Abstract
The prevalence of overweight–obesity has increased sharply among undergraduates worldwide. In 2016, approximately 52% of adults were overweight–obese. This cross-sectional study aimed to investigate the prevalence of overweight–obesity and explore in depth the connection between eating habits and overweight–obesity among Chinese undergraduates.
The study population included 536 undergraduates recruited in Shijiazhuang, China, in 2017. They were administered questionnaires for assessing demographic and daily lifestyle characteristics, including sex, region, eating speed, number of meals per day, and sweetmeat habit. Anthropometric status was assessed by calculating the body mass index (BMI). The determinants of overweight–obesity were investigated by the Pearson χ2 test, Spearman rho test, multivariable linear regression, univariate/multivariate logistic regression, and receiver operating characteristic curve analysis.
The prevalence of undergraduate overweight–obesity was 13.6%. Sex [male vs female, odds ratio (OR): 1.903; 95% confidence interval (95% CI): 1.147–3.156], region (urban vs rural, OR: 1.953; 95% CI: 1.178–3.240), number of meals per day (3 vs 2, OR: 0.290; 95% CI: 0.137–0.612), and sweetmeat habit (every day vs never, OR: 4.167; 95% CI: 1.090–15.933) were significantly associated with overweight–obesity. Eating very fast was positively associated with overweight–obesity and showed the highest OR (vs very slow/slow, OR: 5.486; 95% CI: 1.622–18.553). However, the results of multivariate logistic regression analysis indicated that only higher eating speed is a significant independent risk factor for overweight/obesity (OR: 17.392; 95% CI, 1.614–187.363; P = .019).
Scoremeng = 1.402 × scoresex + 1.269 × scoreregion + 19.004 × scoreeatin speed + 2.546 × scorenumber of meals per day + 1.626 × scoresweetmeat habit and BMI = 0.253 × Scoremeng + 18.592. These 2 formulas can help estimate the weight status of undergraduates and predict whether they will be overweight or obese.
Keywords: eating habits, obesity, overweight, risk factors, undergraduate
1. Introduction
Overweight and obesity are pervasive diseases caused by a variety of factors—such as genetic, environmental, behavioral, social, economic, and cultural factors—that can cause excess energy (lipid) storage in the body.[1] The worldwide prevalence of overweight and obesity has increased sharply over the past decades,[2] and their prevalence among college students has also been increasing. According to a World Health Organization report in 2016, around 52% of adults aged 18 years and above are overweight–obese. At present, overweight and obesity have become a severe global public health issue, affecting the improvement of population quality.[3] Overweight and obesity affect not only the health, quality of life, stature, and somatic function of college students but also their respiratory, cardiovascular, endocrine, and immune systems.[4–6] They also restrict the development of intelligence and psychological characteristics in this population. College students with overweight and obesity are especially prone to various problems such as psychobehavioral deviation and psychological trauma. Juonala et al[7] followed-up with 6328 people with overweight and obesity for 23 years and confirmed that overweight and obesity are early risk factors of future chronic diseases (including coronary heart disease, cerebrovascular disease, type 2 diabetes, and hypertension). Therefore, studies on the risk factors and preventive measures for overweight and obesity in college students have received increasing attention in the field of public health.
Poor eating habits are one of the significant causes of overweight and obesity.[8] Recent studies have shown that eating speed plays a role in obesity[9,10] and diabetes[11–13]; it is, therefore, recommended to chew well and eat slowly. Gradual elevation of blood glucose level is recommended in order to avoid overworking the pancreas by continued and rapid insulin secretion.[14] Studies have also demonstrated that there are several risk factors that can induce overweight and obesity, such as increased intake of high-fat and high-energy food, excessive drinking of carbonated beverages, decreased intake of vegetable fiber, eating snacks, and skipping breakfast.[8] Although the effects of various lifestyle changes on overweight and obesity have been investigated and confirmed in children and working people, they are not well described in the distinctive group of college students. In addition, in considering the abovementioned lifestyle habits as a whole, there are questions about what type of poor behavior is a greater risk factor for overweight and obesity and whether these risk factors are independent of each other. However, these questions have not been simultaneously investigated to date.
In view of the close relationship between the prevalence of overweight–obesity and eating habits, this study aimed to further explore the connection between eating habits and overweight–obesity in Chinese college students, analyze in depth and determine which unhealthy eating behavior is the most critical for overweight–obesity, and verify whether this factor is an independent risk factor for overweight–obesity. We analyzed cross-sectional survey data and created a novel score (Scoremeng) for predicting overweight–obesity in college students in order to curb the prevalence of overweight and obesity and minimize their impact on human health. Our findings provide a scientific basis for managing and preventing overweight and obesity in college students.
2. Materials and methods
2.1. Study population
The participants in our study were 536 undergraduates (including freshmen, sophomores, juniors, and seniors) from Hebei Medical University in Shijiazhuang, China. All students were included in school roll. The present survey was implemented in the form of a strict medical checkup in 2017. The study was approved by the ethics committee of Hebei Medical University, and the study purpose was explained to the participants, who then gave informed consent for participation.
2.2. Anthropometric measurement
For assessing anthropometric status, body mass index (BMI) was calculated from body weight in kilograms divided by the square of height in meters. Subjects with BMI <18.5 kg/m2 were defined as underweight and those with a BMI of 18.5 to 24.9 kg/m2 were defined as having normal weight. In addition, BMI >25 kg/m2 was defined as overweight or obese on the basis of general international criteria.
2.3. Questionnaire survey
This survey included a self-administered questionnaire, in which the participants responded by selecting one of four answers—“very slow/slow”, “ordinary”, “fast”, or “very fast”—to the question “What is your eating speed compared with that of your family and friends who have meals with you?” This question was derived by referring to previous studies.[15,16] The validity of the question is certified given the high level of concordance between friend-reported and self-reported rates of eating. The survey also inquired about the lifestyle factors of the participants, such as grade (freshman, sophomore, junior, or senior), region (urban or rural), frequency of daily meals (twice, three times, four times, or more than four times), breakfast habit (yes or no), on-time meals (yes or no), high-fat diet consumption per week (never, 1–2 days, 3–6 days, or every day), and sweetmeat consumption per week (never, 1–2 days, 3–6 days, or every day).
2.4. Statistical analysis
The results are expressed as mean ± standard error of the mean. The 2-sample t test was used for comparing the mean values of 2 groups and in instances where statistical significance was determined by analysis of variance. The post-hoc 2-tailed Newman–Keuls test was used for comparing 3 or more groups. Associations between BMI and demographic/behavioral characteristics were analyzed by using the Pearson Chi-squared test.
For correlation analysis, the Spearman rho test was used for comparing demographic and behavioral variables. All test results that reached a liberal statistical threshold of P < .2 for each comparison were then entered into a multivariable linear regression model for identifying independently predictive factors of BMI. The risk factors were entered into the same model. Then, the BMI values were converted into natural logarithmic equivalent values for statistical analysis. Variance inflation factors were calculated to quantify the severity of multicollinearity in the multivariate linear regression model. Residual distribution was determined by means of a histogram and the Shapiro–Wilk test; the results demonstrated that the residuals had a well-modeled normal distribution. BMI was compared by the Wilcoxon signed-rank test. Univariate and multivariate logistic regression analyses were performed to calculate the odds ratios (ORs) of each variable for overweight and obese subjects in accordance with its criteria. To certify the independent influence of eating speed on overweight or obesity, the “a × b” interaction—including “eating speed × sex,” “eating speed × region,” “eating speed × number of meals per day,” and “eating speed × sweetmeat habit”—was applied in the multivariate logistic regression analysis. Finally, linear regression analysis was performed to explore the linear correlation between Scoremeng (see below) and BMI. Receiver operating characteristic (ROC) curve analysis was performed to determine the ability of Scoremeng to predict overweight–obesity.
All statistical analyses were performed by using SPSS software (version 21.0; IBM Corp, Beijing, China). P values < .05 were considered statistically significant.
2.5. Establishment of Scoremeng (and Scoreplus) for predicting overweight–obesity
Factors identified as statistically significant indicators of overweight–obesity by single-factor logistic regression analysis were included in a multivariate logistic regression model as well as in Scoremeng.[17] The OR value of each indicator in the multivariate logistic regression model was used as the coefficient and multiplied with the score of the corresponding indicator (the score of an interaction indicator was the average of the relevant indicator scores). The final equation for Scoremeng was derived by adding the multiplication products of each indicator:
 |
Finally, the simplified formula for predicting overweight–obesity was determined to be:
 |
Then, we derived Scoreplus for performing comparisons with Scoremeng. For Scoreplus, statistically significant index scores in the single-factor logistic regression analysis were directly summed:
 |
3. Results
3.1. Participant characteristics
Table 1 presents a summary of participant characteristics. The overall mean participant age was 20 years (range, 17–22 years). Of the 536 participants enrolled in this study, 67 (12.5%) were underweight (BMI < 18.5) and 396 (73.9%) had normal BMI (18.5 ≤ BMI < 25.0); 73 participants (13.6%) had significantly high BMI (BMI ≥25.0). With regard to grade, the participants were distributed as follows: freshmen, 67 (12.5%); sophomores, 202 (37.7%); juniors, 177 (33.0%); and seniors, 90 (16.8%).
Table 1.
Demographic and behavioral characteristics of study participants according to BMI.
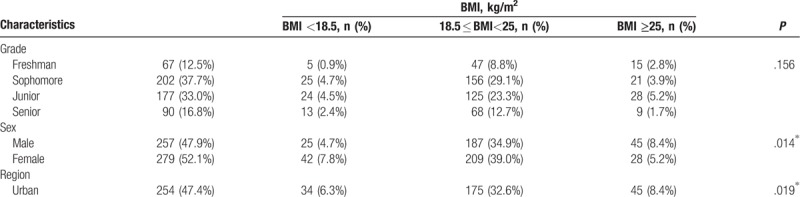
3.2. Association between BMI and demographic/behavioral characteristics of the study participants
Table 1 summarizes the association between BMI and demographic/behavioral characteristics of the participants as well as the proportions of underweight, normal-weight, and overweight participants in accordance with their demographic and behavioral characteristics. BMI was significantly and positively associated with sex (P = .014), region (P = .019), greater eating speed (P for trend < .001), and number of meals per day (P = .018). Sweetmeat habit was also associated with BMI (P = .023).
3.3. Correlation between BMI and participant characteristics
To confirm that sex, region, eating speed, number of meals per day, and sweetmeat habit have an impact on BMI, we further analyzed the correlation of BMI with associated demographic and behavioral characteristics by calculating Spearman correlation coefficients. Sex (ρ = -0.109; P = .012), region (ρ = -0.113; P = .009), eating speed (ρ = 0.168; P < .001), number of meals per day (ρ = -0.134; P = .002), and high-fat diet habit (ρ = 0.091; P = .034) were significantly correlated with BMI (Table 2). In the multivariate linear regression model, with all other variables being held at fixed values, the natural logarithmic BMI remained associated with sex (β = -1.000; P = .001), region (β = -0.734; P = .005), eating speed (β = 0.938; P < .001), number of meals per day (β = -1.147; P < .001), and a high-fat diet habit (β = 0.723; P = .001). However, sweetmeat habit (P > .05) was not obviously associated with BMI in either the Spearman correlation analysis or multivariate linear regression model (Table 2).
Table 1 (Continued).
Demographic and behavioral characteristics of study participants according to BMI.

3.4. Proportional hazards analysis of characteristics related with overweight–obesity in the univariate logistic regression model
Table 3 summarizes the univariate ORs and 95% confidence intervals (95% CIs) for subjects grouped in accordance with general international criteria. The OR for BMI was 1.555 (95% CI, 0.570–4.241) in participants with a normal eating speed relative to those with a very slow/slow eating speed. This figure increased to 3.394 (95% CI, 1.281–8.994) and 5.486 (95% CI, 1.622–18.553), respectively, in participants with fast and very fast eating speeds. Relative to participants who consumed 2 meals per day, the ORs of BMI were 0.290 (95% CI, 0.137–0.612) and 0.190 (95% CI, 0.055–0.657), respectively, in participants who consumed 3 and 4 meals per day. Relative to participants who consumed no sweetmeats in a week, the adjusted ORs of BMI were 2.402 (95% CI, 1.105–5.223), 1.250 (95% CI, 0.433–3.606), and 4.167 (95% CI, 1.090–15.933) in participants who reported consuming sweetmeats 1 to 2 and 3 to 6 days per week and every day of the week, respectively. Male subjects had a higher OR for BMI (1.903; 95% CI, 1.147–3.156) than female subjects. Subjects from urban regions had significantly higher BMI than those from rural regions (OR, 1.935; 95% CI, 1.178–3.240).
Table 2.
Associations between demographic-behavioral characteristics of the participants and the status of BMI.

3.5. Analysis of higher eating speed as an independent risk factor for overweight–obesity
According to the results of univariate logistic proportional regression analysis, the risk factors of overweight–obesity include sex (P = .013), region (P = .010), eating speed (P = .002), number of meals per day (P = .008), and sweetmeat habit (P = .046). We performed multivariate logistic proportional regression analysis to identify the most independent risk factor among these variables and explore the “a × b” interaction (Table 4). Participants with a higher eating speed had a significantly greater risk of overweight–obesity than those with a normal/lower eating speed (OR, 17.392; 95% CI, 1.614–187.363; P = .019; Table 4).
Table 3.
The characteristics and their effect on BMI based on univariate logistic proportional regression analysis.
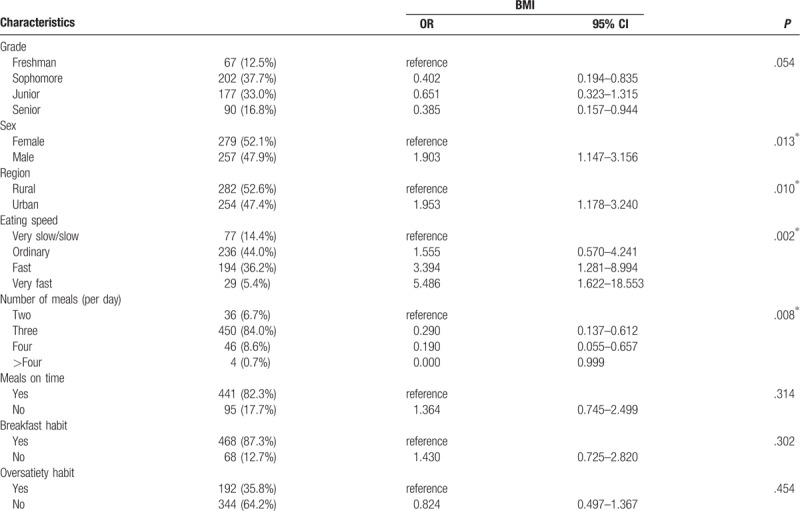
Figure 1A shows the distribution of subjects with BMI values <18.5, 18.5 to 25.0, and ≥25.0 kg/m2 according to sex. Figure 1B shows the distribution of subjects with BMI values <18.5, 18.5 to 25, and ≥25.0 kg/m2 according to region. Figure 1C to F show the distribution of subjects with BMI values <18.5, 18.5 to 25, and ≥25.0 kg/m2 according to eating speed, number of meals per day, high-fat diet habit, and sweetmeat habit, respectively. Figure 2A to F show the relationship of mean BMI with sex, region, eating speed, number of meals per day, high-fat diet habit, and sweetmeat habit according to school grade.
Figure 1.

The distribution of subjects with BMI values <18.5, 18.5–25.0, and ≥25.0 kg/m2 according to sex (A), region (B), eating speed (C), number of meals per day (D), high-fat diet habit (E), and sweetmeat habit (F), respectively.
Figure 2.

The relationship of mean BMI with sex, region, eating speed, number of meals per day, high-fat diet habit, and sweetmeat habit according to school grade.
3.6. Linear correlation between Scoremeng and BMI
The results of linear regression analysis revealed that Scoreplus is not significantly related to BMI (Fig. 3B and Table 5). However, there was a linear correlation between Scoremeng and BMI (P < .05; βmeng = 0.253; bconstantquantity = 18.592; Fig. 3A and Table 5). Thus, we arrived at the following equation:
Figure 3.
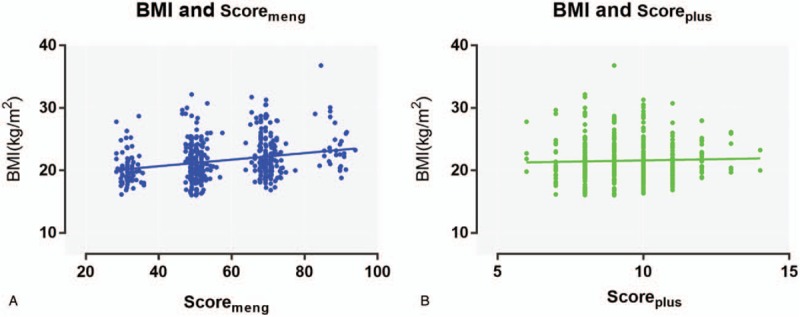
The linear regression analysis. (A) there was a linear correlation between Scoremeng and BMI; (B) Scoreplus is not significantly related to BMI.
Table 3 (Continued).
The characteristics and their effect on BMI based on univariate logistic proportional regression analysis.

Table 5.
The linear regression analysis of Scoremeng (and Scoreplus) for overweight-obesity.

3.7. ROC analysis of the ability of Scoremeng to predict overweight–obesity
We constructed ROC curves to identify an accurate threshold of Scoremeng for predicting BMI (Table 6). Scoremeng was mostly associated with a higher risk of overweight–obesity (area under the curve for BMI, 0.598; 95% CI, 0.529–0.667; P = .007). The optimal predictive threshold of Scoremeng for BMI was 53.26. However, Scoreplus was not a sensitive or specific predictor of overweight–obesity (area under the curve for BMI, 0.495; 95% CI, 0.424–0.567; P = .495; Fig. 4).
Table 4.
The characteristics and their effect on BMI based on multivariate logistic proportional regression analysis.

Figure 4.
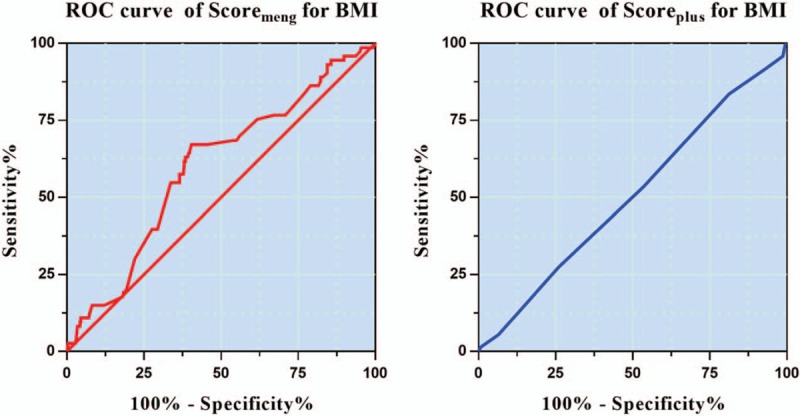
Receiver operating characteristic (ROC) curve analysis of the ability of Scoremeng or Scoreplus to predict overweight–obesity respectively.
Table 6.
Receiver operator characteristic curve analysis of Scoremeng for overweight-obesity.

4. Discussion
This study evaluated the current prevalence of overweight–obesity among Chinese college students and investigated the effects of their eating habits and preferences on the morbidity of overweight–obesity. Our study produced 2 major findings. First, high eating speed is an independent risk factor for overweight and obesity. Second, sex, region, number of meals per day, and sweetmeat habit also have a significant association with overweight and obesity among Chinese college students. Having a fewer number of meals per day and eating more dessert entail a higher risk of overweight and obesity. Men gain weight more easily than do women, and urban students are more prone to gaining weight than rural students.
Several studies have shown a significant positive correlation between eating speed and the morbidity of overweight and obesity in children and adults,[15,16,18,19] which is consistent with the findings of our study. Among the Chinese college students enrolled in this study, the OR for BMI (determined by univariate logistic proportional regression analysis) was 1.555 (95% CI, 0.570–4.241) in participants with a normal eating speed relative to those with a very slow/slow eating speed. This figure increased to 3.394 (95% CI, 1.281–8.994) and 5.486 (95% CI, 1.622–18.553), respectively, in participants with fast and very fast eating speeds. Furthermore, according to the results of multivariate logistic proportional regression analysis, participants with a higher eating speed had a significantly greater risk of overweight–obesity than those with a lower eating speed (OR, 17.392; 95% CI, 1.614–187.363; P = .019). This increased risk can be explained by the following aspects. First, when eating fast, the food enters the body quickly, resulting in a rapid elevation of blood glucose levels. This causes an explosive secretion of insulin, which converts blood glucose into fat, thus promoting overweight and obesity. Second, H1 receptors are distributed in the paraventricular nucleus and ventral hypothalamus. Histamine neuron activation can physiologically influence food intake and eating speed by modulating H1 type of receptors, thus suppressing a psycho-physiological behavior. Therefore, in case of people who eat fast, the fewer the number of times they chew food in their mouth, the fewer the number of histamine neurons activated in their brain. This causes a decrease in the activity of the histamine neurons in suppressing food intake, leading to a decrease in gastrointestinal satiety and, consequently, overeating.[11] Previous studies have found that daily energy intake can increase significantly with an increase in the rate of eating.[20] Of all dietary behaviors, eating speed is the most closely related to overweight and obesity, which suggests that this factor might play a vital role in energy intake. Therefore, health education programs should be implemented to help college students control their eating speed.
In the present study, the morbidity of overweight–obesity in men was higher than that in women, which is consistent with the results of previous studies in China.[21–23] Our results demonstrated that male subjects had a higher OR for BMI (1.903; 95% CI, 1.147–3.156) than female subjects. This difference can be explained by the following factors. Socioeconomic, sociocultural, genetic, and behavioral factors might play an important role in sex-associated differences in overweight–obesity.[23] In Chinese culture, a boy's weight is considered as a symbol of his strength, while girls prefer a slim figure. Compared with boys, girls tend to control their weight and height more easily. According to Zhang et al,[8] boys eat more fried food, drink more sweetened beverages, and spend more time on the TV and computer than do girls. This suggests that boys are more likely to have unhealthy behaviors.
Urban undergraduates gain weight more easily than rural students. In our study, we found that subjects from urban regions had a significantly higher BMI than those from rural regions (OR, 1.935; 95% CI, 1.178–3.240). Yu et al[24] reported a high prevalence of overweight and obesity among middle-aged and elderly people in a downtown area of Beijing. In addition, Herrera et al[25] found that the most vulnerable students in rural areas had the lowest risk of obesity in 2009 and 2013. In urban and rural areas, respectively, the ORs for developing obesity in 2009 were 0.85 (95% CI, 0.82–0.88) and 0.70 (95% CI, 0.64–0.75) in the most vulnerable students and 0.94 (95% CI, 0.91–0.97) and 0.81 (95% CI, 0.74–0.88) in those with moderate vulnerability. The corresponding values in 2013 were 0.96 (95% CI, 0.93–0.98) and 0.89 (95% CI, 0.82–0.96) in the most vulnerable students and 0.99 (95% CI, 95% CI, 0.96–1.02) and 0.94 (95% CI, 0.86–1.02) in students with moderate vulnerability.[25] This finding provides a regional basis for further studies on the risk factors for overweight and obesity.
Can 2 meals per day make you slimmer? In terms of diet frequency, we investigated the relationship between the number of meals per day and overweight–obesity. We found that having 2 meals per day entails a higher risk of overweight and obesity than having 3 or 4 meals per day. The ORs for BMI were 0.290 (95% CI, 0.137–0.612) and 0.190 (95% CI, 0.055–0.657), respectively, in participants who had 3 and 4 meals per day relative to those who had 2 meals per day. According to our findings, most dieters fall into the trap of consuming fewer meals per day for dieting purposes, which is consistent with previous findings.[26] In previous studies, as many as 21.8% of overweight and obese respondents were reported to eat 1 or 2 meals a day as opposed to 16.8% of normal-weight students.[27,28] Similarly, other studies have also confirmed that eating the same amount of food in 1 to 2 meals per day (instead of 5 meals per day, as recommended) will cause faster fat deposition and lead to obesity. Therefore, we should encourage college students to have regular eating habits and avoid “losing weight by dieting.”
With regard to other dietary behaviors, we found that the higher the intake of sugary foods, the more obvious was the overweight or obesity. This finding is supported by previous research.[29,30] Relative to participants who consumed no sweetmeats in a week, the adjusted ORs for BMI were 2.402 (95% CI, 1.105–5.223), 1.250 (95% CI, 0.433–3.606), and 4.167 (95% CI, 1.090–15.933) in participants who consumed sweetmeats 1 to 2 and 3 to 6 days per week and every day of the week, respectively. This trend might be explained by the following reasons. It is well known that the more sugary a food is to eat, the greater will be the risk of developing a variety of oral-health problems, including dental caries and severe periodontal disease with mobile teeth and tooth loss. These conditions will result in decreased occlusal function, finally leading to an unhealthy diet and lifestyle and an increased risk of overweight and obesity. Recent epidemiological studies have also confirmed a link between overweight–obesity and periodontal disease.[31–33] Considering that sugar is an important factor in gaining weight,[34] future intervention measures for preventing overweight and obesity among college students should pay more attention to advising schools to limit the supply of sugary drinks or dessert.
Our study has some limitations. First, the cross-sectional design of this study makes it challenging to build any causal relationship based on the collected data. Prospective and/or interventional studies are necessary to determine the relationship between eating speed and overweight–obesity. The data collection methods used for behavioral datapoints are very vague and might have introduced a risk of bias. Furthermore, according to the guidelines for appreciating the validity of the area under the ROC curve, values between 0.50 and 0.60 indicate failure and those between 0.60 and 0.70 indicate poor accuracy. Given the consistent data in literature linking nonalcoholic fatty liver disease (NAFLD) with obesity/metabolic syndrome, one of the drawbacks of our study is that we did not investigate the applicability of NAFLD in our proposed equations. NAFLD should be investigated as a new criterion for defining metabolic syndrome.
5. Conclusion
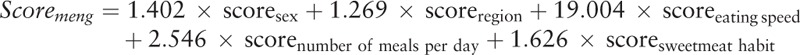 |
In summary, eating speed, sex, region, number of meals per day, and sweetmeat habit are associated with overweight–obesity. Among all dietary behaviors, eating speed is most closely related to overweight and obesity, and high eating speed is an independent risk factor for overweight and obesity. Thus, eating slowly, consuming 3 meals per day, and eating fewer sweetmeats might lead to better dietary habits, which could help prevent overweight–obesity. In addition, differences related to sex and region should be taken into account in health education about overweight–obesity. On the basis of our findings, we have proposed 2 formulas that can help estimate the weight status of undergraduates and predict whether they will be overweight–obese. We have established a practical score (Scoremeng) that might provide individual predictions on overweight–obesity in undergraduates. Scoremeng might help young people identify and avoid high-risk factors for overweight–obesity. Our study subjects were undergraduates, which is a highly representative population. It is necessary to conduct further prospective studies to determine the impact of the most significant risk factor among young people of other age groups.
Acknowledgments
We are thankful to all respondents of this study and workers from the long-term care facilities for their cooperation. We also wish to thank Zhi-Ting Shao for providing statistical assistance and suggestions during the submission process. We did not receive any writing assistance.
Author contributions
Conceptualization: Jia-xu Weng.
Data curation: Jia-xu Weng, Ling-bing Meng.
Formal analysis: Qing-qing Wang, Qi Xie.
Investigation: Hui-bin Liu, Guan-yin Jiang, Ling-bing Meng.
Methodology: Qi Xie.
Project administration: Meng-jie Shan, Yuan-meng Zhang.
Resources: Yang-Fan Zou, Peng Guo, Hui-bin Liu, Ling-bing Meng.
Software: Ya-Lun Dai.
Validation: Yuan-meng Zhang.
Visualization: Guan-yin Jiang.
Writing – original draft: Meng-jie Shan.
Writing – review & editing: Qing-qing Wang.
Footnotes
Abbreviations: BMI = body mass index, CI = confidence interval, NAFLD = nonalcoholic fatty liver disease, OR = odds ratio, ROC = receiver operating characteristic.
L-BM, QX, M-JS, and Y-FZ contributed equally to this work.
The authors declare no conflict of interest. The funding sponsors had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript, and in the decision to publish the results.
References
- [1].Campbell K, Peebles R. Eating disorders in children and adolescents: state of the art review. Pediatrics 2014;134:582–92. [DOI] [PubMed] [Google Scholar]
- [2].Ha KH, Kim DJ. Corrigendum: correction of acknowledgments: epidemiology of childhood obesity in Korea. Endocrinol Metab (Seoul) 2017;32:144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Bhardwaj S, Misra A, Khurana L, et al. Childhood obesity in Asian Indians: a burgeoning cause of insulin resistance, diabetes and sub-clinical inflammation. Asia Pac J Clin Nutr 2008;17 suppl 1:172–5. [PubMed] [Google Scholar]
- [4].Morrison JA, Barton BA, Biro FM, et al. Overweight, fat patterning, and cardiovascular disease risk factors in black and white boys. J Pediatr 1999;135:451–7. [DOI] [PubMed] [Google Scholar]
- [5].Owen CG, Whincup PH, Orfei L, et al. Is body mass index before middle age related to coronary heart disease risk in later life? Evidence from observational studies. Int J Obes (Lond) 2009;33:866–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Raghuveer G. Lifetime cardiovascular risk of childhood obesity. Am J Clin Nutr 2010;91:1514S–9S. [DOI] [PubMed] [Google Scholar]
- [7].Juonala M, Magnussen CG, Berenson GS, et al. Childhood adiposity, adult adiposity, and cardiovascular risk factors. N Engl J Med 2011;365:1876–85. [DOI] [PubMed] [Google Scholar]
- [8].Zhang T, Cai L, Ma L, et al. The prevalence of obesity and influence of early life and behavioral factors on obesity in Chinese children in Guangzhou. BMC Public Health 2016;16:954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Ohkuma T, Hirakawa Y, Nakamura U, et al. Association between eating rate and obesity: a systematic review and meta-analysis. Int J Obes (Lond) 2015;39:1589–96. [DOI] [PubMed] [Google Scholar]
- [10].Lee JS, Mishra G, Hayashi K, et al. Combined eating behaviors and overweight: eating quickly, late evening meals, and skipping breakfast. Eat Behav 2016;21:84–8. [DOI] [PubMed] [Google Scholar]
- [11].Otsuka R, Tamakoshi K, Yatsuya H, et al. Eating fast leads to insulin resistance: findings in middle-aged Japanese men and women. Prev Med 2008;46:154–9. [DOI] [PubMed] [Google Scholar]
- [12].Sakurai M, Nakamura K, Miura K, et al. Self-reported speed of eating and 7-year risk of type 2 diabetes mellitus in middle-aged Japanese men. Metabolism 2012;61:1566–71. [DOI] [PubMed] [Google Scholar]
- [13].Radzeviciene L, Ostrauskas R. Fast eating and the risk of type 2 diabetes mellitus: a case-control study. Clin Nutr 2013;32:232–5. [DOI] [PubMed] [Google Scholar]
- [14].Takamura T, Sakurai M, Nakamura M, et al. Factors associated with improvement of fasting plasma glucose level by mealtime dosing of a rapid-acting insulin analog in type 2 diabetes. Diabetes Res Clin Pract 2007;75:278–84. [DOI] [PubMed] [Google Scholar]
- [15].Ford AL, Bergh C, Sodersten P, et al. Treatment of childhood obesity by retraining eating behaviour: randomised controlled trial. BMJ 2009;340:b5388. [DOI] [PubMed] [Google Scholar]
- [16].Sonoda C, Fukuda H, Kitamura M, et al. Associations among obesity, eating speed, and oral health. Obes Facts 2018;11:165–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Zeng Y, Mayne N, Yang CJ, et al. A nomogram for predicting cancer-specific survival of TNM 8th edition stage I non-small-cell lung cancer. Ann Surg Oncol 2019;[Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- [18].Tanihara S, Imatoh T, Miyazaki M, et al. Retrospective longitudinal study on the relationship between 8-year weight change and current eating speed. Appetite 2011;57:179–83. [DOI] [PubMed] [Google Scholar]
- [19].Zhu B, Haruyama Y, Muto T, et al. Association between eating speed and metabolic syndrome in a three-year population-based cohort study. J Epidemiol 2015;25:332–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Otsuka R, Tamakoshi K, Yatsuya H, et al. Eating fast leads to obesity: findings based on self-administered questionnaires among middle-aged Japanese men and women. J Epidemiol 2006;16:117–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Yi X, Yin C, Chang M, et al. Prevalence and risk factors of obesity among school-aged children in Xi’an, China. Eur J Pediatr 2012;171:389–94. [DOI] [PubMed] [Google Scholar]
- [22].Guo X, Zheng L, Li Y, et al. Prevalence and risk factors of being overweight or obese among children and adolescents in northeast China. Pediatr Res 2013;74:443–9. [DOI] [PubMed] [Google Scholar]
- [23].Song Y, Wang HJ, Ma J, et al. Secular trends of obesity prevalence in urban Chinese children from 1985 to 2010: gender disparity. PLoS One 2013;8:e53069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Yu DN, Xian TZ, Wang LJ, et al. [Analysis of body composition and resting metabolic rate of 858 middle-aged and elderly people in urban area of Beijing]. Zhonghua Liu Xing Bing Xue Za Zhi 2018;39:686–8. [DOI] [PubMed] [Google Scholar]
- [25].Herrera JC, Lira M, Kain J. [Socioeconomic vulnerability and obesity in Chilean schoolchildren attending first grade: comparison between 2009 and 2013]. Rev Chil Pediatr 2017;88:736–43. [DOI] [PubMed] [Google Scholar]
- [26].Zalewska M, Maciorkowska E. Selected nutritional habits of teenagers associated with overweight and obesity. PeerJ 2017;5:e3681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Sygit K, Kollataj W, Gozdziewska M, et al. Lifestyle as an important factor in control of overweight and obesity among schoolchildren from the rural environment. Ann Agric Environ Med 2012;19:557–61. [PubMed] [Google Scholar]
- [28].Kulovitz MG, Kravitz LR, Mermier C, et al. Potential role of meal frequency as a strategy for weight loss and health in overweight or obese adults. Nutrition 2014;30:386–92. [DOI] [PubMed] [Google Scholar]
- [29].Malik VS, Willett WC, Hu FB. Sugar-sweetened beverages and BMI in children and adolescents: reanalyses of a meta-analysis. Am J Clin Nutr 2009;89:438–9. author reply 439-440. [DOI] [PubMed] [Google Scholar]
- [30].Olsen NJ, Heitmann BL. Intake of calorically sweetened beverages and obesity. Obes Rev 2009;10:68–75. [DOI] [PubMed] [Google Scholar]
- [31].Saito T, Shimazaki Y, Sakamoto M. Obesity and periodontitis. N Engl J Med 1998;339:482–3. [DOI] [PubMed] [Google Scholar]
- [32].Saito T, Shimazaki Y. Metabolic disorders related to obesity and periodontal disease. Periodontol 2000 2007;43:254–66. [DOI] [PubMed] [Google Scholar]
- [33].Chaffee BW, Weston SJ. Association between chronic periodontal disease and obesity: a systematic review and meta-analysis. J Periodontol 2010;81:1708–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Malik VS, Popkin BM, Bray GA, et al. Sugar-sweetened beverages, obesity, type 2 diabetes mellitus, and cardiovascular disease risk. Circulation 2010;121:1356–64. [DOI] [PMC free article] [PubMed] [Google Scholar]


