Abstract
Background
The aim of this trial was to comparatively evaluate Icon® resin infiltration and Clinpro™ XT varnish in restoring aesthetics of white spot lesions (WSLs) present post-orthodontic treatment.
Materials and methods
Two hundred forty WSLs were detected in 193 teeth of 12 patients. The participants were analysed—before intervention (T0), immediately after intervention (T1), 3 months later (T2) and 6 months later (T3), with a 1:1 allocation ratio for the application of Icon® resin infiltration and Clinpro™ XT varnish. Using a computer-generated allocation sequence, block randomization was done. A spectrophotometer was used to assess the colour of WSLs and the adjacent enamel, while a DIAGNOdent® was used to assess the fluorescence loss.
Results
Immediately after the intervention, Icon® resin infiltration showed statistically significant better improvement than Clinpro™ XT varnish in restoring the colour (p = 0.000); however, at 3 (p = 0.001) and 6 months (p = 0.000), this was reversed. Except at 3 months, the fluorescence loss sequentially reduced more for Icon® resin infiltration (4.48 ± 1.42 at T0 to 1.48 ± 0.81 at T3) and was not statistically significant.
Conclusions
Clinpro™ XT varnish showed significantly better improvement than Icon® resin infiltration in restoring the colour and lightness of the WSLs at 3 and 6 months. The fluorescence loss significantly recovered with both intervention methods between immediate application and at 6 months. However, Clinpro™ XT varnish-treated WSLs showed a statistically significant difference compared to the adjacent sound enamel at 6 months.
Keywords: White spot lesions, Icon® resin infiltration, Clinpro™ XT varnish
Background
Aesthetics is one of the cornerstone objectives of orthodontic treatment. One of the deleterious effects of orthodontic treatment, primarily caused due to poor oral hygiene maintenance, is the occurrence of white spot lesions (WSLs) [1].
The management of WSLs can be divided into prevention (prior to the formation of WSLs), intervention (during the course of orthodontic treatment) and treatment (after the completion of orthodontic treatment). In the prevention and intervention categories, fluorides in the form of varnish, toothpaste, mouthwash, sealant and miswaks [2]; CPP-ACP, NovaMin®; laser therapy; silver nanoparticles; and ozone have been used extensively [3–7]. However, the clinicians often encounter WSLs post-debonding. The effects of the prevention methods are inadequate due to their effectiveness being restricted to only remineralizing the superficial surface of the lesion and not the body of the lesion [8].
The treatment of the WSLs depends on its severity. The mild forms of WSLs can be left to natural remineralization which occurs over a period of 1 year [1, 9] and through other means such as CPP-ACP [3, 10] and fluoride varnishes [11]. The moderate and severe forms can be treated using bleaching, microabrasion, resin infiltration and restorations [12, 13].
The recent emphasis on the mini aesthetics of tooth such as its colour, texture and enamel translucency has created more concern among patients and orthodontists. This augurs an immediate solution.
With Icon® resin infiltration (DMG America, Englewood, NJ, USA), its acid etchant—15% hydrochloric acid—removes the surface layer of the decalcified area due to its penetration depth of 58 ± 37 μm. [14, 15]. This opens up access to the body of the lesion which allows the resin to occlude the pores. The body of the lesion is rendered watertight by means of the resin which has a refractive index (RI Icon® = 1.44) close to that of healthy enamel (RI = 1.63) [14] and also helps in stopping the diffusion of acids by creating a barrier within the lesion and not on the surface [16, 17].
Icon® resin infiltration has been proved to provide immediate restoration of aesthetics of mild WSLs present post-orthodontic treatment to match that of the adjacent sound enamel [18, 19]. It has been shown to remain durable for 6 months [18] with no significant changes at 12 and 24 months [20]. With moderate lesions, a sequential improvement was seen to occur over a period of time [19]. The fluorescence loss of the WSLs significantly recovered immediately with resin infiltration and remained unchanged at the end of 6 weeks in artificially created WSLs [21]. These factors establish Icon® resin infiltration as a gold standard intervention method in aesthetic restoration of white spot lesions.
Resin-modified glass ionomer cement contains fluoroaluminosilicate glass. The fluoride reacts at the surface to provide an immediate release, while the bulk of the glass matrix offers a reservoir of fluoride for sustained release [22, 23] which is said to provide remineralization.
Clinpro™ XT varnish (3M ESPE, Pymble, New South Wales, Australia), an RMGIC product, has been widely used previously for treating dentinal hypersensitivity [24, 25]. In orthodontics, it is shown to be effective in preventing WSLs from occurring during orthodontic treatment [23, 26, 27] and treating artificially induced demineralized areas [28]. However, its efficacy in treating WSLs present post-orthodontic treatment has not yet been tested.
Specific objective
With both Icon® resin infiltration and Clinpro™ XT varnish, being minimally invasive and site-specific in office single sitting procedures containing composite resin, the aim of this randomized clinical trial was to comparatively evaluate the efficacy of Clinpro™ XT varnish against the ‘gold standard’ Icon® resin infiltration in restoring the aesthetics of the enamel affected by white spot lesions post-orthodontic treatment.
Materials and methods
The study was conducted at the Department of Orthodontics, Sri Ramachandra Institute of Higher Education and Research after the approval from the University’s Institutional Ethics Committee [number: CSP/16/SEP/51/280 dated October 4, 2016].
Trial design
This was a parallel-group, randomized, active-controlled trial with a 1:1 allocation ratio for the application of Icon® resin infiltration and Clinpro™ XT varnish.
Participants, eligibility criteria and settings
Fifty patients who had fixed orthodontic appliances removed during April 2017 were screened for WSLs using Gorelick’s scale [29], and only mild and moderate lesions were considered. This was confirmed using a DIAGNOdent® (KAVO Dental Corporation, Lake, Zurich, IL, USA). Only WSLs having fluorescence loss (Q) scores of 2–9 were considered.
Inclusion criteria
Patients within 14–30 years of age
Symmetrical number of permanent teeth in each arch (mesial to second molars)
Exclusion criteria
Active carious lesions
Facial surface restorations
Deciduous teeth
Fluorosis
Intrinsic and extrinsic strains
Enrollment
A consent form was obtained from those participants willing to be part of the trial.
Sample calculation
Calculations [colour change (ΔE) threshold value = 3.0, d = 0.5, α error = 0.05 and power of study = 85%] were based on the study by Knosel et al. [18] (219 WSLs; 111 control, 108 treatment) to detect a clinically relevant difference between the two trial arms. This indicated that 115 non-cavitated, unrestored WSLs were required in each arm.
Randomization
Using a computer-generated programme (www.randomization.com), block randomization allocation sequence [AABB; ABBA; BBAA; BAAB (A-Icon® resin infiltration, B-Clinpro™ XT varnish)] was generated to equally distribute the intervention methods.
A total of 240 non-cavitated, unrestored WSLs after multibracket treatment were detected in 193 teeth of 12 patients [7 females (18 years ± 2 months), 5 males (20 years ± 6 months)] and formed a part of the study.
Allocation concealment and blinding
The participants were blinded until the allocation of the intervention method. Further blinding was not possible as the intervention methods had different techniques of material application.
Intervention
All the procedures were performed by the same clinician. On completion of orthodontic treatment, residual composite cleanup and polishing were done.
The VITA Easyshade® advance spectrophotometer (VITA Zahnfabrik, Bad Sackingen, Germany) was used to objectively assess the colour of WSLs and the adjacent sound enamel, using the Munsell system: CIE colour parameters (ΔE): L, a and b.
L* refers to the lightness coordinate, and its value ranges from 0 for perfect black to 100 for perfect white. a* and b* are the chromaticity coordinates in the red-green axis and yellow-blue axis, respectively [30, 31].
Similarly, the laser fluorescence method, DIAGNOdent®, was used to assess the fluorescence loss (Q) of WSLs and the adjacent sound enamel present around the lesions.
The DIAGNOdent® illuminates the teeth with blue laser light. The tooth dentin contains atoms called fluorophores which fluoresce green when illuminated with blue laser light. When a WSL is present, it appears as a black area surrounded by green reflected colour and this is seen as fluorescence loss [32].
Intervention methods
Icon® resin infiltration
First, Icon® Etch, DMG, was applied over the WSLs for 2 min. This was followed by water rinsing and air blowing. Then, Icon® Dry, DMG, was applied for 30 s and air blown. Using the provided sponge applicator, Icon® Infiltrant, DMG, was rubbed on and left for 3 min. Subsequently, it was light-cured for 60 s.
CLINPRO™ XT varnish
Thirty-seven percent orthophosphoric acid gel was applied for 15 s. On a paper pad, the paste and liquid components were mixed for 10–15 s using an agate spatula and applied over the WSLs. Subsequently, it was light-cured for 20 s.
Both the treatment methods were assessed before intervention (baseline) [T0], immediately after intervention [T1], 3 months later [T2] and 6 months later [T3].
Photographs were taken during each time period, and the size and location of the WSLs were mapped at T0 for the exactness of the readings at each time interval.
Outcomes
The primary outcome measure was the difference in colour and fluorescence values between the treatment groups over a period of 6 months, and the secondary outcome measure was the difference within the treatment groups.
Statistical analysis
The data was analysed with IBM.SPSS statistics software, version 23.0. Kolmogorov-Smirnov’s test was used to check the normality of the data. To find the significant difference within the groups, at different time intervals, a one-way repeated measures ANOVA was used followed by post hoc Tukey test. Between the groups, independent Student’s t test was used for the intergroup comparison.
Error of method (Table 1)
Table 1.
Error assessment results
| Parameter | Valid (n) | Mean | Minimum | Maximum | Range | SD |
|---|---|---|---|---|---|---|
| WSL on the maxillary tooth | ||||||
| L | 3 | 78.54 | 78.44 | 78.64 | 0.20 | 0.068 |
| a | 3 | 0.86 | 0.47 | 1.25 | 0.78 | 0.258 |
| b | 3 | 18.33 | 18.12 | 18.54 | 0.42 | 0.149 |
| WSL on the mandibular tooth | ||||||
| L | 3 | 74.45 | 74.37 | 74.53 | 0.16 | 0.048 |
| a | 3 | 0.92 | 0.52 | 1.32 | 0.80 | 0.293 |
| b | 3 | 16.69 | 16.48 | 16.90 | 0.42 | 0.131 |
WSL white spot lesions, L lightness, a red-green axis, b yellow-blue axis
The L*a*b* values of one white spot lesion each in the upper and lower arch of one patient were recorded in vivo three times on three consecutive days. The ranges of variance due to measurement error for L value were 0.20 units for the WSL on the maxillary tooth and 0.16 units for WSL on the mandibular tooth. This indicates precision in measurements recorded with spectrophotometer when compared to previous results [33]. All measurements were carried out under normalized conditions to make certain their accuracy and reproducibility.
Results
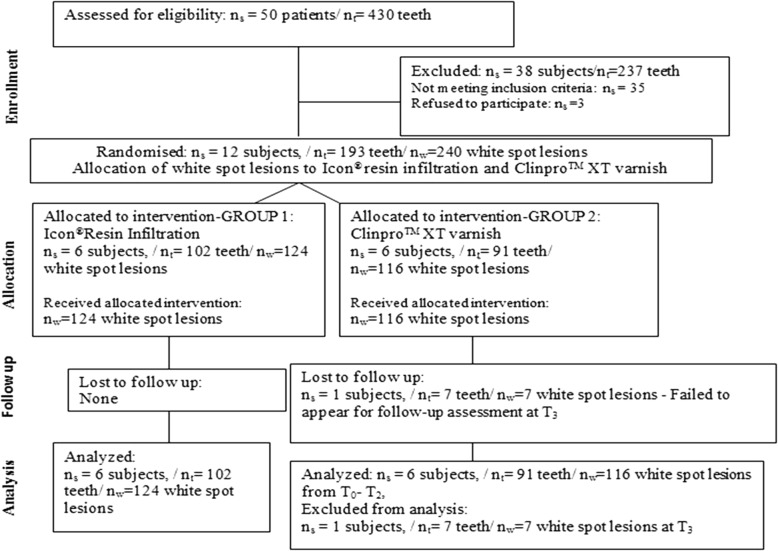
Baseline data and recruitment (Fig. 1)
Fig. 1.
Participant flow and numbers analysed
One hundred twenty-four white spot lesions present in 102 teeth of 6 patients received the allocated intervention method of Icon® resin infiltration, while 116 white spot lesions present in 91 teeth of 6 patients received the allocated intervention method of Clinpro™ XT varnish. At T3, 1 patient under the Clinpro™ XT varnish intervention method was lost to follow-up.
Outcomes and estimation
Analysis of lightness (L) values
Intergroup comparison (Table 2).
Table 2.
Intergroup and intragroup comparison of lightness values at various time intervals
| L values of Icon® resin infiltration | l values of Clinpro™ XT varnish | Intergroup comparison | Intragroup comparison | ||
|---|---|---|---|---|---|
| Icon® resin infiltration | Clinpro™ XT varnish | ||||
| T0 | 73.60 ± 7.71 | 74.62 ± 7.33 | p = 0.295 | T0 vs T1, p = 0.000** | T0 vs T1, p = 0.000** |
| T1 | 78.37 ± 5.94 | 78.93 ± 5.40 | p = 0.446 | T1 vs T2,p = 0.211 | T1 vs T2, p = 0.003** |
| T2 | 80.08 ± 6.46 | 81.68 ± 5.55 | p = 0.041* | T2 vs T3, p = 0.168 | T2 vs T3, p = 0.069 |
| T3 | 81.88 ± 6.27 | 83.69 ± 5.29 | p = 0.017* | T0 vs T3, p = 0.000** | T0 vs T3, p = 0.000** |
| Adjacent sound enamel | 81.67 ± 4.69 | 82.73 ± 4.66 | p = 0.117 | T3 vs adjacent sound enamel, p = 0.999 | T3 vs adjacent sound enamel, p = 0.761 |
Statistical Tests: intergroup comparison—independent Student’s t test; intragroup comparison—one-way repeated measures ANOVA
L lightness, T0 before intervention, T1 immediate after intervention, T2 3 months, T3 6 months
*p < 0.05, **p < 0.01
Clinpro™ XT varnish showed more increase in the L values compared with Icon® resin infiltration, which was statistically significant at T2 and T3.
Intragroup comparison (Table 2)
In Icon® resin infiltration and Clinpro™ XT varnish, a statistically significant increase in the L value was seen from T0 to T1.
In both groups, a statistically significant overall improvement was seen in the L value from T0 to T3.
Analysis of colour changes (ΔE) (Table 3)
Table 3.
a and b values and intergroup comparison of colour changes at various time intervals
| Adjacent sound enamel | T0 | T1 | ΔE1 (T0–T1) | T2 | ΔE2 (T0–T2) | T3 | ΔE3 (T0–T3) | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| a | b | a | b | a | b | a | b | a | b | ||||
| Icon® resin infiltration | 0.20 ± 1.54 | 26.30 ± 7.78 | 0.026 ± 1.76 | 18.39 ± 5.31 | − 0.29 ± 1.38 | 21.47 ± 7.32 | 5.68 ± 1.24 | − 0.37 ± 1.18 | 21.41 ± 6.11 | 7.19 ± 1.17 | − 0.57 ± 1.71 | 23.34 ± 10.93 | 9.66 ± 1.42 |
| Clinpro™ XT varnish | − 0.37 ± 1.14 | 24.08 ± 5.85 | − 0.51 ± 1.41 | 17.71 ± 4.08 | − 0.58 ± 1.23 | 19.58 ± 6.89 | 4.61 ± 1.13 | − 0.63 ± 1.06 | 20.74 ± 6.66 | 7.68 ± 1.12 | − 1.03 ± 1.49 | 23.74 ± 6.66 | 10.59 ± 1.21 |
| Inter group comparison of colour changes | 0.000** | 0.001** | 0.000** | ||||||||||
Statistical tests: intergroup comparison—independent Student’s t test
a red-green axis, b yellow-blue axis, ΔE colour changes, T0 before intervention, T1 immediate after intervention, T2 3 months, T3 6 months
**p < 0.01
Icon® resin infiltration showed a statistically significant colour change value from T0 to T1 (ΔE1) than Clinpro™ XT varnish.
Clinpro™ XT varnish showed a statistically significant colour change value from T0 to T2 (ΔE2) and from T0 to T3 (ΔE3) than Icon® resin infiltration.
Analysis of fluorescence loss (Q)
Intergroup comparison (Table 4).
Table 4.
Intergroup and intragroup comparison of fluorescence loss (Q) values at various time intervals
| Q values of Icon® resin infiltration | Q values of Clinpro™ XT varnish | Intergroup comparison | Intragroup comparison | ||
|---|---|---|---|---|---|
| Icon® resin infiltration | Clinpro™ XT varnish | ||||
| T0 | 4.48 ± 1.42 | 4.60 ± 1.29 | p = 0.498 | T0 vs T1, p = 0.000** | T0 vs T1, p = 0.000** |
| T1 | 2.84 ± 1.53 | 3.14 ± 1.20 | p = 0.094 | T1 vs T2, p = 0.000** | T1 vs T2, p = 0.000** |
| T2 | 2.06 ± 1.05 | 2.05 ± 0.83 | p = 0.935 | T2 vs T3, p = 0.000** | T2 vs T3, p = 0.000** |
| T3 | 1.48 ± 0.81 | 1.51 ± 0.72 | p = 0.767 | T0 vs T3, p = 0.000** | T0 vs T3, p = 0.000** |
| Adjacent Sound Enamel | 1.06 ± 0.58 | 1.08 ± 0.51 | p = 0.80 | T3 adjacent sound enamel, p = 0.050 | T3 adjacent sound enamel, p = 0.016* |
Statistical tests: intergroup comparison—independent Student’s t test; intragroup comparison—one-way repeated measures ANOVA
Q fluorescence loss, T0 before intervention, T1 immediate after intervention, T2 3 months, T3 6 months
*p < 0.05, **p < 0.01
At all other time points except T2, Q value reduction was seen more with Icon® resin infiltration when compared to Clinpro™ XT varnish. However, on comparison, it was not significant.
Intragroup comparison (Table 4).
In both groups, a statistically significant fluorescence loss amelioration was seen from T0 to T1 to T2 to T3.
At T3, in both groups, the amelioration of the fluorescence loss brought the values close to that of the adjacent sound enamel, which was not statistically significant for Icon® resin infiltration but statistically significant for Clinpro™ XT varnish.
Discussion
A parallel-group trial as opposed to a split study design was carried out to avoid any treatment bias to mitigate any carry-across effect of fluorides present in Clinpro™ XT varnish. [34–36]
The difference in the refractive index of the enamel and lesions’ crystals contributes to the whitish nature of the WSLs [37]. WSLs have lower L* values due to the large portions of transmitted light being absorbed and scattered within the micropores of the body of the lesion [38–40]. Hence, the lightness value is of vital importance.
As expected, following the application of Icon® resin infiltration, a significant increase was seen immediately in the lightness of the WSLs, suggestive of an immediate increase in enamel reflectivity (T1). The subsequent increase from T1 to T3 was not statistically significant, showing the durable nature of the material (Table 2).
Surprisingly with Clinpro™ XT varnish, a significant increase was seen immediately in the lightness of the WSLs with its application. It can be hypothesized that the usage of 37% orthophosphoric acid would have penetrated and removed the surface layer of the WSL, opening up access to the body of the lesion. The PC would have further increased with the usage of low viscous resin HEMA. The presence of Bis-GMA could have enhanced the resin reactivity and reflectivity, aiding in the immediate improvement in the optical properties of the WSLs. At T2, a significant increase was further seen in the lightness and this could be attributed to the release of fluoride from the fluoroaluminosilicate glass particles. The small amount of increase seen from T2 to T3 was probably due to the sustained release of fluoride and calcium glycerophosphate from the reservoir of the glass matrix. Further, the overall change seen with Clinpro™ XT was significantly greater than Icon® resin infiltration (Table 2).
The resultant ΔE values calculated at all time intervals for both groups were more than 3.7 ΔE units, which is the critical value for clinical detection [41] and were statistically significant. However, the comparison between the groups showed that Icon® resin infiltration demonstrated a significant immediate improvement, whereas the long-term improvement was more significant with Clinpro™ XT varnish (Table 3).
Icon® resin infiltration showed more revival of the lost fluorescence at T1 than Clinpro™ XT, probably due to the creation of an immediate diffusion barrier within the body of the lesion. At T2, a comparable improvement was seen with both groups. At T3, Icon® resin infiltration showed further amelioration of the fluorescence loss than Clinpro™ XT, though not statistically significant. Both groups at T3 had a Q value lesser than that of the incipient demineralization value range of 2–9 [42]. Yet, the results have to be cautiously interpreted, as Icon® resin infiltration only occludes the acid pathways [15, 43] and does not remineralize the WSLs per se (Table 4).
Clinically, repeated etching was required with Icon® resin infiltration for moderate lesions to provide a preview of the aesthetic result to be expected after infiltration. Both Icon® resin infiltration and Clinpro™ XT varnish provided immediate aesthetic results with mild lesions. However, with moderate lesions, though progressive improvements were seen in both groups, clinically, visible improvements were seen more with Clinpro™ XT at T3 than with Icon® resin infiltration (Fig. 2).
Fig. 2.

Comparison of interventions
While both methods showed a significant increase in improving the aesthetics of the WSLs, the enamel in response to Clinpro™ XT was more comparable to that of the adjacent sound enamel. Icon® resin infiltration has already been proven in restoring the aesthetics of the enamel, and this study offers Clinpro™ XT varnish as an alternative with gratifying short- as well as long-term results.
Further, long-term follow-up is required to see the effects of Clinpro™ XT varnish on moderate WSLs over a year’s period to see if the colour and fluorescence are completely restored.
Conclusion
Immediately after the intervention, Icon® resin infiltration demonstrated a significantly better improvement than Clinpro™ XT varnish in restoring the colour; however, at 3 and 6 months, this was reversed.
At the end of the study period, the fluorescence loss significantly ameliorated in response to both Icon® resin infiltration between immediate intervention and at 6 months.
However, at 6 months, the fluorescence of the white spot lesions infiltrated with Icon® resin was comparable to that of the adjacent sound enamel while those treated with Clinpro™ XT varnish showed a statistically significant difference.
Acknowledgements
The authors would like to acknowledge the university for providing the opportunity to perform the research.
Funding
Not applicable
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- ΔE
Colour changes
- L
Lightness
- Q
Fluorescence loss
- WSLs
White spot lesions
Authors’ contributions
AK performed the intervention methods on the patients and was a major contributor in writing the manuscript. SP analysed and interpreted the patient data and contributed to the writing of the manuscript. Both authors read and approved the final manuscript.
Ethics approval and consent to participate
University’s Institutional Ethics Committee [number: CSP/16/SEP/51/280 dated October 4, 2016]. Institution’s consent form was obtained from those participants willing to be part of the trial.
Consent for publication
Permission has been obtained from the participant (or legal parent or guardian for children) to report individual patient data.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Footnotes
The original version of this article was revised: there was an error in the Materials and methods section concerning the name of an institute.
Change history
7/26/2019
In the publication of this article [1], there is an error in the Materials and methods section.
Contributor Information
Annapurna Kannan, Email: annapurnakannan@gmail.com.
Sridevi Padmanabhan, Email: sridevipadu@gmail.com.
References
- 1.Øgaard B, Rølla G, Arends J. Orthodontic appliances and enamel demineralization: Part 1. Lesion development. Am J Orthod Dentofac Orthop. 1988;94(1):68–73. doi: 10.1016/0889-5406(88)90453-2. [DOI] [PubMed] [Google Scholar]
- 2.Nascimento PL, Fernandes MT, Figueiredo FE, Faria-e-Silva AL. Fluoride-releasing materials to prevent white spot lesions around orthodontic brackets: a systematic review. Braz Dent J. 2016;27(1):101–107. doi: 10.1590/0103-6440201600482. [DOI] [PubMed] [Google Scholar]
- 3.Lopatiene K, Borisovaite M, Lapenaite E. Prevention and treatment of white spot lesions during and after treatment with fixed orthodontic appliances: a systematic literature review. J Oral Maxillofac Res. 2016;7(2):e1. doi: 10.5037/jomr.2016.7201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hoffman DA, Clark AE, Rody WJ, McGorray SP, Wheeler TT. A prospective randomized clinical trial into the capacity of a toothpaste containing NovaMin to prevent white spot lesions and gingivitis during orthodontic treatment. Prog Orthod. 2015;16(1):25. doi: 10.1186/s40510-015-0095-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hsu CY, Jordan TH, Dederich DN, Wefel JS. Effects of low-energy CO2 laser irradiation and the organic matrix on inhibition of enamel demineralization. J Dent Res. 2000;79(9):1725–1730. doi: 10.1177/00220345000790091401. [DOI] [PubMed] [Google Scholar]
- 6.Kronenberg O, Lussi A, Ruf S. Preventive effect of ozone on the development of white spot lesions during multibracket appliance therapy. Angle Orthod. 2009;79(1):64–69. doi: 10.2319/100107-468.1. [DOI] [PubMed] [Google Scholar]
- 7.Borzabadi-Farahani A, Borzabadi E, Lynch E. Nanoparticles in orthodontics, a review of antimicrobial and anti-caries applications. Acta Odontol Scand. 2014;72(6):413–417. doi: 10.3109/00016357.2013.859728. [DOI] [PubMed] [Google Scholar]
- 8.Yamazaki H, Litman A, Margolis HC. Effect of fluoride on artificial caries lesion progression and repair in human enamel: regulation of mineral deposition and dissolution under in vivo-like conditions. Arch Oral Biol. 2007;52(2):110–120. doi: 10.1016/j.archoralbio.2006.08.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bishara SE, Ostby AW. White spot lesions: formation, prevention, and treatment. Semin Orthod. 2008;30(3):174–182. doi: 10.1053/j.sodo.2008.03.002. [DOI] [Google Scholar]
- 10.Bröchner A, Christensen C, Kristensen B, Tranæus S, Karlsson L, Sonnesen L, Twetman S. Treatment of post-orthodontic white spot lesions with casein phosphopeptide-stabilised amorphous calcium phosphate. Clin Oral Investig. 2011;15(3):369–373. doi: 10.1007/s00784-010-0401-2. [DOI] [PubMed] [Google Scholar]
- 11.Featherstone JD. Prevention and reversal of dental caries: role of low level fluoride. Community Dent Oral Epidemiol. 1999;27(1):31–40. doi: 10.1111/j.1600-0528.1999.tb01989.x. [DOI] [PubMed] [Google Scholar]
- 12.Sonesson M, Bergstrand F, Gizani S, Twetman S. Management of post-orthodontic white spot lesions: an updated systematic review. Eur J Orthod. 2016;39(2):116–121. doi: 10.1093/ejo/cjw023. [DOI] [PubMed] [Google Scholar]
- 13.Yetkiner E, Wegehaupt F, Wiegand A, Attin R, Attin T. Colour improvement and stability of white spot lesions following infiltration, micro-abrasion, or fluoride treatments in vitro. Eur J Orthod. 2014;36(5):595–602. doi: 10.1093/ejo/cjt095. [DOI] [PubMed] [Google Scholar]
- 14.Paris S, Meyer-Lueckel H, Kielbassa AM. Resin infiltration of natural caries lesions. J Dent Res. 2007;86(7):662–666. doi: 10.1177/154405910708600715. [DOI] [PubMed] [Google Scholar]
- 15.Meyer-Lueckel H, Paris S, Kielbassa AM. Surface layer erosion of natural caries lesions with phosphoric and hydrochloric acid gels in preparation for resin infiltration. Caries Res. 2007;41(3):223–230. doi: 10.1159/000099323. [DOI] [PubMed] [Google Scholar]
- 16.Paris S, Hopfenmuller W, Meyer-Lueckel H. Resin infiltration of caries lesions: an efficacy randomized trial. J Dent Res. 2010;89(8):823–826. doi: 10.1177/0022034510369289. [DOI] [PubMed] [Google Scholar]
- 17.Doméjean S, Ducamp R, Léger S, Holmgren C. Resin infiltration of non-cavitated caries lesions: a systematic review. Med Princ Pract. 2015;24(3):216–221. doi: 10.1159/000371709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Knösel M, Eckstein A, Helms HJ. Durability of esthetic improvement following Icon resin infiltration of multibracket-induced white spot lesions compared with no therapy over 6 months: a single-center, split-mouth, randomized clinical trial. Am J Orthod Dentofac Orthop. 2013;144(1):86–96. doi: 10.1016/j.ajodo.2013.02.029. [DOI] [PubMed] [Google Scholar]
- 19.Kim S, Kim EY, Jeong TS, Kim JW. The evaluation of resin infiltration for masking labial enamel white spot lesions. Int J Paediatr Dent. 2011;21(4):241–248. doi: 10.1111/j.1365-263X.2011.01126.x. [DOI] [PubMed] [Google Scholar]
- 20.Knösel M, Eckstein A, Helms HJ. Long-term follow-up of camouflage effects following resin infiltration of post orthodontic white-spot lesions in vivo. Angle Orthod. 2019;89(1):33–39. doi: 10.2319/052118-383.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Yuan H, Li J, Chen L, Cheng L, Cannon RD, Mei L. Esthetic comparison of white-spot lesion treatment modalities using spectrometry and fluorescence. Angle Orthod. 2013;84(2):343–349. doi: 10.2319/032113-232.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Justus R. Prevention of white spot lesions. In: iatrogenic effects of orthodontic treatment: decision- making in prevention, diagnosis and treatment. 1. Heidelberg: Springer; 2015. pp. 1–35. [Google Scholar]
- 23.Kumar Jena A, Pal Singh S, Kumar Utreja A. Efficacy of resin-modified glass ionomer cement varnish in the prevention of white spot lesions during comprehensive orthodontic treatment: a split-mouth study. J Orthod. 2015;42(3):200–207. doi: 10.1179/1465313315Y.0000000005. [DOI] [PubMed] [Google Scholar]
- 24.Sohn S, Yi K, Son HH, Chang J. Caries-preventive activity of fluoride-containing resin-based desensitizers. Oper Dent. 2012;37(3):306–315. doi: 10.2341/11-007-L. [DOI] [PubMed] [Google Scholar]
- 25.Bhandary S, Hegde MN. A clinical comparison of in-office management of dentin hypersensitivity in a short term treatment period. Int J Biomed Adv Res. 2012;3:169–174. doi: 10.7439/ijbar.v3i3.338. [DOI] [Google Scholar]
- 26.Shailesh S, Nayak US, Joseph S, Saidath K. To evaluate the clinical efficiency of resin modified glass ionomer varnish in preventing enamel demineralisation during orthodontie treatment. J Pierre Fauchard Acad (India Section) 2012;26(3):95–107. doi: 10.1016/S0970-2199(12)63001-X. [DOI] [Google Scholar]
- 27.Mehta A, Paramshivam G, Chugh VK, Singh S, Halkai S, Kumar S. Effect of light-curable fluoride varnish on enamel demineralization adjacent to orthodontic brackets: an in-vivo study. Am J Orthod Dentofac Orthop. 2015;148(5):814–820. doi: 10.1016/j.ajodo.2015.05.022. [DOI] [PubMed] [Google Scholar]
- 28.Zhou SL, Zhou J, Watanabe S, Watanabe K, Wen LY, Xuan K. In vitro study of the effects of fluoride-releasing dental materials on remineralization in an enamel erosion model. J Dent. 2012;40(3):255–263. doi: 10.1016/j.jdent.2011.12.016. [DOI] [PubMed] [Google Scholar]
- 29.Gorelick L, Geiger AM, Gwinnett AJ. Incidence of white spot formation after bonding and banding. Am J Orthod. 1982;81(2):93–98. doi: 10.1016/0002-9416(82)90032-X. [DOI] [PubMed] [Google Scholar]
- 30.McLaren K. XIII—The development of the CIE 1976 (L* a* b*) uniform colour space and colour-difference formula. J Soc Dye Colour. 1976;92:338–341. doi: 10.1111/j.1478-4408.1976.tb03301.x. [DOI] [Google Scholar]
- 31.Knösel M, Reus M, Rosenberger A, Ziebolz D. A novel method for testing the veridicality of dental colour assessments. Eur J Orthod. 2011;34(1):19–24. doi: 10.1093/ejo/cjq142. [DOI] [PubMed] [Google Scholar]
- 32.Pianotti RS, Ambrozaitis JD, Mc Namara TF. Cariostatic activity of calcium glycerophosphate in hamsters: topical vs dietary administration. J Dent Res. 1976;55(6):1092–1096. doi: 10.1177/00220345760550061501. [DOI] [PubMed] [Google Scholar]
- 33.Sluzker A, Knosel M, Athanasiou AE. Sensitivity of digital dental photo CIE L*a*b* analysis compared to spectrophotometer clinical assessments over 6 months. Am J Dent. 2011;24:300–304. [PubMed] [Google Scholar]
- 34.Lesaffre E, Garcia Zattera MJ, Redmond C, Huber H, Needleman I. Reported methodological quality of split-mouth studies. J Clin Periodontol. 2007;34:756–761. doi: 10.1111/j.1600-051X.2007.01118.x. [DOI] [PubMed] [Google Scholar]
- 35.Lesaffre E, Philstrom B, Needleman I, Worthington H. The design and analysis of split-mouth studies: what statisticians and clinicians should know. Stat Med. 2009;28:3470–3482. doi: 10.1002/sim.3634. [DOI] [PubMed] [Google Scholar]
- 36.Hujoel PP. Design and analysis issues in split mouth clinical trials. Community Dent Oral Epidemiol. 1998;26:85–86. doi: 10.1111/j.1600-0528.1998.tb01932.x. [DOI] [PubMed] [Google Scholar]
- 37.Benson P. Evaluation of white spot lesions on teeth with orthodontic brackets. Semin Orthod. 2008;14(3):200–208. doi: 10.1053/j.sodo.2008.03.005. [DOI] [Google Scholar]
- 38.Fondriest J. Shade matching in restorative dentistry: the science and strategies. Int J Periodontics Restorative Dent. 2003;23:467–479. [PubMed] [Google Scholar]
- 39.Darling CL, Huynh GD, Fried D. Light scattering properties of natural and artificially demineralized dental enamel at 1310nm. J Biomed Optics. 2006;11(3):1–11. doi: 10.1117/1.2204603. [DOI] [PubMed] [Google Scholar]
- 40.Ko CC, Tantbirojn D, Want T, Douglas WH. Optical scattering power for characterization of mineral loss. J Dent Res. 2000;79:1584–1589. doi: 10.1177/00220345000790081001. [DOI] [PubMed] [Google Scholar]
- 41.Johnston WM, Kao EC. Assessment of appearance match by visual observation and colorimetry. J Dent Res. 1989;68(5):819–822. doi: 10.1177/00220345890680051301. [DOI] [PubMed] [Google Scholar]
- 42.Matheus P, Demito CF, Scheibel PC, Bowman SJ, Ramos AL. Correlation between the microscopic evaluation and reading by laser fluorescence of enamel decalcification in bovine teeth: In vitro study. Odonto. 2010;18:31–39. doi: 10.15603/2176-1000/odonto.v18n36p31-39. [DOI] [Google Scholar]
- 43.Meyer-Lueckel H, Paris S. Progression of artificial enamel caries lesions after infiltration with experimental light curing resins. Caries Res. 2008;42(2):117–124. doi: 10.1159/000118631. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.