Abstract
Background and Aims:
Transversus abdominis plane (TAP) and Ilioinguinal/Iliohypogastric (IL/IH) nerve blocks have been advocated in reducing postoperative pain and additional analgesic requirement following lower abdominal surgeries with varied effect. The aim of this study was to determine post-operative analgesic efficacy by comparing dual TAP [combining TAP and IL/IH nerve blocks] and IL/IH nerve block alone for open inguinal hernia repair.
Methods:
Two hundred patients undergoing elective primary unilateral open inguinal hernia repair with a mesh were included in to this trial. Ultrasound-guided dual TAP (D-TAP Group) or IL/IH (IL/IH Group) nerve block were administered to patients following subarachnoid block according to their group allocation, with 0.5% ropivacaine. Post operatively patients were monitored for visual analogue scale (VAS) scores at rest (at 4, 12, 24 and 48h) and during movement (at 24, 48 h, 3 and 6 months). Pain scores at 3 and 6 months were assessed by telephonic interview, using the DN4 questionnaire for neuropathic pain. The statistics was obtained using Chi-square test for proportions in qualitative data and student's unpaired t test for quantitative data. P value <0.05 was considered significant.
Results:
The pain scores at rest (VAS-R) were significantly lower at 12 hours and 24 hours (P < 0.001) in D-TAP group, while pain scores at movement were significantly lower (P < 0.001) in D-TAP group at 24 and 48 hours compared to IL/IH group. The mean time required for first rescue analgesic was longer in D-TAP group (5.590 ± 2.386 hr) in comparison to IL/IH group (3.1053 ± 1.1822h).
Conclusion:
Ultrasound-guided dual TAP block provides more effective post-operative analgesia in open inguinal hernia repair.
Keywords: Iliohypogastric/Ilioinguinal nerve block, postoperative analgesia, transversus abdominis plane block
INTRODUCTION
Open inguinal hernia surgery is one of the most common procedures performed across the world and is associated with pain. The incidence reported to be 11 to 200/10,000 populations in the age group of 16–24 years and over 75 years, respectively.[1,2]
Pain after hernia repair is either due to neuropathic aetiology, resulting from nerve injury or compression and may be due to non-neuropathic cause resulting from scar tissue, mechanical pressure or meshomas. Various treatment modalities have been advocated in postoperative hernia repair pain management. Most of them have been proved inconsistent. Opioids and NSAIDs provide good analgesia but are associated with several undesirable side effects.[3]
Ultrasound (US)-guided Ilioinguinal and Iliohypogastric nerve and TAP block have been established as analgesic adjuncts for post hernia repair pain management,[4,5,6] under general anaesthesia, neuraxial, MAC and infiltration techniques.
US-guided technique of blocking Ilioinguinal and Iliohypogastric nerves have higher success rate compared to conventional technique.[5] TAP block provides analgesia to the parietal peritoneum and skin of the abdomen in infra-umbilical surgeries.[6] Few cadaveric studies showed good analgesic effect in the region between T10 and L1 following a single posterior TAP injection.[7]
Though there are many studies of comparing efficacy of TAP and IL/IH nerve block there is no single study of comparison of dual TAP block and IL/IH nerve block. Hence, the present prospective study was conducted to compare the post-operative analgesic efficacy in both groups in adult patients undergoing open hernia repair. A secondary purpose was to assess requirement of rescue analgesia, length of hospital stay and any complications.
METHODS
This study was registered with Clinical Trials Registry – India (CTRI/2018/01/011590) prospectively. After approval of local ethical committee and written informed consent 200 patients between 18 and 60 years of age American Society of Anaesthesiology (ASA) physical status I–II undergoing elective primary unilateral open inguinal hernia repair with a mesh, were enrolled in to this prospective randomised controlled clinical trial.
Patients who refused to consent to the study, Body Mass Index ≥40 kg/m2, patients who were scheduled for bilateral or recurrent inguinal hernia repair, poorly regulated systemic disease (poorly controlled diabetes or hypertension, severe coronary artery disease, end-stage renal disease), neuromuscular diseases and patients with hypersensitivity to local aesthetic drugs were excluded from the study.
Patients were randomly divided into two groups by using a computer-generated randomisation. Sealed opaque envelopes containing group allocation were opened before the blocks were performed. The dual TAP (D-TAP) group comprised patients who underwent the US-guided TAP block in addition to the US-guided ilioinguinal/iliohypogastric nerve block, while the IL/IH group comprised patients who underwent the US-guided ilioinguinal/iliohypogastric nerve block alone.
In the operating theatre all patients were monitored continuously during the procedure for heart rate (three-lead ECG), non-invasive arterial pressure and oxygen saturation. All patients included in the clinical trial underwent subarachnoid block with Quincke-babcock needle 26G (hyperbaric Bupivacaine 0.5%, 15mg), by the in-charge Anaesthesiologist of the theatre. Spinal block was performed at either L2-L3 or L3-L4 space and the level of sensory and motor block were assessed with cold temperature perception and bromage scale, respectively. Intra-operative hypotension was treated with crystalloids and Intravenous ephederine and bradycardia with intravenous atropine. After confirmation of subarachnoid block patients were given either dual-TAP block or ilioinguinal/iliohypogastric nerve blocks according to the group allocation.
All the nerve blocks were performed under aseptic precautions by the high-resolution ultrasound (LOGIC Q, GE) with 38mm, 6–13 MHZ linear array transducer and by the anaesthetist experienced in the loco-regional anaesthesia.
US-guided dual TAP block (D-TAP Group): Dual TAP is a combined technique of US-guided TAP block with ilio-inguinal and iliohypogastric nerve block. Patients were placed in supine position and with linear hi-frequency transducer, abdomen was scanned between costal margin and iliac crest to identify the three muscular layers of abdomen. The probe position was adjusted to visualise three muscular layers of abdominal wall, the external oblique (most superficial), the internal oblique and transverses abdominis muscles and the peritoneal cavity lies deep to the transversus abdominis muscle [Figure 1]. A short-bevelled needle of 100mm, 22G insulated block needle (B Braun Medical Inc. Stimuplex needle) was inserted in an antero-posterior direction with in-plane approach. After confirming the tip of the needle between aponeurosis of internal oblique and transversus abdominis muscles, Ropivacaine 0.5%, 20 ml was injected with intermittent aspiration and local anaesthetic spread was seen as hypoechoic shadow between the aponeurosis of the internal oblique and transversus abdominis muscles [Figure 2].
Figure 1.
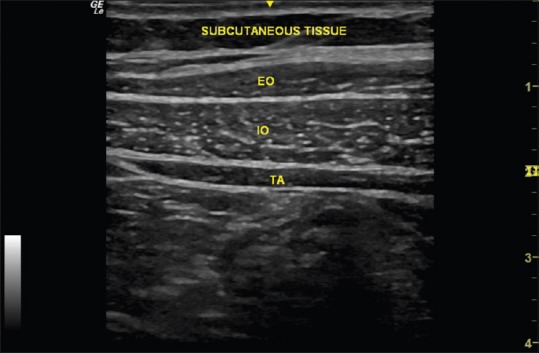
Ultrasound-Guided Transverses abdominis muscle Plane. Visualization of three muscular layers of abdominal wall. EO-External Oblique, IO-Internal Oblique, TA-Transverse Abdominis
Figure 2.
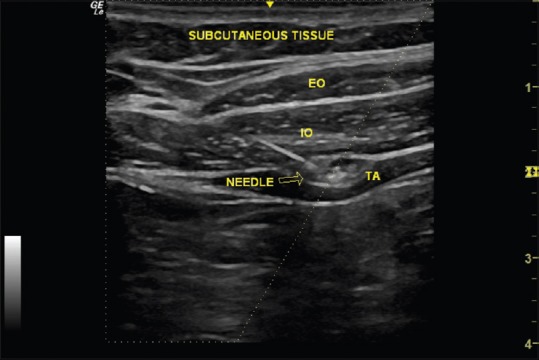
Ultrasound-Guided TAP Block with needle tip placement and drug spread. EO - External Oblique, IO-Internal Oblique, TA-Transverse Abdominis
Ilioinguinal/Iliohypogastric nerve block (IL/IH Group): In supine position, abdomen was scanned through Anterior superior iliac spine (ASIS)-umbilicus line. Ilioinguinal nerve can be visualised between the internal oblique and transverse or external oblique muscles and within 1 to 3 cm from the ASIS. The iliohypogastric nerve lies immediately adjacent [Figure 3]. After confirmation of the sufficient spread of the 10ml of 0.5% ropivacaine, surgery was initiated.
Figure 3.
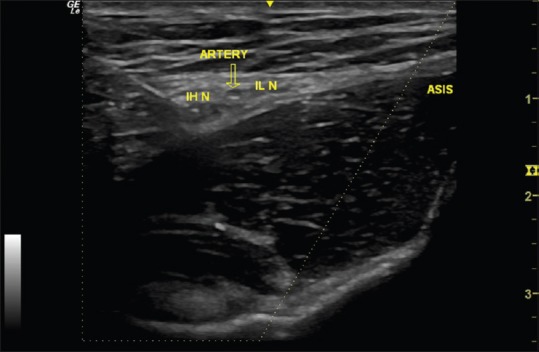
Ultrasound-Guided Ilioiguinal and Iliohypogastric nerve block with needle tip placement. IL/IH - Ilioiguinal/Ilihypogastric nerve, ASIS - Anterior superior iliac spine
A blinded observer unaware of the preoperative intervention assessed pain scores in PACU. Patients were monitored for pain intensity according to visual analogue scale (VAS, 0: no pain, 10: most severe pain), scores at rest (VAS-R) and (at 4, 12, 24 and 48h) and during movement (VAS-M) (at 24, 48 h, 3 and 6 months). Pain scores at 3 and 6 months were assessed by telephonic interview, using the DN4 questionnaire for neuropathic pain.
In the PACU all patients with VAS scores of ≥4 at rest were considered for rescue analgesia and was recorded. Patients were administered with intravenous fentanyl 0.5 μg/kg as rescue analgesia and, after 2 hours if the pain persists (VAS score of ≥4 at rest) even after giving fentanyl intravenous tramadol 50 mg added. Time interval until first analgesic dose and duration of hospital stay were recorded. Intraoperative and postoperative nausea and vomiting were recorded and treated with IV ondansetron and with oral tablets post discharge. Patients were observed for complications, such as urinary retention, hematoma and fever and were treated appropriately.
Patients were interviewed telephonically at 3 and 6 months for continued pain at rest and movement, at the site of hernia repair or in the testis or both. DN4 questionnaire was followed to establish neuropathic pain. A score 1 to each yes answer and score 0 for each no answer. It is likely to be neuropathic pain, if the score is ≥4.
Sample size estimation was done using Open Epi software version 2.3.1. At 95% confidence level and 90% power of the study according to study done by Okur et al.[8] Additional analgesia required in GT group (Group TAP Block) was 10% and GI group (Group IL/IH Block) is 30% of the study subjects. The sample size calculated is 84 in each group, that is 84 in GT group and 84 in GI group. Taking additional 20% for dropouts sample size calculated was 84 + 16 = 100 in each group. All values are expressed as mean ± standard deviation and nonparametric data was expressed as median and min-max values. Chi-square test for proportions in qualitative data. Student's unpaired t–test for quantitative data. P < 0.001 was considered statistically significant with a 95% confidence interval. Data were expressed as mean, median and standard deviation for all quantitative variables.
Rescue analgesia required between the groups was our secondary objective. Since the sample size required for answering the secondary objective was more than the primary objective. Hence we changed the sample size to 100 in each group.
RESULTS
Two hundred patients were enrolled for the study while three patients were excluded from the study due to loss of follow up at 6 months. Hence, a total of 197 patients were included in the analysis (98 patients in D-TAP group and 99 in IL/IH group). Patient characteristics, length of hospital stay, intra operative complications were similar in the groups. The mean time required for the first rescue analgesic dose was 5.59 ± 2.39 and 3.10 ± 1.18 hours with respect to dual TAP and IL/IH group, which was found to be significant (P < 0.001). A significant number of patients in the IL/IH group required rescue doses of fentanyl and tramadol (48.48% vs 12.24%) [Table 1].
Table 1.
Base line demographic characteristics
| D-TAP group | IL/IH group | P | |
|---|---|---|---|
| Age | 52.31±13.54 | 53.81±10.20 | 0.318 |
| BMI (kg/m2) | 26.08±2.47 | 25.30±3.06 | 0.561 |
| Gender | |||
| Male | 98 (98%) | 99 (99%) | 0.978 |
| Female | 02 | 01 | |
| ASA 1 | 72 (72%) | 78 (78%) | 0.539 |
| 2 | 28 (28%) | 22 (22%) | |
| Rescue Analgesic | 12/98 (12.24%) | 48/99 (48.48%) | <0.001 |
| Time to first rescue analgesic dose | 5.590±2.386 | 3.1053±1.1822 | <0.001 |
Values are expressed as mean±SD or number of patients (%). BMI – Body Mass Index, ASA-American Society of Anaesthesiology.
Patients VAS scores in both groups were assessed at rest (VAS-R). Patients receiving dual TAP block, experienced lower pain scores at all time intervals, while a statistically significant data obtained at 12 and 24 hours (P < 0.001) after surgery in D-TAP group compared to IL/IH group [Table 2].
Table 2.
Visual analogue scale scores of pain at rest (VAS-R)
| D-TAP group | IL/IH group | P | |
|---|---|---|---|
| 4 h | 0 (0-1) | 3 (0-4) | 0.008 |
| 12 h | 0 (0-3) | 3 (0-6) | <0.001 |
| 24 h | 0 (0-4) | 3 (0-5) | <0.001 |
| 48 h | 0 (0-1) | 2 (0-4) | 0.004 |
| 3 month | 0 (0-0) | 0 (0-1) | 0.179 |
| 6 month | 0 (0-0) | 0 (0-1) | 0.180 |
Values are expressed as median with inter quartile range (IQR). D-TAP – Dual Tranverses Abdominis Plane block group, IL/IH – Ilioinguinal/Iliohypogastric block group
While comparing VAS at movement between both the groups, pain scores at 24 and 48 hours were significantly lower (P < 0.001) in D-TAP group compared to IL/IH group. At 3months, there was no significant difference in the pain scores at rest. The pain scores at movement after 3months of inguinal hernia surgery, VAS-M scores ≥4 was 18.4% in D-TAP group and 21.89% in IL/IH group [Table 3].
Table 3.
Visual analogue scale scores of pain at movement (VAS-M)
| D-TAP group | IL/IH group | P | |
|---|---|---|---|
| 24 h | 1 (0-2) | 3 (0-5) | <0.001 |
| 48 h | 1 (0-2) | 3 (0-6) | <0.001 |
| 3 month | 0 (0-0) | 0 (0-1) | 0.168 |
| 6 month | 0 (0-0) | 0 (0-1) | 0.182 |
Values are expressed as median with inter quartile range (IQR). D-TAP – Dual Tranverses Abdominis Plane block group, IL/IH – Ilioinguinal/Iliohypogastric block group
There was no statistically significant difference in VAS scores, found between the groups after 6months of surgery, at rest and movement. DN4 questionnaire assessed at 3 months showed a median score of 0 (0-0) in the D-TAP group and 0 (0-1) in the IL/IH group (P < 0.23). There was no significant difference noted for DN4 questionnaire at 6 months [0 (0-1) vs 0 (0-1)] in the dual TAP and IL/IH group, respectively.
Nausea and vomiting were found to be major side effects in both groups with an incidence of 30%, while these side effects were comparable among the groups.
A higher number of patients required rescue analgesic doses in IL/IH group compared to dual TAP group with P value <0.001.
DISCUSSION
In the present study, we have demonstrated that the dual TAP block is superior to either IL/IH nerve block or TAP block in post-operative analgesia.
Hernia surgery generates parietal pain based on the distribution of Ilioinguinal and Iliohypogastric nerve. Neither infiltration nor US-guided IL/IH nerve block reduced the post-operative pain scores or prolonged duration of block.[9]
Various studies have showed TAP or IL/IH nerve blocks have reduced acute post-operative pain, additional analgesic requirements and may reduce the incidence of chronic pain after hernia repair.[4,8]
Few of the studies concluded that, US-guided IH nerve block provides better pain control and longer duration of action than US-guided TAP block in the post-operative period of unilateral open inguinal hernia repair, while others postulated TAP block is more effective in amelioration of acute postoperative pain compared to IL/IH block.[6,10] In contrast, studies have concluded US-guided IL/IH block provides superior analgesia compared to TAP block.[4,10]
In the present study a controlled randomised observer blinded comparison of dual TAP block with IL/IH nerve block was performed to overcome the less satisfactory pain scores with TAP block alone due to chances of sparing of L1 dermatome. To avoid this IL/IH nerve block which blocks L1 dermatome was added. Dual TAP block provides better pain relief, as there is broader anaesthetic distribution of block covering T7 to L1 along the abdominal wall.[11,12] The IL/IH anatomy varies, as both nerves enter the abdominal wall and divide at the level of the iliac crest. Blocking these nerves at the proximal level results in more effective block, as these nerve endings can be blocked with TAP block.[13]
Our trial is comparable with the findings of a study comparing US-guided TAP with IH block by Frassanito et al. found lower pain scores both at rest and on coughing, immediately after surgery, at 2 hours, at discharge, and at 24 hours after surgery compared with the IL/IH group, while in our study we had similar results, in addition lower pain scores were registered at 24 and 48 hours post-surgery in dual TAP block.[14]
Avleine et al. found median VAS pain scores at rest were lower in the US-guided TAP group at 4h, 12h and at 24 h compared to IHN block group, while pain after the first 24h were similar in both groups. These results of pain scores at rest are comparable with our study, while pain at movement after 24h and 48h were significant in dual TAP compared to IL/IH group.[10] The results of DN4 questionnaires and pain scores at 3 and 6 months after surgery were similar in both groups, which is similar to our findings.
Further in a study by, Okur et al. found no significant difference in immediate post-operative pain between the transversus abdominis plane block and iliohypogastric/ilioinguinal nerve block group compared to control group.[8] There was no significant difference in additional analgesic requirement between study groups, which is in contrast to findings of our study, where post-operative analgesic requirement was less in dual TAP group while findings of Aveline et al. matching our results showed less post-operative morphine requirement in TAP group.
There are several limitations to this study. Patients were not blinded to the anaesthetist performing the loco-regional anaesthesia, while they were randomised for block type. There was no control group in the study, as both blocks were proved superior in the previous studies against control group. As these blocks were performed after spinal anaesthesia the risk of nerve injury exists as paraesthesia cannot be elicitated.
To overcome sparing of dermatomes individual nerves were blocked at two sites. For this purpose, dual TAP block can be adapted for open hernia repair.
CONCLUSION
To conclude, US-guided dual TAP block provides more effective post-operative analgesia and reducing additional analgesic requirements.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgements
The authors would like to thank Dr Manjula Associate Professor Dept of Community Medicine S N Medical College Bagalkot.
REFERENCES
- 1.Kurzer M, Kark A, Hussain ST. Day case inguinal hernia repair in the elderly: A surgical priority. Hernia. 2009;13:131–6. doi: 10.1007/s10029-008-0452-3. [DOI] [PubMed] [Google Scholar]
- 2.Aasvang E, Kehlet H. Chronic postoperative pain: The case of inguinal herniorrhaphy. Br J Anaesth. 2005;95:69–76. doi: 10.1093/bja/aei019. [DOI] [PubMed] [Google Scholar]
- 3.Dueholm S, Forrest M, Hjortsø E, Lemvigh E. Pain relief following herniotomy: A double-blind randomized comparison between naproxen and placebo. Acta Anaesthesiol Scand. 1989;33:391–4. doi: 10.1111/j.1399-6576.1989.tb02930.x. [DOI] [PubMed] [Google Scholar]
- 4.Kamal K, Jain P, Bansal T, Ahlawat G. A comparative study to evaluate ultrasound-guided transversus abdominis plane block versus ilioinguinal iliohypogastric nerve block for post operative analgesia in adult patients undergoing inguinal hernia repair. Indian J Anaesth. 2018;62:292–7. doi: 10.4103/ija.IJA_548_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gofeld M, Christakis M. Sonographically guided ilioinguinal nerve block. J Ultrasound Med. 2006;25:1571–5. doi: 10.7863/jum.2006.25.12.1571. [DOI] [PubMed] [Google Scholar]
- 6.Charlton S, Cyna AM, Middleton P, Griffiths JD. Perioperative transversus abdominis plane (TAP) blocks for analgesia after abdominal surgery. Cochrane Database Syst Rev. 2010:CD007705. doi: 10.1002/14651858.CD007705.pub2. doi: 10.1002/14651858.CD007705.pub2. [DOI] [PubMed] [Google Scholar]
- 7.Tran TM, Ivanusic JJ, Hebbard P, Barrington MJ. Determination of spread of injectate after ultrasound-guided transversus abdominis plane block: A cadaveric study. Br J Anaesth. 2009;102:123–7. doi: 10.1093/bja/aen344. [DOI] [PubMed] [Google Scholar]
- 8.Okur O, Tekgul ZT, Erkan N. Comparison of efficacy of transversus abdominis plane block and iliohypogastric/ilioinguinal nerve block for postoperative pain management in patients undergoing inguinal herniorrhaphy with spinal anesthesia: A prospective randomized controlled open-label study. J Anesth. 2017;31:78–85. doi: 10.1007/s00540-017-2378-3. [DOI] [PubMed] [Google Scholar]
- 9.Petersen PL, Mathiesen O, Stjernholm P, Kristiansen VB, Torup H, Hansen EG, et al. The effect of transversus abdominis plane block or local anaesthetic infiltration in inguinalhernia repair: A randomised clinical trial. Eur J Anaesthesiol. 2013;30:415–21. doi: 10.1097/EJA.0b013e32835fc86f. [DOI] [PubMed] [Google Scholar]
- 10.Aveline C, Le Hetet H, Le Roux A, Vautier P, Cognet F, Vinet E, et al. Comparison between ultrasound guided transversus abdominis plane and conventional ilioinguinal/iliohypogastricnerve blocks for day-case open inguinal hernia repair. Br J Anaesth. 2011;106:380–6. doi: 10.1093/bja/aeq363. [DOI] [PubMed] [Google Scholar]
- 11.Stav A, Reytman L, Stav MY, Troitsa A, Kirshon M, Alfici R, et al. Transversus abdominis plane versus ilioinguinal and iliohypogastricnerve blocks for analgesia following open inguinal herniorrhaphy. Rambam Maimonides Med J. 2016;7 doi: 10.5041/RMMJ.10248. doi: 10.5041/RMMJ.10248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tran TM, Ivanusic JJ, Hebbard P, Barrington MJ. Determination of spread of injectate after ultrasound-guided transversus abdominis plane block: A cadaveric study. Br J Anaesth. 2009;102:123–7. doi: 10.1093/bja/aen344. [DOI] [PubMed] [Google Scholar]
- 13.Sviggum HP, Niesen AD, Sites BD, Dilger JA. Trunk blocks 101: Transversus abdominis plane, ilioinguinal-iliohypogastric, and rectus sheath blocks. Int Anesthesiol Clin. 2012;50:74–92. doi: 10.1097/AIA.0b013e31823bc2eb. [DOI] [PubMed] [Google Scholar]
- 14.Frassanito L, Pitoni S, Gonnella G, Alfieri S, Del Vicario M, Catarci S, et al. Utility of ultrasound guided transversus abdominis plane block for day-case inguinal hernia repair. Korean J Anesthesiol. 2017;70:46–51. doi: 10.4097/kjae.2017.70.1.46. [DOI] [PMC free article] [PubMed] [Google Scholar]


