Abstract
Background:
Diagnostic imaging for craniosynostosis currently relies entirely on radiation images, but it has been estimated that a risk of cancer from diagnostic x-rays may exist. Use of ultrasound imaging has been reported, but very little has been written on normal findings of the cranial suture. Also, ultrasound diagnostic methods have not been established. To obtain images for the diagnosis of abnormal sutures in craniosynostosis, we investigated the normal ultrasonographic appearance of the suture. To establish screening methods for craniosynostosis, we prepared a 2-point method for simple evaluation and confirmed its usefulness.
Methods:
Ultrasonography was performed in infants with normal head, deformational plagiocephaly, and craniosynostosis. We focused on the measurement indices and decided on the order for making our observations. Furthermore, we developed an evaluation method (2-point method) and recorded our finding in a useful table.
Results:
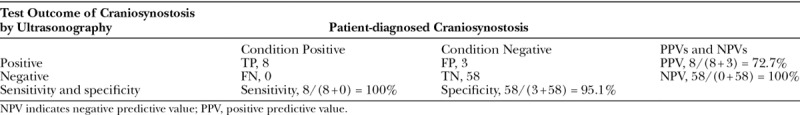
We could clearly judge whether the cranial suture was patent or closed and were able to measure the suture width. Even for 2-year-old children, the width of the sutures at the points measured exceeded the echocardiographic resolution. By using the 2-point evaluation method, all the sutures could be inspected in about 2 minutes. Sensitivity was 100% and specificity was 95.1%.
Conclusions:
Our present studies showed that normal or abnormal suture can be clearly distinguished by ultrasound. By evaluating the fixed points instead of the whole line, it was possible to shorten the inspection time. Ultrasound screening by applying the 2-point method is very useful.
INTRODUCTION
Craniosynostosis is sometimes hidden from view due to cranial deformation. However, very few cases with intrinsical bone fusion are known to exist in cranial deformity of infants. In 115 infants presenting with unilateral posterior cranial flattening, only 1 child had synostotic posterior plagiocephaly (lambdoid synostosis).1 Most of them had deformational plagiocephaly with no bony fusion and no increase in intracranial pressure. In recent years, helmet therapy has been used in deformational plagiocephaly for cosmetic purposes.2,3 The correction rate of plagiocephaly with helmet therapy decreases as the infant’s age increases.4,5 On the other hand, in the case of craniosynostosis it is necessary to perform surgery at an early stage. A delay in surgery beyond the first 9–12 months of life leads to progressive deformity of the cranial base, resulting in abnormal facial growth.6,7
Endoscopic suture resection surgery and postoperative helmet therapy has attracted attention in recent years for the treatment of craniosynostosis.8 The benefits include a short operation time, a short hospitalization period, and prompt recovery.9,10 However, considering the rate of improvement due to the age of helmet therapy, it is desirable to start treatment within 6–8 months of age.4,5 The importance of the early discovery of cranial suture fusion is increasing as treatment methods are changing.
Methods for craniosynostosis diagnosis currently rely entirely on radiographic images such as x-rays and computed tomographic (CT) scans. Risk of cancer from diagnostic x-rays has been estimated.11–14 Children are much more radiosensitive than adults. A 1-year-old infant is 10–15 times as likely as a 50-year-old adult to develop a malignancy from the same dose of radiation.12 We believe that reliable screening methods that are safer than x-rays and CT scans are necessary to differentially diagnose the infants who have craniosynostosis given the large number of those with skull deformities.
Ultrasound examination of the head is used by pediatric neurosurgeons and pediatricians to perform intracranial assessment.15–17 In these examinations, echocardiographic probes are used to inspect the anterior fontanel, which is widely patent. In 1998, Soboleski et al.18 examined excised synostosed suture specimens by high-resolution sonography and reported that the high-resolution sonographic images provided easy means to assess sutural width. Since that report, ultrasound in the diagnosis of craniosynostosis has been reported.19–22 It was applied to infants with head deformity or craniosynostosis and shows that ultrasound is a highly specific and sensitive imaging technique. Sonography was found to be operator dependent with special technologist training required and not feasible in infants older than 13 months.20 Also, they reported that patency is reliably confirmed by ultrasound in sutures wider than 0.5 mm21. In 2017, Pogliani et al.22 reported ultrasound assessment of infants with head deformity or small head circumference and that ultrasound is a highly specific and sensitive imaging technique.
In the abovementioned reports, very little is written about the ultrasonographic findings of the normal cranial suture. To obtain a diagnosis of abnormal sutures in craniosynostosis, it is necessary to know the ultrasonographic findings of normal sutures. Also, ultrasound diagnostic methods have not been established. Therefore, we decided to observe the cranial sutures of normal infants with echocardiographic ultrasound. We were able to recognize sutures with small gaps, and we reported our findings. Moreover, to establish a screening method for craniosynostosis, we developed a 2-point method as a simple evaluation method and confirmed its usefulness.
METHODS
Patients
This study was performed at an outpatient clinic of the Department of Plastic and Reconstructive Surgery in Osaka Medical College and the Department of Pediatric Neurosurgery in Takatsuki Hospital from March 2016 to June 2018. The ethical committees of both hospitals approved this study.
The subject of the study is 43 patients with deformational plagiocephaly, 18 patients with normal skulls, and 8 patients with craniosynostosis (Tables 1 and 2). Infants with deformational plagiocephaly visited Takatsuki hospital every month for helmet therapy. We chose 45 infants of them randomly. Two infants were excluded from the study because they stopped outpatient visits early. The mean patient age was 6.1 months (range, 4–14 months), and the mean follow-up period was 4.8 months (range, 2–8 months). Children with normal skulls routinely visited Osaka Medical College Hospital for the treatment of cleft lip and polysyndactyly. Children with normal skulls routinely visited Osaka Medical College Hospital for the treatment of cleft lip and polysyndactyly. We chose 20 infants of them randomly. Two infants were excluded from the study because they were suspected of having the syndrome. The mean patient age was 7.1 months (range, 1–24 months), and the mean follow-up period was 4.5 months (range, 1–8 months). Children with deformational plagiocephaly and normal skulls underwent echocardiographic examinations at regular intervals. All cases of craniosynostosis underwent surgery after diagnosis by echocardiographic and CT scan examinations (Table 2). The 8 patients consisted of 2 coronal, 2 lambdoid, 2 metopic, and 2 complex craniosynostoses. Bone fusion was also confirmed in intraoperative findings, and ultrasound was also performed directly on the periosteum after elevating the scalp flap. The mean age of patients undergoing the operation was 6.3 months (range 2–14 months).
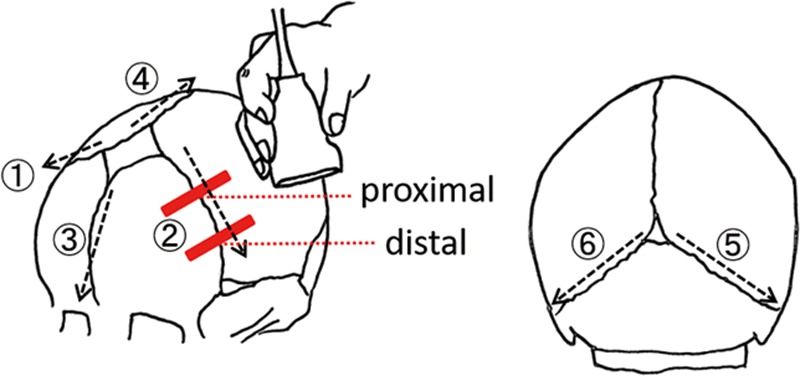
Table 1.
Patient Series of Deformational Plagiocephaly and Normal Infants
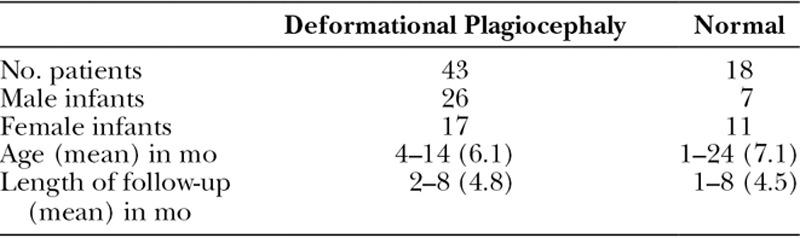
Table 2.
Patient Series of Craniosynostosis
All infants were assessed with cranial ultrasound of the sutures. The procedure was well-tolerated by all the infants, without any sedation. The bilateral coronal, metopic, sagittal, and bilateral lambdoid sutures were searched. Children with deformational plagiocephaly and normal skulls underwent ultrasound examinations at regular intervals after outpatient clinic. Children with craniosynostosis underwent ultrasound examination after preoperative CT diagnosis. Bone fusion was also confirmed in intraoperative findings, and ultrasound was also performed directly on the periosteum after elevating the scalp flap.
Echocardiographic Devices
Since the examinations took place in 2 hospitals, 2 echocardiographic instruments were used, and linear probes for observing the surface layer were used. Assessments using echocardiographic devices Venue 50 (GE Healthcare, Wuxi City, China) and NanoMaxx (SonoSite, Bothell, Wash.) were performed immediately after the clinical examination at Osaka Medical College hospital and Takatsuki hospital, respectively. Linear transducers of 16 and 10 MHz were used with the following parameters: field of view, 1.5 cm; depth of focus, 3 mm; gain, 80 dB. Gel was used as contact medium. All children were examined by the author to avoid interobserver variability.
MEASUREMENT AND EVALUATION METHODS
Measurement Index and Order
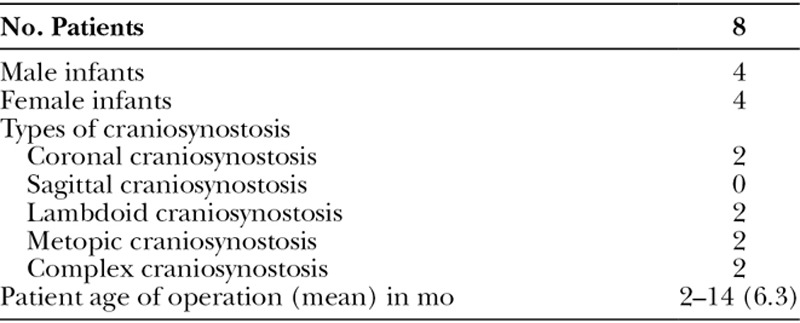
While observing with echocardiographic ultrasound, we focused on the following measurement indices and decided the observation order so that evaluation could be made more easily in a short time (Fig. 1).
Fig. 1.
The ultrasound probe is vertically placed on 2 trisected points of the suture line between the 2 fontanels (red lines). The examiner faces the front of the child’s head and observes the sutures in order of right coronal, left coronal, metopic, and sagittal sutures. The position of the child’s head is reversed only when observing the lambdoid sutures.
The child was seated on the mother’s knee and faced the examiner. First, the examiner confirmed the position of 6 cranial fontanels (anterior fontanel, posterior fontanel, sphenoid fontanels, and mastoid fontanels), and these fontanels were used as measurement indicators. It is faster to minimize changes in the patient’s posture and to examine from the sutures around the anterior fontanel which is easiest to identify. Therefore, the examination was begun in the order of the right coronal, left coronal, metopic, and sagittal suture. Only when observing the lambdoid suture, the direction of the patient’s seating was changed so that the child faced the mother’s chest.
Two-point Method
Furthermore, we have developed an evaluation method, which is easy to visualize (Fig. 2). Whether the suture was normal or fused was judged by using 2 observation points for each suture and was recorded in the table. If the suture was closed at 1 of the 2 points, a judgment was made that the suture was fused.
Fig. 2.
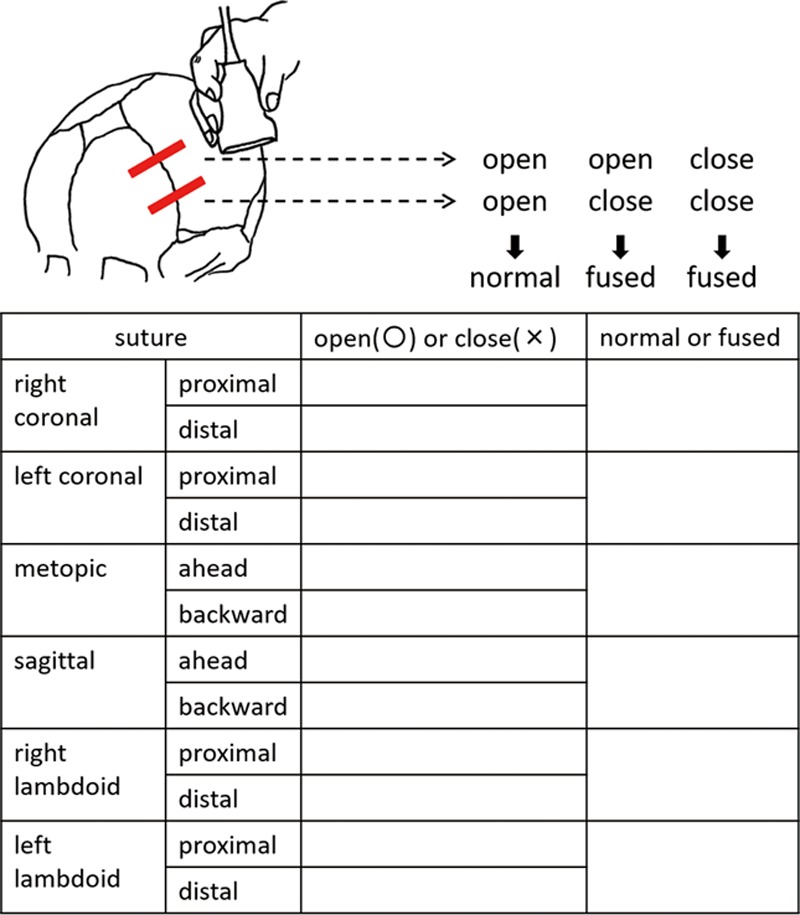
Each observation point is evaluated as open (○) or closed (×) and recorded. If only 1 of the 2 points is marked as closed, it is judged that the suture is fused. From this table, it can be immediately recognized whether the suture is normal or fused.
Measuring the Width of the Suture
The distance of the normal suture was measured for evaluation (Fig. 3). The line connecting the cortical epiphysis with a straight line was taken as the horizontal direction of the upper end. The straight line connecting the boundary between the cortex and medulla was taken as the horizontal direction of the lower end. The average value of the 2 widths (upper end and lower end) was taken as the horizontal width of the suture. The line connecting the vertical distance between the epiphyseal leanings was taken as the vertical direction of the upper end. The line connecting the cortex and medulla border in the vertical direction at the same leanings was taken as the vertical direction of the lower end. The average value of the 2 widths of the upper and lower ends was taken as the vertical width of the suture.
Fig. 3.
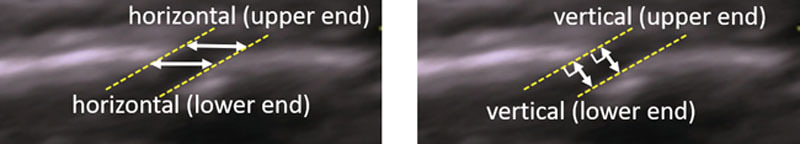
The average of the upper end and the lower end was taken as the horizontal and vertical width of the suture, respectively.
Ultrasounds Images of the Suture in Craniosynostosis
Craniosynostosis was diagnosed by CT examination before surgery (Table 2). Similarly, we investigated patency or closure of all sutures by echocardiographic examination. Sutures were also observed with echocardiography when the bones were exposed during surgery and were directly visible. Four patients underwent endoscopic resection without ultrasound assessment on the periosteum, and closure of the suture was confirmed only by direct observation.
Evaluation of Sensitivity
The ultrasonic examination results were compared with the CT examination as to whether the diagnostic sensitivity was sufficient by our proposed evaluation method (Table 3). The CT results were evaluated as true positive (TP) or true negative (TN). Sensitivity and specificity were calculated, respectively, using the common formula as follows: sensitivity = TP/[TP + false-negative (FN) results] and specificity = TN/[TN + false-positive (FP) results]. Positive predictive values and negative predictive values were calculated using TP/(TP + FP) and TN/(TN + FN).
Table 3.
Statistical Analysis of Ultrasonography in the Diagnosis of Craniosynostosis
RESULTS
Ultrasound Images of the Normal Sutures
In all the normal and deformational plagiocephaly cases, the patency of the sutures was clearly confirmed by echocardiographic ultrasound (Fig. 4). When each fontanel, especially the anterior fontanel, was widely patent, the entire suture lines could be identified from the fontanels at both ends of the suture. Normal cranial sutures were patent if no bridging was found and an anechoic gap was present throughout their entire length. The periosteum, cortical bone, medulla bone, and dural layer could also be identified. In the coronal sutures and lambdoid sutures, bone overlap phenomenon was not particularly regular. Sedation was unnecessary for the patients.
Fig. 4.
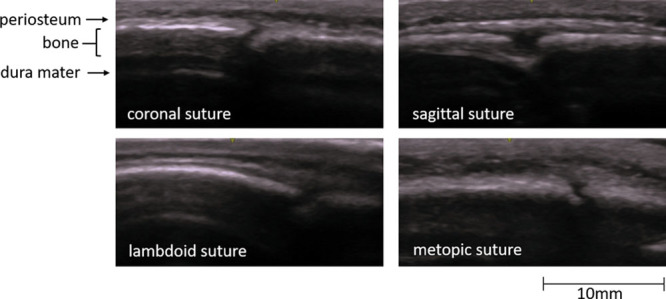
A 2-month-old girl with a normal cranium. All the sutures are clearly open. The sutures have no bridging image and an anechoic gap is present throughout the entire bone. The periosteum, cortical bone, medulla bone, and dura mater could also be identified.
Measuring the Width of the Suture
Furthermore, it was possible to observe suture width over time in normal and deformational plagiocephaly. The value of the normal suture was larger in the horizontal direction than in the vertical direction, and the distance in the horizontal direction could be measured easily (Fig. 5). Therefore, the width of the suture was defined as the horizontal direction with the greatest change depending on age.
Fig. 5.
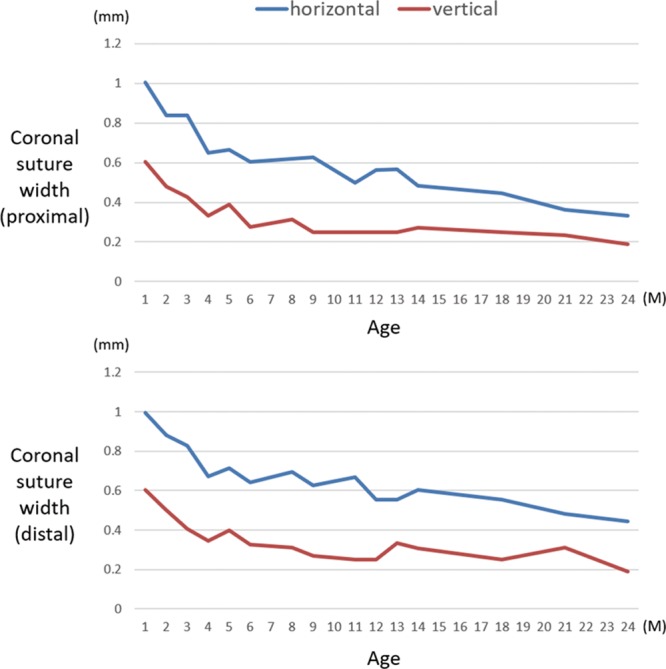
The average widths of the coronal sutures of the normal infants are shown. The values were larger in the horizontal direction than in the vertical direction at both the proximal and distal sites.
In normal and deformational plagiocephaly, the suture width was narrowing with age (Fig. 6). Among all the sutures, the coronal sutures tended to be narrow. The width of the suture exceeded the echocardiographic resolution even at 2 years of age at the cortical suture measurement point.
Fig. 6.
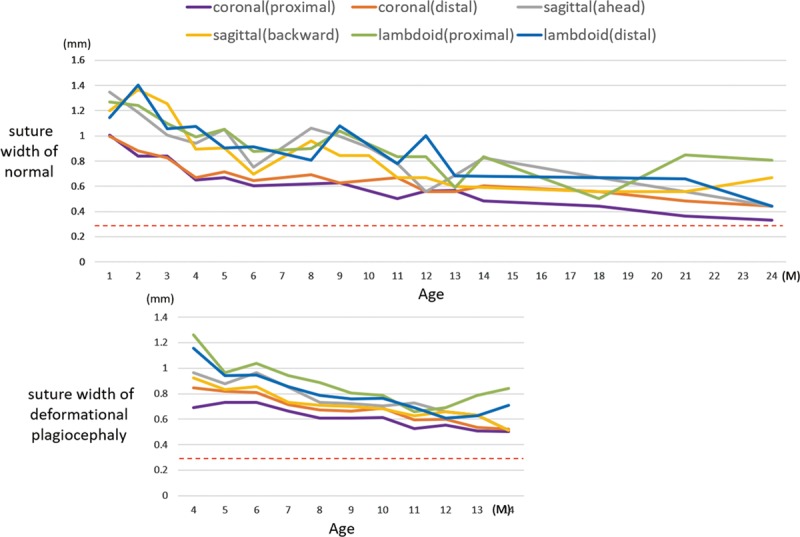
Suture widths of infants with normal skulls and deformational plagiocephaly are gradually narrowing with increasing age. The coronal sutures were the narrowest of all sutures. The widths of the sutures exceeded the echocardiographic resolution (dotted line) even at 2 years of age.
Ultrasound Images of the Sutures in Craniosynostosis
On the other hand, there was no anechoic gap in craniosynostosis and the bone was fused continuously (Fig. 7). The echocardiographic results of craniosynostosis were consistent with all the CT examinations. Results of CT findings, preoperative echogenic findings, intraoperative findings, and echogenic findings on periosteum did not differ. Furthermore, in 4 of 8 cases it was consistent with intraoperative findings and the results when performed directly on the periosteum. The table can be entered quickly in order of measurement and is easy to visualize later.
Fig. 7.
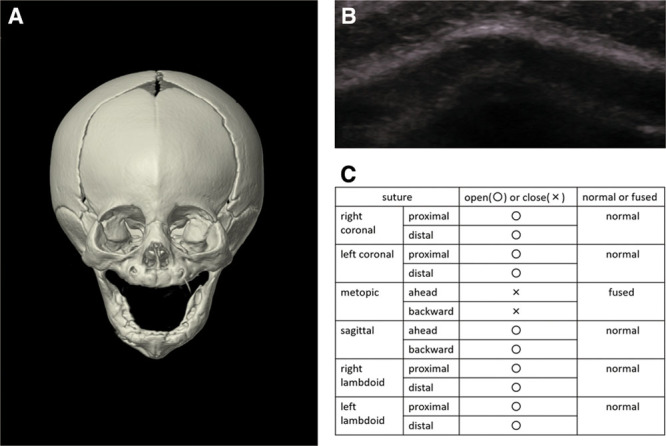
A 5-month-old girl with metopic craniosynostosis. A, Three-dimensional CT confirmed abnormal closure of the metopic suture. B, Ultrasound image showed disappearance of the hypoechogenic gap between the metopic bones. C, Ultrasound results are easy to visualize by filling out the table.
Two-point Method and Evaluation of Sensitivity
According to the evaluation method for the 2-point method that we devised, all the sutures could be inspected in about 2 minutes. Sensitivity was 100% and specificity was 95.1% in the evaluation of 2 points between sutures (Table 3). Two cases of deformational plagiocephaly seemed to have cross-links in the coronal suture at 11 months. However, when observations were made at 12 months, it was confirmed that both cases were clearly patent. One case of deformational plagiocephaly seemed to have cross-links in the coronal suture at 18 months. Because we could not follow the patient, we could not confirm the patency of the suture.
DISCUSSION
It is rare for a patient to receive a first-time diagnosis for craniosynostosis as an outpatient. Even when clinical findings do not lead to diagnosis, follow-up observations are necessary. Although x-ray examination is used as the first choice, it cannot be performed frequently due to the risk of irradiation. Although the 2015 guideline for craniosynostosis recommends repeating x-rays after 1 or 2 months, it says x-rays are not always reliable because of the very young age of the patient.23 In addition, x-rays have low sensitivity, varying from a high of 80% to a low of 60%.24 Although CT examination is high in sensitivity and specificity, it is not recommended for follow-up because of the increased risk of fetal cancer and childhood leukemia by radiation exposure and the sedation necessary.13,14 A 1-year-old infant is 10–15 times as likely as a 50-year-old adult to develop a malignancy from the same dose of radiation.12 The use of helical CT is increasing faster in children than in adults because of the advantage of a short exposure time. This leads to the temptation to use it for screening.12 In cases where cranial deformation is slight or almost no doubt of craniosynostosis, examination with radiation images is high risk. Ultrasound following outpatient examination can easily exclude craniosynostosis, and showing ultrasound findings to the patients’ mothers can give them a sense of security.
Our present studies showed that we could clearly judge the patency or closure of cranial sutures and measure their width. Ultrasound is easy to use because it can be performed over time and does not require sedation. Our 2-point method enabled us to perform examinations quickly—in as little as 2 minutes. There are no reports mentioning how to evaluate ultrasound. Sze et al.19 reported that the entire course of the bilateral lambdoid sutures from the posterior fontanel to the mastoid fontanelle was scanned if visible. Pogliani et al.22 reported that for older infants, the cooperation of parents with songs, toys, or stories was successful as well. It took >15 minutes to observe the whole suture lines as preliminary review before evaluating with the 2-point method. Our method was devised so that anyone can evaluate in a short time. First, the anterior fontanel which is widely patent can be easily found as an indicator. For the other fontanels, if we palpate or place the probe where they are likely to exist, we can identify them because they are wider than the suture width. Therefore, the suture line between the 2 fontanels can be determined. However, observing each suture along the line takes a considerable amount of time due to the infant’s movement. By evaluating the fixed points instead of a line, it was possible to shorten the inspection time. The reasons for making the evaluation by our 2-point method are as follows. One theory states that suture fusion will start from a certain point.25 Craniosynostosis begins in 1 area of a suture and fusion progresses along the suture line (Fig. 8). By observing the 2 fixed points over a period of time, it is possible to capture the partially fused suture at a certain time. If ≥3 points are measured, it will take a long time to evaluate all the sutures. If only 1 point is used, it may take time to diagnose the fusion.
Fig. 8.
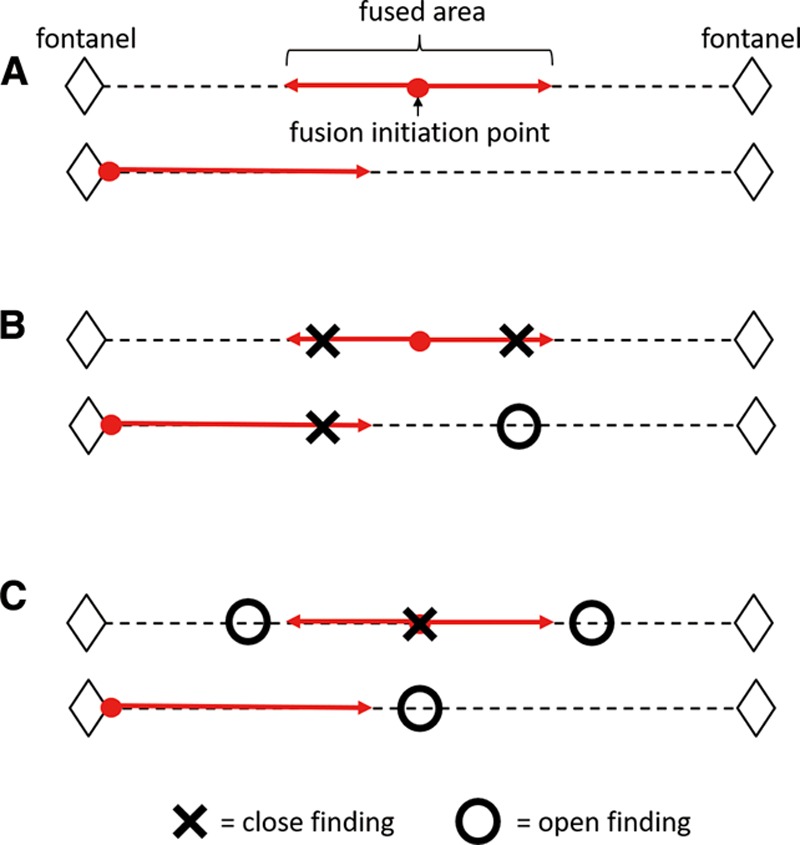
Points of fusion that can be captured by ultrasound in craniosynostosis. A, Fusion was localized, affecting only 1 region of the suture. B, It is possible to determine closure of the suture at a certain time by using the 2-point method. C, Evaluation of 3 points in each suture takes time. Evaluating only 1 point may also take time to diagnose suture fusion.
Also, our studies showed there was no rule to the direction and order of the 2 overlapping bones. These findings showed that bone overlap could not be considered a criterion for diagnosis. It was thought that the fractal figure would proceed early26 (Fig. 9). At birth, sutures are relatively wide and straight. During growth, they gradually wind and the adjacent bones intertwine with each other while maintaining a narrow width. It seems that the process of pattern formation is not clear due to extensive individual variation, and the age at which suture complexity increases is not clear. Therefore, it is not necessary to perform inspection along the suture line. For the ultrasound assessment, the complexity and narrowness of suture do not become much troublesome. Since only the evaluation of patency or closure is performed, the examiner will soon get accustomed to ultrasound.
Fig. 9.
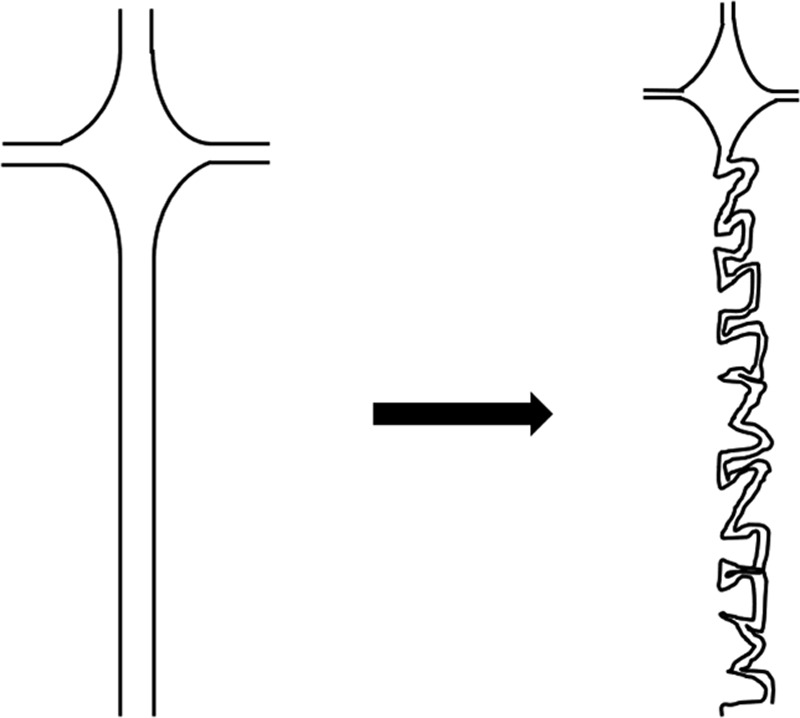
New bone suture is straight and relatively wide. During development, suture is thin, winding, and interdigitated. Increasing suture complexity is correlated with osteoclast activated at sutures as bone grows.
High levels for sensitivity and specificity of ultrasound are reported in the literature. Sze et al.19 reported that mean sensitivity and specificity of ultrasound in distinguishing a patent from a fused suture was 100% and 89%, respectively. Also, Pogliani et al.22 reported that ultrasound displayed a sensitivity of 100% and a specificity of 86%. The 2-point method we developed yielded nearly the same results. Sensitivity and specificity were sufficiently high at 100% and 95.1%, respectively. On the other hand, Regelsberger et al.21 reported x-rays led to misdiagnosis in >13% of the patients in their cohort. It would be undesirable to use x-ray examination with low sensitivity and the risk of exposure as the first-line choice of imaging. Due to the age restrictions for ultrasound examination of suture anatomy, according to a previous study it is difficult to interpret images for infants older than 12–13 months due to narrowing of the suture from <0.5 to 0.6 mm.20,21 In our study, ultrasound resolution exceeded the suture width by ≥0.3 mm, and it was possible to evaluate persons older than 24 months. One case of deformational plagiocephaly has not been followed up after a clear image was displayed at 18 months, and so it is considered that ultrasound evaluation is possible up to 18 months at the present stage.
Medina et al. reported a diagnostic approach algorithm for suspected craniosynostosis.19 While referring to their protocol, we developed the protocol for this study (Fig. 10). Performing ultrasound using this protocol can reduce x-ray exposure time.
Fig. 10.
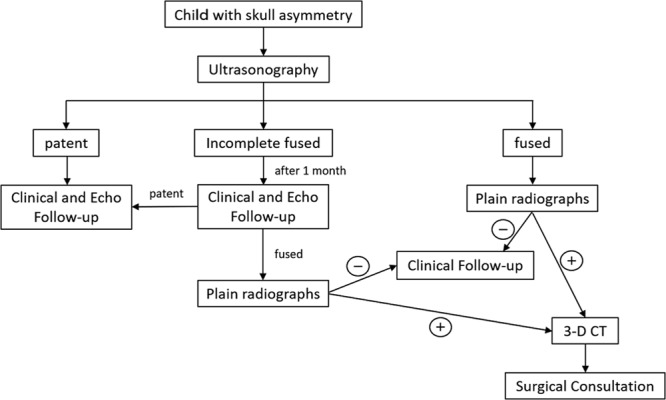
The diagnostic algorithm we proposed. Screening by ultrasonography can reduce the number of x-rays and CT scans. It is considered useful until 18 months of age at the present stage.
This study enabled us to recognize the opening or closing of the cranial suture. In addition, our 2-point method was considered to be sufficiently useful as a screening method. In the future, echocardiographic screening for cranial deformation can lead to early detection of craniosynostosis.
CONCLUSIONS
Screening by ultrasound examination for craniosynostosis is useful, and evaluation is possible in a shorter time by applying the 2-point method.
Footnotes
Published online 3 May 2019.
Presented at the 61st Annual Meeting of the Japan Society of Plastic and Reconstructive Surgery, April 11, 2018, Fukuoka, Japan.
Disclosure: The authors have no financial interest to declare in relation to the content of this article.
REFERENCES
- 1.Mulliken JB, Vander Woude DL, Hansen M, et al. Analysis of posterior plagiocephaly: deformational versus synostotic. Plast Reconstr Surg. 1999;103:371–380. [DOI] [PubMed] [Google Scholar]
- 2.Vles JS, Colla C, Weber JW, et al. Helmet versus nonhelmet treatment in nonsynostotic positional posterior plagiocephaly. J Craniofac Surg. 2000;11:572–574. [DOI] [PubMed] [Google Scholar]
- 3.Flannery AM, Tamber MS, Mazzola C, et al. Congress of neurological surgeons systematic review and evidence-based guidelines for the management of patients with positional plagiocephaly: executive summary. Neurosurgery. 2016;79:623–624. [DOI] [PubMed] [Google Scholar]
- 4.Han MH, Kang JY, Han HY, et al. Relationship between starting age of cranial-remolding-orthosis therapy and effectiveness of treatment in children with deformational plagiocephaly. Childs Nerv Syst. 2017;33:1349–1356. [DOI] [PubMed] [Google Scholar]
- 5.Seruya M, Oh AK, Taylor JH, et al. Helmet treatment of deformational plagiocephaly: the relationship between age at initiation and rate of correction. Plast Reconstr Surg. 2013;131:55e–61e. [DOI] [PubMed] [Google Scholar]
- 6.Panchal J, Uttchin V. Management of craniosynostosis. Plast Reconstr Surg. 2003;111:2032–2048; quiz 2049. [DOI] [PubMed] [Google Scholar]
- 7.Ursitti F, Fadda T, Papetti L, et al. Evaluation and management of nonsyndromic craniosynostosis. Acta Paediatr. 2011;100:1185–1194. [DOI] [PubMed] [Google Scholar]
- 8.Jimenez DF, Barone CM. Endoscopic techniques for craniosynostosis. Atlas Oral Maxillofac Surg Clin North Am. 2010;18:93–107. [DOI] [PubMed] [Google Scholar]
- 9.Rottgers SA, Lohani S, Proctor MR. Outcomes of endoscopic suturectomy with postoperative helmet therapy in bilateral coronal craniosynostosis. J Neurosurg Pediatr. 2016;18:281–286. [DOI] [PubMed] [Google Scholar]
- 10.Ridgway EB, Berry-Candelario J, Grondin RT, et al. The management of sagittal synostosis using endoscopic suturectomy and postoperative helmet therapy. J Neurosurg Pediatr. 2011;7:620–626. [DOI] [PubMed] [Google Scholar]
- 11.Berrington de Gonzalez A, Darby S. Risk of cancer from diagnostic X-rays: estimates for the UK and 14 other countries. Lancet. 2004;363:345–351. [DOI] [PubMed] [Google Scholar]
- 12.Hall EJ. Lessons we have learned from our children: cancer risks from diagnostic radiology. Pediatr Radiol. 2002;32:700–706. [DOI] [PubMed] [Google Scholar]
- 13.Brenner D, Elliston C, Hall E, et al. Estimated risks of radiation-induced fatal cancer from pediatric CT. AJR Am J Roentgenol. 2001;176:289–296. [DOI] [PubMed] [Google Scholar]
- 14.Infante-Rivard C, Mathonnet G, Sinnett D. Risk of childhood leukemia associated with diagnostic irradiation and polymorphisms in DNA repair genes. Environ Health Perspect. 2000;108:495–498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Grant EG, White EM. Pediatric neurosonography. J Child Neurol. 1986;1:319–337. [DOI] [PubMed] [Google Scholar]
- 16.Gupta N, Grover H, Bansal I, et al. Neonatal cranial sonography: ultrasound findings in neonatal meningitis-a pictorial review. Quant Imaging Med Surg. 2017;7:123–131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gupta P, Sodhi KS, Saxena AK, et al. Neonatal cranial sonography: a concise review for clinicians. J Pediatr Neurosci. 2016;11:7–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Soboleski D, Mussari B, McCloskey D, et al. High-resolution sonography of the abnormal cranial suture. Pediatr Radiol. 1998;28:79–82. [DOI] [PubMed] [Google Scholar]
- 19.Sze RW, Parisi MT, Sidhu M, et al. Ultrasound screening of the lambdoid suture in the child with posterior plagiocephaly. Pediatr Radiol. 2003;33:630–636. [DOI] [PubMed] [Google Scholar]
- 20.Regelsberger J, Delling G, Helmke K, et al. Ultrasound in the diagnosis of craniosynostosis. J Craniofac Surg. 2006;17:623–625; discussion 626. [DOI] [PubMed] [Google Scholar]
- 21.Regelsberger J, Delling G, Tsokos M, et al. High-frequency ultrasound confirmation of positional plagiocephaly. J Neurosurg. 2006;105(suppl):413–417. [DOI] [PubMed] [Google Scholar]
- 22.Pogliani L, Zuccotti GV, Furlanetto M, et al. Cranial ultrasound is a reliable first step imaging in children with suspected craniosynostosis. Childs Nerv Syst. 2017;33:1545–1552. [DOI] [PubMed] [Google Scholar]
- 23.Mathijssen IM. Guideline for care of patients with the diagnoses of craniosynostosis: working group on craniosynostosis. J Craniofac Surg. 2015;26:1735–1807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Vinocur DN, Medina LS. Imaging in the evaluation of children with suspected craniosynostosis. Pediatrics. 2009;19:43–52. [Google Scholar]
- 25.Albright AL, Byrd RP. Suture pathology in craniosynostosis. J Neurosurg. 1981;54:384–387. [DOI] [PubMed] [Google Scholar]
- 26.Ieva AD. Takashi M. The fractal geometry of the brain. In: Fractality of Cranial Sutures. 2016:New York: Springer; 157–170.Chapter 10. [Google Scholar]


