Abstract
Background. Although chronic medical conditions (CMCs), depression, and self-rated health (SRH) are associated, their associations may depend on race, ethnicity, gender, and their intersections. In predominantly White samples, SRH is shown to better reflect the risk of mortality and multimorbidity for men than it is for women, which suggests that poor SRH among women may be caused not only by CMCs, but also by conditions like depression and social relations—a phenomenon known as “the sponge hypothesis.” However, little is known about gender differences in the links between multimorbidity, depression, and SRH among African Americans (AAs). Objective. To study whether depression differently mediates the association between multimorbidity and SRH for economically disadvantaged AA men and women. Methods. This survey was conducted in South Los Angeles between 2015 to 2018. A total number of 740 AA older adults (age ≥ 55 years) were enrolled in this study, of which 266 were AA men and 474 were AA women. The independent variable was the number of CMCs. The dependent variable was SRH. Age and socioeconomic status (educational attainment and marital status) were covariates. Depression was the mediator. Gender was the moderator. Structural Equation Modeling (SEM) was used to analyze the data. Results. In the pooled sample that included both genders, depression partially mediated the effect of multimorbidity on SRH. In gender specific models, depression fully mediated the effects of multimorbidity on SRH for AA men but not AA women. For AA women but not AA men, social isolation was associated with depression. Conclusion. Gender differences exist in the role of depression as an underlying mechanism behind the effect of multimorbidity on the SRH of economically disadvantaged AA older adults. For AA men, depression may be the reason people with multimorbidity report worse SRH. For AA women, depression is only one of the many reasons individuals with multiple CMCs report poor SRH. Prevention of depression may differently influence the SRH of low-income AA men and women with multimorbidity.
Keywords: race, gender, Blacks, African Americans, ethnic groups, chronic medical conditions, depression, self-rated health
1. Introduction
Self-rated health (SRH) is a widely accepted indicator of overall health. Poor SRH predicts risk of mortality [1,2,3,4,5,6,7,8,9] in both community [10] and clinical [11] settings. For both the general population [10] and patients with a chronic disease [12], SRH reflects long-term risk of mortality. SRH is a standard outcome in randomized clinical trials (RCTs) [13,14,15,16] and in national cohort surveys in Europe [17,18,19] as well as the US [20,21]. In the US, the Health and Retirement Study (HRS) [22], the Panel Study of Income Dynamics (PSID) [20,21], and the National Health and Nutrition Examination Survey (NHANES) [10] all measure health at the population level using SRH. SRH is also used for cross-country comparisons [23,24,25,26,27,28,29] and policy development [30,31,32,33]. It is used as a reflection of health disparities and inequality [34,35,36,37]. SRH is also used to track the subjective health of individuals with index psychiatric or medical conditions [38].
Although SRH is known to be a valid health measure [1,2,3,4,5,6,7,8,9], SRH may not reflect the same aspects of health across populations distinguished by race, ethnicity, and gender [39]. Although SRH is efficient, cost effective, and time saving [40], poor SRH may not have the same meaning for men as for women [41]. Despite the high acceptability of SRH as a measure of health [1,2,3,4,5,6,7,8,9], SRH may mean different things for different populations.
The use of SRH for group comparisons may be questioned if it is not universally valid and comparable across racial [39] and gender lines [41]. Age, gender, socioeconomic status (SES), health behaviors, chronic medical conditions (CMCs), and depression may differently influence the SRH of people in different countries [42]. If poor SRH means different things for subsections of populations, any comparison of population groups using SRH would be biased [41,43]. Thus, SRH would not be the ideal tool for measuring health in diverse populations [43,44].
Although not all studies agree [45], a large body of evidence suggests that poor SRH may not reflect the same health for subpopulations classified by age, gender, ethnicity, and health status [45,46,47,48,49,50,51,52]. For example, the meaning of SRH may shift according to developmental stage and age [45,47]. Race and ethnicity alter what poor SRH reflects [53,54,55,56]. This is in part because the reference group of each section of the population differs [57,58,59,60,61,62]. Similarly, non-health determinants of SRH vary by race and gender [63,64,65]. For example, socioeconomic status [42,43,63,65] and neighborhood [66] differently impact the SRH of racial and gender groups. In addition, the role of physical health in shaping SRH is not constant across various populations [42]. Finally, even within a given patient population, SRH differently reflects the severity of the condition and outcomes in different racial and gender groups [1,67].
Differences in what shapes SRH may result in differences in the validity of SRH as a predictor of the risk of mortality in different groups [41,56]. Thus, while poor SRH may be an excellent marker of mortality risk for White men, it may not be for African Americans (AAs), Hispanics, or even women [42,43,68]. To understand whether cross-gender, cross-racial, and cross-ethnic comparisons of SRH are valid, we need to compare determinants of poor SRH across various groups. Cross-group comparisons of SRH will only be valid if SRH has the same meaning across populations.
Aims
To better understand how gender impacts SRH in AA older adults [54,69,70,71], this study compared the mediating effect of depression on the effect of multimorbidity on SRH between AA men and AA women. In line with the sponge hypothesis [41,67], we expected multimorbidity to have a stronger effect on SRH among AA men than among AA women. We also expected depression to have a stronger effect on SRH among AA women than among AA men. The sponge hypothesis suggests that, for women, SRH is more inclusive, acting like a sponge to absorb a wide array of social and health factors. In contrast with the sponge-like behavior of SRH among women, SRH among men is thought to be a function of CMCs and multimorbidity alone, uninfluenced by other social and health factors [41].
2. Methods
2.1. Design and Setting
The design was a cross-sectional survey of economically disadvantaged AA older adults in South Los Angeles. The study was performed between 2015 and 2018 [72,73].
2.2. Institutional Review Board (IRB)
The study protocol was approved by the Institutional Review Board (IRB) of the Charles R. Drew University of Medicine and Science (CDU), Los Angeles. All participants signed a written informed consent before being enrolled in the study. Participants received financial incentives.
2.3. Process and Data Collection
The data collection included structured face-to-face interviews and a comprehensive assessment of medications. The interviewers collected data on demographic factors (age and gender), SES (educational attainment, financial difficulty), objective health (CMCs), and subjective health (SRH and depression).
2.4. Participants
The study recruited a convenience sample of economically disadvantaged AA older adults from low-income areas in South Los Angeles, such as the Watts area. Using a convenience sample, AA older adults were eligible if they were AA, were 55 years or older, could complete an interview in English, and resided in the Service Planning Area (SPA) 6. Institutionalized participants were excluded from the study. Other exclusion criteria included being enrolled in any other clinical trials or having poor cognitive performance. This sampling resulted in 740 AAs aged 55 years and older. Our participants were recruited from eleven senior housing apartment units, sixteen predominantly AA churches, and several low-income public housing projects, all located in SPA 6 of Los Angeles County. All of our participants were low-income, underserved, older AAs. The vast majority of older adults in SPA 6 are AAs (49%). About 28% of SPA 6 households are below the federal poverty line (FPL) and 58% of adults have income levels less than 200% of the FPL. About 36% of adults in SPA 6 are uninsured. Between 2013 and 2015, the percentage of homeless AAs in SPA 6 has almost doubled from 39% to 70% [72,73].
2.5. Measures
The current study collected data on demographic factors (gender and age), SES (educational attainment and marital status), and health status (multimorbidity, depression, and SRH).
2.5.1. Dependent Variable
Self-rated health. We asked participants about their overall health. The responses ranged from excellent (1) to poor (5). We treated SRH as a continuous variable with a range from 1 to 5, where a higher score reflects worse health. Poor SRH predicts all-cause mortality in the general population [10,74,75,76] as well as in patients with chronic disease [77,78]. Review articles and multiple original studies have established the high predictive validity of poor SRH as a robust determinant of mortality risk, above and beyond confounders such as SES and health [4,10,79].
2.5.2. Mediator
Depression. This study used the 15-item Geriatric Depression Scale (GDS) Short Form [80] to evaluate depression. Possible responses were “yes” or “no.” A summary score was calculated with a potential range between 0 and 15. A higher score indicated more depression. The GDS Short Form is a highly reliable and valid instrument that has been used extensively in both clinical and community settings to measure depression among older adults [80].
2.5.3. Independent Variable
Multimorbidity/number of chronic medical conditions (CMCs). In this study, multimorbidity was defined as the number of CMCs. Participants were asked about the presence of 11 CMCs. Individuals were asked by the interviewer if a physician had ever told them that they have any of these conditions: Hypertension, heart disease, diabetes, lipid disorder/hypercholesterolemia, cancer, asthma, osteoarthritis, thyroid disorder, chronic obstructive pulmonary disease, rheumatoid arthritis, or gastrointestinal disease [42,81]. Self-reports provide valid information regarding CMCs, although some bias in this approach is to be expected [39,82,83,84,85,86,87].
2.5.4. Confounders
Sociodemographic covariates. Age, educational attainment, and marital status were the covariates in this study. Age was treated as an interval variable. Educational attainment was operationalized as an interval variable (years of schooling). Higher scores indicated more years of education. Marital status was a dichotomous variable (1 = married, 0 = unmarried)
2.5.5. Moderator
Gender. Gender was the effect modifier. Gender was treated as a dichotomous variable (1 = female, 0 = male).
2.6. Statistical Analysis
SPSS 22.0 (SPSS Inc., Chicago, IL, USA) and AMOS 22.0 were used to conduct the data analysis. The frequency (%) and the mean (SD) were reported to describe the sample at the baseline and 10 years later. Pearson correlation was used to calculate the bivariate correlations in the overall sample.
A multi-group Structural Equation Model (SEM) was used for multivariable analysis [54]. In our models, groups were defined based on gender. The number of CMCs (multimorbidity) was the predictor, SRH was the outcome, depression was the mediator, and age, education, and marital status were covariates. These variables were selected based on a review of the literature and on the available variables in our data set. The study did not collect data on income; however, most participants were low income AAs and all lived in economically disadvantaged areas of LA County. We did not include health insurance in our analysis because almost all of our participants had health insurance (mostly Medicare or MediCal). To handle missing data, the Full Information Maximum Likelihood (FIML) method was used. Data were missing in less than 1% of the cases. The final SEM model did not include any constraints or co-variances for errors. The model’s goodness-of-fit was assessed using conventional methods: A non-significant chi-square test (p > 0.05), a comparative fit index (CFI) larger than 0.95, a root mean squared error of approximation (RMSEA) of less than 0.06, and an X2 with less than 4 degrees of freedom. We reported unstandardized regression coefficients for each path.
3. Results
3.1. Descriptive Statistics
A total number of 740 AA economically disadvantaged older adults 55 years or older were enrolled in this study, of which 266 were AA men and 474 were AA women. Table 1 describes the sample, both pooled and by gender. This table shows that AA men and AA women differed in age, number of CMCs, depression, and SRH.
Table 1.
Descriptive Statistics of the sample, both pooled and by gender.
| All n = 740 |
African American Men n = 262 |
African American Women n = 474 |
||||
|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | |
| Age * | 71.73 | 8.37 | 70.79 | 8.32 | 72.26 | 8.36 |
| Educational Attainment * | 12.74 | 2.24 | 12.42 | 2.51 | 12.93 | 2.06 |
| Number of CMCs (Multimorbidity) * | 3.86 | 1.86 | 3.58 | 1.88 | 4.03 | 1.83 |
| Depression | 2.47 | 2.77 | 2.53 | 2.76 | 2.43 | 2.79 |
| Self-Rated Health (SRH) | 3.13 | 1.02 | 3.12 | 1.09 | 3.14 | 0.97 |
| n | % | n | % | n | % | |
| Married * | ||||||
| No | 640 | 86.5 | 215 | 80.8 | 425 | 89.7 |
| Yes | 100 | 13.5 | 51 | 19.2 | 49 | 10.3 |
| Living Alone * | ||||||
| No | 294 | 39.7 | 121 | 45.5 | 173 | 36.5 |
| Yes | 446 | 60.3 | 145 | 54.5 | 301 | 63.5 |
CMC: chronic medical condition; SD: Standard Deviation; * p < 0.05 (independent sample t-test).
3.2. Bivariate Correlations
Table 2 shows the correlation matrix between all the study variables of the sample, both pooled and by gender. As this table shows, in the pooled sample, number of CMCs, depression, and SRH were correlated in the pooled sample and AA men and AA women.
Table 2.
Bivariate correlation matrix of the sample, both pooled and by gender.
| Characteristics | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 |
|---|---|---|---|---|---|---|---|---|
| All | ||||||||
| 1 Gender (Female) | 1 | 0.08 * | 0.11 ** | −0.12 ** | 0.09 * | 0.12 ** | −0.02 | 0.01 |
| 2 Age | −0.18 ** | −0.00 | 0.06 | −0.02 | −0.25 ** | −0.22 ** | ||
| 3 Education | 1 | 0.06 | −0.04 | −0.09 * | −0.07 | −0.03 | ||
| 4 Married | 1 | −0.41 ** | −0.02 | −0.07 | −0.08 * | |||
| 5 Living alone | 1 | 0.09 * | 0.12 ** | 0.08 * | ||||
| 6 Number of CMCs (Multimorbidity) | 1 | 0.32 ** | 0.27 ** | |||||
| 7 Depression | 1 | 0.37 ** | ||||||
| 8 Self-Rated Health (SRH) | 1 | |||||||
| AA Men | ||||||||
| 2 Age | 1 | −0.25 ** | 0.01 | −0.04 | −0.06 | −0.23 ** | −0.28 ** | |
| 3 Education | 1 | 0.16 ** | −0.10 | −0.07 | −0.06 | −0.04 | ||
| 4 Married | 1 | −0.48 ** | −0.03 | −0.10 | −0.11 | |||
| 5 Living alone | 1 | 0.10 | 0.15 * | 0.12 | ||||
| 6 Number of CMCs (Multimorbidity) | 1 | 0.38 ** | 0.19 ** | |||||
| 7 Depression | 1 | 0.30 ** | ||||||
| 8 Self-Rated Health (SRH) | ||||||||
| AA Women | ||||||||
| 2 Age | 1 | −0.16 ** | 0.00 | 0.10 * | −0.01 | −0.27 ** | −0.19 ** | |
| 3 Education | 0.01 | −0.02 | −0.12 ** | −0.07 | −0.03 | |||
| 4 Married | 1 | −0.35 ** | 0.02 | −0.05 | −0.06 | |||
| 5 Living alone | 1 | 0.06 | 0.11 * | 0.05 | ||||
| 6 Number of CMCs (Multimorbidity) | 1 | 0.29 ** | 0.32 ** | |||||
| 7 Depression | 1 | 0.41 ** | ||||||
| 8 Self-Rated Health (SRH) | 1 |
* p < 0.05, ** p < 0.01.
3.3. Structural Equation Modeling (SEM) in the Pooled Sample
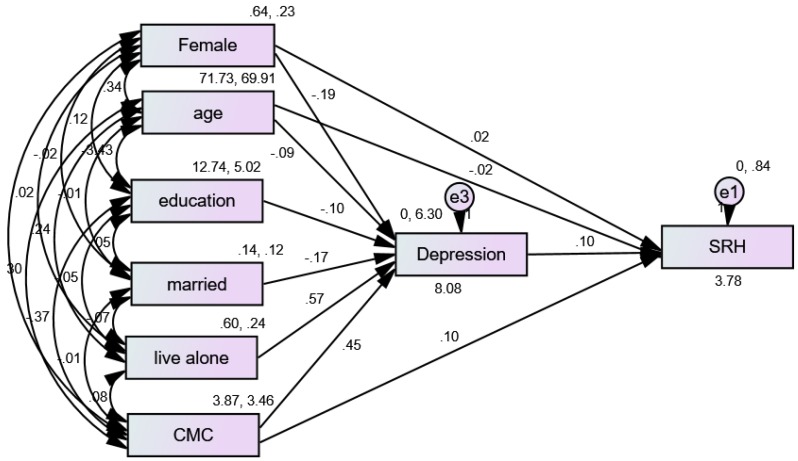
The fit of our first model was very good (CMIN = 4.11, degree of freedom [DF] = 3, p = 0.250, CMIN/DF = 1.370, CFI = 0.998, RMSEA = 0.022 (90%CI = 0.000–0.070). Figure 1 shows the results of a SEM with multimorbidity (number of CMCs) as the predictor, depression as the mediator, and SRH as the outcome variable in the pooled sample. According to this model, depression only partially mediated the effects of multimorbidity on SRH in the pooled sample (Table 3).
Figure 1.
Summary of the Structural Equation Modeling (SEM) overall.
Table 3.
Summary of the Structural Equation Modeling (SEM) in the pooled sample.
| Characteristics | Estimate (S.E.) | p |
|---|---|---|
| → Depression | ||
| Gender (female) | −0.19 (0.20) | 0.340 |
| Marital status (married) | −0.17 (0.30) | 0.559 |
| Number of CMCs (multimorbidity) | 0.45 (0.05) | <0.001 |
| Living alone | 0.57 (0.21) | 0.006 |
| Age | −0.09 (0.01) | <0.001 |
| Education | −0.10 (0.04) | 0.022 |
| → Self-Rated Health (SRH) | ||
| Gender (female) | 0.02 (0.07) | 0.795 |
| Age | −0.02 (0.00) | <0.001 |
| Number of CMCs (multimorbidity) | 0.10 (0.02) | <0.001 |
| Depression | 0.10 (0.01) | <0.001 |
SE: Standard Error; CMC: chronic medical condition
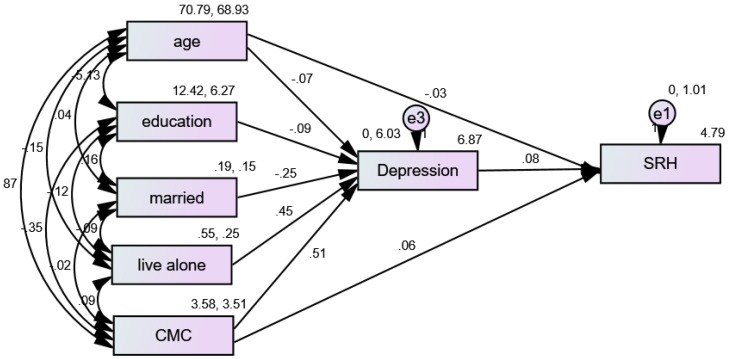
3.4. Structural Equation Modeling (SEM) in African American (AA) Men
The fit of our multi-group model was very good (CMIN = 5.22, DF = 6, p = 0.001, CMIN/DF = 8.981, CFI = 1.000, RMSEA = 0.000 (90%CI = 0.000–0.044). Figure 2 shows the results of an SEM with number of CMCs (multimorbidity) as the predictor, depression as the mediator, and SRH as the outcome variable for AA men. According to this model, depression fully mediated the effects of multimorbidity on SRH in the pooled sample. In a model that also included depression (as the mediator), multimorbidity did not impact SRH for AA men (Table 4).
Figure 2.
Summary of the Structural Equation Modeling (SEM) in African American (AA) men.
Table 4.
Summary of the Structural Equation Modeling (SEM) in African American (AA) men and women.
| Characteristics | Estimate (S.E.) | p | Estimate (S.E.) | p |
|---|---|---|---|---|
| Men | Women | |||
| → Depression | ||||
| Marital status (married) | −0.25 (0.44) | 0.571 | −0.13 (0.41) | 0.752 |
| Number of CMCs (multimorbidity) | 0.51 (0.08) | <0.001 | 0.41 (0.06) | <0.001 |
| Living alone | 0.45 (0.35) | 0.193 | 0.65 (0.26) | 0.012 |
| Age | −0.07 (0.02) | <0.001 | −0.10 (0.01) | <0.001 |
| → Self-Rated Health (SRH) | ||||
| Education | −0.09 (0.06) | 0.162 | −0.10 (0.06) | 0.078 |
| Age | −0.03 (0.01) | <0.001 | −0.01 (0.01) | 0.021 |
| Number of CMCs (multimorbidity) | 0.06 (0.04) | 0.115 | 0.12 (0.02) | <0.001 |
| Depression | 0.09 (0.03) | <0.001 | 0.11 (0.02) | <0.001 |
SE: Standard Error; CMC: chronic medical condition
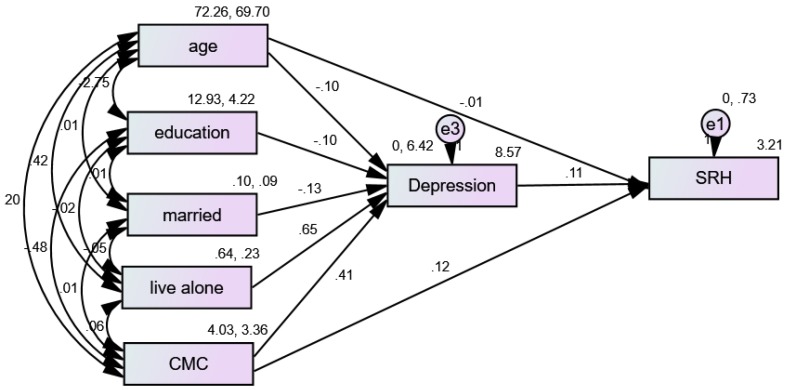
3.5. Structural Equation Modeling (SEM) in African American (AA) Women
Figure 3 shows the results of an SEM with multimorbidity as the predictor, depression as the mediator, and SRH as the outcome variable for AA women. According to this model, depression only partially mediated the effects of multimorbidity on SRH in the pooled sample. While depression was in the model, multimorbidity still impacted SRH for AA men (Table 4).
Figure 3.
Summary of the Structural Equation Modeling (SEM) in African American (AA) women.
4. Discussion
In this convenience sample of economically disadvantaged AA older adults, there were gender differences in the way depression mediated the association between multimorbidity and SRH. Depression fully mediated the association between multimorbidity and poor SRH in economically disadvantaged AA men, but not in economically disadvantaged AA women. Depression was the reason low-income AA men with multimorbidity reported poor SRH, but it was more than depression that caused low-income AA women with multimorbidity to report poor SRH.
In a recent study of a smaller sample of low-income AA adults, the SRH of women was found to operate like a sponge, absorbing more affective and contextual information, as opposed to AA men’s SRH [83]. However, that study did not differentiate mediators of SRH by gender, as we have done.
Our results contribute to the literature on gender differences in SRH. In studies conducted in mainly White samples, poor SRH predicted the risk of mortality among men much better than among women [41,88]. In one of the studies, the author argued that in women, SRH may reflect more contextual and affective information, whereas for men, the main determinant of SRH is multimorbidity (number of CMCs) [41]. In another study, gender difference in the predictive power of poor SRH on the risk of mortality was attenuated by controlling for co-morbid conditions, suggesting that multimorbidity is one of the reasons SRH better predicts mortality among men than among women [88]. However, most of this research used samples that were predominantly White [41]. The main contribution of this study is to extend this literature to AAs. In a study of AA individuals with diabetes, SRH reflected glucose control for AA men but not for AA women [67]. In another study of people with diabetes, worse glycemic control (higher HbA1c) was associated with worse levels of SRH in males and females only when all age groups were combined. However, in younger people, the same association was stronger for women than for men, probably due to diabetes-related worries as a result of high HbA1c [89].
In contrast to our results, there are also studies that do not confirm major gender differences in SRH. In one study that spanned 12 years, the Health and Retirement Study (HRS), males and females were compared for trajectories and determinants of SRH. The study, which is mainly composed of Whites, did not show gender differences in SRH levels at baseline. However, SRH declined faster for men than for women over time. Onset of development of CMCs, health behaviors such as smoking, and rate of retirement explain this gender difference in trajectory of SRH over time [90]. In a study that used the 2002–2015 National Health Interview Survey (NHIS) data, ordered logistic regression models were applied to predict SRH as a function of two dozen health conditions, including multimorbidity, physical symptoms, mental health, function, healthcare use, and health behaviors, by gender. The study found almost no evidence supporting the sponge hypothesis. The study failed to show systematic gender variation in the structure of SRH. The study showed that men and women use a wide-range of health-related frames of reference, mostly in a similar way, to make judgments regarding their own health. The following gender difference was observed: At mid-life and older ages, men are more likely than women to weigh physical functioning and negative health behaviors as a factor contributing to their SRH. This study suggested that women report worse SRH than men only through mid-adulthood. This pattern reverses as they age. The study also showed that the female disadvantage in SRH is fully attributable to SES differences. The authors argued that SRH can be used to measure gender differences in health [45]. A study of veterans also did not find major gender differences; however, it did find that exposure to warfare casualties was more predictive of SRH for men than women [91]. These results, however, differ from our study, which suggests SRH may not be comparable between AA men and women.
Our study supports the findings of most researchers that race/ethnicity, gender, and SES have complex effects in shaping what poor SRH means [68,81,92,93,94]. For example, education and income improve the SRH of White but not AA individuals and families [63,64,65]. At the same time, SRH predicts risk of mortality of Whites but not AAs [1,56]. This is because SRH does not reflect the same aspect of health for ethnic groups [43,44] and also across countries [42,95,96,97]. In the Fragile Families and Child Well-Being Study, which followed 2407 AAs and 894 Whites for five years for changes in SRH, in all ethnic groups, anxiety and drinking problems were predictive of poor SRH at baseline and over time. The study documented cross-ethnic variation in the combined (additive) effects of anxiety and depression on SRH. For AAs, depression and anxiety both predicted a worse trajectory of SRH over time. For Whites, depression predicted worse baseline SRH, while anxiety predicted better SRH at baseline and over time [92]. In another cross-sectional study, which borrowed data from the National Survey of American Life 2003 and included 3570 AAs, anxiety and depression had independent (i.e., separate) effects on mental SRH [68].
Our results suggest that AA men demonstrate lower SRH when depressed compared to AA women. This is an interesting finding that highlights a relative disadvantage of AA men compared to AA women when it comes to the impact of depression on SRH in the presence of multimorbidity. This finding contributes to the literature on race, gender, and health. The older work of James Stewart [98] and the more recent work of Tommy Curry (The Man-Not) [99] help us understand the contribution of structural racism in the life of AA men. Studies by Watkin [100,101], Powell [102,103,104], Neighbors [105], and Griffith [106] show us the interpersonal aspects of depression among AA men. Their work helps us understand the multi-level determinants of depression in AA men, suggesting that a combination of masculinity and racism increases the risk of depression for AA men. This is probably why even among high SES AA men, but not among high SES AA women, we observe an increased risk of depression and psychological distress [81,107,108].
One of the findings of this study was that AA women may be more vulnerable to the effects of living alone on depression compared to AA men. While social support is shown to be important for mental health in all groups [109,110,111], social relations are particularly consequential for AAs [112,113,114,115,116]. Social support promotes mental health directly and buffers the effect of stress [117]. There is literature that suggests social support may be more crucial for mental health of AAs than Whites [118,119,120,121]. In these studies, social support shows a stronger effect on the mental health of AAs than Whites. There are also many studies showing different relevance of social support to the health and wellbeing of men and women [70,122,123,124,125,126,127,128,129,130,131,132,133,134].
Limitations
There are several limitations to this study, which may be inherent to our study design. Due to a cross-sectional study design, we cannot infer causal associations. We also did not have data on personal or household income. We did not expect a large distribution of income, as all participants were of retirement age and were living in one of the most economically disadvantaged areas of South LA. Health insurance was also present in almost all our participants. Finally, we did not include marital status to reduce collinearity, because we had living alone as a confounder. Furthermore, self-reporting bias must be recognized as a possibility since we did not have access to clinical validations of CMCs or formal diagnoses by mental health providers. There is a need for future studies to replicate these findings using medical chart review or administrative data. The smaller number of AA men in comparison with AA women in our sample may have resulted in differential statistical power. Finally, non-random sampling reduces the generalizability of our results. These limitations were inevitable because we performed a secondary analysis of an existing data set. Despite these limitations, this study contributes to the literature on the intersections of race, gender, and the meaning of SRH, with a particular focus on older adults in a low-income urban setting.
5. Conclusions
In summary, there are gender differences in SRH among low-income AA older men and women with multimorbidity. For low-income AA older men, depression is the reason individuals with multimorbidity report poor SRH. For low-income AA older women, more than depression is involved. More research is needed to investigate other factors contributing to poor SRH among AAs with multimorbidity. Future research should examine whether pain, anxiety, social isolation, or other domains have an impact on SRH among low-income AA women with multiple CMCs.
Author Contributions
M.B. designed the study, conducted the study, collected data, and revised the manuscript. J.S. contributed in the data collection and performing the study. S.A. prepared the first draft of the paper. All authors approved the final draft.
Funding
This study was supported by the Center for Medicare and Medicaid Services (CMS) Grant 1H0CMS331621 to Charles R. Drew University of Medicine and Science (PI: M. Bazargan). Additionally, Bazargan is supported by the NIH under Award # “54MD008149” and # R25 MD007610 (PI: M. Bazargan), 2U54MD007598 (PI: J. Vadgama), and U54 TR001627 (PIs: S. Dubinett, and R. Jenders). Assari is partly supported by the CMS grant 1H0CMS331621 (PI: M. Bazargan) and the National Institute on Minority Health and Health Disparities (NIMHD) grant U54 MD007598 (PI = M. Bazargan).
Conflicts of Interest
The authors declare no conflicts of interest.
References
- 1.Assari S. Self-rated Health and Mortality due to Kidney Diseases: Racial Differences in the United States. Adv. Biomed. Res. 2018;7:4. doi: 10.4103/2277-9175.223738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Godaert L., Godard-Sebillotte C., Allard Saint-Albin L., Bousquet L., Bourdel-Marchasson I., Fanon J.L., Drame M. Self-rated health as a predictor of mid-term and long-term mortality in older Afro-Caribbeans hospitalised via the emergency department. Qual. Life Res. 2018;27:91–96. doi: 10.1007/s11136-017-1693-3. [DOI] [PubMed] [Google Scholar]
- 3.Grove B.E., Schougaard L.M., Hjollund N.H., Ivarsen P. Self-rated health, quality of life and appetite as predictors of initiation of dialysis and mortality in patients with chronic kidney disease stages 4-5: A prospective cohort study. BMC Res. Notes. 2018;11:371. doi: 10.1186/s13104-018-3472-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Idler E.L., Benyamini Y. Self-rated health and mortality: A review of twenty-seven community studies. J. Health Soc. Behav. 1997;38:21–37. doi: 10.2307/2955359. [DOI] [PubMed] [Google Scholar]
- 5.Nery Guimaraes J.M., Chor D., Werneck G.L., Carvalho M.S., Coeli C.M., Lopes C.S., Faerstein E. Association between self-rated health and mortality: 10 years follow-up to the Pro-Saude cohort study. BMC Public Health. 2012;12:676. doi: 10.1186/1471-2458-12-676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Phung T.K.T., Siersma V., Vogel A., Waldorff F.B., Waldemar G. Self-rated versus Caregiver-rated Health for Patients with Mild Dementia as Predictors of Patient Mortality. Am. J. Geriatr. Psychiatry. 2018;26:375–385. doi: 10.1016/j.jagp.2017.06.005. [DOI] [PubMed] [Google Scholar]
- 7.Schnittker J., Bacak V. The increasing predictive validity of self-rated health. PLoS ONE. 2014;9:e84933. doi: 10.1371/journal.pone.0084933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Szybalska A., Broczek K., Puzianowska-Kuznicka M., Slusarczyk P., Chudek J., Skalska A., Mossakowska M. Self-rated health and its association with all-cause mortality of older adults in Poland: The PolSenior project. Arch. Gerontol. Geriatr. 2018;79:13–20. doi: 10.1016/j.archger.2018.07.016. [DOI] [PubMed] [Google Scholar]
- 9.Thong M.S., Kaptein A.A., Benyamini Y., Krediet R.T., Boeschoten E.W., Dekker F.W., Netherlands Cooperative Study on the Adequacy of Dialysis Study Group Association between a self-rated health question and mortality in young and old dialysis patients: A cohort study. Am. J. Kidney Dis. 2008;52:111–117. doi: 10.1053/j.ajkd.2008.04.001. [DOI] [PubMed] [Google Scholar]
- 10.Idler E.L., Angel R.J. Self-rated health and mortality in the NHANES-I Epidemiologic Follow-up Study. Am. J. Public Health. 1990;80:446–452. doi: 10.2105/AJPH.80.4.446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lainscak M., Farkas J., Frantal S., Singer P., Bauer P., Hiesmayr M., Schindler K. Self-rated health, nutritional intake and mortality in adult hospitalized patients. Eur. J. Clin. Investig. 2014;44:813–824. doi: 10.1111/eci.12300. [DOI] [PubMed] [Google Scholar]
- 12.Wennberg P., Rolandsson O., Jerden L., Boeing H., Sluik D., Kaaks R., Teucher B., Spijkerman A., Bueno de Mesquita B., Dethlefsen C., et al. Self-rated health and mortality in individuals with diabetes mellitus: Prospective cohort study. BMJ Open. 2012;2:e000760. doi: 10.1136/bmjopen-2011-000760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gonzalez M., Sjolin I., Back M., Ogmundsdottir Michelsen H., Tanha T., Sandberg C., Schiopu A., Leosdottir M. Effect of a lifestyle-focused electronic patient support application for improving risk factor management, self-rated health, and prognosis in post-myocardial infarction patients: Study protocol for a multi-center randomized controlled trial. Trials. 2019;20:76. doi: 10.1186/s13063-018-3118-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Duberg A., Hagberg L., Sunvisson H., Moller M. Influencing self-rated health among adolescent girls with dance intervention: A randomized controlled trial. JAMA Pediatr. 2013;167:27–31. doi: 10.1001/jamapediatrics.2013.421. [DOI] [PubMed] [Google Scholar]
- 15.Diaz E., Bruce N., Pope D., Diaz A., Smith K.R., Smith-Sivertsen T. Self-rated health among Mayan women participating in a randomised intervention trial reducing indoor air pollution in Guatemala. BMC Int. Health Hum. Rights. 2008;8:7. doi: 10.1186/1472-698X-8-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Steptoe A., Perkins-Porras L., Hilton S., Rink E., Cappuccio F.P. Quality of life and self-rated health in relation to changes in fruit and vegetable intake and in plasma vitamins C and E in a randomised trial of behavioural and nutritional education counselling. Br. J. Nutr. 2004;92:177–184. doi: 10.1079/BJN20041177. [DOI] [PubMed] [Google Scholar]
- 17.Mavaddat N., Kinmonth A.L., Sanderson S., Surtees P., Bingham S., Khaw K.T. What determines Self-Rated Health (SRH)? A cross-sectional study of SF-36 health domains in the EPIC-Norfolk cohort. J. Epidemiol. Community Health. 2011;65:800–806. doi: 10.1136/jech.2009.090845. [DOI] [PubMed] [Google Scholar]
- 18.Westerlund H., Kivimaki M., Singh-Manoux A., Melchior M., Ferrie J.E., Pentti J., Jokela M., Leineweber C., Goldberg M., Zins M., et al. Self-rated health before and after retirement in France (GAZEL): A cohort study. Lancet. 2009;374:1889–1896. doi: 10.1016/S0140-6736(09)61570-1. [DOI] [PubMed] [Google Scholar]
- 19.Delpierre C., Datta G.D., Kelly-Irving M., Lauwers-Cances V., Berkman L., Lang T. What role does socio-economic position play in the link between functional limitations and self-rated health: France vs. USA? Eur. J. Public Health. 2012;22:317–321. doi: 10.1093/eurpub/ckr056. [DOI] [PubMed] [Google Scholar]
- 20.Etherington N. Re-evaluating gender differences in self-rated health: The importance of cohort. J. Women Aging. 2017;29:150–162. doi: 10.1080/08952841.2016.1108737. [DOI] [PubMed] [Google Scholar]
- 21.McDonough P., Berglund P. Histories of poverty and self-rated health trajectories. J. Health Soc. Behav. 2003;44:198–214. doi: 10.2307/1519808. [DOI] [PubMed] [Google Scholar]
- 22.Lee S.J., Moody-Ayers S.Y., Landefeld C.S., Walter L.C., Lindquist K., Segal M.R., Covinsky K.E. The relationship between self-rated health and mortality in older black and white Americans. J. Am. Geriatr. Soc. 2007;55:1624–1629. doi: 10.1111/j.1532-5415.2007.01360.x. [DOI] [PubMed] [Google Scholar]
- 23.Torsheim T., Nygren J.M., Rasmussen M., Arnarsson A.M., Bendtsen P., Schnohr C.W., Nielsen L., Nyholm M. Social inequalities in self-rated health: A comparative cross-national study among 32,560 Nordic adolescents. Scand. J. Public Health. 2018;46:150–156. doi: 10.1177/1403494817734733. [DOI] [PubMed] [Google Scholar]
- 24.Lee Y. Does Context Matter? Literacy Disparities in Self-rated Health Using Evidence from 17 Developed Countries. Am. J. Health Behav. 2017;41:287–300. doi: 10.5993/AJHB.41.3.8. [DOI] [PubMed] [Google Scholar]
- 25.Kim S., Kim C.Y., You M.S. Civic participation and self-rated health: A cross-national multi-level analysis using the world value survey. J. Prev. Med. Public Health. 2015;48:18–27. doi: 10.3961/jpmph.14.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.French D.J., Browning C., Kendig H., Luszcz M.A., Saito Y., Sargent-Cox K., Anstey K.J. A simple measure with complex determinants: Investigation of the correlates of self-rated health in older men and women from three continents. BMC Public Health. 2012;12:649. doi: 10.1186/1471-2458-12-649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Prus S.G. Comparing social determinants of self-rated health across the United States and Canada. Soc. Sci. Med. 2011;73:50–59. doi: 10.1016/j.socscimed.2011.04.010. [DOI] [PubMed] [Google Scholar]
- 28.Hanibuchi T., Nakaya T., Murata C. Socio-economic status and self-rated health in East Asia: A comparison of China, Japan, South Korea and Taiwan. Eur. J. Public Health. 2012;22:47–52. doi: 10.1093/eurpub/ckq174. [DOI] [PubMed] [Google Scholar]
- 29.Bardage C., Pluijm S.M.F., Pedersen N.L., Deeg D.J.H., Jylha M., Noale M., Blumstein T., Otero A. Self-rated health among older adults: A cross-national comparison. Eur. J. Ageing. 2005;2:149–158. doi: 10.1007/s10433-005-0032-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Gonzales G., Ehrenfeld J.M. The Association between State Policy Environments and Self-Rated Health Disparities for Sexual Minorities in the United States. Int. J. Environ. Res. Public Health. 2018;15:1136. doi: 10.3390/ijerph15061136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Dowling A., Enticott J., Russell G. Measuring self-rated health status among resettled adult refugee populations to inform practice and policy—A scoping review. BMC Health Serv. Res. 2017;17:817. doi: 10.1186/s12913-017-2771-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Badland H., Mavoa S., Livingston M., David S., Giles-Corti B. Testing spatial measures of alcohol outlet density with self-rated health in the Australian context: Implications for policy and practice. Drug Alcohol Rev. 2016;35:298–306. doi: 10.1111/dar.12341. [DOI] [PubMed] [Google Scholar]
- 33.Spurling G., Hayman N. Self-rated health status in an urban indigenous primary care setting: Implications for clinicians and public health policy. Aust. N. Z. J. Public Health. 2010;34:598–601. doi: 10.1111/j.1753-6405.2010.00627.x. [DOI] [PubMed] [Google Scholar]
- 34.Kravitz-Wirtz N. Cumulative Effects of Growing Up in Separate and Unequal Neighborhoods on Racial Disparities in Self-rated Health in Early Adulthood. J. Health Soc. Behav. 2016;57:453–470. doi: 10.1177/0022146516671568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sibai A.M., Rizk A., Chemaitelly H. Self-rated health disparities among disadvantaged older adults in ethnically diverse urban neighborhoods in a Middle Eastern country. Ethn. Health. 2017;22:490–509. doi: 10.1080/13557858.2016.1244736. [DOI] [PubMed] [Google Scholar]
- 36.Centers for Disease Control and Prevention Racial/ethnic disparities in self-rated health status among adults with and without disabilities—United States, 2004–2006. MMWR Morb. Mortal. Wkly. Rep. 2008;57:1069–1073. [PubMed] [Google Scholar]
- 37.Cagney K.A., Browning C.R., Wen M. Racial disparities in self-rated health at older ages: What difference does the neighborhood make? J. Gerontol. B Psychol. Sci. Soc. Sci. 2005;60:S181–S190. doi: 10.1093/geronb/60.4.S181. [DOI] [PubMed] [Google Scholar]
- 38.Maguire P.A., Reay R.E., Raphael B. Correlates of a single-item Self-Rated Mental Health Question in people with schizophrenia. Australas. Psychiatry. 2016;24:473–477. doi: 10.1177/1039856216638789. [DOI] [PubMed] [Google Scholar]
- 39.Chandola T., Jenkinson C. Validating self-rated health in different ethnic groups. Ethn. Health. 2000;5:151–159. doi: 10.1080/713667451. [DOI] [PubMed] [Google Scholar]
- 40.Meng Q., Xie Z., Zhang T. A single-item self-rated health measure correlates with objective health status in the elderly: A survey in suburban beijing. Front. Public Health. 2014;2:27. doi: 10.3389/fpubh.2014.00027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Assari S. Gender differences in the predictive role of self-rated health on short-term risk of mortality among older adults. SAGE Open Med. 2016;4:2050312116666975. doi: 10.1177/2050312116666975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Assari S., Lankarani M.M. Does Multi-morbidity Mediate the Effect of Socioeconomics on Self-rated Health? Cross-country Differences. Int. J. Prev. Med. 2015;6:85. doi: 10.4103/2008-7802.164413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Assari S. Psychiatric Disorders Differently Correlate with Physical Self-Rated Health across Ethnic Groups. J. Pers. Med. 2017;7:6. doi: 10.3390/jpm7040006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Assari S. Ethnic Groups Differ in How Poor Self-Rated Mental Health Reflects Psychiatric Disorders. J. Racial Ethn. Health Disparities. 2018;5:728–736. doi: 10.1007/s40615-017-0417-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Zajacova A., Huzurbazar S., Todd M. Gender and the structure of self-rated health across the adult life span. Soc. Sci. Med. 2017;187:58–66. doi: 10.1016/j.socscimed.2017.06.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.McAlpine D.D., McCreedy E., Alang S. The Meaning and Predictive Value of Self-rated Mental Health among Persons with a Mental Health Problem. J. Health Soc. Behav. 2018;59:200–214. doi: 10.1177/0022146518755485. [DOI] [PubMed] [Google Scholar]
- 47.Spuling S.M., Wolff J.K., Wurm S. Response shift in self-rated health after serious health events in old age. Soc. Sci. Med. 2017;192:85–93. doi: 10.1016/j.socscimed.2017.09.026. [DOI] [PubMed] [Google Scholar]
- 48.Altman C.E., Van Hook J., Hillemeier M. What Does Self-rated Health Mean? Changes and Variations in the Association of Obesity with Objective and Subjective Components Of Self-rated Health. J. Health Soc. Behav. 2016;57:39–58. doi: 10.1177/0022146515626218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Lee S., Schwarz N., Goldstein L.S. Culture-Sensitive Question Order Effects of Self-Rated Health Between Older Hispanic and Non-Hispanic Adults in the United States. J. Aging Health. 2014;26:860–883. doi: 10.1177/0898264314532688. [DOI] [PubMed] [Google Scholar]
- 50.Lee S., Schwarz N. Question context and priming meaning of health: Effect on differences in self-rated health between Hispanics and non-Hispanic Whites. Am. J. Public Health. 2014;104:179–185. doi: 10.2105/AJPH.2012.301055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Peersman W., Cambier D., De Maeseneer J., Willems S. Gender, educational and age differences in meanings that underlie global self-rated health. Int. J. Public Health. 2012;57:513–523. doi: 10.1007/s00038-011-0320-2. [DOI] [PubMed] [Google Scholar]
- 52.McMullen C.K., Luborsky M.R. Self-rated health appraisal as cultural and identity process: African American elders’ health and evaluative rationales. Gerontologist. 2006;46:431–438. doi: 10.1093/geront/46.4.431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Garbarski D., Dykema J., Croes K.D., Edwards D.F. How participants report their health status: Cognitive interviews of self-rated health across race/ethnicity, gender, age, and educational attainment. BMC Public Health. 2017;17:771. doi: 10.1186/s12889-017-4761-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Kawada T. Self-rated health and mortality with special reference to black-white difference. Ann. Epidemiol. 2017;27:295. doi: 10.1016/j.annepidem.2016.08.019. [DOI] [PubMed] [Google Scholar]
- 55.Alang S.M., McCreedy E.M., McAlpine D.D. Race, Ethnicity, and Self-Rated Health Among Immigrants in the United States. J. Racial Ethn. Health Disparities. 2015;2:565–572. doi: 10.1007/s40615-015-0106-y. [DOI] [PubMed] [Google Scholar]
- 56.Assari S., Lankarani M.M., Burgard S. Black-white difference in long-term predictive power of self-rated health on all-cause mortality in United States. Ann. Epidemiol. 2016;26:106–114. doi: 10.1016/j.annepidem.2015.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Chand R., Parker E., Jamieson L. Differences in, and Frames of Reference of, Indigenous Australians’ Self-rated General and Oral Health. J. Health Care Poor Underserved. 2017;28:1087–1103. doi: 10.1353/hpu.2017.0099. [DOI] [PubMed] [Google Scholar]
- 58.Siordia C., Nguyen H.T. The Comparative Frame of Reference in Self-Rated Health Questions Matters When Predicting Difficulty with Activities of Daily Living. J. Frailty Aging. 2015;4:175–180. doi: 10.14283/jfa.2015.59. [DOI] [PubMed] [Google Scholar]
- 59.Sargent-Cox K.A., Anstey K.J., Luszcz M.A. Patterns of longitudinal change in older adults’ self-rated health: The effect of the point of reference. Health Psychol. 2010;29:143–152. doi: 10.1037/a0017652. [DOI] [PubMed] [Google Scholar]
- 60.Sargent-Cox K.A., Anstey K.J., Luszcz M.A. Determinants of self-rated health items with different points of reference: Implications for health measurement of older adults. J. Aging Health. 2008;20:739–761. doi: 10.1177/0898264308321035. [DOI] [PubMed] [Google Scholar]
- 61.Manderbacka K., Kareholt I., Martikainen P., Lundberg O. The effect of point of reference on the association between self-rated health and mortality. Soc. Sci. Med. 2003;56:1447–1452. doi: 10.1016/S0277-9536(02)00141-7. [DOI] [PubMed] [Google Scholar]
- 62.Manderbacka K., Lundberg O. Examining points of reference of self-rated health among Swedish oldest old. Arch. Gerontol. Geriatr. 1996;23:47–60. doi: 10.1016/0167-4943(96)00707-8. [DOI] [PubMed] [Google Scholar]
- 63.Assari S. Socioeconomic Status and Self-Rated Oral Health; Diminished Return among Hispanic Whites. Dent. J. 2018;6:11. doi: 10.3390/dj6020011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Assari S., Caldwell C.H., Mincy R.B. Maternal Educational Attainment at Birth Promotes Future Self-Rated Health of White but Not Black Youth: A 15-Year Cohort of a National Sample. J. Clin. Med. 2018;7:93. doi: 10.3390/jcm7050093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Assari S., Lapeyrouse L.M., Neighbors H.W. Income and Self-Rated Mental Health: Diminished Returns for High Income Black Americans. Behav. Sci. 2018;8:50. doi: 10.3390/bs8050050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Assari S., Caldwell C.H., Zimmerman M.A. Perceived Neighborhood Safety During Adolescence Predicts Subsequent Deterioration of Subjective Health Two Decades Later; Gender Differences in a Racially-Diverse Sample. Int. J. Prev. Med. 2015;6:117. doi: 10.4103/2008-7802.170431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Assari S., Lankarani M.M., Piette J.D., Aikens J.E. Self-Rated Health and Glycemic Control in Type 2 Diabetes: Race by Gender Differences. J. Racial Ethn. Health Disparities. 2018;5:721–727. doi: 10.1007/s40615-017-0416-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Assari S., Dejman M., Neighbors H.W. Ethnic Differences in Separate and Additive Effects of Anxiety and Depression on Self-rated Mental Health Among Blacks. J. Racial Ethn. Health Disparities. 2016;3:423–430. doi: 10.1007/s40615-015-0154-3. [DOI] [PubMed] [Google Scholar]
- 69.Okamoto K., Momose Y., Fujino A., Osawa Y. Gender differences in the relationship between self-rated health (SRH) and 6-year mortality risks among the elderly in Japan. Arch. Gerontol. Geriatr. 2008;47:311–317. doi: 10.1016/j.archger.2007.08.013. [DOI] [PubMed] [Google Scholar]
- 70.Kavanagh A.M., Bentley R., Turrell G., Broom D.H., Subramanian S.V. Does gender modify associations between self rated health and the social and economic characteristics of local environments? J. Epidemiol. Community Health. 2006;60:490–495. doi: 10.1136/jech.2005.043562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Spiers N., Jagger C., Clarke M., Arthur A. Are gender differences in the relationship between self-rated health and mortality enduring? Results from three birth cohorts in Melton Mowbray, United Kingdom. Gerontologist. 2003;43:406–411. doi: 10.1093/geront/43.3.406. discussion 372–405. [DOI] [PubMed] [Google Scholar]
- 72.Assari S., Smith J.L., Zimmerman M.A., Bazargan M. Cigarette Smoking among Economically Disadvantaged African-American Older Adults in South Los Angeles: Gender Differences. Int. J. Environ. Res. Public Health. 2019;16:1208. doi: 10.3390/ijerph16071208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Bazargan M., Smith J.L., Cobb S., Barkley L., Wisseh C., Ngula E., Thomas R.J., Assari S. Emergency Department Utilization among Underserved African American Older Adults in South Los Angeles. Int. J. Environ. Res. Public Health. 2019;16:1175. doi: 10.3390/ijerph16071175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Schoenfeld D.E., Malmrose L.C., Blazer D.G., Gold D.T., Seeman T.E. Self-rated health and mortality in the high-functioning elderly—A closer look at healthy individuals: MacArthur field study of successful aging. J. Gerontol. 1994;49:M109–M115. doi: 10.1093/geronj/49.3.M109. [DOI] [PubMed] [Google Scholar]
- 75.Heidrich J., Liese A.D., Lowel H., Keil U. Self-rated health and its relation to all-cause and cardiovascular mortality in southern Germany. Results from the MONICA Augsburg cohort study 1984–1995. Ann. Epidemiol. 2002;12:338–345. doi: 10.1016/S1047-2797(01)00300-3. [DOI] [PubMed] [Google Scholar]
- 76.Moreno X., Huerta M., Albala C. Global self-rated health and mortality in older people. Gac. Sanit. 2014;28:246–252. doi: 10.1016/j.gaceta.2013.07.006. [DOI] [PubMed] [Google Scholar]
- 77.Dasbach E.J., Klein R., Klein B.E., Moss S.E. Self-rated health and mortality in people with diabetes. Am. J. Public Health. 1994;84:1775–1779. doi: 10.2105/AJPH.84.11.1775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Mavaddat N., Parker R.A., Sanderson S., Mant J., Kinmonth A.L. Relationship of self-rated health with fatal and non-fatal outcomes in cardiovascular disease: A systematic review and meta-analysis. PLoS ONE. 2014;9:e103509. doi: 10.1371/journal.pone.0103509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Idler E.L., Russell L.B., Davis D. Survival, functional limitations, and self-rated health in the NHANES I Epidemiologic Follow-up Study, 1992. First National Health and Nutrition Examination Survey. Am. J. Epidemiol. 2000;152:874–883. doi: 10.1093/aje/152.9.874. [DOI] [PubMed] [Google Scholar]
- 80.Kurlowicz L. The Geriatric Depression Scale (GDS) Geriatr. Nurs. 1999;20:212–213. doi: 10.3928/0098-9134-19990701-09. [DOI] [PubMed] [Google Scholar]
- 81.Assari S. Combined Racial and Gender Differences in the Long-Term Predictive Role of Education on Depressive Symptoms and Chronic Medical Conditions. J. Racial Ethn. Health Disparities. 2017;4:385–396. doi: 10.1007/s40615-016-0239-7. [DOI] [PubMed] [Google Scholar]
- 82.Martin L.M., Leff M., Calonge N., Garrett C., Nelson D.E. Validation of self-reported chronic conditions and health services in a managed care population. Am. J. Prev. Med. 2000;18:215–218. doi: 10.1016/S0749-3797(99)00158-0. [DOI] [PubMed] [Google Scholar]
- 83.Agyemang C., Denktas S., Bruijnzeels M., Foets M. Validity of the single-item question on self-rated health status in first generation Turkish and Moroccans versus native Dutch in the Netherlands. Public Health. 2006;120:543–550. doi: 10.1016/j.puhe.2006.03.002. [DOI] [PubMed] [Google Scholar]
- 84.Radeos M.S., Cydulka R.K., Rowe B.H., Barr R.G., Clark S., Camargo C.A., Jr. Validation of self-reported chronic obstructive pulmonary disease among patients in the ED. Am. J. Emerg. Med. 2009;27:191–196. doi: 10.1016/j.ajem.2008.01.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Pastorino S., Richards M., Hardy R., Abington J., Wills A., Kuh D., Pierce M., The National Survey of Health and Development Scientific and Data Collection Teams Validation of self-reported diagnosis of diabetes in the 1946 British birth cohort. Prim. Care Diabetes. 2015;9:397–400. doi: 10.1016/j.pcd.2014.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Vigen C., Kwan M.L., John E.M., Gomez S.L., Keegan T.H., Lu Y., Shariff-Marco S., Monroe K.R., Kurian A.W., Cheng I., et al. Validation of self-reported comorbidity status of breast cancer patients with medical records: The California Breast Cancer Survivorship Consortium (CBCSC) Cancer Causes Control. 2016;27:391–401. doi: 10.1007/s10552-016-0715-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Fontanelli M.M., Teixeira J.A., Sales C.H., Castro M.A., Cesar C.L., Alves M.C., Goldbaum M., Marchioni D.M., Fisberg R.M. Validation of self-reported diabetes in a representative sample of Sao Paulo city. Rev. Saude Publica. 2017;51:20. doi: 10.1590/s1518-8787.2017051006378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Nishi A., Kawachi I., Shirai K., Hirai H., Jeong S., Kondo K. Sex/gender and socioeconomic differences in the predictive ability of self-rated health for mortality. PLoS ONE. 2012;7:e30179. doi: 10.1371/journal.pone.0030179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Unden A.L., Elofsson S., Andreasson A., Hillered E., Eriksson I., Brismar K. Gender differences in self-rated health, quality of life, quality of care, and metabolic control in patients with diabetes. Gend. Med. 2008;5:162–180. doi: 10.1016/j.genm.2008.05.003. [DOI] [PubMed] [Google Scholar]
- 90.Rohlfsen L.S., Jacobs Kronenfeld J. Gender Differences in Trajectories of Self-Rated Health in Middle and Old Age: An Examination of Differential Exposure and Differential Vulnerability. J. Aging Health. 2014;26:637–662. doi: 10.1177/0898264314527477. [DOI] [PubMed] [Google Scholar]
- 91.Wang J.M., Lee L.O., Spiro A., 3rd Gender differences in the impact of warfare exposure on self-rated health. Women’s Health Issues. 2015;25:35–41. doi: 10.1016/j.whi.2014.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Assari S. Separate and Combined Effects of Anxiety, Depression and Problem Drinking on Subjective Health among Black, Hispanic and Non-Hispanic White Men. Int. J. Prev. Med. 2014;5:269–279. [PMC free article] [PubMed] [Google Scholar]
- 93.Assari S. Suicide Attempts in Michigan HealthCare System; Racial Differences. Brain Sci. 2018;8:124. doi: 10.3390/brainsci8070124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Assari S., Moazen-Zadeh E. Ethnic Variation in the Cross-sectional Association between Domains of Depressive Symptoms and Clinical Depression. Front. Psychiatry. 2016;7:53. doi: 10.3389/fpsyt.2016.00053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Assari S. Cross-country variation in additive effects of socio-economics, health behaviors, and comorbidities on subjective health of patients with diabetes. J. Diabetes Metab. Disord. 2014;13:36. doi: 10.1186/2251-6581-13-36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Desesquelles A.F., Egidi V., Salvatore M.A. Why do Italian people rate their health worse than French people do? An exploration of cross-country differentials of self-rated health. Soc. Sci. Med. 2009;68:1124–1128. doi: 10.1016/j.socscimed.2008.12.037. [DOI] [PubMed] [Google Scholar]
- 97.Jiao J., Drewnowski A., Moudon A.V., Aggarwal A., Oppert J.M., Charreire H., Chaix B. The impact of area residential property values on self-rated health: A cross-sectional comparative study of Seattle and Paris. Prev. Med. Rep. 2016;4:68–74. doi: 10.1016/j.pmedr.2016.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Stewart J.B., Scott J.W. The institutional decimation of Black American males. West. J. Black Stud. 1978;2:82. [Google Scholar]
- 99.Curry T.J. The Man-Not: Race, Class, Genre, and the Dilemmas of Black Manhood. Temple University Press; Philadelphia, PA, USA: 2017. [Google Scholar]
- 100.Watkins D.C., Walker R.L., Griffith D.M. A meta-study of Black male mental health and well-being. J. Black Psychol. 2010;36:303–330. doi: 10.1177/0095798409353756. [DOI] [Google Scholar]
- 101.Watkins D.C. Depression over the adult life course for African American men: Toward a framework for research and practice. Am. J. Men’s Health. 2012;6:194–210. doi: 10.1177/1557988311424072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Matthews D.D., Hammond W.P., Cole-Lewis Y., Nuru-Jeter A., Melvin T. Racial Discrimination and Depressive Symptoms Among African-American Men: The Mediating and Moderating Roles of Masculine Self-Reliance and John Henryism. Psychol. Men Masc. 2013;14:35–46. doi: 10.1037/a0028436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Hammond W.P. Taking it like a man: Masculine role norms as moderators of the racial discrimination-depressive symptoms association among African American men. Am. J. Public Health. 2012;102(Suppl. 2):S232–S241. doi: 10.2105/AJPH.2011.300485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Hammond P. Real men get depressed. Nurs. Times. 1995;91:58. [PubMed] [Google Scholar]
- 105.Sellers S.L., Neighbors H.W., Bonham V.L. Goal-striving stress and the mental health of college-educated Black American men: The protective effects of system-blame. Am. J. Orthopsychiatry. 2011;81:507–518. doi: 10.1111/j.1939-0025.2011.01116.x. [DOI] [PubMed] [Google Scholar]
- 106.Griffith D.M. “I AM a Man”: Manhood, Minority Men’s Health and Health Equity. Ethn. Dis. 2015;25:287–293. doi: 10.18865/ed.25.3.287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Assari S., Gibbons F.X., Simons R. Depression among Black Youth; Interaction of Class and Place. Brain Sci. 2018;8:108. doi: 10.3390/brainsci8060108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Assari S. Educational Attainment Better Protects African American Women than African American Men Against Depressive Symptoms and Psychological Distress. Brain Sci. 2018;8:182. doi: 10.3390/brainsci8100182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Wang J., Mann F., Lloyd-Evans B., Ma R., Johnson S. Associations between loneliness and perceived social support and outcomes of mental health problems: A systematic review. BMC Psychiatry. 2018;18:156. doi: 10.1186/s12888-018-1736-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Snowden M.B., Steinman L.E., Carlson W.L., Mochan K.N., Abraido-Lanza A.F., Bryant L.L., Duffy M., Knight B.G., Jeste D.V., Leith K.H., et al. Effect of physical activity, social support, and skills training on late-life emotional health: A systematic literature review and implications for public health research. Front. Public Health. 2014;2:213. doi: 10.3389/fpubh.2014.00213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Haber M.G., Cohen J.L., Lucas T., Baltes B.B. The relationship between self-reported received and perceived social support: A meta-analytic review. Am. J. Community Psychol. 2007;39:133–144. doi: 10.1007/s10464-007-9100-9. [DOI] [PubMed] [Google Scholar]
- 112.Taylor R.J., Chatters L.M., Lincoln K., Woodward A.T. Church-Based Exchanges of Informal Social Support among African Americans. Race Soc. Probl. 2017;9:53–62. doi: 10.1007/s12552-017-9195-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Nguyen A.W., Taylor R.J., Chatters L.M. Church-Based Social Support Among Caribbean Blacks in the United States. Rev. Relig. Res. 2016;58:385–406. doi: 10.1007/s13644-016-0253-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Nguyen A.W., Chatters L.M., Taylor R.J., Mouzon D.M. Social Support from Family and Friends and Subjective Well-Being of Older African Americans. J. Happiness Stud. 2016;17:959–979. doi: 10.1007/s10902-015-9626-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Cross C.J., Taylor R.J., Chatters L.M. Family Social Support Networks of African American and Black Caribbean Adolescents. J. Child Fam. Stud. 2018;27:2757–2771. doi: 10.1007/s10826-018-1116-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Chatters L.M., Taylor R.J., Woodward A.T., Nicklett E.J. Social support from church and family members and depressive symptoms among older African Americans. Am. J. Geriatr. Psychiatry. 2015;23:559–567. doi: 10.1016/j.jagp.2014.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Krause N. Exploring the stress-buffering effects of church-based and secular social support on self-rated health in late life. J. Gerontol. B Psychol. Sci. Soc. Sci. 2006;61:S35–S43. doi: 10.1093/geronb/61.1.S35. [DOI] [PubMed] [Google Scholar]
- 118.Assari S., Moghani Lankarani M. Secular and Religious Social Support Better Protect Blacks than Whites against Depressive Symptoms. Behav. Sci. 2018;8:46. doi: 10.3390/bs8050046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Assari S. Race and Ethnicity, Religion Involvement, Church-based Social Support and Subjective Health in United States: A Case of Moderated Mediation. Int. J. Prev. Med. 2013;4:208–217. [PMC free article] [PubMed] [Google Scholar]
- 120.Lincoln K.D., Chatters L.M., Taylor R.J. Psychological distress among black and white Americans: Differential effects of social support, negative interaction and personal control. J. Health Soc. Behav. 2003;44:390–407. doi: 10.2307/1519786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Krause N. Church-based social support and health in old age: Exploring variations by race. J. Gerontol. B Psychol. Sci. Soc. Sci. 2002;57:S332–S347. doi: 10.1093/geronb/57.6.S332. [DOI] [PubMed] [Google Scholar]
- 122.Sonnenberg C.M., Deeg D.J., van Tilburg T.G., Vink D., Stek M.L., Beekman A.T. Gender differences in the relation between depression and social support in later life. Int. Psychogeriatr. 2013;25:61–70. doi: 10.1017/S1041610212001202. [DOI] [PubMed] [Google Scholar]
- 123.Sacco P., Bucholz K.K., Harrington D. Gender differences in stressful life events, social support, perceived stress, and alcohol use among older adults: Results from a National Survey. Subst. Use Misuse. 2014;49:456–465. doi: 10.3109/10826084.2013.846379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Okamoto K., Tanaka Y. Gender differences in the relationship between social support and subjective health among elderly persons in Japan. Prev. Med. 2004;38:318–322. doi: 10.1016/j.ypmed.2003.10.010. [DOI] [PubMed] [Google Scholar]
- 125.Landman-Peeters K.M., Hartman C.A., van der Pompe G., den Boer J.A., Minderaa R.B., Ormel J. Gender differences in the relation between social support, problems in parent-offspring communication, and depression and anxiety. Soc. Sci. Med. 2005;60:2549–2559. doi: 10.1016/j.socscimed.2004.10.024. [DOI] [PubMed] [Google Scholar]
- 126.Honjo K., Kawakami N., Takeshima T., Tachimori H., Ono Y., Uda H., Hata Y., Nakane Y., Nakane H., Iwata N., et al. Social class inequalities in self-rated health and their gender and age group differences in Japan. J. Epidemiol. 2006;16:223–232. doi: 10.2188/jea.16.223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Hajek A., Brettschneider C., Lange C., Posselt T., Wiese B., Steinmann S., Weyerer S., Werle J., Pentzek M., Fuchs A., et al. Gender differences in the effect of social support on health-related quality of life: Results of a population-based prospective cohort study in old age in Germany. Qual. Life Res. 2016;25:1159–1168. doi: 10.1007/s11136-015-1166-5. [DOI] [PubMed] [Google Scholar]
- 128.Cross C.J., Taylor R.J., Chatters L.M. Ethnic and Gender Differences in Family Social Support among Black Adolescents. Healthcare. 2018;6:20. doi: 10.3390/healthcare6010020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Cheng S.T., Chan A.C. Social support and self-rated health revisited: Is there a gender difference in later life? Soc. Sci. Med. 2006;63:118–122. doi: 10.1016/j.socscimed.2005.12.004. [DOI] [PubMed] [Google Scholar]
- 130.Chemaitelly H., Kanaan C., Beydoun H., Chaaya M., Kanaan M., Sibai A.M. The role of gender in the association of social capital, social support, and economic security with self-rated health among older adults in deprived communities in Beirut. Qual. Life Res. 2013;22:1371–1379. doi: 10.1007/s11136-012-0273-9. [DOI] [PubMed] [Google Scholar]
- 131.Caetano S.C., Silva C.M., Vettore M.V. Gender differences in the association of perceived social support and social network with self-rated health status among older adults: A population-based study in Brazil. BMC Geriatr. 2013;13:122. doi: 10.1186/1471-2318-13-122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Berard D.M., Vandenkerkhof E.G., Harrison M., Tranmer J.E. Gender differences in the influence of social support on one-year changes in functional status in older patients with heart failure. Cardiol. Res. Pract. 2012;2012:616372. doi: 10.1155/2012/616372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Bartley M., Martikainen P., Shipley M., Marmot M. Gender differences in the relationship of partner’s social class to behavioural risk factors and social support in the Whitehall II study. Soc. Sci. Med. 2004;59:1925–1936. doi: 10.1016/j.socscimed.2004.03.002. [DOI] [PubMed] [Google Scholar]
- 134.Cobb S., Assari S. Self-Rated Health in African American Men and Women; Evidence for Sponge Hypothesis. Int. J. Environ. Res. Public Health. 2019 doi: 10.34172/ijer.2020.05. Under Review. [DOI] [PMC free article] [PubMed] [Google Scholar]