Supplemental Digital Content is available in the text.
Abstract
Background:
Hyaluronic acid (HA), a large glycosaminoglycan involved in proliferation, migration, and tissue repair, is suggested to be an important factor for keratinocyte activation and re-epithelialization. The experimental hypothesis of this study was that HA accelerates re-epithelialization, and we aimed to investigate the effect of exogenous intradermal HA during deep dermal, incisional wound healing in vivo in humans, the primary endpoint being re-epithelialization.
Methods:
A total of 8 standardized deep dermal incisional wounds (depth 1.6 mm, width 1.8 mm) per subject were induced in 10 healthy volunteers. Two of the wound sites per subject were pretreated with injections of HA and 2 with saline solution. At 2 time points (24 hours and 14 days), 2 biopsies for each treatment group (one for histology and one for proteomics) were taken. Skin erythema was measured at 24-hour intervals for 14 days as a surrogate measurement of inflammation.
Results:
At 24 hours, 8 of 9 wounds pretreated with HA showed complete re-epithelization, whereas none of the wounds pretreated with saline had re-epithelized. Wounds pretreated with HA also showed a 10-fold regulation of 8 identified proteins involved in wound healing compared to wounds treated with saline solution. No difference in inflammation, as measured as erythema, could be seen between any of the groups.
Conclusions:
We conclude that HA accelerates re-epithelialization and stimulates an altered protein expression in vivo in human deep dermal incisional skin wounds, but has no effect on the inflammation process as measured by erythema.
INTRODUCTION
Wound healing is a complex biological process defined as barrier restoration, involving cross talk between keratinocytes, fibroblasts, and immune cells.1 During the initial phase of wound healing, keratinocytes are activated, alter their gene expression, and migrate over the wound surface. Delayed wound healing can be due to both reduced and excessive inflammation.2,3
Hyaluronic acid (hyaluronan, HA) is a large glycosaminoglycan and an essential extracellular component of skin.4 It is active throughout the entire process of wound healing being involved in proliferation, migration, and tissue remodeling.5,6 It has been suggested that an increase in HA is an important factor for keratinocyte activation and re-epithelialization and that it inhibits terminal differentiation, but it has not been clearly determined whether HA has to be endogenously synthesized or whether exogenous HA provides the same stimulation.7 It is proposed that HA plays an important role in the fast and scar-free fetal wound healing seen during the first and second trimester.8–11 We have previously shown that, in an in vitro human wound model, the degradation of HA in amniotic fluid impairs the ability of this fluid to accelerate re-epithelialization.12 Factors stimulating HA synthesis increase proliferation and epidermal thickness.13 Native HA has a very high molecular mass of 1000–8000 kDa and is gradually degraded into smaller fragments.14 Fragment properties depend on the molecular weight with large molecules being immunosuppressive, whereas smaller fragments are proinflammatory.15
A minimally invasive human in vivo cutaneous wound model for the evaluation of innate skin reactivity and healing status has previously been described.16 In the present article, a commercially available system called tissue viability imaging (TiVi), which utilizes polarized spectroscopy, was used to assess erythema intensity as a surrogate for inflammation17 and the model is supplemented with a tissue biopsy. Skin biopsies of the deep dermal incisional wound can be analyzed histologically, for example, for epidermal re-epithelialization or by proteomic studies to ascertain the protein expression. Proteomic studies contribute to a better understanding and characterization of the molecular composition of the tissue and by which means an intervention alters the skin’s response.
In the present study, we aimed to investigate the influence of exogenous HA on re-epithelialization, erythema, and protein expression in a minimally invasive in vivo human deep dermal incisional wound model. The experimental hypothesis is that HA accelerates complete re-epithelialization, which is the primary endpoint.
METHODS
Subjects
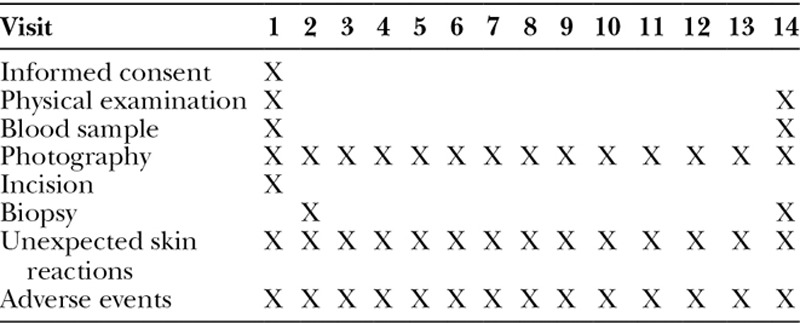
After approval by the local Ethics Committee at Linköping University, Sweden (register number 2013/371-31), and securing written and oral informed consent, 10 healthy, non-nicotine using male volunteers between 20 and 27 years of age (mean: 23) were recruited and enrolled in the study. The sample size was based on an 80% power calculation. The study was performed according to the Declaration of Helsinki. Subjects reporting a history of poor wound healing or an altered response to minimal trauma to the skin were excluded (see table, Supplemental Digital Content 1, which shows inclusion and exclusion criteria, http://links.lww.com/PRSGO/B46). According to the plan of assessments (Table 1), all subjects underwent a physical examination and had blood samples taken at the first visit and at day 14 (see table, Supplemental Digital Content 2, which shows blood samples, http://links.lww.com/PRSGO/B47). One subject had blood results outside the reference range and was excluded from further analysis. Left proximal ventral forearm skin was chosen as the study site and had to be uninjured and scar free in all subjects. The study period was 14 days, and a case report form was set up for each participant. Signs of skin reaction or adverse events were noted at each visit.
Table 1.
Plan of Assessments
Wound Maneuver and Biopsies
The subjects were positioned with their left arms supported at heart level in a fixed position on a table. Injections, creation of wounds, and biopsy specimen collection were carried out by one of the authors (E.N.) using loupes (magnification 2.5×, stereo).
The forearm skin was cleaned with chlorhexidine (5 mg/ml; Fresenius Kabi, Uppsala, Sweden). A total of 8 standardized deep dermal incisional wounds (depth 1.6 mm, width 1.8 mm) per subject were made using single-use semiautomatic spring-loaded sterile blood collection lancets (HAEMOLANCE plus; HaeMedic, HTL-STREFA S.A., Ozorków, Poland). A swab soaked in saline solution was held over the site for 5 minutes to minimize bleeding. According to the randomization, 4 sites on each subject were pretreated with an intradermal injection of 0.05 ml HA (Hyalgan/natriumhyaluronat 10 mg/ml; Takeda Pharma AB, Solna, Sweden) (group 1) and 4 additional sites were injected with 0.05 ml of saline solution (9 mg/ml; Fresenius Kabi AB, Uppsala, Sweden) (group 2). Injections were made entering the skin from the side with a U-100 insulin 29-gauge/0.33-mm ø needle (Becton Dickinson, Franklin Lakes, New Jersey) approximately 8 mm from the planned wound site. The volume of the injection was chosen as it created wheals of about 0.5 mm in diameter, judged suitable for wounding and biopsies.
After the incisions with the lancets, subject remained 1 hour for observation and any skin reactions or adverse events were noted. At the end of the hour, the study area was photographed with TiVi for assessment of skin erythema. The study sites were left without a dressing, and subjects were asked not to expose the study sites to friction from clothing or activities. Two biopsies, one for histology and one for proteomics, from treatment groups 1 and 2 were taken at 2 time points (24 h and 14 d) from all subjects.
Biopsies were taken during local anesthesia (Carbocain/mepivain hydrochlorid 10 mg/ml; AstraZeneca AB, Södertälje, Sweden), which was administered proximal to the study sites and after the skin was washed with chlorhexidine. A 2-mm biopsy punch (Integra Miltex, York, Pa.) was used. The biopsy wounds were closed with an absorbable stitch and wound closure tape. A compression dressing was put around the forearm to minimize bleeding and hematoma formation. The subjects were instructed to remove the external dressing after 1 hour, leaving the wound site open. The biopsies for proteomic analysis were immediately heat stabilized with Denator Stabilizer T1 (Denator, Göteborg, Sweden) and stored at −20°C until analysis.
Histology
The biopsies were fixed overnight in 4% neutral buffered formaldehyde. Then, they were dehydrated through an ethanol-xylene series and embedded in paraffin orientated, so that cross sections of the wounds were generated. Sections (7 µm thick) from the center of the specimens, including the epidermis and a deep dermal central wound, were mounted, deparaffinized, rehydrated, and stained with hematoxylin and eosin.
Re-epithelialization was determined by 2 independent observers (E.N. and G.K.), of whom one was blinded (G.K.), by light microscopy. The 2 observers were in agreement when determining re-epithelialization and no further analysis was made. Only a total epithelialization was regarded as a positive result. Images were captured using a BX41 light microscope (×20/0.50; ×40/0.75) and a DP 70 CCD camera (Olympus, Solna, Sweden).
Statistical comparisons of scoring of re-epithelialization were made using nonparametric McNemar’s test. Probabilities of less than 0.05 were accepted as significant. Statistical analyses were conducted using GraphPAD Prism 5.0 (GraphPAD Software Inc., La Jolla, Calif.).
Proteomics
The biopsies were moved to Eppendorf tubes and 300 µl of the solution [9 M urea, 4% 3-((3-cholamidopropyl) dimethylammonio)-1-propanesulfonate (wt/vol), 65 mM dithiothreitol, 2% Pharmalyte 3–10 (vol/vol), trace of bromophenol blue] was added. The biopsies were then homogenized by sonication 3 × 10 seconds. The mixture was incubated for 2 hours at 4°C followed by 1 hour of centrifugation at 20,000g. An aliquot of 10 µl was used for measuring the protein concentration with a Quant kit (GE Healthcare, Uppsala, Sweden) according to the manufacturer’s recommendations. Fifteen micrograms of protein from each subject were pooled into 8 groups according to the intervention randomization and 100 µg of the pooled samples were analyzed by 2-dimensional gel electrophoresis with a horizontal setup (IPGphore and Multiphore) (GE Healthcare) according to the method described by Görg et al.18 The separated proteins were stained with silver19 and analyzed as previously described.20
Quantitation of the amount of protein in a spot was assessed as background corrected optical density (OD), integrated over all pixels in the spot expressed as integrated OD using PDQuest software (Bio-Rad Laboratory Bio-Rad Laboratories, Solna, Sweden) and only those spots with over 10-fold changes in volume after were defined as altered. The altered protein spots were excited from the gel, in-gel digested with trypsin, and the extracted peptides identified with mass spectrometry.
Tissue Viability Imaging
To assess temporal and spatial changes in red blood cell concentration (erythema), the TiVi700 TiVi system (WheelsBridge AB, Linköping, Sweden) was used.17,21 The study sites were photographed using TiVi 1 hour after the wounds were made and thereafter at approximately 24-hour intervals over a period of 14 days. All measurements were done at a constant room temperature of 23°C.
The camera was positioned 30 cm directly above the test area. In all photographs, regions of interest (ROI) 3 mm in ø(diameter), centering each wound and an undamaged area on the subject’s skin were selected. The mean TiVi value data for each ROI were generated using the built-in analysis feature of the WheelsBridge software and exported to Microsoft Excel 2010 (Microsoft Corporation) and GraphPad Prism 5.0 (GraphPAD Software Inc.) for further calculations and analysis. The mean TiVi-value generated from an undamaged skin area was subtracted from the mean TiVi-values obtained from the ROIs encircling the incisions to show only the relative change in the erythema intensity for each subject.
Mean TiVi values for the ROIs were arranged into 2 data sets according to group (HA and NaCl). The difference in effect of treatment on the erythema intensity was calculated using a paired, two-tailed t test. Probabilities of less than 0.05 were accepted as significant. Statistical analyses were conducted using GraphPAD Prism 5.0 (GraphPAD Software Inc.).
RESULTS
All 10 subjects completed the investigation, and no unexpected skin reactions or adverse events were reported. Subject 7 was excluded from further analysis due to prolonged activated partial thromboplastin time. All other laboratory results were within reference ranges both at the beginning and at the end of the study.
Histologically, Wounds Treated with HA Re-epithelialized in 24 Hours
Histologically, we found the wounds to be deep dermal, as they did not reach through the dermal layer. Wounds treated with HA showed a complete re-epithelialization at 24 hours in 8 of 9 wounds. No re-epithelialization could be seen in the group with wounds that were injected with saline solution (McNemar’s test, P = 0.0133) (Table 2).
Table 2.
Results from a Histological Evaluation of the Re-epithelialization at 24 Hours

At 24 hours, the majority of cells seen in the wound histologically were assessed to be red blood cells and inflammatory cells. After 14 days, a clearly visible dermal scar with few remaining inflammatory cells was noted and all wounds in both groups were re-epithelialized. Figure 1 shows Hematoxylin and eosin staining of biopsies demonstrating different grades of re-epithelialization.
Fig. 1.

Hematoxylin and eosin staining of biopsies demonstrating different grades of re-epithelialization. Completely healed epidermis was seen in the group treated with HA after 24 hours (A and C). In contrast, wounds treated with saline solution (9 mg/ml) showed incomplete healing after 24 hours (B and D). At day 14, all wounds in all groups were re-epithelialized. E and G, Wounds treated with HA at day 14. F and H, Wounds treated with saline solution at day 14. Arrows indicate wound sites and wound directions. Scale bar = 500 µm.
Proteomics
In all, 168 protein spots were matched in all 4 gels and included for spot quantification. Eight protein spots were, at 24 hours, 10-fold or more upregulated or downregulated comparing wounds treated with HA to wounds treated with NaCl. At day 14, 9 protein spots were 10-fold or more upregulated or downregulated comparing wounds treated with HA to wounds treated with NaCl. Some proteins were identified in multiple isoforms that differed in molecular weight or isoelectric point (the pH at which a protein carries no net charge). All identified proteins are listed in table, Supplemental Digital Content 3, which displays a list of identified proteins, http://links.lww.com/PRSGO/B48 and Figure 2 shows the differences in the levels expressed as OD between the groups. Network analysis for all altered proteins using Search Tool for the Retrieval of Interacting Genes/Proteins showed that 8 of the proteins were involved in wound healing (Fig. 3). The false discovery rate for the identified pathway was 0.0158.
Fig. 2.

Altered proteins expressed as OD. Differences in the levels of altered proteins in wounds treated with HA and saline solution (NaCl). The y axis represents the quantity expressed as OD, and x axis represents the different proteins expressed as accession number according to the protein database UniProt (http//expasy.org).
Fig. 3.
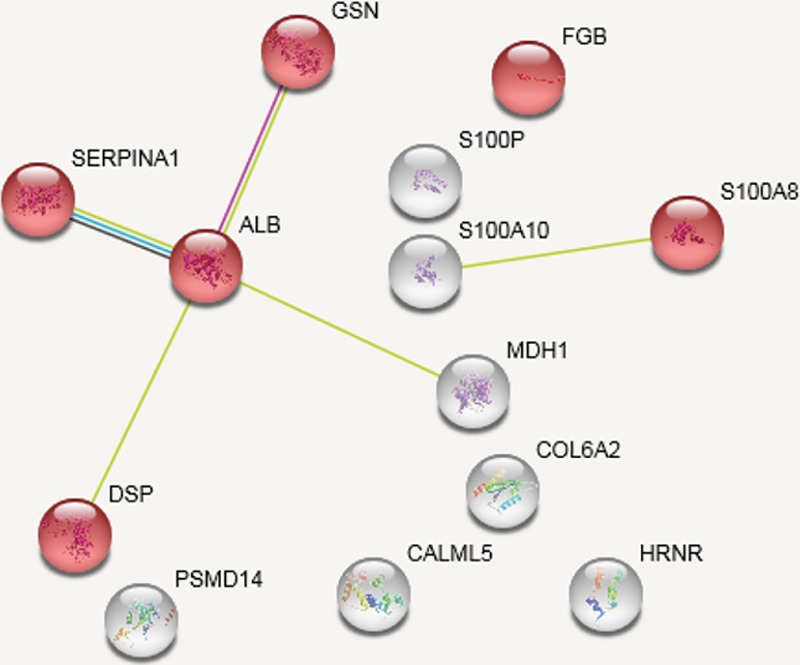
Pathway analysis of altered proteins. The red network nodes represent proteins involved in wound healing. The edges represent protein -protein interaction and include different types of associations depicted by the colored lines; known interactions: pink, predicted interactions; green (gene neighborhood), blue (gene co-occurrence), and red (gene fusions); other interactions: olive green (textmining), black (co-expression), and purple (protein homology). The nodes are marked with the gene name of the proteins and the corresponding protein name is listed in table, Supplemental Digital Content 3, which displays a list of identified proteins, http://links.lww.com/PRSGO/B48. ALB (Albumin), DSP (Dermcidin), FGB(Fibrinogen beta chain), GSN (Gelsolin).
TiVi Showed No Differences at Group Level in Erythema Intensity after Injection of HA
All subjects showed a similar increase in red blood cell concentration in response to the incisional wounds, demonstrating the most pronounced erythema 24 hours post wounding. The erythematous responses subsided over time and had returned to near baseline levels at day 14 in all subjects. No difference between the treatments in erythema intensity could be detected (t test, P = 0.27) (Fig. 4).
Fig. 4.
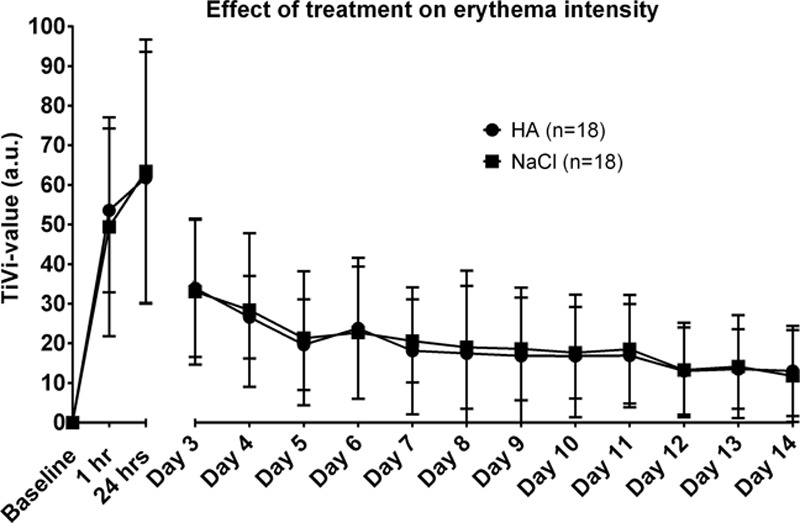
Results from TiVi. Wounds treated with HA or saline solution (NaCl) at a group level (n = 18) are shown as mean TiVi-values (erythema intensity). No difference in the erythema intensity between the groups could be detected using the TiVi-system. Data were normalized by the subtraction of baseline (TiVi-values for unprovoked skin). Error bars show ±SD.
DISCUSSION
In the present study, we have successfully extended a previously described human, minimally invasive wound healing model16 to include parameters such as evaluation of histological re-epithelialization and quantification of protein expression at the wound site. We demonstrate that wounds treated with exogenous HA show accelerated re-epithelialization and an altered protein expression compared with wounds treated with saline solution. A more robust method, TiVi, has replaced laser Doppler imaging for assessment of erythema as a surrogate marker for inflammation.
The wounds and biopsy specimens were intended to be as small as possible to minimize scarring, but still be of a size that could be prepared for histology and containing enough protein for analysis. The ventral forearm was judged particularly suitable as study site as the dermis in this location is thin and less hirsute. The wounds were easily detectable at histology when using the standard procedure for cutting cross sections and staining. Histology showed well-centered standardized wounds extending into the dermis.
The histological results show that injection of HA has a positive effect on re-epithelialization that is not seen after saline solution injections. This supports the hypothesis that HA stimulates migration and proliferation of keratinocytes.12,22–23We saw these effects even though the HA was exogenous and administered intradermally. Analysis with immunohistochemistry is needed to further study the nature of the cell infiltrate and possible changes following the intervention. The focus in the present study was on the re-epithelialization part of the wound healing process and detailed study of the dermal infiltrate is under continued study.
The inflammatory response as reflected by erythema was found to reach its peak at 24 hours after the wounding and then gradually decline for 2 weeks as the healing process progressed. These results are in concordance with previous findings.16,23 We did not, however, find any differences in the inflammatory response between the groups as reflected by the lack of change in degree and time course of the erythema in the dermal wounds. This suggests that the mechanism of the effect of exogenous intradermal HA does not involve the inflammatory response during the wound healing process, at least when measured by TiVi. A limitation of the method is the fact that erythema may not reflect all aspects of variability in inflammation.
Aspects of the HA administration itself need to be considered. The HA was administered at day 1 and had a molecular weight of 500–730 kDa. No further injections were given. The half-life of HA is short in skin,25 and metabolism of HA gives rise to shorter HA fragments, which sometimes exert different biological effects than those seen by high molecular weight HA. Generally, high molecular weight HA is considered to promote cell quiescence because HA break down products signal injury.15,26–28 In our study, no analysis of HA concentration or HA size profiling over time were done. According to the literature, little is known about HA molecular weight distribution in vivo in pathological settings and further studies are warranted.29
The proteomics analysis should be considered a pilot study that shows the potential use of proteomics to investigate the molecular mechanisms in wound healing. Additional study analyzing samples from individual subjects are warranted. Also, supplementary investigation of the proteins identified as upregulated or downregulated in this study is required. An initial analysis shows a wide range of proteins altered, such as albumin and the Protein S100 family with general roles in cell activation and wound healing30,31 and Galectin-7 and Hornerin with more epithelial cell relevance.32 Network analysis further demonstrated altered proteins involved in wound healing.
We conclude that exogenous intradermal HA accelerates re-epithelialization and alters protein expression in human in vivo deep dermal skin wounds. Knowledge of the re-epithelialization process is valuable for development of new therapies for accelerated wound healing and our results indicate that HA might be an important component in future regimes aiming at an improved wound closure. Further studies will focus on addressing the dermal component of wound healing after treatment with HA and analyzing protein concentrations from individual samples and interpretation of altered proteins.
ACKNOWLEDGMENTS
We thank Kristina Briheim, senior laboratory technician, for her excellent technical assistance throughout this study and Jonathan Rakar for his valuable work with earlier versions of the manuscript.
Supplementary Material
Footnotes
Published online 3 May 2019.
Work was done in Linköping, Sweden.
Preliminary data has been presented at 2015 4th TERMIS World Congress, Boston, MA.
Supported by ALF Grants, Region Östergötland, Sweden.
Disclosure: Dr. Anderson and Dr. Henricson both work in areas of interest to the company (WheelsBridge AB) that develop and market the tissue viability imaging system used for the quantification of red blood cell concentrations in skin. Dr. Anderson has shares and limited involvement in the company (www.wheelsbridge.se). Dr. Henricson assisted the company in the early development state and has a royalty agreement with WheelsBridge AB.
Supplemental digital content is available for this article. Clickable URL citations appear in the text.
REFERENCES
- 1.Pastar I, Stojadinovic O, Yin NC, et al. Epithelialization in wound healing: a comprehensive review. Adv Wound Care (New Rochelle). 2014;3:445–464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Strbo N, Yin N, Stojadinovic O. Innate and adaptive immune responses in wound epithelialization. Adv Wound Care (New Rochelle). 2014;3:492–501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.MacLeod AS, Mansbridge JN. The innate immune system in acute and chronic wounds. Adv Wound Care (New Rochelle). 2016;5:65–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Toole BP. Hyaluronan: from extracellular glue to pericellular cue. Nat Rev Cancer. 2004;4:528–539. [DOI] [PubMed] [Google Scholar]
- 5.Almond A. Hyaluronan. Cell Mol Life Sci. 2007;64:1591–1596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chen WY, Abatangelo G. Functions of hyaluronan in wound repair. Wound Repair Regen. 1999;7:79–89. [DOI] [PubMed] [Google Scholar]
- 7.Tammi RH, Tammi MI. Hyaluronan accumulation in wounded epidermis: a mediator of keratinocyte activation. J Invest Dermatol. 2009;129:1858–1860. [DOI] [PubMed] [Google Scholar]
- 8.Aya KL, Stern R. Hyaluronan in wound healing: rediscovering a major player. Wound Repair Regen. 2014;22:579–593. [DOI] [PubMed] [Google Scholar]
- 9.Longaker MT, Chiu ES, Adzick NS, et al. Studies in fetal wound healing. V. A prolonged presence of hyaluronic acid characterizes fetal wound fluid. Ann Surg. 1991;213:292–296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.West DC, Shaw DM, Lorenz P, et al. Fibrotic healing of adult and late gestation fetal wounds correlates with increased hyaluronidase activity and removal of hyaluronan. Int J Biochem Cell Biol. 1997;29:201–210. [DOI] [PubMed] [Google Scholar]
- 11.Estes JM, Adzick NS, Harrison MR, et al. Hyaluronate metabolism undergoes an ontogenic transition during fetal development: implications for scar-free wound healing. J Pediatr Surg. 1993;28:1227–1231. [DOI] [PubMed] [Google Scholar]
- 12.Nyman E, Huss F, Nyman T, et al. Hyaluronic acid, an important factor in the wound healing properties of amniotic fluid: in vitro studies of re-epithelialisation in human skin wounds. J Plast Surg Hand Surg. 2013;47:89–92. [DOI] [PubMed] [Google Scholar]
- 13.Pasonen-Seppänen S, Karvinen S, Törrönen K, et al. EGF upregulates, whereas TGF-beta downregulates, the hyaluronan synthases Has2 and Has3 in organotypic keratinocyte cultures: correlations with epidermal proliferation and differentiation. J Invest Dermatol. 2003;120:1038–1044. [DOI] [PubMed] [Google Scholar]
- 14.Cowman MK, Lee HG, Schwertfeger KL, et al. The content and size of hyaluronan in biological fluids and tissues. Front Immunol. 2015;6:261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jiang D, Liang J, Noble PW. Hyaluronan as an immune regulator in human diseases. Physiol Rev. 2011;91:221–264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Varol AL, Anderson CD. A minimally invasive human in vivo cutaneous wound model for the evaluation of innate skin reactivity and healing status. Arch Dermatol Res. 2010;302:383–393. [DOI] [PubMed] [Google Scholar]
- 17.McNamara PM, O’Doherty J, O’Connell ML, et al. Tissue viability (TiVi) imaging: temporal effects of local occlusion studies in the volar forearm. J Biophotonics. 2010;3:66–74. [DOI] [PubMed] [Google Scholar]
- 18.Görg A, Drews O, Lück C, et al. 2-DE with IPGs. Electrophoresis. 2009;30 (Suppl 1):S122–S132. [DOI] [PubMed] [Google Scholar]
- 19.Shevchenko A, Wilm M, Vorm O, et al. Mass spectrometric sequencing of proteins silver-stained polyacrylamide gels. Anal Chem. 1996;68:850–858. [DOI] [PubMed] [Google Scholar]
- 20.Ghafouri B, Ståhlbom B, Tagesson C, et al. Newly identified proteins in human nasal lavage fluid from non-smokers and smokers using two-dimensional gel electrophoresis and peptide mass fingerprinting. Proteomics. 2002;2:112–120. [PubMed] [Google Scholar]
- 21.O’Doherty J, Henricson J, Anderson C, et al. Sub-epidermal imaging using polarized light spectroscopy for assessment of skin microcirculation. Skin Res Technol. 2007;13:472–484. [DOI] [PubMed] [Google Scholar]
- 22.Oksala O, Salo T, Tammi R, et al. Expression of proteoglycans and hyaluronan during wound healing. J Histochem Cytochem. 1995;43:125–135. [DOI] [PubMed] [Google Scholar]
- 23.Kaya G, Rodriguez I, Jorcano JL, et al. Selective suppression of CD44 in keratinocytes of mice bearing an antisense CD44 transgene driven by a tissue-specific promoter disrupts hyaluronate metabolism in the skin and impairs keratinocyte proliferation. Genes Dev. 1997;11:996–1007. [DOI] [PubMed] [Google Scholar]
- 24.Gurtner GC, Werner S, Barrandon Y, et al. Wound repair and regeneration. Nature. 2008;453:314–321. [DOI] [PubMed] [Google Scholar]
- 25.Tammi R, Säämänen AM, Maibach HI, et al. Degradation of newly synthesized high molecular mass hyaluronan in the epidermal and dermal compartments of human skin in organ culture. J Invest Dermatol. 1991;97:126–130. [DOI] [PubMed] [Google Scholar]
- 26.Prosdocimi M, Bevilacqua C. Exogenous hyaluronic acid and wound healing: an updated vision. Panminerva Med. 2012;54:129–135. [PubMed] [Google Scholar]
- 27.David-Raoudi M, Tranchepain F, Deschrevel B, et al. Differential effects of hyaluronan and its fragments on fibroblasts: relation to wound healing. Wound Repair Regen. 2008;16:274–287. [DOI] [PubMed] [Google Scholar]
- 28.Litwiniuk M, Krejner A, Speyrer MS, et al. Hyaluronic acid in inflammation and tissue regeneration. Wounds. 2016;28:78–88. [PubMed] [Google Scholar]
- 29.Monslow J, Govindaraju P, Puré E. Hyaluronan—a functional and structural sweet spot in the tissue microenvironment. Front Immunol. 2015;6:231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Donato R, Cannon BR, Sorci G, et al. Functions of S100 proteins. Curr Mol Med. 2013;13:24–57. [PMC free article] [PubMed] [Google Scholar]
- 31.Kerkhoff C, Voss A, Scholzen TE, et al. Novel insights into the role of S100A8/A9 in skin biology. Exp Dermatol. 2012;21:822–826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Panjwani N. Role of galectins in re-epithelialization of wounds. Ann Transl Med. 2014;2:89. [DOI] [PMC free article] [PubMed] [Google Scholar]


