Abstract
This study aims to investigate urban-rural differences in characteristics and risk factors of ischemic stroke in northern China.
The present cross-sectional study was based on the High-risk Population Screening and Intervention Project for Stroke. The cluster sampling method was used to select urban and rural screening sites in northern China. By collecting information and screening the data, patients with ischemic stroke were obtained and a control group with similar gender, age, and regional distribution was selected among the nonischemic stroke patients. Then, the demographic and risk factors of patients with ischemic stroke were described and analyzed.
The prevalence of ischemic stroke in northern China was 2.88%, with a greater prevalence in rural areas than in urban areas (3.32% vs 2.43%), and a greater prevalence in males than in females (3.06% vs 2.73%). Furthermore, rural stroke patients were younger than urban stroke patients. Hypertension, family history of stroke, and smoking were the top 3 independent risk factors for ischemic stroke. Overweight/obesity and low education were associated with increased ischemic stroke in urban areas, while low education was associated with less ischemic stroke in rural areas. In addition, the prevalence of alcoholism, dyslipidemia, diabetes, and obvious overweight/obesity was greater in urban areas, while high-salt diet and low education and income were more prevalent in rural regions. Moreover, the smoking index was higher in rural areas than in urban areas.
The characteristics and risk factors of ischemic stroke differ between rural and urban areas, which could be used to design specific preventative measures.
Keywords: ischemic stroke, north China, risk factors, rural, urban
1. Introduction
Stroke has become the main cause of death worldwide, and is the leading cause of disability and death of adults in China.[1–4] The latest national research revealed that rural areas experienced greater stroke changes, when compared with cities, and that the incidence, prevalence, and mortality of rural stroke all surpassed those in urban areas.[5] Ischemic stroke is the main subtype of stroke, and its medical cost is much higher, when compared with other cardiovascular and cerebrovascular diseases.[5–7] Hence, it has become one of the most important sources of economic burden, and a major public health problem in China.
Multiple genetic and environmental risk factors contribute to ischemic stroke. The common controllable risk factors include hypertension, diabetes, atrial fibrillation, hyperlipidemia, smoking, alcohol, high-salt diet, and lack of exercise.[8] For a disease with high disability and without effective treatment, it is particularly important to control its risk factors. The prevalence of stroke is undoubtedly attributed to the increased burden of vascular risk factors in developing countries.[9] Controlling risk factors can avoid the occurrence of most strokes and reduce economic burden.[10–12] Studies have found that the distribution of risk factors for ischemic stroke differ in urban and rural populations, which may be correlated to the differences in economic status, education, environmental status, and living habits.[5,13–15] Thus, studying the differences of risk factors for ischemic stroke between urban and rural areas is important for targeted prevention and control.
The latest survey revealed that the stroke burden is greater in north China than in south China.[5] However, there is a lack of large-scale epidemiological studies on cerebral infarction in northern China. The present study relied on the special medical reform project of the National Health and Family Planning Commission, the High-risk Population Screening and Intervention Project for Stroke. A large population at a high risk of stroke in northern China was obtained, and the characteristics and risk factors of ischemic stroke in urban and rural areas were compared. The aim of the present study was to provide evidence for the targeted control of risk factors for ischemic strokes in urban and rural areas.
2. Subjects and methods
2.1. Ethical statement
Ethical approval was obtained from the Ethics Committee of the First Hospital of Shanxi Medical University. A written informed consent was obtained from each participant.
2.2. Study areas
In 12 areas of northern China, including Liaoning, Jilin, Heilongjiang, Beijing, Hebei, Shanxi, Inner Mongolia, Shandong, Henan, Xinjiang, Shaanxi, and Gansu, a total number of 100 reasonably distributed urban and rural areas were selected as screening sites. These areas had convenient transportation, and was feasible for the long-term tracking of high-risk groups. A cluster sampling approach was used for each screening site to obtain the target screening populations, and ≥2000 individuals were required per screening site. The sample size was estimated based on the national survey for the prevalence of ischemic stroke.
2.3. Subject selection criteria
Inclusion criteria were residents who were aged ≥40 years, who have lived in the area for at least 6 months (born before January 1, 1977), and volunteered to participate in the study. Exclusion criteria were subjects who were unable to complete screening for severe illness, or who do not meet the above criteria.
Additional criteria for patients with ischemic stroke were patients with a history of ischemic stroke and have available records (diagnosed by a secondary hospital or above) or on-site brain imaging data (necessary symptoms of neurological deficit); patients with strokes caused by tumors, poisoning, or trauma were excluded. Criteria for the control group were patients with similar gender, age, and location of ischemic stroke population, and were randomly selected among the noncerebral infarction populations.
2.4. Screening methods
The “2016 Comprehensive Cardiovascular and Cerebrovascular Risk Factors Communities and Township Populations Intervention Questionnaire” was used to conduct the face-to-face screening of the incorporated object. Individuals with ischemic stroke and controls, who have complete information, were screened. The data collection and technical route is presented in Fig. 1.
Figure 1.
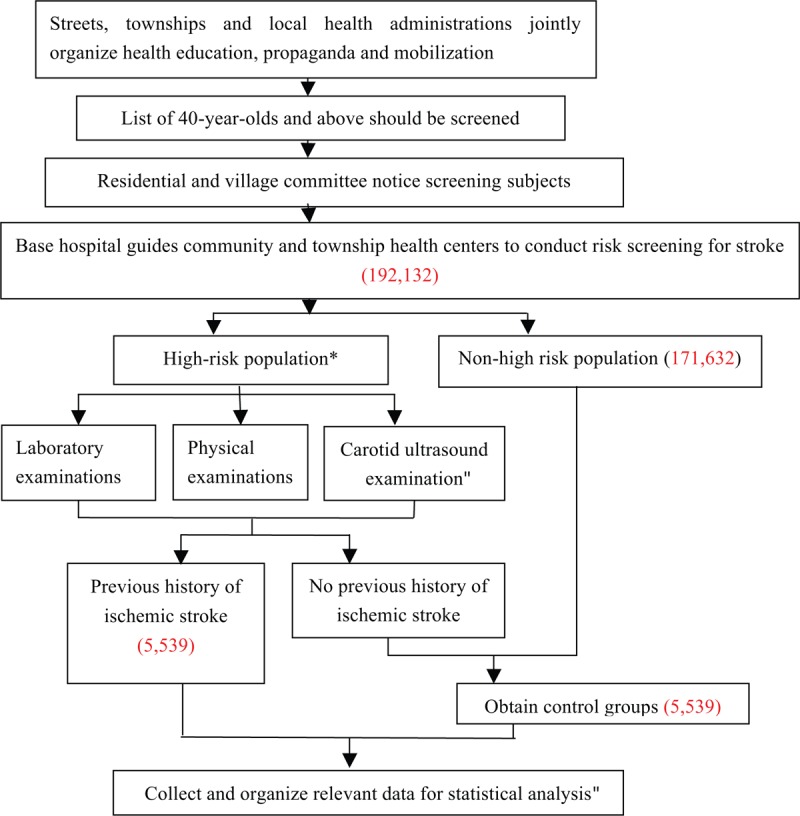
The technical route.
2.5. Diagnostic criteria
The diagnostic criteria were as follows: hypertension: systolic blood pressure ≥140 mm Hg and/or diastolic blood pressure ≥90 mm Hg, or the use of anti-hypertensive medications[16]; Diabetes: fasting blood glucose ≥7.0 mmol/L or nonfasting time blood glucose ≥11.0 mmol/L, or the use of hypoglycemic drugs[17]; Dyslipidemia: total cholesterol ≥6.22 mmol/L, triglyceride ≥2.26 mmol/L, high-density lipoprotein cholesterol <1.04 mmol/L, low-density lipoprotein cholesterol ≥4.14 mmol/L, one or more abnormalities, or the use of lipid-lowering drugs[18]; Physical exercise: ≥3 times per week, at least 30 minutes of moderate to intense exercises, or engaging in moderate to severe manual labor; Smoking: continuous or cumulative smoking for 6 months or more; Atrial fibrillation: definitive diagnosis at secondary hospitals and above, or with available electrocardiographic support; Overweight or obesity: BMI ≥26 was considered obviously overweight, while BMI ≥28 was considered obese [BMI = weight (kg)/height (m2)]; Alcoholism: frequent heavy drinking was defined as drinking white wine ≥3 times/week, at ≥100 grams each time; Family history of stroke: parents or siblings in the family have stroke; Past transient ischemic attack (TIA): definitive diagnosis at secondary hospitals or above; High-salt diet: daily salt intake ≥6 g; Educational level: secondary school/high school and above was considered as high education level, while junior high school and below was considered as low education level; Income level: an annual income >10,000 Y was considered as high income level, while an annual income <10,000 Y was considered as low income level.
2.6. Quality control
The investigators were required to be professionally trained and qualified, fully understand the contents of the questionnaire, be loyal to their original intentions, and conduct inquiries in easy-to-understand languages. When the survey was completed, a certain number of questionnaires were randomly selected to verify the completeness and authenticity.
2.7. Statistical analysis
Excel was used to build the database, and the SPSS 24.0 statistical software (Statistical Product and Service Solutions, https://www.ibm.com/products/spss-statistics) was used for statistical analysis. The qualitative data were represented as numbers and percentages, and Chi-square test was used for comparisons between 2 groups. Quantitative data with a normal distribution were expressed as mean ± standard deviation, and comparisons between 2 groups were performed using independent-sample t test. Non-normal distribution data were expressed as median (interquartile range), and the Mann–Whitney U test was used for comparison. Multivariate logistic regression analysis was used to calculate the odds ratios (ORs) and 95% confidence interval (95% CI). A 2-tailed P < .05 was considered statistically significant.
3. Results
3.1. Basic information
A total of 192,131 subjects were screened, including 93,943 (48.90%) subjects in urban areas and 98,188 (51.10%) subjects in rural areas. Among these participants, 90,218 (46.96%) were males. Furthermore, 5539 (2.88%) patients had ischemic stroke. Among these patients, 2280 (2.43%) patients were from urban areas, while 3259 (3.32%) patients were from rural areas. There was a higher prevalence in urban areas than in rural areas (P < .001). Among these ischemic stroke patients, there were more male patients than female patients [2761 (3.06%) vs 2778 (2.73%); P < .001].
3.2. Baseline characteristics of the ischemic stroke population
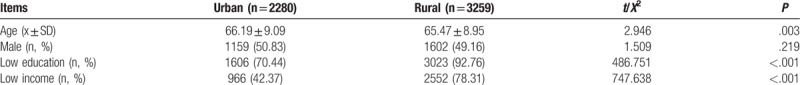
The baseline characteristics of patients with ischemic stroke are presented in Table 1. Age was greater (66.19 ± 9.09 vs 65.47 ± 8.95 years, P = .003), while low-education and low-income percentages (both, P < .001) were lower in urban patients with ischemic stroke, when compared with patients in rural areas. Among the 5539 patients with ischemic stroke, 2439 (44.03%) patients were of working-age (<65 years). However, there was no difference in gender between urban and rural ischemic stroke patients (Table 1).
Table 1.
Demographic characteristics of the patients with ischemic stroke in urban and rural areas in northern China.
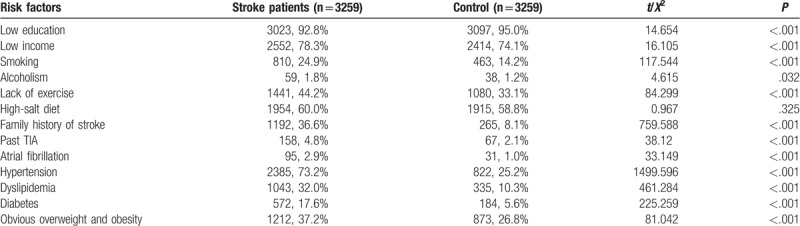
3.3. Exposure to risk factors for stroke in the population
The stroke risk factors that urban and rural ischemic stroke patients and controls are exposed to are presented in Tables 2 to 4. Except for high-salt diet and low education, the exposure rates of risk factors were higher in the ischemic stroke group, when compared with the control group, in both urban and rural populations (Tables 2 and 3). Furthermore, the percentage of low-income patients was higher in urban stroke patients, when compared with urban controls (Table 2), while this percentage was lower in rural stroke patients, when compared with rural controls (Table 3). The multivariate regression analysis revealed that hypertension, family history of stroke, smoking, dyslipidemia, diabetes, and lack of exercise were common independent risk factors for ischemic stroke in both urban and rural areas (Table 4). Obvious overweight or obesity and low education were the risk factors for urban stroke patients, while atrial fibrillation was a risk factor for rural stroke patients (Table 4). In addition, low education was a protective factor for rural stroke patients (Table 4).
Table 2.
Exposure of stroke risk factors in urban patients with ischemic stroke.
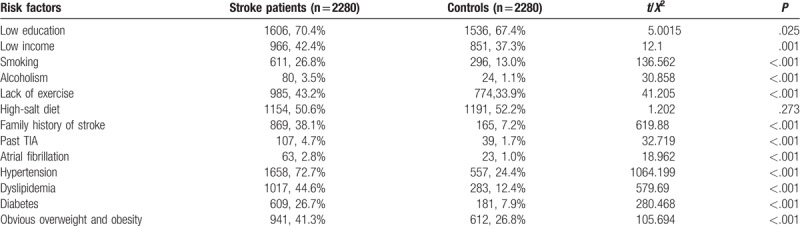
Table 4.
The multivariate analysis of risk factors in urban and rural patients with ischemic stroke.
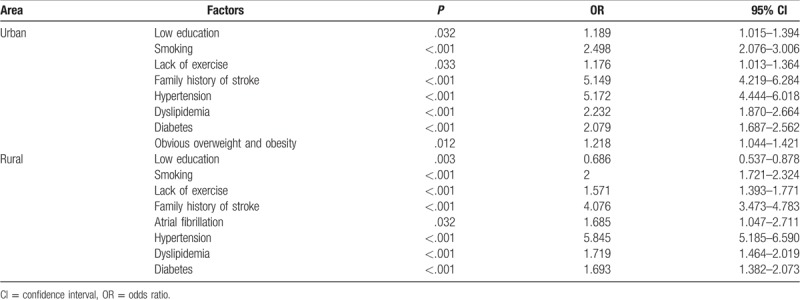
Table 3.
Exposure of stroke risk factors in rural patients with ischemic stroke.
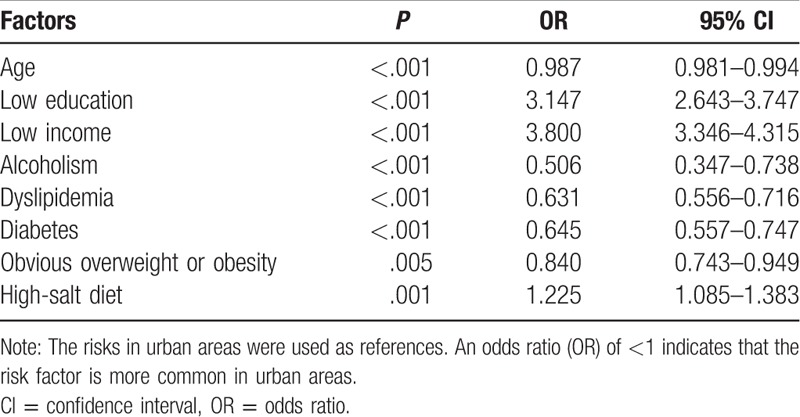
3.4. Comparison of stroke risk factors in urban and rural ischemic stroke populations
A comparison of risk factors between urban and rural areas is presented in Tables 5 and 6. The top 3 risk factors for ischemic stroke in urban patients were hypertension (72.72%), high-salt diet (50.61%), and dyslipidemia (44.61%), while the top 3 risk factors in rural patients were hypertension (73.18%), high-salt diet (59.96%), and lack of exercise (44.22%). The exposure rates of diabetes mellitus, dyslipidemia, overweight or obesity, and heavy drinking were higher in urban areas, while the exposure rate of high-salt diet was higher in rural areas. In addition, the stratified study of gender revealed that smoking and alcoholism have an obviously higher exposure rate in male cerebral infarction groups, when compared with female cerebral infarction groups (Table 5). In the multifactor analysis, aging, alcoholism, dyslipidemia, diabetes, and obvious overweight or obesity were the more common stroke risk factors in urban areas, while low education, low income, and high-salt diet were more common in rural areas (Table 6).
Table 5.
Ischemic stroke risk factors in urban and rural areas.
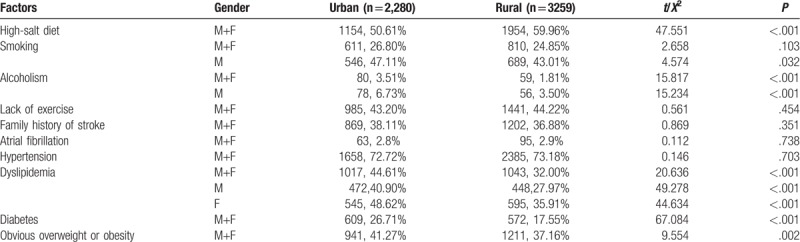
Table 6.
The multivariate analysis of exposed stroke risk factors in urban and rural areas.
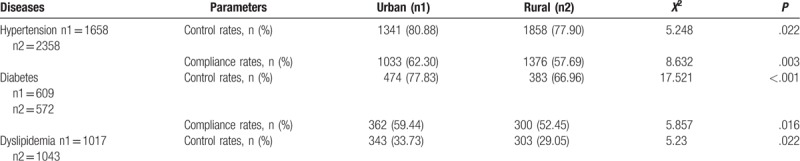
3.5. Control of chronic disease in ischemic stroke patients
The chronic disease control in ischemic stroke patients is presented in Table 7. The control rates of hypertension, diabetes, and dyslipidemia were significantly higher in urban ischemic stroke patients, when compared with rural ischemic stroke patients. In addition, it was also found that the compliance rates of blood pressure and blood glucose were significantly higher in urban areas, when compared with rural areas.
Table 7.
Chronic disease control in ischemic stroke patients.
4. Discussion
Stroke seriously endangers the lives and health of the people. The present study revealed that nearly half of the stroke patients were of the working age, which would undoubtedly cause heavy burden on families and the society. Furthermore, the incidence of stroke in China is lower in the south, when compared with the north, but this incidence is higher in the countryside, when compared with the cities.[5] Hence, it is of great significance to compare the characteristics and risk factors of stroke in high-risk populations between urban and rural areas in northern China.
The present study found that the prevalence of ischemic stroke in patients who were ≥40 years old in northern China was 2.88%, which was higher than the results (1.79%) of a national study.[3] Furthermore, the prevalence was higher in rural areas than in urban areas, and male patients were greater than female patients, which is consistent with previous results.[5] In addition, it was found that the control rates of hypertension and diabetes were significantly lower in the rural ischemic stroke population, when compared with those in urban areas. The risk of stroke increases with age. Furthermore, it was found that the average age of ischemic stroke was 65 years, and that rural stroke patients were slightly younger than urban patients. A previous study revealed that stroke occurred mainly in subjects who were greater than 60 years old in China.[3] A study in India reported that the median age of stroke was 67 years, and that the stroke patients in developing countries were younger than those in developed countries.[9] Therefore, an age of approximately 65 years is the key age for the prevention and treatment of ischemic stroke. Hypertension, as the most common risk factor for stroke, accounts for 88% of stroke patients, and results in 73% of the stroke burden.[5] Furthermore, its population attributable risk for stroke is 53.2%.[3] The present study also revealed that it is the most relevant independent risk factor for ischemic stroke in urban and rural areas (OR = 5.712/5.845), and the rate of exposure in an ischemic stroke population was slightly higher in the village, when compared with the city (72.72% vs 73.18%), which is consistent with the view reported in eastern China, Uganda, and Northern Sweden, in which hypertension is more common in rural stroke patients.[14,15,19] However, the specific reasons are yet to be clarified.
The prevalence of cardiovascular risk factors has been increasing each year in China.[13,20–22] It was found that dyslipidemia, obvious overweight or obesity, and diabetes were more prevalent in urban stroke patients, which is consistent with several national studies.[5,6,13,14] Furthermore, the prevalence of dyslipidemia was higher in female patients than in male patients, which might be due to the relatively high rate of dyslipidemia among postmenopausal women.[23] Studies have found that urban areas have more overweight or obese subjects, and the highest urban-rural difference was in subjects who are greater than 60 years old.[24] The Uganda study also reported a similar urban-rural difference.[15] These findings are similar to the present results. However, the correlation between socioeconomic status and overweight/obesity is reversed in developed countries.[19] Although the prevalence of overweight/obesity is higher in urban areas than in rural areas, the growth in the latter is accelerating.[24]
The relationship between drinking and stroke remains controversial. A recent meta-analysis on 27 prospective studies suggested that mild to moderate drinking may reduce the risk of cerebral infarction, while alcoholism is associated with an increased risk of all stroke subtypes.[25] The present study included heavy drinking as a risk factor, which is more specific than the drinking used in previous studies. However, the drinking habits of abstainers were not investigated in the present investigation, which could underestimate the true contribution of this risk factor to cerebral infarction. This is a possible reason why it was not identified as an independent risk factor for ischemic stroke in the whole study population. Nevertheless, it was found that heavy drinking in the ischemic stroke population was more common in the city than in the village, and this was still the case after adjusting for other confounding factors. Studies have shown that low income can reduce alcoholism and the morbidity and mortality of alcoholism-related disease.[26] A Danish hospital-based study of ischemic stroke found that the stroke risk of individuals with the lowest education was 36% higher, when compared with individuals with the highest education, while for individuals in the lowest income group, this was almost twice of that in individuals in the highest income group.[27] In contrast, low education in the present study was identified as a protective factor for ischemic stroke in rural areas, which warrants further investigation. Furthermore, it was found that high-salt diet is a risk factor for ischemic stroke, especially in rural areas. This is consistent with the fact that there was a gradual increase in salt intake from south to north China,[28] and that people in less economically developed regions take more salt.[29]
Smoking is the second most important risk factor for stroke after hypertension.[30] It was found that smoking was a major risk factor for male stroke patients, and that the prevalence of smoking was higher in urban areas than in rural areas, which is consistent with the findings of a study conducted in India.[31] It was also found that the smoking index was significantly higher in rural areas, which was similar to a previous survey.[32] Furthermore, family history of stroke, atrial fibrillation, and lack of exercise are also important risk factors for ischemic stroke.[22,33–35] Although the present study did not reveal any difference between urban and rural areas, caution should still be taken. Atrial fibrillation has been a major risk factor for ischemic stroke.[36] However, the present study failed to identify atrial fibrillation as a risk factor, which is probably because the prevalence of atrial fibrillation was relatively low in the study population.
In summary, the distribution characteristics of risk factors for ischemic stroke in northern China were obtained. It was found that hypertension was the most common stroke risk factor. Furthermore, rural stroke patients were younger and associated with low income and education, and more salinity dietary, while urban stroke patients had a higher prevalence of diabetes, dyslipidemia, and overweight/obesity. More specific measures should be taken to control risk factors for ischemic stroke.
The strength of the present study was the large sample size and wide coverage. However, there were a few limitations. First, merely stroke survivors of cerebral infarction, who were >40 years old, were included. Second, the specific forms of physical exercise and actual salt intake were not specifically stratified. Third, other risk factors, such as air pollution, infections, nationalities, and psychological and social pressures, were not included. Lastly, this was a cross-sectional study.
Acknowledgments
We thank the grant support from the Stroke Prevention Project of National Health Commission of the People's Republic of China (GN-2016F0002).
Author contributions
Data curation: Hui Sang, Tingting Liu, Weidong Liu, Jian Li.
Writing – original draft: Yang Li, Xin Zhang.
Writing – review & editing: Xiaoyuan Niu.
Footnotes
Abbreviations: BMI = body mass index, CI = confidence interval, TIA = transient ischemic attack.
YL and XZ contributed equally to this work.
The authors have no conflicts of interest.
References
- [1].Feigin VL, Forouzanfar MH, Krishnamurthi R, et al. Global and regional burden of stroke during 1990-2010: findings from the Global Burden of Disease Study 2010. Lancet 2014;383:245–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Słomka A, Switonska M, Sinkiewicz W, et al. Assessing circulating factor VIIa-antithrombin complexes in acute ischemic stroke: a pilot study. Clin Appl Thromb Hemost 2017;23:351–9. [DOI] [PubMed] [Google Scholar]
- [3].Guan T, Ma J, Li M, et al. Rapid transitions in the epidemiology of stroke and its risk factors in China from 2002 to 2013. Neurology 2017;89:53–61. [DOI] [PubMed] [Google Scholar]
- [4].Tsai CF, Thomas B, Sudlow CL. Epidemiology of stroke and its subtypes in Chinese vs white populations: a systematic review. Neurology 2013;81:264–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Wang W, Jiang B, Sun H, et al. Prevalence, incidence, and mortality of stroke in China: results from a nationwide population-based survey of 480 687 adults. Circulation 2017;135:759–71. [DOI] [PubMed] [Google Scholar]
- [6].Chen W, Gao R, Liu L, et al. China cardiovascular disease report 2016 outline. Chin Circ J 2017;32:521–30. [Google Scholar]
- [7].Mozaffarian D, Benjamin EJ, Go AS, et al. American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics–2015 update: a report from the American Heart Association. Circulation 2015;131:e29–322. [DOI] [PubMed] [Google Scholar]
- [8].O’Donnell MJ, Xavier D, Liu L, et al. Risk factors for ischaemic and intracerebral haemorrhagic stroke in 22 countries (the INTERSTROKE study): a case-control study. Lancet 2010;376:112–23. [DOI] [PubMed] [Google Scholar]
- [9].Sridharan SE, Unnikrishnan JP, Sukumaran S, et al. Incidence, types, risk factors, and outcome of stroke in a developing country: the Trivandrum Stroke Registry. Stroke 2009;40:1212–8. [DOI] [PubMed] [Google Scholar]
- [10].Kim JS. Stroke in Asia: a global disaster. Int J Stroke 2014;9:856–7. [DOI] [PubMed] [Google Scholar]
- [11].Kuklina EV, Tong X, George MG, et al. Epidemiology and prevention of stroke: a worldwide perspective. Expert Rev Neurother 2012;12:199–208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Jia Q, Liu L, Wang Y. Risk factors and prevention of stroke in the Chinese population. J Stroke Cerebrovasc Dis 2011;20:395–400. [DOI] [PubMed] [Google Scholar]
- [13].Li Q, Wu H, Yue W, et al. Prevalence of stroke and vascular risk factors in China: a nationwide community-based study. Sci Rep 2017;7:6402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Mi T, Sun S, Du Y, et al. Differences in the distribution of risk factors for stroke among the high-risk population in urban and rural areas of Eastern China. Brain Behav 2016;6:e00461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Nakibuuka J, Sajatovic M, Nankabirwa J, et al. Stroke-risk factors differ between rural and urban communities: population survey in central Uganda. Neuroepidemiology 2015;44:156–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Chinese Committee for the Prevention, Treatment of Hypertension Prevention Guidelines. Guidelines for prevention and treatment of hypertension in China 2010. Chin J Cardiovasc Dis 2011;39:701–8. [Google Scholar]
- [17].Chinese Medical Association Diabetes Branch. Guidelines for the prevention and treatment of type 2 diabetes in China (2010 Edition). Chin J Pract Rural Doct 2012;19:54–109. [Google Scholar]
- [18].Xu H, Zhai Z, Lu Z. Summary and interpretation of guidelines for prevention and treatment of dyslipidemia in Chinese adults (2007). Chin J Geriatr Cardiovasc Cerebrovasc Dis 2008;10:238–40. [Google Scholar]
- [19].Lindroth M, Lundqvist R, Lilja M, et al. Cardiovascular risk factors differ between rural and urban Sweden: the 2009 Northern Sweden MONICA cohort. BMC Public Health 2014;14:825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Chen R, Ovbiagele B, Feng W. Diabetes and stroke: epidemiology, pathophysiology, pharmaceuticals and outcomes. Am J Med Sci 2016;351:380–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Cai L, He J, Song Y, et al. Association of obesity with socio-economic factors and obesity-related chronic diseases in rural southwest China. Public Health 2013;127:247–51. [DOI] [PubMed] [Google Scholar]
- [22].Bogiatzi C, Hackam DG, Mcleod AI, et al. Secular trends in ischemic stroke subtypes and stroke risk factors. Stroke 2014;45:3208–13. [DOI] [PubMed] [Google Scholar]
- [23].Choi Y, Chang Y, Kim BK, et al. Menopausal stages and serum lipid and lipoprotein abnormalities in middle-aged women. Maturitas 2015;80:399–405. [DOI] [PubMed] [Google Scholar]
- [24].Wu Y, Ma G, Hu Y, et al. Current status of overweight and obesity in Chinese residents. Chin J Prev Med 2005;39:316–20. [PubMed] [Google Scholar]
- [25].Larsson SC, Wallin A, Wolk A, et al. Differing association of alcohol consumption with different stroke types: a systematic review and meta-analysis. BMC Med 2016;14:178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Holmes J, Meng Y, Meier PS, et al. Effects of minimum unit pricing for alcohol on different income and socioeconomic groups: a modelling study. Lancet 2014;383:1655–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Andersen KK, Stedingjessen M, Dalton SO, et al. Socioeconomic position and incidence of ischemic stroke in Denmark 2003–2012. A nationwide hospital-based study. J Am Heart Assoc 2014;3:pii: e000762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Xu G, Ma M, Liu X, et al. Is there a stroke belt in China and why? Stroke 2013;44:1775–83. [DOI] [PubMed] [Google Scholar]
- [29].Yu D, He Y, Fang H, et al. Salt intake of adult residents in China from 2010 to 2012. Chin J Prev Med 2016;50:217–20. [DOI] [PubMed] [Google Scholar]
- [30].Shah RS, Cole JW. Smoking and stroke: the more you smoke the more you stroke. Expert Rev Cardiovasc Ther 2010;8:917–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Goyal A, Yusuf S. The burden of cardiovascular disease in the Indian subcontinent. Indian J Med Res 2006;124:235–44. [PubMed] [Google Scholar]
- [32].Li Q, Hsia J, Yang G. Prevalence of smoking in China in 2010. N Engl J Med 2011;364:2469–70. [DOI] [PubMed] [Google Scholar]
- [33].Chung JW, Kim BJ, Han MK, et al. Family history and risk of recurrent stroke. Stroke 2016;47:1990–6. [DOI] [PubMed] [Google Scholar]
- [34].Freedman B, Potpara TS, Lip GY. Stroke prevention in atrial fibrillation. Lancet 2016;388:806–17. [DOI] [PubMed] [Google Scholar]
- [35].Kubota Y, Iso H, Yamagishi K, et al. Daily total physical activity and incident stroke. Stroke 2017;48:1730–6. [DOI] [PubMed] [Google Scholar]
- [36].Joundi RA, Cipriano LE, Sposato LA, Saposnik G. Response to letter regarding article, “Ischemic Stroke Risk in Patients With Atrial Fibrillation and CHA2DS2-VASc Score of 1: Systematic Review and Meta-Analysis”. Stroke 2016;47:e194. [DOI] [PubMed] [Google Scholar]


