Abstract
Background:
Patients requiring posterior lumbar surgery have increased annually. Incision infection after lumbar surgery has serious consequences for patients. However, data on the related factors of incision infection after lumbar surgery in diabetic patients are limited. Therefore, this study aimed to analyze diabetic patients who underwent lumbar surgery and to explore the risk factors of perioperative incision infection to provide a scientific basis for perioperative intervention of lumbar spine surgery and reduce risk of incision infection in such patients.
Methods:
We retrospectively reviewed data of diabetic patients who underwent posterior lumbar surgery from 2011 to 2016. A total of 523 diabetic patients undergoing posterior lumbar surgery were analyzed for the influence of various risk factors on postoperative incision infection. Univariate and multivariate logistic regression was performed. The test level was α=.05, and P < .05 was considered statistically significant.
Results:
In the past 6 years, among the 523 diabetic patients, the incidence of incision infection after posterior lumbar surgery was approximately 7.1%, of which the shallow incision infection rate was 4.2% and the deep incision infection rate was 2.9%. Incision infection of posterior lumbar surgery in diabetic patients is related to smoking, preoperative glycosylated hemoglobin A1c, postoperative albumin (Alb), surgical segment, operation time, and intraoperative blood loss, especially on postoperative fasting blood glucose, postoperative postprandial blood glucose, local subcutaneous fat thickness, and operation sequence (odds ratio >5.00). Meanwhile, sex, age, body mass index (BMI), preoperative Alb, and newly diagnosed diabetes were not highly correlated with incision infection after posterior lumbar surgery.
Conclusion:
Local subcutaneous fat thickness is a better indicator for predicting incision infection compared with BMI. In diabetic patients undergoing lumbar surgery, actively controlling blood glucose fluctuations, restoring normal diet early after surgery, and optimizing surgical procedures to reduce trauma and operative time can effectively reduce the risk of infection after posterior lumbar surgery.
Keywords: diabetes, incision infection, multifactor analysis, posterior lumbar surgery
1. Introduction
Posterior lumbar surgery is one of the effective and common surgical methods in lumbar surgery.[1] The surgical incision is deep and often requires internal fixation. Once an incision infection occurs, the patient's hospital stay is prolonged and patient's medical cost increased.[2] A multicenter study showed that the incidence of incision infection after posterior lumbar surgery was 3.0%.[3] Diabetes is an independent risk factor for incision infection after surgery, and incision infection in diabetic patients is 2 to 5 times that of non-diabetes.[4]
According to the 2016 Global Burden of Disease Study, the number of diabetic people is currently around 420 million, and there will be as many as 700 million by 2025.[5] The proportion of patients with degenerative lumbar disease seeking treatment is increasing, with an estimated 5% to 20% affected by diabetes.[6] However, data on the related factors of incision infection after lumbar surgery in diabetic patients are limited.[7,8] To determine the risk factors of perioperative incision infection in diabetic patients, intervention or early warning for its risk factors has important clinical significance for patients undergoing lumbar spine surgery.
Therefore, this study aimed to analyze diabetic patients who underwent lumbar surgery and to explore the risk factors of perioperative incision infection to provide a scientific basis for perioperative intervention of lumbar spine surgery and reduce the risk of incision infection in diabetic patients.
2. Materials and methods
2.1. Ethics statement
This is approved by Ethics Committee of Xiangya Hospital of Central South University (2017121127).
2.2. Patients
In this retrospective study, 523 diabetic patients underwent posterior lumbar surgery from January 2011 to December 2016 in Xiangya Hospital (295 men and 228 women), including 212 patients with lumbar spinal stenosis, 107 patients with lumbar disc herniation, 172 patients with lumbar spondylolisthesis, and 32 patients with lumbar vertebrae fracture. All the operation had been performed under the leadership of a surgeon with the title of deputy director or above. Randomized double-blind method was used to exclude the differences caused by the different surgeons. The study's exclusion criteria were as follows: patients younger than 18 years or older than 80 years; patients diagnosed with spinal tuberculosis, spinal tumors, intervertebral space infection; and patients with missing or incomplete data.
2.3. Diagnostic criteria for infected patients
There are 2 common types of posterior lumbar surgery infections. First, shallow surgical incision infection refers to involvement skin and subcutaneous tissue in the incision site. The infection occurs within 30 days after surgery and at least has one of the following two items: the shallow incision presents redness, swelling, heat, and pain, or purulent secretions; incision secretions are positive for bacterial culture. Second, deep incision infection refers to surgery-related and intra-incision deep soft tissue infection that occurs within 30 days after surgery without implant involvement and within 1 year after implantation and at least has 1 of the following 4 items: from the deep incision or puncture to the pus; naturally split or opened by the surgeon, with purulent discharge or fever ≥38°C, local pain, or tenderness; resurgical exploration, histopathological, or imaging examination revealed evidence of deep incision abscess or other infections; and positive colony culture.
2.4. Definition of diabetic patients and newly diagnosed diabetes
Adopting WHO 1999 Diabetes Diagnostic Criteria to distinguish patients with diabetes. Diabetic symptoms (typical symptoms include polydipsia, polyuria, and unexplained weight loss) can be diagnosed with one of the following 3: Random blood sugar >11.1 mmol/L; fasting blood glucose (FBG) ≥7.0 mmol/L; 2 hours after glucose loading, blood sugar >11.1 mmol/L. If there are no diabetic symptoms, the blood sugar should be determined repeatedly on another day to make a definite diagnosis. In this study, diabetic patients refer to those who have been diagnosed as having diabetes in the past, newly diagnosed diabetic patients refer to those who have not been diagnosed as having diabetes before admission, and the results of post-admission tests indicate diabetes mellitus.
2.5. Definitions of smoking
People who smoke continuously or accumulatively for ≥6 months in their lifetime were defined as smokers by WHO in 1997.
2.6. Evaluation indicators
A retrospective study was performed to record postoperative infections and noninfected patients, and were divided into infected and noninfected groups. Sex, age, body mass index (BMI), smoking, newly diagnosed diabetes, preoperative glycosylated hemoglobin A1c (HbA1c), preoperative albumin (Alb), postoperative FBG, postoperative postprandial blood glucose (PBG), postoperative Alb, surgical segment, operation time, intraoperative blood loss, local subcutaneous fat thickness, and surgical sequence were collected for all patients. Finally, all data were analyzed using statistical methods.
During data collection, the patient's preoperative magnetic resonance T1-weighted imaging was directly retrieved by ICPACS image processing software (DHC, China), and the subcutaneous fat thickness of T12-L5 vertebral body level was measured. The average value represented the subcutaneous fat thickness (Fig. 1). FBG and PBG values were averaged for all dates 3 days after surgery.
Figure 1.

Measurement of subcutaneous fat thickness. (A) Female, 56 years’ old, BMI = 21.16 kg/m2, diagnosis: lumbar disc herniation, mean subcutaneous fat thickness = 1.38 cm. (B) Male, 31 years’ old, BMI = 41.85 kg/m2, diagnosis: lumbar disc herniation. The average thickness of subcutaneous fat = 5.56 cm.
2.7. Statistical analysis
Statistical analysis was performed using SPSS 22.0 software (SPSS Inc, Chicago, IL). All indicators were counted. One-way analysis of variance was used to analyze the relationship between each evaluation index and incision infection after posterior lumbar surgery. Multivariate logistic regression analysis was performed to analyze the independent risk factors of incision infection, and statistically significant indices of univariate analysis were included in independent variables of multivariate analysis. The test level was α = 0.05, and P < .05 was considered statistically significant.
3. Results
Of the 523 diabetic patients, 486 had no incision infection, and 37 had incision infection. Among them, 22 had shallow incision infection and 15 patients had deep incision infection. The incidence of shallow incision infection was 4.2%, the incidence of deep incision infection was 2.9%, and the overall infection rate was 7.1%.
3.1. Single-factor analysis of incision infection after lumbar spine surgery
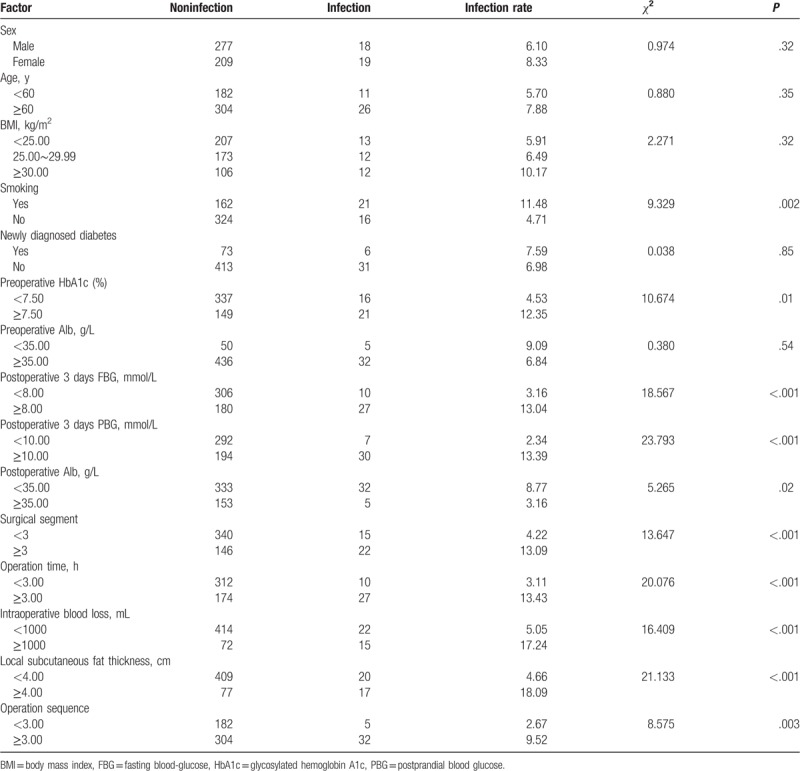
Univariate analysis by χ2 test showed no significant differences in sex, age, BMI, newly diagnosed diabetes, and preoperative Alb between the infected group and noninfected group (P > .05). Smoking, preoperative HbA1c, postoperative FBG, postoperative PBG, postoperative Alb, surgical segment, operation time, intraoperative blood loss, local subcutaneous fat thickness, and operation sequence were statistically significant (P < .05, Table 1).
Table 1.
Univariate analysis of observation index and incision infection after lumbar spine surgery in diabetic patients.
3.2. Multifactor analysis of incision infection after lumbar surgery in diabetic patients
Further multivariate logistic regression analysis showed that 10 risk factors were closely related to incision infection after lumbar surgery (P < .05, Table 2), namely, smoking (odds ratio [OR] = 3.830, P = .021), preoperative HbA1c (OR = 4.629, P = .01), postoperative FBG (OR = 5.710, P = .001), postoperative PBG (OR = 7.736, P = .002), postoperative Alb (OR = 3.032, P = .017), surgical segment (OR = 4.258, P = .004), operation time (OR = 4.869, P = .001), intraoperative blood loss (OR = 3.049, P = .011), local subcutaneous fat thickness >4.00 cm (OR = 5.562, P = .003), and surgical sequence (OR = 5.361, P = .012). Among them, the OR values of postoperative FBG, postoperative PBG, local subcutaneous fat thickness, and surgical sequence were as high as ≥5.
Table 2.
Multivariate analysis of incision infection after lumbar surgery in diabetic patients.

3.3. Effect of subcutaneous fat thickness and operation sequence on incision infection after posterior lumbar surgery in diabetic patients
As shown in Figure 2, when the subcutaneous fat thickness exceeds 4 cm, the incidence of incision infection in lumbar patients after lumbar surgery is sharply increased. For every 1-cm fat thickness, the incision infection rate is increased by 9%. Figure 3 shows that lumbar surgery as the third operation was increased by about 2 to 3 times than the first 3 operations. The fourth operation was increased by about 6 times than the first 2 operations.
Figure 2.
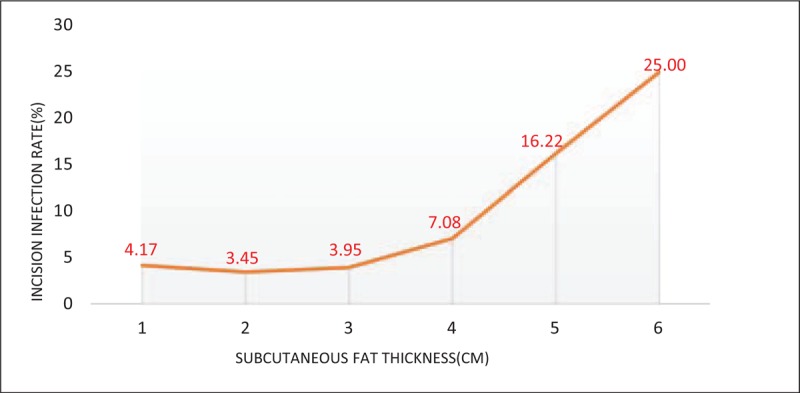
Relationship between subcutaneous fat thickness and incision infection after posterior lumbar surgery in diabetic patients. When the subcutaneous fat thickness exceeds 4.00 cm, the incidence of incision infection after lumbar spine surgery in diabetic patients is sharply increased, for each 1 cm thick fat, the incision infection rate is increased by 9%.
Figure 3.

Relationship between operation sequence and incision infection after posterior lumbar surgery in diabetic patients. Lumbar surgery as the third operation was increased by about 2 to 3 times than the first 2 operations. The fourth operation was increased by about 6 times than the first 2 operations.
4. Discussion
Diabetes itself is an independent risk factor for incision infection. This study shows that in the past 6 years, in our spine surgery department, the overall infection rate of lumbar spine in diabetic patients is 7.1%. Compared with the previous study, the infection rate in lumbar surgery at 4.8% to 7.2% in diabetic patients is consistent.[3,4]
The difference in infection rate in different studies may be affected by the difference in the skill level of the operator, operating room conditions, and diagnosis of postoperative incision infection. However, Li et al[9] showed that specialist hip unit surgeons did not have any significant influence on reducing rates of surgical site infection.
We found that BMI was not a risk factor for incision infection after posterior lumbar surgery in diabetic patients, which is contrary to results of previous studies which considered BMI to be an independent risk factor for incision infection after lumbar surgery.[10,11] Furthermore, Lee et al[12] showed that the local fat thickness (skin to spine process distance) >5 cm in patients with a surgical site infection increased by 4 times. This retrospective study further found that subcutaneous fat thickness in univariate and multivariate analyses showed statistical significance. And Liu et al[13] showed that the waist-to-hip ratio (WHR) was the obesity index that most strongly correlated with insulin secretion at each phase among obese patients. WHR may be a good predictor for insulin secretion function of β-cell. The reason may be that the effect of BMI on incision infection may be related to the prediction of the thickness of the subcutaneous fat at the surgical site. Moreover, BMI did not consider weight distribution, especially in diabetic patients, central obesity accounted for 45.4%,[14] and the use of BMI alone to predict the risk of incision infection after lumbar surgery in diabetic patients was biased. The use of local subcutaneous fat thickness to predict incision infection after lumbar surgery in diabetic patients is a better indicator than BMI.
Among the blood glucose-related indicators, preoperative HbA1c, postoperative FBG, and postoperative PBG were risk factors for incision infection after lumbar surgery in diabetic patients. On the one hand, Wu et al[15] showed that diabetic patients with poor blood sugar management often have microvascular disease, which caused local insufficiency of blood supply. On the other hand, hyperglycemia increases plasma osmotic pressure, inhibits the phagocytic ability of white blood cells, and reduces the body's anti-infective ability.[16] Hence, the incision healing rate slows down and the probability of infection increases. Cancienne et al[7] showed that HbA1c ≥7.50% leads to a 2.9-fold increase in the risk of incision infection after surgery in diabetic patients. Han et al[17] also considered that HbA1c ≤8% will reduce the incidence of incision infection after total knee arthroplasty in diabetic patients. The 2015 AAGBI perioperative management of diabetes patients pointed out that the recommended perioperative blood glucose of 6 to 10 mmol/L will obviously reduce the risk of perioperative cardiovascular and incision infections.[18]
In this study, the incidence of incision infection was slightly higher in newly diagnosed diabetes than in previously diagnosed diabetes, but the difference was not statistically significant. Anxiety is more common in newly diagnosed diabetes[19] and newly diagnosed diabetes lacks diabetes diet management experience,[20] both of this making control of perioperative blood glucose more difficult than previously diagnosed diabetic patients. However, considering the relatively mild complications of diabetes in newly diagnosed diabetic patients, the effect of incision infection may be offset. Therefore, whether newly diagnosed diabetes is a risk factor for incision infection after lumbar surgery in diabetic patients still requires in-depth investigation.
For perioperative management of diabetic patients, preoperative FBG should be controlled at 6 to 8 mmol/L for elective surgery, and PBG should be controlled between 7 mmol/L and 10 mmol/L 2 hours after meal. For diabetes diet education, there should be rational use of diabetes drugs. If necessary, patients should use insulin to control blood sugar instead of oral medication.
The incidence of incision infection in the third or later operation is 3 to 7 times that of the previous 2 operations. Xu[21] believes that the more the operating table is placed at the back of the operating room, the more bacteria are bring about by the moving staff and exchange of supplies in the operating room, increasing the chance of infection after surgery at 2 to 3 times. On the contrary, Sarin et al[22] found that the longer the fasting period, the greater the effect of insulin resistance caused by fasting on postoperative blood glucose level. Therefore, scheduling surgery of diabetic patients as the first 2 operations of the day is an effective way to reduce the incision infection after lumbar surgery.
Smoking is a risk factor for incision infection after lumbar surgery of diabetic patients. Sorensen et al[23] also showed an increased risk of incision infection in smokers, and a strict cessation of smoking for 4 weeks before surgery reduced the risk of incision infection, as nicotine and tar in cigarettes affect vasoconstriction. This is based on the presence of microvascular lesions in long-term diabetic patients, which further aggravates local blood circulation disorders around the incision, resulting in prolonged incision healing and increased risk of infection. For patients with long-term smoking history, our department routinely conducts health education, preoperative strict smoking cessation or nicotine replacement therapy for 4 weeks, postoperative routine nebulization, promotion of sputum excretion, and other perioperative interventions to reduce the risk of postoperative incision infection in diabetic patients.
Postoperative nutritional status in diabetic patients is a risk factor for incision infection. Tominaga et al[24] reported that preoperative hemoglobin >110 g/L and total platelet >60 g/L is essential to reduce postoperative incision infection. In this study, preoperative Alb level was not associated with incision infection, but postoperative Alb. The possible reason was that postoperative Alb level was the real factor that affects incision infection, while preoperative Alb level represented preoperative nutritional status. However, its correlation with incision infection is severely affected by the loss of nutrients caused by intraoperative bleeding, which makes it impossible to accurately represent the nutritional level of postoperative patients; thus, it cannot stably predict the incidence of incision infection. Therefore, postoperative patients with Alb <35 g/L are supplemented with Alb, and early interventions to strengthen nutrition status help reduce the risk of incision infection.
Surgical segment, operation time, and intraoperative blood loss were risk factors for postoperative incision infection in diabetic patients, which is consistent with previous studies.[25,26] The operation time is >3 hours, the tissue exposure time is long, the incision surface of the surgical incision is in contact with the air for a long time, and the duration of pulling the compressed tissue during the operation is long, which increases the possibility of tissue ischemic necrosis and mechanical damage, leading to risk of incision infection. The greater the amount of intraoperative blood loss, the greater the loss of nutrients, and the lower the body's resistance, the weaker the body's ability to heal the incision. Therefore, according to the specific circumstances of the patient, it is generally recommended to reduce the surgical segment as much as possible, select the surgical method with less trauma, carefully read imaging results before surgery, pay attention to the anatomical variation, be proficient of the surgical procedure, shorten the operation time, simplify the operation, and reduce the continuous traction time. Thorough bleeding assessment, combined with hemostasis if necessary, can help reduce the risk of postoperative incision infection in diabetic patients.
In summary, diabetic patients are prone to incision infection after lumbar surgery. Use of local subcutaneous fat thickness to predict incision infection is superior to BMI. For diabetic patients requiring posterior lumbar surgery, preoperative risk factors should be assessed. Patients with more risk factors should be given high attention and reasonable intervention for risk factors. In addition to actively controlling fluctuations in blood sugar levels, returning to normal diet early after surgery, and optimizing surgical procedures to reduce trauma and operative time can effectively reduce the risk of infection after posterior lumbar surgery in diabetic patients.
5. Study limitations
The limitation of this study was an insufficient case of incision infection, which could have led to inadequate analysis of some factors and to other risk factors not being identified. Therefore, a larger sample is needed in future studies to validate these results.
Author contributions
Data curation: Wang Peng.
Formal analysis: Yan Liang.
Methodology: Miao Li.
Project administration: Jian-Huang Wu.
Resources: Dong-Sheng Li, Kai-Hui Du.
Writing – original draft: Wang Peng.
Writing – review & editing: Wang Peng, Yan Liang, Tao Lu.
Jian-Huang Wu orcid: 0000-0001-6604-8128.
Footnotes
Abbreviations: Alb = albumin, BMI = body mass index, CI = confidence interval, FBG = fasting blood-glucose, HbA1c = glycosylated hemoglobin A1c, MRI = magnetic resonance imaging, OR = odds ratio, PBG = postprandial blood glucose.
The author reports no conflicts of interest.
The work has not already been published and has not been submitted simultaneously to any other journal. We agree to transfer the copyrights for this journal if accepted for publications.
This work was supported by the National Natural Science Foundation of China (81472073).
References
- [1].Wang XY, Hu ZH, Hu JZ, et al. Surgical treatment for lumbar discogenic low back pain. J Central South Univ (Med Ed) 2006;31:607–12. [PubMed] [Google Scholar]
- [2].Lai Q, Song Q, Guo R, et al. Risk factors for acute surgical site infections after lumbar surgery: a retrospective study. J Orthop Surg Res 2017;12: [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Wang T, Wang H, Yang DL, et al. Factors predicting surgical site infection after posterior lumbar surgery: a multicenter retrospective study. Medicine (Baltimore) 2017;96:e6042. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- [4].Wang J, Hao SX, Liu XH, et al. Analysis of risk factors for early infection after posterior lumbar surgery. J Aerospace Med 2017;1330–2. [Google Scholar]
- [5].The L. Untangling the complications of diabetes. Lancet 2018;391:2389. [DOI] [PubMed] [Google Scholar]
- [6].Kim CH, Chung CK, Shin S, et al. The relationship between diabetes and the reoperation rate after lumbar spinal surgery: a nationwide cohort study. Spine J 2015;15:866–74. [DOI] [PubMed] [Google Scholar]
- [7].Cancienne JM, Werner BC, Chen DQ, et al. Perioperative hemoglobin A1c as a predictor of deep infection following single-level lumbar decompression in patients with diabetes. Spine J 2017;17:1100–5. [DOI] [PubMed] [Google Scholar]
- [8].Guzman JZ, Iatridis JC, Skovrlj B, et al. Outcomes and complications of diabetes mellitus on patients undergoing degenerative lumbar spine surgery. Spine (Phila Pa 1976) 2014;39:1596–604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Li X, Li H, Bu J, et al. Do specialist hip unit surgeons have any significant influence on reducing rates of surgical site infection? Int Orthop 2015;39:207–8. [DOI] [PubMed] [Google Scholar]
- [10].Pereira BJA, de Holanda CVM, Ribeiro CAA, et al. Impact of body mass index in spinal surgery for degenerative lumbar spine disease. Clin Neurol Neurosur 2014;127:112–5. [DOI] [PubMed] [Google Scholar]
- [11].Durand WM, Eltorai AEM, Depasse JM, et al. Risk factors for unplanned reoperation within 30 days following elective posterior lumbar spinal fusion. Global Spine J 2017;8:388–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Lee JJ, Odeh KI, Holcombe SA, et al. Fat thickness as a risk factor for infection in lumbar spine surgery. Orthopedics 2016;39:e1124–8. [DOI] [PubMed] [Google Scholar]
- [13].Liu MM, Liu QJ, Wen J, et al. Waist-to-hip ratio is the most relevant obesity index at each phase of insulin secretion among obese patients. J Diabetes Complications 2018;32:670–6. [DOI] [PubMed] [Google Scholar]
- [14].Zhou F, Wang XL, Dou JT. A new strategy for obesity management in patients with type 2 diabetes from the 2017 edition of the ADA guidelines. Drug Evaluation 2018;10–3. [Google Scholar]
- [15].Wu D, Wu C, Zhong Y. The association between paraoxonase 1 activity and the susceptibilities of diabetes mellitus, diabetic macroangiopathy and diabetic microangiopathy. J Cell Mol Med 2018;22:4283–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Dryden M, Baguneid M, Eckmann C, et al. Pathophysiology and burden of infection in patients with diabetes mellitus and peripheral vascular disease: focus on skin and soft-tissue infections. Clin Microbiol Infect 2015;21:27–32. [DOI] [PubMed] [Google Scholar]
- [17].Han H, Kang S. Relations between long-term glycemic control and postoperative wound and infectious complications after total knee arthroplasty in type 2 diabetics. Clin Orthop Surg 2013;5:118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Barker P, Creasey PE, Dhatariya K, et al. Peri-operative management of the surgical patient with diabetes 2015. Anaesthesia 2015;70:1427–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Chai S, Yao B, Xu L, et al. The effect of diabetes self-management education on psychological status and blood glucose in newly diagnosed patients with diabetes type 2. Patient Educ Couns 2018;101:1427–32. [DOI] [PubMed] [Google Scholar]
- [20].Li X, Zhou Q, Zou F, et al. Effectiveness of systematic self-management education on blood sugar level of patients in the community with type 2 diabetes. J Central South Univ (Med Ed) 2012;37:355–8. [DOI] [PubMed] [Google Scholar]
- [21].Xu JJ. Correlation between operation sequence and incision infection after lumbar degenerative disease. Nanchang University Master's Thesis Electronic Journal 2017. [Google Scholar]
- [22].Sarin A, Chen L, Wick EC. Enhanced recovery after surgery-Preoperative fasting and glucose loading—a review. J Surg Oncol 2017;116:578–82. [DOI] [PubMed] [Google Scholar]
- [23].Sorensen LT. Wound healing and infection in surgery. The clinical impact of smoking and smoking cessation: a systematic review and meta-analysis. Arch Surg 2012;147:373–83. [DOI] [PubMed] [Google Scholar]
- [24].Tominaga H, Setoguchi T, Ishidou Y, et al. Risk factors for surgical site infection and urinary tract infection after spine surgery. Eur Spine J 2016;25:3908–15. [DOI] [PubMed] [Google Scholar]
- [25].Ogihara S, Yamazaki T, Maruyama T, et al. Prospective multicenter surveillance and risk factor analysis of deep surgical site infection after posterior thoracic and/or lumbar spinal surgery in adults. J Orthop Sci 2015;20:71–7. [DOI] [PubMed] [Google Scholar]
- [26].Meng F, Cao J, Meng X. Risk factors for surgical site infections following spinal surgery. J Clin Neurosci 2015;22:1862–6. [DOI] [PubMed] [Google Scholar]


