Abstract
Prior to the 2014–2016 Ebola epidemic, Sierra Leone’s Ministry of Health and Sanitation had no infection prevention and control programme. High rates of Ebola virus disease transmission in healthcare facilities underscored the need for infection prevention and control in the healthcare system. The Ministry of Health and Sanitation led an effort among international partners to rapidly stand up a national infection prevention and control programme to decrease Ebola transmission in healthcare facilities and strengthen healthcare safety and quality. Leadership and ownership by the Ministry of Health and Sanitation was the catalyst for development of the programme, including the presence of an infection prevention and control champion within the ministry. A national policy and guidelines were drafted and approved to outline organisation and standards for the programme. Infection prevention and control focal persons were identified and embedded at public hospitals to manage implementation. The Ministry of Health and Sanitation and international partners initiated training for new infection prevention and control focal persons and committees. Monitoring systems to track infection prevention and control implementation were also established. This is a novel example of rapid development of a national infection prevention and control programme under challenging conditions. The approach to rapidly develop a national infection prevention and control programme in Sierra Leone may provide useful lessons for other programmes in countries or contexts starting from a low baseline for infection prevention and control.
Keywords: health systems, viral haemorrhagic fevers, infection prevention and control, public health
Summary box.
Inadequate infection prevention and control in Sierra Leone contributed to high rates of Ebola virus disease transmission in healthcare settings during the 2014–2016 West Africa epidemic.
The Sierra Leone Ministry of Health and Sanitation rapidly stood up a permanent national infection prevention and control programme for healthcare personnel and patient safety.
Ownership, financial commitment and leadership from the Ministry of Health and Sanitation were critical and should be promoted in other settings.
This process was a novel example of establishing a national infection prevention and control programme in a resource-limited setting during a public health crisis.
Introduction
Sierra Leone experienced an unprecedented epidemic of Ebola virus disease (EVD) from 2014 to 2016. The first case in country was reported on 24 May 2014. By the end of October 2014, 3854 laboratory-confirmed cases were reported, including 199 cases (5.2%) among healthcare personnel.1 Healthcare personnel had one of the highest rates of EVD in the epidemic, with infection 21–32 times more likely than the general adult population.2 General wards, not EVD isolation wards,3 4 were higher risk since unrecognised patients with EVD admitted to general wards exposed other patients, healthcare personnel and caregivers.5
The high frequency of EVD transmission in general healthcare facilities was primarily a consequence of absent infection prevention and control (IPC) infrastructure and systems compounded by gaps in knowledge and practices among healthcare personnel and unavailable supplies and personal protective equipment.6 The high EVD transmission in general healthcare facilities led to a major impact in the national healthcare system. Healthcare facilities were perceived by the community as high-risk settings for EVD.3 As a result, healthcare utilisation dropped dramatically during the epidemic,7 8 and a general perception of healthcare system collapse was widely reported.9 10
Prior to the 2014–2016 Ebola epidemic, Sierra Leone had no IPC programme, as was the case in many countries across Africa. IPC programmes at the national, district and facility level did not exist, nor were there dedicated IPC staff at government healthcare facilities. Since IPC was not subsumed within any other programme, policies, human resources and training programmes in IPC were also absent. A rapid assessment of IPC in six districts in October 2014 identified multiple IPC gaps in facilities.6
Recognising the critical need for establishing IPC capacity, the Sierra Leone Ministry of Health and Sanitation (MoHS) rapidly created a national programme to provide leadership and coordination for IPC activities throughout the healthcare system. Here we describe the first year of implementation and lessons learnt from a national IPC programme in Sierra Leone centred on the development of a national policy, human resources, technical guidelines, training and education, and monitoring during the Ebola epidemic.
Sierra Leone healthcare system
Sierra Leone had an estimated population of 7.1 million in 2015, with over 40% residing in urban areas.11 There are 14 administrative districts across four regions of the country. The health system is composed of public services, private services and traditional healthcare practices. Primary care is provided at peripheral health units (PHUs), which also includes a community health worker extension. Secondary and tertiary care is provided at district and referral hospitals (table 1).
Table 1.
Sierra Leone government healthcare facilities
| Level of care | Type of facility | Catchment area | Number* |
| Primary | Maternal and child health posts | <5000 persons Village level |
559 |
| Community health posts | 5000–10 000 persons Small town level |
386 | |
| Community health centres | 10 000–20 000 persons Chiefdom level |
229 | |
| Secondary | District and regional referral hospitals | 21 | |
| Tertiary | Referral hospitals | 3 |
*2016 Ministry of Health and Sanitation data.13
As of 2015, there were 1264 public and private health facilities serving the country, including 40 hospitals.12 The Government of Sierra Leone owned 24 of these hospitals, with the rest owned by a mix of private companies, non-governmental organisations and faith-based organisations. Hospitals owned by the Government of Sierra Leone will be referred to as government hospitals. The national healthcare workforce was estimated at 9900 healthcare personnel as of 2016.13 Given the estimated population, this translates to three physicians per 100 000 population and 50 nurses and midwives per 100 000 population.13
Ministry ownership
Leadership and ownership by the MoHS were identified as essential to the short-term success of IPC promotion during the Ebola epidemic and the long-term success of IPC in routine healthcare delivery during the post-Ebola period. International partners, such as US Centers for Disease Control and Prevention (CDC), WHO and non-governmental organisations, such as Infection Control Africa Network (ICAN), provided technical and implementation support, but the MoHS was responsible for the creation, acceleration and long-term sustainability of the programme. A timeline of significant milestones and activities for the first year of the national IPC programme is presented in figure 1.
Figure 1.
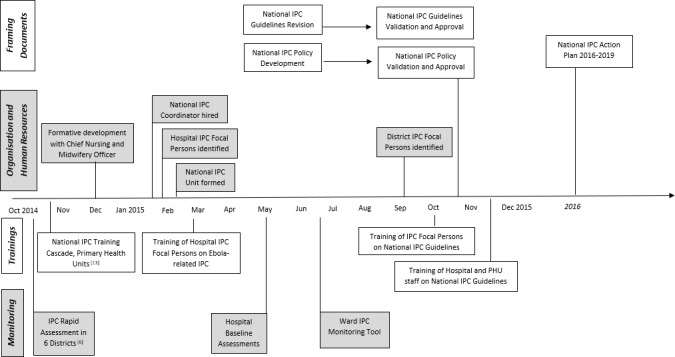
Milestones of the Sierra Leone national IPC programme, 2014–2015. The national IPC programme began with formative discussions in fall 2014. By February 2015, a national IPC coordinator was hired, the national IPC unit was established and hospital IPC focal persons were identified at government hospitals. Further milestones including development of framing documents, organisation and human resources, trainings and monitoring. IPC, infection prevention and control.
The MoHS chief nursing and midwifery officer, an IPC ‘champion’,14 aided the development of the IPC programme and provided the overall leadership and vision. This IPC champion provided recommendations for the programme’s organisational structure based on experience in the Sierra Leone government healthcare system, maintained communication with senior leaders at MoHS on decisions and progress and collaborated closely with humanitarian aid agencies and international partners. The IPC champion facilitated the creation of a new MoHS unit for IPC and collaborated with the chief nurse at each government hospital, also known as the hospital matron, to appoint IPC focal persons at government hospitals and district health offices.
MoHS also committed to salary support for IPC staff, both within the national IPC unit (NIPCU) and IPC focal persons at government hospitals and district health offices. Although humanitarian aid funding could have covered salaries given the influx of resources during the Ebola epidemic, MoHS considered it necessary for long-term ownership and financial sustainability that salary funding stay within MoHS.
National IPC policy
A new national IPC policy formalised the organisational structure and requirements of the programme. This policy defined roles, responsibilities, reporting and accountability processes at each level of the healthcare system. International partners assisted MoHS in drafting the national IPC policy. MoHS directorates and other stakeholders reviewed the draft policy document at a 2-day validation workshop, followed by approval from the chief medical officer and Minister of Health and Sanitation.
The national IPC policy outlined the creation of IPC positions at national, district and facility levels. At the national level, the policy designated a national IPC coordinator to oversee the development, implementation and evaluation of the programme. These activities included developing strategic documents, creating technical and training materials, liaising with MoHS directorates, generating national IPC progress reports and evaluating the implementation of IPC activities. Leadership was central to all improvement efforts, and the national IPC coordinator was appointed to lead the NIPCU, which became the primary coordinating body for MoHS IPC activities during the latter half of the Ebola epidemic. The NIPCU is now the lead unit for all IPC activities across the healthcare sector. The formation of the NIPCU was an essential step in institutionalising a national IPC programme, creating a central hub for IPC leadership, coordination and advocacy.
In each of the 14 Sierra Leone districts, the policy mandated IPC focal person positions to coordinate and implement IPC activities. The policy also specified a district IPC supervisor to provide mentorship and support for facility IPC focal persons. The district IPC personnel were also assigned to oversee IPC at all PHUs15 across 14 districts in Sierra Leone. PHU IPC focal persons were appointed to work under the authority of the district IPC supervisor with responsibility for a geographic cluster of PHUs.
The policy created an IPC focal person position with responsibility for overseeing IPC at each government hospital. The MoHS chief nursing and midwifery officer (ie, the IPC champion) communicated directly with each hospital matron to identify an experienced, respected clinician, most often a nurse, to transition full-time duties to the management of IPC at the hospital. Each of the Sierra Leone government hospitals appointed an IPC focal person in February 2015. Their responsibilities were built around a multimodal improvement approach and included training all facility staff on infection control practices, monitoring IPC practices across the hospital, generating reports for hospital leadership, leading quality improvement initiatives for IPC and liaising with pharmacy, environmental services and other departments. Hospital IPC focal persons reported on action plans, assessments, training and implementation to district-level IPC personnel. As outlined in the national policy, district IPC personnel then reported information to the NIPCU.
National IPC guidelines
Development of the Sierra Leone national IPC guidelines began in May 2015. The guidelines set standards for safe, high-quality patient care and healthcare personnel safety during routine healthcare delivery. The CDC and WHO collaborated on the initial drafting and technical review of the document through the establishment of a guideline finalisation group. The CDC and WHO working group reviewed each draft guideline chapter for technical consistency. A team of two reviewers revised each chapter, which was then reviewed by the NIPCU for context and quality control. The MoHS organised a 2-day validation workshop in August 2015 that provided an opportunity for comment and feedback from MoHS directorates and other stakeholders and was an important step to secure buy-in. The chief medical officer and Minister of Health and Sanitation formally approved the document following revisions from the workshop. As a first step for guideline implementation, the NIPCU developed a standard IPC training package for healthcare personnel. Facilities rolled out the IPC guideline training via international partner support throughout late 2015.
Training and education
Healthcare personnel in Sierra Leone did not receive formal in-service IPC training before the Ebola epidemic. In late 2014, MoHS led a partnership among multiple organisations to cascade national IPC training to over 4200 PHU staff within the context of the ongoing epidemic of EVD.16 PHUs were a first stop for community members presenting with symptoms of Ebola. This standardised training focused on IPC practices to keep healthcare personnel safe and emphasised messaging to screen, isolate and refer suspect cases. International partners conducted supervision visits every 2 weeks, using a structured assessment, to check on IPC practices and supply availability.
After creation of hospital IPC Focal person positions in the national IPC policy and selection at each facility by the chief nursing and midwifery officer and hospital matrons, MoHS organised orientation training. Hospital IPC focal persons were responsible for improving IPC practices to limit Ebola transmission in their assigned hospital and beginning to integrate IPC into routine patient care. Newly appointed hospital IPC focal persons attended an initial 10-day training in March 2015. MoHS held this training with support from the ICAN and CDC. The training oriented hospital IPC focal persons to their roles and responsibilities and taught IPC practices. The focus of the training was preventing Ebola transmission in hospitals during the Ebola epidemic.
Ebola-related IPC training for government hospital staff was cascaded nationally after the IPC focal person training in March 2015. By November 2015, 6448 clinical and support staff at hospitals had received IPC training. Each training roll-out was paired with mentorship or supervision activities. Following the initial IPC focal person training, a mentorship programme was set up through a partner consortium, which is the Ebola Response Consortium. The mentorship programme matched a hospital IPC focal person with a full-time mentor (a clinician from outside Sierra Leone) to guide the transition to full-time duties in IPC.
Formation of IPC committees
The national IPC policy also called for the formation of IPC committees at national, district and facility (ie, hospital) levels (table 2) and provided each committee with terms of reference. The national IPC advisory committee provided input on IPC policy, strategic plans, guidelines, procedures and management issues and reviewed progress towards national goals. This committee was also necessary to advocate for financial and human resources for IPC.
Table 2.
Sierra Leone IPC committees structure as outlined in the national IPC policy
| Committee | Committee chair | Attending stakeholders | Meeting frequency |
| National IPC advisory committee | Chief medical officer |
|
Quarterly |
| District IPC committee | District IPC focal person |
|
Monthly |
| Hospital IPC committee | Hospital IPC focal person |
|
Monthly |
The district IPC committee reviewed progress at PHUs and government hospitals, worked to resolve challenges with facility-level implementation of national standards and provided budget input to support the district medical officer. The district IPC committee also supported district logistic officers to strengthen supply procurement and distribution.
At government hospitals, the IPC committee reviewed hospital assessments and other data provided by the IPC focal person and addressed facility IPC issues that required coordination across wards. The hospital committee also provided input to support the hospital medical superintendent in formulating the IPC component of the hospital budget. International partners supported the development of fit for purpose, effective and action-focused hospital IPC committees, including training on functions of an IPC committee and involvement in initial meetings to provide mentorship. Stakeholder involvement was crucial to getting the committees established and functioning.
Monitoring of IPC implementation
Various methods and tools were used to track IPC implementation at the facility level. A quality assurance checklist was deployed for routine supervision visits in conjunction with the national Ebola IPC training at PHUs.16 This standards-based checklist for screening, isolation and referral identified areas for immediate action during supervision visits. As the national IPC programme was scaling up, 24 government hospitals performed an assessment of IPC infrastructure, systems and practices in early-to-middle 2015. The assessment highlighted that while many IPC activities were implemented, there was still much to be done (table 3). The MoHS and partners also developed a ward monitoring tool for IPC focal persons to use as a ‘quick check’ on wards. This scored tool collected data on IPC supplies, waste management and environmental cleanliness, hand hygiene, personal protective equipment use, sharps management, screening and monitoring for Ebola. The tool provided opportunities for direct coaching from the IPC focal person. Some IPC focal persons also used the ward monitoring tool to promote competitive improvement among wards, with the ward scoring the highest monthly total receiving a certificate from the IPC focal person.
Table 3.
Selected IPC indicators of government hospitals (n=24)
| Domain | Total (%)* |
| Designated IPC focal person with formal IPC training | 23/24 (95.8) |
| IPC committee formed | 13/20 (65.0) |
| All persons screened for Ebola on arrival to facility | 10/24 (41.7) |
| Functional hand hygiene stations for screening | 18/24 (75.0) |
| Designated screener present | 21/24 (87.5) |
| Dedicated isolation area | 21/24 (87.5) |
| Medical waste segregated | 6/24 (25.0) |
| Incinerator present | 17/23 (73.9) |
| Incinerator functioning | 11/17 (64.7) |
| Water available 24 hours a day | 10/24 (41.7) |
*Not all facilities completed every question; denominator listed for each domain.
IPC, infection prevention and control.
Lessons learnt
Establishing a national IPC programme during a public health crisis was not without its challenges. Without MoHS ownership, including an IPC champion, the IPC programme might not have been sustained beyond the end of the Ebola epidemic. Appointing NIPCU as the central coordinating body led to improved communication and harmonisation of IPC resources across partners. Before the development of the national IPC programme, coordination, including duplication of activities, was a challenge. To this day, the NIPCU is lead for integration of IPC into the health system and can act as a model for countries looking to establish national IPC programmes.
Many human resources were available from partners to rapidly collaborate on the national IPC policy, national technical guidelines and training materials. Although the expedited timeline for developing these technical materials is not feasible for many countries, the collaboration and working group approach should be considered in other settings. A key challenge was implementing a monitoring and evaluation plan given the many parallel reporting structures in place during the Ebola epidemic. A monitoring and evaluation framework should be developed, approved and operationalised from the beginning when creating a national IPC programme.
Implementation at the district level presented challenges unique to overseeing IPC across many facilities. Access to transportation for district IPC staff was difficult, particularly for PHUs located a considerable distance from the district centre. Though all districts and facilities initially staffed IPC positions, personnel turnover has since occurred for district and facility IPC posts. Implementation at the district level was incremental compared with the hospital level. Planning for district IPC programmes should carefully consider resources needed for day-to-day support activities not specific to healthcare, such as transportation, fuel and cellular airtime expenses.
IPC was one of the key strategies during the response to prevent healthcare-related EVD infections. As stated earlier, healthcare personnel had one of the highest risks of EVD infection during the outbreak.2 From July 2014 to February 2015, healthcare personnel as a proportion of all cases decreased from 12% to 1%.2 While this decrease occurred during the scale up of the IPC programme, it cannot be directly attributed to IPC. The combination of many interventions likely contributed to the reduction in healthcare personnel infections. IPC should be scaled in other outbreak settings to protect healthcare personnel from infection.
Due to MoHS leadership and commitment to continue IPC beyond the Ebola epidemic, IPC has continued to be prioritised in Sierra Leone. To this day, there is still a national IPC coordinator in NIPCU and staffing of IPC focal persons in government hospitals. The longevity of the national IPC programme in Sierra Leone is evidence that investing in health systems strengthening in parallel to emergency response can lead to a sustainable programme. IPC was a critical element of the post-Ebola Presidential Recovery Plan (2016), and a National IPC Action Plan (2016–2019) was drafted to strategically direct investments in IPC across Sierra Leone. The MoHS has continued to strengthen capacity for IPC through multifacility quality improvement projects, development of an IPC certification course and surveillance of surgical site infections.
Conclusion
Sierra Leone rapidly established a government-led IPC programme during the Ebola epidemic. The programme included a national IPC policy, human resources, national technical guidelines, training initiatives and monitoring and evaluation within the context of strengthened leadership and the development of a culture of safety and improvement across the health system. This process was a novel example of the establishment of a national IPC programme in a resource-limited setting during a public health crisis. The approach in the first year of Sierra Leone’s national IPC programme laid the foundation for continual improvement in healthcare personnel and patient safety and provides useful lessons for other programmes in countries or contexts where an IPC programme is absent.
Acknowledgments
The work presented here is the combined effort of many individuals and organisations. The authors would like to acknowledge the dedication of healthcare personnel in Sierra Leone during the Ebola epidemic, with a special dedication to those who lost their lives to Ebola. Organisations within the Ebola Response Consortium facilitated implementation, namely, Action Contre la Faim, Concern Worldwide, GOAL, the International Rescue Committee, Marie Stopes Sierra Leone, Medicos del Mundo and Save the Children. The authors also acknowledge the WHO Country Office, the CDC Country Office and many staff from both organisations that assisted with this work while deployed for Ebola response and recovery activities during 2014–2016.
Footnotes
Handling editor: Alberto L Garcia-Basteiro
Contributors: All listed authors contributed substantially to the planning and implementation of work described in this practice report. KW drafted the initial manuscript, and all authors revised it critically for important intellectual content. All authors listed approved final version of the manuscript. All authors agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately answered and resolved.
Funding: The work described here was supported in part by emergency funding from the US government and WHO.
Disclaimer: The findings and conclusions in this report are those of the author(s) and do not necessarily represent the official position of the Centers for Disease Control and Prevention or the WHO.
Competing interests: None declared.
Patient consent for publication: Not required.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: No additional data are available.
References
- 1. Kilmarx PH, Clarke KR, Dietz PM, et al. Ebola virus disease in health care workers--Sierra Leone, 2014. MMWR Morb Mortal Wkly Rep 2014;63:1168–71. [PMC free article] [PubMed] [Google Scholar]
- 2. Organization WH Health worker Ebola infections in Guinea, Liberia and Sierra Leone: a preliminary report, 2015. [Google Scholar]
- 3. Olu O, Kargbo B, Kamara S, et al. Epidemiology of Ebola virus disease transmission among health care workers in Sierra Leone, may to December 2014: a retrospective descriptive study. BMC Infect Dis 2015;15 10.1186/s12879-015-1166-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Senga M, Pringle K, Ramsay A, et al. Factors underlying Ebola virus infection among health workers, Kenema, Sierra Leone, 2014-2015. Clin Infect Dis 2016;63:454–9. 10.1093/cid/ciw327 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Dunn AC, Walker TA, Redd J, et al. Nosocomial transmission of Ebola virus disease on pediatric and maternity wards: Bombali and Tonkolili, Sierra Leone, 2014. Am J Infect Control 2016;44:269–72. 10.1016/j.ajic.2015.09.016 [DOI] [PubMed] [Google Scholar]
- 6. Pathmanathan I, O'Connor KA, Adams ML, et al. Rapid assessment of Ebola infection prevention and control needs--six districts, Sierra Leone, October 2014. MMWR Morb Mortal Wkly Rep 2014;63:1172–4. [PMC free article] [PubMed] [Google Scholar]
- 7. Elston JWT, Moosa AJ, Moses F, et al. Impact of the Ebola outbreak on health systems and population health in Sierra Leone. J Public Health 2016;38:673–8. 10.1093/pubmed/fdv158 [DOI] [PubMed] [Google Scholar]
- 8. Brolin Ribacke KJ, Saulnier DD, Eriksson A, et al. Effects of the West Africa Ebola Virus Disease on Health-Care Utilization - A Systematic Review. Front Public Health 2016;4 10.3389/fpubh.2016.00222 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Dynes MM, Miller L, Sam T, et al. Perceptions of the risk for Ebola and health facility use among health workers and pregnant and lactating women--Kenema District, Sierra Leone, September 2014. MMWR Morb Mortal Wkly Rep 2015;63:1226–7. [PubMed] [Google Scholar]
- 10. O'Hare B. Weak health systems and Ebola. Lancet Glob Health 2015;3:e71–2. 10.1016/S2214-109X(14)70369-9 [DOI] [PubMed] [Google Scholar]
- 11. Leone SS, GoS L. Population and housing census. Freetown, Sierra Leone, 2015. [Google Scholar]
- 12. Ministry of Health and Sanitation SL Health sector recovery plan (2015-2020); 2015.
- 13. Ministry of Health and Sanitation SL Human resources for health strategy, 2017-2021; 2017.
- 14. Damschroder LJ, Banaszak-Holl J, Kowalski CP, et al. The role of the champion in infection prevention: results from a multisite qualitative study. Qual Saf Health Care 2009;18:434–40. 10.1136/qshc.2009.034199 [DOI] [PubMed] [Google Scholar]
- 15. UNICEF Sierra Leone health facility Survey 2014: assessing the impact of the EVD outbreak on health systems in Sierra Leone, 2014. [Google Scholar]
- 16. Levy B, Rao CY, Miller L, et al. Ebola infection control in Sierra Leonean health clinics: a large cross-agency cooperative project. Am J Infect Control 2015;43:752–5. 10.1016/j.ajic.2015.03.011 [DOI] [PubMed] [Google Scholar]


