Abstract
This retrospective cohort study evaluated the effects of different frequencies of physical therapy intervention on the total knee arthroplasty (TKA) and total hip arthroplasty (THA) risk of osteoarthritis (OA) patients.
We sampled 438,833 insurants from Taiwan National Health Insurance Research Database for patients diagnosed as having OA during 2000 to 2013. OA who received physical therapy within in the first year of OA diagnosis were divided based on the number of sessions they received in that first year: >24, 13–23, and <12 sessions.
The results revealed that the TKA and THA incidence rates among patients aged 60 to 80 years were respectively 3.5% and 0.9% in the >24 cohort and 4.9% and 1.4% (all P < .001) in the comparison cohort. Moreover, the HRs of TKA and THA in the >24 cohort were 0.77 (0.67–0.87, P < .001) and 0.71 (0.53–0.96, P = .024), respectively. By contrast, no significant differences were noted between the 13–23 and <12 cohorts and their respective comparison cohorts.
In conclusion, our study results indicated that elderly patients aged 60 to 80 years who underwent >24 physical therapy sessions within 1 year of receiving an OA diagnosis exhibited reduced of TKA and THA risks.
Keywords: hip arthroplasty, knee arthroplasty, osteoarthritis, physical therapy
1. Introduction
The rapid aging of the global population has become a national concern in Taiwan. With the increase in the elderly population every year, several aging-related diseases are being clinically reported. Among the diseases of the skeletal muscular system in this population, osteoarthritis (OA) of the knee joint is the most common. The prevalence rate of knee OA among the elderly population (aged >65 years) is approximately 30–40%.[1] Moreover, with the increase in age, the degree of knee joint deterioration increases.[2] In addition to medical treatment, physical therapy intervention is most commonly used as a conservative treatment of degenerative knee OA. OA is characterized by cartilage wear and erosion,[3] and repairing and remodeling the related cartilage destruction is impossible.[4] The literature highlight that exercise can improve OA symptoms[5]; however, patients may not be easily able to develop a normal exercise habit if the pain is severe. Therefore, physical therapy with the use of instruments and exercise is a more effective alternative for most patients. Physical therapy delays disease progression and improves the time course of the joint arthroplasty.[6] Primary OA is the most common condition, particularly in middle-aged and elderly people aged >55 years.[7]
OA treatment includes surgery, drug intervention, and exercise.[8] Because repair and remodeling of the cartilage is impossible, the treatment mainly aims to eliminate pain, improve mobility, and avoid body deterioration caused by aging. Limited function leads to disability, in turn affecting the patients’ quality of life.[9] Engaging in the conservative exercise treatment can not only alleviate OA but also delay the deterioration of articular cartilage and stabilize the disease in patients with initial OA; moreover, the side effects of exercise therapy are fewer than those of other treatments.[10] Therefore, many physicians often encourage patients to actively engage in physical therapy. Clinical trials on physical therapy in patients with initial OA have evidenced its short-term effectiveness in symptom relief. However, whether it is effective in the long term and the appropriate time to start treatment so as to effectively delay the time course of artificial joint arthroplasty remain unclear.[10–12]
Therefore, this study mainly explored whether the use of frequent physical therapy during the early stages of OA delays joint deterioration, thus reducing the risk of joint arthroplasty.
2. Materials and methods
2.1. Data sources
With a longitudinal retrospective design, this study analyzed data of a random sample of 3 million among 23 million people from the National Health Insurance Research Database (NHIRD) in Taiwan. The study period was from 2000 to 2013. The Institutional Review Board of Show Chwan Memorial Hospital approved this study (IRB-No. 1050305) and waived the requirement of informed consent because the datasets in the NHIRD have no identifiable personal information.
2.2. Study design
We conducted a nationwide cohort study by recruiting OA patients from the NHIRD. The large sample size of the NHIRD facilitated the investigation of the effects of early treatment on patients with OA. We screened for individuals who received the first diagnosis of degenerative OA on the basis of International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) code 715, and the comparison cohort was matched to the physical therapy cohorts by age, sex, and index year. All OA patients had at least three outpatient records of OA; we considered any diagnosis after at least 1 year without an OA outpatient visit to be new. Early treatment was defined as physical therapy treatment in the first year after OA diagnosis.
Patients with a past history of OA were excluded, followed by patients who had undergone joint arthroplasty. Patients aged <18 or >80 years were also excluded. Subsequently, patients with no history of OA for at least 1 year before the index year were only considered to ensure consistency in disease severity and duration among the OA patients. The baseline measurement time points for all cohorts were based on the same index year.
According to the time of initial treatment and duration of physical therapy, the patients with OA were divided into several cohorts. The patients who received physical therapy within the first year of OA diagnosis were divided into 3 treatment cohorts: >24, 13–23, and <12 sessions. Consequently, each treatment cohort was age, sex, and index year matched with a comparison cohort comprising people who received the physical therapy 1 year after the diagnosis; the pairing was in the ratios of 1:4, 1:4, and 1:1 for >24, 13–23, and <12 cohorts, respectively. For risk assessment, the ethnic cohorts obtained after matching were divided into the following age groups: 18–39, 40–59, and 60–80 years (Fig. 1).
Figure 1.

Data Process Flow. Study subjects were identified from a nationwide cohort of 3 million people from 1 January 2000 to 31 December 2013 and were divided into the Treatment cohort: Number of physical treatments started within 1 year after osteoarthritis. Comparison cohort: physical treatment after 1 year composed of age-, sex-, index date and propensity score-matched people.
2.3. Definition section
We subgrouped the patients on the basis of when they began rehabilitation (treatment codes: 42001–42016, 43001–43008, and 43026) into the early rehabilitation (>24 times in the first year; n = 7987) and delayed rehabilitation (physical therapy after 1 year; n = 128,608) cohorts. The following comorbidities presenting before the date of the initial total hip arthroplasty (THA) and total knee arthroplasty (TKA) were considered: OA (ICD-9-CM: 715), hyperlipidemia (ICD-9-CM: 272), hypertension (HTN; ICD-9-CM: 401–405), diabetes mellitus (DM; ICD-9-CM: 250), and chronic kidney disease (ICD-9-CM: 250.4, 274.1,283.11,403.∗1, 404.∗2, 404.∗3,440.1,442.1,447.3,572.4,580–588, 642.1, 646.2).
2.4. Statistical analysis
The study conducted patient demographic data statistics and then with 1:4 and 1:1 pairing for sampled patients through propensity score tendency stratification, by matching controls the confounding factor to reduce possible bias. Propensity score matching (PSM) was performed using sex, age, and index year. The baseline characteristics and comorbidities did not differ between the treatment and comparison cohorts after PSM[13].
According to the data type, risk assessment statistics and statistical values, such as hazard ratios (HRs) and their 95% confidence intervals (95% CIs), were obtained using the t test, Chi-square test or Fisher exact test, and Cox regression analysis. All analyses were performed on SAS (version 9.1), R (version 3.1), and SPSS (version 21). A 2-tailed P of <.05 was considered significant.
3. Results
3.1. Cohort characteristics
In total, 438,833 patients were diagnosed as having OA from 2000 to 2013. Both the study and comparison cohorts were age, sex, and index year matched. The >24, 13–23, and <12 cohorts comprised 7987, 13,692, and 105,717 patients (Table 1), respectively, with their comparison cohorts including 31,948, 54,768, and 105,717 people, respectively. In the >24 cohort, average age was 62.1 years (P = .686); the proportion of patients with HTN, hyperlipidemia, and DM was 68.1%, 42.7%, and 34.0%, respectively (all P < .001); and the mean follow-up periods of the treatment and comparison cohorts were 6.95 and 7.23 person-years, respectively. In the 13–23 cohort, average age was 60.4 years (P = .711) and the mean follow-up periods of the treatment and comparison cohorts were 7.19 and 7.29 person-years, respectively. Finally, in the <12 treatment cohort, average age was 59.7 years (P = .879); no significant differences were observed in the proportions of HTN, hyperlipidemia, DM, and chronic kidney disease; and the mean follow-up periods of the treatment and comparison cohorts were 8.00 and 8.05 person-years, respectively.
Table 1.
Comparison of demographics and comorbidities.

3.2. Incidence of joint arthroplasty
In the >24, 13–23, and <12 cohorts (Table 2), TKA incidence rates were 3.5% (4.9% in comparison cohort; P < .001), 3.9% (4.4% in comparison cohort; P < .001), and 4.4% (4.7% in comparison cohort; P = .091), respectively. Furthermore, in the >24, 13–23, and <12 cohorts, THA incidence rates were 0.9% (1.4% in comparison cohort; P < .001), 1.2% (1.3% in comparison cohort; P = .311), and 1.3% (1.3% in comparison cohort; P = .314), respectively.
Table 2.
Comparison of artificial arthroplasty surgery.

3.3. Age-wise risk assessment
3.3.1. In patients aged 60 to 80 years
In the >24, 13–23, and <12 cohorts (Table 3), TKA HRs (95%CIs) were 0.77 (0.67–0.87, P < .001), 0.94 (0.85–1.04, P = .214), and 0.96 (0.91–1.00, P = .066), respectively. Furthermore, the >24, 13–23, and <12 cohorts, TKA HRs (95%CIs) were 0.71 (0.53–0.96, P = .024), 1.10 (0.90–1.34, P = .340), and 1.00 (0.90–1.11, P = .977), respectively.
Table 3.
Hazard ratios for artificial arthroplasty surgery assessment for different age cohorts.
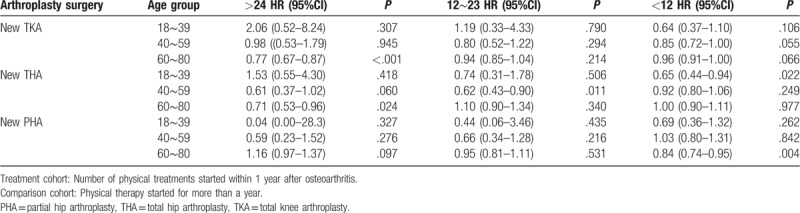
3.3.2. In patients aged 40 to 59 years
In the >24, 13–23, and <12 cohorts (Table 3), TKA HRs (95%CIs) were 0.98 (0.53–1.79, P < .945), 0.80 (0.52–1.22, P = .294), and 0.85 (0.72–1.00, P = .066), respectively. the >24, 13–23, and <12 cohorts, TKA HRs (95%CIs) were 0.71 (0.53–0.96, P = .024), 0.62 (0.43–0.90, P = .011), and 0.92 (0.8–1.06, P = .249).
3.3.3. In patients aged 18 to 39 years
In the >24, 13–23, and <12 cohorts (Table 3), TKA HRs (95%CIs) were 2.06 (0.52–8.24, P = .307), 1.19 (0.33–4.33, P = .790), and 0.64 (0.37–1.1, P = .106), respectively. Furthermore, the >24, 13–23, and <12 cohorts, THA HRs (95%CIs) were 1.53 (0.55–4.30, P = .418), 0.74 (0.31–1.78, P = .506), and 0.65 (0.44–0.94, P = .022), respectively.
4. Discussion
Few studies have reported the effects of specific timings of physical therapy intervention in recent years.[14,15] Several studies have evaluated suitable timings for physical therapy intervention after joint arthroplasty[16–19]; however, such studies on physical therapy intervention before joint arthroplasty are lacking. On comparison, we noted that patients who received physical therapy >24 sessions in the first year after OA diagnosis had a significantly lower TKA incidence rate than did those who received physical therapy after 1 year of the diagnosis (3.5% vs 4.9%, P < .001); similar results were noted for THA incidence rates (0.9% vs 1.4%, P < .001). The present study revealed that frequent and early physical therapy significantly reduces THA and TKA risk in patients with OA. The three patient cohorts were compared with propensity score-, sex-, age-, and index year-matched comparison cohorts. Thus, in the >24 cohort, the risk of TKA and THA were low [0.77 (P < .001) and 0.74 (P = .001), respectively].
By contrast, no differences in the incidence rates of TKA or THA were noted between the 13–23 and <12 cohorts and their respective comparison cohorts. In our study, undergoing >24 physical therapy sessions within 1 year of receiving an OA diagnosis can significantly reduce the risk of joint arthroplasty.
Our study demonstrated that the TKA and THA risk was relatively low only in >60-year-old patients who received >24 physical therapy sessions in the first year after OA diagnosis (Figs. 2 and 3). However, when the number of sessions was <24, no such significant effect was noted. Among the patients aged <60 years, no significant differences in TKA and THA incidence rates were observed between the treatment and comparison cohorts—even after early or more number of physical therapy sessions were conducted.
Figure 2.

Cumulative incidence of total knee arthroplasty (log rank P < .001) Development by >24 physical therapy sessions in the first year and delay physical therapy after 1 year cohorts.
Figure 3.

Cumulative incidence of total hip arthroplasty (log rank P < .001) development by >24 physical therapy sessions in the first year and delay physical therapy after 1 year cohorts.
Because the time course of arthritis is slow, at the therapeutic level, patients are always expected to be treated early for a more favorable prognosis; however, most patients may not be able to receive regular treatment or may receive insufficient treatment. The world population is rapidly aging; consequently, the number of elderly people is increasing at a fast pace. OA is a common skeletal muscular disease in the elderly population. As age advances, the incidence of skeletal muscular diseases increases. Repairing the degenerated joints is impossible; nevertheless, through early and frequent physical therapy, the deterioration of the joints can be delayed, and patient activity can be improved.
4.1. Study limitation
This study used the NHIRD as the source to analyze the data of OA patients from 2000 to 2013. First, the NHIRD does not comprise data on the patients’ place of residence, socioeconomic background, lifestyle habits, and immediate treatment evaluation (e.g., smoking, MI, and family history). Second, because of certain factors other than OA, the patient may have actually received physical therapy; however, no treatment code registration status is available in the NHIRD, which may cause an underestimation of the rate of physical therapy after OA diagnosis. Third, during diagnosis on the basis of ICD-9 diagnostic codes, the physician may make a classification error. Fourth, this observation study precluded the assumption of a causal relationship.
4.2. Future directions
Clinicians could be aware of the association between physical therapy and risks of TKA and THA and provide optimal treatments.
5. Conclusion
Our study indicated that patients aged 60 to 80 years who underwent >24 physical therapy sessions within 1 year of receiving an OA diagnosis exhibited reduced risks of TKA and THA. Elderly patients with degenerative joints should be provided early and frequent physical therapy in addition to conventional treatment.
Author contributions
Data curation: Yuan-Tsung Tseng
Formal analysis: Yuan-Tsung Tseng
Funding acquisition: Chun-Hsiang Wang.
Resources: Wen-ching Tsai, Hsing-Ting Wang
Supervision: Chun-Hsiang Wang
Writing – original draft: Wei-Heng Chen.
Footnotes
Abbreviations: CKD = chronic kidney disease, DM = diabetes mellitus, FTA = foot and toe joint arthroplasty, HPL = hyperlipidemia, HR = hazard ratio, HTN = hypertension, NHIRD = National Health Insurance Research Database, PHA = partial hip arthroplasty, PSA = partial shoulder arthroplasty, TAA = total ankle arthroplasty, TEA = total elbow arthroplasty, THA = total hip arthroplasty, TKA = total knee arthroplasty, TSA = total shoulder arthroplasty.
W-CT contributed equally to this work.
This work was supported in part by the Tainan Municipal Hospital Research Grants (RA16006, RD:105–13).
The research data source, the NHIRD, was provided by the Central Health Insurance Bureau and the National Health Research Institutes.
The authors declare no conflict of interest.
References
- [1].Liao CY, Chan HT, Chao E, et al. Comparison of total hip and knee joint replacement in patients with rheumatoid arthritis and osteoarthritis: a nationwide, population-based study. Singapore Med J 2015;56:58–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Felson DT, Naimark A, Anderson J, et al. The prevalence of knee osteoarthritis in the elderly. The Framingham Osteoarthritis Study. Arthritis Rheumatol 1987;30:914–8. [DOI] [PubMed] [Google Scholar]
- [3].Kleemann R, Krocker D, Cedraro A, et al. Altered cartilage mechanics and histology in knee osteoarthritis: relation to clinical assessment (ICRS Grade). Osteoarthritis Cartilage 2005;13:958–63. [DOI] [PubMed] [Google Scholar]
- [4].Lories RJ, Luyten FP. The bone–cartilage unit in osteoarthritis. Nat Rev Rheumatol 2011;7:43–9. [DOI] [PubMed] [Google Scholar]
- [5].Roos EM, Dahlberg L. Positive effects of moderate exercise on glycosaminoglycan content in knee cartilage: a four-month, randomized, controlled trial in patients at risk of osteoarthritis. Arthritis Rheumatol 2005;52:3507–14. [DOI] [PubMed] [Google Scholar]
- [6].Foster NE, Healey EL, Holden MA, et al. A multicentre, pragmatic, parallel group, randomised controlled trial to compare the clinical and cost-effectiveness of three physical therapy-led exercise interventions for knee osteoarthritis in older adults: The BEEP trial protocol (ISRCTN: 93634563). BMC Musculoskeletal Disord 2014;15:254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Peat G, McCarney R, Croft P. Knee pain and osteoarthritis in older adults: a review of community burden and current use of primary health care. Ann Rheum Dis 2001;60:91–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Hochberg MC, Altman RD, April KT, et al. American College of Rheumatology 2012 recommendations for the use of nonpharmacologic and pharmacologic therapies in osteoarthritis of the hand, hip, and knee. Arthritis Care Res 2012;64:465–74. [DOI] [PubMed] [Google Scholar]
- [9].Fransen M, McConnell S, Harmer AR, et al. Exercise for osteoarthritis of the knee: a Cochrane systematic review. Br J Sports Med 2015;49:1554–7. [DOI] [PubMed] [Google Scholar]
- [10].Holsgaard-Larsen A, Clausen B, Søndergaard J, et al. The effect of neuromuscular exercise compared with instruction in analgesic use on knee function in patients with early knee osteoarthritis–one year outcome of the exerpharma randomized trial. Osteoarthritis Cartilage 2017;25:S49. [DOI] [PubMed] [Google Scholar]
- [11].Kon E, Filardo G, Drobnic M, et al. Non-surgical management of early knee osteoarthritis. Knee Surg Sports Traumatol Arthrosc 2012;20:436–49. [DOI] [PubMed] [Google Scholar]
- [12].Bennell KL, Hinman RS. A review of the clinical evidence for exercise in osteoarthritis of the hip and knee. J Sci Med Sport 2011;14:4–9. [DOI] [PubMed] [Google Scholar]
- [13].Obermeyer Z, Makar M, Abujaber S, et al. Association between the Medicare hospice benefit and health care utilization and costs for patients with poor-prognosis cancer. JAMA 2014;312:1888–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Deyle GD, Henderson NE, Matekel RL, et al. Effectiveness of manual physical therapy and exercise in osteoarthritis of the knee: a randomized, controlled trial. Ann Intern Med 2000;132:173–81. [DOI] [PubMed] [Google Scholar]
- [15].Veerbeek JM, van Wegen E, van Peppen R, et al. What is the evidence for physical therapy poststroke? A systematic review and meta-analysis. PloS One 2014;9:e87987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Gilbey HJ, Ackland TR, Wang AW, et al. Exercise improves early functional recovery after total hip arthroplasty. Clin Orthop Relat Res 2003;408:193–200. [DOI] [PubMed] [Google Scholar]
- [17].Fortin PR, Clarke AE, Joseph L, et al. Outcomes of total hip and knee replacement: preoperative functional status predicts outcomes at six months after surgery. Arthritis Rheum 1999;42:1722–8. [DOI] [PubMed] [Google Scholar]
- [18].Munin MC, Rudy TE, Glynn NW, et al. Early inpatient rehabilitation after elective hip and knee arthroplasty. JAMA 1998;279:847–52. [DOI] [PubMed] [Google Scholar]
- [19].Parvataneni HK, Shah VP, Howard H, et al. Controlling pain after total hip and knee arthroplasty using a multimodal protocol with local periarticular injections: a prospective randomized study. J Arthroplasty 2007;22:33–8. [DOI] [PubMed] [Google Scholar]


