Abstract
The aim of the study was to evaluate the human immunodeficiency virus (HIV) treatment cascade and mortality in migrants and citizens living with HIV in Botswana.
Retrospective 2002 to 2016 cohort study using electronic medical records from a single center managing a high migrant case load.
Records for 768 migrants and 3274 citizens living with HIV were included. Maipelo Trust, a nongovernmental organization, funded care for most migrants (70%); most citizens (85%) had personal health insurance. Seventy percent of migrants and 93% of citizens had received antiretroviral therapy (ART). At study end, 44% and 27% of migrants and citizens, respectively were retained in care at the clinic (P < .001). Among the 35% and 60% of migrants and citizens on ART respectively with viral load (VL) results in 2016, viral suppression was lower among migrants (82%) than citizens (95%) (P < .001). Citizens on ART had a median 157-unit [95% confidence interval (CI) 122–192] greater increase in CD4+ T-cell count (last minus first recorded count) than migrants after adjusting for baseline count (P < .001). Five-year survival was 92% (95% CI = 87.6–94.8) for migrants and 96% (95% CI = 95.4–97.2) for citizens. Migrants had higher mortality than citizens after entry into care (hazard ratio = 2.3, 95% CI = 1.34–3.89, P = .002) and ART initiation (hazard ratio = 2.2, 95% CI = 1.24–3.78, P = .01).
Fewer migrants than citizens living with HIV in Botswana were on ART, accessed VL monitoring, achieved viral suppression, and survived. The HIV treatment cascade appears suboptimal for migrants, undermining local 90-90-90 targets. These results highlight the need to include migrants in mainstream-funded HIV treatment programs, as microepidemics can slow HIV epidemic control.
Keywords: antiretroviral therapy, human immunodeficiency virus, migrants, mortality, treatment cascade, viral suppression
1. Introduction
To reach human immunodeficiency virus (HIV) epidemic control, Joint United Nation Program on HIV and AIDS proposed the 90-90-90 and the Fast-Track's 95-95-95 targets, now pillars of the world's approach to HIV treatment.[1,2] The strategy seeks to control HIV using testing to identify and treat all people living with HIV (PLHIV), and achieve zero discrimination. The ultimate goal is HIV incidence reduction. These targets cannot be achieved without addressing microepidemics among subpopulations at increased risk of HIV and providing equitable access to care.[3] Despite progress globally and in sub-Saharan Africa toward the 90-90-90 targets,[4] some populations remain highly vulnerable, including mobile populations, and are often excluded from mainstream HIV treatment programs and experience specific barriers to healthcare.
In sub-Saharan Africa, international migration generally occurs from poorer to more economically and politically stable nations. Mobile populations that move within a country (internal migration) or cross borders (international migration) are a priority in the HIV response.[5,6] Although the extent of the association between migration and HIV transmission is debated, population mobility hinders HIV prevention and treatment,[7] with migrants living with HIV often struggling to access treatment.[8,9]
Botswana is an upper middle-income country that attracts refugees, asylum seekers, and immigrants (migrants or noncitizens), including those from countries with high HIV prevalence, such as Zimbabwe, Zambia, and South Africa.[10] In 2015, an estimated 161,000 documented migrants in Botswana represented ∼7% of the total population.[11] With many unskilled and undocumented migrant workers entering Botswana, this figure undoubtedly underestimates the migrant population. The influx of migrant labor into Botswana may hamper HIV prevention and control strategies at the end stages of the epidemic.
Although economically and politically stable, Botswana has the third-highest adult HIV prevalence globally—18.5%.[12] The country's HIV response is commendable; an estimated 87.4% of citizens diagnosed and living with HIV receive antiretroviral therapy (ART) and an estimated 96.5% are virologically suppressed.[13] However, while citizens have free ART access, migrants must obtain Botswana citizenship, marry a citizen, be born to a citizen, or be documented refugees confined to a camp to qualify. Many international migrants in Botswana do not qualify and cannot afford medical care and HIV treatment. Cost, negative attitudes of medical staff, fear of police/immigration officers, and language are additional barriers to migrant healthcare.[14]
Maipelo Trust, a nongovernmental organization (NGO) funded primarily by the US-based NGO Cover the Globe, subsidizes or fully funds services such as HIV diagnostics and ART for financially constrained migrants in Botswana. The funding supports the Independence Surgery, a private clinic in Gaborone, that since 2002 has provided HIV care to migrants from Zimbabwe, Zambia, Kenya, Mozambique, and other countries, and to Botswana citizens funded through a public-private partnership (PPP).
We report the outcomes of independence surgery patients, comparing retention of migrants and citizens in the latter stages of the HIV treatment cascade (ART coverage, viral suppression, and retention in care at the clinic), and mortality after entry into care and after ART initiation.
2. Design
We conducted a retrospective cohort study of all PLHIV attending the Independence Surgery, Gaborone, Botswana between 2002 and 2016. Electronic medical records (EMRs) capturing socioeconomic, laboratory, and clinical data of PLHIV were analyzed to determine funding pathway, ART status, immunological status (CD4+ T-cell count), viral suppression, retention in care at the clinic, and mortality.
2.1. Setting
Citizens’ HIV care was self-funded or through personal health insurance or the PPP. The PPP scheme operated between February 2006 and November 2013; thereafter, PPP patients and other citizens used government clinics. Migrants at the Independence Surgery self-paid, had personal health insurance, or were partially/fully funded by the Maipelo Trust (which fully or partially funded ART, but rarely laboratory costs). Migrant families were financially means tested; the Trust fully funded ART for those earning less than United States dollar (USD) 200/month, or partially fund (5% co-payment if earning USD200-400/month. Higher-earning migrant families self-paid for ART entirely, as did those with personal health insurance. All migrant patients received free consultations from volunteer clinicians. A standard first-line ART regimen with zidovudine-lamivudine-efavirenz costs approximately USD20/month, whereas tenofovir-emtricitabine-efavirenz costs approximately USD25/month. HIV RNA viral load (VL) test costs USD15.
2.2. Study participants
All PLHIV accessing the clinic between January 2002 and December 2016 were included. Children were defined as anyone younger than 18 years.[15] Some patients were on ART when referred to the clinic. PLHIV were categorized as migrants (individuals born outside the country, without Botswana citizenship) or citizens (individuals with a national identity card).
2.3. Definitions of variables
World Health Organization immunological staging was used to determine CD4+ T-cell categories based on the following CD4+ counts; severe: <200 cells/μL; advanced: 200 to 349 cells/μL; mild: 350 to 499 cells/μL; and none/not significant: ≥500 cells/μL.[16] ART coverage included all patients ever on ART, before first clinic visit or initiated at the clinic. The viral suppression threshold was defined as per national guidelines at VL <400 copies/mL.[17]
Retention in care at the Independence Surgery was defined as being in care (a documented clinic/pharmacy visit or laboratory visit/test) during the study's final year (2016) irrespective of ART status.[18] All patients lost to follow-up (LTFU), transferred, dead or with incomplete records to verify retention were classified as not retained in care. LTFU was based on a 90-day window of a missed clinic/pharmacy refill/laboratory visit for a patient initially in care.
Funding pathways for migrants were NGO fully funded, NGO partially funded, self-paying/personal health insurance, and refugee.
2.4. Procedures/data sources
A Microsoft Excel database was generated from the EMR system, containing all records for individuals with an ART initiation date (or on ART at first clinic visit), ART regimen, and/or a follow up VL in 2002 to 2016. ART regimens were based on a non-nucleoside reverse transcriptase inhibitor or protease inhibitor, or integrase inhibitor with a nucleoside reverse transcriptase inhibitor backbone. Viral suppression was assessed in the final study year for patients retained in care.
2.5. Statistical methods
We used descriptive statistics to describe funding pathway, ART coverage, viral suppression, and mortality for migrants and citizens. Groups were compared using Pearson's Chi-squared test. Logistic regression was used to identify associations between key variables (sex, age, duration of ART, ART regimen, CD4+ count, migrant/citizen) with viral suppression and retention in care; CD4+ count categories (<200; 200–349; 350–499; >500 cells/μL) were used. Kaplan-Meier analysis with log-rank statistics was used to compare time to ART initiation.
All-cause mortality was evaluated by Kaplan-Meier functions and Cox proportional hazards regression. Cohort entry was determined as the date of first clinic visit for PLHIV, and patients were censored at transfer out of care, LTFU, or end of sampling period (December 2016). To estimate the total effect of citizenship status on all-cause survival, we performed an unadjusted analysis. The total effect of citizenship on survival was estimated using an adjusted analysis. We hypothesized that the effects of citizenship on survival would be mediated by ART, baseline degree of illness, age at care entry, and period effects; we then performed a multivariable analysis adjusting for ART initiation, baseline CD4+ count, age, and calendar year at care entry to estimate residual direct effects. Effect measure modification was explored using graphical methods; no interaction effects were sufficiently influential to retain in the model. Due to potential for survival bias between care entry and ART initiation, we performed a complementary analysis on new initiators of ART—left truncated at ART initiation—to evaluate survival, unadjusted and adjusted for age, CD4+ count, and year at clinic entry.
Baseline and follow-up CD4+ counts for ART patients were compared using mean CD4+ counts and CD4+ count categories between groups using chi-squared tests. Proportions of migrant and citizen patients with severe immunosuppression (CD4+ count <200 cells/μL) were compared at baseline and follow-up. Immunological response for patients on ART was analyzed using quantile median regression; CD4+ counts were compared between baseline and follow-up CD4+ count at study end. A median regression was preferred over conventional mean regression due to marked skew in the CD4+ count data which was further resistant to common transformations (i.e., the count data remained skewed after log and square-root transformation). Factors associated with immunological response levels were analyzed in a univariate logistic regression model containing gender, age, duration of ART, ART regimen, CD4+ count, and migration status.
Statistical significance was defined as a 2-sided P value <.05. Analysis was performed using Stata version 14 statistical software (College Station, TX).
2.6. Ethical considerations
The Botswana Ministry of Health Human Research Review Committee, Children's Mercy Institutional Review Board, Monash University, and University of Washington approved the study. Consent was waived because the study involved a retrospective chart review with deidentified data. The study was classified as posing minimal risk to study participants.
3. Results
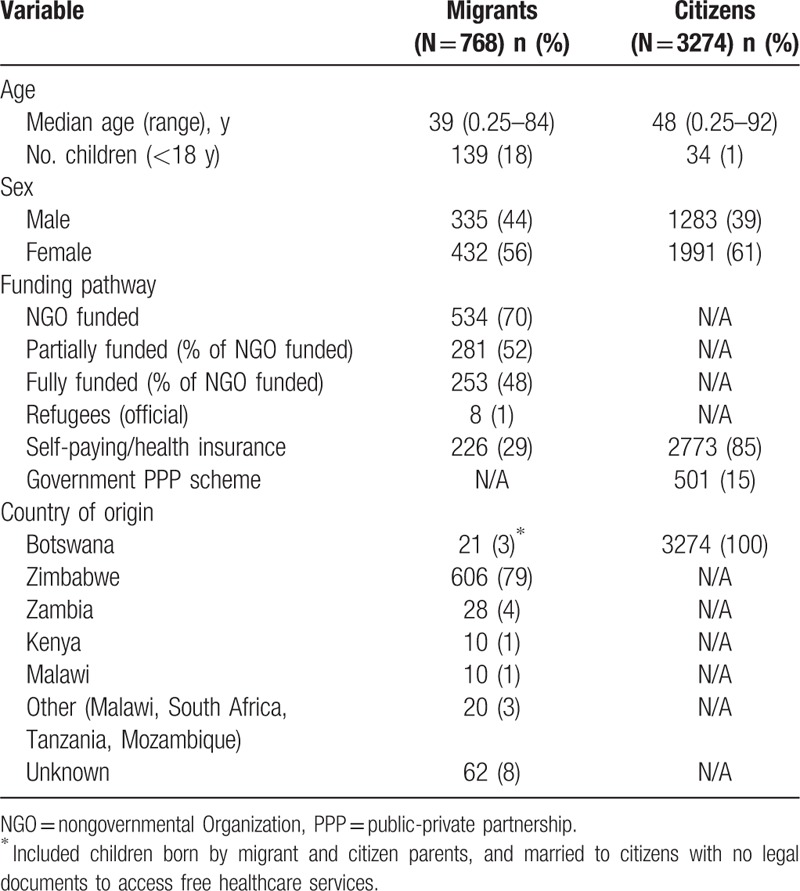
Of the 4042 PLHIV registered at the clinic in 2002 to 2016, 20% (n = 768) were migrants and 80% (n = 3274) citizens (Table 1). At first clinic visit, migrants were younger and included more children than citizens (18% vs 1%). Most patients were female (56% and 61% among migrants and citizens, respectively). Migrants’ care was funded by the NGO (70%) (partially/fully funded) or self-paid/personal health insurance (29%). Most migrants receiving HIV care at the clinic were from Zimbabwe (79%). Most citizens had HIV care funded through personal health insurance (85%) or the PPP scheme (15%) (Table 1).
Table 1.
Demographic characteristics of migrants and citizens.
3.1. ART coverage
Ninety percent (n = 3642) of all PLHIV received ART during the study; 77% (n = 593) of migrants and 65% (n = 2385) initiated ART at the clinic. Migrants initiated ART more rapidly than citizens; median times to ART initiation from first clinic visit were 11 days [interquartile range (IQR): 1–142 days] and 91 days (IQR: 7–748), respectively (P < .001). Seventy-six percent of migrants and 58% of citizens initiated ART within 6 months of first clinic visit (P < .001).
ART coverage was higher among NGO fully funded migrants (77%; n = 195) than refugees (60%; n = 3), NGO partially funded migrants (46%; n = 246), and self-paying/personal health insurance migrants (29%; n = 226). Citizens on the PPP scheme were more likely to be on ART (99%; n = 498) than self-paying/personal health insurance citizens (85%; n = 2773). Self-paying/personal health insurance migrants were less likely to be on ART than self-paying/personal health insurance citizens (P < .001) (Table 2).
Table 2.
Clinical outcomes of migrants and citizens on antiretroviral therapy.
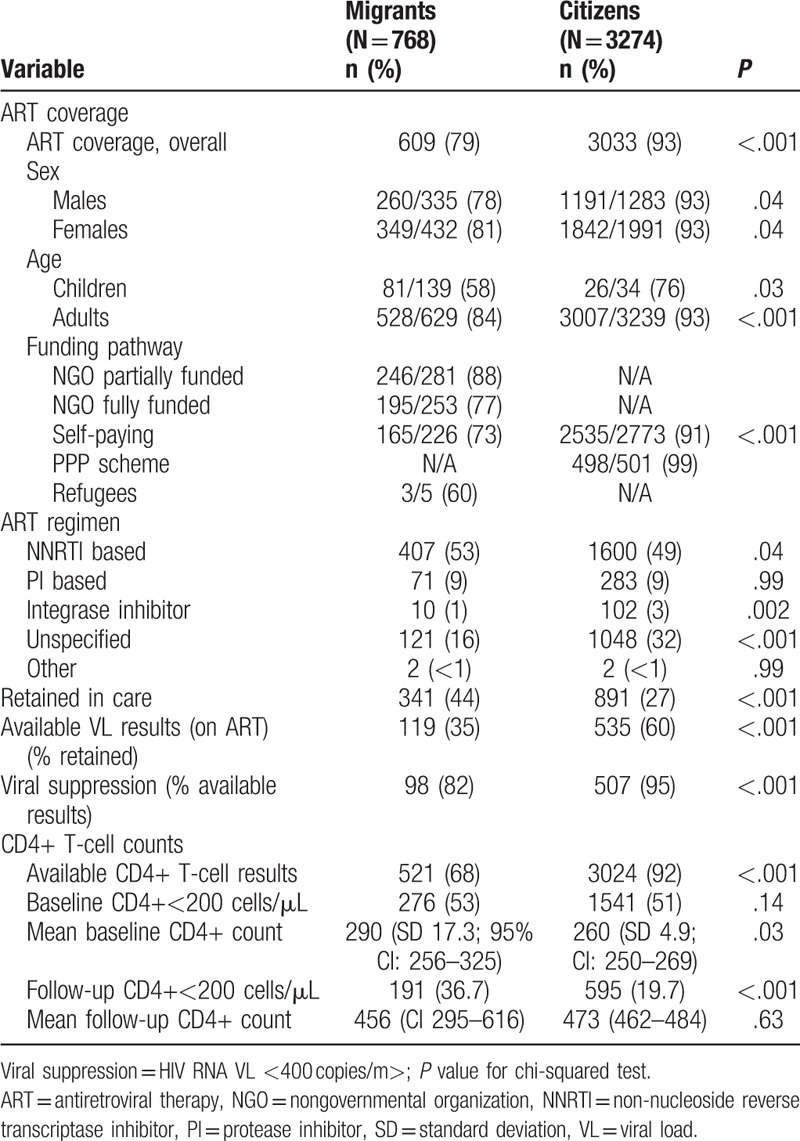
3.2. Retention in care at the Independence Surgery
Of 768 migrants, 44% (n = 341) were retained in care at the Independence Surgery in the last study year; 48% (n = 372) had incomplete records to ascertain retention, 2% (n = 18) had transferred, and 5% (n = 37) died. Of the 3274 citizens, 27% (n = 891) were retained in care, 70% (n = 2261) transferred to government clinics, and 4% (n = 122) died. The overall median time retained in care was 4.3 years (IQR: 0.2–9.8 years); 1.2 years (IQR: 0.1–4.2 years) for migrants, and 5.9 years (IQR: 1.2–10.3) for citizens.
Self-paying/personal health insurance migrants (50/226) were less likely to be retained in care than self-paying citizens (891/2773) (22% vs 32%; P = .002). Fifty-eight percent (n = 146) of NGO fully funded migrants, 49% (n = 139) of partially funded migrants and 6 of 8 (75%) refugees were retained in care.
Due to a high proportion of citizens being transferred to government clinics in November 2013, a higher proportion of migrants were classified as retained in care at the Independence Surgery (44%; n = 341) than citizens (27%, n = 891) [unadjusted odds ratio (OR) = 0.54; P < .001]. Overall, female sex (unadjusted OR 1.25; P < .002), Zimbabwe nationality (OR 1.99; P < .001), and baseline CD4+ count category 350 to 499 (unadjusted OR 1.26; P = .04 vs CD4+ count <200 cells/μL) were associated with retention in care at the Independence Clinic.
3.3. Viral suppression
Of 341 migrants retained in care, 35% (n = 119) had VL results and 82% (n = 98) had viral suppression. Of the 891 citizens retained in care, 60% (n = 535) had VL results and 95% (n = 507) had viral suppression. Migrants had significantly lower viral suppression than citizens (P < .001) (Table 2).
Self-paying citizens had the highest viral suppression (95%; 507/534), followed by self-paying migrants (93%; 26/28) and NGO fully funded migrants (84%; 31/37). The lowest level of viral suppression was among partially funded migrants (75%; 38/51). All 3 refugees with VL results were virologically suppressed.
In univariate analysis, citizenship (unadjusted OR 1.40; P = .01), female sex (OR 1.39; P < .001), and baseline CD4+ count 200 to 249 cells/μL (compared to <200 cells/μL) (OR 1.35; P = .01) were associated with greater odds of viral suppression. Children had lower odds of viral suppression (OR = 0.49; P = .02).
The HIV treatment cascade for migrants and citizens (Fig. 1) shows ART coverage, viral suppression, and retention in care at Independence Surgery. Overall, the HIV treatment cascade for migrants was inferior to that of citizens.
Figure 1.
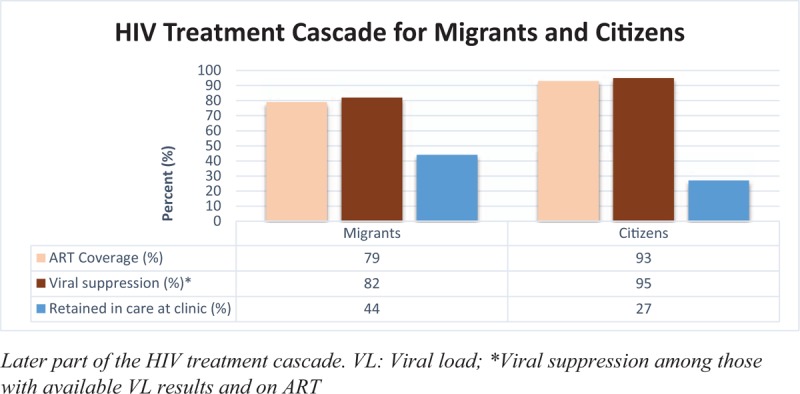
Human immunodeficiency virus (HIV) treatment cascade for migrants and citizens. ART = antiretroviral therapy.
3.4. Immunological response
Sixty-eight percent of migrants and 92% of citizens had baseline CD4+ count results; the proportions of migrants and citizens with severe immunosuppression (CD4+ count <200 cells/μL) at baseline were similar (Table 2). A quantile median regression analysis showed citizens on ART had a median 157-unit (95% CI 122–192) greater increase in CD4+ count (last minus first recorded count) than migrants after adjusting for baseline count (P < .001). Female sex was associated with a median 47-unit (95% CI 19–75) greater increase in CD4+ count than male sex (P < .001). A baseline CD4+ count category 200 to 349 cells/μL was associated with a median 59-unit (95% CI 88–30) greater decrease in CD4+ count than CD4+ count <200 cells/μL (P < .001).
3.5. Mortality
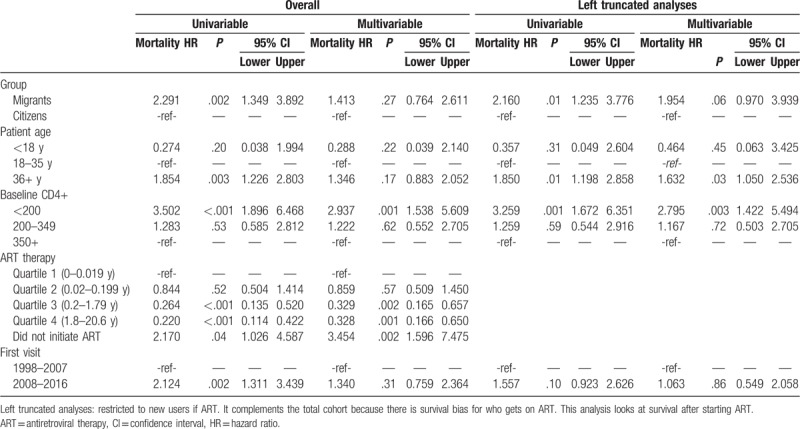
Mortality was higher among migrants, with overall 5-year survival of 92% (95% CI: 87.6–94.8) compared to 96% (95% CI: 95.4–97.2) for citizens (P < .001) (Fig. 2). Crude hazard of mortality was significantly higher among migrants, and those aged >35 years, those with a baseline CD4+ count <200 cells/μL, and those not on ART (Table 3). The relationship between migrant status and mortality was nonsignificant after adjustment for these covariates. When restricted to those who initiated ART at the clinic, crude survival was still lower in migrants, and in people aged >35 years and with CD4+ count <200 cells/μL (Table 3).
Figure 2.
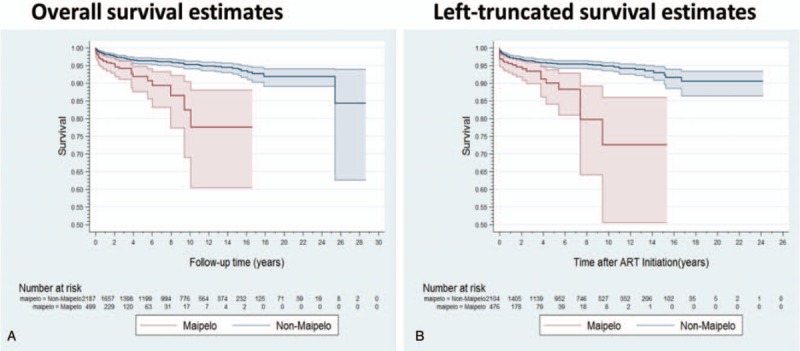
Kaplan-Meier survival estimates for migrants (Maipelo) versus citizens (non-Maipelo).
Table 3.
Cox models: overall and left-truncated mortality for migrants and citizens.
4. Discussion
Few researchers have compared HIV outcomes of migrants and citizens in sub-Saharan Africa. We found that migrants in Botswana had lower ART coverage, VL monitoring while on ART, viral suppression rates, and higher mortality than citizens. The study highlights how nationality and access to treatment services influence outcomes amongst PLHIV in Botswana.
National HIV prevalence in Botswana is estimated to be >20%,[11,19] similar to a recent estimate of 20% among migrants in peri-urban settings.[20] However, 2 previous migrant HIV prevalence estimates were 1% and 29%.[21,22] Although the prevalence of HIV in migrant populations in Botswana is uncertain, high prevalence in neighboring source countries suggests migrants should be considered in the local HIV response. Importantly, social mixing occurs between migrants and citizens,[23] so sexual networks of migrants and citizens are probable. Hence, migrants can facilitate HIV spread if they are unable to access or be maintained on treatment.
Botswana has achieved high HIV treatment coverage and viral suppression rates among its citizens, meeting the 90-90-90 targets.[4,13] This study, however, suggests that treatment coverage and viral suppression in migrants is lower than in citizens; moreover, migrants experience later HIV testing and diagnosis.[24,25] Although migrants can access free HIV testing in Botswana, they cannot access free HIV treatment from a government clinic. Other studies show lack of access to healthcare services is often a barrier to HIV treatment among migrant populations, who are typically socioeconomically disadvantaged.[26] In our study, only 29% of migrants had personal health insurance or could self-pay for HIV care and one percent had accessed HIV care through a refugee camp. Given the Maipelo Trust supports only a minority of migrants living with HIV in Botswana, with many migrants unaware of the NGO's support, and others unable to afford visits and VL testing, many migrants in Botswana lack access to HIV care and treatment. Consequently, migrants will engage in care late, increasing time to viral suppression, leading to poorer outcomes, and increased transmission risk.[21] However, the results of our study suggest migrants with access to care do relatively well, as evidenced by shorter time to ART initiation in migrants than citizens. The hope is to align migrant HIV care to the national program which includes early/same day ART initiation and the use of dolutegravir in first-line regimen. In addition, treatment coverage was high in individuals fully funded by the NGO, suggesting that where there is equal access, positive outcomes are expected.
At baseline, about half of migrants and citizens had severe immunosuppression, but citizens had better immune response to treatment. Our findings echo a European study showing migrants had significantly lower CD4+ counts and more acquired immunodeficiency syndrome events at baseline.[27] This study also showed that migrants were less likely to initiate ART, and had higher virologic and treatment failure. Children had lower odds of viral suppression compared to adults most-likely because children had better access to VL testing. However, the concern is whether children are being left behind with low viral suppression.[28,29] Where ART initiation and viral suppression rates are low, due to socioeconomic factors, immunological response is slow, as seen in migrants in Botswana. In other settings, late HIV diagnosis remains a concern, especially in migrants.[30,31]
Overall survival in migrants was worse, but may be mitigated by ART use. The greater mitigation of mortality risk in the overall cohort than in those initiating ART during the study suggests that ART initiation is a major driver of the observed mortality effect. However, other factors, which treatment cannot address, such as baseline illness (CD4+ count) and age, also affect survival. Our result suggests that not all the effects of citizenship status on survival are mediated by ART initiation, baseline degree of illness (CD4+ count), age, or period effects (as a measure of healthcare system changes over time). Migrants experienced higher mortality, often related to baseline characteristics, and whilst mortality may be partially mitigated by ART initiation, other interventions may be necessary to reduce mortality, such as earlier diagnosis and entry into care. Other factors related to noncitizen status may also contribute to mortality but were not measured here.
Healthcare systems often fail migrants; mobility is known to be associated with ART nonadherence, LTFU, deterioration in CD4+ count, HIV-related death, drug resistance, and noncontinuity of HIV care.[25] In our study, fewer migrants than citizens initiated ART, possibly because of transport costs; these were (possibly) undocumented migrants unable to move freely and/or whose income-generating activity precluded medical appointments. While our study did not capture migrants’ legal status, undocumented migrants are more likely to be LTFU and treatment access and success has also been shown to vary, sometimes depending on migration status. Ridolfo et al[32] found that the frequency of LTFU was higher in undocumented than documented migrants, but they had similar viral suppression rates. In our study, viral suppression was significantly higher in citizens (73%) than migrants (66%); a study in Kenya found similar, unacceptably low viral suppression rates in refugees and host nationals (74% and 70%; P = .66).[33]
Where policies promote equal access to ART and other healthcare services, migrants may achieve similar outcomes to citizens. Since 2007, South Africa has provided ART to refugee/asylum seekers with or without documentation.[34] McCarthy et al[35] demonstrated good treatment outcomes among foreigners/migrants receiving ART in South Africa; foreigners living with HIV had faster median time to ART initiation (14 vs 21 days, P = .008), as in our study (11 vs 101 days, P < .001). In our study, migrants rapidly initiated ART because clinicians tried to expedite treatment in some migrants who could not afford baseline laboratory investigations. Citizens in our study sometimes moved between private and government clinics. In the South African study, migrants had fewer hospital admissions, fewer missed appointments for ART initiation, better retention in care, lower mortality, and were less likely to fail ART than citizens. Ignoring undocumented status seems to promote healthcare access for migrants, leading to better outcomes.[36] We did not collect data on nutritional status and other opportunistic infections which may impact mortality.[37,38]
Tanser et al[25] found that migrants experience disparities in healthcare access due to legal status, unfamiliarity with the host environment, poor communication skills, and negative experience of culturally insensitive healthcare services and practices. As outlined above, citizens and migrants mix in Botswana, although the extent of their social and sexual networks is unknown and there have been no phylogenetic studies confirming HIV transmission between these groups. However, given the nature of how HIV transmits it is likely that not providing access to testing and treatment for migrants will negatively impact on Botswana's efforts to reduce HIV incidence.
The main limitations of our study were incomplete records and missing data. This hampered correctly classifying patients as retained or not retained in care, as well as viral suppression. We did not follow up patients who missed visits or those who transferred out to determine mortality or other clinical outcomes. Attempts to contact LTFU patients were hampered by inability to conduct home visits and patients’ cross-border mobility. The clinic also transitioned from a paper-based to EMR system during the study, which may have affected data entry.
5. Conclusion
Migrants living with HIV have poorer clinical outcomes than citizens, probably due to inability to pay for HIV care and treatment services. Migrants described herein were less likely to be on treatment or access VL monitoring, and had low viral suppression and higher mortality than citizens. The HIV treatment cascade was suboptimal for migrants and likely to negatively impact on the 90-90-90 target achievement; this will affect population-level HIV incidence reduction due to ongoing viremia in this subpopulation. These results highlight the need to include migrants in mainstream-funded HIV treatment programs, as microepidemics can slow or reverse HIV epidemic control.
Acknowledgments
The authors are grateful to patients living with HIV who attended Independence Surgery during the study period and the staff who assist them daily. The team is also thankful to Brian R. Lee who conducted the mortality analysis and Campbell Aitken for editing and proof reading the manuscript. Brian R. Lee and Campbell Aitken gave permission to be named.
Author contributions
Conception and design: TM, DY, LC, RK; Acquisition of data: RK, LC, TM, DD; Analysis and interpretation: TM, DY, BM, TS, SM, JHL, B-WS, SC, MS, MH, DD; Drafting and revising manuscript critically for important intellectual content: TM, DY, BM, TS, SM, JHL, B-WS, SC, MS, MH, DD.
Conceptualization: Tafireyi Marukutira, Dwight Yin, Laura Cressman, Ruth Kariuki, Shreshth Mawandia, Jenny H. Ledikwe, Bazghina-Werq Semo, Diana Dickinson.
Data curation: Tafireyi Marukutira, Dwight Yin, Laura Cressman, Ruth Kariuki, Brighid Malone, Tim Spelman, Diana Dickinson.
Formal analysis: Tafireyi Marukutira, Dwight Yin, Tim Spelman, Shreshth Mawandia, Diana Dickinson.
Investigation: Tafireyi Marukutira, Diana Dickinson, Dwight Yin.
Methodology: Tafireyi Marukutira, Dwight Yin, Shreshth Mawandia, Jenny H Ledikwe, Bazghina-Werq Semo, Suzanne Crowe, Mark Stoove, Margaret Hellard, Diana Dickinson.
Project administration: Tafireyi Marukutira, Laura Cressman, Ruth Kariuki, Diana Dickinson, Dwight Yin.
Resources: Tafireyi Marukutira, Diana Dickinson, Dwight Yin.
Supervision: Tafireyi Marukutira, Tim Spelman, Suzanne Crowe, Mark Stoove, Margaret Hellard, Diana Dickinson, Dwight Yin.
Validation: Tafireyi Marukutira, Laura Cressman, Ruth Kariuki, Brighid Malone, Tim Spelman, Shreshth Mawandia, Diana Dickinson, Dwight Yin.
Visualization: Tafireyi Marukutira, Ruth Kariuki, Brighid Malone, Tim Spelman, Shreshth Mawandia, Diana Dickinson, Dwight Yin.
Writing – original draft: Tafireyi Marukutira, Dwight Yin, Shreshth Mawandia, Bazghina-Werq Semo.
Writing – review and editing: Tafireyi Marukutira, Dwight Yin, Laura Cressman, Ruth Kariuki, Brighid Malone, Tim Spelman, Shreshth Mawandia, Jenny H Ledikwe, Bazghina-Werq Semo, Suzanne Crowe, Mark Stoove, Margaret Hellard, Diana Dickinson.
Tafireyi Marukutira orcid: 0000-0003-1142-6114.
Footnotes
Abbreviations: AIDS = acquired immunodeficiency syndrome, ART = antiretroviral therapy, CI = confidence interval, EMR = electronic medical records, HIV = human immunodeficiency virus, HR = hazard ratio, IQR = interquartile range, LTFU = lost to follow-up, NGO = nongovernmental organization, OR = odds ratio, PLHIV = people living with HIV, PPP = public private partnership, USD = United States dollar, VL = viral load.
A poster abstract was presented at the International acquired immunodeficiency syndrome Society (IAS) Conference, Amsterdam, Netherlands, July 2018. Abstract number: WEPEB141.
TM is supported by the Australian Government for his PhD studies. MH receives a Fellowship from the National Health and Medical Research Council of Australia and an investigator initiated funding from Gilead Sciences, Abbvie, and GSK for research unrelated to HIV care. The remaining authors report no conflicts of interest.
References
- [1].UNAIDS. 90-90-90 An ambitious treatment target to help end the AIDS epidemic. Geneva, Switzerland: UNAIDS; 2014. Available at http://www.unaids.org/sites/default/files/media_asset/90-90-90_en.pdf. Accessed July 6, 2018. [Google Scholar]
- [2].UNAIDS. Fast-track commitments to end AIDS by 2030. Geneva: UNAIDS; 2016. Available at http://www.unaids.org/sites/default/files/media_asset/fast-track-commitments_en.pdf. Accessed August 16, 2018. [Google Scholar]
- [3].Brown AE, Attawell K, Hales D, et al. Monitoring the HIV continuum of care in key populations across Europe and Central Asia. HIV Med 2018;19:431–9. [DOI] [PubMed] [Google Scholar]
- [4].UNAIDS. Ending AIDS: Progress towards the 90–90–90 targets. UNAIDS; 2017. Available at http://www.unaids.org/sites/default/files/media_asset/Global_AIDS_update_2017_en.pdf. Accessed August 16, 2018. [Google Scholar]
- [5].World Health Organization (WHO). Consolidated guidelines on HIV testing services. WHO; 2015. Available at http://apps.who.int/iris/bitstream/10665/179870/1/9789241508926_eng.pdf. Accessed July 6, 2018. [Google Scholar]
- [6].International Organization for Migration (IOM). Glossary on Migration, International Migration Law IOM; 2011. Available at https://www.iom.int/key-migration-terms. Accessed May 24, 2018. [Google Scholar]
- [7].Kenyon C, Colebunders R, Voeten H, et al. Migration intensity has no effect on peak HIV prevalence: an ecological study. BMC Infect Dis 2014;14:350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Alvarez-del Arco D, Fakoya I, Thomadakis C, et al. High levels of postmigration HIV acquisition within nine European countries. AIDS 2017;31:1979–88. [DOI] [PubMed] [Google Scholar]
- [9].Fakoya I, Alvarez-del Arco D, Woode-Owusu M, et al. A systematic review of post-migration acquisition of HIV among migrants from countries with generalised HIV epidemics living in Europe: implications for effectively managing HIV prevention programmes and policy. BMC Public Health 2015;15:561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].UNAIDS. Global AIDS update. Geneva, Switzerland: UNAIDS; 2016. Available at http://www.unaids.org/sites/default/files/media_asset/global-AIDS-update-2016_en.pdf. Accessed July 6, 2018. [Google Scholar]
- [11].International Organization for Migration (IOM). Botswana Country Facts and Figures: IOM; 2016 Available at https://www.iom.int/countries/botswana. Accessed July 6, 2018. [Google Scholar]
- [12].Statistics Botswana. Botswana AIDS Impact Survey 2013. Central Statistics Office; 2014. Available at http://www.statsbots.org.bw/sites/default/files/publications/BOTSWANA%20AIDS%20IMPACT%20SURVEY%20IV%202013.pdf. Accessed July 18, 2018. [Google Scholar]
- [13].Gaolathe T, Wirth KE, Holme MP, et al. Botswana's progress toward achieving the 2020 UNAIDS 90-90-90 antiretroviral therapy and virological suppression goals: a population-based survey. Lancet HIV 2016;3:e221–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Moroka T, Tshimanga M. Barriers to and use of health care services among cross-border migrants in Botswana: implications for public health. Int J Migrat Health Social Care 2010;5:33–42. [Google Scholar]
- [15].Government of Botswana (GoB). Children Act, 2009, (2009). Act No. 8 of 2009. GoB; 2009. Available at http://www.ilo.org/dyn/natlex/natlex4.detail?p_lang=en&p_isn=97343. Accessed July 9, 2018. [Google Scholar]
- [16].World Health Organization (WHO). WHO case definitions of HIV for surveillance and revised clinical staging and immunological classification of HIV-related disease in adults and children. WHO; 2007. Available at http://apps.who.int/iris/handle/10665/43699. Accessed August 16, 2018. [Google Scholar]
- [17].Ministry of Health, Botswana. Handbook of the Botswana 2016 integrated HIV clinical care guidelines. MoH Botswana; 2016. Available at http://apps.who.int/medicinedocs/en/m/abstract/Js22413en/. Accessed July 6, 2018. [Google Scholar]
- [18].Geng EH, Nash D, Kambugu A, et al. Retention in care among HIV-infected patients in resource-limited settings: emerging insights and new directions. Curr HIV/AIDS Rep 2010;7:234–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].UNAIDS. Country factsheets: UNAIDS, 2017. Available at http://www.unaids.org/en/regionscountries/countries/botswana. Accessed August 6, 2018. [Google Scholar]
- [20].Marukutira T, Alwano M-G, Behel S, et al. Immigrants and Botswana's ART Program: Potential Barriers to Epidemic Control. Conference on Retroviruses and Opportunistic Infections (CROI); February 13–16, 2017; Seattle, USA 2017. Available at http://www.croiconference.org/sessions/immigrants-and-botswana%E2%80%99s-art-program-potential-barriers-epidemic-control-0. Accessed July 18, 2018. [Google Scholar]
- [21].McGrath N, Eaton JW, Newell M-L, et al. Migration, sexual behaviour, and HIV risk: a general population cohort in rural South Africa. Lancet HIV 2015;2:e252–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Norris AH, Weisband YY, Wiles M, et al. Prevalence of sexually transmitted infections among Tanzanian migrants: a cross-sectional study. Int J STD AIDS 2017;28:991–1000. [DOI] [PubMed] [Google Scholar]
- [23].Voeten HA, Vissers DC, Gregson S, et al. Strong association between in-migration and HIV prevalence in urban sub-Saharan Africa. Sex Transm Dis 2010;37:240–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Aung E, Blondell SJ, Durham J. Interventions for increasing HIV testing uptake in migrants: a systematic review of evidence. AIDS Behav 2017;21:2844–59. [DOI] [PubMed] [Google Scholar]
- [25].Tanser F, Barnighausen T, Vandormael A, et al. HIV treatment cascade in migrants and mobile populations. Curr Opin HIV AIDS 2015;10:430–8. [DOI] [PubMed] [Google Scholar]
- [26].Zihindula G, Meyer-Weitz A, Akintola O. Access to health care services by refugees in Southern Africa: a review of literature. South Afr J Demogr 2015;16:96–109. [Google Scholar]
- [27].Saracino A, Lorenzini P, Lo Caputo S, et al. Increased risk of virologic failure to the first antiretroviral regimen in HIV-infected migrants compared to natives: data from the ICONA cohort. Clin Microbiol Infect 2016;22:288.e1-8. [DOI] [PubMed] [Google Scholar]
- [28].Puga D, Cerutti B, Molisana C, et al. Still far from 90-90-90: virologic outcomes of children on antiretroviral therapy in nurse-led clinics in Rural Lesotho. Pediatr Infect Dis J 2016;35:78–80. [DOI] [PubMed] [Google Scholar]
- [29].Davies M-A, Pinto J. Targeting 90-90-90 don’t leave children and adolescents behind. J Int AIDS Soc 2015;18:20745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Van Opstal SE, Van der Zwan JS, Wagner MN, et al. Late presentation of HIV infection in the Netherlands: reasons for late diagnoses and impact on vocational functioning. AIDS and Behav 2018;22:2593–603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Telfer B, Selvey C, Bowden V, et al. Predictors of late diagnosis for people newly diagnosed with HIV infection in NSW. Australian HIV and AIDS Conference; November 6–8, 2017; Canberra, Australia. Available at https://az659834.vo.msecnd.net/eventsairaueprod/production-ashmpublic/15613d60eb00463685268ff99ea3537. Accessed August 6, 2018. [Google Scholar]
- [32].Ridolfo AL, Oreni L, Vassalini P, et al. Effect of legal status on the early treatment outcomes of migrants beginning combined antiretroviral therapy at an outpatient clinic in Milan Italy. J Acquir Immune Defic Syndr 2017;75:315–21. [DOI] [PubMed] [Google Scholar]
- [33].Mendelsohn JB, Spiegel P, Grant A, et al. Low levels of viral suppression among refugees and host nationals accessing antiretroviral therapy in a Kenyan refugee camp. Confl Health 2017;11:11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Department of Health, Republic of South Africa. Revenue directive from Chief Financial Officer to all Provincial Health Revenue Managers HIV/AIDS Directorates dated September 19, 2007 regarding: Refugees/Asylum Seekers with or without a Permit. Available at http://www.probono.org.za/Downloads/asylum_seekers.pdf. Accessed August 18, 2018. [Google Scholar]
- [35].McCarthy K, Chersich MF, Vearey J, et al. Good treatment outcomes among foreigners receiving antiretroviral therapy in Johannesburg, South Africa. Int J STD AIDS 2009;20:858–62. [DOI] [PubMed] [Google Scholar]
- [36].Mendelsohn JB, Schilperoord M, Spiegel P, et al. Is forced migration a barrier to treatment success? Similar HIV treatment outcomes among refugees and a surrounding host community in Kuala Lumpur, Malaysia. AIDS Behav 2014;18:323–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Liu E, Spiegelman D, Semu H, et al. Nutritional status and mortality among HIV-infected patients receiving antiretroviral therapy in Tanzania. J Infect Dis 2011;204:282–90. [DOI] [PubMed] [Google Scholar]
- [38].Cox JA, Kiggundu D, Elpert L, et al. Temporal trends in death causes in adults attending an urban HIV clinic in Uganda: a retrospective chart review. BMJ Open 2016;6:e008718. [DOI] [PMC free article] [PubMed] [Google Scholar]


