Supplemental Digital Content is available in the text.
Abstract
Background:
Trigger finger release (TFR) is a common surgical procedure, representing a financial burden to the healthcare system. Our null hypothesis is that the choice surgical setting [operating room (OR) versus procedure room (PR)] and anesthetic type [local-only or monitored anesthesia care (MAC)] do not affect surgical encounter costs for TFR.
Methods:
Adult patients undergoing isolated unilateral TFR between May 2014 and December 2017 by 5 fellowship-trained hand surgeons at a single academic medical center were identified by Current Procedural Terminology (CPT) code (26055). We excluded patients undergoing revision surgery, tenosynovectomy, or additional procedures. Using our institution’s information technology value tools, we calculated total direct costs for each surgical encounter, which were compared between groups. Univariate and multivariable gamma regression were used to model costs.
Results:
Of 210 included patients, 54% (113/210) of cases were performed in the PR and 46% (97/210) in the OR. No significant differences in demographics were observed between PR and OR groups. Compared to local-only in the PR, the OR with local-only, and OR with MAC, demonstrated 2.2- and 3.2-fold greater median costs. Multivariable models suggested that use of the OR independently led to 221% [95% Confidence interval: 137%–345%; P < 0.01] greater mean costs than the PR, and use of MAC was associated with 30% (95% confidence interval: 13%–49%; P < 0.01) greater mean costs for OR cases than local-only, while controlling for other confounders.
Conclusion:
Performing TFR in the PR setting under local-only anesthesia minimizes surgical encounter direct costs for this common procedure.
INTRODUCTION
The value of health care delivered in the United States has received increased attention in the past decade, in part due to policy changes that have included value-based payment models.1,2 Trigger finger, or stenosing tenosynovitis, is one of the most common clinical entities involving the hand, affecting as much as 3% of the general population and 17% of diabetics.3–6 Therefore, treatment costs attributed to this condition represent a burden to the healthcare system.
Although it is clear that surgeons have several options to consider when performing trigger finger release (TFR) surgery for appropriately indicated patients, including choice of surgical setting and anesthetic type, the associated cost implications are less clear but may be substantial. With regard to anesthetic type, performing TFR under local anesthetic without sedation has been shown to be effective,7–10 while other anesthetic methods including Bier block, monitored anesthesia care (MAC), regional block, or general anesthesia are also well-established options.
Performing TFR under local-only anesthesia administered by the surgeon in a procedure room (PR) may provide an opportunity to reduce costs by eliminating the need for an anesthesia team, by reducing need for routine preoperative medical testing,11 and allowing for “wide-awake local anesthesia no tourniquet” (WALANT) surgery in ambulatory- or clinic-based PRs. WALANT has been utilized successfully for TFR,12–14 yielding significant cost-reductions in the context of the US Military Healthcare System12 and in Canada.14 It remains unclear whether these results are generalizable to the majority of the US population covered by commercial and nonmilitary government payers.
Given that surgical setting and anesthetic type have cost implications without proven impact on overall patient outcomes in the current literature, costs should be considered in the surgical treatment of trigger finger. Our institution has developed a “Value Driven Outcomes” (VDO) database containing detailed patient- and item-level total direct cost and payment data for a variety of healthcare services. This has successfully identified areas of high variability in cost,15–18 leading to improved value of care delivered.1 In the current study, the VDO tool was utilized to test our null hypothesis that choice surgical setting and anesthetic type do not affect total direct costs related to TFR surgery.
METHODS
This IRB-approved retrospective cost analysis study included all adult (≥18 years of age) consecutive patients undergoing isolated unilateral trigger digit release between May 2014 and December 2017 by fellowship-trained hand surgeons at a single tertiary academic institution. Trigger finger and thumb releases were included. Patients were identified by CPT code (26005), and corresponding basic demographic and surgical data were tabulated. Manual chart review of all operative, anesthesia, and clinic notes was performed to record the surgical setting and anesthesia type. Patients undergoing additional simultaneous procedures including other surgeries, injections, or bilateral and/or multidigit trigger releases were excluded. Also excluded were patients undergoing revision TFR, tenosynovectomy, flexor digitorum superficialis slip excision, or those undergoing surgery before July 2014 (corresponding with initiation of WALANT hand surgery at our institution). The decision to perform TFR in PR versus operating room (OR) was based upon patient preference using a shared decision-making model.
WALANT Protocol
Patients were not required to undergo preoperative medical or anesthesia evaluation regardless of their comorbidities. All WALANT surgeries were performed in a PR setting, adjacent to the ambulatory surgery center ORs. Patients were brought directly from the surgical waiting room into the PR and placed supine on an OR table with an adjacent mobile hand table, where local anesthesia was administered to the operative site in standard sterile fashion using a formulation of 4.5 cm3 of 1% lidocaine and 4.5 cm3 of 0.5% bupivacaine with 1:100,000 epinephrine buffered with 1 cm3 of 8.4% sodium bicarbonate (10:1 ratio).9 An injection of approximately 5 cm3 was done before the subsequent formal preparation and draping of the surgical site to allow time for the epinephrine to fully act as a vasoconstrictor. Phentolamine was available for use if critical digital ischemia occurred.19
Patients were not asked to disrobe, and the arm was exposed and sterilized to the level of the elbow. All home medications including anticoagulation agents were not held before nor discontinued after the procedure, and patients were not required to fast before the procedure. No cardiovascular monitoring was used, nor was an intravenous (IV) line placed. Staffing of the PR included an attending hand surgeon, medical assistant to assist with achieving field sterility, hand surgery fellow or resident, and a nurse assigned specifically to the PR setting. A sterile nonpneumatic tourniquet was available for use if requested by the attending surgeon. After the procedure, patients received postoperative care instructions and were discharged directly to home or selfcare.
Operating Room Protocol
Patients receiving surgery in the OR, by comparison, were required to fast for at least 8 hours before the procedure, disrobed and placed into a surgical gown, had an IV placed, and underwent routine evaluation by an anesthesiologist in the preprocedural setting before being taken back by gurney to the OR. Choice of anesthesia performed in the OR was based on surgeon’s and anesthesiologist’s preference and included local-only anesthesia using a 1:1 mix of plain lidocaine (1%) and bupivacaine (0.5%), or MAC supplemented with the same local anesthetic mix. A forearm tourniquet was used to minimize intraoperative bleeding. In accord with hospital policy, intraoperative cardiovascular monitoring was routinely supervised by an attending anesthesiologist. After the surgery, the patients were taken by gurney to the postanesthesia care unit where further cardiovascular monitoring and nursing services were utilized, and then they were discharged to the care of a companion after receiving postoperative care instructions.
Total direct cost data were extracted from the VDO database for each individual surgical encounter. The VDO information technology tool draws prospectively collected payment data and patient- and item-level total direct cost data from our institution’s data warehouse for specific patient encounters. VDO costing methods have been previously described, yielding total direct costs for materials used for patient care, facility utilization direct costs (including sterile processing costs), and time-based cost allocations including procedure/operative time and cost of staff involved in care (nursing, surgical technicians, and medical assistants).1,15–18 As the outcome measure was total direct costs, rather than payments, reimbursement for the surgeon, anesthesiologist, and facility were not included – however, time-allocated costs for the surgeon, anesthesiologist, and facility use were captured by the database. Further description of all cost categories captured by the VDO tool are provided in SDC 1 (see appendix, Supplementa1 Digital Content 1 which displays breakdown of Value-Driven Outcomes database categories for total direct costs, INSERT LINK HERE).
Regardless of the surgery setting and anesthesia type, transverse or longitudinal incisions were used depending on surgeon preference for trigger finger releases, and transverse incisions along with the metacarpophalangeal joint flexion crease were universally used for trigger thumb releases. Through the resulting incision, which was approximately 1.25 cm in length, the A1 pulley was sectioned sharply or using tenotomy scissors. Wounds were irrigated and closed with 5-0 nylon horizontal mattress sutures, and a bulky soft dressing was placed.
Cost data were normalized using each individual’s cost divided by the median cost in the PR group, to comply with institutional guidelines prohibiting the public reporting of any financial data related to the details of confidentially disclosed contractual agreements. At our institution, both PR and OR are located within an ambulatory surgery center, and the PR is considered a place of service 22 (a PR within a hospital). Both PR and OR incur a facility cost.
Patient age was summarized as mean ± SD and categorical variables were summarized as count and percentage (%). Patient characteristics were compared between PR and OR using a Student’s t test for age, and a Fisher’s exact or chi-squared test for categorical demographic variables. Comparisons in insurance type were not performed, as this variable would affect payments but not the study outcome (total direct costs). We were interested in comparing costs among the following groups defined by a combination of operation location (OR or PR) and anesthesia type used for this surgery at our institution (local or MAC). As such, the 3 groups identified included PR/Local-Only, OR/Local-Only, and OR/MAC. Relative group costs were calculated relative to the lowest group (PR/Local-Only) by dividing each distinct group median by the lowest group median. Total direct costs were compared across groups using Kruskal-Wallis tests, followed by Nemenyi post hoc tests to conduct pair-wise tests among the groups adjusted for multiple comparisons.20 Univariate and multivariable gamma regression models with a log link were performed to identify factors associated with surgical direct costs, where the factors considered included age, anesthesia time, digit involved, marital status, provider, race, sex, surgery setting, and surgery time. Because surgical time and MAC anesthesia were specific to OR cases, an additional multivariable analysis was performed within the OR cohort to determine the effect of these variables. Statistical significance was assessed at the 0.05 level, and all tests were 2-tailed.
An a priori power analysis was performed. We based our sample size calculations on a medium effect size of 0.40 in SD units. We expected a 1:1 ratio of PR versus OR cases for TFR based on prior experience. With a 2-sided, 2-sample t test, we needed a total sample size of 200 (100 PR and 100 OR) to detect a medium effect size of 0.40 for cost between PR and OR groups with 80% power at a 0.05 alpha level.
RESULTS
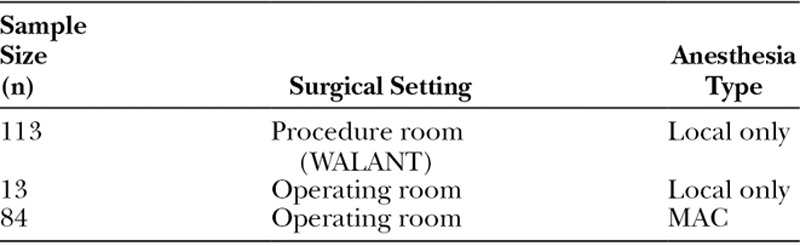
Patient baseline characteristics and surgical details are summarized in Table 1 for the 210 included patients. Mean age was 60.1 ± 11.0 years, and 60% were female. There were no significant differences in baseline patient characteristics between PR and OR groups. The breakdown of TFR surgeries by surgical setting and anesthesia type is illustrated in Table 2 with associated sample sizesa total of 3 unique groups were identified.
Table 1.
Patient Baseline Characteristics and Surgical Details
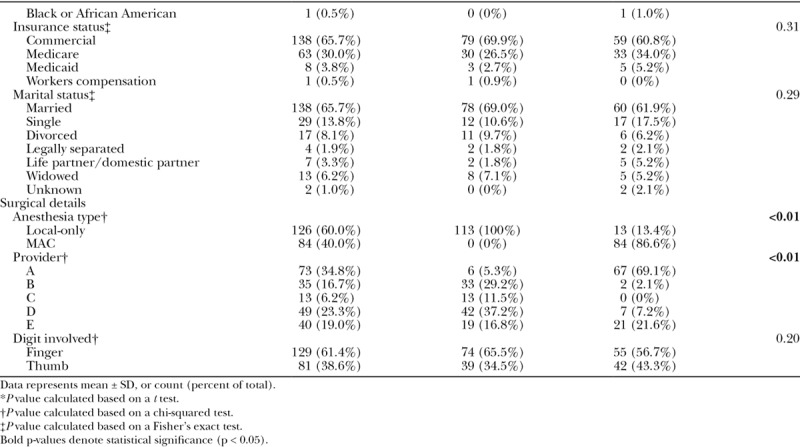
Table 2.
Summary of Unique Study Groups Based upon Surgical Setting and Anesthesia Type
Total direct costs differed significantly between each TFR release group (P < 0.05; Figure 1). TFR performed under WALANT (PR with local-only anesthesia) was associated with the lowest total direct costs (relative cost of 1.0). Performing TFR in the OR under local-only anesthesia was associated with direct costs that were 2.2-fold times the median cost of WALANT [95% confidence interval (CI): 1.71–4.07; P < 0.01], and using MAC anesthesia in the OR was 3.2-fold more costly (95% CI: 3.12–3.39; P < 0.01).
Fig. 1.
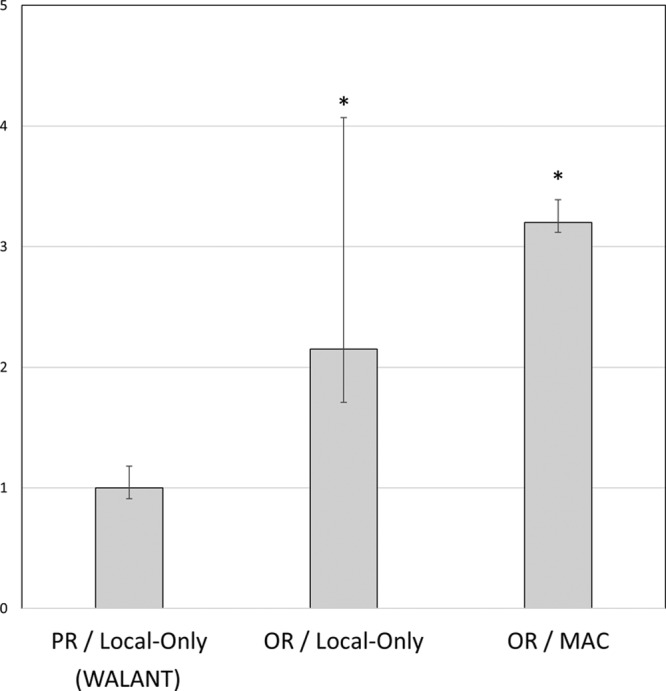
Surgical encounter direct costs. Data represent median ± standard error of the mean. As the reference group, the mean cost for the PR / Local-Onlyl (WALANT) group was normalized to 1.0. *P < 0.05 as compared to left-sided neighboring value per Kruskal-Wallis tests and Nemenyi post hoc multiple comparison tests. Values over graph bars represent fold-change differences relative to the reference group (WALANT).
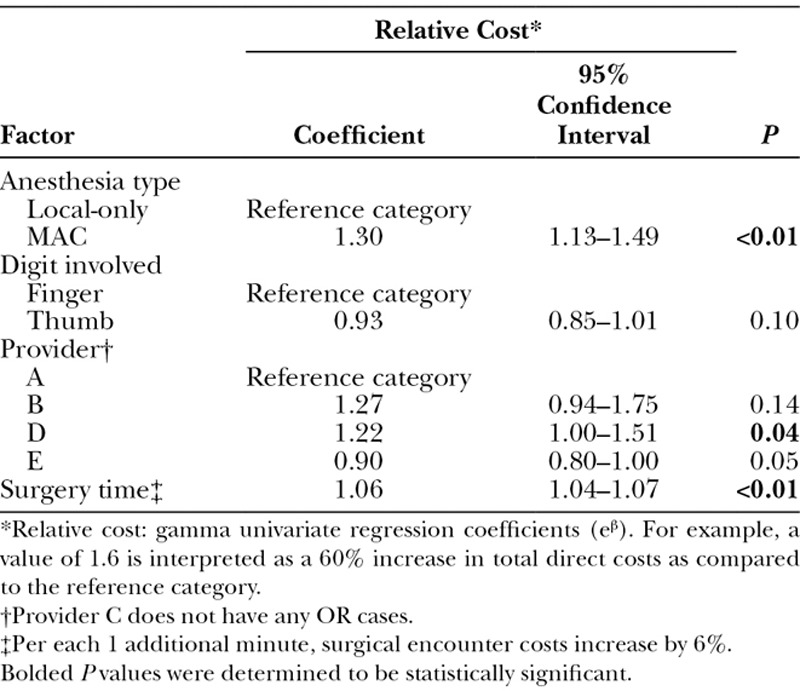
Univariate analysis suggested that surgical setting, anesthesia type, provider, surgical time, and anesthesia time were significantly associated with surgical direct costs for TFR (Table 3). While controlling for anesthesia type, provider, and digit type (thumb versus finger), multivariable gamma regression modeling for all TFR cases (Table 4) revealed that the OR was on average significantly more costly than the PR by 221% (95% CI: 137%–345%; P < 0.01). For TFR performed in the OR (Table 5), use of MAC anesthesia was on average 30% more costly than local-only anesthesia (95% CI: 13%–49%; P < 0.01), and each additional 1 minute of surgical time increased surgical costs by an average of 6% (95% CI: 4%–7%; P < 0.01).
Table 3.
Univariate Analysis to Identify Factors Associated with Surgical Encounter Total Direct Costs
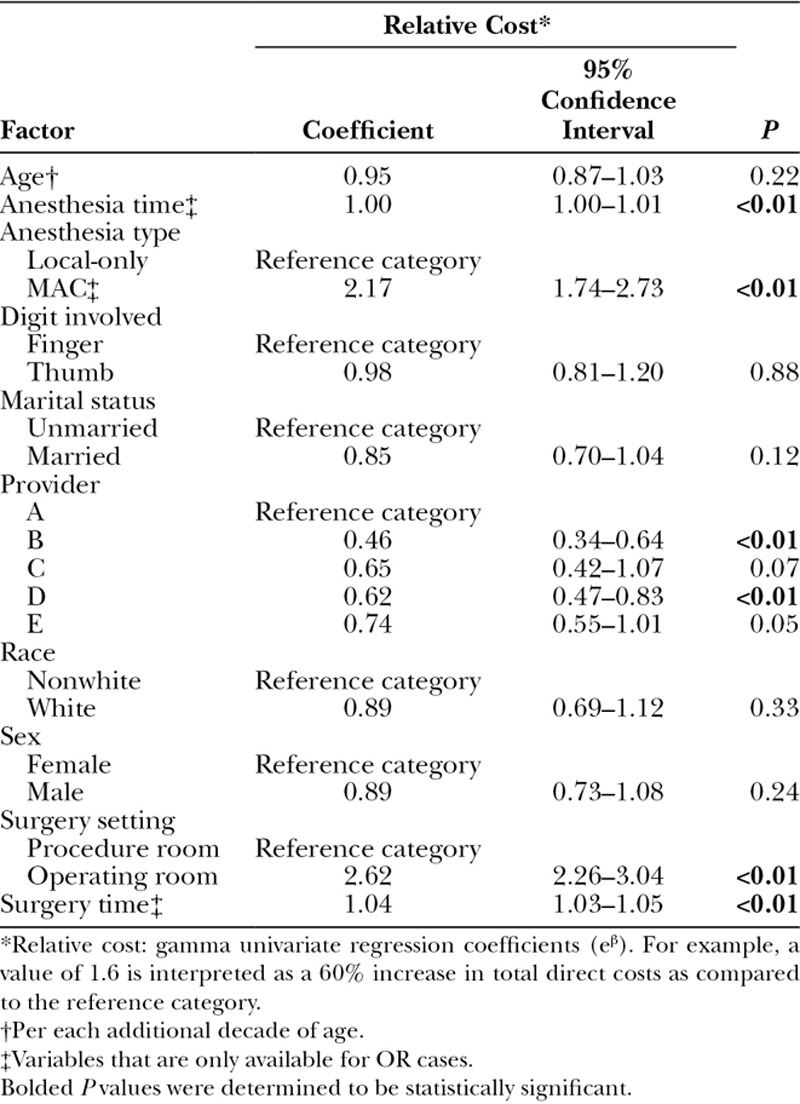
Table 4.
Multivariable Gamma Regression Analysis to Identify Factors Associated with Surgical Encounter Total Direct Costs for All Cases
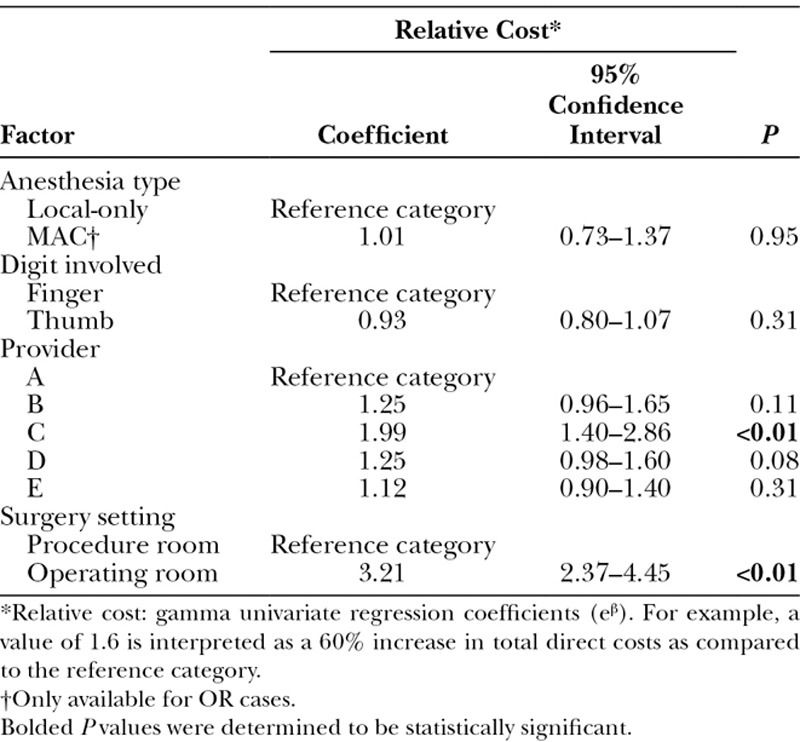
Table 5.
Multivariable Gamma Regression Analysis to Identify Factors Associated with Surgical Encounter Total Direct Costs for OR Cases
DISCUSSION
The main finding of this study is that performing TFR using surgeon-administered local-only anesthetic in a PR setting was the least costly TFR method at our institution. Use of the ambulatory surgery center OR resulted in a 221% cost increase as compared to the PR independent of other factors. Therefore, we reject our null hypothesis that choice of surgical setting (OR versus PR), and anesthetic type (local versus MAC) does not affect costs for TFR.
Surgical setting contributed significantly to surgical costs independent of anesthesia type, as performing the surgery under local-only in the OR, versus under local-only in the PR, significantly increased surgical direct costs by 2.2-fold. Insignificance of anesthesia type in our primary multivariable model is difficult to interpret given that MAC anesthesia was unique to the OR group, and the OR group showed significantly greater costs than the PR. Due to association of these 2 variables (use of OR and MAC anesthesia), we believe that the multivariable analysis specific to the OR subgroup would yield a more accurate estimate of additional costs associated with use of MAC anesthesia over local-only anesthesia. As such, we conclude that anesthesia type independently influences TFR surgery costs, because we found that surgical direct costs were significantly greater by 1.3-fold for MAC as compared to local-only, for cases done in the OR.
Our findings regarding the cost-saving potential of WALANT and the impact of surgical setting on cost are congruent with previous literature. Rhee et al. observed 70% cost savings for TFR performed under WALANT as opposed to the OR in their series of 33 TFR cases.12 The authors projected nearly $400,000 in savings to the Military Health Care System by performing 100 surgeries in a clinic-based PR rather than the OR. Lalonde and Martin have also reported success in performing a multitude of procedures under WALANT in Canada.7,8 Despite these promising findings, the generalizability to the nonmilitary population in the United States is questionable. Luther et al. performed a cost-minimization study that suggested immediate TFR in the office was the least costly of 4 treatment algorithms studied for diabetic patients.21 Total costs of care for immediate release in the clinic and OR were estimated as $642 versus $1,203, respectively, or $750 versus $1,344 when accounting for additional care provided to address minor and major complications. However, these figures included costs for associated nonsurgical care including office visits, making it difficult to discern surgical cost differences between the 2 settings. By specifically elucidating cost differences between surgical settings and anesthesia type for TFR and controlling for other factors that could potentially lead to cost variation, the results of the current study are complimentary to those of Luther et al.
Limitations of the current study deserve mention. Initial identification of patients by procedure code and the retrospective study design introduce potential for selection bias. Generalizability of our results may be limited by our unique pricing agreements between our institution and suppliers, which may affect total direct costs and lead to differences between institutions. Given that we could not identify any patients undergoing TFR in a main hospital OR setting, we could not analyze cost differences based upon this variable. Nonetheless, it has been previously established that the hospital-based OR setting is significantly more expensive than an ambulatory surgery setting for carpal tunnel release surgery.17,22 We believe that excluding this costlier surgical setting does not curtail the goal of the current investigation, which is to highlight opportunities for cost-savings for TFR surgery. We are unable to comment on costs associated with TFR treatment strategies beyond those performed at our institution. This includes use of Bier blocks, regional anesthesia, or general anesthesia. We also did not evaluate costs associated with percutaneous A1 pulley release, which has gained popularity in recent years but is not performed at our institution.23–25 As we did not evaluate costs related to preoperative or postoperative care following trigger finger release, our results are not intended to reflect cost savings beyond the surgical encounter itself. We speculate that it is possible that evaluating costs for the treatment process in its entirety may uncover even greater cost savings afforded by WALANT, through minimization of the need for preoperative medical evaluation.11 We did not evaluate the opportunity cost associated with PR utilization, which may afford the ability to perform more surgeries per unit time through increased efficiency.8 The VDO database does not include indirect cost data such as housekeeping, electricity, or property rent/depreciation. Although the relative dollar amounts reported in this manuscript allow for comparison of costs and payments between groups, an additional limitation is that our institution does not allow raw cost data to be presented. Despite a lack of evidence supporting superior clinical outcomes for one TFR technique over another,21 and paucity of literature supporting differences in outcomes based upon anesthesia type or operative setting, it deserves emphasis that we did not perform a true cost-effectiveness analysis. Therefore, our results describe only cost differences rather than differences in value or quality-adjusted life years between treatment strategies. However, our results may be useful for guiding future cost-effectiveness studies.
In conclusion, this study demonstrates substantial cost-savings for trigger release surgery performed under WALANT (local-only anesthesia in the PR setting) for a US nonmilitary population. Compared to WALANT, other variations of TFR are associated with 2.2- to 3.2-fold greater total direct costs, depending on the chosen surgical setting and anesthesia type.
Footnotes
Published online 3 May 2019.
Supported by the University of Utah Study Design and Biostatistics Center, with funding in part from the National Center for Research Resources and the National Center for Advancing Translational Sciences, National Institutes of Health, through Grant 5UL1TR001067-02 (formerly 8UL1TR000105 and UL1RR025764).
Disclosure: The authors have no financial interest to declare in relation to the content of this article.
Supplemental digital content is available for this article. Clickable URL citations appear in the text.
REFERENCES
- 1.Lee VS, Kawamoto K, Hess R, et al. Implementation of a value-driven outcomes program to identify high variability in clinical costs and outcomes and association with reduced cost and improved quality. JAMA. 2016;316:1061–1072. [DOI] [PubMed] [Google Scholar]
- 2.Kawamoto K, Martin CJ, Williams K, et al. Value Driven Outcomes (VDO): a pragmatic, modular, and extensible software framework for understanding and improving health care costs and outcomes. J Am Med Inform Assoc. 2015;22:223–235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Brown E, Genoway KA. Impact of diabetes on outcomes in hand surgery. J Hand Surg Am. 2011;36:2067–2072. [DOI] [PubMed] [Google Scholar]
- 4.Griggs SM, Weiss AP, Lane LB, et al. Treatment of trigger finger in patients with diabetes mellitus. J Hand Surg Am. 1995;20:787–789. [DOI] [PubMed] [Google Scholar]
- 5.Koh S, Nakamura S, Hattori T, et al. Trigger digits in diabetes: their incidence and characteristics. J Hand Surg Eur Vol. 2010;35:302–305. [DOI] [PubMed] [Google Scholar]
- 6.Strom L. Trigger finger in diabetes. J Med Soc N J. 1977;74:951–954. [PubMed] [Google Scholar]
- 7.Lalonde D, Martin A. Epinephrine in local anesthesia in finger and hand surgery: the case for wide-awake anesthesia. J Am Acad Orthop Surg. 2013;21:443–447. [DOI] [PubMed] [Google Scholar]
- 8.Lalonde D, Martin A. Tumescent local anesthesia for hand surgery: improved results, cost effectiveness, and wide-awake patient satisfaction. Arch Plast Surg. 2014;41:312–316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lalonde DH, Wong A. Dosage of local anesthesia in wide awake hand surgery. J Hand Surg Am. 2013;38:2025–2028. [DOI] [PubMed] [Google Scholar]
- 10.Rozanski M, Neuhaus V, Reddy R, et al. An open-label comparison of local anesthesia with or without sedation for minor hand surgery. Hand (N Y). 2014;9:399–405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Davison PG, Cobb T, Lalonde DH. The patient’s perspective on carpal tunnel surgery related to the type of anesthesia: a prospective cohort study. Hand (N Y). 2013;8:47–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rhee PC, Fischer MM, Rhee LS, et al. Cost savings and patient experiences of a clinic-based, wide-awake hand surgery program at a military medical center: a critical analysis of the first 100 procedures. J Hand Surg Am. 2017;42:e139–e147. [DOI] [PubMed] [Google Scholar]
- 13.Leblanc MR, Lalonde DH, Thoma A, et al. Is main operating room sterility really necessary in carpal tunnel surgery? A multicenter prospective study of minor procedure room field sterility surgery. Hand (N Y). 2011;6:60–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Leblanc MR, Lalonde J, Lalonde DH. A detailed cost and efficiency analysis of performing carpal tunnel surgery in the main operating room versus the ambulatory setting in Canada. Hand (N Y). 2007;2:173–178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kazmers NH, Lazaris EL, Allen CM, et al. Comparison of surgical encounter direct costs for three methods of cubital tunnel decompression. Plast Reconstr Surg. 2019;143:503–510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kazmers NH, Judson CH, Presson AP, et al. Evaluation of factors driving cost variation for distal radius fracture open reduction internal fixation. J Hand Surg Am. 2018;43:606.e1–614.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kazmers NH, Presson AP, Xu Y, et al. Cost implications of varying the surgical technique, surgical setting, and anesthesia type for carpal tunnel release surgery. J Hand Surg Am. 2018;43:971.e1–977.e1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chalmers PN, Granger E, Nelson R, et al. Factors affecting cost, outcomes, and tendon healing after arthroscopic rotator cuff repair. Arthroscopy. 2018;34:1393–1400. [DOI] [PubMed] [Google Scholar]
- 19.Zhang JX, Gray J, Lalonde DH, et al. Digital necrosis after lidocaine and epinephrine injection in the flexor tendon sheath without phentolamine rescue. J Hand Surg Am. 2017;42:e119–e123. [DOI] [PubMed] [Google Scholar]
- 20.Pohlert T. The pairwise multiple comparison of mean ranks package (PMCMR). 2014. [cited 2017 07/01/2017]; Available at http://CRAN.R-project.org/package=PMCMR.
- 21.Luther GA, Murthy P, Blazar PE. Cost of immediate surgery versus non-operative treatment for trigger finger in diabetic patients. J Hand Surg Am. 2016;41:1056–1063. [DOI] [PubMed] [Google Scholar]
- 22.Nguyen C, Milstein A, Hernandez-Boussard T, et al. The effect of moving carpal tunnel releases out of hospitals on reducing United States health care charges. J Hand Surg Am. 2015;40:1657–1662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gancarczyk SM, Jang ES, Swart EP, et al. Percutaneous trigger finger release: a cost-effectiveness analysis. J Am Acad Orthop Surg. 2016;24:475–482. [DOI] [PubMed] [Google Scholar]
- 24.Guo D, McCool L, Senk A, et al. Minimally invasive thread trigger digit release: a preliminary report on 34 digits of the adult hands. J Hand Surg Eur Vol. 2018;43:942–947. [DOI] [PubMed] [Google Scholar]
- 25.Weiss ND, Richter MB. Percutaneous release of trigger digits. Am J Orthop (Belle Mead NJ). 2017;46:E263–E267. [PubMed] [Google Scholar]


