Summary:
The risk for minor local complications for abdominoplasty remains high despite advances in strategies in recent years. The most common complication is the formation of seroma with reported rates ranging from 15% to 40%. The use of incisional negative-pressure wound therapy (iNPWT) on closed surgical sites has been shown to decrease the infection, dehiscence, and seroma rates. Thus, this article aims to determine whether an iNPWT dressing, Prevena Plus, is able to reduce postoperative drainage and seroma formation in patients who undergo abdominoplasty. Sixteen consecutive patients who underwent abdominoplasty by a single surgeon were dressed with standard dressings and iNPWT dressings. Total drain output, day of drain removal, and adverse events were compared between cohorts with a minimum follow-up of 6 months. The iNPWT group demonstrated a significantly less amount of fluid drainage with a mean total fluid output of 370 ± 275 ml compared to 1269 ± 436 ml mean total drainage from controls (P < 0.001). Time before removal of both drains was almost halved in the iNPWT group with an average of 5.3 ± 1.6 days, which was significantly less than the average time of 10.6 ± 2.9 days seen in control patients (P < 0.001). No observed adverse events were recorded in either group. Our findings show that iNPWT for a closed abdominoplasty incision decreases the rate of postoperative fluid accumulation and results in earlier drain removal.
BACKGROUND
Abdominoplasty remains one of the most popular plastic surgical procedures performed worldwide.1 Despite the adoption of less radical techniques, the procedure is still considered high risk.2 Although there has been a steady decline in serious life-threatening complications,3,4 local complications such as seroma and infection are reported in 15–40% of patients.3–5
The introduction of negative-pressure wound therapy (NPWT) has revolutionized the management of both acute and chronic wounds and provided a simpler and more convenient way of initiating and hastening the wound healing process. In recent years, NPWT has been trialed in closed incisional wounds.6–13 Biomechanical studies on closed incisional negative-pressure wound therapy (iNPWT) have shown similar pathophysiologic changes seen in an open wound NPWT: increased blood flow and decreased edema, decreased lateral and shear stress at the suture lines, and increased lymphatic clearance with the reduction in seroma/hematoma.14 Many surgical specialties are now utilizing iNPWT dressings on closed wound areas on patients considered as high risk for complications with positive results.13
This study aimed to determine whether the use of iNPWT dressing in patients undergoing an abdominoplasty can reduce postoperative drainage output and adverse events compared to standard postoperative dressings.
METHODS
Patient Selection
A prospective consecutive cohort study was undertaken at 2 centers in Sydney, Australia (Macquarie University Hospital and Kareena Private Hospital). All patients who underwent abdominoplasty from February to October 2017 performed by a single surgeon were included. Patients were dressed with either standard postoperative dressings using 2-octyl cyanoacrylate skin adhesive (DERMABOND PRINEO Skin Closure System, Johnson and Johnson, Puerto Rico) or using an iNPWT system (Prevena Plus Incisional Management System, KCI Acelity, San Antonio, Tex.). Patient demographics, total drain output, day of drain removal, and postoperative outcomes were recorded and compared.
Procedure Technique and Dressing Application
A standard abdominoplasty procedure was undertaken in all patient utilizing liposuction on the flanks and not the abdominoplasty flap. Two standard 15FR suction drains were inserted before closure sited laterally on each side. Standard layered closure of the Scarpa’s and skin layers was done using 3-0 and 4-0 resorbable monofilament sutures (MONOCRYL and STRATAFIX, Ethicon).
Seven consecutive patients were dressed with skin adhesive and tapes (Prineo), whereas the remaining 9 consecutive patients were dressed with the iNPWT Prevena System encompassing the whole incision (Fig. 1). This dressing delivered the negative pressure at 125 mm Hg and was kept in place for 7 days and removed thereafter.
Fig. 1.
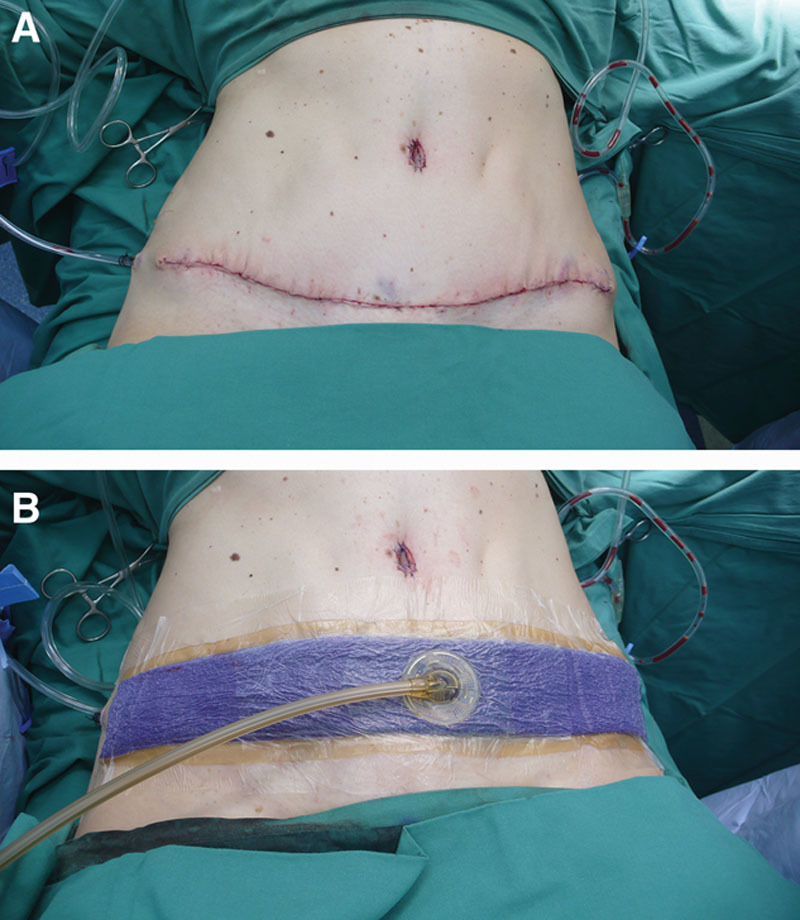
Application of iNPWT (Prevena Plus Incisional Management System) over abdominoplasty incision. A, Immediate postoperative abdominoplasty incision with 2 drains on each side. B, Prevena cut into desired length encompassing the whole incision with hydrocolloid barrier lining to ensure proper delivery of negative pressure throughout the system with SENSA T.R.A.C. Pad placed in the middle of the dressing and connected to the iNPWT therapy unit.
An abdominal binder was applied over the dressings to all patients and maintained for 6 weeks. Drains were removed if the total output was less than 50 ml/day. All patients were discharged from the hospital on postoperative day 7 and were followed up at 2 weeks, 4 weeks, and 6 months post operatively.
Statistical Analyses
All data were tabulated and analyzed using the statistical program Sigma Plot 13 (Systat Software, Inc., San Jose, Calif.). A Student t test was used to compare the total amount of fluid drained from patients with standard and experimental dressings. A Mann–Whitney rank sum test was used to test for differences in the time of drain removal between the 2 groups. A P value <0.05 was considered significant.
RESULTS
Sixteen patients, all female, were included in the study. Seven patients, with a mean age of 49 years (range, 33–61 years) and a mean average body mass index (BMI) of 35.36 kg/m2 (23.7–57.9 kg/m2), were included in the control group who were dressed with standard dressings. Nine patients who were included in the treatment group with iNPWT had a mean age of 41 years and average BMI of 29.94 kg/m2 (range, 25.4–37.1 kg/m2). All patients had no history of tobacco use, no previous personal or family history of diabetes, or any other comorbidities. The 2 groups also had similar average weight of tissue removed (1.2 kg for control versus 1.0 kg for iNPWT).
The iNPWT group demonstrated a significant reduction in fluid drainage with a mean amount of fluid output of 370 ± 275 ml compared to 1269 ± 436 ml total drainage (Fig. 2) from patients with control dressings (P < 0.001). Moreover, the time before removal of both drains was almost halved in patients with iNPWT with an average of 5.3 ± 1.6 days, which was significantly less than the average time of 10.6 ± 2.9 days (Fig. 3) seen in control patients (P < 0.001). Similarly, the maximum time that any drain remained in situ was significantly less in iNPWT patients at 6.4 ± 1.0 days versus 12.6 ± 0.98 for the control group (P < 0.001).
Fig. 2.
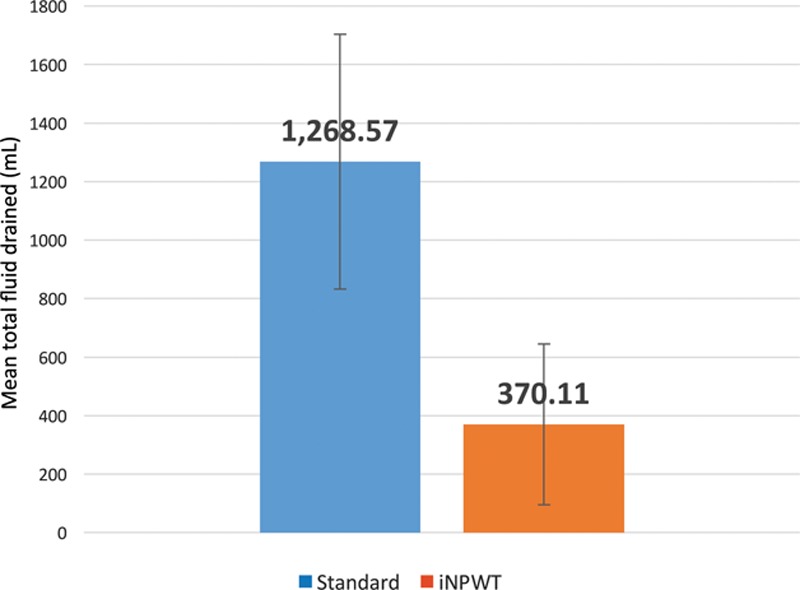
Mean total amount of fluid drained from patients who underwent abdominoplasty with standard dressings or iNPWT dressings, P = 0.00018.
Fig. 3.
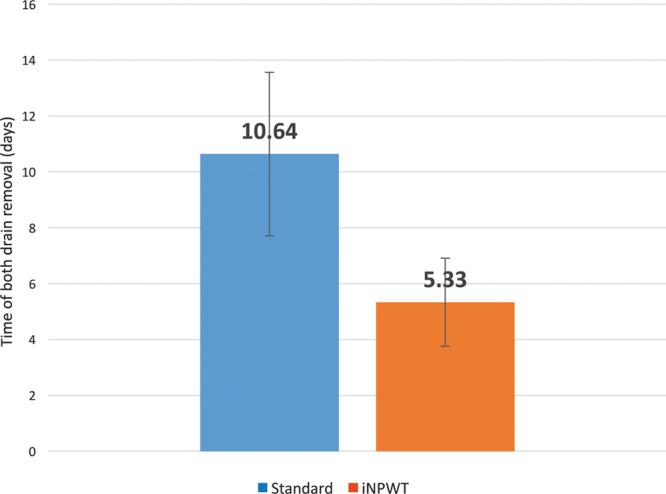
Average time of removal of both drains in patients who underwent abdominoplasty with standard vs iNPWT dressings, P < 0.001.
No major complications were encountered in either group. One patient in the control group developed hypertrophic scars and underwent subsequent steroid/laser treatment. Three patients (2 from the iNPWT and 1 from the control group) required dog-ear corrections at the 6-month mark. One patient had a minor granuloma and delayed healing of their umbilicus that resolved with topical silver treatment within 2 weeks.
DISCUSSION
This study has clearly demonstrated a consistent reduction (70%) of mean total fluid output after the application of iNPWT on patients undergoing elective abdominoplasties (Fig. 2) and allowed drain removal in half the time compared with control (Fig. 3). We did note a slight increase in drain output for the iNPWT group on day 2 (Fig. 4) coincident with mobilization. Our findings are supported by a similar study2 on postbariatric abdominal dermolipectomy patients in 2011.
Fig. 4.
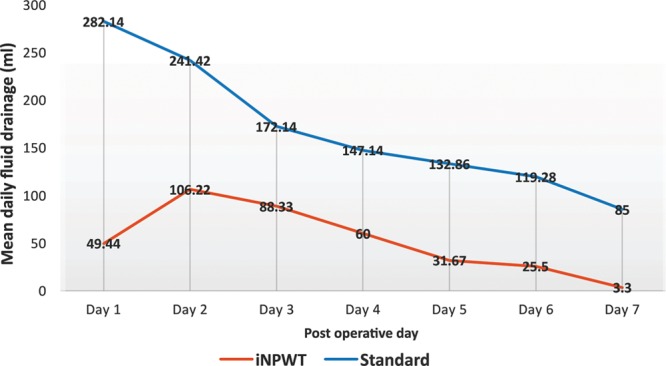
Mean daily fluid drainage for the first 7 days of abdominoplasty patients with standard and iNPWT dressings.
Incisional NPWT has been recommended to be used on patients with comorbidities and those with high-risk surgical wounds.13 Although none of our patients had significant comorbidity, both groups had high BMI averages. It is well known that obese patients are at an increased risk of wound complications such as seroma and wound dehiscence15–19 due to increased tension on suture lines and poor perfusion of adipose tissue.16
Surgical strategies that reduce drainage in abdominoplasty also include using progressive tension sutures and tissue adhesives, but studies to date are limited.20 A prospective, randomized control trial to investigate the benefits of iNPWT incorporating other strategies, such as quilting sutures and tranexamic acid, is warranted.
Footnotes
Published online 16 May 2019.
Disclosure: Dr. Deva is an advisor, an educator, and a research coordinator for Mentor (Johnson & Johnson), Allergan, and Acelity. He is an educator for Sientra and Motiva (Establishment labs).
REFERENCES
- 1.American Society of Plastic Surgeons. 2017 cosmetic plastic surgery statistics. 2018. https://www.plasticsurgery.org/documents/News/Statistics/2017/plastic-surgery-statistics-report-2017.pdf. Accessed April 2, 2018.
- 2.Dragu A, Schnürer S, Unglaub F, et al. Wide topical negative pressure wound dressing treatment for patients undergoing abdominal dermolipectomy following massive weight loss. Obes Surg. 2011;21:1781–1786. [DOI] [PubMed] [Google Scholar]
- 3.Vidal P, Berner JE, Will PA. Managing complications in abdominoplasty: a literature review. Arch Plast Surg. 2017;44:457–468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Neaman KC, Armstrong SD, Baca ME, et al. Outcomes of traditional cosmetic abdominoplasty in a community setting: a retrospective analysis of 1008 patients. Plast Reconstr Surg. 2013;131:403e–410e. [DOI] [PubMed] [Google Scholar]
- 5.Matarasso A, Matarasso DM, Matarasso EJ. Abdominoplasty: classic principles and technique. Clin Plast Surg. 2014;41:655–672. [DOI] [PubMed] [Google Scholar]
- 6.Hyldig N, Birke-Sorensen H, Kruse M, et al. Meta-analysis of negative-pressure wound therapy for closed surgical incisions. Br J Surg. 2016;103:477–486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gombert A, Barbati ME, Wittens C, et al. Effect of a new incision management system (PREVENA®) on wound healing after endophlebectomy of the common femoral vein: a case series. J Med Case Rep. 2016;10:130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Condé-Green A, Chung TL, Holton LH, III, et al. Incisional negative-pressure wound therapy versus conventional dressings following abdominal wall reconstruction: a comparative study. Ann Plast Surg. 2013;71:394–397. [DOI] [PubMed] [Google Scholar]
- 9.Blackham AU, Farrah JP, McCoy TP, et al. Prevention of surgical site infections in high-risk patients with laparotomy incisions using negative-pressure therapy. Am J Surg. 2013;205:647–654. [DOI] [PubMed] [Google Scholar]
- 10.Grauhan O, Navasardyan A, Tutkun B, et al. Effect of surgical incision management on wound infections in a poststernotomy patient population. Int Wound J. 2014;11(suppl 1):6–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Matatov T, Reddy KN, Doucet LD, et al. Experience with a new negative pressure incision management system in prevention of groin wound infection in vascular surgery patients. J Vasc Surg. 2013;57:791–795. [DOI] [PubMed] [Google Scholar]
- 12.Reddy VS. Use of closed incision management with negative pressure therapy for complex cardiac patients. Cureus. 2016;8:e506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Willy C, Agarwal A, Andersen CA, et al. Closed incision negative pressure therapy: international multidisciplinary consensus recommendations. Int Wound J. 2017;14:385–398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wilkes RP, Kilpad DV, Zhao Y, et al. Closed incision management with negative pressure wound therapy (CIM): biomechanics. Surg Innov. 2012;19:67–75. [DOI] [PubMed] [Google Scholar]
- 15.WHO. Obesity: Preventing and Managing the Global Epidemic. Report of a WHO Consultation (WHO Technical Report Series 894). 2000; Geneva: World Health Organization; 0512–3054. [PubMed] [Google Scholar]
- 16.Hahler B. An overview of dermatological conditions commonly associated with the obese patient. Ostomy Wound Manage. 2006;52:34–36, 38, 40 passim. [PubMed] [Google Scholar]
- 17.Arnaoutakis DJ, Scully RE, Sharma G, et al. Impact of body mass index and gender on wound complications after lower extremity arterial surgery. J Vasc Surg. 2017;65:1713.e1–1718.e1. [DOI] [PubMed] [Google Scholar]
- 18.Giordano SA, Garvey PB, Baumann DP, et al. The impact of body mass index on abdominal wall reconstruction outcomes: a comparative study. Plast Reconstr Surg. 2017;139:1234–1244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Owei L, Swendiman RA, Kelz RR, et al. Impact of body mass index on open ventral hernia repair: a retrospective review. Surgery. 2017;162:1320–1329. [DOI] [PubMed] [Google Scholar]
- 20.Gutowski KA. Evidence-based medicine: abdominoplasty. Plast Reconstr Surg. 2018;141:286e–299e. [DOI] [PubMed] [Google Scholar]


