Abstract
Rationale:
Valgus knees are relatively rare in the clinic. Treatments for valgus deviations >90° represent a surgical challenge to achieve a balance between the soft tissue and bone and prevent nerve damage.
Patient concerns:
A 63-year-old woman with valgus deviations >90° in both knees complained that she had been unable to walk for 50 years.
Diagnoses:
Congenital malformation valgus deformity.
Interventions:
Bilateral total knee arthroplasty (TKA) was performed using a rotating hinge knee instrument from Endo-Model for axial correction and stabilization of the joint.
Outcomes:
The patient fully recovered 3 months after surgery. At the follow-up 6 years after the operation, the function of the knee joint clearly improved. The knee society score (KSS) increased from 35 to 90.
Lessons:
Constrained implants are commonly used to stabilize the joint and correct the bone axis in patients with severe ligamental instability, gross deformity, bone loss, and extreme deviation of the straight leg axis. Intraoperative exploration of the common peroneal nerve and the postoperative flexed position of the knee joints could help prevent nerve injuries.
Keywords: total knee arthroplasty, valgus deformity, hinge knee
1. Introduction
Total knee arthroplasty (TKA) is used to treat knee valgus deformity, and approximately 10% of all patients who require TKA present with valgus deformity.[1,2] According to the Keblish classification, the femorotibial angle (FTA) can be measured on the x-ray image of the valgus deformity; a mild angle is <15°, a moderate degree is 15° to 30°, and a severe deformity is an angle >30°.[3] Because of the different tensions of soft tissue and bone defects, different prostheses can be selected. For mild deformities and some moderate and severe knee valgus deformities, we can first release the lateral collateral ligament through tenolysis of the soft tissue then release the posterolateral articular capsule, the iliotibial band and the lateral head of the gastrocnemius, biceps tendon, and popliteal tendon tissue. Thus, soft-tissue balance can be obtained. For moderate and some severe valgus knee deformities, posterior cruciate-retaining total knee prostheses, constrained condylar knee prostheses, or varus-valgus constrained implants can be used to obtain a good result.[4] Some of the more severe valgus knee deformities with bone defects need to be fixed with an extension rod and the placement of a spacer block to achieve balance and stability. However, for some patients with severe deformities of the valgus knee, surface prostheses with soft tissue release are unable to achieve balance and stability. These cases often require the use of a hinge knee prosthesis to solve the problem. Hinge knee prostheses with good coronal stability can stably replace soft-tissue balance, but complications of looseness can occur, which are mainly due to sagittal alignment because the sagittal plane outputs a high amount of power; this pull eventually leads to prosthesis loosening.[5–7] Nonetheless, the loosening rate of the Endo-Model hinge prosthesis reported in the previously published literature is low.[8–11]
Knee valgus deformities can be congenital or may occur secondary to conditions such as osteoarthrosis, rheumatic diseases, and posttraumatic arthritis, or to an overcorrection following a valgus osteotomy.[4] Valgus deviations <20°, which account for approximately 95% of all valgus knees, are relatively easy to correct with surgery.[2] However, the correction of valgus deviations >20° is a challenging undertaking for joint surgeons.[2,12] Herein, we report a case of severe valgus deformity with a valgus deviation >90° in a 63-year-old woman who was successfully treated with TKA. To the best of our knowledge, this is the first documented case of successful treatment of a >90° valgus deformity with TKA. The patient and her family have consented to the publication of this article.
2. Case report
A 63-year-old woman presented at our hospital with congenital malformation valgus deformity >90° (Fig. 1A, B). An x-ray of the knee showed a malformed femoral condyle and tibial plateau with severe bone defects (Fig. 2). According to the Keblish classification, this case was classified as a severe deformity.[3] The patient has not been able to walk normally since the age of 12. The muscle strength of the quadriceps was low. A physical examination showed that all ligaments around the knee were slack. Through the above examination, the patient's knee society score (KSS) score was assessed to be 35.[13] The knee extension reached 90°, and the flexion reached 80°.
Figure 1.

(A, B) Preoperative photograph of the patient showing severe knee valgus deformity.
Figure 2.

Preoperative x-ray radiograph (nonweight-bearing) showing malformations and bony defects in the femoral condyle and the tibial plateau.
Before the operation, we created a three dimensional model of both knees, simulated the patella trajectory and carefully examined the patient's soft tissue tightness. Due to the presence of severe bone defection and the severe relaxation of the medial and lateral soft tissue devices, the Endo-Model rotating hinge knee prosthesis was chosen for the patient, and a bilateral TKA was performed. The knee joints were exposed via a medial parapatellar approach to achieve a good view because we did need to worry about soft-tissue balance. The femoral condyles were severely deformed with a small lateral femoral condyle and a relatively large medial femoral condyle. Tibial extorsion, lateral dislocation of the patella, and severe degeneration of articular surfaces of the femur, tibia, and patella were also observed. Bone hyperplasia and syndesmophyte formation around the joint were observed along with the worn medial and lateral menisci. The anterior and posterior cruciate ligaments were almost invisible.
After resection of the hyperplastic osteophyte and synovial membrane, the iliotibial band was first released, then the lateral retinaculum was released. Subsequently, the lateral ligament was directly incised.
Because the ligaments around the knee were slack, the Endo-Model rotating hinge knee prosthesis was used. Based on the preoperative x-ray, the femoral canal in the medial femoral condyle was selected as the entry point for the intramedullary guide. After the internal rotation, external rotation, alignment, and tautness of the knee joint were tested to meet the physiological requirements, the Germany Link knee prosthesis (left knee: tibia size 55 mm/160 mm, femur size 55 mm/160 mm, poly size 16 mm; the right knee prosthesis was the same size as the left) was installed. Full release of the patellar lateral retinaculum and strengthening of the patellar medial retinaculum were performed to correct the lateral patellar dislocation. After surgery, the knees were in good alignment. The ankle activity was normal. One day after surgery, the patient was unable to dorsiflex the ankle joints. The nervus peroneus communis was suspected to have been damaged by traction. The patient received an oral methylamine dispersible tablet and performed joint functional exercises. One week after surgery, the movements of the knee joint ranged from 5° to 90°. The x-ray image showed an appropriate prosthesis position (Fig. 3).
Figure 3.
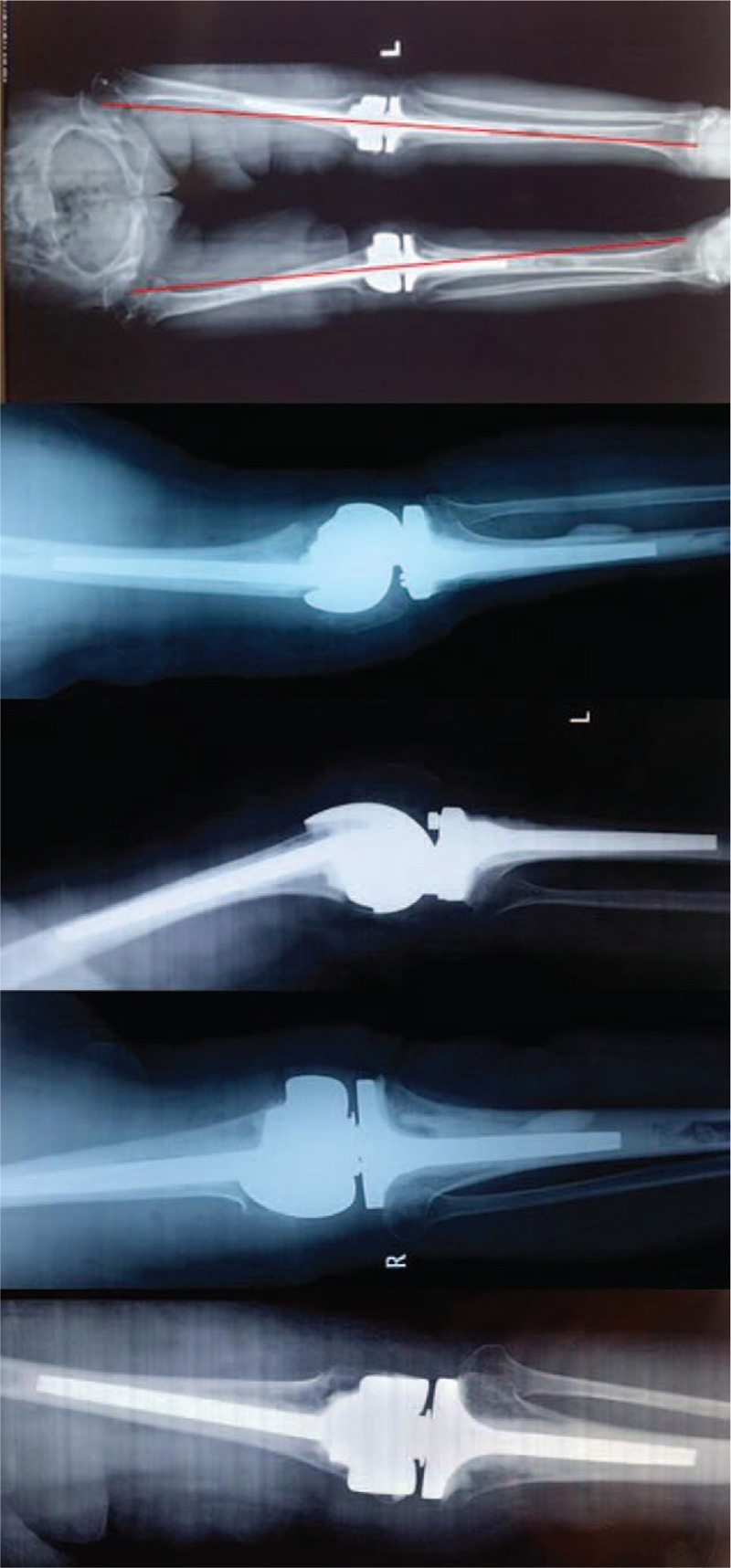
Postoperative x-ray radiograph showing the implanted prosthesis.
The only postoperative complication was an injury to the peroneal nerve, which led to loss of dorsiflexion at both ankle joints. However, the patient was able to walk with the use of walking aids. The patient was regularly followed up, and the ankle motion deficit was found to be completely recovered 3 months after surgery. At the follow-up 6 years after the operation, the knee extension reached 180°, knee flexion reached 125°, and the active joint function clearly improved (Fig. 4). The KSS had improved to 80 at the 2-year follow-up, 87 at the 4-year follow-up, and 90 at 6-year follow-up.
Figure 4.

Postoperative photograph after 18 months showing complete recovery of dorsiflexion.
3. Discussion
A primary TKA for a valgus knee deformity of >20° represents a challenge for orthopedic surgeons.[12] Herein, we present our experience with a 63-year-old woman with a severe valgus knee deformity angle >90°, which was classified as a severe deformity. During surgery, we released the lateral collateral ligament soft tissues and excised the medial and lateral meniscus and the remaining cruciate ligament. A rotating hinge knee instrument was used to correct the bone axis and stabilize the joint. The use of hinged implants in primary TKA should be restricted to patients with severe bony deformities or ligamentous instability, especially in elderly patients.[14] Constrained implants are frequently used for primary TKA in patients with moderate and severe genu valgum (>10°).[15] Constrained TKA is commonly performed to stabilize the joint and correct the bone axis in patients with severe ligamental instability, gross deformity, bone loss, and extreme deviation of the straight leg axis. In the present case, a rotating hinge knee prosthesis was selected.
A medial or lateral parapatellar approach can be used to perform TKA for valgus knee deformities. The lateral patellar incision is commonly used in mild-to-moderate valgus knee deformities to simply release the lateral structure. Given the position of the patella in the present case, the lateral parapatellar approach was not suitable to gain adequate exposure of the knee joint; thus, the medial parapatellar approach was used. Injury to the peroneal nerve is a common complication of TKA. The peroneal nerve injury is common when TKA is performed to correct valgus knee deformities, with an incidence of 2% to 3%.[16–19] We should pay more attention to the tension in the nerve, which could be alleviated by cutting off the fibular head, if necessary in osteotomy. Postoperatively, the knees were placed in 10° of flexion for 3 to 4 days to prevent stretching of the peroneal nerve, and active and passive range-of-motion exercises (range from 10° to 70°) were allowed.[20] In the present case, based on the preoperative evaluation of the surgical procedure, we believed that the peroneal nerve would not be transected, and thus we did not expose the peroneal nerve during the operation. However, postoperatively, the patient was unable to dorsiflex the ankle. Traction injury to the common peroneal nerve may result in the loss of ankle function. A traction injury to the common peroneal nerve was likely caused by straightening the knees. This complication could have been avoided by positioning of the knees in a flexed position after surgery and then gradually straightening the knees back out. Fortunately, the patient fully recovered 3 months after surgery.
Patellar dislocation or subluxation is a common finding in valgus knees. Patellar dislocation associated with congenital disorders appears to be classifiable into the following 3 types: conditions due to soft tissue laxity and increased joint laxity; conditions due to patellar hypoplasia and skeletal dysplasia of the femur and tibia; and conditions due to soft tissue fibrosis and contracture.[21] An abnormal patellar trajectory in the mild-to-moderate valgus knee can be corrected after knee arthroplasty.[22] In severe valgus conditions, the lateral patellar retinaculum, popliteus tendon, and the lateral portion of the gastrocnemius may require detachment to restore the anatomical axis of the limb. An anteromedial tibial tubercle transfer may be performed to correct patellar dislocation. In the present case, we corrected the severe abnormal patellar trajectory and tibial internal rotation by releasing the patellar lateral surface, vastus lateralis, and the intramuscular gap of the rectus femoris. A Z-shaped release of the biceps femoris was also performed. Since the patellar trajectory was still not completely corrected, we subsequently released the lateral collateral ligament by creating multiple needle punctures, incising the vastus lateralis, and extending it by malposed-suture to completely correct the patella trajectory.
In summary, in this rare case, we successfully performed TKA using a rotating hinge knee instrument for the treatment of a valgus deformity angle >90° associated with severe bony defects in the femur and tibia. The patellar dislocation was corrected without the use of anteromedial tibial tubercle transfer. Postoperatively, the patient experienced bilateral loss of ankle dorsiflexion due to a traction injury to the common peroneal nerve, which, however, was completely recovered in 3 months. Intraoperative exploration of the common peroneal nerve and postoperative flexed positioning of the knee joints could help prevent nerve injuries. However, since the hinge prosthesis was highly restricted, the lifetime of the prosthesis is a cause of concern. We still need to conduct long-term follow-ups of the patient.
Author contributions
Data curation: Jianbin Guo.
Funding acquisition: Yakang Wang, Yumin Zhang.
Investigation: Yumin Zhang.
Resources: Wei Song, Tao Ma.
Software: Yumin Zhang.
Supervision: Jianbin Guo, Guihua Cao, Yakang Wang, Wei-xia Yang.
Footnotes
Abbreviations: FTA = femorotibial angle, KSS = knee society score, TKA = total knee arthroplasty.
YW and WY have contributed equally to this work.
Consent for Publication: Informed written consent was obtained from the patient for publication of this case report.
This work was supported by the Shaanxi Science and Technology Research and Development Foundation of China (Number 2014K11-03-06-07) the Shaanxi Natural Science Foundation of China (Number 2019JQ-536).
None of the authors have conflicts of interest.
References
- [1].Elkus M, Ranawat CS, Rasquinha VJ, et al. Total knee arthroplasty for severe valgus deformity. Five to fourteen-year follow-up. J Bone Joint Surg Am 2004;86:2671–6. [DOI] [PubMed] [Google Scholar]
- [2].Ranawat AS, Ranawat CS, Elkus M, et al. Total knee arthroplasty for severe valgus deformity. J Bone Joint Surg Am 2005;87:271–84. [DOI] [PubMed] [Google Scholar]
- [3].Keblish PA. The lateral approach to the valgus knee. Surgical technique and analysis of 53 cases with over two-year follow-up evaluation. Clin Orthop Relat Res 1991;271:52–62. [PubMed] [Google Scholar]
- [4].Rossi R, Rosso F, Cottino U, et al. Total knee arthroplasty in the valgus knee. Int Orthop 2014;38:273–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Run-hua H, Xi-fu S, Fei HU, et al. Analysis of clinical effect of the treatment of patients with end-stage gonarthrosis combined with valgus knee deformity by total knee arthroplasty. J Clin Orthop 2017;3:310–3. 317. [Google Scholar]
- [6].Chaojie X, Shuaijie LV, Peijian T. Overview of total knee arthroplasty surgery on the patients with knee valgus deformity. Shanghai Med Pharma J 2015;7:57–62. [Google Scholar]
- [7].Yakang W, Jianbin G, Tao W, et al. Application of hinged knee prosthesis in total knee arthroplasty for patients with severe valgus knee. J Pract Orthop 2018;24:701–5. [Google Scholar]
- [8].Plutat J, Friesecke C, Klüber D. [Endo-Model hinged prosthesis--a model with a future? Experiences and outcome after 20 years use]. Orthopade 2000;29:S56–8. [DOI] [PubMed] [Google Scholar]
- [9].Sanguineti F, Mangano T, Formica M, et al. Total knee arthroplasty with rotating-hinge Endo-Model prosthesis: clinical results in complex primary and revision surgery. Arch Orthop Trauma Surg 2014;134:1601–7. [DOI] [PubMed] [Google Scholar]
- [10].Nieder E. Sled prosthesis, rotating knee and hinge prosthesis: St. Georg model and ENDO-model. Differential therapy in primary knee joint arthroplasty. Orthopade 1991;20:170–80. [PubMed] [Google Scholar]
- [11].Barrack RL. Evolution of the rotating hinge for complex total knee arthroplasty. Clin Orthop Relat Res 2001;292–9. [DOI] [PubMed] [Google Scholar]
- [12].Nikolopoulos D, Michos I, Safos G, et al. Current surgical strategies for total arthroplasty in valgus knee. World J Orthop 2015;6:469–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Insall JN, Dorr LD, Scott RD, et al. Rationale of the Knee Society clinical rating system. Clin Orthop Relat Res 1989;13–4. [PubMed] [Google Scholar]
- [14].Gehrke T, Kendoff D, Haasper C. The role of hinges in primary total knee replacement. Bone Joint J 2014;96-B:93–5. [DOI] [PubMed] [Google Scholar]
- [15].Rawal J, Devany AJ, Jeffery JA. Arthroplasty in the valgus knee: comparison and discussion of lateral vs medial parapatellar approaches and implant selection. Open Orthop J 2015;9:94–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Idusuyi OB, Morrey BF. Peroneal nerve palsy after total knee arthroplasty. Assessment of predisposing and prognostic factors. J Bone Joint Surg Am 1996;78:177–84. [DOI] [PubMed] [Google Scholar]
- [17].Asp JP, Rand JA. Peroneal nerve palsy after total knee arthroplasty. Clin Orthop Relat Res 1990;233–7. [PubMed] [Google Scholar]
- [18].Rose HA, Hood RW, Otis JC, et al. Peroneal-nerve palsy following total knee arthroplasty. A review of the hospital for special surgery experience. J Bone Joint Surg Am 1982;64:347–51. [PubMed] [Google Scholar]
- [19].Nercessian OA, Ugwonali OF, Park S. Peroneal nerve palsy after total knee arthroplasty. J Arthroplasty 2005;20:1068–73. [DOI] [PubMed] [Google Scholar]
- [20].Zhou X, Wang M, Liu C, et al. Total knee arthroplasty for severe valgus knee deformity. Chin Med J (Engl) 2014;127:1062–6. [PubMed] [Google Scholar]
- [21].Kitta Y, Niki Y, Udagawa K, et al. Severe valgus deformity of the knee with permanent patellar dislocation associated with melorheostosis: a case report and review of the literature. Knee 2014;21:589–93. [DOI] [PubMed] [Google Scholar]
- [22].Merkow RL, Soudry M, Insall JN. Patellar dislocation following total knee replacement. J Bone Joint Surg Am 1985;67:1321–7. [PubMed] [Google Scholar]


