Abstract
Knee osteoarthritis is a degenerative disease occurring in elderly people worldwide. For severe knee osteoarthritis, total knee replacement is the final treatment option. Traditional Chinese medicine (TCM) is popular in Taiwan and has been shown to exert therapeutic effects on knee osteoarthritis. We investigated the long-term clinical effects of TCM for reducing the need for total knee replacement risk in patients with knee osteoarthritis.
We used the National Health Insurance Research Database to conduct a retrospective study of patients with knee osteoarthritis between 1997 and 2003 in Taiwan. Data from the date of diagnosis of knee osteoarthritis to total knee replacement were assessed using the Cox regression proportional hazards model, and the Kaplan–Meier survival curve was used to determine the association between total knee replacement risk and TCM use.
A total of 34,231 patients with knee osteoarthritis, who were diagnosed by orthopedic or rehabilitation physicians between 1997 and 2003 were included. Patients were categorized into 2 groups: 26,257 (76.7%) were TCM users and 7974 (23.3%) were TCM non-users. The mean follow-up period was 9.26 years. Multivariate regression demonstrated that using TCM may decrease the need for total knee replacement in patients with knee osteoarthritis (adjusted hazards ratio [aHR] = 0.69, 95% confidence interval [95% CI]: 0.64–0.77) compared with TCM non-users. A relationship between longer TCM use and reduced total knee replacement use was observed, especially in patients who used TCM for ≥120 days (aHR = 0.49, 95% CI: 0.42–0.56).
The results of this study suggested that TCM is associated with a reduced risk of total knee replacement in patients with knee osteoarthritis, with enhanced benefits from longer durations of TCM use.
Keywords: acupuncture, Chinese herbal medicine, knee osteoarthritis, traditional Chinese medicine
1. Introduction
Knee osteoarthritis is a common disease in the elderly population worldwide, and it is the single most common cause of lower limb disability in adults over 50 years of age.[1] Typically, patients with knee osteoarthritis develop symptoms and signs of bilateral knee pain and stiffness, joint swelling and deformation, and quadriceps weakness and wasting.[2] As the disease progresses, walking and standing might become increasingly difficult, and persistent pain at night will also impede sleep.[3] Nonsurgical treatment of patients with knee osteoarthritis includes a variety of interventions led by physical therapists: exercise, changes in activity, weight loss for obese persons, and use of walking canes, analgesics, and nonsteroidal anti-inflammatory drugs (NSAIDs) and glucosamine.[4–6] However, total knee replacement is still the final treatment option for severe pain and poor response to nonoperative therapies, and its application is rising rapidly.[7] Unfortunately, patients who report minor or no improvement of their symptoms and pain after total knee arthroplasty (TKA) remains high, ranging from 5% to 40%.[8]
A large number of patients with knee osteoarthritis received traditional Chinese medicine (TCM) treatment,[9] and a systematic review of randomized controlled trials showed that TCM could significantly improve visual analog scale for pain (VAS) scores and physical performance.[10] Moreover, several clinical trials reported the efficacy of TCM in pain relief; restoration of function, and mobility.[11–13] However, there is still no large-scale study evaluating the long-term efficacy of TCM on knee osteoarthritis. The aim of this study was to determine the long-term clinical effects of TCM on reducing the need for total knee replacement in patients with knee osteoarthritis.
2. Methods
2.1. Data source
The National Health Insurance Research Database (NHIRD) is a collection of medical information for more than 99% of the population in Taiwan. The national health insurance administration of Taiwan government recorded medical information including diagnoses, drugs, surgery from outpatient and inpatient services, and collected patient insurance information such as coverage, location, age, and gender.[14] NHIRD was divided into several smaller databases, each of them containing randomly sampled data of 1 million people according to different years, as well as over a long-term observation period from January 1996 to the end of December 2012. In the present study, we used one of the sub-databases, the Longitudinal Health Insurance Database 2005, which had a demographic distribution similar to NHIRD. The National health insurance administration used the International Classification of Diseases, 9th revision, Clinical Modification (ICD-9-CM)[14,15] as the primary diagnostic record type, and included all outpatient and inpatient diagnoses in the NHIRD. NHIRD recorded the amount insured in New Taiwan dollars (NT$), and the exchange rate to US dollar was about 31.1. Several studies have been performed so far to verify if the use of NHIRD for a long time to trace the efficacy of TCM is feasible.[16,17]
2.2. Study cohort identification
We selected patients with knee osteoarthritis from all the 1 million people in LHID 2005[18] as shown in the flow chart in Figure 1. We included knee osteoarthritis diagnosis by orthopedic or rehabilitation physicians (ICD-9-CM: 715.16, 715.26, 715.36) between January 1, 1997 and December 31, 2003 (n = 36,016). Knee osteoarthritis is a slowly degenerative disease that lasts for many years in most patients. When patients were in different disease stage, the risk of undergoing knee replacement surgery was also different. To ensure that all patients in the cohort have a similar initial state, we only included patients newly diagnosed after 1997. Therefore, we excluded patients who were diagnosed before 1997 (n = 1,702), with uncompleted demographic data (n = 24), and who had undergone knee replacement surgery within 1 year after knee osteoarthritis diagnosis (n = 59). Finally, 34,231 patients with newly diagnosed knee osteoarthritis were included in our study.
Figure 1.
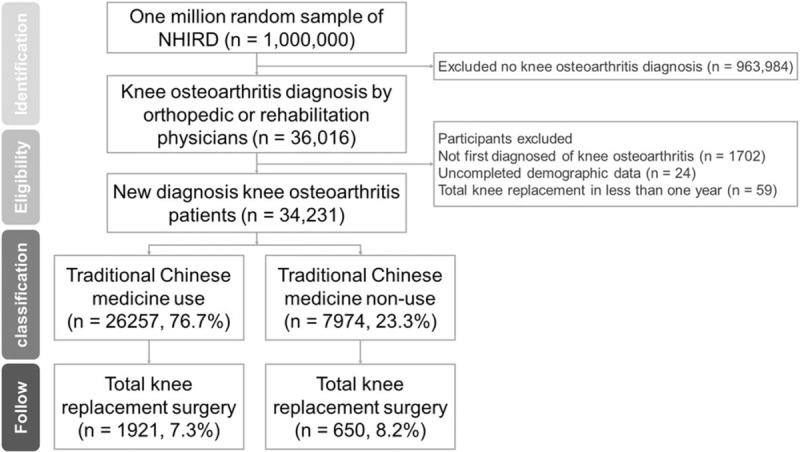
Recruitment flow chart of patients with knee osteoarthritis with medical treatment for total knee replacement. We enrolled 34,231 patients who were divided into 2 groups: TCM treatment group (26,257 patients, 76.7%) and non-TCM treatment group (7974 patients, 23.3%). In the TCM group, 1921 (7.3%) accepted total knee replacement surgery, while 650 (8.2%) from the non-TCM group received the surgery. TCM = Traditional Chinese medicine.
2.3. Traditional Chinese medicine
We used the following steps to distinguish between patients who used or did not use the TCM treatment.[19] First, we acquired all outpatient medical data of patients with knee osteoarthritis from the sub-dataset of NHIRD “Ambulatory care expenditures by visits” files, which contained the date of medical treatment, medical institutions, visiting physicians, and number of prescribed days between 1997 and 2012. Second, we excluded all outpatient records before knee osteoarthritis diagnosis or later than total knee replacement surgery. Third, patients who have received TCM treatment were assigned to the TCM group, and the rest were allocated to the non-TCM group. In the present study, TCM treatment including Chinese herbal medicine and acupuncture. Fourth, we linked the outpatient data to the “Details of ambulatory care orders” files, which contained detailed treatment information such as the names, frequency, and dosage of drugs, and the acupuncture treatment times (procedure code B41-B46). Finally, we calculated the cumulative duration of TCM treatment and times of acupuncture for each patient in the TCM groups. There were 26,257 (76.7%) TCM user and 7974 (23.3%) TCM non-user groups patients in the final analysis. To understand the time-response relationship of TCM treatment, we classified TCM users into 3 groups according to the duration of TCM treatment with sensitivity analysis: less than 1 month (<30 days), more than 1 season (≥120 days), as well as between a month and a quarter (30–120 days). Moreover, 3 different groups were defined based on the number of acupuncture treatments: <6 times, 6 to 12 times, and ≥12 times. To determine the cut point, we analyzed the frequency distribution of patients with knee osteoarthritis receiving TCM and acupuncture treatment and calculated the 33 and 66 percentiles. When the patient received the acupuncture for less than 6 times, we might consider that the patient's willingness to accept TCM is lower, according to the previous study.[17] We also analyzed the effect of different TCM formulae, which has been reported to relieve the symptoms of knee osteoarthritis.[20]
2.4. Study outcomes
The primary outcome of this study was the total knee replacement risk of the patients with knee osteoarthritis. Since there were no pain scores and radiographic reports in the NHIRD, we used TKA as an indicator of extreme worsening knee osteoarthritis and nonresponsiveness to nonsurgical therapy.[21] We collected all medical data from the initial knee osteoarthritis diagnosis until December 31, 2012, and selected the ICD9-procedure code 81.54 (total knee replacement). The follow-up period began with the diagnosis of knee osteoarthritis and ended with the first total knee replacement; the patients who did not undergo surgery were followed up until the end of December 31, 2012.
2.5. Covariate assessment
We adjusted the participants’ demographic data, including the age at diagnosis (<60, 60–70, 70–80, and ≥ 80 years) and sex. Because the area of residence might affect medical resources and medical behavior, we divided the living area into 4 degrees based on the urbanization level: very high, high, moderate, and low. Since the NHIRD did not include the patients’ salary information, we used the insured amount by the annual income calculation as an indicator of annual income.[22] We also adjusted the comorbidities, which might influence the progress of osteoarthritis, including diabetes mellitus (ICD-9-CM: 249 and 250), chronic kidney disease (ICD-9-CM:585, 586, and 588), cerebral vascular accident (ICD-9-CM:430–438), hypertension (ICD-9-CM:401–405), and rheumatoid arthritis (ICD-9-CM:714). To estimate the severity of the knee osteoarthritis, we used the accumulation dosage of NSAIDs use.
2.6. Statistical analysis
We used the Kaplan–Meier survival curve and log-rank tests to examine the differences in the risk of total knee replacement. We calculated the hazard ratio (HR) and the accompanying 95% confidence intervals (95% CI) by Cox proportional regression models, and adjusted possible covariates that were mentioned above. We used 2-tail tests, and significance level was set at P-values < .05. Logistic regression was conducted to compare the distributed differences of demographic characteristics and comorbidities between TCM and non-TCM groups. We compared the HRs between TCM and non-TCM users, the different groups of patients with increasing use of TCM, and the cumulative times of acupuncture. Data were organized and analyzed using the statistical software SAS (version 9.4; SAS Institute Inc, Cary, NC), while the MedCalc software (version 16.8.4) was applied to draw the survival curve.
3. Results
We included 34,231 patients newly diagnosed with knee osteoarthritis, of whom 26,257 (76.7%) were TCM users and 7,974 (23.3%) were TCM non-users. The mean follow-up period was 9.3 years with a standard deviation (SD) of 2.71 years. At the end of the study, a total of 1921 (7.3%) patients in the TCM user group underwent total replacement surgery. Furthermore, 650 (8.2%) of the patients in the non-TCM group received surgery, as shown in Figure 1.
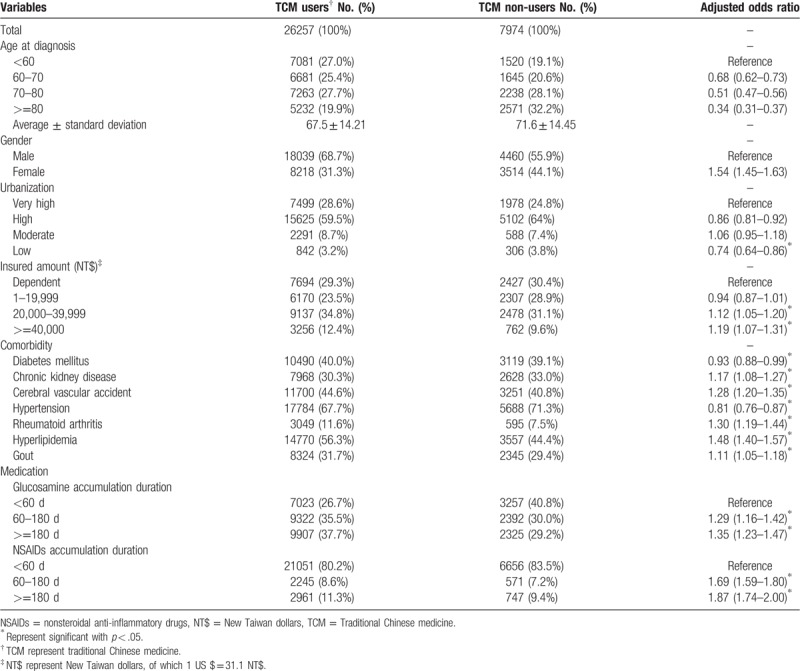
Table 1 summarizes the results of the comparisons of the demographic characteristics and comorbidities between TCM and non-TCM groups. The mean age at diagnosis was 67.5 years (SD 14.21 years) in the TCM group, which was younger than the non-TCM group (71.6 ± 14.45 years). The tendency to accept TCM treatment decreased with age, and the adjusted odds ratio (aOR) and 95% CI in 60 to 70 years, 70 to 80 years, and ≥80 years were 0.68 (0.62–0.73), 0.51 (0.47–0.56), and 0.34 (0.31–0.37), respectively. Women had a higher tendency to use TCM compared with men, and the aOR (95% CI) was 1.54 (1.45–1.63) compared with men. The willingness to use TCM was higher in the upper-income groups, with an aOR (95% CI) of 1.12 (1.05–1.20) in patients with an insured amount of 20,000 to 39,999 NT$, and 1.19 (1.07–1.31) in those insured at more than 40,000 NT$. Comorbidities also influenced the application of TCM treatment, the patients with diabetes mellitus, chronic kidney disease, cerebral vascular accident, rheumatoid arthritis, hyperlipidemia, and gout displayed a higher tendency to use TCM. Besides, NSAID and glucosamine treatment might increase the use of TCM, the longer the cumulative use time, the stronger the tendency to use.
Table 1.
Demographic characteristics and comorbidity disease of the knee osteoarthritis cohort.
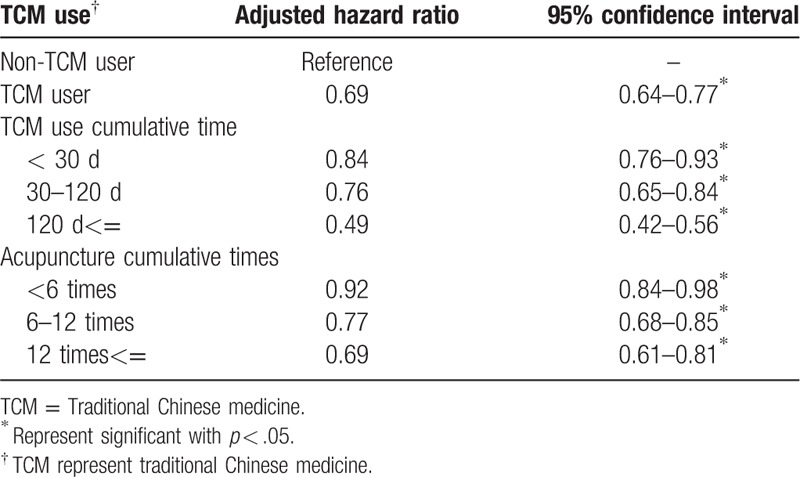
The multivariable Cox model measured the HRs (95% CI) of TCM treatment for total knee replacement in the knee osteoarthritis cohort as shown in Table 2. Compared with patients with knee osteoarthritis who did not receive TCM, a lower adjusted HR (aHR; 0.69 [0.64–0.77]), after adjusted demographic factors and comorbidities, was observed in the TCM users. The aHR decreased with the increase of TCM cumulative times. Indeed, the aHR (95% CI) with TCM use of less than 30 days, 30 to 120 days, and more than 120 days was 0.84 (0.76–0.93), 0.76 (0.65–0.84), and 0.49 (0.42–0.56), respectively. A similar trend appeared in patients treated with acupuncture. The more acupuncture treatment times, the lower was the risk of knee joint replacement, and the aHR (95% CI) was 0.92 (0.84–0.98), 0.77 (0.68–0.85), and 0.69 (0.61–0.81) in acupuncture treatment of less than 6 times, 6 to 12 times, and more than 12 times, respectively, as showed in Table 3.
Table 2.
Hazard ratios of total knee replacement risk in different demographic factor and comorbidity disease, analyzed by multivariable cox proportional hazards regression model and 95% confidence intervals.
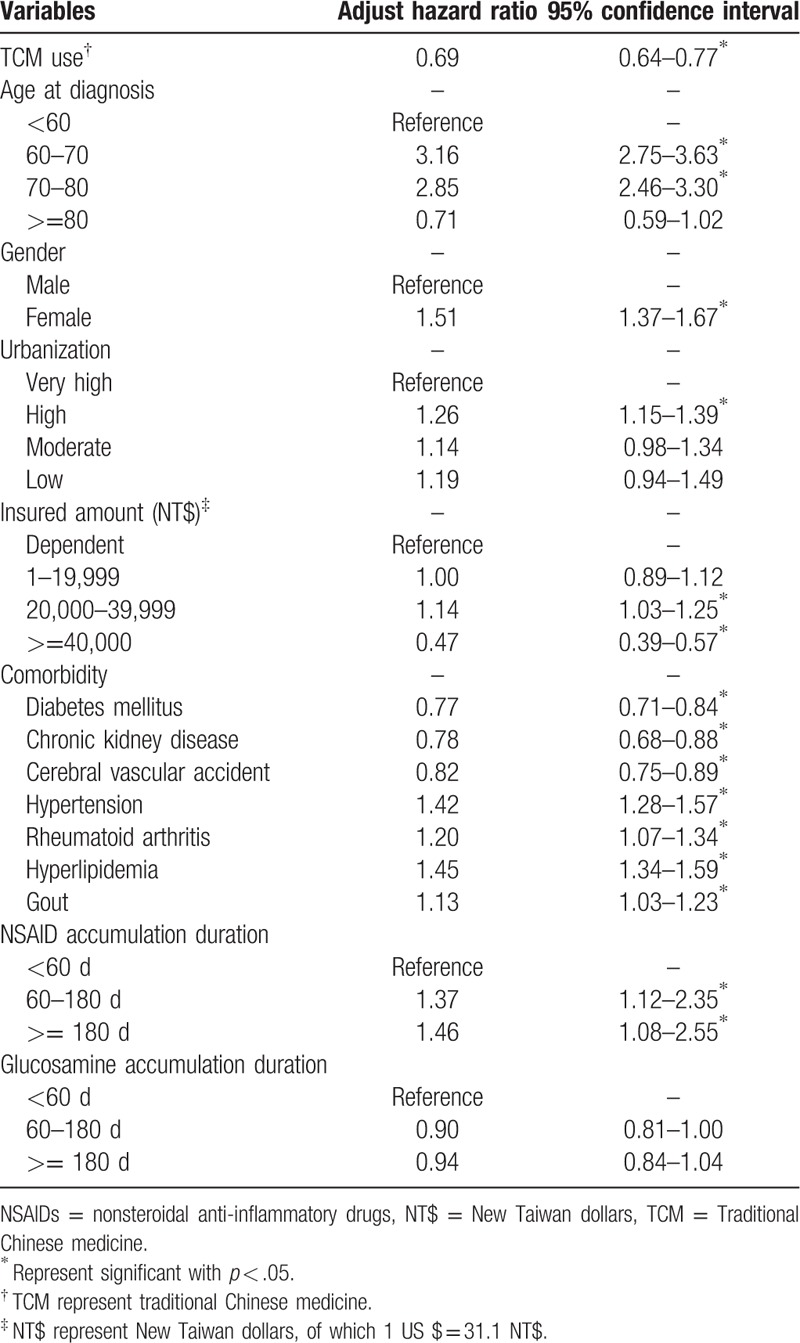
Table 3.
Multivariable Cox model measured hazard ratios and 95% confidence intervals of traditional Chinese medicine cumulative duration for total knee replacement in knee osteoarthritis cohort.
We showed the survival curve of total knee replacement surgery in patients with knee osteoarthritis in Figure 2. Kaplan–Meier survival curves and log-rank analyses revealed significant differences in the rates of total knee replacement surgery between TCM and non-TCM users (log-rank test, P < .001). We present the survival curve of total knee replacement surgery in patients with knee osteoarthritis according to TCM time stratification in Figure 3. TCM usage for <30, 30 to 120, and ≥120 days resulted in significantly reduced rates of total knee replacement surgery (log-rank test, P < .001)
Figure 2.
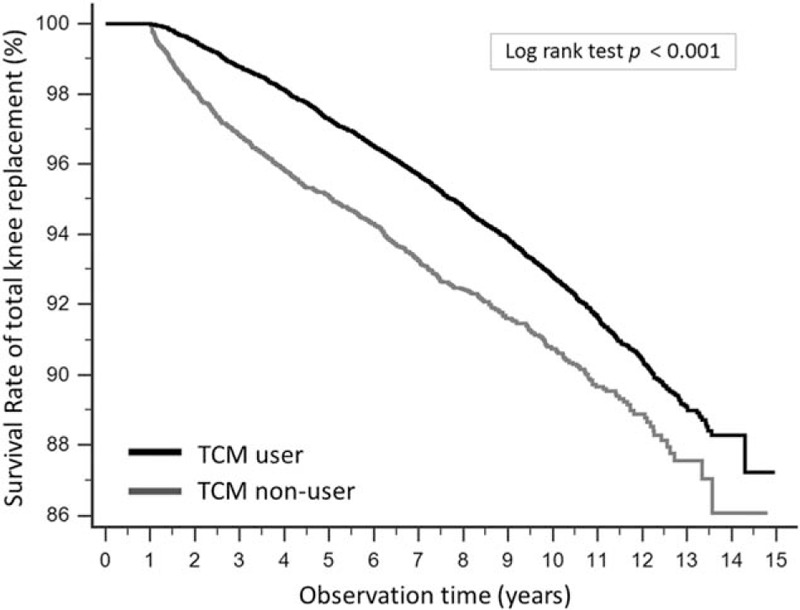
Survival curve of total knee replacement surgery in patients with knee osteoarthritis. Kaplan–Meier survival curves and log-rank analyses revealed significant differences in the rates of total knee replacement surgery between TCM and non-TCM users (log-rank test, P < .001). TCM = Traditional Chinese medicine.
Figure 3.
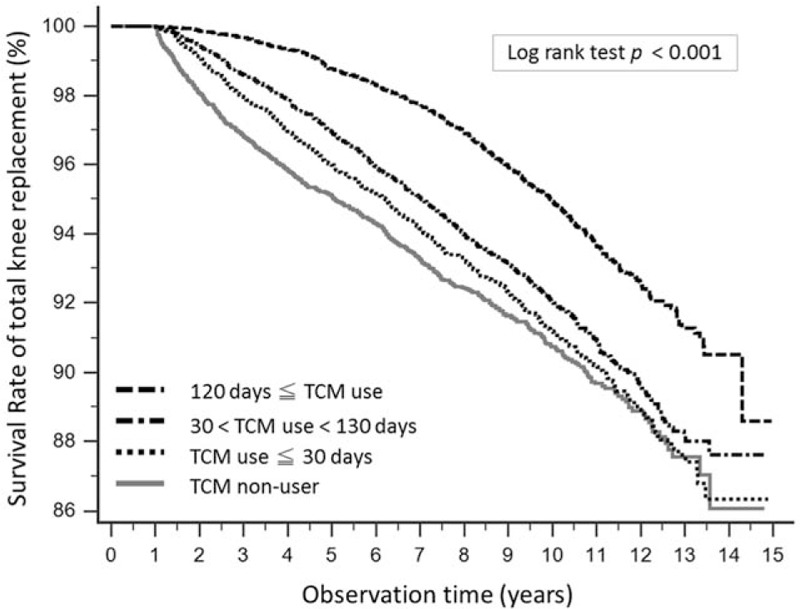
Survival curve of total knee replacement surgery in patients with knee osteoarthritis according to traditional Chinese medicine time stratification. TCM usage for <30, 30 to 120, and ≥120 d resulted in significantly reduced rates of total knee replacement surgery (log-rank test, P < .001). TCM = Traditional Chinese medicine.
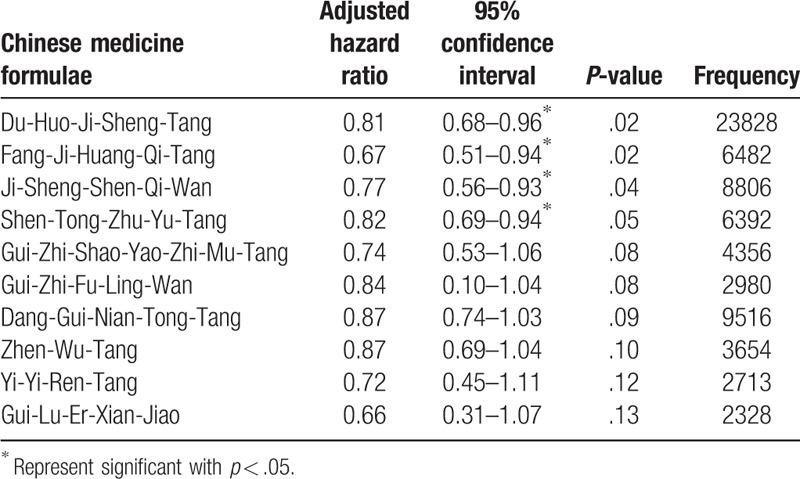
We calculated the HRs for the total replacement risk, analyzed by different demographic factors and comorbidities (Table 2). Compared with patients younger than 60 years, the aHR (95% CI) of 60 to 70 years old patients was 3.16 (2.75–3.63), and the aHR (95% CI) of 70 to 80 years old patients was 2.85 (2.46–3.30). However, the aHR (95% CI) of patients more than 80 years old was 0.71 (0.59–1.02). Female patients had a higher risk of total knee replacement than men, and the aHR (95% CI) was 1.51 (1.37–1.67). Different comorbidities also affected the risk of total knee replacement in our study. Hypertension, hyperlipidemia, gout, rheumatoid arthritis significantly increased with the risk of knee replacement, and the aHR (95% CI) was 1.42 (1.28–1.57), 1.45 (1.34–1.59), 1.13 (1.03–1.23), and 1.20 (1.07–1.34), respectively. In contrast, patients with diabetes mellitus, chronic kidney disease, and cerebral vascular accident were less likely to have knee surgery. With the increase of using NSAIDs, the risk of surgery was higher. The aHR (95% CI) was 1.37 (1.12–2.35), and 1.46 (1.08–2.55) for patients received NSAID accumulation duration 60 to 180 days and more than 180 days. The accumulation duration glucosamine did not significantly affect the risk of TKA, with aHR (95% CI) of 0.90 (0.81–1.00) and 0.94 (0.84–1.04) for treatments of 60 to 180 days and more than 180 days, respectively. We analyzed the formulae of TCM practices used in patients with knee osteoarthritis, as showed in Table 4. All these TCM formulae were related to lower total knee replacement risk. The aHR (95% CI) was 0.81 (0.68–0.96) for Du-Huo-Ji-Sheng-Tang (DHJST), 0.67 (0.51–0.94) for Fang-Ji-Huang-Qi-Tang (FJHQT), 0.77 (0.56–0.93) for Ji-Sheng-Shen-Qi-Wan, and 0.82 (0.69–0.94) for Shen-Tong-Zhu-Yu-Tang.
Table 4.
Adjusted hazards ratio of the total knee replacement for the possible effective Chinese medicine formulae in knee osteoarthritis patients.
The independent t test for accumulated hospitalization costs in patients with knee osteoarthritis showed in Figure 4. TCM users have lower hospitalization costs (average 202301.7 NT$) compared to non-TCM users (average 259041.9 NT$), and the P-value was less than .01. Besides, TCM users have lower hospitalization days (average 30.5 days) compared to non-TCM users (average 43.5 days), and the P-value of independent t test was less than .001 as showed in Figure 5.
Figure 4.
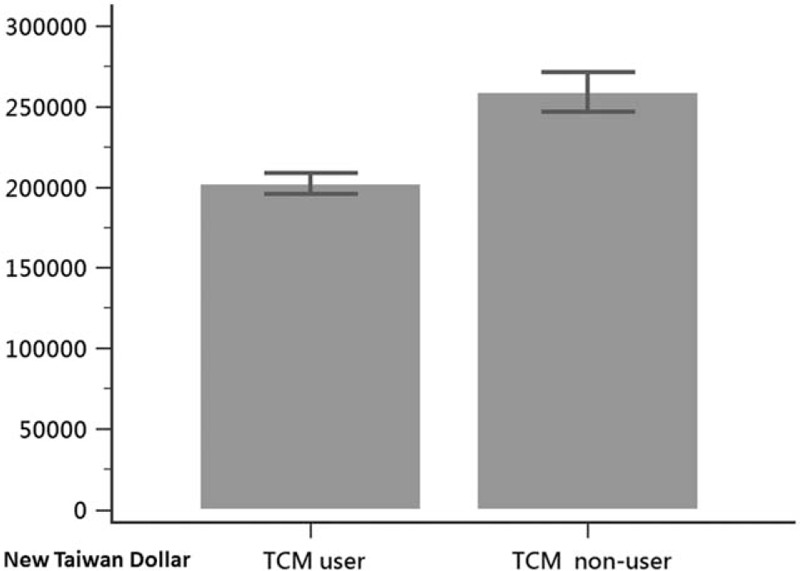
Independent t test for accumulated hospitalization costs in patients with knee osteoarthritis. TCM users have lower hospitalization costs (average 202301.7 New Taiwan Dollar) compared to non-TCM users (average 259041.9 New Taiwan Dollar), and the P-value was less than .01. TCM = Traditional Chinese medicine.
Figure 5.
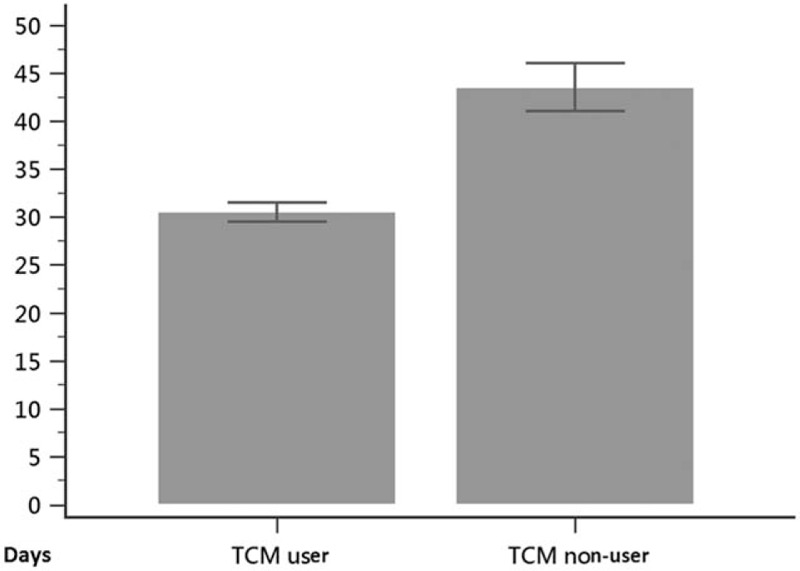
Independent t test for accumulated hospitalization days in patients with knee osteoarthritis. TCM users have lower hospitalization days (average 30.5 d) compared to non-TCM users (average 43.5 d), and the P-value was less than .001. TCM = Traditional Chinese medicine.
4. Discussion
The present study is the first that used a nationwide database to investigate the long-term efficacy of acupuncture and TCM in patients with knee osteoarthritis. The results showed that acupuncture and TCM could reduce the risk of total knee replacement, and the efficacy increased with the treatment time. Based on the results of this study, we propose the inclusion of TCM and acupuncture in the long-term treatment of knee osteoarthritis.
In the presented study, we found that acupuncture treatment can reduce the risk of TKA, and this effect increased with the frequency of the intervention. The World Health Organization indicated acupuncture treatment for knee osteoarthritis since 1980.[23] The American College of Rheumatology and Osteoarthritis Research Society International also recommend acupuncture as a symptomatic treatment for patients with knee osteoarthritis who are unwilling to conduct a TKA.[4,24] In the TCM theory, inserting the fine needle to the acupoints can rebalance the qi (also called “chi” which means the vital energy) over the body and dredge the meridians of the lesions.[25] The commonly used acupoints for knee osteoarthritis are ST34 (Liang-qiu), Xi-Yan, ST36 (Zu-San-Li), GB34 (Yang-Ling-Quan), and SP9 (Yin-Ling-Quan).[26] All these acupoints are in close proximity with the knee, and most of them are located on the muscle attached by the tibia/fibula or patella. Modern medical research has demonstrated an analgesic effect of acupuncture through a gate-control mechanism that elevates the pain threshold; other studies also reported an association with the release of neurotransmitters.[27,28] The afferent nerve stimulation to the spinal cord can release endorphin or other monoamines that block the pain signal and result in an analgesic effect.[29] Several systematic review and meta-analysis studies have reported that acupuncture treatment for more than 4 weeks resulted in a significant pain reduction based on the VAS score or the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC),[30,31] and improved functional mobility and life quality in comparison to treatment with sham acupuncture or muscle strengthening exercises.[26,32] Based on our findings, we found that the more frequent the acupuncture treatment, the lower is the risk of total knee replacement, probably of symptom relief by the treatment.
Since long-term use of NSAIDs was confirmed to exert adverse effects on gastrointestinal bleeding and renal function,[33] the alternative herbal medicine in treating knee osteoarthritis has been studied recently. The most famous Chinese herbal formula for knee osteoarthritis was DHJST, which consists of 15 single herbs, and is commonly used in patients with arthralgia. The effect of DHJST consists of dispelling the wind and dampness, in addition to enriching the qi and blood of the body according to the TCM theory. The possible mechanism of the effects of DHJST may be promoting chondrocyte proliferation and regulating the expression of vascular endothelial growth factor and hypoxia-inducible factor-1α.[34] A 2016 meta-analysis study including several published clinical trials reported that DHJST in combination with conventional therapy (glucosamine or sodium hyaluronate injection) for 4 to 12 weeks reduced the pain VAS score and improved the WOMAC score of knee osteoarthritis.[35] A prospective clinical study also demonstrated that DHJST significantly improved the knee osteoarthritis symptoms in the first 2 weeks of treatment.[36] In consist to previous studies, our present findings demonstrated that DHJST reduced the risk of total knee replacement surgery by 18% in patients with knee osteoarthritis.
In most patients with knee osteoarthritis, effusion is observed, which causes knee joint swelling and limits the range of motion. However, the effusion of the knee osteoarthritis continued to accumulate during inflammation. Many Chinese herbal formulas function by dispelling the phlegm and expelling the water from the body, including FJHQT, Zhen-Wu-Tang, and Yi-Yi-Ren-Tang. FJHQT, also named Boogie in Japan, is composed mainly of the Sinomeniumstem and Astragalus root and has been reported to reduce joint effusion by suppressing the production of pro-inflammatory cytokine IL-1β and increasing the hyaluronan concentrations in the synovial fluid.[37] A recent clinical study demonstrated that oral administration of FJHQT for 12 weeks lowered the knee effusion in patients with osteoarthritis without any adverse effects.[38] In our study cohort, FJHQT was the most effective Chinese herbal formula for patients with knee osteoarthritis and lowered the risk of total knee replacement (HR: 0.68; 95% CI: 0.50–0.93). The assumed mechanism was decreasing the effusion of the knee.
The rehabilitation program of knee osteoarthritis includes strengthening the quadriceps muscles and increasing functional mobility of the knee.[39,40] Enhancing muscle strength and endurance can typically alleviate the loading of the knee and protect the knee from injury.[41] A previous clinical study demonstrated that Gui-Lu-Er-Xian-Jiao (GLEXJ) treatment for 12 weeks increased the muscle strength, especially the knee extensor muscles, and lowered the articular pain and Lequesne index scoresin comparison with patients who were not treated with GLEXJ.[42] The composition of GLEXJ consists of the antlers of Cervusnippon Temminck, carapace of Chinemysreevesii (Gray), root of Panax ginseng C. A. Mey., and fruit of Lyciumbarbarum L. In our study, the prescription frequency of GLEXJ was not as much as that of other formulae, probably because the expensive drugs that were made of pills were not reimbursed by our national health insurance. Nevertheless, GLEXJ still reduced the risk of total knee replacement by up to 36%, although the effect was not statistically difference.
The root of Achyranthes bidentata Blume, which is typically used due to its medicinal efficacy for the lower limb according to the TCM theory, is the central herb of 3 TCM formulae, namely DHJST, Ji-Sheng-Shen-Qi-Wan, and Shen-Tong-Zhu-Yu-Tang. In the present study, we found that these 3 compounds can reduce the risk of total joint replacement surgery. Previous studies showed that A bidentata Blume reduces cartilage degradation by inhibiting nuclear factor κB activation and promotes chondrocyte proliferation.[43,44] Moreover, it could alleviate bone deterioration and inhibit osteoclast differentiation.[45] We conclude that A bidentata Blume could be a valid ingredient in all the above-mentioned TCM formulae.
Based on our findings, patients with diabetes, chronic kidney disease, cerebral vascular accident were associated with a reduced likelihood of receiving total knee replacement, which is in agreement with a previous large-scale study.[46] A possible explanation for this observation is that these comorbidities increase the complication and risk related to the surgery,[47,48] thereby reducing the willingness of patients to undergo total knee replacement. Previous studies suggested that these diseases should be included in the relative contraindications to knee replacement surgery.[49] Rheumatoid arthritis is also an inflammatory disease of the joint, and the prevalence of rheumatoid arthritis is about one-tenth in patients with degenerative arthritis. In our study, rheumatoid arthritis significantly increased the need for surgery and affected the use of TCM; therefore, rheumatoid arthritis is an important confounder for this study. However, we did not include patients with rheumatoid arthritis but not knee osteoarthritis because they have different clinical symptoms and prognosis and therefore differ from patients with knee osteoarthritis.
TCM therapy could be an alternative treatment for patient with knee osteoarthritis. The TCM is widely used in many countries and acupuncture is known to be efficacious in knee osteoarthritis.[50] Our research showed that TCM users have lower hospitalization costs and hospital stays compared to non-TCM users. National Health Insurance in Taiwan reimbursed the medical cost of TCM including CHM and acupuncture. Under the National Health Insurance program payment, the medication fee of CHM is about 1 USD per day,[51] which is relatively affordable than any other treatment for knee osteoarthritis (hyaluronic acid injection, platelet-rich plasma injection). Besides, the cost of acupuncture including diagnosis fee accounts for 18 USD at the 1st time,[51] and the 2nd to 6th times are 7 USD in Taiwan.[51] With efficacy and effectiveness, TCM seems to be a cost-effectiveness therapy among patients with knee osteoarthritis.
There are several limitations in the present study. First, the NHIRD did not include the tests related to the patients’ knee activity, visual pain scales, and X-rays image reports. In addition, body weight and body mass index (BMI) would influence the prognosis of knee osteoarthritis. Unfortunately, the NHIRD did not provide weight or BMI data. Therefore, we have adjusted diseases including hypertension, hyperlipidemia, and diabetes mellitus; these diseases highly correlated with BMI, so it may be possible to reduce research bias partially. These data are relevant for assessing the course of knee osteoarthritis. Thus, we followed the patients from the first diagnosis of knee osteoarthritis to avoid the difference in severity among patients. Therefore, we could only represent the state of the disease with the time from first visit. We also listed the NSAIDs cumulative dosage represented as a severity among patients with knee osteoarthritis. Second, this study is a national survey of Taiwan, and the results may not apply to other ethnic groups. Third, this study contained only TCM practices covered by NHIRD, while other treatments that are not included in the health care system such as tai chi, qi-gong, and folk medicines were not addressed in the study; this might lead to an underestimation of the use of TCM. Forth, the presented studies did not evaluate the side effects of TCM or CHM, and the retrospective cohort research methods cannot avoid the placebo effect, which affects the validity of the study. We still expect more randomized double-blind trials to reduce the interference of the placebo effect. Finally, NHIRD did not describe the acupuncture point in each acupuncture treatment, therefore we were not available to provide the acupuncture points in our paper. However, each TCM doctor select different acupuncture points according to the patient's symptoms and the experience of doctors, and the most common acupuncture points for knee osteoarthritis in previous clinical trials were ST34, ST36, Xiyan, GB34, and SP9.[26]
In conclusion, the results of this nationwide population-based study suggested that TCM and acupuncture were associated with a reduced risk of total knee replacement in patients with knee osteoarthritis, with enhanced benefits from longer durations of TCM use. We suggest that both the TCM and acupuncture could play a greater role in the treatment of knee osteoarthritis.
Author contributions
Conceptualization: Shun-Ku Lin.
Data curation: Pei-Chia Lo, Yao-Chien Tsai, Shun-Ku Lin.
Formal analysis: Pei-Chia Lo, Shun-Ku Lin.
Investigation: Yao-Chien Tsai, Shun-Ku Lin.
Methodology: Fong-Cheng Lin.
Project administration: Fong-Cheng Lin, Shun-Ku Lin.
Validation: Fong-Cheng Lin.
Writing – original draft: Pei-Chia Lo, Shun-Ku Lin.
Writing – review and editing: Fong-Cheng Lin, Yao-Chien Tsai, Shun-Ku Lin.
Shun-Ku Lin orcid: 0000-0003-0067-2280.
Footnotes
Abbreviations: 95% CI = 95% confidence interval, aHR = adjusted hazard ratio, CHM = Chinese herbal medicine, DHJST = Du-Huo-Ji-Sheng-Tang, FJHQT = Fang-Ji-Huang-Qi-Tang, GLEXJ = Gui-Lu-Er-Xian-Jiao, HR = hazard ratio, ICD-9-CM = the International Classification of Diseases, Ninth Revision, Clinical Modification, NHIRD = National Health Insurance Research Database, NSAIDs = nonsteroidal anti-inflammatory drugs, TCM = traditional Chinese medicine, VAS = visual analog scale, WOMAC = western Ontario and McMaster universities osteoarthritis index.
P-CL and F-CL contributed equally to this work.
The work was supported by the Taipei City Hospital (TPECH-105-008 and TPECH-10601-62-071). The conclusions of this study do not represent the opinions of the Bureau of National Health Insurance, the Department of Health, or the National Health Research Institute.
The authors have no conflicts of interest to disclose.
References
- [1].Wood L, Peat G, Thomas E, et al. Knee osteoarthritis in community-dwelling older adults: are there characteristic patterns of pain location? Osteoarthr Cartilage 2007;15:615–23. [DOI] [PubMed] [Google Scholar]
- [2].Zhang W, Doherty M, Peat G, et al. EULAR evidence based recommendations for the diagnosis of knee osteoarthritis. Ann Rheum Dis 2009;69:483–9. [DOI] [PubMed] [Google Scholar]
- [3].Creamer P, Lethbridge-Cejku M, Hochberg MC. Where does it hurt? Pain localization in osteoarthritis of the knee. Osteoarthr Cartilage 1998;6:318–23. [DOI] [PubMed] [Google Scholar]
- [4].Hochberg MC, Altman RD, April KT, et al. American College of Rheumatology 2012 recommendations for the use of nonpharmacologic and pharmacologic therapies in osteoarthritis of the hand, hip, and knee. Arthritis Care Res 2012;64:465–74. [DOI] [PubMed] [Google Scholar]
- [5].Siemieniuk RAC, Harris IA, Agoritsas T, et al. Arthroscopic surgery for degenerative knee arthritis and meniscal tears: a clinical practice guideline. BMJ 2017;357:j1982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Reginster JY, Bruyere O, Neuprez A. Current role of glucosamine in the treatment of osteoarthritis. Rheumatology (Oxford) 2007;46:731–5. [DOI] [PubMed] [Google Scholar]
- [7].Cram P, Lu X, Kates SL, et al. Total knee arthroplasty volume, utilization, and outcomes among Medicare beneficiaries, 1991-2010. JAMA 2012;308:1227–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Sakellariou VI, Poultsides LA, Ma Y, et al. Risk assessment for chronic pain and patient satisfaction after total knee arthroplasty. Orthopedics 2016;39:55–62. [DOI] [PubMed] [Google Scholar]
- [9].Chen FP, Chang CM, Hwang SJ, et al. Chinese herbal prescriptions for osteoarthritis in Taiwan: analysis of national health insurance dataset. BMC Complement Altern Med 2014;14:91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Chen B, Zhan H, Marszalek J, et al. Traditional Chinese medications for knee osteoarthritis pain: a meta-analysis of randomized controlled trials. Am J Chin Med 2016;44:677–703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Weiner DK, Moore CG, Morone NE, et al. Efficacy of periosteal stimulation for chronic pain associated with advanced knee osteoarthritis: a randomized, controlled clinical trial. ClinTher 2013;35:1703–20. [DOI] [PubMed] [Google Scholar]
- [12].Liu JT, Tang DZ, Li XF, et al. Golden plaster for pain therapy in patients with knee osteoarthritis: study protocol for a multicenter randomized, double-blind, placebo-controlled trial. Trials 2013;14:383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Ha CW, Park YB, Min BW, et al. Prospective, randomized, double-blinded, double-dummy and multicenter phase IV clinical study comparing the efficacy and safety of PG201 (Layla) and SKI306X in patients with osteoarthritis. J Ethnopharmacol 2016;181:1–7. [DOI] [PubMed] [Google Scholar]
- [14].National Health Research Institutes. National Health Insurance Research Database. Available at: http://nhirdnhriorgtw/en/Data_Subsetshtml#S3. [Accessed on May 7, 2018]. [Google Scholar]
- [15].Centers for Disease Control and Prevention. The International Classification of Diseases: 9th Revision, Clinical Modification: ICD-9-CM. Available at: https://www.cdc.gov/nchs/icd/icd9cm.htm. [Accessed May 7, 2018]. [Google Scholar]
- [16].Lin SK, Tsai YT, Lo PC, et al. Traditional Chinese medicine therapy decreases the pneumonia risk in patients with dementia. Medicine 2016;95:e4917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Liu JM, Lin PH, Hsu RJ, et al. Complementary traditional Chinese medicine therapy improves survival in patients with metastatic prostate cancer. Medicine 2016;95:e4475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Lin SK, Yan SH, Lai JN, et al. Patterns of Chinese medicine use in prescriptions for treating Alzheimer's disease in Taiwan. Chin Med 2016;11:12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Yu MC, Lin SK, Lai JN, et al. The traditional Chinese medicine prescription patterns of Sjögren's patients in Taiwan: a population-based study. J Ethnopharmacol 2014;155:435–42. [DOI] [PubMed] [Google Scholar]
- [20].Hou PW, Fu PK, Hsu HC, et al. Traditional Chinese medicine in patients with osteoarthritis of the knee. J Tradit Complement Med 2015;5:182–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Mahomed NN, Barrett J, Katz JN, et al. Epidemiology of total knee replacement in the United States medicare population. J Bone Joint Surg Am 2005;87:1222–8. [DOI] [PubMed] [Google Scholar]
- [22].Lin PH, Lin SK, Hsu RJ, et al. The use and the prescription pattern of traditional Chinese medicine among urolithiasis patients in Taiwan: a population-based study. J Altern Complement Med 2016;22:88–95. [DOI] [PubMed] [Google Scholar]
- [23].International Academy of Medical Acupuncture, Inc. Acupuncture: Review and Analysis of Reports on Controlled Clinical Trials. World Health Organization. Available at: http://www.iama.edu/OtherArticles/acupuncture_WHO_full_report.pdf. [Accessed May 7, 2018]. [Google Scholar]
- [24].Zhang W, Moskowitz RW, Nuki G, et al. OARSI recommendations for the management of hip and knee osteoarthritis, part II: OARSI evidence-based, expert consensus guidelines. Osteoarthr Cartilage 2008;16:137–62. [DOI] [PubMed] [Google Scholar]
- [25].Wisneski L, Anderson L. The scientific basis of integrative medicine. Evid Based Complement Alternat Med 2005;2:257–9. [Google Scholar]
- [26].Manyanga T, Froese M, Zarychanski R, et al. Pain management with acupuncture in osteoarthritis: a systematic review and meta-analysis. BMC Complement Altern Med 2014;14:312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Han JS. Acupuncture analgesia. Pain 1985;21:307–10. [DOI] [PubMed] [Google Scholar]
- [28].Felson DT, Lawrence RC, Hochberg MC, et al. Osteoarthritis: new insights. Part 2: treatment approaches. Ann Intern Med 2000;133:726–37. [DOI] [PubMed] [Google Scholar]
- [29].Mata J, Cabrera S, Sanchís P, et al. Electro-acupuncture for treatment of knee pain from osteoarthritis and the possible endocrinology changes: a study protocol for a randomized controlled trial. Trials 2015;16:248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Kwon YD, Pittler MH, Ernst E. Acupuncture for peripheral joint osteoarthritis: a systematic review and meta-analysis. Rheumatology 2006;45:1331–7. [DOI] [PubMed] [Google Scholar]
- [31].Manheimer E, Cheng K, Linde K, et al. Acupuncture for peripheral joint osteoarthritis. Cochrane Database Syst Rev 2010;20:CD001977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Corbett M, Rice S, Madurasinghe V, et al. Acupuncture and other physical treatments for the relief of pain due to osteoarthritis of the knee: network meta-analysis. Osteoarthr Cartilage 2013;21:1290–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Lo PC, Tsai YT, Lin SK, et al. Risk of asthma exacerbation associated with nonsteroidal anti-inflammatory drugs in childhood asthma: a nationwide population-based cohort study in Taiwan. Medicine 2016;95:e5109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Wu G, Chen W, Fan H, et al. DuhuoJisheng decoction promotes chondrocyte proliferation through accelerated G1/S transition in osteoarthritis. Int J Mol Med 2013;32:1001–10. [DOI] [PubMed] [Google Scholar]
- [35].Zhang W, Wang S, Zhang R, et al. Evidence of Chinese herbal medicine Duhuo Jisheng decoction for knee osteoarthritis: a systematic review of randomised clinical trials. BMJ open 2016;6:e008973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Lai JN, Chen HJ, Chen CC, et al. DuhuoJisheng Tang for treating osteoarthritis of the knee: a prospective clinical observation. Chin Med 2007;2:4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Fujitsuka N, Tamai M, Tsuchiya K, et al. Boiogito, a Kampo medicine, improves hydrarthrosis in a rat model of knee osteoarthritis. BMC Complement Altern Med 2015;15:451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Majima T, Inoue M, Kasahara Y, et al. Effect of the Japanese herbal medicine, Boiogito, on the osteoarthritis of the knee with joint effusion. Sports Med Arthrosc Rehabil Ther Technol 2012;4:3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Schilke JM, Johnson GO, Housh TJ, et al. Effects of muscle-strength training on the functional status of patients with osteoarthritis of the knee joint. Nurs Res 1996;45:68–72. [DOI] [PubMed] [Google Scholar]
- [40].Stevens JE, Mizner RL, Snyder-Mackler L. Quadriceps strength and volitional activation before and after total knee arthroplasty for osteoarthritis. J Orthop Res 2003;21:775–9. [DOI] [PubMed] [Google Scholar]
- [41].Slemenda C, Brandt KD, Heilman DK, et al. Quadriceps weakness and osteoarthritis of the knee. Ann Intern Med 1997;127:97–104. [DOI] [PubMed] [Google Scholar]
- [42].Tsai CC, Chou YY, Chen YM, et al. Effect of the herbal drug guiluerxianjiao on muscle strength, articular pain, and disability in elderly men with knee osteoarthritis. Evid Based Complement Alternat Med 2014;2014:297458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [43].Xu XX, Zhang XH, DiaoY, et al. Achyranthes bidentate saponins protect rat articular chondrocytes against interleukin-1β-induced inflammation and apoptosis in vitro. Kaohsiung J Med Sci 2017;33:62–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [44].Weng X, Lin P, Liu F, et al. Achyranthes bidentata polysaccharides activate the Wnt/β-catenin signaling pathway to promote chondrocyte proliferation. Int J Mol Med 2014;34:1045–50. [DOI] [PubMed] [Google Scholar]
- [45].Jiang Y, Zhang Y, Chen W, et al. Achyranthes bidentata extract exerts osteoprotective effects on steroid-induced osteonecrosis of the femoral head in rats by regulating RANKL/RANK/OPG signaling. J Transl Med 2014;12:334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [46].Leung YY, Allen JC, Ang LW, et al. Diabetes mellitus and the risk of total knee replacement among Chinese in Singapore, the Singapore Chinese health study. Sci Rep 2017;7:40671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [47].Kandemir T, Muslu S, Kalayci D, et al. Effects of systemic disorders on postoperative complications after simultaneous bilateral total knee replacement. Turk J Anaesthesiol Reanim 2015;43:169–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [48].Warth LC, Pugely AJ, Martin CT, et al. Total joint arthroplasty in patients with chronic renal disease: is it worth the risk? J Arthroplasty 2015;9Suppl:51–4. [DOI] [PubMed] [Google Scholar]
- [49].Courtney PM, Rozell JC, Melnic CM, et al. Who should not undergo short stay hip and knee arthroplasty? Risk factors associated with major medical complications following primary total joint arthroplasty. J Arthroplasty 2015;9Suppl:1–4. [DOI] [PubMed] [Google Scholar]
- [50].Manheimer E, Cheng K, Linde K, et al. Acupuncture for peripheral joint osteoarthritis. Cochrane Database Syst Rev 2010;1:CD001977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [51].National Health Insurance Medical Service Payment Items and Payment Standards. Available at: https://www.nhi.gov.tw/Resource/webdata/29088_3_2.%E7%AC%AC%E5%9B%9B%E9%83%A8%E4%B8%AD%E9%86%AB%E6%94%AF%E4%BB%98%E6%A8%99%E6%BA%96(104.7.17%E5%85%AC%E5%91%8A%E6%96%B0%E5%A2%9E).pdf. Accessed May 25, 2019. [Google Scholar]


