Abstract
Resistance exercise bands are a core component of any physical activity strengthening program. Strength training can mitigate the development of sarcopenia, the loss of muscle mass or strength and function with aging. Yet, the adherence of such behavioral exercise strategies in a home-based setting are fraught with issues of monitoring and compliance. Our group developed a Bluetooth-enabled resistance exercise band capable of transmitting data to an open-source platform. In this work, we developed an application to capture this information in real-time, and conducted three usability studies in two mixed-aged groups of participants (n=6 each) and a group of older adults with obesity participating in a weight-loss intervention (n=20). The system was favorable, acceptable and provided iterative information that could assist in future deployment on ubiquitous platforms. Our formative work provides the foundation to deliver home-based monitoring interventions in a high-risk, older adult population.
Keywords: Application, mHealth, older adult, resistance exercise band, sarcopenia
I. Introduction
SARCOPENIA is the loss of muscle mass, strength and/or function with aging [1] and is strongly associated with an increased risk of disability, morbidity and mortality [2], [3]. Resistance exercises incorporating the use of free weights or resistance exercise bands are proven modalities that alter the trajectory of the loss of function accompanied by changes in muscle physiology [4]. Typically, these weights or bands are used in behavior-based programs [5], including those conducted at senior or community centers. Older adults can greatly benefit from their use and they have been shown to increase their physical function and overall quality of life [6].
In-person exercise regimens enhance compliance through engagement, monitoring, and feedback [7], [8]. As a lack of transportation is a major barrier for older adults, in-person session attendance is often difficult, particularly in rural, remote areas [9]. This creates a major gap in a population that is at high risk of disability. One potential solution is deploying a device at home that can capture clinically relevant exercise data.
In this work, we built an application that can acquire an individual’s ability to perform such exercises on the pre-existing Amulet platform [10] (see Background). Our team previously created a connected, Bluetooth-enabled resistance exercise band capable of relaying repetitions, measuring of relative force, and frequency of use [11], [12]. This specific contribution applies user-centered design principles [13] in two groups of mixed-aged persons, and in a third cohort of older adults with obesity participating in a weight-loss intervention. The goal of this work was to develop a formative application able to capture such data. This institutional review board approved study allowed the use of mixed-methods [14] (qualitative and quantitative), to evaluate this new application. This application ultimately permits us to gain data related to the type of band, the type of exercise performed, and the degree of relative force generated. We then would be able to use a cloud-based, machine-learning algorithm to analyze the data that ultimately can convey this information to practicing clinicians.
In the remaining paper, we describe a number of components that are essential in gaining an understanding of the formative nature of this work. We describe related work on the Amulet platform and use of resistance bands. The work is dependent on a systems engineering framework [15] of user-centered design that ultimately uses the end-user in the development of the application and its functions. We subsequently delineate the limitations and future work.
II. Background
We describe in this section the Amulet platform on which the Connected Resistance Exercise Band application operates, and how this platform allowed us to fulfill the goals of this project. We discuss the use of resistance exercise bands, the device we created to ascertain strength, and the need to develop mHealth technologies for older adults and their design challenges.
A. Amulet Wearable Device Platform
The Amulet is an open-source hardware and software platform for writing energy- and memory-efficient sensory applications [10]. It is a wrist worn device with built-in sensors and peripherals that include on its main board: an accelerometer, buttons, capacitive touch slider, haptic buzzer, two LEDs embedded in the case, and a battery. The hardware also contains two microcontrollers including an MSP430 running applications and an nRF51822 for communicating with peripheral Bluetooth Low Energy (BLE) devices. A secondary storage board consists of a micro-SD card reader and a low-power display screen. This is an energy-efficient platform that is useful in the development of mHealth applications that can monitor physiological and behavioral health of the wearer, lasting days to weeks prior to needing recharging (Fig. 1).
Fig. 1.

(a) Fully assembled Amulet device; (b) internal Amulet peripherals; (c) screen; (d) case
B. Resistance Exercise Bands & Exercise Types
A number of commercially available exercise bands are available, both in tubing and in latex band forms. These are all very affordable (i.e., 25 feet cost ~$20 USD) and easily attached to handles. Such bands are available in different colors which represent different levels of resistance (i.e., yellow, red, green, blue, black). A given patient may increase the color of band throughout their exercise program suggesting an improvement in strength. Resting length of the band is usually defined as the length of the unstretched tubing. Each of these tubings can extend up to 200% in length. Previously published equations have demonstrated a relationship between elongation percentage ((final – initial length) ÷ initial length) and force [16].
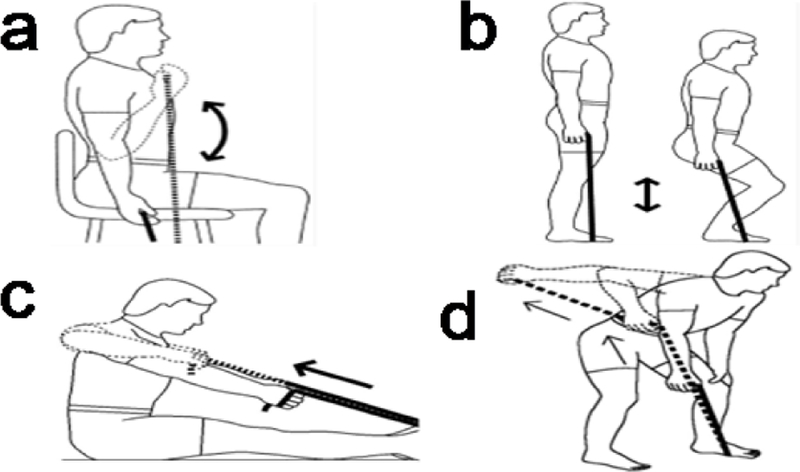
Resistance band usability has been established [17], [18] and they are common elements in any physical activity resistance program for older adults. Physical therapists use these bands to enhance current exercise strategies. The four most commonly performed exercises are bicep (elbow) flexion, abduction (shoulder lift), elbow extension (seated rows) and elbow kickback or tricep extension (see Fig. 5).
Fig. 5.
Representative exercises conducted to evaluate the TheraBand application as part of the Usability Assessment: a) Bicep flexion; b) abduction or shoulder lift; c) elbow extension or seated rows; and d) elbow kickback or tricep extension)
C. Older Adults and Technology
Older adults aged 65 and older are the fastest growing group using information and communication technologies [19]. This is in direct contrast to the belief that this group has considerable difficulties and aversion to using such tools. As this population has considerable number of medical comorbidities and health conditions, it is currently a target for emerging mHealth applications for health monitoring [20]. Older adults, though, have a considerable number of sensory and motor challenges (i.e., hearing or vision impairment, sensory neuropathies or numbness, arthritis) that prevent the typical usage of routine technologies [21], [22]. Hence, ease of use is a significant factor in developing such technologies, mandating the need for using the end-user as part of the prototype development and design process [23].
D. Bluetooth-Enabled Resistance Band
This previously described device was a joint venture between Dartmouth-Hitchcock and the Thayer School of Engineering at Dartmouth College (Fig. 2) [12]. Briefly, we used a commercially available Green TheraBand rated for 4.6 lbs of resistance at 100% elongation. This tubing was connected to a Tekscan FlexiForce A201 sensor whose detection ranges from 0–25 lbs. Force is applied between the resistance tube’s end and the handle when the device is in use. Relative force was collected at a rate of 10 readings per second and can be sent to any BLE device. Data was ported through a custom PCB to a RedBear BLE Nano device powered by a Lithium-ion battery, then wirelessly visualized in real-time through an application.
Fig. 2.

Bluetooth Resistance Exercise Band
E. Amulet-Related Applications
Our previous work has successfully allowed us to create specific applications for the Amulet device. We developed both ActivityAware and GeriActive meant to assess daily activity levels. A Support Vector Machine activity-level detection model was used to train the model using volunteer subjects performing common physical activities (sit, standing, laying down, walking, running), and an accuracy of 94.3% with a leave-one-subject-out cross-validation. The preliminary feedback demonstrated the potential to be usable and useful, with a battery life of over one week. This work suggests the feasibility of being able to create an application, unique to older adults using the Amulet platform.
III. Related Work
There have been very few BLE connected devices that send data to the user. Also, we present data below on related Amulet-related applications and usability assessments in older adults from our group that support the development of this work.
A. Current Resistance Band-Connected Devices
The ability to measure relative force for immediate feedback is a novel contribution of this technology. These designs are generally bulky, and are ergonomically problematic. Two products have shown potential to transmit fitness data to smartphone applications: LiftUp and Xiaomi [24], [25]. To our knowledge, the only device that is available commercially is the Rolyan Smart Handle (Performance Health, Warrenville, IL) [26]. This version permits remote feedback by displaying the peak relative force of a repetition of a given exercise using a flat elastic TheraBand connected to a bulky, rigid handle. Only the last set of numbers can be transmitted to their custom, proprietary application. All data ultimately must be manually offloaded before the device is turned off. The Rolyan device is meant to be a multi-patient mHealth device rather than a unique device per person.
B. Monitoring of Activity Using the BLE-Enabled Device
A feasibility evaluation using the BLE-enabled resistance exercise band on six older adults permitted recruitment as part of an existing weight-loss study [27]. The goal of this study was to lose weight and improve muscle strength. Each subject connected the device to an iOS Lightblue application after its demonstration by an instructor, completing all four exercises each. Data was evaluated using a peak detection algorithm that determined the number of repetitions – defined as a peak of the measured relative force exerted on the connected exercise band (Fig. 3). This algorithm consisted of a local regression (LOESS) smoothing with a second-degree polynomial term. Noise was assessed as the ratio of the LOESS smoothed to recorded value, and signal to noise ratio was subsequently assessed. The mean number of repetitions were evaluated for each exercise (mean 16.76±1.71), and the intraclass correlation between blinded readers was 0.899 (95% CI: 0.824,0.947; p<0.001). Mean signal-to-noise ratio ranged between 1.06±0.09 to 1.29±0.27. Mean differences between the maximal and minimal peaks (and their corresponding standard deviations for each of the four exercises were: 66.71±42.19, 34.00±30.74, 18±10.75, and 23.71±20.37. This study demonstrated the feasibility of capturing such data using BLE and the ability to algorithmically ascertain the number of repetitions and duration of exercises. It also demonstrates that the dynamics of each exercise may need to be accounted for in future testing and could be used in prediction modeling.
Fig. 3.

Example of Recorded Relative Force for Exercises performed by the BLE-Enabled Device [27]
C. Desire of Older Adults and Technology
Our group has conducted a number of studies evaluating the feasibility and usability of mHealth technologies in older adult populations. We conducted qualitative interviews in a group of 29 patient participants aged 72.9±4.6 years using the Amulet platform [28]. Questions focused on the importance of using a broad range of applications and devices for healthy aging and wellness. We identified the following features that are important to this population: i) need to track, monitor and have visual representation of data; ii) the importance of a usable and esthetically pleasing interface that could be used with the population’s sensory abnormalities; iii) the need to view data off the device, on a specific dashboard on a phone, desktop, or tablet; iv) relaying of information to the participant’s provider; and v) the desire to track information other than steps or physical activity. This study suggests that applications could be developed using the Amulet platform that could address these shortcomings.
IV. Study Goals
Based on the preliminary data, there was a need to develop an application that captures such data on a longitudinal basis, with minimal effort or input by the patient participant. Our goal was to develop the TheraBand application using the open-source Amulet platform. We used an adaptive systems engineering framework [15] and user-centered design principles [29] to guide the multi-stage, iterative design. This transdisciplinary process includes user input throughout the development. We conducted three separate evaluations using distinct sets of participants with an intent of improving the application, its esthetics, and its usability.
V. Study Methods, Application Development & Assessment
A. Study Setting
We collected data from 32 volunteer subjects under a study protocol approved by the Committee for the Protection of Human Subjects at Dartmouth College, and the study protocol was conducted at the Centers for Health and Aging, at Dartmouth-Hitchcock Medical Center. The center is located on the New Hampshire/Vermont border in a geographically isolated area, over two hours away from the closest urban centers.
B. Patient Participants
Usability studies are generally recommended to have at least five participants in each iteration so as robust conclusions can be drawn and for key usability factors to be identified that otherwise would prevent usage of an application in the future [30]. The larger the number of users testing a given system, the more likely the study will capture the ability to reach construct saturation. With each set of individuals’ feedback, we made additional modifications, developing a subsequent version of the application.
All participants were volunteers recruited locally at the local center or through clinician referral at the medical center. Three groups of patient participants participated as part of this design process: two groups (n=6 each) of mixed aged adults (younger: <65 years; and older than age ≥65 years (n=6); and a group of older adults (≥65 years) with obesity with a body mass index ≥ 30kg/m2 (n=20). To enhance the generalizability of the application’s usage, we had no specific restrictions on our study population’s selection criteria other than age for a specific cohort. We documented the person’s age, sex, race, and Hispanic status.
C. TheraBand Application Goals and Development
The Amulet’s TheraBand application had a number of goals to address: i) connect to the BLE resistance exercise band; ii) record the relative force exerted while performing each of the four sets of exercises; iii) logging of the data for analysis on a micro-SD card located within the Amulet folder; and iv) displaying summary information about the relative force on the device’s display through the application. Once the application was designed, the purpose was to assess its usability.
We then programmed the application with QP Modeler (QM), a software development environment used for the application development on the Amulet platform. QM is a freeware graphical modeling tool for implementing and designing real-time embedded software in C or C++ based on hierarchical state machines and event-driven QP real-time frameworks.
D. Final Connected TheraBand Application
The Connected TheraBand application was designed to contain various states corresponding to different functionality (Fig. 4). The TheraBand application starts in the “off” state. Pressing the lower left button on the Amulet initiates the application, switching it to the “connection” state in which the Amulet tries to connect with the TheraBand device using BLE. Once the connection is established, the red LED light turns on, at which time the application switches to the “view exercises” state. In this state, the user can view the trends of the maximum relative force exerted for each of the four exercises. The user then presses the button to toggle to the “choose exercise state” at the time they are ready to perform an exercise. In this state, the user then selects the exercise that is about to be performed using the slider. The user then presses the lower left button to switch to the “choose band color” state, where they select the TheraBand’s color using the slide. The user then presses the button to switch to the “summary state” where a summary is displayed of the selected exercise and band color. A user can then switch to the previous study state, adjusting and altering it with the slider.
Fig. 4 (a).

Snapshot of TheraBand application states: Off (a); Connection (b); View of band color (c); Initiation of Exercise (d)
E. User-Centered Design Procedures
After voluntary agreement to join the study, we provided all individuals a research project information sheet. Each participant was compensated $10 for their time at the conclusion of the study. We provided all participants with an Amulet with the TheraBand application which all wore on their dominant hand. Participants were also video-recorded as part of these activities – which was agreed to in advance.
The study personnel showed each participant the TheraBand to provide them an opportunity to look at the device, in addition to be able to try the device. No formal evaluation was conducted at this time. We instructed all participants that the purpose of the study was to evaluate and test our newly designed application. A brief description regarding the overall intent of the study and its results was provided to participants. We described what the process of the study would entail including a description of the protocol that follows. We conducted a “Think aloud” usability test, used in previous research [31] that can facilitate the detection of design issues. The overall duration of testing lasted between 20 and 30 minutes.
The study staff was trained by the lead author (J.A.B) on how to conduct a usability assessment, importantly, noting the importance of minimizing conversation by the staff allowing the participant to express their thoughts. The TheraBand was connected to the Amulet by the study personnel with the patient present after which the navigation of the application was demonstrated. During the recorded session, the participant was asked to do the following tasks, as study personnel noted their reactions, thoughts, and comments were recorded by the study personnel: a) asked participants to look at the face screen of the application; b) inform the participant how it is shown that the TheraBand is connected; c) scrolling up/down to view the exercise and the graph; d) pressing the buttons to select a given exercise; e) move the slider to choose an exercise and/or return back to the previous screen; f) comment on the haptic vibration with each screen change; g) ability to choose an exercise; h) opinion on the LED light; i) how to end the exercise; j) how to disconnect the TheraBand. We also asked them to retrace the steps following this Think Aloud protocol and identified the steps and places where it was most challenging for the patient. This “teach-back” method has been used successfully in ascertaining understanding of situations (i.e., informed consent [32]. Each individual was asked to perform each of the exercises shown in Fig. 5, and asked to use the TheraBand application accordingly.
F. Quantitative Surveys & Subjective Interview Questions
Each participant completed a set of numerical surveys evaluating the usability of the TheraBand application. Single item questions evaluated specific components of the application on a Likert scale of 1 to 10. Participant confidence in using the application, their overall satisfaction and the perceived helpfulness in using this application with the BLE-enabled TheraBand were asked on a scale of 1 to 10. The System Usability Scale is a 10-item questionnaire asking individuals to assess the system on a 5-point scale (strongly agree, agree, neutral, disagree, strongly disagree). The scale is an industry standard that is used on small sample sizes, with scores ranging from 0–100 [33]. Items from the Post-study System Usability Questionnaire [34] is a 19-item (range of 1–7) developed by IBM. This scale provides an overall satisfaction, system usefulness, information quality and inference score. There were nine items used in this evaluation. Finally, we assessed whether the application: a) was easy to navigate; b) was clear and consistently able to return to a previous screen; c) was clearly labeled (i.e. text); d) interface/screen appropriate; e) labeling and font size clear and concise; f) text was easy to understand; and g) font size and spacing easy to read.
At its conclusion, individuals engaged in an open-ended interview, answering qualitative questions including: the participant’s overall impression of the application; the overall impression of the TheraBand; how easy the application was to use; and to list the most positive and negative aspects of the application. All interview sessions were video-recorded and transcribed by study staff.
VI. Data Analysis
All data was aggregated and entered into a Microsoft Excel spreadsheet, after which it was imported into STATA (version 14, College Station, TX). Descriptive statistics described the study cohort using mean ± standard deviation, and counts (percentages). Scales were aggregated and missing data was imputed using the unconditional mean imputation method. Qualitative comments were transcribed and grouped by concepts in three major categories.
VII. Cycle i – Younger & Older Adults
Our first cohort of six adults (age range 25–83, 80% female) felt that the screen was appropriate in size, the font and its size made it reasonable to read, and that pushing the button allowed for participant input. A number of suggestions were provided to improve the initial formative design. Participants felt the need for a back button should an error be made, specifically if an incorrect exercise was selected. The touch slider on the device was difficult to maneuver and participants preferred the use of a button than the slider. Some preliminary changes in text (change BTN to Button) were made to increase readability. Participants liked the graphical representation of the data; yet they expressed preference having this graph presented at the conclusion of the exercise. Their feelings were that at the time of this evaluation, the graph presented itself on the screen at the same time as the conduct of the exercises. This mixed aged population was generally encouraging in proceeding with the application development.
VIII. Cycle ii – Younger & Older Adults
We made changes to the application to adapt for the aforementioned concerns and conducted a usability assessment on a mixed population of both younger and older adults (age range 24–71 years; 80% female).
General comments included that the system was very simple to use and easy to learn. The fonts were appealing as they were large. However, this cohort was much more critical in their assessment. First, the participants wanted clarity on the type of exercise. Second, the abbreviation of certain terms were unclear (Exercise 1, 2, 3 or 4). Third, the top button on the Amulet confused individuals as to its function.
A number of changes were made at this stage. The existing numeric exercise labels were replaced with the names of the exercise. To promote future sustainability and use of different color bands, a separate screen including the option to select the band color included. Vibrations were eliminated – patients felt that this was distracting to the overall purpose of the application’s function. Wording was changed from “Press Button to Start” to “View Exercise.” Finally, the application screens were altered to allow the connection of the TheraBand throughout the duration of performing exercises. We found no statistical differences in any of our usability parameters between younger or older adults among Cycle I or Cycle II.
IX. Cycle III–Older Adults with Obesity
The final testing permitted some minor modifications to optimize the application in this formative development. There were 20 older adults (mean age 70.3±15.9 years, 75% female) who assessed the application after all the changes applied in the above iterations. The final changes performed included: a) changing the position of the graph to not appear after the home screen but to be shown at the conclusion of the exercises; b) that the exercise list should come up after the home screen; c) eliminate duplication of two similar screens; d) ensuring that there are options at each step of the application to navigate back to the main (home) screen; and e) permitting scrolling either using the slider or the button to choose the specific exercise. A number of useful qualitative comments were provided by participants. We list some representative comments in Table I.
TABLE I.
Selective Qualitative Comments from Cycle 3 Participants
| Domain | Representative Comments |
|---|---|
| Overall | I like being able to use metrics. |
| I am looking forward to using it. | |
| I want this app – I think it would be fun to use and motivating. | |
| Positive Feedback | Very updated – would be great to keep track of movement and exercise. |
| The app was quite easy to use overall but would need to use it a second time to master it better. | |
| Negative Feedback | Real-time data would be difficult to see during exercise – ideal to have a dashboard. |
| Need detailed instructions and time to absorb and learn. | |
| With the exception of the slider, the app seems relatively easy to use. |
X. Results from the Three Usability Cycles
Tables II and III represent the quantitative survey data from all three usability cohorts, separately presenting both means ± standard deviation for each of the questions. There were no differences in tasks across each cohort among any of the selected tasks listed in Table II (all p>0.05). All tasks had favorable ‘ease,’ except for scrolling up/down to choose the exercise, its selection, and wanting to start the exercise.
TABLE II.
Selective User Tasks of Theraband Application (Scored 1 to 10)
| Cohort #1 | Cohort #2 | Cohort #3 | ||||
|---|---|---|---|---|---|---|
| Task | Mean ± SD | Median (IQR) | Mean ± SD | Median (IQR) | Mean ± SD | Median (IQR) |
| Scrolling up/down to choose exercise | 6.83 ± 2.79 | 8 [5–9] | 7.33 ± 2.34 | 8 [5,9] | 6.35 ± 2.7 | 6.5 [5,8] |
| Selection of exercise | 6.5 ± 2.81 | 8 [4–8] | 8.2 ± 1.83 | 8 [8,10] | 7.6 ± 2.48 | 8 [6,9.5] |
| Connection screen | 8.5 ± 1.87 | 9 [8–10] | 9 ± 1.26 | 9 [5–10] | 8.8 ± 1.61 | 9.5 [8,10] |
| Turning TheraBand ‘on’; button | 9.17 ± 0.98 | 9.5 [8–10] | 9.4 ± 0.81 | 9.5 [9.1–10] | 9.0 ± 1.47 | 9.5 [8.5, 10] |
| Selection of wanting to start exercise | 8 ± 2.28 | 10 [9,10] | 9.66 ± 0.82 | 10 [10,10] | 7.2 ± 2.54 | 8 [5,9] |
| Viewing of the graph | 9.5 ± 0.84 | 10 [9–10] | 6.67 ± 3.78 | 8 [3,10]] | 8.2 ± 2.72 | 10 [6,10] |
| Vibration when changing | 7.83 ± 3.54 | 9.5 [7–10] | 7.2 ± 3.54 | 8.5 [5,10] | 8.2 ± 2.73 | 10 [8,10] |
| Going back to main screen | 8.17 ± 1.17 | 8 [7–9] | 6.8 ± 3.19 | 7.5 [6,9] | 8.4 ± 1.75 | 9 [8,10] |
| Light on when connected | 8.5 ± 1.52 | 8.5 [8–10] | 8.67 ± 1.97 | 9.5 [8,10] | 9.0 ± 1.54 | 10 [8.9,10] |
| Back button | 8 ± 1.67 | 8 [8–9] | 5.83 ± 3.97 | 7 [1,9] | 8.44 ± 1.33 | 9 [8,10] |
Cohort 1 – Older adults; Cohort 2 – Younger Adult; Cohort 3 – Older adults with obesity. All items are evaluated on a 1 to 10 Likert scale, where 1 indicates “very difficulty” and 10 indicates “very easy”. Median and interquartile range (IQR) are represented.
TABLE III.
Representative User Opinions of Theraband Application Features
| Opinion on Specifics of Application | Cohort #1 | Cohort #2 | Cohort #3 | |||
|---|---|---|---|---|---|---|
| Mean ± SD | Median (IQR) | Mean ± SD | Median (IQR) | Mean ± SD | Median (IQR) | |
| Is the app easy to navigate? | 7.83 ± 2.99 | 8.5 [8,10] | 6.83 ± 3.66 | 8 [6,9] | 7.3 ± 2.52 | 8 [6.5,9] |
| Is there a clear and consistent way to go back on every screen? | 8.33 ± 1.37 | 8 [7,10] | 3.5 ± 4.42 | 1.5 [0,9] | 6.15 ± 2.89 | 9 [7,9] |
| Are the labels and buttons text clear and concise? | 6.33 ± 3.93 | 7.5 [2,10] | 5.67 ± 3.61 | 4.5 [3,10] | 7.0 ± 2.90 | 8 [5,9] |
| Is the number of buttons reasonable? | 9.17± 0.98 | 9.5 [8,10] | 6.67 ± 4.27 | 8.5 [3,10] | 8.0 ± 2.0 | 8.5 [6.5,10] |
| Is the interface/screen appropriate? | 8.67 ± 1.75 | 9.5 [7,10] | 8.17 ± 4.02 | 10 [9,10] | 7.3 ± 2.5 | 8 [6,9] |
| Is the text easy to understand? | 8 ± 3.16 | 9.5 [7,10] | 8.5 ± 2.81 | 10 [8,10] | 7.3 ± 2.81 | 8 [5.5,9.5] |
| Is the font size and spacing lead to good readability? | 9.17 ± 1.33 | 10 [8,10] | 9.7 ± 0.82 | 10 [10,10] | 7.1 ± 3.32 | 8 [5.5,10] |
| I am confident that I will be able to use this system. | 9.16 ± 0.98 | 9.5 [8,10] | 7.8 ± 2.43 | 8 [8,8.6] | 8.6 ± 1.6 | 9 [8,10] |
| I am satisfied with how easy it is to use the system. | 7.83 ± 1.47 | 7.5 [7,9] | 6.49 ± 2.22 | 7.3 [7,7.3] | 7.4 ± 2.37 | 8 [5,9] |
| I think this application will be helpful for me. | 7.1 ± 2.21 | 7.8 [5,8] | 6.32 ± 3.11 | 7.6 [7,7.63] | 8.18 ± 2.44 | 9 [7.9,10] |
Cohort 1 – mixed-aged cohort; Cohort 2 – mixed-aged cohort; Cohort 3 – older adults (age ≥ 65 years) with obesity. All items are evaluated on a 1 (strongly disagree) to 10 (strongly agree) Likert scale. Median and interquartile range (IQR) are also represented.
Table III outlines specific user opinions of the application’s features. There were no differences in scoring across each of the three usability cohorts (all p>0.05). Participants identified navigating between screens (range 3.5–8.33) and the buttons on the Amulet (5.67–7.0) as being somewhat problematic. Confidence and satisfaction in using the system were high at 8.6±1.6 and 7.4±2.37, respectively, in the last cohort. The older adult cohort (Cohort 3) felt that the application could be helpful.
The distinct usability scales administered to the participants demonstrated guarded scores. The System Usability scale scoring was 64.6±20.3, 60.9±13.2, and 64.6±15.6, in the three cohorts, respectively (p=0.88). The Post-Study System Usability questionnaire demonstrated non-significant trends (p=0.61) across the three usability studies around the median mark (range: 2.56–2.78).
XI. Discussion
This usability study on the connected resistance band application provides constructive information that could permit further development and deployment in future commercial systems for home-based use. Using the amulet prototype device provides a foundation that will allows the application to be transferred to more ubiquitous devices, surmounting challenges of design observed in prototypes. The content of the application was favorable and that the basic functions were easy to use beyond the functions of the scrolling, which we believe were highly dependent on hardware features of the proposed amulet.
Our system has the capability of monitoring repetitions and relative force in real-time, a feature that has not yet been explored to our knowledge in other developments. The system provides immediate feedback to the participant regarding progress in exercise. The usability data suggests older adults were able to navigate its usage, overcoming doubts of technology literacy in older adults.
A major advantage of using the amulet platform is its ability to create open-source applications, unlike other fitness devices like other commercial devices. Hence, we are able to explore patterns that otherwise would not be able to be captured using proprietary devices. Additional features to prompt individuals in future iterations of the application can be integrated to promote compliance and encourage physical activity.
This study incorporates the end-user in its development. While our earlier usability assessments had mixed-aged cohorts, the latter cohort of older adults is more representative of the target population we will use in our future studies. Understanding the differences in the design and its appeal is critical in the forthcoming stages of application development.
XII. Limitations of the Current Approach
Our experimental approach has several limitations. The conducting of usability studies in a laboratory-based controlled environment may provide different data and results than that observed in a free-living setting. We recognize that we had different numbers of subjects in each of our usability cohorts and the characteristics of each of these persons are likely different, yet this may enhance generalizability. We based our recruitment strategies on convenience sampling in a target population; hence, it is unclear whether our study population is truly representative of the general older adult population.
The current application operates only on the amulet platform. This significantly limits generalizability and scalability for future use. This current application needs optimization to view and record data over longer periods of time. A current data-pipeline does not exist connecting such data to cloud-based servers that can potentially conduct computational analysis that are resource intense. We anticipate that these barriers are surmountable in future studies.
The current application is optimized for only four types of bands and exercises. There are additional bands and exercises available and are conducted; these should be considered in future studies. The amulet display is in black and white and not in color which limits the positive esthetics of the current approach. As part of this pilot project, we aimed to limit our scope and design to components that can readily be applied on more ubiquitous platforms in the majority of the population.
XIII. Future Directions
This preliminary work provides considerable promise to extend this line of research both in terms of advancing the capabilities of the BLE-enabled TheraBand, but also in enhancing the design of the application. To enhance widespread generalizability, our next steps are to adapt this application to function on ubiquitous platforms such as an iOS or Android. The additional practical design issues that must be addressed with the device may have potentially undermined the favorability of the application. Future integration and programming into a commercial platform will provide more pragmatic and real-world feel of this application.
Our team’s ultimate goal is to develop a multi-component, home-based exercise intervention in older adults using this application. We strongly believe that such technologies could successfully act as a behavioral adjunct to current health promotion interventions in older adults. Once established, the application could potentially lead to the development of a patient/clinician dashboard permitting the bi-directional feedback. The application can be adapted for other strategies designed to examine effectiveness and mechanisms most critical to changing behavior at home. Long-term, this line of research has the potential to improve the health of a rapidly aging population at risk for sarcopenia [35]
While outside the scope of this current study, improving the application of algorithms to identify, classify and report specific data by accounting for the inter-person and inter-exercise variation will enhance the clinical impact this system can have. Utilizing a cloud-based infrastructure will allow for real-time assessment and feedback increasing the utility to patients and clinicians. Our research fills a gap by developing the first step in creating an application allowing clinician-patient feedback of resistance exercise programs using a BLE Resistance Band in patients at-risk for sarcopenia. This work also provides foundational information on the features and components most important in a home-based physical therapy delivery system. The application and device may surmount problems of delivering interventions in busy settings [36] while supporting home monitoring by closing an incomplete loop of data collection, feedback to the user and assessment to the clinician.
XIV. Conclusion
In this work, we present an application for capturing the relative force, repetitions and duration of using a Bluetooth-enabled resistance exercise band. This is, to our knowledge, the first open-source application available for such use. After applying a systems-engineering approach and by including end-users in the application design, our results suggest that there is promise in the formative design, storyboarding and utility of this application for future use and testing. The application contains the necessary core information that is acceptable to patients for the conducting of future planning and enhancements, with a goal of improving physical activity of older adults.
Fig. 4 (b).

Snapshot of states of TheraBand application: a) specific exercise type; b) choosing an exercise; c) connected; and d) specific exercise type
Acknowledgment
We thank the members of the Amulet team for their assistance, including Jacob Sorber, Joseph Skinner, Josiah Hester, Taylor Hardin, Travis Peters, and Varun Mishra.
This research is supported in part by the National Science Foundation (CNS-1314281 and CNS-1619970, by the National Institute on Aging under NIH (K23-AG051681), The content is solely responsibility of the authors and does not necessarily represent the official views of the NSF or the NIH.
Contributor Information
J. A. Batsis, Dartmouth-Hitchcock, Geisel School of Medicine at Dartmouth College, and The Dartmouth Institute for Health Policy & Clinical Practice, Lebanon, NH, 03756 USA
G. G. Boateng, Dartmouth College, Hanover, NH, 03755, USA. He is now with the Eidgenössische Technische Hochschule Zürich ETH, Zurich, Switzerland
L. M. Seo, Geisel School of Medicine at Dartmouth College, Hanover, NH, 03755, USA
C. L. Petersen, Dartmouth Institute for Health Policy & Clinical Practice, Lebanon, NH, 03756 USA
K. L. Fortuna, Dartmouth-Hitchcock and the Geisel School of Medicine, Lebanon, NH, 03756 USA
E. V. Wechsler, Thayer School of Engineering at Dartmouth College, Hanover, NH, 03755, USA
R. J. Peterson, Dartmouth College, Hanover, NH, 03755, USA
S. B. Cook, University of New Hampshire, Durham, NH 03824, USA
D. Pidgeon, Dartmouth-Hitchcock, Lebanon, NH, 03756 USA
R. S. Dokko, Dartmouth College, Hanover, NH, 03755, USA
R. J. Halter, Thayer School of Engineering at Dartmouth College, Hanover, NH, 03755, USA
D. F. Kotz, Dartmouth College, Hanover, NH, 03755, USA
References
- [1].Studenski SA, Peters KW, Alley DE, Cawthon PM, McLean RR, Harris TB, et al. The FNIH sarcopenia project: rationale, study description, conference recommendations, and final estimates. J Gerontol A Biol Sci Med Sci 2014;69:547–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Batsis JA, Mackenzie TA, Emeny RT, Lopez-Jimenez F, Bartels SJ. Low Lean Mass With and Without Obesity, and Mortality. J Gerontol A Biol Sci Med Sci 2017. [DOI] [PMC free article] [PubMed]
- [3].Batsis JA, Mackenzie TA, Lopez-Jimenez F, Bartels SJ. Sarcopenia, sarcopenic obesity, and functional impairments in older adults: National Health and Nutrition Examination Surveys 1999–2004. Nutr Res 2015;35:1031–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Peterson MD, Rhea MR, Sen A, Gordon PM. Resistance exercise for muscular strength in older adults. Ageing Res Rev 2010;9:226–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Villareal DT, Aguirre L, Gurney AB, Waters DL, Sinacore DR, Colombo E, et al. Aerobic or Resistance Exercise, or Both in Dieting Obese Older Adults. N Engl J Med 2017;376:1943–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Rejeski WJ, Ambrosius WT, Burdette JH, Walkup MP, Marsh AP. Community Weight Loss to Combat Obesity and Disability in At-Risk Older Adults. J Gerontol A Biol Sci Med Sci 2017. [DOI] [PMC free article] [PubMed]
- [7].Mohr DC, Cuijpers P, Lehman K. Supportive accountability: a model for providing human support to enhance adherence to eHealth interventions. J Med Internet Res 2011;13:e30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Noah B, Keller MS, Mosadeghi S, Stein L, Johl S, Delshad S, et al. Impact of remote patient monitoring on clinical outcomes: an updated meta-analysis of randomized controlled trials. npj Digital Medicine 2018;1:20172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Anderson-Lewis C, Darville G, Mercado RE, Howell S, Di Maggio S. mHealth Technology Use and Implications in Historically Underserved and Minority Populations in the United States: Systematic Literature Review. JMIR Mhealth Uhealth 2018;6:e128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Hester J, Lord S, Halter R, Kotz D, Sorber J, Peters T, et al. Amulet: An Energy-Efficient, Multi-Application Wearable Platform. Proceedings of the 14th ACM Conference on Embedded Network Sensor Systems CD-ROM - SenSys ‘162016. p. 216–29. [Google Scholar]
- [11].Wechsler EV, Batsis JA, Kotz DF, Skinner J, Zagaria AB, Peterson RA, et al. Development of a ‘Smart’ TheraBand to Assess Strength. J Am Geriatr Soc 2017;65:S218–S. [Google Scholar]
- [12].Wechsler EV. Development of a Smart Resistance Exercise Band to Assess Strength Hanover, NH: Dartmouth College; 2018. [Google Scholar]
- [13].Samaras GM, Horst RL. A systems engineering perspective on the human-centered design of health information systems. J Biomed Inform 2005;38:61–74. [DOI] [PubMed] [Google Scholar]
- [14].Creswell JW, Fetters MD, Ivankova NV. Designing a mixed methods study in primary care. Ann Fam Med 2004;2:7–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Shenhar AJ, Bonen Z. The new taxonomy of systems: toward an adaptive systems engineering framework. IEEE Transactions on Systems, Man, and Cybernetics - Part A: Systems and Humans 1997;27:137–45. [Google Scholar]
- [16].Uchida MC, Nishida MM, Sampaio RAC, Moritani T, Arai H. Thera-band® elastic band tension: reference values for physical activity. J Phys Therapy Science 2016;28:1266–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Guex K, Daucourt C, Borloz S. Validity and reliability of maximal-strength assessment of knee flexors and extensors using elastic bands. J Sport Rehabil 2015;24:151–5. [DOI] [PubMed] [Google Scholar]
- [18].Andersen LL, Vinstrup J, Jakobsen MD, Sundstrup E. Validity and reliability of elastic resistance bands for measuring shoulder muscle strength. Scand J Med Sci Sports 2016. [DOI] [PubMed]
- [19].Ao Aging. Internet Usage and Online Activities of Older Adults. Administration on Aging; 2013.
- [20].Batsis JA, Naslund JA, Gill LE, Masutani RK, Agarwal N, Bartels SJ. Use of a Wearable Activity Device in Rural Older Obese Adults: A Pilot Study. Gerontol Geriatr Med 2016;2:2333721416678076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Larizza MF, Zukerman I, Bohnert F, Busija L, Bentley SA, Russell RA, et al. In-home monitoring of older adults with vision impairment: exploring patients’, caregivers’ and professionals’ views. J Am Med Inform Assoc 2014;21:56–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Ball C, Franco A, Tyrrell J, Couturie P. Videoconferencing and the hard of hearing. J Telemed Telecare 1998;4:57–9. [DOI] [PubMed] [Google Scholar]
- [23].Mitzner TL, Boron JB, Fausset CB, Adams AE, Charness N, Czaja SJ, et al. Older Adults Talk Technology: Technology Usage and Attitudes. Comput Human Behav 2010;26:1710–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].LiftUp. LiftUp: Strength training reimagined In: Kickstarter, editor.2018.
- [25].John J XIaomi Launches the Move It Smart Exercise Resistance Band Priced at 549 Yuan (~$83) In: gizmochina, editor.2017.
- [26].Rolyan Smart Handle. Performance Health2018 p. Rolyan Smart Handle. [Google Scholar]
- [27].Petersen C, Weschler EV, Halter RJ, Boateng G, Proctor P, Kotz D, et al. Detection and Monitoring of Repetitions Using an mHealth Enabled Resistance Band. CHASE 2018: Third IEEE/ACM Conference on Connected Health: Applications, Systems and Engineering Technologies. Washington, DC2018. [PMC free article] [PubMed] [Google Scholar]
- [28].Batsis JA, Zagaria A, Kotz DF, Bartels SJ, Boateng GG, Proctor PO, et al. Usability evaluation for the Amulet Wearable Device in rural older adults with obesity. Gerontechnology 2018;17:151–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Samaras GM, Horst RL. A systems engineering perspective on the human-centered design of health information systems. Journal of Biomedical Informatics 2005;38:61–74. [DOI] [PubMed] [Google Scholar]
- [30].Macefield R How to Specify the Participant Group Size for Usability Studies: A Practitioner’s Guide. Journal of Usability Studies 2009;5:2009. [Google Scholar]
- [31].Black AC, Serowik KL, Schensul JJ, Bowen AM, Rosen MI. Build a better mouse: directly-observed issues in computer use for adults with SMI. Psychiatr Q 2013;84:81–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Prochnow JA, Meiers SJ, Scheckel MM. Improving Patient and Caregiver New Medication Education Using an Innovative Teach-back Toolkit. J Nurs Care Qual 2018. [DOI] [PubMed]
- [33].Brooke J System Usability Scale: A Retrospective. Journal of Usability Studies 2013;8:29–40. [Google Scholar]
- [34].F JR Psychometric Evaluation of the Post-Study System Usability Questionnaire: The PSSUQ. Proceedings of the Human Factors and Ergonomics Society Annual Meeting 1992;36:1259–60. [Google Scholar]
- [35].Batsis JA, Barre LK, Mackenzie TA, Pratt SI, Lopez-Jimenez F, Bartels SJ. Variation in the prevalence of sarcopenia and sarcopenic obesity in older adults associated with different research definitions: dual-energy X-ray absorptiometry data from the National Health and Nutrition Examination Survey 1999–2004. J Am Geriatr Soc 2013;61:974–80. [DOI] [PubMed] [Google Scholar]
- [36].Gamm LD, Hutchison LL, Dabney BJ, Dorsey AM. Rural Health People 2010: A Companion Document to Health People 2010 College Station, Texas: The Texas A&M University System Health Science Center, School of Rural Public Health, Southwest Rural Health Research Center; 2003. [Google Scholar]