Summary:
A 49-year-old man underwent intraoperatively modified procedure from superficial to radical parotidectomy with excision of the facial nerve 4 branches, temporal, zygomatic, buccal, and mandibular. We have dissected and harvested the branches of the great auricular nerve to repair the defects of the temporal, zygomatic, buccal, and mandibular nerves without microsurgery aid. The aims of the repair were just to mark the nerve endings, to try autologous grafting, and to avoid neuroma(s) formation, although neuroma(s) formations from motor nerves are rare. We did an immediate temporary nonmicrosurgical nerve grafting, and we have sutured each nerve anastomosis by 2–3 stitches of Prolene 6–0. We have observed facial nerve branches’ recovery on the second month, even with radiation therapy, and then gradually more improvements on the third month and then on the sixth month of the follow-up. Finally, the procedure results in permanent sensational functional outcome after 1 year. Because we did not plan a microsurgical repair, this case report does not support any intended nonmicrosurgical procedures for facial nerve repair, but it raises questions for laboratory and animal investigations about the size of Prolene we have used, grip repair taking the epineurium and fascicle in mass closure, and the positive fast functional results. In surgical environments where microscope or microinstruments are lacking, one can still perform primary nerve grafting.
Parotid cancer causes facial nerve impairment in 20% of cases.1–4 Specificity of computed tomography (CT) and magnetic resonance imaging (MRI) is indicated to define tissue invasions.5 However, fine needle aspiration cytology6 and MRI5,7 showed 5% false sensitivity result and this insensitivity is reported in this case.
There are many controversies regarding the timing of facial nerve repair,3,5 and many techniques were described8–10 for the reconstruction of the facial nerve defects after parotidectomy.11–13
PATIENT INFORMATION
A 49-year-old male patient, smoker and lawyer, was presented with the history of parotid mass, slowly growing for >2 years ago. Patient has no relevant medical or surgical history, and there are no other relevant histories.
CLINICAL FINDINGS/TIMELINE
Patient has lesion sized 3 cm × 4 cm, firm in consistency, not tender, and mobile under the skin without any functional impairment of the facial muscles or sensations as indicated clinically. Consent for clinical photography has been given by the patient. There is no delay from the time of presentation to intervention.
DIAGNOSTIC ASSESSMENTS
There are not conclusive findings of malignancy or facial nerve invasions, neither by magnetic resonant image nor by fine needle aspiration cytology. Cytology showed only cellular atypia before surgery.
THERAPEUTIC INTERVENTION
The planned surgery was mass excision within the superficial parotidectomy.
INTERVENTION DETAILS
Under general anesthesia and in supine position, the patient’s head has been elevated and turned to the left side. Preauricular incision was extended around the ear lobule till behind the right ear. After dissection, the mass showed stony hardness at the base, fixation to the underlying structures and huge invasions to facial nerve branches: temporal, zygomatic, buccal, and mandibular. Radical excision of the parotid gland was done with the resection of 4 facial nerve branches (Fig. 1).
Fig. 1.
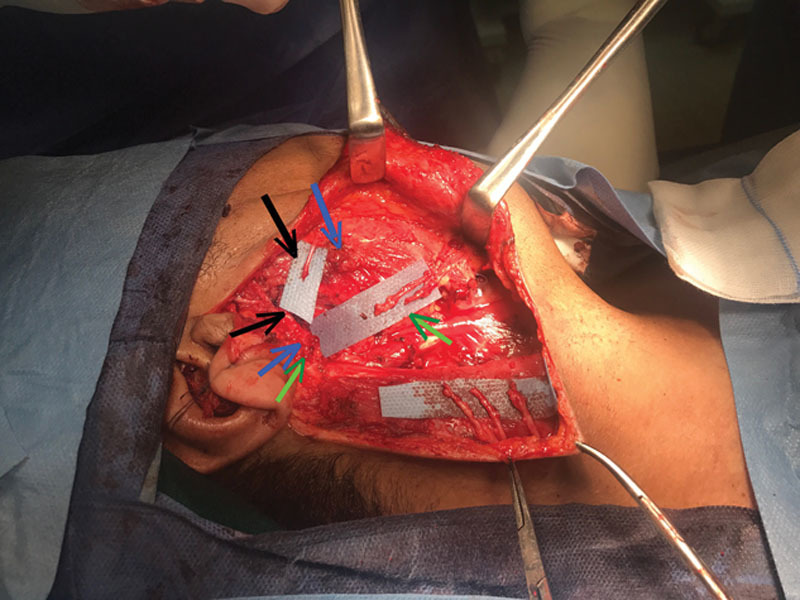
Surgical field immediately after tumor excision. Facial nerve branches’ deficits and nerve endings are indicated by the black arrows for temporal branch, blue arrow indicates the zygomatic branches’ stumps, and the green arrow indicates the buccal and mandibular branches. Note: there are three big divisions of the great auricular nerve in the posterior flap of the wound, which are used for grafting.
In this case, the intraoperative theater has neither microsurgical instruments14 nor intraoperative frozen section biopsy tool,12 but the positive finding was the presence of 3 divisions of the great auricular nerve, which were available in the posterior flap of the wound.
Because we did not plan a microsurgical repair, the choices we had were just a wound closure11 or a nerves’ endings marking by micro clips or by burying them14 to avoid neuroma(s) and injury from radiation therapy.
We thought about the possible wound bed fibrosis, possible necrosis after radiotherapy, and future tissue damage for the entire surgical field. So why not we use the available great auricular nerves? Just to mark the endings, to try autologous grafting, and to avoid neuroma(s) formation.
Surgeons did an immediate temporary nonmicrosurgical grafting for the defects in facial nerve branches by Prolene 6–0 (Fig. 2). Two to three stitches for each site were taken the epineurium and fascicle in mass closure grip. We covered the proximal and distal anastomosis by posterior belly of digastric muscle and masseteric fascia, respectively, as shield.14
Fig. 2.
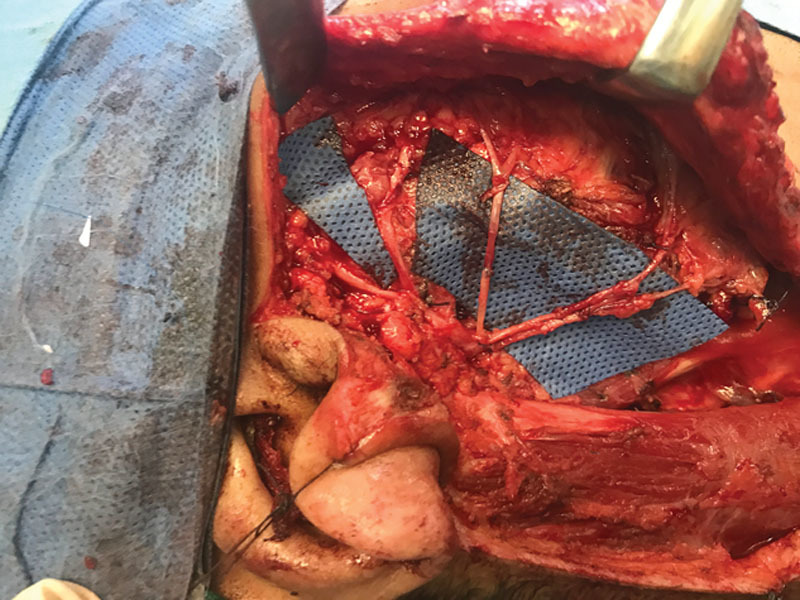
Intraoperative repair of the resected parts of the temporal, zygomatic, buccal, and mandibular nerves by nonmicrosurgical anastomosis.
FOLLOW-UP AND OUTCOMES
After 5 days, the histopathology report showed completely excised mass with safe deep and lateral resection margins. It concluded that the diagnosis is an infiltrating adenocarcinoma with positive lymph nodes metastasis, L.Ns 4/4.
This case showed surprising recovery, which was so fast before the sixth month,12,14 as patient has started facial movements on the 37th day of surgery during his radiation therapy (see video, Supplemental Digital Content 1, which shows that patient has regained most of the function but with some dyskinesia and depressor menti muscle wasting on the 85th day postoperative, http://links.lww.com/PRSGO/B56).
Video Graphic 1.

See video, Supplemental Digital Content 1, which shows patient has regained most of function but with some dyskinesia and depressor menti muscle wasting on the 85th day postoperative, http://links.lww.com/PRSGO/B56.
This clinical progress has encouraged the surgeons to wait, and they have found an excellent functional outcome during the follow-up period. Facial nerve function regained at 3 months, and it was better at 6 months and then has been fully recovered after 1 year without any fasciculation or muscle dyskinesia (Fig. 3).
Fig. 3.

Patient after 1 year of surgery has an excellent functional outcome for facial nerve branches.
After 1 year, there were not any residual metabolic activities anywhere or residual lesions of the operative field (see video, Supplemental Digital Content 2, which shows full functional recovery of facial nerve branches 1 year later and informed verbal consent from the patient, http://links.lww.com/PRSGO/B57).
Video Graphic 2.

See video, Supplemental Digital Content 2, which shows full functional recovery of facial nerve branches 1 year later and informed verbal consent from the patient, http://links.lww.com/PRSGO/B57.
DISCUSSION
In relevant literature, parotid cancer usually impairs facial nerve.3,4,13 In this patient, the facial nerve has been invaded within the anatomical distribution to upper and lower trunk divisions. The upper trunk gave off temporal and zygomatic branches, and the lower trunk gave off branches to buccal, mandibular, and cervical nerves.
All nerve repair techniques are depending on microsurgery aid.5,11 The nerve repair results have improved after the evolution of magnifying loupes and microscopy.11 After that era, there is no any literature report about the nerve repair without microsurgery.
Primary end-to-end nerve anastomosis and cable graft interposition have produced functional outcomes better than nerve substitution techniques.16 Epineural nerve repair has wide acceptance and is practiced more than fascicular repair.17,18 In this case, the surgeon did not do any of them, but he just repaired the nerve in one grip, taking the epineurium and fascicle in mass closure. Although the first sign of return of facial functions is usually encountered around 6 months, and then recovery continues up to 2 years,14,16 this case showed surprising recovery, which was so fast as the patient started facial twitches on the 37th day! In this case, recovery was started during his postoperative radiotherapy, this encouraged the surgeons to wait and observe, and then they found an excellent progress. Although, intraoperatively, we cared for fine handling and proper nerve endings’ orientation, nerve gratings for the defects were done without microsurgery. It was technically easy and took few minutes. Shielding15 the bridge grafts by masseteric fascia and digastric muscle could be a beneficial support for repair and protection from radiotherapy damage.
Because we did not plan a microsurgical repair, we have simply grafted the facial nerve branches by interposition grafts of greater auricular nerve. Patient has a superior functional outcome during the follow-up period even with radiation therapy, at 3 months, 6 months, and after 1 year, without muscle wasting, twitching, or dyskinesia.
CONCLUSIONS
The primary take-home messages from this case report are as follows: in surgical environments where microscope or microinstruments are lacking, one can still perform primary nerve grafting. Based on our observation in this case report, further laboratory and animal investigations of the nonmicrosurgical nerve grafting could make sense.
Footnotes
Published online 16 May 2019.
Disclosure: The authors have no financial interest to declare in relation to the content of this article.
REFERENCES
- 1.Terhaard C, Lubsen H, Tan B, et al. Facial nerve function in carcinoma of the parotid gland [published correction appears in Eur J Cancer. 2007;43(12):1883]. Eur J Cancer. 2006;42:2744–2750. [DOI] [PubMed] [Google Scholar]
- 2.Bussu F, Parrilla C, Rizzo D, et al. Clinical approach and treatment of benign and malignant parotid masses, personal experience. Acta Otorhinolaryngol Ital. 2011;31:135–143. [PMC free article] [PubMed] [Google Scholar]
- 3.Owusu JA, Truong L, Kim JC. Facial nerve reconstruction with concurrent masseteric nerve transfer and cable grafting. JAMA Facial Plast Surg. 2016;18:335–339. [DOI] [PubMed] [Google Scholar]
- 4.Malgrozata W, Tomaz K, Grezyana B. The presence of facial nerve weakness on diagnosis of a parotid gland malignant process. Eur Arch Otolaryngol 2012;269:1177–1182. doi: 10.1007/s00405-011-1882-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sánchez-Burgos R, Otero TG, Lassaletta L, et al. Facial nerve reconstruction following radical parotidectomy and subtotal parotidectomy for advanced malignant parotid neoplasms. Ann Maxillofac Surg. 2015;5:203–207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gudm JK, Ajan A, Abtahi J. The accuracy of fine-needle aspiration cytology for diagnosis of parotid gland mass: a clinicopathological study of 114 patients. J App Oral Sci. 2016;24:561–667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ying L, Jia LA, Yai Tan T, et al. Accuracy of diagnosis of salivary gland tumors with the use of ultrasonography, magnetic resonance image: a meta-analysis. Oral Maxillofac Radiol. 2017;119:238–245. [DOI] [PubMed] [Google Scholar]
- 8.Gur E, Zuker RM, Zaretski A, et al. Incomplete facial paralysis: the use of the ipsilateral residual facial nerve as a donor nerve for facial reanimation. Plast Reconstr Surg. 2018;142:202–214. [DOI] [PubMed] [Google Scholar]
- 9.Hontanilla B, Olivas J, Cabello Á, et al. Cross-face nerve grafting versus masseteric-to-facial nerve transposition for reanimation of incomplete facial paralysis: a comparative study using the FACIAL CLIMA evaluating system. Plast Reconstr Surg. 2018;142:179–191. [DOI] [PubMed] [Google Scholar]
- 10.Chuang DC, Lu JC, Chang TN, et al. Comparison of functional results after cross-face nerve graft-, spinal accessory nerve-, and masseter nerve-innervated gracilis for facial paralysis reconstruction: the Chang Gung experience. Ann Plast Surg. 2018;81:S21–S29. Available at file:///C:/Users/top/Downloads/SAP-D-17-00322.pdf. Accessed August 2018. [DOI] [PubMed] [Google Scholar]
- 11.Gordin E, Lee TS, Ducic Y, et al. Facial nerve trauma: evaluation and considerations in management. Craniomaxillofac Trauma Reconstr. 2015;8:1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nicoli F, D Ambrosia C, David L, et al. Microsurgical dissection of facial nerve in parotidectomy: a discussion of technique and long term results. Gland Surg. 2017;6:308–314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ching S, Thoma A, Archibald S, et al. A novel method of grafting facial nerve defects results from parotidectomy. Can J Plast Surg. 2002;10:53–55. [Google Scholar]
- 14.Darrouzet V, and de Mones del Pujol E. Facial nerve grafting: indications and techniques. In Atlas D’acces Libre En Chirurgie Orl Et Cervico-Faciale. 2017;Open Education, by Fédération de Chirurgie de la Base du Crâne CHU Bordeaux, Université de Bordeaux; 1–10. Available at https://vula.uct.ac.za/access/content/group/ba5fb1bd-be95-48e5-81be-586fbaeba29d/Indications%20and%20techniques%20of%20facial%20nerve%20grafting.pdf. Accessed September 2018. [Google Scholar]
- 15.Özmen OA, Falcioni M, Lauda L, et al. Outcomes of facial nerve grafting in 155 cases: predictive value of history and preoperative function. Otol Neurotol. 2011;32:1341–1346. [DOI] [PubMed] [Google Scholar]
- 16.Humphrey CD, Kriet JD. Nerve repair and cable grafting for facial paralysis. Facial Plast Surg. 2008;24:170–176. [DOI] [PubMed] [Google Scholar]
- 17.Siemionow M, Bobkiewicz A, Cwykiel J, et al. Epineural sheath jacket as a new surgical technique for neuroma prevention in the rat sciatic nerve model. Ann Plast Surg. 2017;79:377–384. [DOI] [PubMed] [Google Scholar]
- 18.Matsumine H, Takeuchi Y, Sasaki R, et al. Adipocyte-derived and dedifferentiated fat cells promoting facial nerve regeneration in a rat model. Plast Reconstr Surg. 2014;134:686–697. [DOI] [PubMed] [Google Scholar]


