Compliance with ethical standards
Conflict of interest
The authors declare that they have no conflict of interest.
Research approval and ethical considerations
The research protocol was approved by the Ethics Committee, Faculty of Medicine, Ain-Shams University. A written consent from each participant was obtained after providing a clear explanation of the study.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- Abaza SM, Rayan HZ, Soliman RH, Nemr NA, Mokhtar AB. Subtype analysis of Blastocystis sp. isolates from symptomatic and asymptomatic patients in Suez Canal University Hospitals Ismailia Egypt. PUJ. 2014;7:56–67. [Google Scholar]
- AbdelHameed DM, Hassanin OM. Proteases activity of Blastocystis hominis subtype 3 in symptomatic and asymptomatic patients. Parasitol Res. 2011;109:321–327. doi: 10.1007/s00436-011-2259-x. [DOI] [PubMed] [Google Scholar]
- AbouGamra MM, Elwakil HS, El Deeb HK, Khalifa KE, Abdel-Hafiz HE. The potential use of 29 kDa protein as a marker of pathogenicity and diagnosis of symptomatic infections with Blastocystis hominis. Parasitol Res. 2011;108(5):1139–1146. doi: 10.1007/s00436-010-2156-8. [DOI] [PubMed] [Google Scholar]
- Abu El-Fetouh NI, Abdelmegeed ES, Attia RA, El-Dosoky I, Azab MS. Genotyping of Blastocystis hominis symptomatic isolates and kinetics of associated local CD3 and CD20 cell infiltrate. PUJ. 2015;8:115–122. [Google Scholar]
- Alfellani MA, Stensvold CR, Vidal-Lapiedra A, Onuoha ES, Fagbenro-Beyioku AF, Clark CG. Variable geographic distribution of Blastocystis subtypes and its potential implications. Acta Trop. 2013;126:11–18. doi: 10.1016/j.actatropica.2012.12.011. [DOI] [PubMed] [Google Scholar]
- Arisue N, Hashimoto T, Yoshikawa H, Nakamura Y, Nakamura G, Nakamura F. Phylogenetic position of Blastocystis hominis and of stramenopiles inferred from multiple molecular sequence data. J Eukaryot Microbiol. 2002;49:42–53. doi: 10.1111/j.1550-7408.2002.tb00339.x. [DOI] [PubMed] [Google Scholar]
- Boreham PFL, Stenzel DJ. Blastocystis in humans and animals: morphology, biology, and epizootiology. Adv Parasitol. 1993;32:1–70. doi: 10.1016/S0065-308X(08)60206-7. [DOI] [PubMed] [Google Scholar]
- Bradford MM. Rapid and sensitive method for the quantitation of microgram quantities of protein utilizing the principle of protein-dye binding. Anal Biochem. 1976;72:248–254. doi: 10.1016/0003-2697(76)90527-3. [DOI] [PubMed] [Google Scholar]
- Cassidy MF, Stenzel DJ, Boreham PFL. Electron microscopy of surface structures of Blastocystis sp. from different hosts. Parasitol Res. 1994;80:505–511. doi: 10.1007/BF00932698. [DOI] [PubMed] [Google Scholar]
- Chan KH, Chandramathi S, Suresh K, Chua KH, Kuppusamy UR. Effects of symptomatic and asymptomatic isolates of Blastocystis hominis on colorectal cancer cell line, HCT116. Parasitol Res. 2012;110:2475–2480. doi: 10.1007/s00436-011-2788-3. [DOI] [PubMed] [Google Scholar]
- Chandramathi S, Suresh K, Kuppusamy UR. Solubilized antigen of Blastocystis hominis facilitates the growth of human colorectal cancer cells HCT116. Parasitol Res. 2010;106(4):941–945. doi: 10.1007/s00436-010-1764-7. [DOI] [PubMed] [Google Scholar]
- Chen X, Singh M, Ho L, Tan S, Yap E. Characterization of protein profiles and cross-reactivity of Blastocystis antigens by sodium dodecyl sulfate–polyacrylamide gel electrophoresis and immunoblotting analysis. Parasitol Res. 1999;85:343–346. doi: 10.1007/s004360050559. [DOI] [PubMed] [Google Scholar]
- Clark CG, Diamond LS. Methods for cultivation of luminal parasitic protists of clinical importance. Clin Microbiol Rev. 2002;15(3):329–341. doi: 10.1128/CMR.15.3.329-341.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunn LA, Boreham PFL, Stenzel DJ. Ultra-structural variation of Blastocystis hominis stocks in culture. Int J Parasitol. 1989;19:43–56. doi: 10.1016/0020-7519(89)90020-9. [DOI] [PubMed] [Google Scholar]
- Eida AM, Eida MM. Identification of Blastocystis hominis in patients with irritable bowel syndrome using microscopy and culture compared to PCR. PUJ. 2008;1(2):87–92. [Google Scholar]
- El-Gayar EK, Mahmoud MM. Do protozoa play a role in carcinogenesis? PUJ. 2014;7:80–85. [Google Scholar]
- El-Wakil HS, Talaat RM. Genetic analysis of Blastocystis hominis isolated from symptomatic and asymptomatic human hosts in Egypt. J Egypt Soc Parasitol. 2009;39:99–109. [PubMed] [Google Scholar]
- Fadl HO, El-Akkad DMH, Abd El-Fattah DS, El-Bolaky HA, El-Bassiouni SO. Study of the protein profiles of Blastocystis isolates from symptomatic and asymptomatic subjects. Med J Cairo Univ. 2016;84(3):349–353. [Google Scholar]
- Garcia LS. Diagnostic medical Parasitology. 6. Washington: ASM Press; 2015. [Google Scholar]
- Gericke A, Burchard G, Knobloch J, Walderich B. Isoenzyme patterns of Blastocystis hominis patient isolates derived from symptomatic and healthy carriers. Trop Med Int Health. 1997;2(3):245–253. doi: 10.1046/j.1365-3156.1997.d01-258.x. [DOI] [PubMed] [Google Scholar]
- Hegazy MM, Maklouf LM, El Hamshary EM, Dawoud HA, Eida AM. Protein profile and morphometry of cultured human Blastocystis hominis from children with gastroenteritis and healthy ones. J Egypt Soc Parasitol. 2008;38(2):453–464. [PubMed] [Google Scholar]
- Ho LC, Armiugam A, Jeyaseelan K, Yap EH, Singh M. Blastocystis elongation factor-1alpha: genomic organization, taxonomy, and phylogenetic relationships. Parasitology. 2000;121:135–144. doi: 10.1017/S0031182099006113. [DOI] [PubMed] [Google Scholar]
- Init I, Mak J, Top S, Zulhainan Z, Prummon-Gkol S, Nissapatorn V, Wan-Yussof W, Anuar A. Polypeptides associated with in vitro cyst formation of Blastocystis hominis. Southeast Asian J Trop Med Public Health. 2003;34:727–732. [PubMed] [Google Scholar]
- Kumarasamy V, Kuppusamy UR, Jayalakshmi P, Samudi C, Ragavan ND, Kumar S. Exacerbation of colon carcinogenesis by Blastocystis sp. PLoS ONE. 2017;12(8):e0183097. doi: 10.1371/journal.pone.0183097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laemmli UK. Cleavage of structure proteins during the assembly of the head of bacteriophage T4. Nature. 1970;227:680–685. doi: 10.1038/227680a0. [DOI] [PubMed] [Google Scholar]
- Lanuza MD, Carbajal JA, Villar J, Mir A, Borrás R. Soluble protein and antigenic heterogeneity in axenic Blastocystis hominis isolates: pathogenic implications. Parasitol Res. 1999;85:93–97. doi: 10.1007/s004360050515. [DOI] [PubMed] [Google Scholar]
- Mohamed AM, Ahmed MA, Ahmed SA, Al-Semany SA, Alghamdi SS, Zaglool DA. Predominance and association risk of Blastocystis hominis subtype I in colorectal cancer: a case-control study. Infect Agents Cancer. 2017;12:21. doi: 10.1186/s13027-017-0131-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Müller H. Four serologically different groups within the species of Blastocystis hominis. Zentralbl Bakteriol. 1994;280:403–408. doi: 10.1016/S0934-8840(11)80604-3. [DOI] [PubMed] [Google Scholar]
- Nagel R, Cuttell L, Stensvold CR, Mills PC, Bielefeldt-Ohmann H, Traub RJ. Blastocystis subtypes in symptomatic and asymptomatic family members and pets and response to therapy. Intern Med. 2012;J42:1187–1195. doi: 10.1111/j.1445-5994.2011.02626.x. [DOI] [PubMed] [Google Scholar]
- Parija SC, Jeremiah SS. Symposium on Blastocystis: taxonomy, biology, and virulence. Trop Parasitol. 2013;3:17–25. doi: 10.4103/2229-5070.113894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Poirier P, Wawrzyniak I, Viverès CP, Delbac F, El Alaoui H. New insights into Blastocystis sp.: a potential link with irritable bowel syndrome. PLoS Pathog. 2012;8(3):e1002545. doi: 10.1371/journal.ppat.1002545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ragavan ND, Govind SK, Chye TT, Mahadeva S. Phenotypic variation in Blastocystis sp. ST3. Parasites Vectors. 2014;7:404. doi: 10.1186/1756-3305-7-404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramírez JD, Sánchez A, Hernández C, Flórez C, Bernal MC, Giraldo JC, Reyes P, López MC, García L, Cooper PJ, et al. Geographic distribution of human Blastocystis subtypes in South America. Infect Genet Evol. 2016;41:32–35. doi: 10.1016/j.meegid.2016.03.017. [DOI] [PubMed] [Google Scholar]
- Scanlan PD. Blastocystis past pit falls and future perspectives. Trends Parasitol. 2012;28:327–334. doi: 10.1016/j.pt.2012.05.001. [DOI] [PubMed] [Google Scholar]
- Silberman JD, Sogin ML, Leipe DD, Clark CG. Human parasite finds taxonomic home. Nature. 1996;380:398. doi: 10.1038/380398a0. [DOI] [PubMed] [Google Scholar]
- Souppart L, Sanciu G, Cian A, Wawrzyniak I, Delbac F, Capron M, et al. Molecular epidemiology of human Blastocystis isolates in France. Parasitol Res. 2009;105:413–421. doi: 10.1007/s00436-009-1398-9. [DOI] [PubMed] [Google Scholar]
- Steer H. Blastocystis hominis and Colorectal Cancer. Ann R Coll Surg Engl. 2007;89:539. doi: 10.1308/003588407X202155. [DOI] [Google Scholar]
- Stensvold CR. Blastocystis-genetic diversity and molecular methods for diagnosis and epidemiology. Trop Parasitol. 2013;3:26–34. doi: 10.4103/2229-5070.113896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stensvold CR, Arendrup MC, Jespersgaard C, Mølbak K, Nielsen HV. Detecting Blastocystis using parasitologic and DNA-based methods: a comparative study. Diagn Microbiol Infect Dis. 2007;59:303–307. doi: 10.1016/j.diagmicrobio.2007.06.003. [DOI] [PubMed] [Google Scholar]
- Stensvold CR, Suresh GK, Tan KS, Thompson RC, Traub RJ, et al. Terminology for Blastocystis subtypes a consensus. Trends Parasitol. 2007;23:93–96. doi: 10.1016/j.pt.2007.01.004. [DOI] [PubMed] [Google Scholar]
- Suresh K, Howe J, Chong SY, Ng GC, Ho LC, Loh AK, Ramachandran NP, Yap EH, Singh M. Ultra-structural changes during in vitro encystment of Blastocystis hominis. Parasitol Res. 1994;80:327–335. doi: 10.1007/BF02351875. [DOI] [PubMed] [Google Scholar]
- Tan KS. New insights on classification, identification, and clinical relevance of Blastocystis sp. Clin Microbiol Rev. 2008;21:639–665. doi: 10.1128/CMR.00022-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tan TC, Suresh KG. Predominance of amoeboid forms of Blastocystis hominis in isolates from symptomatic patients. Parasitol Res. 2006;98:189–193. doi: 10.1007/s00436-005-0033-7. [DOI] [PubMed] [Google Scholar]
- Tan TC, Suresh KG, Smith HV. Phenotypic and genotypic characterization of Blastocystis hominis isolates implicates subtype 3 as a subtype with pathogenic potential. Parasitol Res. 2008;104:85–93. doi: 10.1007/s00436-008-1163-5. [DOI] [PubMed] [Google Scholar]
- Toth M, Fridman R. Assessment of gelatinases (MMP-2 and MMP-9) by gelatin zymography. Methods Mol Med. 2001;57(10):160–163. doi: 10.1385/1-59259-136-1:163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Upcroft JA, Dunn LA, Dommet LS, Healey A, Upcroft P, Boreham PFL. Chromosomes of Blastocystis hominis. Int J Parasitol. 1989;19:879–883. doi: 10.1016/0020-7519(89)90114-8. [DOI] [PubMed] [Google Scholar]
- Wu Z, Mirza H, Tan KSW. Intra-subtype variation in entero adhesion accounts for differences in epithelial barrier disruption and is associated with metronidazole resistance in Blastocystis subtype-7. PLoS Negl Trop Dis. 2014;8:e2885. doi: 10.1371/journal.pntd.0002885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu Z, Mirza H, Teo JDW, Tan KSW. Strain-dependent induction of human enterocyte apoptosis by Blastocystis disrupts epithelial barrier and ZO-1 organization in a caspase 3- and 9-dependent manner. Biomed Res Int. 2014 doi: 10.1155/2014/209163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yason JA, Tan KSW. Membrane surface features of Blastocystis subtypes. Genes. 2018;9:417. doi: 10.3390/genes9080417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zaman V, Howe J, Ng M, Goh TK. Scanning electron microscopy of the surface coat of Blastocystis hominis. Parasitol Res. 1999;85:974–976. doi: 10.1007/s004360050668. [DOI] [PubMed] [Google Scholar]
- Zhang X, Zhang S, Qiao J, Wu X, et al. Ultra-structural insights into morphology and reproductive mode of Blastocystis hominis. Parasitol Res. 2012;110:1165–1172. doi: 10.1007/s00436-011-2607-x. [DOI] [PubMed] [Google Scholar]