Abstract
Patient experiences with the health-care system are increasingly seen as a vital measure of health-care quality. This study examined whether workplace social capital and employee outcomes are associated with patients’ perceptions of care quality across multiple clinic sites in a diverse, urban safety net care setting. Data from clinic staff were collected using paper and pencil surveys and data from patients were collected via a telephone survey. A total of 8392 adult primary care patients and 265 staff (physicians, nurses, allied health, and support staff) were surveyed at 10 community health clinics. The staff survey included brief measures of workplace social capital, burnout, and job satisfaction. The patient-level outcome was patients’ overall rating of the quality of care. Factor analysis and reliability analysis were conducted to examine measurement properties of the employee data. Data were aggregated and measures were examined at the clinic site level. Workplace social capital had moderate to strong associations with burnout (r = −0.40, P < .01) and job satisfaction (r = 0.59, P < .01). Mean patient quality of care rating was 8.90 (95% confidence interval: 8.86-8.94) ranging from 8.57 to 9.18 across clinic sites. Pearson correlations with patient-rated care quality were high for workplace social capital (r = 0.88, P = .001), employee burnout (r = −0.74, P < .05), and satisfaction (r = 0.69, P < .05). Patient-perceived clinic quality differences were largely explained by differences in workplace social capital, staff burnout, and satisfaction. Investments in workplace social capital to improve employee satisfaction and reduce burnout may be key to better patient experiences in primary care.
Keywords: clinician-patient relationship, outpatient satisfaction data, organizational culture, patient satisfaction, team communication
Introduction
The Institute for Healthcare Improvement’s Triple Aim is a framework used by organizations and coalitions in the quest toward the dimensions of better population health, improved care experience, and lower per capita costs (1). Today, the concept that Berwick and colleagues introduced is taught in medical schools, added to hospital mission statements, and worked into provider-payer contracts (1 –3). Payment reforms like accountable care organizations now mean that synchronous improvement in all 3 aims will lead to better reimbursement. Meanwhile, morale of health-care providers and staff is low and worsening. A survey conducted in 2014 found that 54% of physicians reported at least 1 symptom of burnout, climbing from 46% just 3 years earlier (4). Separate research found that 34% and 37% of nurses in hospitals and nursing homes, respectively, suffer from burnout in direct patient care roles (5). The magnitude of these frightening statistics inspired Drs. Bodenheimer and Sinsky to introduce a fourth aim: improving joy in practice for clinicians and staff (6).
Prior research has supported a link between this new fourth aim and the original third aim. A systematic review found that, in the majority of studies, poor clinician and staff well-being was associated with more medical errors (7). A number of studies have described positive associations between employee satisfaction/burnout and patient experience and care quality (5,8 –11). And lastly, burnout leads to high levels of absenteeism and staff turnover, increasing costs to health-care institutions (12).
In primary care, due to a growing provider shortage and increasingly challenging scope of work, the situation has been especially dire (13 –15). One study found that higher satisfaction scores for physicians and patients were associated with better continuity of care, lower no-show rates, and greater use of nonclinician staff in providing direct patient care (16). The search for joy in practice has lead one of us (D.M.) to travel the country with colleagues to describe what high-performing primary care practices do differently (17). It was clear from that work that research is needed to better understand the nuances of how teams work together and how that work relates to the experience of patients.
Health-care leaders acknowledge the importance of reducing burnout among clinicians and staff; however, the ways to do this remain elusive. Organizational behavior literature suggests that enhancing teamwork is at least part of the solution (18). Shortell and colleagues identified 3 factors that influence clinical team effectiveness: organizational culture, commitment to quality improvement, and presence of a team champion (19,20). Grace and colleagues found that perceptions of greater team culture were associated with less reported emotional exhaustion among primary care clinicians (21). Furthermore, their study found that tighter team structure only reduced symptoms of burnout (eg, emotional exhaustion) among clinicians reporting high team culture—in practices with low team culture, team structure had little effect on emotional exhaustion (21).
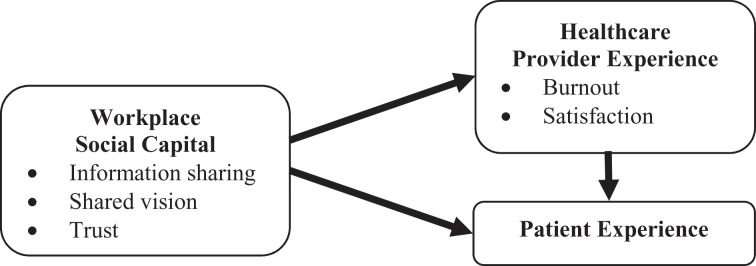
Our study builds on this work to better understand solutions to burnout and opportunities to improve employee well-being (and in turn patient experience) by measuring a dimension of teamwork called workplace social capital. Specifically, we focus on an “internal” dimension of workplace social capital conceptualized as the combination of information sharing, shared vision, and trust between team members. Authors have described the concept “bonding” social capital as referring to the strength and characteristics internal to homogenous groups or team (22 –26). Prior studies have previously established associations between employee burnout and patient satisfaction, particularly among nurses (5,12,27,28). Our research is distinct from this prior work in that we examine social capital concepts that are specific to the relationships among individuals working together as part of a social unit. The purpose of our study is to explore how workplace social capital is linked to employee experiences and patient experience in a multisite primary care environment. An important and unique contribution of this analysis is that we operationalized social capital as a workplace level (here, a primary care clinic) concept as opposed to a characteristic of individual employees or classes of employees. Our conceptual model is thus illustrated in Figure 1. Based on this model, we hypothesized that higher measures of workplace social capital (at the clinic level) and better employee self-rated outcomes (satisfaction and burnout) would be positively associated with patients’ perception of quality.
Figure 1.
Conceptual model of internal workplace social capital and provider and patient experience.
Methods
The MetroHealth institutional review board approved this study. This was an observational study focused on examining associations between workplace social capital, health-care provider experience, and patient experiences. For the purposes of this study, we developed and tested the “Practice Experience Survey,” a 23-item survey.
Setting
This study took place at an urban, academic safety net medical center in the Upper Midwest whose patient population is largely composed of minority groups and individuals of low income. The medical center employs more than 400 primary care and specialty care physicians and records more than 750 000 outpatient visits annually.
Workplace Social Capital Measures
Drawing on the work of Leana and Pil (29), workplace social capital was measured using survey items based on Nahapiet and Ghoshal’s 3 facets of social capital: structural, relational, and cognitive (30). The structural facet of social capital was operationalized as information sharing among clinic employees and measured using items adapted from items developed by Hyatt and Ruddy (31). These items ask respondents to rate how strongly they agree or disagree (on a 5-point scale) with statements asking if people: (1) engage in open and honest communication with one another, (2) share and accept constructive criticisms without making it personal, and (3) willingly share information with one another.
The relational facet of social capital was operationalized as trust among clinic employees. The trust measure consists of 3 items adapted from previous work on trust conducted by Pearce and colleagues (32,33). These items ask respondents to rate how strongly they agree or disagree (on a 5-point scale) with statements asking if: (1) they can rely on people in the clinic, (2) coworkers are considerate of one another’s feelings, and (3) coworkers have confidence in one another.
The cognitive facet of social capital was operationalized as 3 items assessing shared vision among employees within a clinic. These items were adapted from research in organizational behavior by Tsai (34) and from Sinkula and colleagues (35). Respondents were asked to rate how strongly they agree or disagree (on a 5-point scale) with statements asking if people: (1) share the same ambitions and vision for the clinic, (2) share a commonality of purpose, and (3) are committed to the goals of the clinic.
Employee Outcomes
Burnout (or emotional exhaustion) was measured with a modified 5-item scale utilized by Conley and Woosley in their study of role stress among elementary and secondary school teachers (36). The scale lists specific conditions and asks respondents to specify how often they experienced the described condition in the past month. The burnout items ask respondents to consider how often (never or rarely, occasionally, often, or almost always) they have experienced the following during the past month: (1) feeling fatigued and unable to “get going,” (2) feeling physically used up at the end of the day, (3) being emotionally drained from work, (4) feeling “burned out” from work, and (5) feeling “run down” at the end of the workday. Previous studies have demonstrated that burnout is an important employee outcome in a variety of professions (37 –40).
The job satisfaction measure is comprised of 6 items designed to measure the respondents’ interest in their job, enjoyment found in their work, and overall satisfaction derived from their employment (41). These items ask respondents to rate how satisfied they are with their employment “situation” (on a 5-point scale ranging from not at all satisfied to very satisfied). The situations include type of work, quality of direct supervision, satisfaction with leaders, working conditions, amount of praise received, and current overall level of satisfaction with their job.
Patient Quality Rating
The primary patient outcome for this study was a single item from the Clinician and Group Consumer Assessment of Healthcare Providers and Systems (CG-CAHPS) patient self-report survey (42). The CG-CAHPS is a standardized survey that was designed to help health-care organizations understand patients’ perspectives of their experience of care in the outpatient setting. The question selected as outcome for this study asks patients to give an overall rating of the quality of health care received on a scale from 1 to 10 (43).
Employee Sample
A total of 265 employees in 10 primary care outpatient clinics completed the Practice Experience Survey. This sample represents more than 50% of the staff at the clinics. Employees were eligible to participate if they had direct contact with patients. This included physician providers (33%), nurses (19%), medical technology assistants (10%), patient service representatives (12%), and other professionals (27%), which include social workers and financial counselors, physical therapists, and other allied health personnel. This was an anonymous paper and pencil survey.
Patient Sample
A total of 8392 adult primary care patients were surveyed at 10 community health clinics of a large, urban safety net health system. This represents a 5% random sample of all patients seen at participating outpatient clinics during the 6 months prior to and the 6 months immediately following the employee survey. The health-care system serving as the primary research site functions as a safety net care system and the practices participating in this study are reflective of the broader population served and the communities in Ohio which the patients reside.
We contracted with an outside vendor, Quality Data Management, to randomly survey patients about their experiences. Patients completed these surveys over the telephone, via a computer-assisted telephone interview. The vendor collected some limited demographic information from participants: 69.5% were female and 30.5% were male; by age, 17.7% were under 25, 8.3% were 25 to 34, 12.2% were 35 to 44, 44.6% were 45 to 64, and 17.1% were 65 and over; by race, 54.8% were black, 37.0% were white, 4.9% were Hispanic, and 3.3% were from other unspecified racial and ethnic groups.
Data Analysis
Initially, frequency tables and univariate descriptive statistics were used to examine the data for distributional assumptions and outliers. Confirmatory factor analysis (44) (CFA) was then used to examine the measurement structure of the workplace social capital scale. Confirmatory factor analysis is a statistical technique useful for understanding the measurement structure of a set of related indicators or survey questions and is particularly appropriate for a scenario such as the current study where the structure of specific indicators and scales is explicitly hypothesized due to prior theoretical work (44,45). Due to the overlapping nature of the dimensions being measured, we hypothesized a second-order factor structure with 3 first-order subscales and a single unifying latent variable representing workplace social capital. Our primary test for the fit of these models was the Comparative Fit Index (CFI), computed as the discrepancy function adjusted for sample size and has a range from 0 to 1. Higher values indicate better fit and CFI values of 0.90 or greater indicate acceptable model fit (46). We also report the similarly interpreted Tucker-Lewis Index (TLI) and the root mean square error of approximation (RMSEA). Values close to or below .06 have been considered acceptable for RMSEA (46). Cronbach α was used to examine the reliability of all the composite scales (47). All of the employee scales were reliable and showed high internal consistency (Table 1). Analysis of variance was conducted to examine between clinic differences on the employee workplace social capital, burnout, and satisfaction scales. Pearson correlations (48) were used to estimate the relationship among each of the workplace social capital subscales and with burnout and satisfaction. A structural equation model (49,50) was used to estimate the associations between the workplace social capital latent variable and the employee outcomes of burnout and satisfaction. Bivariate plots and correlation coefficients were used to examine the associations between employee variables and the CG-CAHPS patient rating of overall care quality. Due to the skewed distribution of the patient quality measure (as in most studies, patients give highly positive ratings), the bootstrap method with 1000 samples was used to estimate 95% confidence intervals (CIs) for all estimates (51). Analyses were conducted using SPSS version 21 and AMOS (52,53).
Table 1.
Internal Consistency Analysis.
| Scale | Cronbach α | No. of Items |
|---|---|---|
| Trust | .805 | 3 |
| Shared vision | .828 | 3 |
| Information sharing | .788 | 3 |
| Workplace social capital | .903 | 9 |
| Burnout | .937 | 5 |
| Satisfaction | .861 | 6 |
Results
Results of the CFA model indicated adequate to good fit of the model (CFI = .97, TLI = .94, RMSEA = .075, χ2 = 59.9, df = 24, P < .001), with high (>.80) factor loadings; the second-order factor structure was thus confirmed. In analysis of variance results, the workplace social capital and employee outcome measures all demonstrated significant variation across sites (Table 2). Employee workplace social capital measures had moderate-to-strong bivariate correlations with employee outcomes (Table 3). Higher shared vision, stronger trust, and better information sharing were moderately correlated with higher job satisfaction and lower burnout. The burnout and satisfaction measures were further added to the second-order factor model to determine the associations with the error-corrected workplace social capital latent variable (Figure 2). Associations between the latent variable for workplace social capital and burnout and satisfaction are similar (though slightly higher) than the composite indicator constructed as the mean of the observed indicators (a reasonable result, as the mean of the observed indicators is not error corrected).
Table 2.
Analysis of Variance for the Difference in Workplace Social Capital and Employee Outcomes Across Clinic Sites.a
| F | Significance (2-Tailed) | R 2 | |
|---|---|---|---|
| Trust | 2.819 | .004 | .058 |
| Shared vision | 2.786 | .004 | .057 |
| Information sharing | 4.373 | .000 | .103 |
| Workplace social capital | 4.475 | .000 | .135 |
| Burnout | 4.52 | .000 | .107 |
| Satisfaction | 4.946 | .000 | .119 |
a N = 265, df = 9.
Table 3.
Associations Between Employee Social Capital and Employee Outcomes.a
| Trust | Vision | Information Sharing | Workplace Social Capital | Burnout | Satisfaction | |
|---|---|---|---|---|---|---|
| Social capital | ||||||
| Trust | 1 | |||||
| Vision | .697b | 1 | ||||
| Information sharing | .681b | .657b | 1 | |||
| Employee outcomes | ||||||
| Burnout | −.323b | −.327b | −.423b | −.400b | 1 | |
| Satisfaction | .511b | .471b | .572b | .585b | −.591b | 1 |
a N = 265.
b Correlation is significant at the 0.01 level (2-tailed).
Figure 2.
Second-order factor model of internal workplace social capital with effects on burnout and satisfaction, N = 265: CFI = .96, TLI = 94, RMSEA = .069, χ2 = 90.4, df = 40, P <.001. Model path coefficients are standardized correlations, and item-level parameters are squared multiple correlations. CFI indicates Comparative Fit Index; RMSEA, root mean square error of approximation; TLI, Tucker-Lewis Index.
The mean patient quality of care rating was 8.90 (95% CI: 8.86-8.94) ranging from 8.57 to 9.18 across clinic sites. Overall patient quality ratings were in the good-to-average range for the clinics in this study, but some sites performed significantly better than others.
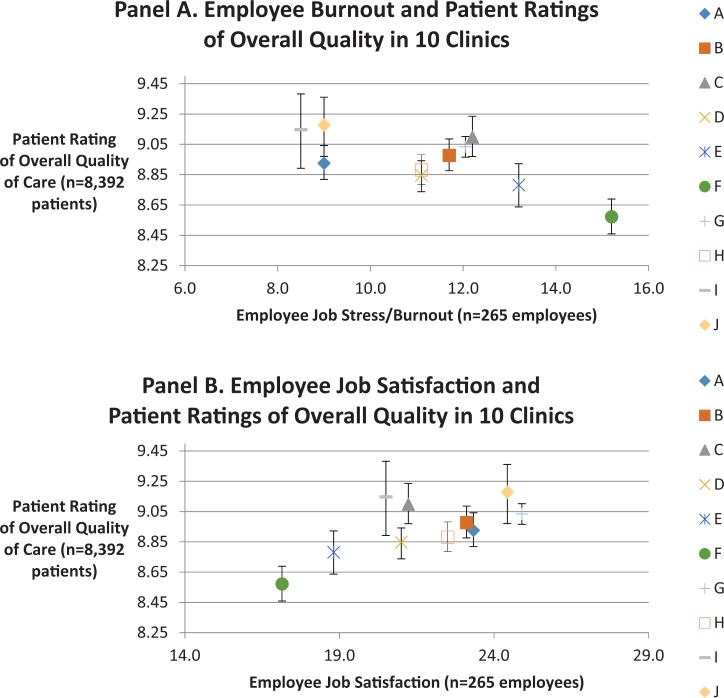
In clinic-level analysis, the differences in patient perceived quality ratings were almost completely explained by differences in employee burnout and satisfaction (Figure 3). Clinics with the higher levels of burnout had lower patient ratings of overall care quality, while clinics with higher levels of satisfaction had higher patient ratings of overall care quality. Pearson correlations with patient ratings of care quality were very strong for burnout (r = −0.74, P < .05), satisfaction (r = 0.69, P < .05), shared vision (r = 0.68, P < .05), and information sharing (r = 0.63, P = .05). The correlation between patient quality of care ratings and trust was moderate and not statistically significant (r = 0.45, P > .10; Table 4).
Figure 3.
Clinic-level associations between employee outcomes and patient experience. Whiskers in the Figure 3 panels represent 95% confidence intervals.
Table 4.
Associations Between Patient Ratings of Quality and Employee Rating of Workplace Social Capital and Outcomes.a
| Pearson Correlation | Significance (2-Tailed) | |
|---|---|---|
| Trust | .446 | .197 |
| Vision | .682 | .030 |
| Information sharing | .630 | .051 |
| Workplace social capital | .884 | .001 |
| Burnout | −.745 | .013 |
| Satisfaction | .688 | .028 |
a Employee N = 265, patient N = 8392.
Discussion
Based on the model presented in Figure 1, we had hypothesized that higher levels of workplace social capital would be positively associated with satisfaction and inversely associated with burnout and that these health-care employee outcomes would in turn influence patient ratings of care quality. Our study found strong correlations between patient quality of care ratings and two critical employee outcomes: burnout and satisfaction. In further analysis, practices with the highest level of employee satisfaction and lowest burnout had the best patient ratings of overall quality, while practices with low levels of employee satisfaction and higher burnout had the worst patient ratings of overall quality. Taken together, these findings suggest that workplace social capital could be a key characteristic of effective health-care teams. The clinic-level linkage between clinician and staff well-being and patient satisfaction is an important observation for health-care administrators and other officials seeking to improve quality and outcomes in primary care settings.
This study has several important limitations. Employee surveys were anonymous. This design decision was necessary in order to receive honest evaluations of the workplace environment from employees who work there; the anonymous surveys omitted employee characteristics such as gender, race/ethnicity, and years employed in order to avoid suspicion of identifiability. Though unlikely, this observational study design constraint leaves open the possibility of potential confounding, in that unmeasured employee demographic characteristics could be driving both employee outcomes and patient ratings of quality. Response rate data were not available for the patient survey. The computerized vendor system is designed to continue sampling until reaching the 5% threshold, and response rate data were not available from the vendor. The use of a single health-care system is a further limitation, and we look forward to future work that investigates whether these results can be replicated in other venues.
While prior studies in other organizational settings have shown salutary associations between other measures of social capital, burnout, and employee satisfaction, we undertook this study to assess the extent to which these employee-level constructs are associated with patient experiences within a health-care setting. Understanding the interrelationship between these constructs is a necessary step in designing interventions aimed at improving and maintaining levels of workplace social capital and ultimately patient outcomes. In addition, the newly developed measures have strong psychometric properties and are brief enough to be administered with efficiency even in a busy safety net health-care organization.
Our findings suggest that in general, workplace social capital subscales are easily adapted for use in a variety of organizational venues and are fairly robust in their relationships to one another and to employee outcomes. The theory that social networks usually coexist within other networks can be extended to health-care organizations (54). When patients navigate the health-care system, they become aware of the gaps and flaws in these networks. A fruitful line of future inquiry would be to examine the efficacy of actively promoting internal workplace social capital for health-care teams. This would allow researchers and health-care administrators to learn more about how to cultivate care teams that improve the experience and quality of care.
Our results indicate the potential of ties among employees to help narrow such gaps. Processes of building internal workplace social capital must first create a sense of community based on shared values and common goals. This is paramount for promoting collaborative working relationships that are necessary to ensure high quality, high value care and services and implement successful practice transformation. As has been observed in other settings, higher levels of internal workplace social capital in health-care organizations will allow employees to resolve collective problems more easily, allow information to flow more freely and facilitate the attainment of goals, better prepare providers to deal with conflict, and improve individuals’ lives.
Most encouraging is that our results parallel those of another similar study which found evidence that patient satisfaction with nursing care was associated with patient intentions to recommend the hospital (8). Our work extends this prior research substantially. The prior study examined only inpatient data and had a small sample size when compared with the current study. The robustness of these findings in primary care is further evidence of the important link between the workplace experiences of health-care professionals and the outcomes of the patients for whom they provide care.
Confirming the conceptual model presented in Figure 1, the strong association between internal workplace social capital and employee outcomes suggests the potential for a mediating relationship through which structural, relational, and cognitive workplace social capital influence employee outcomes (burnout and satisfaction), which in turn influences patient ratings of quality. Although our study design prevented a direct test of mediation, future studies (in particular those with a longitudinal design) should consider this mediation model.
Efforts to enhance workplace social capital could be a potentially effective mechanism for moving closer to the coevolving goals of the quadruple aim (6). One potential avenue would be to use a collaborative learning approach in which employees in high-performing clinics serve as models for lower performing clinics. Health-care organizations interested in delivering high value care and improving patient ratings of care quality should look closely at these potential mechanisms for promoting the joy of practice among health-care professionals, with specific attention to reducing burnout and increasing satisfaction.
Author biographies
Adam Perzynski is assistant professor of Medicine and Sociology in the Center for Health Care Research and Policy at MetroHealth and Case Western Reserve University. His research methods expertise ranges from focus groups and ethnography to psychometrics and structural equation modelling. Dr. Perzynski's work represents a career long effort to infuse the study of biomedical scientific problems with the knowledge, theories and methods of social science.
Aleece Caron is the senior medical educator at The MetroHealth System and is responsible for developing and evaluating provider education curricula with particular focus on Practice Based Learning and Improvement and communication and interpersonal skills. Specifically, she has led and participated in dozens of successful educational and quality improvement projects and have had extensive experience mentoring faculty, residents and students on their QI projects, many of which have been presented nationally. She leads the Quality Improvement Faculty Development course for the MetroHealth System and the NCQA PCMH QI program for the system.
David Margolius is the medical lead for MetroHealth's main campus Internal Medicine practice and the associate division director for General Internal Medicine. Apart from his clinical and administrative roles he serves as the director of a semi-annual conference for the regional health improvement collaborative, Better Health Partnership. His research interests are in implementing team-based care and redesigning primary care.
Joseph J Sudano Jr is a medical sociologist and health services researcher and faculty member in the Population Health Unit in the Center for Health Care Research and Policy, Case Western Reserve University at The MetroHealth System and assistant professor in the Department of Medicine, Case Western Reserve University. He is also the director of Education in the Center for Reducing Health Disparities at Case Western Reserve University. His current research interests include: disparities in health care access, utilization and health outcomes concentrating on minorities and other vulnerable populations; and the social determinants of health including community/contextual characteristics.
Footnotes
Declaration of Conflicting Interests: The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: Dr Perzynski reports being cofounder of Global Health Metrics, LLC and royalty agreements with Springer Publishing and Taylor Francis. Dr Sudano reports being cofounder of Global Health Metrics, LLC.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Berwick DM, Nolan TW, Whittington J. The triple aim: care, health, and cost. Health Aff (Millwood). 2008;27(3):759–69. [DOI] [PubMed] [Google Scholar]
- 2. Berwick DM. Launching accountable care organizations—the proposed rule for the Medicare Shared Savings Program. N Engl J Med. 2011;364:e32. [DOI] [PubMed] [Google Scholar]
- 3. Berwick DM, Feeley D, Loehrer S. Change from the inside out: health care leaders taking the helm. JAMA. 2015;313:1707–8. [DOI] [PubMed] [Google Scholar]
- 4. Shanafelt TD, Hasan O, Dyrbye LN, Sinsky C, Satele D, Sloan J, et al. Changes in burnout and satisfaction with work-life balance in physicians and the general US working population between 2011 and 2014. Mayo Clin Proc. 2015;90:1600–13. Elsevier. [DOI] [PubMed] [Google Scholar]
- 5. McHugh MD, Kutney-Lee A, Cimiotti JP, Sloane DM, Aiken LH. Nurses’ widespread job dissatisfaction, burnout, and frustration with health benefits signal problems for patient care. Health Aff (Millwood). 2011;30:202–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Bodenheimer T, Sinsky C. From triple to quadruple aim: care of the patient requires care of the provider. Ann Fam Med. 2014;12:573–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Hall LH, Johnson J, Watt I, Tsipa A, O’Connor DB. Healthcare staff wellbeing, burnout, and patient safety: a systematic review. PLoS One. 2016;11:e0159015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Atkins PM, Marshall BS, Javalgi RG. Happy employees lead to loyal patients. J Health Care Mark. 1996;16:14. [PubMed] [Google Scholar]
- 9. Shirley ED, Sanders JO. Patient satisfaction: implications and predictors of success. J Bone Joint Surg Am. 2013;95:e69. [DOI] [PubMed] [Google Scholar]
- 10. Barr DA. The effects of organizational structure on primary care outcomes under managed care. Ann Inter Med. 1995;122:353–9. [DOI] [PubMed] [Google Scholar]
- 11. Williams ES, Manwell LB, Konrad TR, Linzer M. The relationship of organizational culture, stress, satisfaction, and burnout with physician-reported error and suboptimal patient care: results from the MEMO study. Health Care Manage Rev. 2007;32:203–12. [DOI] [PubMed] [Google Scholar]
- 12. Kaldenberg DO, Regrut B. Do satisfied patients depend on satisfied employees? Or, do satisfied employees depend on satisfied patients? QRC Advis. 1999;15:9–12. [PubMed] [Google Scholar]
- 13. Bodenheimer T. Primary care—will it survive? N Engl J Med. 2006;355:861–4. [DOI] [PubMed] [Google Scholar]
- 14. Linzer M, Manwell LB, Williams ES, Bobula JA, Brown RL, Varkey AB, et al. ; MEMO (Minimizing Error, Maximizing Outcome) Investigators. Working conditions in primary care: physician reactions and care quality. Ann Inter Med. 2009;151:28–36. [DOI] [PubMed] [Google Scholar]
- 15. Rabatin J, Williams E, Baier Manwell L, Schwartz MD, Brown RL, Linzer M. Predictors and outcomes of burnout in primary care physicians. J Prim Care Community Health. 2016;7:41–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Linn LS, Brook RH, Clark VA, Davies AR, Fink A, Kosecoff J. Physician and patient satisfaction as factors related to the organization of internal medicine group practices. Med Care. 1985;23:1171–8. [DOI] [PubMed] [Google Scholar]
- 17. Sinsky CA, Willard-Grace R, Schutzbank AM, Sinsky TA, Margolius D, Bodenheimer T. In search of joy in practice: a report of 23 high-functioning primary care practices. Ann Fam Med. 2013;11:272–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Hoegl M, Gemuenden HG. Teamwork quality and the success of innovative projects: a theoretical concept and empirical evidence. Organization Sci. 2001;12:435–49. [Google Scholar]
- 19. Shortell SM, Jones RH, Rademaker AW, Gillies RR, Dranove DS, Hughes EF, et al. Assessing the impact of total quality management and organizational culture on multiple outcomes of care for coronary artery bypass graft surgery patients. Med Care. 2000;38:207–17. [DOI] [PubMed] [Google Scholar]
- 20. Shortell SM, Marsteller JA, Lin M, Pearson ML, Wu SY, Mendel P, et al. The role of perceived team effectiveness in improving chronic illness care. Med Care. 2004;42:1040–8. [DOI] [PubMed] [Google Scholar]
- 21. Willard-Grace R, Hessler D, Rogers E, Dubé K, Bodenheimer T, Grumbach K. Team structure and culture are associated with lower burnout in primary care. J Am Board Fam Med. 2014;27:229–38. [DOI] [PubMed] [Google Scholar]
- 22. Adler PS, Kwon SW. Social capital: prospects for a new concept. Acad Manag Rev. 2002;27:17–40. [Google Scholar]
- 23. Gulliford MC, Jack RH, Adams G, Ukoumunne OC. Availability and structure of primary medical care services and population health and health care indicators in England. BMC Health Serv Res. 2004;4:12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Leonard M. Bonding and bridging social capital: reflections from Belfast. Sociology. 2004;38:927–44. [Google Scholar]
- 25. Newell S, Tansley C, Huang J. Social capital and knowledge integration in an ERP project team: the importance of bridging and bonding. British J Manage. 2004;15:S43–57. [Google Scholar]
- 26. Woolcock M, Narayan D. Social capital: implications for development theory, research, and policy. World Bank Res Obs. 2000;15:225–49. [Google Scholar]
- 27. Vahey DC, Aiken LH, Sloane DM, Clarke SP, Vargas D. Nurse burnout and patient satisfaction. Med Care. 2004;42:II57–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Mayer TA, Cates RJ. Leadership for Great Customer Service: Satisfied Patients, Satisfied Employees. Chicago, IL: Health Administration Press; 2004. [Google Scholar]
- 29. Leana CR, Pil FK. Social capital and organizational performance: evidence from urban public schools. Organization Sci. 2006;17:353–66. [Google Scholar]
- 30. Nahapiet J, Ghoshal S. Social capital, intellectual capital, and the organizational advantage. Acad Manag Rev. 1998;23:242–66. [Google Scholar]
- 31. Hyatt DE, Ruddy TM. An examination of the relationship between work group characteristics and performance: once more into the breech. Pers Psychol. 1997;50:553–85. [Google Scholar]
- 32. Pearce JL, Bigley GA, Branyiczki I. Procedural justice as modernism: placing industrial/organisational psychology in context. App Psychol. 1998;47:371–96. [Google Scholar]
- 33. Pearce J, Sommer S, Morris A, Frideger M. A configurational approach to interpersonal relations: profiles of workplace social relations and task interdependence. Irvine: Graduate School Management, University of California; 1992. [Google Scholar]
- 34. Tsai W. Social structure of “coopetition” within a multiunit organization: coordination, competition, and intraorganizational knowledge sharing. Organiz Sci. 2002;13:179–90. [Google Scholar]
- 35. Sinkula JM, Baker WE, Noordewier T. A framework for market-based organizational learning: linking values, knowledge, and behavior. J Academy Marketing Sci. 1997;25:305. [Google Scholar]
- 36. Conley S, Woosley SA. Teacher role stress, higher order needs and work outcomes. J Edu Admin. 2000;38:179–201. [Google Scholar]
- 37. Kalliath TJ, O’Driscoll MP, Gillespie DF, Bluedorn AC. A test of the Maslach Burnout Inventory in three samples of healthcare professionals. Work Stress. 2000;14:35–50. [Google Scholar]
- 38. Maslach C, Jackson SE. The measurement of experienced burnout. J Organizat Behav. 1981;2:99–113. [Google Scholar]
- 39. Dhurup M, Dubihlela D. Sport coaching officials and their stressors: work overload, role ambiguity, role conflict and the influence on job satisfaction of sport coaching officials in Gauteng province, South Africa: sport coaching. Afr J Phys Health Educ Recr Dance. 2014;20:732–44. [Google Scholar]
- 40. Pitney WA, Stuart ME, Parker J. Role strain among dual position physical educators and athletic trainers working in the high school setting. Phys Educ. 2008;65:157. [Google Scholar]
- 41. Allen NJ, Meyer JP. The measurement and antecedents of affective, continuance and normative commitment to the organization. J Occup Organ Psychol. 1990;63:1–18. [Google Scholar]
- 42. The Consumer Assessment of Healthcare Providers and Systems (CAHPS) Program: Surveys and Tools to Advance Patient-Centered Care. Agency for Healthcare Research and Quality. Rockville, MD.
- 43. Hays RD, Shaul JA, Williams VS, Lubalin JS, Harris-Kojetin LD, Sweeny SF, et al. Psychometric properties of the CAHPS™ 1.0 survey measures. Med Care. 1999;37:MS22–MS31. [DOI] [PubMed] [Google Scholar]
- 44. Brown TA. Confirmatory Factor Analysis for Applied Research. New York, NY: Guilford Publications; 2014. [Google Scholar]
- 45. Fox RJ. Confirmatory Factor Analysis. Hoboken, NJ: Wiley Online Library; 1983. [Google Scholar]
- 46. Hu Lt, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct Equ Model. 1999;6:1–55. [Google Scholar]
- 47. Cronbach LJ. Test “reliability”: its meaning and determination. Psychometrika. 1947;12:1–16. [DOI] [PubMed] [Google Scholar]
- 48. Mukaka M. A guide to appropriate use of correlation coefficient in medical research. Malawi Med J. 2012;24:69–71. [PMC free article] [PubMed] [Google Scholar]
- 49. Bollen KA. Structural Equations with Latent Variables. Hoboken, NJ: John Wiley & Sons; 2014. [Google Scholar]
- 50. Bollen KA, Long JS. Testing Structural Equation Models. Thousand Oaks, CA: Sage; 1993. [Google Scholar]
- 51. Efron B, Tibshirani RJ. An Introduction to the Bootstrap. Boca Raton, FL: CRC Press; 1994. [Google Scholar]
- 52. SPSS. IBM SPSS Statistics Version 21. Boston, MA: International Business Machines Corp; 2012:126. [Google Scholar]
- 53. Arbuckle J. AMOS 21 Reference Guide. Chicago, IL: Small Waters Corporation; 2012. [Google Scholar]
- 54. Palla G, Derényi I, Farkas I, Vicsek T. Uncovering the overlapping community structure of complex networks in nature and society. Nature. 2005;435:814–18. [DOI] [PubMed] [Google Scholar]