Abstract
Background:
Rotator cuff calcific tendinopathy (RCCT) is frequently diagnosed in patients with shoulder pain, but there is no consensus on its treatment such as rest, nonsteroidal anti-inflammatory drugs (NSAIDs), physical therapy, subacromial corticosteroid injection (SAI), extracorporeal shock wave therapy (ESWT), and ultrasound-guided percutaneous lavage (UGPL). The aim of the study was to compare the effectiveness of UGPL with other techniques in the treatment of RCCT.
Methods:
Literature searches of PubMed, EMBASE, OVID, Cochrane Library, Web of Science, Chinese Biomedical Literature, Wanfang, Weipu Journal, and CNKI databases were performed up to August 2018. Only randomized controlled trials (RCTs) comparing UGPL vs other methods for RCCT were included. Data collection and extraction, quality assessment, and data analyses were performed according to the Cochrane standards.
Results:
Eight RCTs were included with 617 cases in all. The result of meta-analysis showed that: there were significant differences between the UGPL and ESWT group in 12-month follow-up VAS, constant shoulder score (CSS), the average particle size of the calcium deposition, and the calcification disappearance rate. However, there was no significant difference in complication between 2 groups.
Conclusion:
The present meta-analysis indicates that UGPL has certain clinical effect for calcifying tendinitis of rotator cuff. Compared with ESWT, UGPL may be superior in clinical pain relief and calcification clearance. However, owing to the limited quality and quantity of the included studies, additional high-quality RCTs are needed to confirm these findings.
Keywords: extracorporeal shock wave therapy, meta-analysis, rotator cuff calcific tendonitis, ultrasound-guided percutaneous lavage
1. Introduction
Rotator cuff calcific tendonitis (RCCT) is one of the leading causes of chronic shoulder pain.[1] An early large-scale study of 12,122 individuals by Bosworth et al reported an overall prevalence of 2.7%, peak prevalence in the third to fifth decades of life, and tendency to afflict women more than men.[2–4] It is generally a very painful but self-limiting condition[5–7] that is usually manageable with appropriate non-operative treatments such as rest, non-steroidal anti-inflammatory drugs (NSAIDs), physical therapy, and subacromial corticosteroid injection (SAI). Nevertheless, failure of these non-operative treatment methods may necessitate surgical treatment.[8–10]
Surgical management options include arthroscopic procedures to remove the calcified deposit and subacromial decompression, both of which have been proven effective for restoring shoulder function and reducing pain. Controversies exist, however, regarding the optimal extent of calcification removal, the long-term impact on the rotator cuff tendons, and the use of subacromial decompression.
Surgery for chronic RCCT is gradually being superseded by new minimally invasive options such as extracorporeal shock wave therapy (ESWT) and ultrasound-guided percutaneous lavage (UGPL). Several studies[11–13] have shown that UGPL and ESWT can significantly improve RCCT-related pain, shoulder joint function, and patient quality of life. ESWT is often recommended as a second-line therapy prior to surgical management,[14,15] as it is non-invasive and relatively easy to perform in the outpatient setting. Several studies[16–21] conducted over the last 2 decades have demonstrated the effectiveness of ESWT for treating RCCT compared to placebo, and a systematic review by Wang[22] affirmed the clinical efficacy of ESWT. However, this procedure can be extremely painful when the patient is in hyperalgesic crisis. Ultrasound-guided percutaneous lavage is also relatively inexpensive and safe compared to other guidance modalities, such as computed tomography and magnetic resonance imaging. It can be used during needle decompression for calcium deposits with or without subacromial steroid injection in cases of calcific tendinitis. However, the relative efficacy of UGPL compared to other treatments for RCCT is still unclear.
To provide robust support for clinical decisions, we conducted a systematic review and meta-analysis of currently available prospective randomized controlled trials comparing the effectiveness and safety of UGPL to other methods.
2. Materials and methods
2.1. Search strategy and study selection
We searched the following online databases for eligible articles published up to August 2018 comparing UGPL to other methods for the treatment of RCCT: PubMed, EMBASE, OVID, Cochrane Library, Web of Science, Chinese Biomedical Literature database, Wanfang data, Weipu Journal database, and National Knowledge Infrastructure (CNKI). The search terms and key words were as follows: “ultrasound”, “needling”, “lavage”, “calcific”, “calcified”, “rotator cuff”, “tendinitis”, “tendinopathy”, “shoulder”, and “randomized controlled trial”. Google Scholar was also searched to investigate potentially relevant literature. In addition, the reference lists of included studies and all related review articles were checked for additional trials, published or unpublished. Language and publication status date were not restricted, and gray literature as well as ongoing trials were also investigated.
2.2. Inclusion and exclusion
Study inclusion criteria were as follows:
-
1.
patients: patients diagnosed with rotator cuff calcific tendinopathy;
-
2.
intervention: ultrasound-guided percutaneous lavage or other methods such as rest, physical therapy, NSAIDs, SAI, and ESWT;
-
3.
outcome: visual analogue scale (VAS), mean size of the deposits at last follow-up, constant shoulder score (CSS), calcification disappearance rate, need for surgery, and complications;
-
4.
study design: prospective randomized controlled trial (RCT).
Exclusion criteria were as follows:
-
1.
retrospective studies, single-case reports, animal studies, reviews, meta-analysis, posters, or abstracts;
-
2.
study objective or intervention measures failed to meet the inclusion criteria;
-
3.
duplicates or multiple publications of the same study;
-
4.
studies without usable data.
2.3. Quality assessment
The quality of the included studies was assessed independently by 2 reviewers using the Cochrane Risk of Bias Tool of Review Manager Version 5.3 (Copenhagen, Denmark: The Nordic Cochrane Centre, The Cochrane Collaboration). Appraisal criteria included random sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessment, incomplete outcome data, selective reporting, and other sources of bias. Each of these factors was recorded as low risk, unclear risk, or high risk. If data were unclear, we contacted authors for clarification whenever possible. Disagreements were resolved by third party adjudication.
2.4. Data extraction
Data were extracted for all studies that met the inclusion criteria. For each study, 2 review authors independently completed data extraction forms tailored to the requirements of this review. All disagreements were resolved by discussion between the 2 review authors. If disagreement could not be resolved, a third review author was asked to complete the data extraction form and discuss the paper with the other 2 authors until a consensus was reached.
2.5. Statistical analysis
2.5.1. Heterogeneity test and effect value
This study used Review Manager 5.3 software for meta-analysis. Risk ratios (RRs) were calculated for dichotomous variables in each study. Standardized mean difference (SMD) or weighted mean difference (WMD) was calculated for continuous variables, and 95% confidence intervals (CIs) were determined for all effect sizes. Heterogeneity was analyzed using χ2 tests before meta-analysis (P = .05). If there was no heterogeneity (P ≥ .05, I2 < 50%), a fixed effect model was used. Otherwise (P < .05) a random effect model was used. Sensitivity analysis was conducted by step-wise removal of datasets. Datasets causing significant changes in pooled results when removed were analyzed further to assess the reason. We then judged the results for stability and strength. If the heterogeneity was too large to analyze, descriptive analyses are presented.
2.5.2. Publication bias
Potential publication bias was judged by Begg test/Egger test. The robustness of the combined data was assessed by sensibility analysis. A P value ≤ .05 was considered statistically significant.
3. Results
3.1. Search results
The detailed steps of literature selection are shown in Figure 1. The initial database search yielded 254 studies. No data was obtained from gray literature investigations or ongoing trials (we received no answers from authors we contacted). After removal of duplicates, 138 articles remained for review, of which 103 did not match our inclusion criteria according to title and abstract assessment. Of the remaining 35 papers, 26 did not meet the inclusion criteria after full-article assessment, and 2[23,24] were published by the same team at different times. Finally, 8 articles[24–31] (including 1 Master's degree thesis[29]) with a total of 617 patients were included in the meta-analysis. All of the included trials were RCTs.
Figure 1.
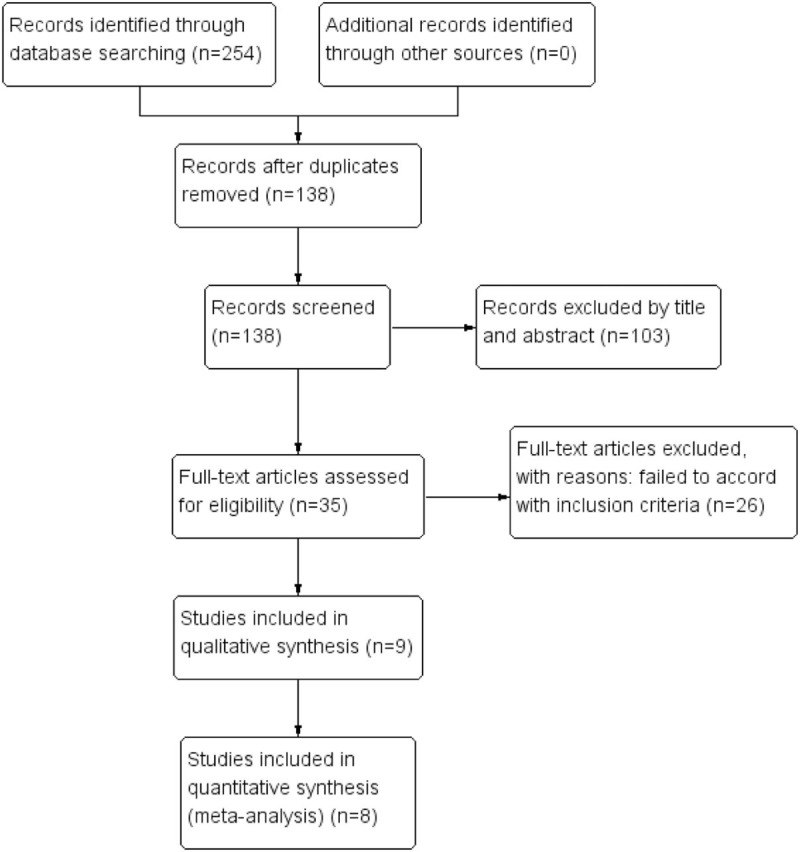
The flow chart of literature selection.
3.2. Quality assessment and basic information
According to The Cochrane Collaboration Risk of Bias Tool, the quality of all RCTs was acceptable (Fig. 2), and 4 RCTs reported the method of randomization. Three RCTs were conducted through computer-generated lists, 1 through randomized numbers, 2 through sealed envelopes, and 2 reported blinding of the surgeons and participants. No study showed an unclear bias due to incomplete outcome data or selective outcome reporting.
Figure 2.
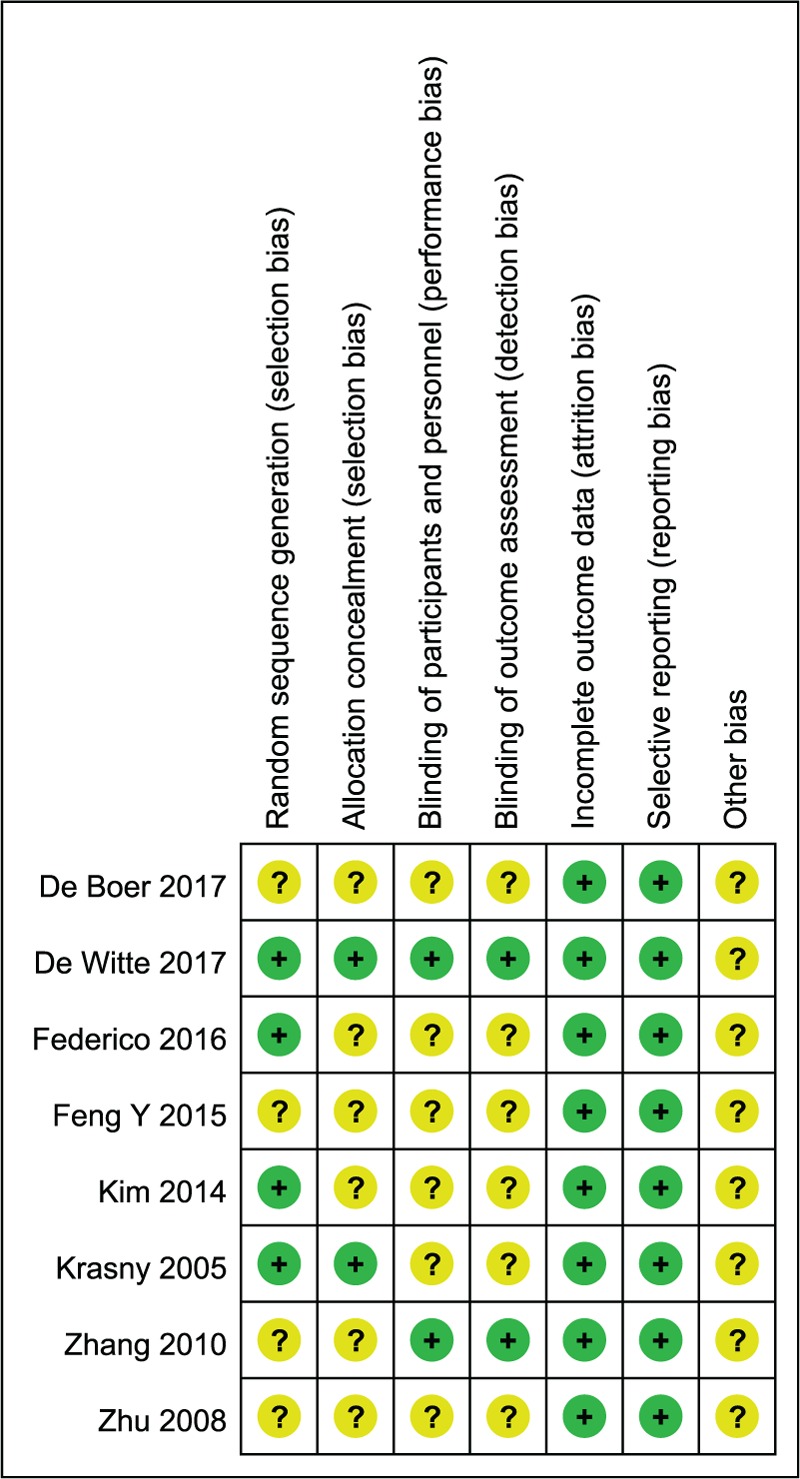
Risk of bias assessment summary of this meta-analysis.
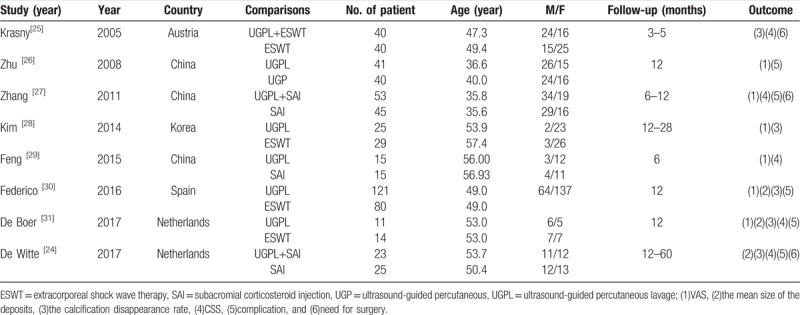
3.3. Demographic characteristics
Demographic characteristics are summarized in Table 1. Baseline characteristics UGPL and control groups were similar.
Table 1.
Summary of study and patient characteristics.
3.4. Visual analog score
Six articles with a total of 489 patients reported relevant data regarding VAS. In the subgroup analysis, 2 trials reported VAS at 3 months, pooled data showed no significant difference between 2 groups (WMD = −1.11; 95%CI = −2.74 to 0.52, P = .18; I2 = 85%, P = .009). 2 trials reported VAS at 6 months, pooled data showed no significant difference between 2 groups (WMD = −0.79; 95%CI = −2.20 to 0.62, P = .27; I2 = 81%, P = .02). 4 trials showed that the UGPL group had lower VAS (WMD = −1.96; 95%CI = −2.20 to −1.72, P < .00001; I2 = 9%, P = .35; Fig. 1) at 12 months (Fig. 3).
Figure 3.
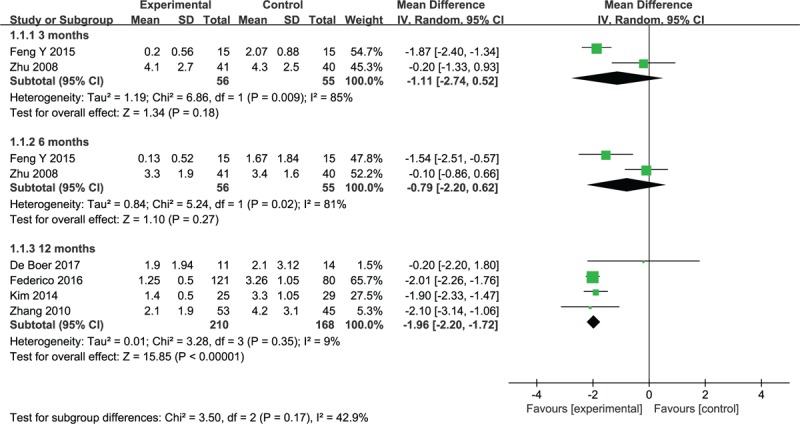
Forest plot of visual analog score between 2 groups at 3, 6, and 12 months.
3.5. The mean size of the deposits
Three studies with a total of 280 patients reported relevant data regarding the mean size of the deposits, the meta-analysis showed significantly smaller size of the deposits in the UGPL group (WMD = −3.13; 95%CI = −5.07 to −1.20, P = .002; I2 = 99%, P < .00001; Fig. 4).
Figure 4.
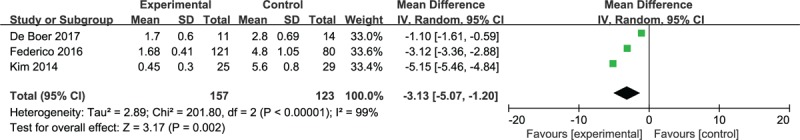
Forest plot of the mean size of the deposits between 2 groups.
3.6. The calcification disappearance rate
A total of 5 studies reported relevant data regarding the calcification disappearance rate (220 patients in the UGPL group and 184 in the control group). Pool the data revealed that the patients in UGPL group significantly increased the calcification disappearance rate (RR = 1.73; 95%CI = 1.44 to 2.07, P < .00001; I2 = 0%, P = .68; Fig. 5).
Figure 5.
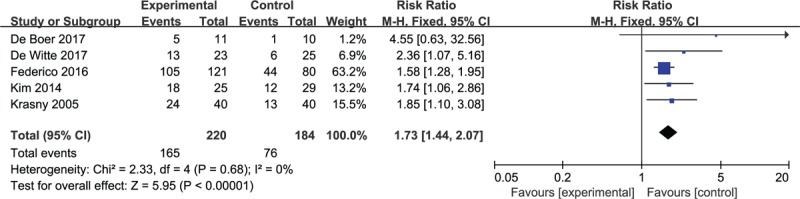
Forest plot of the calcification disappearance rate between 2 groups.
3.7. Constant shoulder score
Five articles with 281 patients provided data on CSS. Pool the data revealed that the patients in UGPL group significantly increased CSS (WMD = 10.49; 95%CI = 6.99 to 13.98, P < .00001; I2 = 0%, P = .89; Fig. 6).
Figure 6.
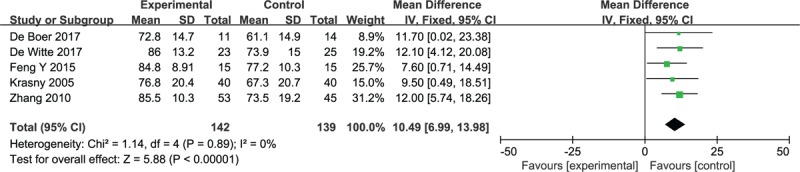
Forest plot of constant shoulder score between 2 groups.
3.8. Need for surgery
Only 3 studies with a total of 226 patients reported relevant data regarding need for surgery. The meta-analysis showed that people need for surgery was significantly lower in the UGPL group (RR = 0.45; 95%CI = 0.25 to 0.78, P = .005; I2 = 0%, P = .98; Fig. 7).
Figure 7.
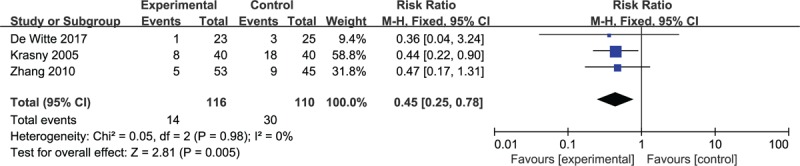
Forest plot of need for surgery between 2 groups.
3.9. Complication
Five studies with a total of 449 patients reported relevant data regarding complication. Pooled data showed no significant difference between 2 groups (RR = 1.79; 95%CI = 0.14 to 22.70, P = .65; I2 = 66%, P = .05; Fig. 8).
Figure 8.
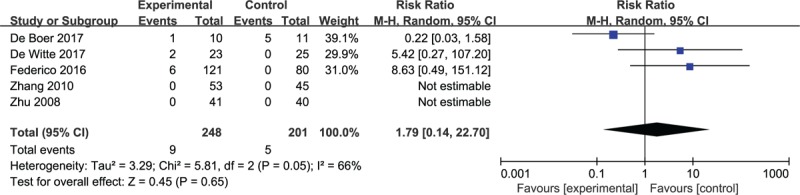
Forest plot of complication between 2 groups.
3.10. Publication bias
Begg plots are shown in Figs. 9–11. Neither VAS nor CSS results showed evidence of publication bias (P Begg test = 0.174 for VAS; P Begg test = 0.806 for CSS), while significant publication bias was apparent for calcification disappearance rate (P Begg test = 0.027).
Figure 9.
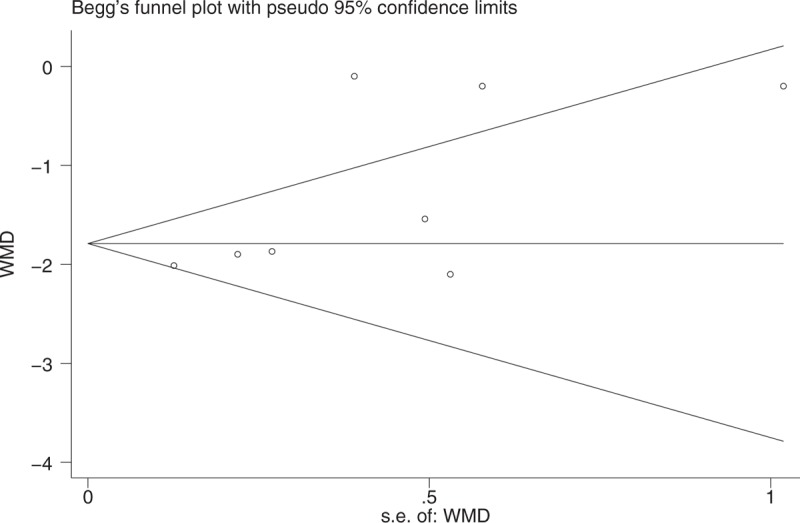
Funnel plots for publication bias test for VAS.
Figure 11.
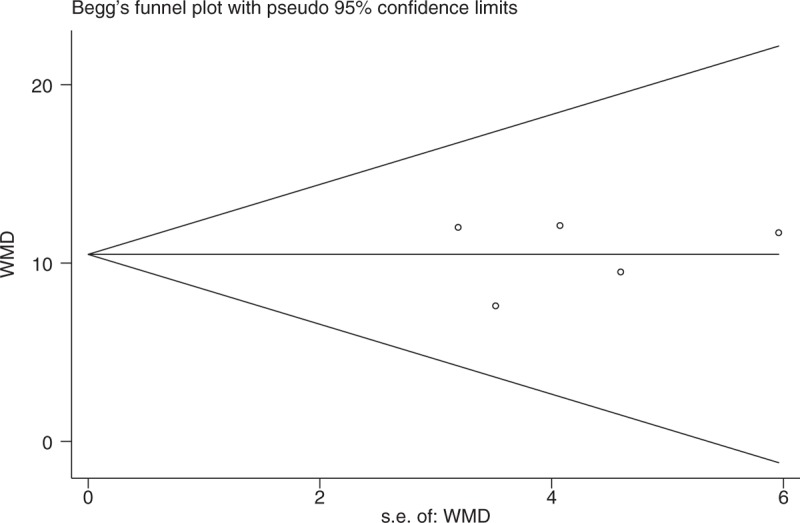
Funnel plots for publication bias test for CSS.
Figure 10.
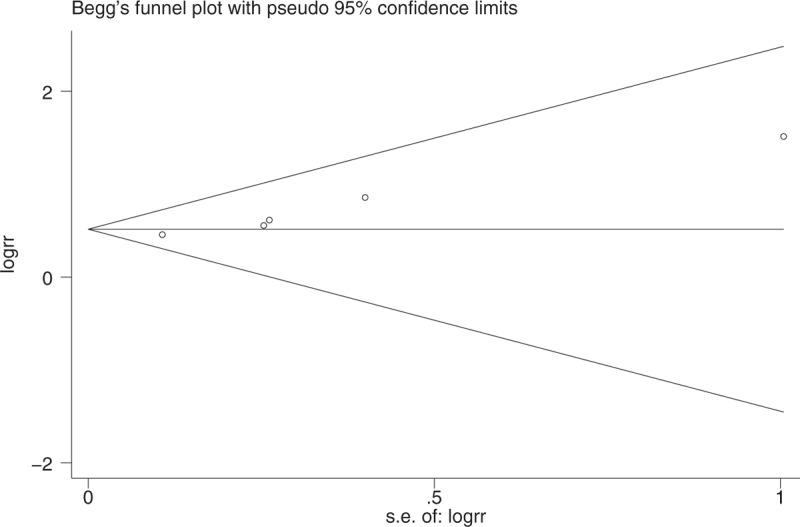
Funnel plots for publication bias test for the calcification disappearance rate.
3.11. Sensitivity analysis
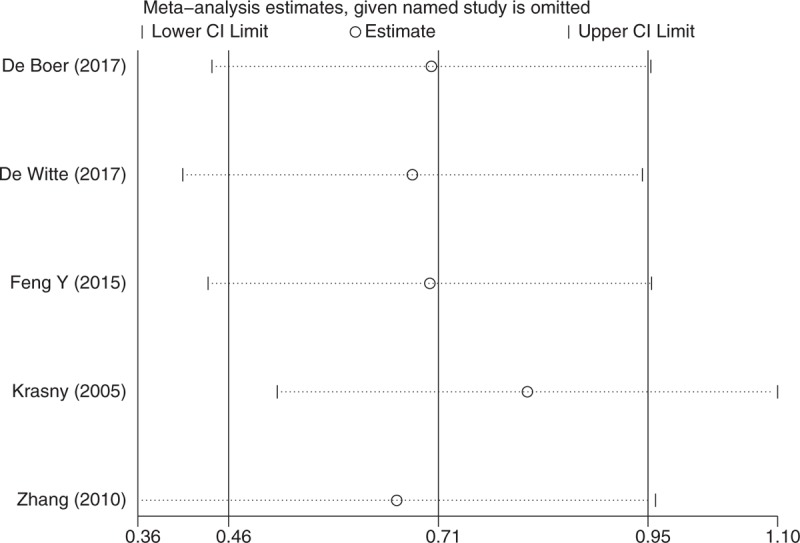
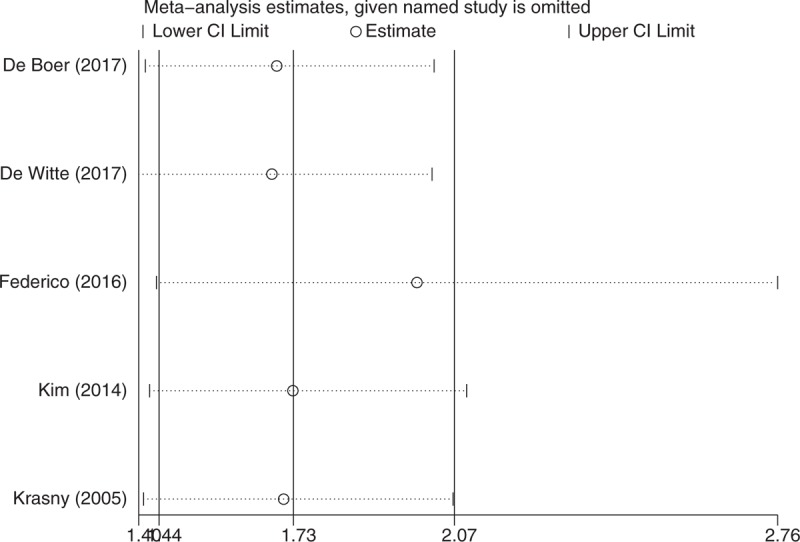
Sensitivity analysis indicated our current data were relatively steady and credible (Figs. 12–14).
Figure 12.
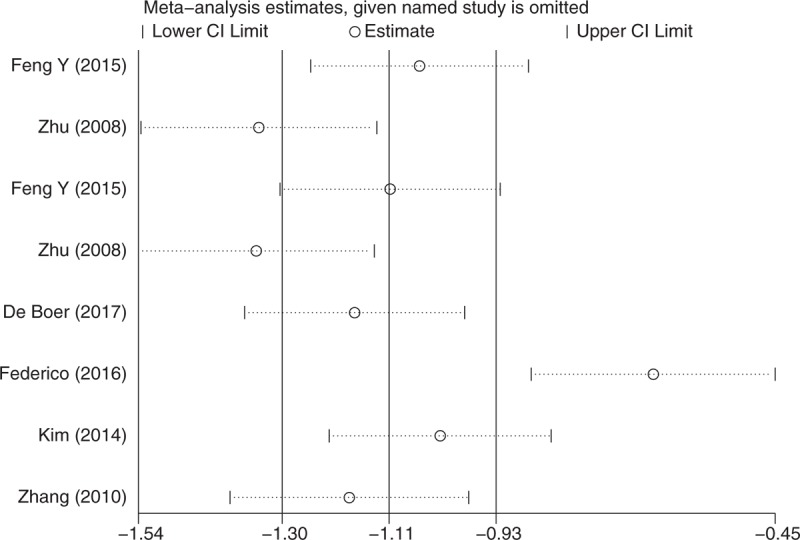
Sensitivity analysis: for VAS.
Figure 14.
Sensitivity analysis: for CSS.
Figure 13.
Sensitivity analysis: for the calcification disappearance rate.
4. Discussion
The pathological processes underlying deposition of calcium hydroxyapatite crystals in the shoulder tendon remain unclear. The condition may be related to fibrosis and necrosis of the tendon, with subsequent degeneration, while others have proposed that the disorder is non-degenerative. Uthoff[32] proposed that calcium deposition is mediated by cartilage cells, and divided it into 4 stages:
-
1.
the pre-calcific phase,
-
2.
formative phase,
-
3.
resorptive phase, and
-
4.
post-calcific phase.
At present, a variety of treatment methods are used for calcific tendinitis, including rest, NSAIDs, physical therapy, SAI, ESWT, and UGPL. Many clinical studies have reported substantial advantages of UGPL, such as significant pain relief, maintenance of function, and reduction of calcium deposits, resulting in enhanced popularity. However, there is still no consensus on the optimal method as several RCTs have failed to draw a unanimous conclusion. To facilitate a clinical decision regarding RCCT treatment, we conducted this meta-analysis to compare the advantages and disadvantages of UGPL to other methods. Indeed, UGPL significantly reduced the VAS, mean size of the deposits, and rate of subsequent surgery, improved CSS, and increased the calcification disappearance rate compared to other treatments, with no increase in complication rate.
The goal of therapy is obviously to control pain and maintain function. Once pain is controlled, function may be maintained through exercises to extend the range of motion and strengthen the rotator cuff. This meta-analysis showed that UGPL was superior for clinical pain relief and shoulder joint function recovery at 12 months follow-up. Federico[30] and De Boer[31] found that the VAS score was significantly lower in the UDPL group than the non-UGPL group. In addition, De Boer[31] reported that Oxford score and patient satisfaction were significantly higher following UGPL than ESWT at 1-year follow-up, while Kim[28] found better ASES and SST scores following UGPL than ESWT.
Recovery of shoulder joint function requires amelioration of postoperative shoulder pain. Patients receiving UGPL were more willing to exercise because the pain level was lighter. Lanza[33] conducted a 10-year follow-up of 287 patients and found better VAS and CSS scores in the UGPL group, results subsequently confirmed by Niazi.[34] Several retrospective studies[35–38] on UGPL for RCCT drew similar conclusions, affirming the safety and effectiveness of UGPL. Few studies have reported on complications of UGPL, such as vagus nerve stimulation and pain.[39,40] Notably, Sconfienza[41] reported a case of suppurative synovitis in 2004 that may have been caused by invasion of joint bursa and incomplete skin disinfection in order to enhance access to the calcification focus.
In view of the good clinical efficacy of UGPL for treatment of RCCT, some practitioners have attempted to improve the technique or combine it with other methods. For example, Sconfienza[42] found that warm physiological saline is better than room temperature physiological saline for irrigation. According to Yoo[37] and Merolla,[39] UGPL combined with SAI or ESWT can achieve acceptable clinical efficacy.
The following limitations of our meta-analysis should be acknowledged. First, the majority of studies lacked allocation concealment or blinding. Second, we included RCTs from different countries and with different diagnostic criteria, which introduced substantial clinical heterogeneity. Third, there were too few trials in this meta-analysis to assess some outcomes such as the mean size of the deposits and need for surgery. Fourth, the quality score of these studies is relatively low, which affects the credibility of this outcome to some extent. Therefore, more trials of high quality, multicenter, and large sample size will be included in the future. Finally, the follow-up times of included studies were relatively short. Therefore, larger scales RCTs with longer follow-up durations are needed to confirm our results.
Current evidence supports the clinical efficacy and safety of ultrasound-guided percutaneous lavage for calcifying tendinitis of rotator cuff. Compared to ESWT, UGPL may provide superior pain relief, restoration and maintenance of function, and calcification clearance. Due to limited quality and quantity of the included trials, additional high-quality prospective clinical studies are required to verify these conclusions.
Acknowledgments
The authors appreciate the work of editors and anonymous reviewers.
Author contributions
Conceptualization: Xiao Chen.
Data curation: Tao Zhang, Yanji Duan, Jing Chen, Xiao Chen.
Formal analysis: Xiao Chen.
Funding acquisition: Tao Zhang, Yanji Duan.
Investigation: Xiao Chen.
Methodology: Xiao Chen.
Resources: Tao Zhang, Yanji Duan.
Software: Jing Chen, Xiao Chen.
Supervision: Jing Chen, Xiao Chen.
Writing – original draft: Tao Zhang.
Writing – review & editing: Xiao Chen.
Xiao Chen orcid: 0000-0001-8782-4309.
Footnotes
Abbreviations: CSS = constant shoulder score, ESWT = extracorporeal shock wave therapy, NSAIDs = nonsteroidal anti-inflammatory drugs, RCCT = Rotator cuff calcific tendonitis, RCT = randomized controlled trial, SAI = subacromial corticosteroid injection, UGPL = ultrasound-guided percutaneous lavage, VAS = visual analogue scale.
Our study has been approved by the ethics committee of The First People's Hospital of Neijiang and People's Hospital of Changshou Chongqing.
The authors have no conflicts of interest to declare.
References
- [1].Harmon PH. Methods and results in the treatment of 2,580 painful shoulders, with special reference to calcific tendinitis and the frozen shoulder. Am J Surg 1958;95:527–44. [DOI] [PubMed] [Google Scholar]
- [2].Louwerens JK, Sierevelt IN, van Hove RP, et al. Prevalence of calcific deposits within the rotator cuff tendons in adults with and without subacromial pain syndrome: clinical and radiologic analysis of 1219 patients. J Shoulder Elbow Surg 2015;24:1588–93. [DOI] [PubMed] [Google Scholar]
- [3].Welfling J, Kahn MF, Desroy M, et al. Calcifications of the shoulder. II. The disease of multiple tendinous calcifications. Rev Rhum Mal Osteoartic 1965;32:325–34. [PubMed] [Google Scholar]
- [4].Bosworth B. Calcium deposits in the shoulder and subacromial bursitis: a survey of 12,122 shoulders. J Am Med Assoc 1941;116:2477–82. [Google Scholar]
- [5].Diehl P, Gerdesmeyer L, Gollwitzer H, et al. Calcific tendinitis of the shoulder. Orthopade 2011;40:733–46. [DOI] [PubMed] [Google Scholar]
- [6].Gosens T, Hofstee DJ. Calcifying tendinitis of the shoulder: advances in imaging and management. Curr Rheumatol Rep 2009;11:129–34. [DOI] [PubMed] [Google Scholar]
- [7].Speed CA, Hazleman BL. Calcific tendinitis of the shoulder. N Engl J Med 1999;340:1582–4. [DOI] [PubMed] [Google Scholar]
- [8].Jacobs R, Debeer P. Calcifying tendinitis of the rotator cuff: functional outcome after arthroscopic treatment. Acta Orthop Belg 2006;72:276–81. [PubMed] [Google Scholar]
- [9].Ark JW, Flock TJ, Flatow EL, et al. Arthroscopic treatment of calcific tendinitis of the shoulder. Arthroscopy 1992;8:183–8. [DOI] [PubMed] [Google Scholar]
- [10].Seil R, Litzenburger H, Kohn D, et al. Arthroscopic treatment of chronically painful calcifying tendinitis of the supraspinatus tendon. Arthroscopy 2006;22:521–7. [DOI] [PubMed] [Google Scholar]
- [11].Arirachakaran A, Boonard M, Yamaphai S, et al. Extracorporeal shock wave therapy, ultrasound-guided percutaneous lavage, corticosteroid injection and combined treatment for the treatment of rotator cuff calcific tendinopathy: a network meta-analysis of RCTs. Eur J Orthop Surg Traumatol 2017;27:381–90. [DOI] [PubMed] [Google Scholar]
- [12].Bannuru RR, Flavin NE, Vaysbrot E, et al. High-energy extracorporeal shock-wave therapy for treating chronic calcific tendinitis of the shoulder: a systematic review. Ann Intern Med 2014;160:542–9. [DOI] [PubMed] [Google Scholar]
- [13].Castillo-Gonzalez FD, Ramos-Alvarez JJ, Rodriguez-Fabian G, et al. Treatment of the calcific tendinopathy of the rotator cuff by ultrasound-guided percutaneous needle lavage. two years prospective study. Muscles Ligaments Tendons J 2014;4:220–5. [PMC free article] [PubMed] [Google Scholar]
- [14].Gerdesmeyer L, Wagenpfeil S, Haake M, et al. Extracorporeal shock wave therapy for the treatment of chronic calcifying tendonitis of the rotator cuff: a randomized controlled trial. JAMA 2003;290:2573–80. [DOI] [PubMed] [Google Scholar]
- [15].Wang CJ, Yang KD, Wang FS, et al. Shock wave therapy for calcific tendinitis of the shoulder: a prospective clinical study with two-year follow-up. Am J Sports Med 2003;31:425–30. [DOI] [PubMed] [Google Scholar]
- [16].Greis AC, Derrington SM, McAuliffe M. Evaluation and nonsurgical management of rotator cuff calcific tendinopathy. Orthop Clin 2015;46:293–302. [DOI] [PubMed] [Google Scholar]
- [17].Vignesh KN, McDowall A, Simunovic N, et al. Efficacy of ultrasound-guided percutaneous needle treatment of calcific tendinitis. Am J Roentgenol 2014;204:148–52. [DOI] [PubMed] [Google Scholar]
- [18].Bazzocchi A, Pelotti P, Serraino S, et al. Ultrasound imaging-guided percutaneous treatment of rotator cuff calcific tendinitis: success in short-term outcome. Br J Radiol 2016;89: 20150407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Sahan MH, Serbest S, Tiftikci U, et al. Reliability of magnetic resonance imaging in ratator cuff and biceps tendon pathologies. J Clin Anal Med 2017;8suppl 4:310–5. [Google Scholar]
- [20].Serbest S, Tiftikci U, Askin A, et al. Preoperative and post-operative sleep quality evaluation in rotator cuff tear patients. Knee Surg Sports Traumatol Arthrosc 2017;25:2109–13. [DOI] [PubMed] [Google Scholar]
- [21].Sahan MH, Serbest S, Tiftikci U, et al. Evaluation of arthroscopic rotator cuff repair results in patients with anterior greater tubercle cysts. J Orthop Surg 2019;27: 2309499019825602. [DOI] [PubMed] [Google Scholar]
- [22].Wang QY, Liu ST, Wei XC, et al. Excroproeal shock wave therapy for calcifying tendinitis of rotator cuff: a meta-analysis. Chin J Front Med Sci (Electronic Version) 2017;9: 1-6+173. [Google Scholar]
- [23].de Witte PB, Selten JW, Navas A, et al. Calcific tendinitis of the rotator cuff: a randomized controlled trial of ultrasound-guided needling and lavage versus subacromial corticosteroids. Am J Sports Med 2013;41:1665–73. [DOI] [PubMed] [Google Scholar]
- [24].de Witte PB, Kolk A, Overes F, et al. Rotator cuff calcific tendinitis: ultrasound-guided needling and lavage versus subacromial corticosteroids: five-year outcomes of a randomized controlled trial. Am J Sports Med 2017;45:3305–14. [DOI] [PubMed] [Google Scholar]
- [25].Krasny C, Enenkel M, Aigner N, et al. Ultrasound-guided needling combined with shock-wave therapy for the treatment of calcifying tendonitis of the shoulder. J Bone Joint Surg Br 2005;87:501–7. [DOI] [PubMed] [Google Scholar]
- [26].Zhu J, Jiang Y, Hu Y, et al. Evaluating the long-term effect of ultrasound-guided needle puncture without aspiration on calcifying supraspinatus tendinitis. Adv Ther 2008;25:1229–34. [DOI] [PubMed] [Google Scholar]
- [27].Zhang J, Ebraheim N, Lause GE. Ultrasound-guided injection for the biceps brachii tendinitis: results and experience. Ultrasound Med Biol 2011;37:729–33. [DOI] [PubMed] [Google Scholar]
- [28].Kim YS, Lee HJ, Kim YV, et al. Which method is more effective in treatment of calcific tendinitis in the shoulder? Prospective randomized comparison between ultrasound-guided needling and extracorporeal shock wave therapy. J Shoulder Elbow Surg 2014;23:1640–6. [DOI] [PubMed] [Google Scholar]
- [29].Feng Y. The study on the short term clinical outcome of the treatment under sonographically guided acupotomy percutaneous neddle·-knife aspiration and lavage technique in calcific tendinitis of the shoulder. Nanjing Univ Chin Med 2015. [Google Scholar]
- [30].Del Castillo-Gonzalez F, Ramos-Alvarez JJ, Rodriguez-Fabian G, et al. Extracorporeal shockwaves versus ultrasound-guided percutaneous lavage for the treatment of rotator cuff calcific tendinopathy: a randomized controlled trial. Eur J Phys Rehabil Med 2016;52:145–51. [PubMed] [Google Scholar]
- [31].De Boer FA, Mocking F, Nelissen EM, et al. Ultrasound guided needling vs radial shockwave therapy in calcific tendinitis of the shoulder: a prospective randomized trial. J Orthop 2017;14:466–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Uhthoff HK, Sarkar K, Maynard JA. Calcifying tendinitis: a new concept of its pathogenesis. Clin Orthop Relat Res 1976;164–8. [PubMed] [Google Scholar]
- [33].Lanza E, Banfi G, Serafini G, et al. Ultrasound-guided percutaneous irrigation in rotator cuff calcific tendinopathy: what is the evidence? A systematic review with proposals for future reporting. Eur Radiol 2015;25:2176–83. [DOI] [PubMed] [Google Scholar]
- [34].Niazi G, Hetta W. The role of ultrasound guided percutaneous needle aspiration and lavage (barbotage) in the treatment of calcific tendinitis. Egypt J Radiol Nucl Med 2015;46:63–70. [Google Scholar]
- [35].del Cura JL, Torre I, Zabala R, et al. Sonographically guided percutaneous needle lavage in calcific tendinitis of the shoulder: short- and long-term results. AJR Am J Roentgenol 2007;189:W128–134. [DOI] [PubMed] [Google Scholar]
- [36].Lin JT, Adler RS, Bracilovic A, et al. Clinical outcomes of ultrasound-guided aspiration and lavage in calcific tendinosis of the shoulder. HSS J 2007;3:99–105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Yoo JC, Koh KH, Park WH, et al. The outcome of ultrasound-guided needle decompression and steroid injection in calcific tendinitis. J Shoulder Elbow Surg 2010;19:596–600. [DOI] [PubMed] [Google Scholar]
- [38].De Zordo T, Ahmad N, Odegaard F, et al. US-guided therapy of calcific tendinopathy: clinical and radiological outcome assessment in shoulder and non-shoulder tendons. Ultraschall Med 2011;32Suppl 1:S117–23. [DOI] [PubMed] [Google Scholar]
- [39].Merolla G, Bianchi P, Porcellini G. Ultrasound-guided subacromial injections of sodium hyaluronate for the management of rotator cuff tendinopathy: a prospective comparative study with rehabilitation therapy. Musculoskelet Surg 2013;97Suppl 1:49–56. [DOI] [PubMed] [Google Scholar]
- [40].Aina R, Cardinal E, Bureau N, et al. Calcific shoulder tendinitis: treatment with modified US-guided fine-needle technique. Radiology 2001;221:455–61. [DOI] [PubMed] [Google Scholar]
- [41].Sconfienza L, Randelli F, Sdao S, et al. Septic bursitis after ultrasound-guided percutaneous treatment of rotator cuff calcific tendinopathy. PM R 2014;6:746–8. [DOI] [PubMed] [Google Scholar]
- [42].Sconfienza LM, Bandirali M, Serafini G, et al. Rotator cuff calcific tendinitis: does warm saline solution improve the short-term outcome of double-needle US-guided treatment? Radiology 2012;262:560–6. [DOI] [PubMed] [Google Scholar]


