Abstract
Background:
Blepharoplasty is one of the most common procedures performed. To achieve optimal results in periorbital rejuvenation, a systematic approach to patients that addresses all the problems in the periorbital region is important. The aim of this study is to analyze blepharoplasty patients according to preoperative deformities and postoperative results and to create a basic algorithm for periorbital aesthetic surgery.
Methods:
Patients who underwent periorbital aesthetic surgery were examined retrospectively. Patients’ medical records and preoperative and postoperative photographs were analyzed. Preoperative and postoperative photographs were analyzed for 6 main criteria: brow position, blepharoptosis, canthal tilt, excess skin or deficiencies, excess subcutaneous tissue or deficiencies, and periorbital skin rhytides. After the anatomical analyses, researchers rated the results as optimal or suboptimal.
Results:
In total, 176 patients’ medical records were analyzed. Among them, 154 were women and 22 were men. The mean age was 43.8 years. No comorbid situation was detected in 133 of these patients. The postoperative result was evaluated as suboptimal in 151 patients (86%) and optimal in 25 patients (14%). An algorithm was proposed for the systematic evaluation of periorbital surgery patients to achieve satisfactory results.
Conclusions:
A simple 6-step checklist is designed to define periorbital deformities and to achieve the optimal youthful appearance.
INTRODUCTION
Eyelid surgery was the third most common cosmetic surgical procedure performed in 2017 after breast augmentation and liposuction, according to the International Society of Aesthetic Plastic Surgeons.1 This procedure is in the armamentarium of 92% of plastic surgeons and representing the highest percentage among other cosmetic procedures.1 Many surgeons classify eyelid surgery as “easy to do” or “a basic operation.” This attitude diminishes the attention needed to achieve an optimal result. A detailed preoperative evaluation is a key to success in obtaining optimal results for optimal youthful appearance. It is imperative for surgeons to approach the patient with a systematic way to determine the patients’ needs. Taking a systematic approach in every operation decreases the chances of missing certain problems and deformities.2,3 In recent years, blepharoplasty operations evolved into periorbital aesthetic surgery concept to achieve a better, younger, and more dynamic look. It is not possible to have a dynamic look with just an excision of the excess upper lid skin and neglecting brow ptosis or a negative canthal tilt. The aim of this study is to analyze patients who underwent eyelid surgery, to present suboptimal results, to determine the causes of suboptimal results, and to create a basic and reproducible algorithm for periorbital aesthetic surgery.
METHODS
Patients who underwent periorbital aesthetic surgery between May 2015 and March 2018 in 2 different clinics were examined retrospectively. Patients’ medical records and their preoperative and postoperative 6-month photographs were analyzed. Patients’ age, sex, comorbidities, anesthesia type, operations underwent, and postoperative complications were noted. Preoperative and postoperative photographs were analyzed for 6 main criteria: (1) brow position, (2) blepharoptosis, (3) canthal tilt, (4) excess skin/deficiency, (5) excess subcutaneous tissue/deficiency, and (6) periorbital skin rhytides. Brow position was accepted as normal if the brow was above the supraorbital rim in females and on the supraorbital rim in males. Blepharoptosis was accepted as mild if the upper lid margin covers 2 mm of the limbus, moderate if it covers 3–4 mm, and severe if it covers >4 mm. Canthal tilt was accepted as neutral if both the canthus was on the same horizontal level, positive if the lateral canthus was higher, and negative if the lateral canthus was positioned lower than medial canthus. After the anatomical and overall appearance analyses, researchers rated the results as optimal or suboptimal. If 4 or <4 criteria were addressed/corrected in the patients, the results were accepted as suboptimal. If >4 criteria were in aesthetic standards, results were accepted as optimal. All procedures performed in this study were in accordance with the ethical standards of the institutional research committee and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards. All participants signed a written informed consent.
RESULTS
In this retrospective study, 176 patients’ medical records and photographs were analyzed. Among them, 154 were women and 22 were men. The mean age was 43.8 years (range 19–84). No comorbid situation was detected in 133 of these patients. Hypertension was the leading comorbidity that was seen with 18 patients. Eleven patients have diabetes mellitus and 7 have lung disease. Seven patients have >1 comorbid disease. Sixty-seven patients were smokers, 24 of whom were smoking >1 package/d. The operations of 137 patients were performed under nerve blocks and local anesthesia, whereas 25 operations were performed under general anesthesia and 14 with sedation and local anesthesia. The most common complication was asymmetry, as seen in 47 patients (26%). Chemosis and allergic reactions were seen in 19 patients, scleral show in 6 patients, corneal abrasion in 2 patients, and permanent skin discoloration in 1 patient. Analyzed preoperative and postoperative photographs were standard in all patients. Each surgeon used his/her personal same camera routinely. The photographs were taken from the same distance with flashlight. Full-face and close-up frontal, oblique, and lateral views with eyes open and closed were evaluated. The postoperative result was evaluated as suboptimal in 151 patients (86%) and optimal in only 25 patients (14%). An algorithm was proposed for a systematic evaluation of periorbital surgery patients to achieve optimal results (Figs. 1–6).
Fig. 1.
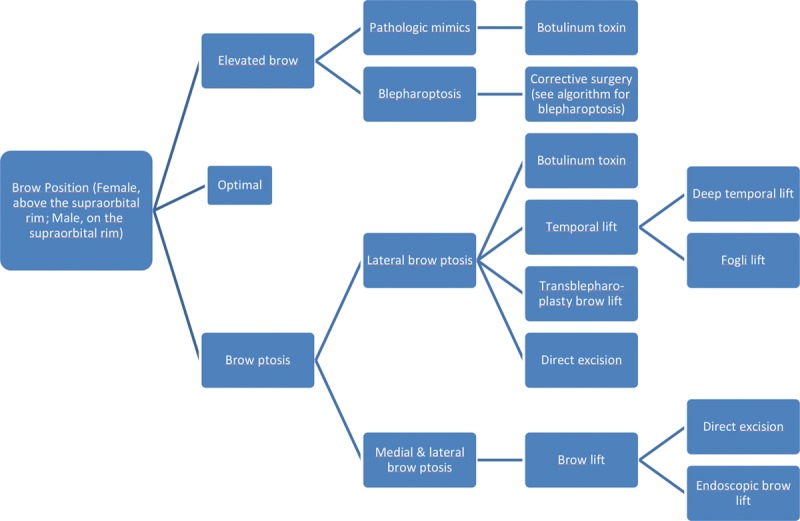
First step: brow position.
Fig. 6.
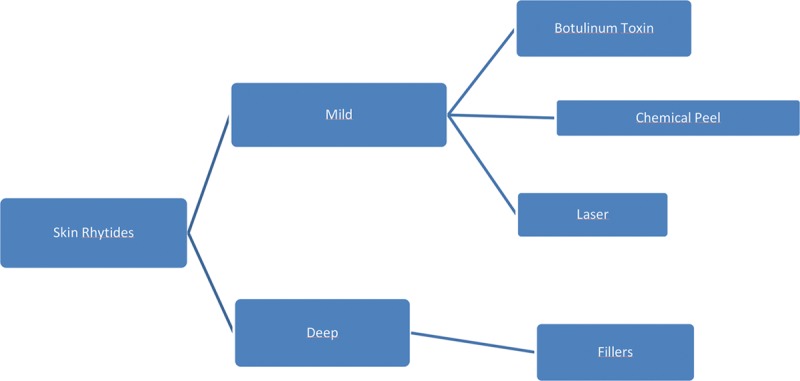
Sixth step: skin rhytides.
Fig. 2.
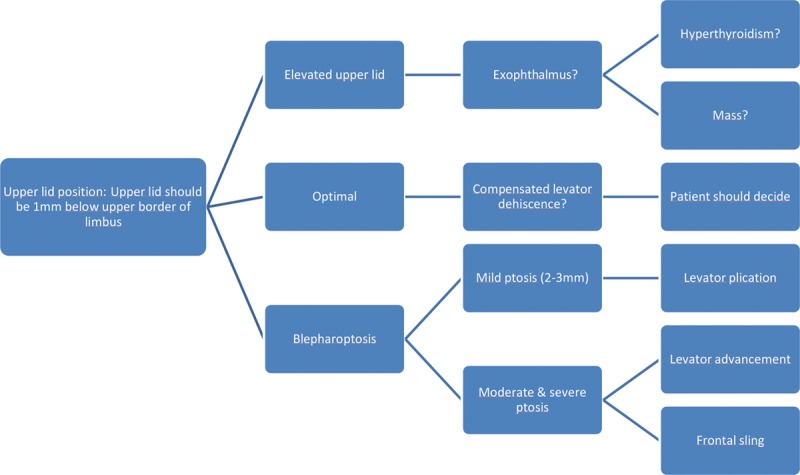
Second step: upper lid position.
Fig. 3.
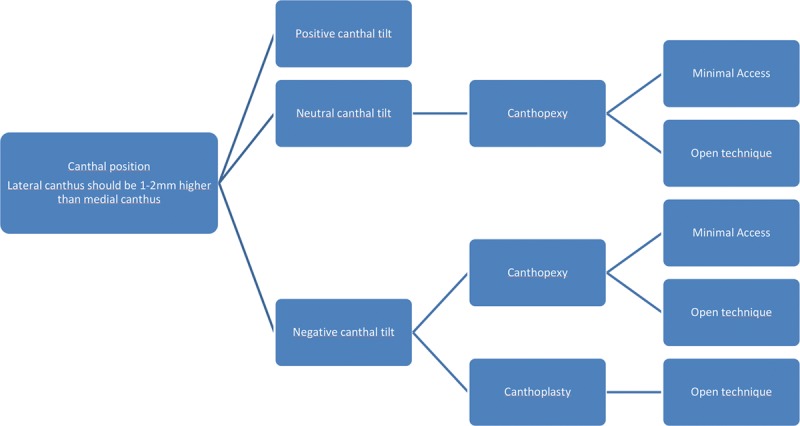
Third step: canthal position.
Fig. 4.
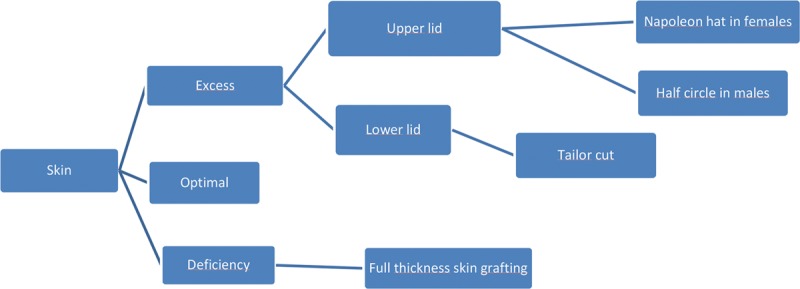
Fourth step: skin.
Fig. 5.
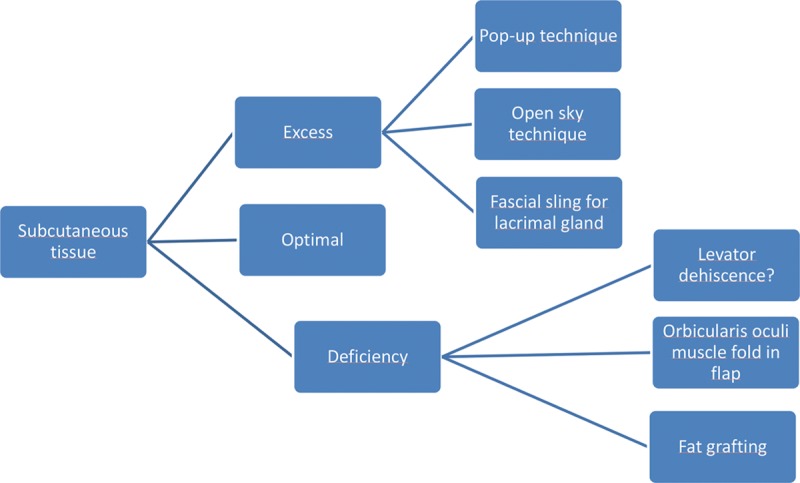
Fifth step: subcutaneous tissue.
CASE SAMPLES
Case 1
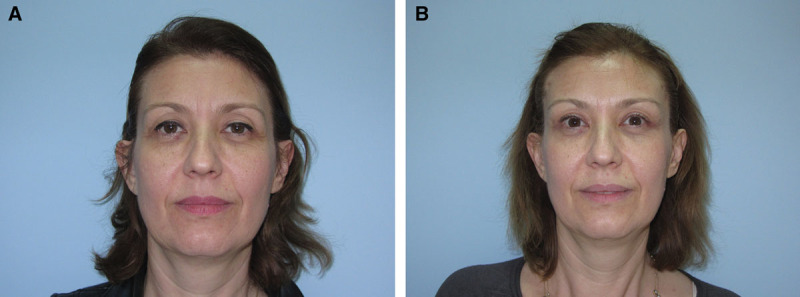
A 43-year-old woman applied with a desire to get rid of her tired look. Preoperative examination only addressed levator dehiscence, excess skin on upper and lower lids, and fat pads in lower lids. She was operated on under a nerve block and local anesthesia. Levator reattachment was performed on both eyes. Skin excision was performed in both the upper and lower eyelids. Fat pad redistribution was done in the upper eyelids, and fat pad excision was done in the lower eyelids. No interventions were conducted for brow positions or canthal tilt. The retrospective evaluation of preoperative photographs revealed brow asymmetry: the left brow was positioned lower than the right brow. Mild blepharoptosis was seen in both eyes: the upper lid covers 2–3 mm of the limbus. A neutral canthal tilt was seen in both eyes. Excess skin and subcutaneous tissue was evident in the lower eyelids, whereas skin and subcutaneous tissue deficiency was seen in the upper eyelids (Fig. 7A). In the postoperative photograph evaluation, left brow ptosis was evident, causing asymmetry. Blepharoptosis was corrected in both eyes. A neutral canthal tilt was observed to cause a tired look, and minimal scleral show was evident, especially in the lateral parts. Skin and soft-tissue balance of lower eyelids was evaluated as good. Hollowing of the upper eyelids was corrected with levator reattachment. The left upper eyelid had more skin due to the asymmetry of the brow positions, though discoloration of the lower eyelids was the main concern of the patient (Fig. 7B). The result was evaluated as suboptimal.
Fig. 7.
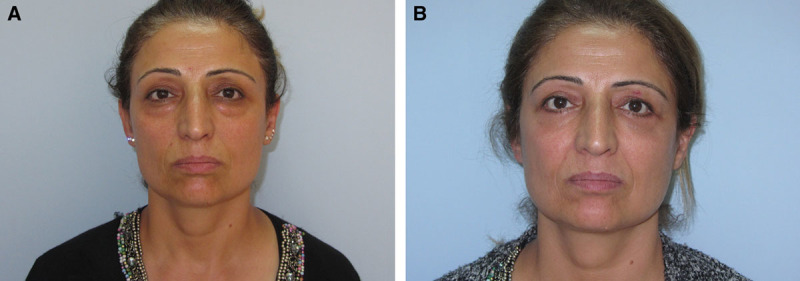
Case 1. A, A 43-year-old patient underwent bilateral levator reattachment and skin excision. B, The postoperative picture reveals left brow ptosis, a neutral canthal tilt, and scleral show.
Case 2
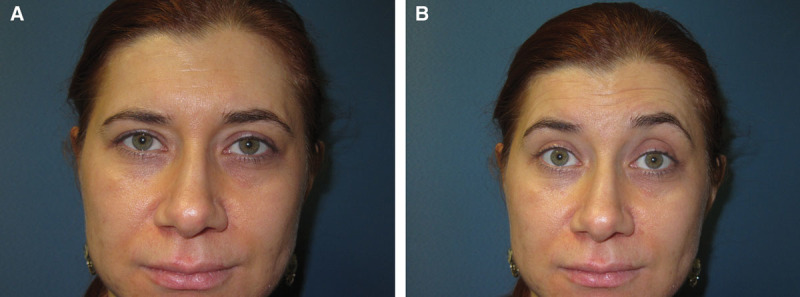
A 52-year-old male patient who was a heavy smoker (2 packages/d) applied with a complaint of looking older than his actual age. In preoperative examination, brow ptosis and excess skin in upper and lower lids were revealed. There was a laxity in snap-back test of lower lids. He was operated on under sedation and local anesthesia. Brow lifting was achieved with a seagull-type middle forehead skin excision. A skin, orbicularis oculi, and fat excision were done in the upper eyelids, and a skin excision was done in the lower eyelids. No interventions were done for canthal positions and blepharoptosis. No complication was seen related to smoking. The retrospective evaluation of preoperative photographs showed severe bilateral brow ptosis, no blepharoptosis, a neutral canthal tilt, and excess skin in both the upper and lower eyelids (Fig. 8A). Meanwhile, an evaluation of postoperative photographs show brow ptosis to be corrected, no blepharoptosis, a neutral canthal tilt causing a tired look, and no skin excess in either eyelids. Scleral show was evident in the left eye, causing asymmetry (Fig. 8B). The overall result was evaluated as suboptimal.
Fig. 8.
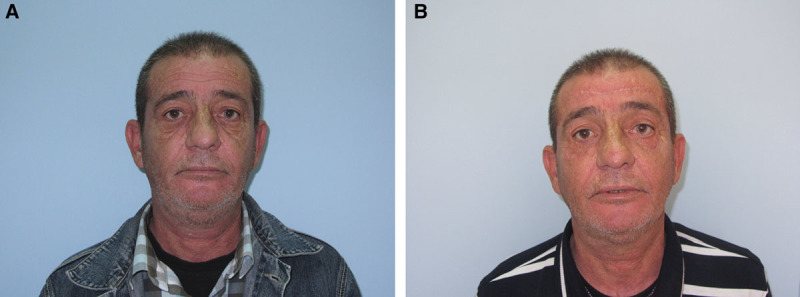
Case 2. A, A 52-year-old patient underwent direct excision brow lifting and a skin and subcutaneous excision of the upper and lower eyelids. B, Postoperatively, a neutral canthal tilt and scleral show are detected.
Case 3
A 47-year-old female patient applied with droopy eyelids. Preoperatively, brow ptosis, blepharoptosis, and excess skin in upper eyelids were examined. She was operated on under local anesthesia and nerve block. Brow lifting was achieved with a deep temporal lift. Blepharoptosis was corrected with levator reattachment. A skin excision was made in the upper eyelids, and the orbicularis oculi muscle fold-in flap was used to increase the soft-tissue support of the upper eyelids. Nothing was done for the canthal position and lower eyelid. The retrospective evaluation of preoperative photographs showed bilateral brow ptosis, especially in the lateral parts; a moderate degree of bilateral blepharoptosis (upper eyelid covers 4 mm of the limbus); a positive canthal tilt; excess skin in both the upper and lower eyelids; soft-tissue deficiency in the upper eyelids; and periorbital rhytides (Fig. 9A). A postoperative photograph evaluation showed brow ptosis to be corrected, blepharoptosis to be corrected, a positive canthal tilt, and good skin and soft-tissue balance in the upper eyelids, but excess skin in the lower eyelids and periorbital rhytides were still present (Fig. 9B). The overall result was evaluated as suboptimal.
Fig. 9.
Case 3. A, A 47-year-old female patient with deep temporal brow lifting, levator reattachment, a skin excision on the upper eyelid, and an orbicularis oculi muscle fold-in flap. B, A postoperative evaluation revealed excess skin in the lower eyelids, and periorbital rhytides were still present.
DISCUSSION
Upper eyelid blepharoplasty is one of the most common aesthetic procedures done by plastic surgeons.4,5 The overall patient satisfaction is high in these operations.6 The critical change in the gaze with only an excision of excess skin plays an important role in this satisfaction rate. However, to achieve an optimal youthful appearance around the periorbital region, the upper and lower lids, together with the brow and periorbital skin, and periorbital relation with frontal and cheek region should be evaluated. Addressing only one of the components, concentrating just the patient complaints leads to suboptimal surgical results. Analyzing the periorbital area systematically will reduce the rate of ignoring other problems that can cause suboptimal results. A systematic approach with predefined algorithms is a proven way to generate optimal results in aesthetic operations, such as lower blepharoplasty and breast augmentation.2,3,7 In this article, we analyzed the periorbital area in 6 steps and defined basic approaches for each problem.
The first step is the brow position. The optimal brow position is different for males and females. Brow position should be above the supraorbital rim in women, whereas it should be on the supraorbital rims for men.8 If the patient has elevated brows, attention should be paid to underlying blepharoptosis. Mild blepharoptosis can be compensated for by the frontalis muscle, which can cause excess wrinkling of the forehead and elevated brows. The surgeon should examine the dynamic brow motions to understand better the deformities. Some asymmetries can only be seen with brow movement (Fig. 10A, B). In this patient, a compensated levator dehiscence in the left eye resulted in the left frontalis muscle being overworked. Such deformities can be easily neglected if an appropriate physical examination is not performed. Pathological mimics can be considered as another cause of elevated brows. The botulinum toxin is the best way to block an overworked frontalis muscle. Although it is an expensive and temporary treatment, patient satisfaction rates are quite high. Brow ptosis is a problem harder to solve. Lateral brow ptosis is more common, and the botulinum toxin can solve this problem if the lateral part of the frontalis muscle can elevate the lateral part of the brow effectively. Surgical options for lateral brow ptosis include a temporal incision brow lift, transblepharoplasty brow lift, and direct skin excision.9–12 The deep temporal lift and Fogli lift are commonly used methods, as they are easy and effective. Transblepharoplasty brow lifting is recommended, especially for bold males and patients who do not want extra incisions. A direct skin excision brow lift is suitable for older patients with excess frontal wrinkles and for patients who are not suitable for general anesthesia because of comorbidities. Endoscopic brow lifting can be preferred for correcting medial brow ptosis. The seagull-pattern skin excision can solve both medial and lateral brow ptosis, though the technical details of these operations are beyond the objective of this study.
Fig. 10.
Dynamic brow examination. A and B, With dynamic brow motion, overworking of the left frontalis muscle is revealed.
The second step is the evaluation of the upper eyelid position according to the limbus. The upper eyelid covers 1 mm of the upper part of the limbus in a normal position.13 Hyperthyroidism or a mass causing exophthalmos should be kept in mind in case of an elevated upper eyelid. A further investigation of hormone levels and malignancies should be performed. Compensated levator dehiscence can be unnoticed if the surgeon does not perform a full analysis. As seen in Fig. 10A, a slight change in the supratarsal fold is a clue for levator dehiscence. When the patient elevates their brows intentionally, the difference between both eyes becomes evident (Fig. 10B). In such cases, patients should choose correction of the compensated levator dehiscence, because reattachment of the levator aponeurosis may result in ptosis of the unaffected eye or brow, as explained by Hering’s law.14 Levator plication is efficient if the patient has mild ptosis and good levator function. In moderate to severe ptosis cases, levator muscle advancement procedures solve the problem often. Delicate surgical skills and a good understanding of levator muscle anatomy are needed for these cases. The frontal sling procedure is only indicated if the levator muscle has no function.15
The third step is evaluating the canthal position. A positive canthal tilt is essential for an attractive and younger look.16 The lateral canthus should be located at least 2 mm higher than the medial canthus on the horizontal axis. The open technique for canthopexy and canthoplasty can be preferred if it is combined with an upper blepharoplasty operation. Minimal access canthopexy is sufficient in most cases with a negative canthal tilt.
Subcutaneous tissue should be evaluated in the fourth step. Excess subcutaneous tissue should be reduced carefully. Two basic techniques used for subcutaneous fat removal are pop-up and the open-sky technique. If the septum is incised from end to end for excision of fat pads, it is called open-sky technique. If the fat pads excised from small stab incisions, it is called pop-up technique. The open-sky technique is preferred for the better harmony of fat removal. In cases with a hanging lacrimal gland, a fascial sling for repositioning the gland should be performed.17 Levator dehiscence should be questioned in patients with subcutaneous tissue deficiency. Subcutaneous tissue can be retracted with levator dehiscence, and reattaching the levator aponeurosis can solve this problem. The orbicularis oculi muscle fold-in flaps may be a good alternative for replacing deficient subcutaneous tissue. If these techniques are insufficient, fat grafting, especially from the mons pubis, should be performed. Lower lid subcutaneous tissue should also be reduced minimally. Instead of excision of the fats in lower lid compartments, reorganizing them to blur the lid-cheek junction should be considered. Fat grafting can be helpful to correct tear trough deformity. In aging faces, midface fat pads should be suspended to support lower lid.
Evaluating the skin is the fifth step. Excess skin of the upper lid can be excised with a Napoleon hat-style incision in females and a half-circle style incision in males.9 A lower lid skin excision should be done conservatively, and the tailor-cut technique is appropriate. If there is skin excess, subciliary incision with skin-muscle flap is preferred, but if there is only subcutaneous fat excess a transconjunctival approach was preferred for fat pad removal. Full-thickness skin grafting is the primary treatment method for skin deficiency, which is a highly rare situation in primary blepharoplasty cases. The contralateral eyelid or preauricular region is the choice of donor areas for skin grafting.
The last step is to evaluate skin rhytides in the periorbital region. Botulinum toxin injections can lower the appearance of skin rhytides and improve surgical periorbital operations. Skin resurfacing with a carbon dioxide laser or a chemical peel improves the skin’s quality; therefore, it is offered to patients in conjunction with surgery.
The anatomy of the periorbital region and surgical procedures to correct pathologies of this region are well defined in the literature. A simple 6-step algorithm is designed to address all the pathologies and to achieve optimal results. In the presented case series, no detailed preoperative examination was performed, thus the postoperative results were suboptimal. The aim of this study is creating a basic, easily performed algorithm to evaluate the periorbital area thus avoid missing out any deformities that can end up with suboptimal results. In this study, only physician’s evaluated the surgical results. Patient satisfaction rates and patient-recorded outcomes can be integrated to this study design to further evaluate suboptimal results.
Footnotes
Published online 16 May 2019.
Disclosure: The authors report no conflicts of interest. The authors alone are responsible for the content and writing of this article.
REFERENCES
- 1.International Society of Aesthetic Plastic Surgery. ISAPS International Survey on Aesthetic/Cosmetic Procedures Performed in 2017. Available at https://www.isaps.org/wp-content/uploads/2018/10/ISAPS_2017_International_Study_Cosmetic_Procedures.pdf. Accessed November 11, 2018.
- 2.Rohrich RJ, Ghavami A, Mojallal A. The five-step lower blepharoplasty: blending the eyelid-cheek junction. Plast Reconstr Surg. 2011;128:775–783. [DOI] [PubMed] [Google Scholar]
- 3.Tebbetts JB, Adams WP. Five critical decisions in breast augmentation using five measurements in 5 minutes: the high five decision support process. Plast Reconstr Surg. 2005;116:2005–2016. [PubMed] [Google Scholar]
- 4.Koulaxouzidis G, Momeni A, Simunovic F, et al. Aesthetic surgery performed by plastic surgery residents: an analysis of safety and patient satisfaction. Ann Plast Surg. 2014;73:696–700. [DOI] [PubMed] [Google Scholar]
- 5.American Society of Plastic Surgeons. New Statistics Reveal the Shape of Plastic Surgery. Available at https://www.plasticsurgery.org/news/press-releases/new-statistics-reveal-the-shape-of-plastic-surgery. Accessed November 11, 2018.
- 6.Herruer JM, Prins JB, van Heerbeek N, et al. Patient-reported outcome measurement in upper blepharoplasty: how to measure what the patient sees. J Plast Reconstr Aesthet Surg. 2018;71:1346–1351. [DOI] [PubMed] [Google Scholar]
- 7.Rohrich RJ, Villanueva NL, Afrooz PN. Refinements in upper blepharoplasty: the five-step technique. Plast Reconstr Surg. 2018;141:1144–1146. [DOI] [PubMed] [Google Scholar]
- 8.Codner MA, Kikkawa DO, Korn BS, Pacella SJ. Blepharoplasty and brow lift. Plast Reconstr Surg. 2010;126:1e–17e. [DOI] [PubMed] [Google Scholar]
- 9.Zoumalan CI, Roostaeian J. Simplifying blepharoplasty. Plast Reconstr Surg. 2016;137:196e–213e. [DOI] [PubMed] [Google Scholar]
- 10.Graham DW, Heller J, Kurkjian TJ, et al. Brow lift in facial rejuvenation: a systematic literature review of open versus endoscopic techniques. Plast Reconstr Surg. 2011;128:335e–341e. [DOI] [PubMed] [Google Scholar]
- 11.Fogli AL. Temporal lift by galeapexy: a review of 270 cases. Aesthetic Plast Surg. 2003;27:159–65; discussion 166. [DOI] [PubMed] [Google Scholar]
- 12.Tyers AG. Brow lift via the direct and trans-blepharoplasty approaches. Orbit. 2006;25:261–265. [DOI] [PubMed] [Google Scholar]
- 13.Drolet BC, Sullivan PK. Evidence-based medicine: blepharoplasty. Plast Reconstr Surg. 2014;133:1195–1205. [DOI] [PubMed] [Google Scholar]
- 14.Erb MH, Kersten RC, Yip CC, et al. Effect of unilateral blepharoptosis repair on contralateral eyelid position. Ophthalmic Plast Reconstr Surg. 2004;20:418–422. [DOI] [PubMed] [Google Scholar]
- 15.Gürdal C, Erdener U, Orhan M, et al. Autogenous versus allograft fascia lata in frontal sling surgery–long-term results. Eur J Ophthalmol. 2003;13:202–206. [DOI] [PubMed] [Google Scholar]
- 16.Tepper OM, Steinbrech D, Howell MH, et al. A retrospective review of patients undergoing lateral canthoplasty techniques to manage existing or potential lower eyelid malposition: identification of seven key preoperative findings. Plast Reconstr Surg. 2015;136:40–49. [DOI] [PubMed] [Google Scholar]
- 17.Friedhofer H, Orel M, Saito FL, et al. Lacrimal gland prolapse: management during aesthetic blepharoplasty: review of the literature and case reports. Aesthetic Plast Surg. 2009;33:647–653. [DOI] [PubMed] [Google Scholar]


