Supplemental Digital Content is available in the text
Keywords: Glasgow-Blatchford score, prognosis, Rockall score, upper gastrointestinal hemorrhage
Abstract
The Glasgow-Blatchford scores (GBS) and Rockall scores (RS) are commonly used for stratifying patients with nonvariceal upper gastrointestinal hemorrhage (NVUGIH). Although predictive value of these scoring methods has been extensively validated, their clinical effectiveness remains unclear. The following study evaluated the GBS and RS scoring system with reference to bleeding, needs for further surgery, endoscopic intervention and death, in order to verify their effectiveness and accuracy in clinical application.
Patients who presented with NVUGIH, or who were consequently diagnosed with the disease (by endoscopy examination) between January 1, 2008, and December 31, 2012 were enrolled in the study. GBS and RS scores were compared to predict bleeding, the needs for further surgery, endoscopic intervention, death by ROC curves and AUC value.
Among 2977 patients, the pre-endoscopic RS and complete RS score (CRS) were superior to the GBS score (AUC: 0.842 vs 0.804 vs 0.622, respectively) for predicting the mortality risk in patients. The pre-endoscopic RS score predicting re-bleeding was significantly higher than the CRS and the GBS score (AUC: 0.658 vs 0.548 vs 0.528, respectively). In addition, the 3 scoring systems revealed to be poor predictors of surgical operation effectiveness (AUC: 0.589 vs 0.547 vs 0.504, respectively).
Our data demonstrated that the GBS and RS scoring systems could be used to predict outcomes in patients with nonvariceal upper gastrointestinal bleeding.
1. Introduction
Non-variceal upper gastrointestinal hemorrhage (NVUGIH) is bleeding of the digestive tract proximal to the ligament of Treitz, that is, bleeding of the pancreatic or bile ducts, and bleeding from the proximal anastomosis after gastrojejunostomy.[1] The incidence of NVUGIH is 20-60/100,000 people,[2–4] and is particularly high among elderly patients who carry other types of systemic diseases; the mortality rate in these patients is about 7% to 14%.[5] The prognosis of upper gastrointestinal bleeding may vary from mild to life- threatening.[4] Patients with mild bleeding might fully recover without specific clinical treatment, while those with severe bleeding may experience severe complication and even death if they do not receive the treatment for the condition. Thus, it is extremely important to classify NVUGIH severity based on patients’ clinical profiles.
Over the last decade, the management of upper gastrointestinal hemorrhage and understanding of its stratification risk have become a hot topic among researches.[6] Besides, early diagnosis, as well as accurate stratification of patients with higher mortality risk and risk of re-bleeding, may significantly increase the efficiency of medical treatment since these data can be used by emergency physicians when making final decisions.[7,8] So far, multiple scoring systems that stratify patients into those with high and low risk have been developed.[9,10] Nevertheless, the controversies related to risk stratification, role of endoscopic therapy, the needs for further surgery, endoscopic intervention and death still remain. Accordingly, there is no consensus on how to approach such patients.[11] To date, all the existing studies have focused on in-hospital or 30 days mortality.
Glasgow-Blatchford scores (GBS) and complete Rockall scores (CRS) are commonly used for stratifying NVUGIH cases in terms of risk. Thus far, numerous clinical studies have validated their predictive value; yet, their clinical effectiveness remains unclear. In addition, little data are available concerning this critical condition in China. The following study examined the effectiveness and accuracy of GBS and CRS scoring systems in clinical application in Chinese patients.
2. Methods
2.1. Patients
This study was retrospectively conducted at Kunming Medical University and other seven medical centers (Chinese PLA General Hospital, Beijing Tian Tan Hospital, Zhongshan Hospital, Fudan University, Xi’an Central Hospital, First Affiliated Hospital, Nanjing Medical University, First Affiliated Hospital, Zhejiang Chinese Medical University, Zhongshan Hospital, Xiamen University, First People's Hospital of Foshan). The ethics committee from Kunming Medical University approved the study. Patients who presented with NVUGIH, or who were diagnosed with the disease (by endoscopy examination) between January 1, 2008, and December 31, 2012 were included in this study. The inclusion criteria were the following:
-
1.
NVUGIH defined as hematemesis, melena, coffee grounds vomiting, fresh blood vomiting or positive fecal occult blood test;
-
2.
bleeding unrelated to varices as confirmed by endoscopy. Patients < 18 years old and those with primary diagnoses other than NVUGIH were excluded from the study.
The diagnosis of NVUGIH was based on International Classification of Diseases, Ninth Revision (ICD-9) diagnosis codes.
2.2. Treatment
All patients underwent a gastrointestinal endoscopy after hospital admission. During this study, all patients received a combination of proton pump inhibitors, and fluid resuscitation that secured airway and breathing. The updated British Society of Gastroenterology guidelines were followed for general management.[12]
2.3. Data collection
Data collection was performed at each medical center using a standard table with an electronic medical record system. For each participant, the following information were collected: gender, age, history of upper gastrointestinal bleeding, syncope, cardiac failure or liver disease, number of hospitalization days, hospitalization costs, clinical symptoms, blood pressure, heart rate, laboratory parameters, endoscopic diagnosis, Forrest classification, treatment and outcome data in the form of interventions (bleeding, the needs for further surgery, endoscopic intervention) or death, etc. The data entry was controlled by 2-pass verification of all collected data to ensure the quality of the data.
2.4. Analysis of GBS and pre-endoscopic RS
The pre-endoscopic RS, CRS[3] (Table 1) and GBS[4] (Table 2) were calculated based on patients pre-endoscopic and endoscopic variables.
Table 1.
Baseline characteristics of 2977 patients.
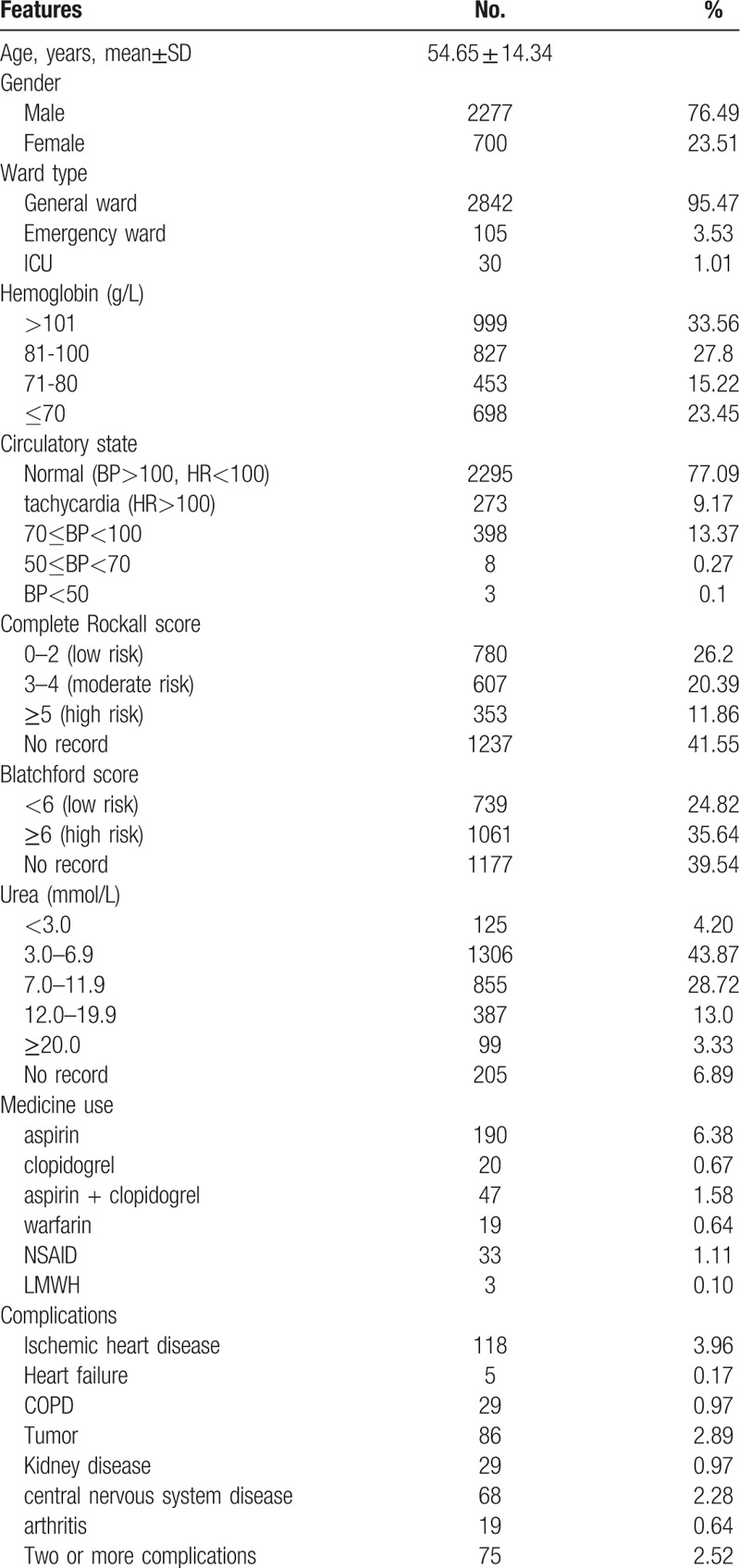
Table 2.
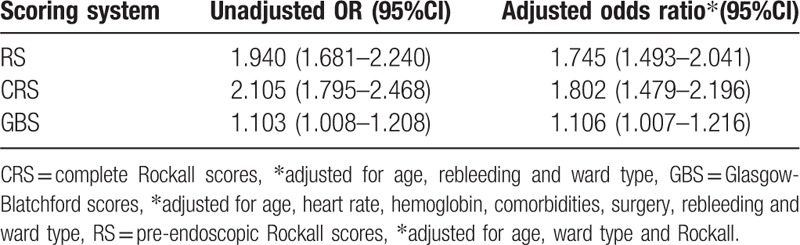
Relationship between different scoring system and separate outcome of death.
2.5. Statistical analysis
SPSS software (version 17.0, SPSS, Chicago, IL) was used for all statistical analyses in this study. The clinical demographic and epidemiologic features were analyzed using a descriptive statistical method (mean ± standard deviation, percentage, median, and interquartile range). Between-group comparisons of normally distributed data were performed using Student's t test. Data with non-normal distribution were compared using rank-sum tests. Count data were compared using chi-square tests. Comparisons between the scores for separate death outcomes, endoscopic or surgical therapy were made by calculating the areas under the receiver-operator characteristic (ROC) curves with 95% CI. Accuracy was tested by calculating the area under the curve (AUC) of the ROC curve, where AUC ≥ 0.70 indicated that the scoring system had good accuracy. The AUCs were compared using Z tests. A P value < 0.05 was considered statistically significant.
3. Results
A total of 2977 patients with NVUGIH were included in the study. The mean age of patients was 54.65 ± 14.34 years, the ratio of men to women was 3.25:1, and the mean hospitalization duration was 9.48 ± 8.4 days. Among all patients, 19.65% (585/2977) underwent emergency endoscopy and the median time from gastrointestinal bleeding to gastroscopy was 72 hours (36–120 hours), and 23.45% (698/2977) received a transfusion of red blood cell suspensions. A total of 19.08% (568/2977) of patients had high-risk peptic ulcer bleeding. A total of 5.34% (159/2977) underwent endoscopic therapy, with a treatment rate of 16.9% in high-risk peptic ulcer patients (96/568) (Table 1). Patients were scored using the CRS and GBS criteria, followed by risk stratification. Based on the Rockall score, 1780 patients were at low risk, 927 at moderate risk, and 270 at high risk (Table S1, Table S2), based on the Blatchford scores, 414 patients were at low-risk and 2123 at high-risk (Table S3, Table S4).
When adjusting for age, ward type and Rockall, the odds ratio of death for pre-endoscope RS was 1.745 (95%CI: 1.493–2.041). Moreover, when adjusting for age, re-bleeding and ward type, the odds ratio of death for CRS was 1.802 (95%CI: 1.479–2.196). Interestingly, when adjusting for age, heart rate, hemoglobin, comorbidities, surgery, re-bleeding and ward type, the death odds ratio for GBS was 1.106 (95%CI: 1.007–1.216) (Table 2).
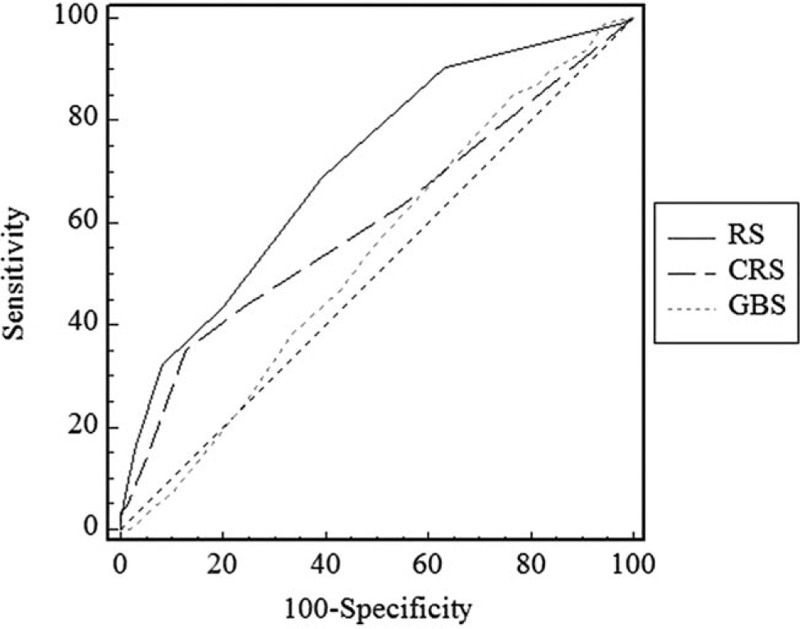
ROC curves were plotted for the 3 scoring systems with reference to their prediction of mortality, rebleeding, and need for surgery (Table 3). The AUCs for the pre-endoscopic RS, CRS, and GBS to predict mortality were 0.842 (95%CI: 0.827–0.855), 0.804 (95% CI: 0.788–0.818), and 0.622 (95% CI: 0.603–0.640), respectively (Fig. 1).
Table 3.
Diagnostic value of different scoring system for predicting mortality, surgical therapy or re-bleeding.
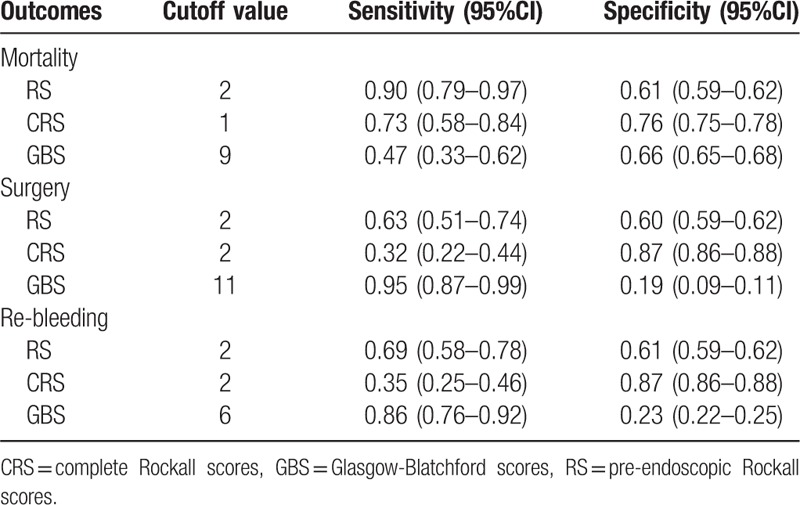
Figure 1.
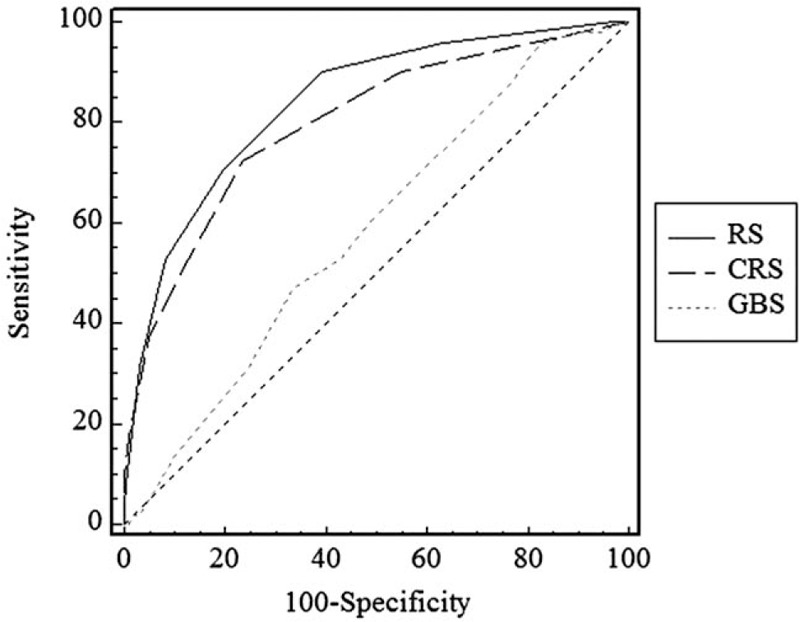
The accuracy of the pre-endoscopic Rockall score, complete Rockall score, and Blatchford score in predicting mortality (the area under the ROC curves: RS = 0.839, CRS = 0.798, GBS = 0.585).
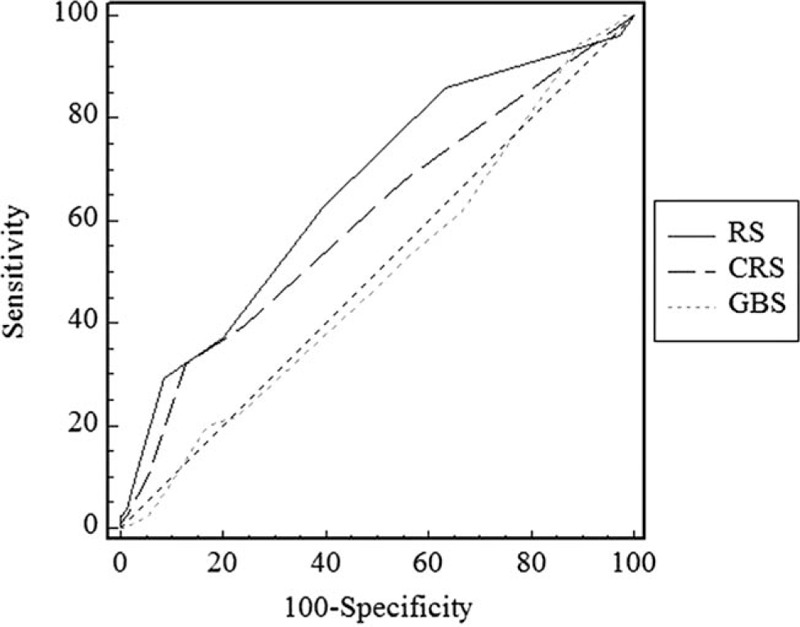
The AUCs for the pre-endoscopic RS, CRS, and GBS to predict rebleeding were 0.658 (95% CI: 0.640–0.676), 0.548 (95% CI: 0.529–0.566), and 0.528 (95% CI: 0.509–0.546), respectively (Fig. 2).
Figure 2.
The accuracy of the pre-endoscopic Rockall score, complete Rockall score, and Blatchford score in predicting rebleeding (the area under the ROC curves: RS = 0.707, CRS = 0.601, GBS = 0.536).
The AUCs for the pre-endoscopic RS, CRS, and GBS in predicting the need for surgery were 0.589 (95% CI: 0.571–0.608), 0.547 (95% CI: 0.528–0.565), and 0.504 (95% CI: 0.485–0.523), respectively (Fig. 3).
Figure 3.
The accuracy of the pre-endoscopic Rockall score, complete Rockall score, and Blatchford score in predicting surgery (the area under the ROC curves: RS = 0.660, CRS = 0.602, GBS = 0.491).
4. Discussion
The GBS and RS are widely used for stratifying NVUGIH cases in terms of risk. Nevertheless, their clinical effectiveness remains unclear, and there is little evidence available for Asian population. The aim of the present study was to verify the efficiency and accuracy of these 2 scoring systems in clinical application in Chinese patients. In this study, we collectively analyzed the clinical outcomes in 2977 individuals with NVUGIH according to GBS and RS scoring systems. Among the 2977 patients, the pre-endoscopic RS and CRS were superior to the GBS score (P < .01) in predicting mortality. The pre-endoscopic RS predicting re-bleeding was better than the CRS and the GBS score (P < .01). Nonetheless, these 3 scoring systems were poor predictors of surgical operation ability (AUC: 0.589 vs 0.547 vs 0.504, respectively). Our data collectively demonstrated that the GBS and RS systems could be used to predict clinical outcomes in nonvariceal upper gastrointestinal bleeding.
NVUGIH is an acute, severe condition that can lead to serious consequences. The RS and GBS scoring systems, are currently used in clinical settings for stratifying the risk of NVUGIH where RS is the more popular one.[13] In 2010, the International Consensus on NVUGIH clearly identified the risk assessment methods for such patients.[2] In 2011,[14] the Asia-Pacific Working Group consensus on NVUGIH formulated NVUGIH treatment guidelines that were adapted to Asian population based on the actual conditions of people in the Asia-Pacific region (e.g., economic level and drug metabolism), while also collating research related to NVUGIH risk assessment in the Asia-Pacific region.[15] Unfortunately, there is a lack of large-sample randomized controlled trials that would provide a higher level of evidence.
The pre-endoscopic RS and CRS revealed positive predictive value for mortality, which was consistent with the study results reported by Dicu et al[16] The prediction ability for re-bleeding was significantly higher in pre-endoscopic RS, compared with the CRS. Nevertheless, its predictive value for the need for surgery was poor. Lima and colleagues[17] have also shown that the RS could not predict surgery or endoscopic intervention and re-bleeding, while it could predict the value for mortality. A study conducted at Beijing Xuanwu Hospital in geriatric patients has indicated that the scoring system has good predictive value for mortality, re-bleeding, and surgery. Yet, Lima and his team[17] have shown that the pre-endoscopic RS unsatisfactorily predicts endoscopic intervention, re-bleeding, and death. It is important to note that, in our study, 1771 patients were <60 years old, 999 were 60 to 79 years old, and 207 were ≥80 years old, and patients ≥60 years accounted for 40.5% of the study population. In the study by Dicu et al, patients above 70 years accounted for 33% of the total population, and thus the observed differences might be related to the age of the research subjects.
The GBS scoring system,[4,18,19] is used during outpatient treatment or upon admission to the hospital to determine whether patients can receive outpatient treatment or treatment with early discharge within 24 hours. Its clinical advantage is that patients with Blatchford score of 0 points can be categorized as low risk, which results in saving medical resources.[20] In the present study, the predictive value of GBS scoring system for mortality, re-bleeding, and surgery was not satisfactory. Yet, Bryant et al[21] did not prove that the predictive value of the Blatchford score with reference to the need for inpatient transfusion and surgery is superior to the CRS. The predictive values for endoscopic intervention, re-bleeding, and mortality differed from our research results, which might be due to the inclusion of patients with variceal upper gastrointestinal bleeding. A recent study[22] has indicated that GBS performs has relatively good performance in prediction of the need for clinical interventions (endoscopic intervention, angiographic embolization, and surgery) in patients with cancer.
Our comparison of the 3 scoring systems revealed that the pre-endoscopic RS and CRS were both superior to the GBS in their prediction of mortality. The pre-endoscopic RS was better at predicting re-bleeding than the CRS and GBS. All 3 scoring systems had poor efficiency power in predicting the need for surgery. Nonetheless, in high-risk patients with peptic ulcer bleeding, the RS has better predictive power for 30-day mortality than the GBS.[23] In addition, the GBS does not have the predictive value for endoscopic intervention.[24] A retrospective study[25] has shown that the mortality rates of high-risk patients with GBS >12 points could be reduced if these patients underwent endoscopic examination within 13 hours. Therefore, endoscopic examination should be performed as soon as possible in patients with a GBS >12 points.[20]
This study has some limitations that have to be pointed out: first, this is a retrospective study, which means that compared to the randomized case control studies the evidence level is limited. Moreover, the record of clinical outcomes is limited to the events that happened during the stay at hospital, which could cause bias. However, all patients were followed up for relevant severe outcomes, which in our opinion should not devalue the main findings reported in this article.
Our results showed that the Blatchford and Rockall scoring systems can be used for prediction of clinical outcomes in nonvariceal upper gastrointestinal bleeding, which is consistent with previous reports. The application of the GBS scoring system in emergency and cancer patients has been constantly validated, and future studies should further refine the scope of the scoring system for clinical application. In addition, more high-quality clinical trials are required for further verification.
Author contributions
Conceptualization: Ming-Liang Lu, Yunsheng Yang.
Data curation: Ming-Liang Lu, Gang Sun, Hua Huang, Xiaomei Zhang, Youqing Xu, Shiyao Chen, Ying Song, Xueliang Li, Bin Lv, Jianlin Ren, Xueqing Chen, Hui Zhang, Chen Mo, Yanzhi Wang.
Formal analysis: Ming-Liang Lu, Gang Sun, Hua Huang, Xiaomei Zhang, Youqing Xu, Shiyao Chen, Ying Song, Xueliang Li, Bin Lv, Jianlin Ren, Xueqing Chen, Hui Zhang, Chen Mo, Yanzhi Wang, Yunsheng Yang.
Funding acquisition: Yunsheng Yang.
Investigation: Ming-Liang Lu.
Methodology: Ming-Liang Lu.
Project administration: Yunsheng Yang.
Writing – original draft: Ming-Liang Lu.
Writing – review & editing: Gang Sun, Hua Huang, Xiaomei Zhang, Youqing Xu, Shiyao Chen, Ying Song, Xueliang Li, Bin Lv, Jianlin Ren, Xueqing Chen, Hui Zhang, Chen Mo, Yanzhi Wang, Yunsheng Yang.
Supplementary Material
Footnotes
Abbreviations: AUC = area under the curve, CI = confidence interval, CRS = complete Rockall Score, GBS = Glasgow-Blatchford score, ICD = International Classification of Diseases, Ninth Revision, NVUGIH = nonvariceal upper gastrointestinal bleeding, ROC = receiver operating characteristic curve, RS = Rockall Score.
The design, collection of all the data and data analysis were supported by Hundreds of Young and Middle-Aged Academic and Technical Backbone Projects in Kunming Medical University (Grant No. 60117190431) and Grant Major Scientific Research Projects of Ministry of Health Industry (Grant No. 201002020).
The authors declare that they have no conflict of interest.
Supplemental Digital Content is available for this article.
References
- [1].Managing acute upper gastrointestinal bleeding. Lancet 2011;377:1048. [DOI] [PubMed] [Google Scholar]
- [2].Barkun AN, Bardou M, Kuipers EJ, et al. International consensus recommendations on the management of patients with nonvariceal upper gastrointestinal bleeding. Ann Intern Med 2010;152:101–13. [DOI] [PubMed] [Google Scholar]
- [3].Rockall TA, Logan RF, Devlin HB, et al. Risk assessment after acute upper gastrointestinal haemorrhage. Gut 1996;38:316–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Blatchford O, Murray WR, Blatchford M. A risk score to predict need for treatment for upper-gastrointestinal haemorrhage. Lancet 2000;356:1318–21. [DOI] [PubMed] [Google Scholar]
- [5].Gonzalez-Gonzalez JA, Monreal-Robles R, Garcia-Compean D, et al. Nonvariceal upper gastrointestinal bleeding in elderly people: Clinical outcomes and prognostic factors. J Dig Dis 2017;18:212–21. [DOI] [PubMed] [Google Scholar]
- [6].Rockall TA. Risk scoring in acute upper gastrointestinal haemorrhage. Dig Liver Dis 2006;38:10–1. [DOI] [PubMed] [Google Scholar]
- [7].Chandra S, Hess EP, Agarwal D, et al. External validation of the Glasgow-Blatchford Bleeding Score and the Rockall Score in the US setting. Am J Emerg Med 2012;30:673–9. [DOI] [PubMed] [Google Scholar]
- [8].Cheng DW, Lu YW, Teller T, et al. A modified Glasgow Blatchford Score improves risk stratification in upper gastrointestinal bleed: a prospective comparison of scoring systems. Aliment Pharmacol Ther 2012;36:782–9. [DOI] [PubMed] [Google Scholar]
- [9].Ko IG, Kim SE, Chang BS, et al. Evaluation of scoring systems without endoscopic findings for predicting outcomes in patients with upper gastrointestinal bleeding. BMC Gastroenterol 2017;17:159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Islam MS, Uddin MZ, Ali MS, et al. Modified Blatchford Score for risk stratification in adult patient with nonvariceal upper gastrointestinal haemorrhage and their short term hospital outcome. Mymensingh Med J 2017;26:490–7. [PubMed] [Google Scholar]
- [11].Koksal O, Ozeren G, Ozdemir F, et al. Prospective validation of the Glasgow Blatchford scoring system in patients with upper gastrointestinal bleeding in the emergency department. Turk J Gastroenterol 2012;23:448–55. [DOI] [PubMed] [Google Scholar]
- [12].Siau K, Chapman W, Sharma N, et al. Management of acute upper gastrointestinal bleeding: an update for the general physician. J R Coll Physicians Edinb 2017;47:218–30. [DOI] [PubMed] [Google Scholar]
- [13].Robertson M, Majumdar A, Boyapati R, et al. Risk stratification in acute upper GI bleeding: comparison of the AIMS65 score with the Glasgow-Blatchford and Rockall scoring systems. Gastrointest Endosc 2016;83:1151–60. [DOI] [PubMed] [Google Scholar]
- [14].Sung JJ, Chan FK, Chen M, et al. Asia-Pacific Working Group consensus on non-variceal upper gastrointestinal bleeding. Gut 2011;60:1170–7. [DOI] [PubMed] [Google Scholar]
- [15].Sung JJ, Chiu PC, Chan FKL, et al. Asia-Pacific working group consensus on non-variceal upper gastrointestinal bleeding: an update 2018. Gut 2018;67:1757–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Dicu D, Pop F, Ionescu D, et al. Comparison of risk scoring systems in predicting clinical outcome at upper gastrointestinal bleeding patients in an emergency unit. Am J Emerg Med 2013;31:94–9. [DOI] [PubMed] [Google Scholar]
- [17].Custodio Lima J, Garcia Montes C, Kibune Nagasako C, et al. Performance of the Rockall scoring system in predicting the need for intervention and outcomes in patients with nonvariceal upper gastrointestinal bleeding in a Brazilian setting: a prospective study. Digestion 2013;88:252–7. [DOI] [PubMed] [Google Scholar]
- [18].Robins GG, Sarwar MS, Armstrong MJ, et al. Evaluation of the need for endoscopy to identify low-risk patients presenting with an acute upper gastrointestinal bleed suitable for early discharge. Postgrad Med J 2007;83:768–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Pang SH, Ching JY, Lau JY, et al. Comparing the Blatchford and pre-endoscopic Rockall score in predicting the need for endoscopic therapy in patients with upper GI hemorrhage. Gastrointest Endosc 2010;71:1134–40. [DOI] [PubMed] [Google Scholar]
- [20].Shahrami A, Ahmadi S, Safari S. Full and modified Glasgow-Blatchford bleeding score in predicting the outcome of patients with acute upper gastrointestinal bleeding; a diagnostic accuracy study. Emerg (Tehran) 2018;6:e31. [PMC free article] [PubMed] [Google Scholar]
- [21].Bryant RV, Kuo P, Williamson K, et al. Performance of the Glasgow-Blatchford score in predicting clinical outcomes and intervention in hospitalized patients with upper GI bleeding. Gastrointest Endosc 2013;78:576–83. [DOI] [PubMed] [Google Scholar]
- [22].Ahn S, Lim KS, Lee YS, et al. Blatchford score is a useful tool for predicting the need for intervention in cancer patients with upper gastrointestinal bleeding. J Gastroenterol Hepatol 2013;28:1288–94. [DOI] [PubMed] [Google Scholar]
- [23].Lee MS, Cheng CL, Liu NJ, et al. Comparison of Rockall and Blatchford scores to assess outcome of patients with bleeding peptic ulcers after endoscopic therapy. Hepatogastroenterology 2013;60:1990–7. [PubMed] [Google Scholar]
- [24].Ur-Rahman A, Guan J, Khalid S, et al. Both full Glasgow-Blatchford score and Modified Glasgow-Blatchford score predict the need for intervention and mortality in patients with acute lower gastrointestinal bleeding. Dig Dis Sci 2018;63:3020–5. [DOI] [PubMed] [Google Scholar]
- [25].Lim LG, Ho KY, Chan YH, et al. Urgent endoscopy is associated with lower mortality in high-risk but not low-risk nonvariceal upper gastrointestinal bleeding. Endoscopy 2011;43:300–6. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


