Abstract
The acoustic startle reflex is a sensitive index of “anxiety” and “fear.” Potentiation of startle by conditioned and unconditioned fear stimuli appears to be mediated by the amygdala. CholecystokininB (CCKB) agonists increase “anxiety” in laboratory animals and induce “panic” in humans. Here, we investigate the role CCKB receptor-mediated mechanisms in the amygdala in the potentiation of startle. First, intra-amygdala infusions of the CCKB receptor agonist pentagastrin (0, 0.01, 0.1, 1, and 10 nm) produced a dose-related potentiation of acoustic startle responses. At the highest dose, startle amplitudes were increased up to 90% above preinfusion baseline levels. Second, similar infusions of pentagastrin had no effect on locomotor activity over the same time course, showing that increases in startle responsivity after infusions of pentagastrin are not attributable to nonspecific changes in motor activity. Third, infusions of similar doses of pentagastrin into the striatum or nucleus accumbens did not potentiate startle responses. Fourth, pretreatment with the CCKB receptor antagonist L-365,260 (0.1 mg/kg, i.p.) attenuated the potentiation of startle produced by intra-amygdala infusions of pentagastrin. Finally, intra-amygdala infusion of the CCKB receptor-selective antagonist PD-135158 (10 μg) blocked the potentiation of startle produced by i.c.v. infusions of pentagastrin, suggesting that i.c.v. infusions of pentagastrin potentiate startle responses via activation of amygdala CCKB receptors. These results show that amygdala CCKB receptor-mediated mechanisms are involved in the potentiation of acoustic startle responses.
Keywords: startle; anxiety; fear; locomotor activity; i.c.v.; microinjection; pentagastrin; cholecystokinin; striatum; PD-135158; L-365,260
The acoustic startle reflex is a short-latency motor response to a loud and unexpected noise. The reflex involves the rapid and sequential activation of muscles along the length of the body. Experimental manipulations that increase “anxiety” or “fear” increase startle response amplitudes in rats (see, for example, Davis, 1992). For example, startle responses are increased when evoked in the presence of stimuli paired with footshocks (“fear-potentiated startle”) (Davis et al., 1993). In humans, stimuli that are associated with “fear” potentiate startle responses (Grillon et al., 1994). The anxiolytic diazepam blocks fear-potentiated startle in humans (Patrick et al., 1996), and typical (diazepam: Davis, 1979) and atypical (buspirone: Kehne et al., 1988) anxiolytic drugs block fear-potentiated startle in rats.
Previous work has shown that CCK potentiates startle reflexes (see, for example, Fendt et al., 1995; Frankland et al., 1996). CCK is a peptide that is found in the gastrointestinal tract and throughout the brain (Vanderhaeghen et al., 1975; Saito et al., 1980; Gaudreau et al., 1983; Moran et al., 1986). The action of CCK is mediated by two receptor subtypes, A and B (Innis and Snyder, 1980).
Systemic administration of the CCKB receptor agonist pentagastrin increases startle amplitudes (Zhou et al., 1996). Conversely, systemic administration of the CCKB receptor antagonist L-365,260 attenuates fear-potentiated startle in rats (Josselyn et al., 1995a). These results are consistent with the anxiogenic and anxiolytic effects of systemically administered CCKB agonists and antagonists, respectively, in a range of behavioral paradigms including the elevated plus maze, light–dark box, punished responding, and social interaction (see, for example, Hughes et al., 1990; Harro and Vasar, 1991; Rataud et al., 1991; Singh et al., 1991; Männistö et al., 1994; Rex et al., 1994). These studies suggest that CCKB receptors mediate a constellation of behaviors associated with “anxiety” (see, for example, Harro et al., 1993).
Intracerebroventricular (i.c.v.) infusion of the CCKBreceptor agonist pentagastrin potentiates startle (Frankland et al., 1996). The question raised is which central CCKB receptors mediate these effects. The amygdala plays a critical role in mediating the behavioral and autonomic responses to fear and anxiety and, in particular, the potentiation of startle by “fear”- or “anxiety”-evoking stimuli (see, for example, Davis, 1992). Furthermore, CCK-containing neurons are distributed throughout the amygdaloid complex and, in particular, are concentrated in the lateral, basolateral, and cortical nuclei of the amygdala (Larssen and Rehfeld, 1979; McDonald, 1985; Vanderhaeghen, 1985; Ingram et al., 1989;Schiffmann and Vanderhaeghen, 1991; Pu et al., 1994).
The present series of studies tests the proposal that activation of amygdala CCKB receptors is important in the potentiation of startle responses. We show that infusions of pentagastrin into the amygdala, but not the striatum or nucleus accumbens, potentiate startle responses and that these increases in startle amplitude are not attributable to changes in motor activity. In addition, we show that potentiation of startle after intra-amygdala infusions of pentagastrin is attenuated by systemic pretreatment with the CCKBantagonist L-365,260. Finally, we show that intra-amygdala infusions of the CCKB antagonist PD-135158 block the potentiation induced by i.c.v. infusions of pentagastrin.
The results reported here were presented previously at the Society for Neuroscience meeting, 1995, San Diego (Josselyn et al., 1995b).
MATERIALS AND METHODS
Animals
Experimentally naive Wistar rats (Charles River, Montréal, Canada) weighing 275–300 gm at the time of surgery were used in these experiments. Rats were housed individually in a 12 hr light/dark cycle (lights off at 9:00 A.M.) with food and water freely available. All testing was carried out between 9:00 A.M. and 4:00 P.M.
Startle apparatus
Amplitudes of startle reactions were determined using a stabilimeter that was housed in a sound-attenuated chamber (46 × 4l × 4l cm interior) (Cassella and Davis, 1986). The stabilimeter consisted of a Plexiglas cage with wire mesh walls on the long side, compressed between four springs on the top and bottom within a heavy steel frame. The cage measured 8 × 8 × l5 cm, allowing the rat to orient in only one of two directions at any given time. Movements of the rat were recorded by an accelerometer (Endevco 2217E) embedded in a rubber bung and placed between the bottom of the cage and the base of the heavy steel frame. The output of the accelerometer was filtered at 2 Hz, amplified 10 times, and integrated by an Endevco Signal Conditioner (model 2775A), then displayed on a storage oscilloscope (Hitachi VC-6025A).
Acoustic stimuli were produced by a Pacer 8 Ω speaker placed within the sound-insulated chamber at a distance of 10 cm from the long side of the cage. Acoustic stimuli were 4 msec, 119 dB noise bursts (measured by a Bruel and Kjaer modular Precision Sound Level Meter, model 2231). Background white noise levels were maintained at 75 dB throughout testing.
Locomotor apparatus
Locomotor boxes (33 × 34 × 22.5 cm) consisted of two opposing sheet-metal side walls, one wire grid front wall, and a Plexiglas back wall. The floor was a wire grid, and the top was Plexiglas. Two infrared emitters, one located near the front and the other near the rear wall of the cage, were 11 cm apart and 2.5 cm above the grid floor. Two infrared sensors on the opposite side were connected to a computer that recorded the number of photobeam interruptions in 5 min intervals.
Surgery
For implantation of guide cannulae, rats were pretreated with atropine sulfate (0.4 mg/kg, i.p.), anesthetized with sodium pentobarbital (60 mg/kg, i.p.), and placed in a standard stereotaxic instrument. For Experiments 1, 2, and 4, cannulae (23-gauge) were bilaterally aimed at a region including the basolateral, lateral, central, and medial amygdala nuclei (coordinates: AP −2.6 mm, ML ±4.0–5.0 mm, DV 8.0 mm; from Paxinos and Watson, 1986). For Experiment 3, cannulae were aimed at the striatum or nucleus accumbens (coordinates: AP +0.7 mm, ML ±1.0–2.0 mm, DV 4.0–8.0 mm). In Experiment 5, cannulae were bilaterally implanted in the amygdala and in a unilateral cerebral ventricle site (coordinates: AP −0.8 mm, ML +1.2 mm, DV 4.0 mm). Guide cannulae were secured in place with jeweler’s screws and dental cement.
Habituation and matching procedure
For startle testing (Experiments 1 and 3–5), 1 week after surgery each rat was exposed to habituation sessions over two consecutive days. In these sessions, rats were placed in the startle box and 5 min later presented with 60 startle stimuli at 30 sec intertrial intervals (ITIs). On the basis of their mean startle amplitudes in the second of these two sessions, rats were matched into groups with similar response levels. This matching ensures that any changes in startle amplitudes after drug treatments cannot be attributed to different basal levels of responding. Formal testing commenced 1–2 d after this habituation session.
Drugs
The CCKB receptor-selective agonist pentagastrin (0, 0.01, 0.1, 1.0, and 10.0 nm in 0.5 μl for infusions into tissue, or 100 nm in 5 μl for i.c.v. infusions; Sigma, St. Louis, MO) was dissolved in 50 mm sodium bicarbonate. The CCKB receptor-selective antagonist L-365,260 [(R)N- (2,3-dihydro -1-methyl-2-oxo-5-phenyl-1H-1,4-benzodiazepin-3-yl)-N′(3-methylphenyl)-urea; Merck Sharp and Dohme, Harlow, UK] was homogeneously suspended in saline containing Tween-80 (0.1%). A similar saline and Tween solution served as vehicle. Systemic injections were delivered in a volume of 1.0 ml/kg body weight (i.p.). The CCKB receptor-selective antagonist PD-135158 [0 or 10 μg in 0.5 μl; CAM 1028; 4-{2-[3-(1H-indol-3-yl)-2-methyl-1-oxo-2{1,7,7-trimethyl-bicyclo[2,2,1]hept-2-yl-4-oxo-[1S 1α,2β[S*(S*)]4α]}]}-butanoateN-methyl-d-glucamine; bicyclo system 1S-endo; Parke Davis Neuroscience Research Centre, Cambridge, UK] was dissolved in saline.
Drug infusions
Hamilton microsyringes (5 μl) mounted in an infusion pump were used to infuse the drugs. For infusions into tissue (Experiments 1–5), drugs were infused at a constant rate of 0.25 μl/min. The volume of these infusions was 0.5 μl. For i.c.v. infusions (Experiment 5), drugs were infused at a constant rate of 1.0 μl/min. The volume of these infusions was 5.0 μl. Injection cannulae (30-gauge; Plastic Products) were connected to the microsyringe by polyethylene tubing. After infusions, injection cannulae were left in place for an additional 60 sec to ensure diffusion of the drug.
Histology
At the completion of the testing, rats were anesthetized and perfused transcardially with saline (0.9%) and then formalin (4%). Brains were removed and stored in formalin with 25% sucrose for at least 24 hr. Brains were then blocked and frozen to −15°C, and 40 μm coronal sections were cut from tissue including the cerebral ventricle, amygdaloid complex, and striatum. Sections were mounted on gelatin-coated slides, stained for cresyl violet, and coverslipped. Cannula placement was verified under a light microscope.
Experimental procedures
Experiment 1: effect of intra-amygdala infusions of pentagastrin on startle
A total of 57 rats was used in this experiment. Each rat was placed in the stabilimeter and 5 min later was presented with 40 noise bursts (119 dB) at 30 sec ITIs. Rats were then removed and infused with pentagastrin [0 nm (n = 6), 0.01 nm (n = 8), 0.1 nm(n = 10), 1 nm (n = 8), or 10 nm (n = 7)]. (Subsequent histological analysis showed that in some rats one (n = 9) or both (n = 9) cannulae were located outside of the amygdala.) Immediately after infusions, rats were placed back in the stabilimeter and 5 min later were presented with 60 startle stimuli at 30 sec ITIs over a period of 30 min. To avoid potential tissue damage arising from multiple injections, a between-subjects design was used in which each rat received only a single infusion of pentagastrin or vehicle.
Experiment 2: effect of intra-amygdala infusions of pentagastrin on locomotion
To control for the possibility that increases in startle amplitudes result from decreases in motor activity (Wecker and Ison, 1986; Plappert et al., 1993), in Experiment 2 we tested whether similar intra-amygdala infusions of pentagastrin affect locomotor activity. A randomly selected subset (n = 24) of rats tested for startle in Experiment 1 was used in this experiment. Rats were divided randomly into five groups receiving intra-amygdala infusions of pentagastrin [0 nm (n = 6), 0.01 nm (n = 5), 0.1 nm(n = 4), 1 nm (n = 4), or 10 nm (n = 5)] as described above. Rats were then placed into the locomotor boxes, and their locomotor activity was monitored over 30 min. This test period matched the time course of postinfusion startle testing in Experiment 1.
Experiment 3: effect of intrastriatal and intra-accumbens infusions of pentagastrin on startle
In Experiment 3, the effects of infusions of pentagastrin into the striatum and the nucleus accumbens, two other regions that are rich in CCKB receptors (Emson et al., 1982), were assessed. The procedure used was identical to that used in Experiment 1. Rats were randomly divided into groups receiving either intrastriatal infusions of pentagastrin [0 nm (n = 3), 0.1 nm (n = 4), or 10 nm(n = 3)] or intra-accumbens infusions of pentagastrin [0 nm (n = 4), 0.1 nm(n = 4), or 10 nm (n = 5)].
Experiment 4: effect of systemically injected L-365,260 on potentiated startle after intra-amygdala infusions of pentagastrin
We have found previously that systemic administration of the CCKB antagonist L-365,260 attenuates fear-potentiated startle (Josselyn et al., 1995a). In Experiment 4, we tested whether similar systemic administration of L-365,260 also blocks potentiation of startle responses after intra-amygdala infusion of pentagastrin (Experiment 1). In our earlier work, the minimum effective dose of L-365,260 that blocked fear-potentiated startle was 0.1 mg/kg (Josselyn et al., 1995a). The largest increase in startle produced by intra-amygdala infusions of pentagastrin was produced by the 10 nm dose (Experiment 1). Therefore, the effects of systemic administration of L-365,260 (0 or 0.1 mg/kg) on the potentiation of startle produced by intra-amygdala infusions of pentagastrin (10 nm) were tested. Fourteen experimentally naive rats were used in this study. Before the commencement of formal testing, rats were exposed to a single habituation session in which they received 60 startle stimuli presentations at 30 sec ITIs. Two to three days after this habituation session, rats received an injection of either L-365,260 or its vehicle (i.p.) and were then placed in the stabilimeter. Five minutes later, 20 startle stimuli were presented at 30 sec ITIs. The rats were then removed and received bilateral infusions of pentagastrin into the amygdala (10 nm) as described above in Experiment 1. After drug infusion, rats were replaced in the startle testing apparatus and 5 min later presented with 80 startle stimuli at 30 sec ITIs over 40 min. Two days later, the experiment was repeated. Those rats that had originally received an injection of L-365,260 received an injection of vehicle, or vice versa.
Previously, it has been shown that systemic injections of the same dose of L-365,260 has no effect on baseline startle responding (Josselyn et al., 1995a). Therefore, a vehicle (intra-amygdala) versus L-365,260 (systemic) control group is not included here.
Experiment 5: effect of intra-amygdala infusion of PD-135158 on potentiated startle after i.c.v. infusions of pentagastrin
Previously, we have shown that i.c.v. infusions of pentagastrin (100 nm) potentiate startle (Frankland et al., 1996). Therefore, in this experiment we tested whether the potentiation of startle produced by i.c.v. infusions of pentagastrin is blocked by intra-amygdala infusions of the CCKB antagonist PD-135158. Before the commencement of formal testing, naive rats (n = 9) were exposed to a single habituation session in which they received 60 startle stimuli presentations at 30 sec ITIs. Two to three days after this habituation session, rats were placed in the startle stabilimeter and presented with 40 startle stimuli at 30 sec ITIs. The rats were then removed and, first, received bilateral intra-amygdala infusions of PD-135158 (0 or 10 μg; infused at a constant rate of 0.25 μl/min). Immediately after this, rats received unilateral i.c.v. infusions of pentagastrin (100 nm; 5 μl infused at a constant rate of 1.0 μl/min). Rats were then replaced in the startle testing apparatus and 5 min later presented with 80 startle stimuli at 30 sec ITIs over 40 min. Two days later, the experiment was repeated. Those rats that had initially received bilateral intra-amygdala microinjections of PD-135158 received an injection of vehicle, or vice versa.
In a pilot study, we found that intra-amygdala infusions of PD-135158 (0 or 10 μg) had no effect on baseline startle responses (F(1,6) = 1.28, p > 0.05; data not shown). Therefore, a vehicle (intra-amygdala) versus vehicle (i.c.v.) control group is not included here.
Data analysis
In each of the experiments, only rats with both cannulae located within the amygdala (Experiments 1, 2, 4, and 5) or striatum (Experiment 3) were included in subsequent statistical analysis. For amygdala infusions, rats were included if cannulae were located within the amygdaloid complex (including the central, basolateral, medial, or lateral nuclei). In some rats, both cannulae were located outside of this region. These rats were placed in a “miss” group and subsequently analyzed. Rats with only one cannula located in the amygdala (Experiments 1, 2, 4, and 5) or striatum (Experiment 3) were not subsequently analyzed.
For startle experiments (Experiments 1, 3, 4, and 5), raw postinfusion startle scores for each rat were converted to a proportion of preinfusion baseline score. For each rat, the raw postinfusion startle scores were divided by the mean of the last 10 preinfusion trials. The last 10 trials reflect stable preinfusion startle amplitudes, because startle amplitudes normally habituate to asymptotic levels after 10–15 min of testing (Plappert et al., 1993). Therefore, this proportion score reflects the effect of drug infusion on startle with scores > 1.0 reflecting potentiation of startle and scores < 1.0 reflecting suppression of startle.
To evaluate statistically the effect of drug infusions on startle, proportions of preinfusion baseline scores were compared across time using ANOVA. For Experiments 1 and 3, mixed ANOVAs were conducted with Drug as a between-subjects variable and Time as a within-subjects variable. For Experiments 4 and 5, repeated-measures ANOVAs were performed with Drug (L-365,260, Experiment 4; PD-135158, Experiment 5) and Time as within-factor variables. For the locomotion study (Experiment 2), a mixed ANOVA was performed with Drug as a between-factor variable and Time as a within-factor variable.
RESULTS
Experiment 1: effect of intra-amygdala infusion of pentagastrin on startle
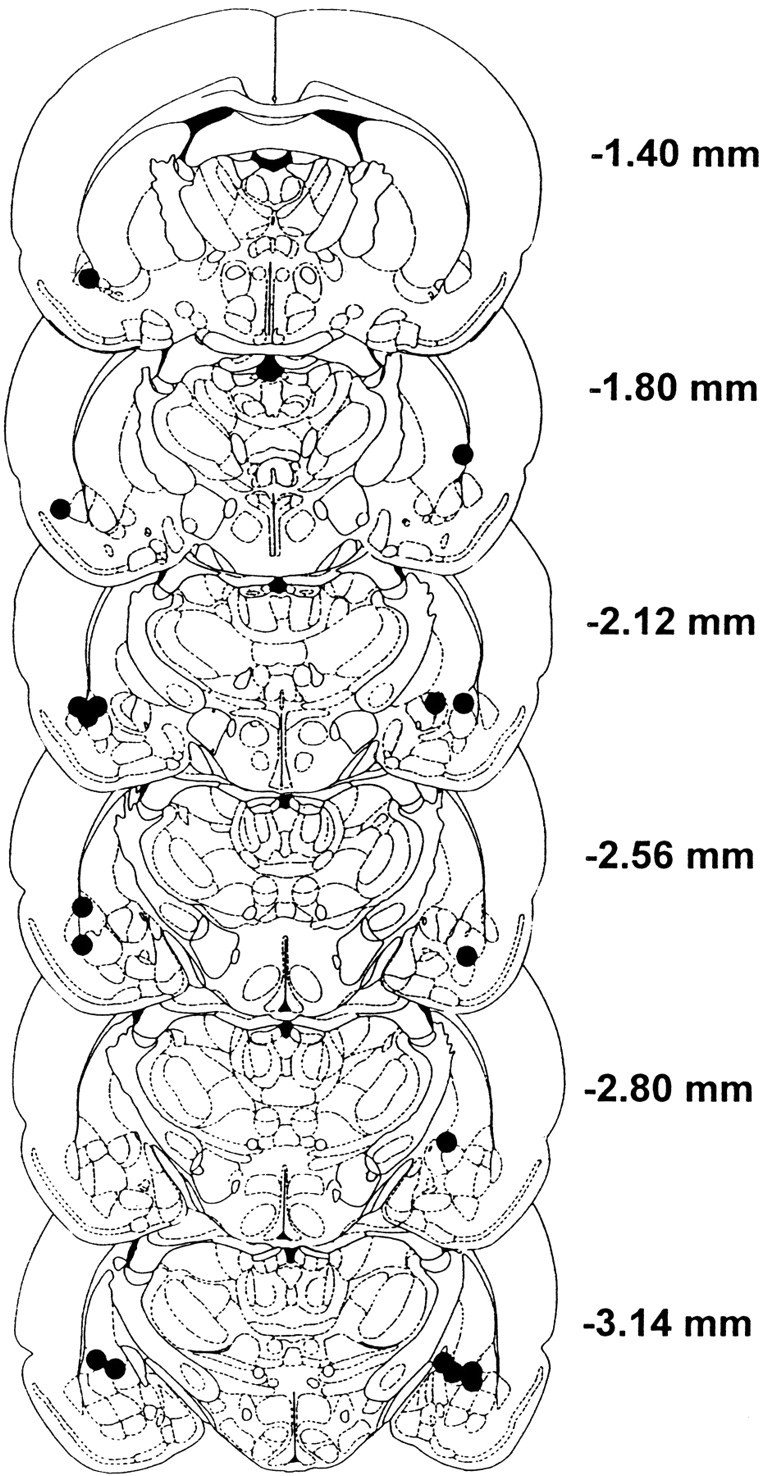
Histological analyses showed that 39 rats had both cannulae located within the amygdaloid complex (Fig. 1). The amygdaloid complex is defined here as including the basolateral, lateral, central, and medial nuclei of the amygdala (Paxinos and Watson, 1986).
Fig. 1.
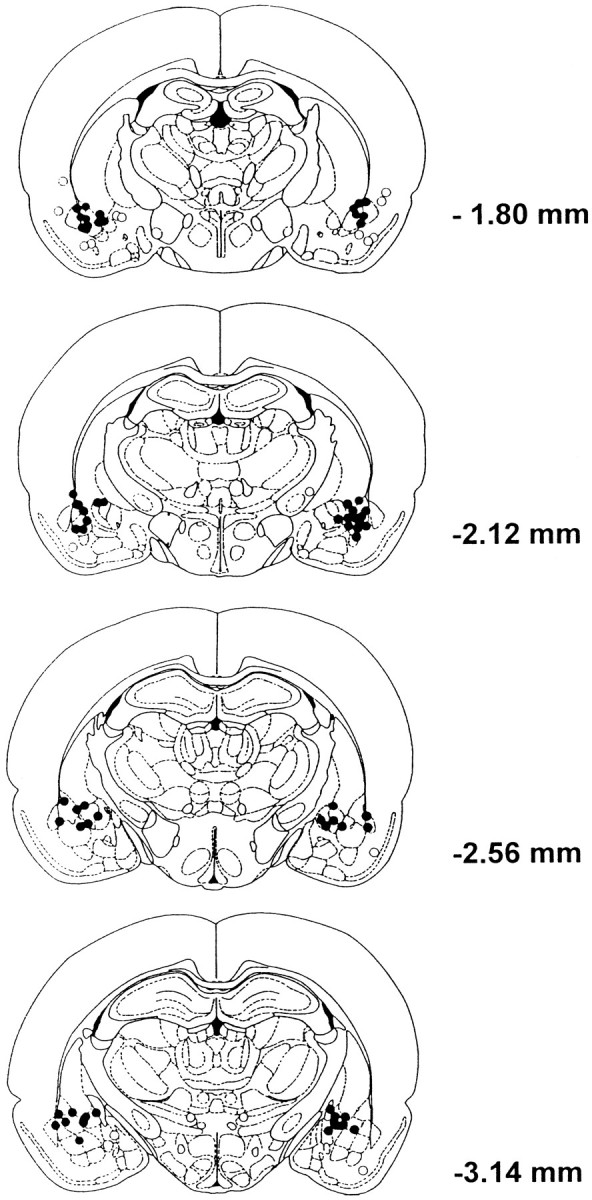
Location of injection sites in rats in Experiment 1 shown on coronal sections (Paxinos and Watson, 1986).Numbers to the right of each section represent the anterior–posterior coordinate with respect to bregma. Closed circles represent the locations of cannula tips within the amygdala. Open circles represent locations of cannula tips found outside of the amygdala. Data from rats with a single misplaced cannula were not included in statistical analyses. Rats with both cannulae located outside the amygdaloid complex were included in a “miss” group and subsequently analyzed.
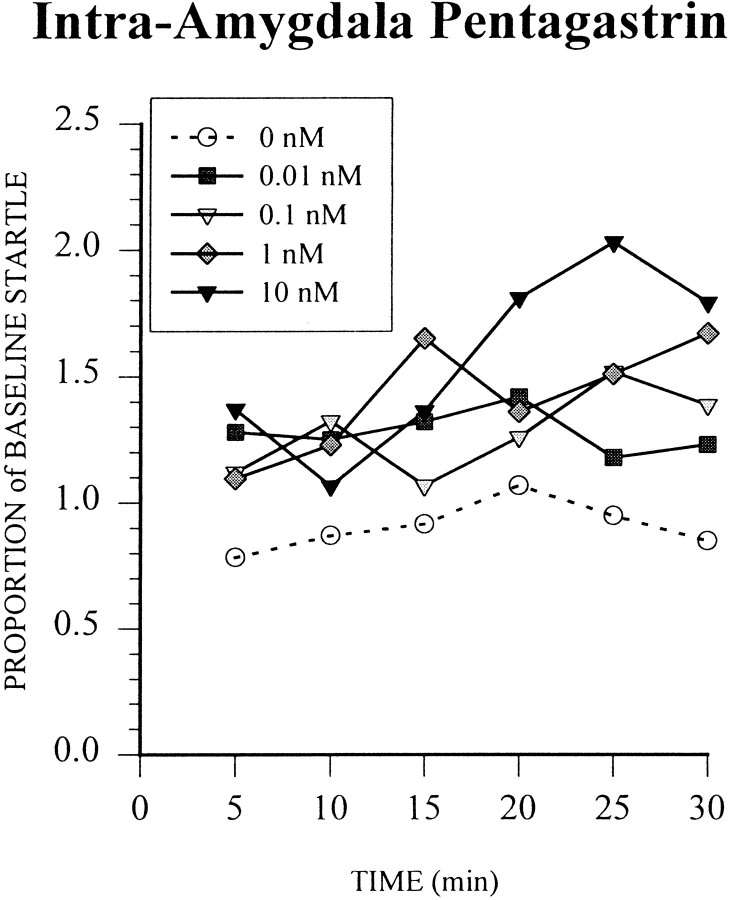
Intra-amygdala infusions of pentagastrin increased acoustic startle responses in a dose-related manner (Fig. 2). At the highest dose (10 nm), startle amplitudes were increased to levels 80–100% (over preinfusion baseline levels) 20–30 min postinfusion. Initial preinfusion baselines did not differ between groups (F(1,4) = 0.23, p > 0.05), so postinfusion changes in startle responsivity cannot be accounted for by differences in initial baselines. An ANOVA was carried out on the postinfusion startle data with Dose (5 levels: 0, 0.01, 0.1, 1, and 10 nm pentagastrin) as a between-factor variable and Time (6 levels: 5 min bins) as a within-factor variable. There was a significant Dose × Time interaction (F(20,170) = 1.67, p < 0.05), reflecting increased startle responsivity over time for rats infused with higher doses (1 or 10 nm) of pentagastrin. There was also a significant effect of Time (F(5,170) = 3.97, p < 0.01), reflecting increased startle responsivity over time. Post hoc analyses (Newman–Keuls;p < 0.05) revealed that startle amplitudes after infusions of 1 and 10 nm were significantly greater than those after infusions of vehicle at 30 min and at 25 and 30 min postinfusion, respectively.
Fig. 2.
The effect of intra-amygdala infusions of pentagastrin (0, 0.01, 0.1, 1, and 10 nm) on startle responding. Startle was tested for 30 min after drug infusion at 30 sec ITIs. Postinfusion startle scores are expressed as a proportion compared to preinfusion baseline (see Materials and Methods). Means ± SE for each dose, averaged across the 30 min test, are shown in Figure 3.
In 9 rats, both cannulae were located outside of the amygdaloid complex. To determine whether infusions of pentagastrin into areas outside of the amygdala affected startle amplitudes, data from these rats were combined into a “miss” group. There was no effect of dose on startle amplitudes in this “miss” group (F(3,5) = 3.06, p > 0.05), so the data from all doses were combined. An ANOVA on the mean startle amplitudes averaged over the 30 min test period for all groups, including the “miss” group, was performed. There was a significant effect of Group (F(5,42) = 4.38,p < 0.05). Post hoc analyses showed that startle amplitudes after intra-amygdala infusions of vehicle did not differ from those in the “miss” group (p = 0.28). However, startle amplitudes after intra-amygdala infusions of all doses of pentagastrin (0.01, 0.1, 1.0, or 10 nm) were significantly greater than those in the “miss” group (p < 0.05). These data show that the startle-potentiating effects of pentagastrin are restricted to intra-amygdala infusions (Fig. 3).
Fig. 3.
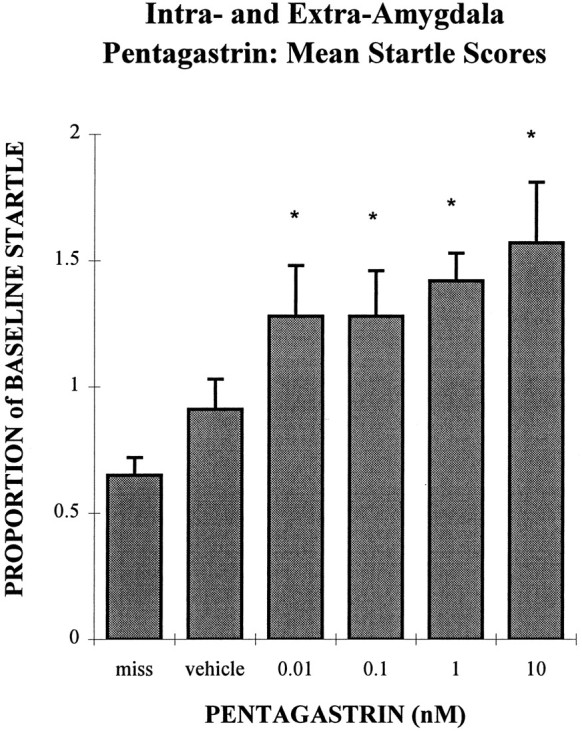
Bar chart comparing the mean postinfusion startle amplitudes in the “miss” group to those receiving intra-amygdala infusions of pentagastrin (0, 0.01, 0.1, 1, and 10 nm). Mean startle amplitudes (±SEM) are shown collapsed over the entire 30 min postinfusion test period. Startle amplitudes after infusion of vehicle into the amygdala are not different compared to those after infusions of any dose of pentagastrin outside of the amygdala (the “miss” group; p > 0.05). However, mean startle amplitudes after intra-amygdala infusion of all doses of pentagastrin are significantly greater than after similar infusions of pentagastrin into areas neighboring the amygdala (the “miss” group; *p < 0.05).
Experiment 2: effect of intra-amygdala infusions of pentagastrin on locomotion
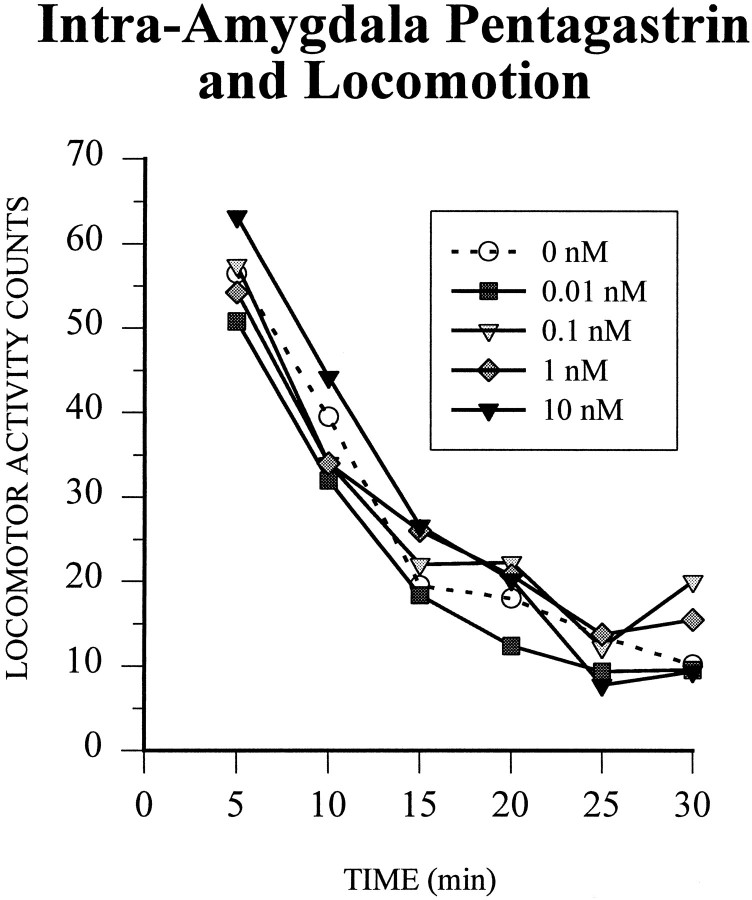
Intra-amygdala infusions of pentagastrin (0, 0.01, 0.1, 1.0, or 10 nm) had no effect on locomotor activity levels (Fig.4). Locomotor activity was measured over 30 min after infusion. This matches the time period over which startle was measured postinfusion in Experiment 1. Activity levels declined exponentially with time to approach asymptotic levels after ∼25 min. A mixed ANOVA was performed on the number of crossovers (consecutive breaks of front and rear infrared beams). There was a significant effect of Time (F(5,95) = 96.89, p < 0.001), reflecting a decrease in activity over time. However, there was no significant effect of pentagastrin on locomotor activity (F(4,19) = 0.58, p > 0.05).
Fig. 4.
The effect of intra-amygdala infusions of pentagastrin (0, 0.01, 0.1, 1, and 10 nm) on locomotor activity. Pentagastrin had no effect on locomotor activity over the 30 min test period.
Experiment 3: effects of intrastriatal and intra-accumbens infusions of pentagastrin on startle
Histological analyses showed that 10 rats had both cannulae located within the striatum (including both the dorsal and the ventral aspects of the striatum), whereas 13 rats had both cannulae located within the nucleus accumbens (Fig. 5). The effects of infusions of pentagastrin into these sites on startle amplitudes are shown in Figure 6. In these experiments, a similar range of doses (0, 0.1, and 10 nm) was tested over the same postinfusion time course (30 min) as in Experiment 1. An ANOVA was carried out on the postinfusion startle data with Dose (3 levels: 0, 0.1, or 10 nm pentagastrin) as a between-factor variable and Time (6 levels: 5 min bins) as a within-factor variable. For intrastriatal infusions, there was no significant effect of Dose (F(2,7) = 3.31, p = 0.10) and Time (F(5,35) = 1.05, p > 0.05) on startle responding. However, there was a clear trend for the highest dose of pentagastrin (10 nm) to decrease startle amplitudes. For intra-accumbens infusions, there was no significant effect of Dose (F(2,10) = 2.14,p > 0.05) or Time (F(5,50) = 1.19, p > 0.05) on startle responding.
Fig. 5.
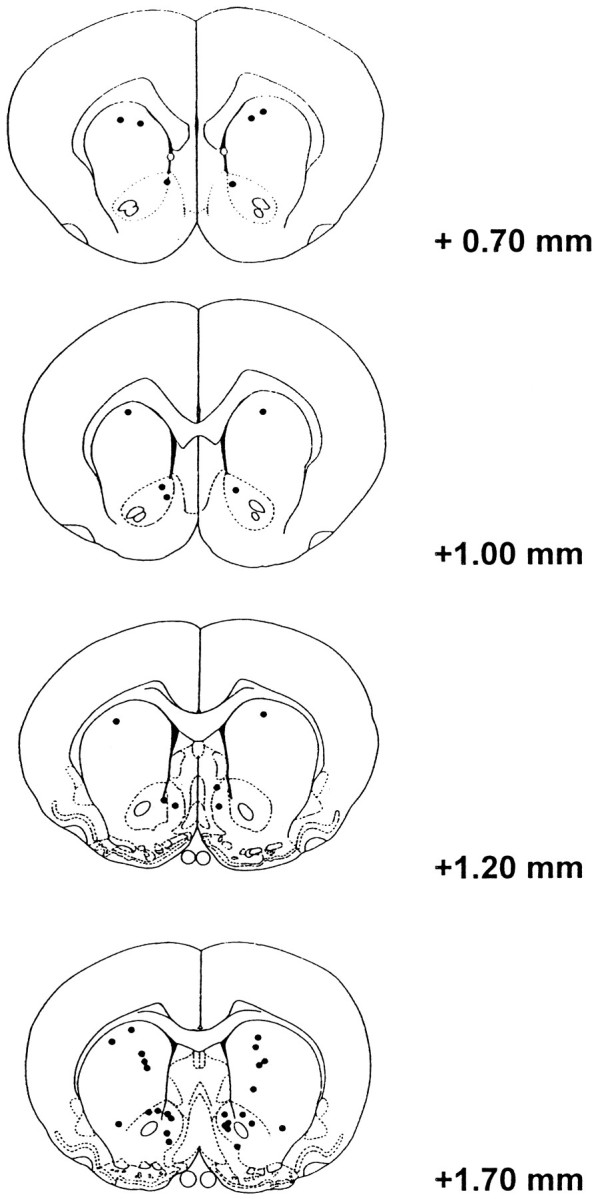
Location of injection sites in rats in Experiment 3 shown on coronal sections (Paxinos and Watson, 1986).Numbers to the right of each section represent the anterior–posterior coordinate with respect to bregma. Closed circles represent the locations of cannula tips within the striatum. Open circles represent locations of misplaced cannula tips.
Fig. 6.
Bar chart showing the effect of (A) intrastriatal and (B) intra-accumbens infusions of pentagastrin (0, 0.1, and 10 nm) on startle. Startle was tested for 30 min after drug infusion at 30 sec ITIs. Postinfusion startle scores (±SEM) are expressed as a proportion compared to preinfusion baselines (see Materials and Methods) and are averaged over the entire 30 min test period.
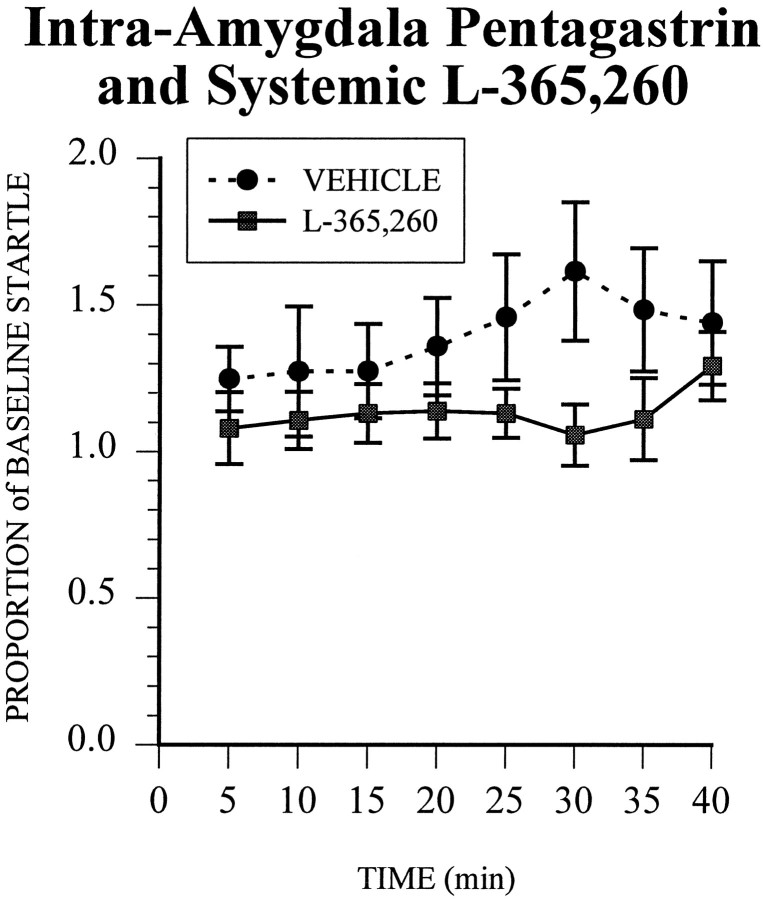
Experiment 4: effects of systemically injected L-365,260 on potentiated startle after intra-amygdala infusions of pentagastrin
Pretreatment with systemic injections of the CCKBreceptor antagonist L-365,260 attenuated the potentiation of startle induced by intra-amygdala infusions of pentagastrin (Fig.7). Histological analyses showed that cannulae were located within the amygdaloid complex (including the basolateral, lateral, central, and medial nuclei of the amygdala; data not shown) and were similarly distributed to those in Experiment 1. There were no differences in preinfusion startle amplitudes (F(1,13) = 0.68, p > 0.05), so differences between initial baselines cannot account for any subsequent differences in startle responsivity. In rats pretreated with systemic vehicle injections, intra-amygdala infusions of pentagastrin potentiated startle responses by 50–60% at 25–40 min postinfusion. This potentiation is consistent with, albeit slightly smaller in magnitude than, the potentiation after intra-amygdala pentagastrin infusions in Experiment 1. In rats pretreated with systemic injections of L-365,260, intra-amygdala infusions of pentagastrin only slightly increased startle responding over preinfusion baseline levels. Whereas startle responsivity was reduced by L-365,260 at all time intervals across the 60 min test period, the effect of drug (L-365,260 vs vehicle) only approached significance (F(1,13) = 3.70, p = 0.077). Planned comparisons performed on each interval revealed that startle amplitudes were significantly higher in rats receiving vehicle injections compared to L-365,260 injections 30 min postinfusion (p < 0.05).
Fig. 7.
The effect of systemic injections of the CCKB antagonist L-365,260 on potentiation of startle induced by intra-amygdala infusions of pentagastrin infusions. Startle responses (±SEM) are shown across time. All rats received intra-amygdala infusions of pentagastrin (10 nm) and systemic injections of L-365,260 (0.1 mg/kg) or its vehicle. Startle responses after intra-amygdala infusions of pentagastrin were attenuated by systemic injections of L-365,260.
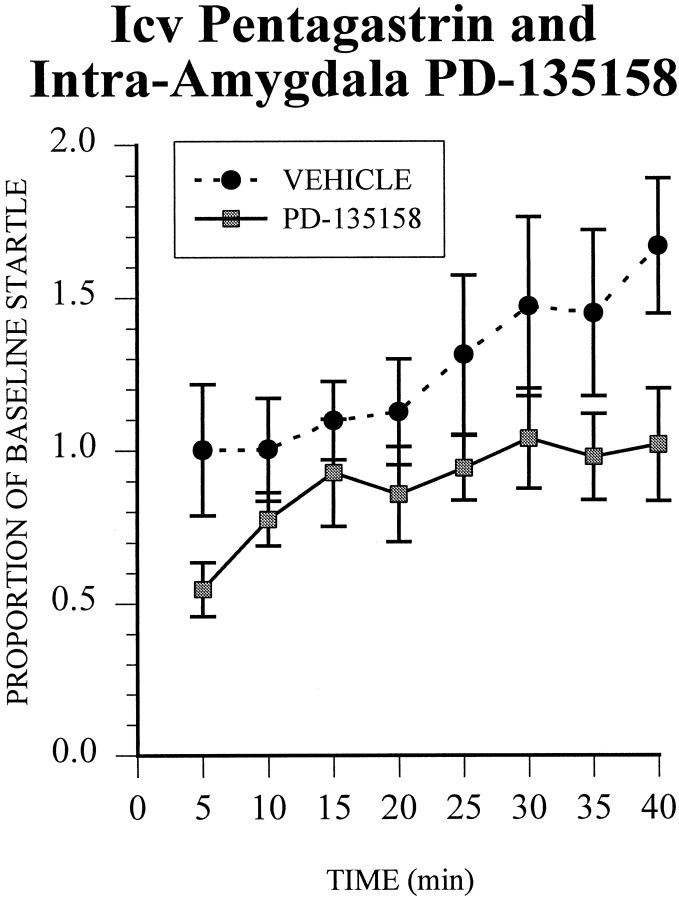
Experiment 5: effects of intra-amygdala infusions of PD-135158 on potentiated startle after i.c.v. infusions of pentagastrin
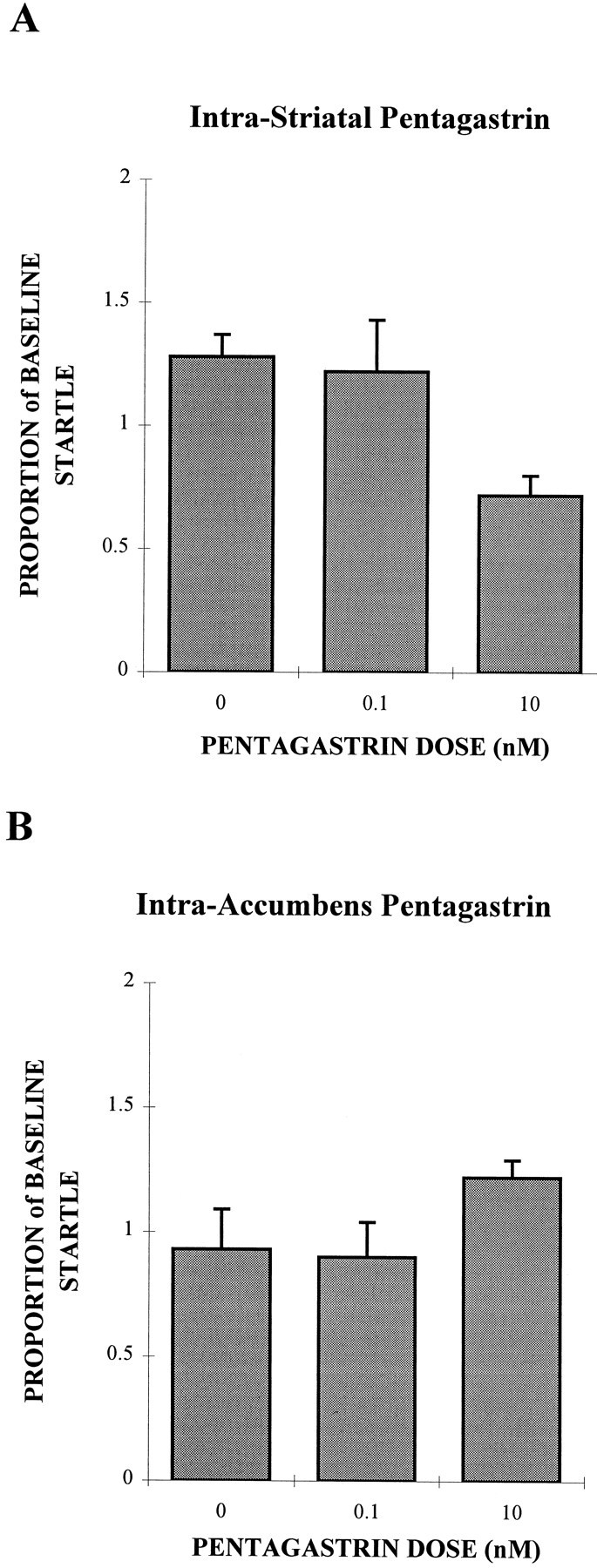
Cannulae tips were located in the amygdaloid complex, close to the basolateral amygdala (Fig. 8). Intra-amygdala infusions of the CCKB receptor-selective antagonist reduced the potentiation of startle induced by i.c.v. infusions of pentagastrin (Fig. 9). Preinfusion baselines were not different between groups (F(1,8) = 1.06, p> 0.05), so differences between initial baselines cannot account for any subsequent changes in startle responding. In the control condition, in which rats received i.c.v. pentagastrin infusions and bilateral vehicle infusions into the amygdala, startle amplitudes increased steadily over time to ∼90% above preinfusion baseline levels. In contrast, startle amplitudes were stable, or slightly increased, after intra-amygdala infusions of PD-135158 together with i.c.v. infusions of pentagastrin. An ANOVA with Drug (2 levels: 0 and 10 μg PD-135158) and Time (eight 5 min bins) as within-factor variables was performed. PD-135158 infusions into the basolateral amygdala reduced startle responses after i.c.v. pentagastrin infusions compared to controls that received intra-amygdala infusions of vehicle (F(1,8) = 5.12, p = 0.054).
Fig. 8.
Location of injection sites in rats in Experiment 5 shown on coronal sections (Paxinos and Watson, 1986).Numbers to the right of each section represent the anterior–posterior coordinate with respect to bregma. Closed circles represent the locations of cannula tips within the amygdala.
Fig. 9.
The effect of intra-amygdala infusions of the CCKB antagonist PD-135158 on potentiation of startle induced by i.c.v. pentagastrin infusions. Startle responses (±SEM) are shown across time. All rats received i.c.v. infusions of pentagastrin (100 nm) and bilateral intra-amygdala infusions of PD-135158 (10 μg) or its vehicle. Startle responses after i.c.v. pentagastrin infusions were reduced by intra-amygdala infusions of PD-135158, although this attenuation was not statistically significant (p = 0.054).
DISCUSSION
The above series of experiments provides evidence that the neuropeptide CCK potentiates startle responding via activation of amygdala CCKB receptors. In Experiment 1, intra-amygdala infusions of the CCKB receptor-selective agonist pentagastrin potentiated startle responses in a dose-related manner. In Experiment 2, similar intra-amygdala infusions of pentagastrin had no effect on locomotor activity over the same time period, suggesting that changes in startle responsivity observed in Experiment 1 are not attributable to changes in motor activity. In Experiment 3, infusions of similar doses of pentagastrin into the striatum or nucleus accumbens did not increase startle, suggesting that the potentiating effects of central infusions of pentagastrin on startle may be localized to amygdala sites. In Experiment 4, the potentiation of startle after intra-amygdala infusions of pentagastrin was attenuated by pretreatment with systemic injections of the CCKB receptor-selective antagonist L-365,260. This finding is consistent with the finding that systemic injections of the same dose of L-365,260 attenuate fear-potentiated startle (Josselyn et al., 1995a). In Experiment 5, increases in startle induced by i.c.v. pentagastrin infusions were attenuated by intra-amygdala infusions of the CCKBreceptor-selective antagonist PD-135158. Together, these results provide support for the idea that amygdala CCKB receptors facilitate the expression of behaviors associated with “anxiety.”
Previously, we found that i.c.v. infusions of pentagastrin potentiate startle responses by ∼70–100% (Frankland et al., 1996). The major aim of the present studies was to determine which brain region (or regions) mediates these effects. Here we show that activation of CCKB receptors in the amygdala potentiates startle responses. Startle responses after infusion of the highest dose (10 nm in 0.5 μl) of pentagastrin increased startle amplitudes by up to 100% over baseline preinfusion levels. This dose is 100-fold lower than the dose of pentagastrin required to potentiate startle responses when infused i.c.v. (100 nm in 5 μl;Frankland et al., 1996). Because decreases in motor activity are associated with increases in startle amplitudes (Wecker and Ison, 1986;Plappert et al., 1993), it is necessary to test whether drug infusions have nonspecific effects on locomotor activity in experiments such as these. However, we found that similar doses of pentagastrin had no effect on locomotor activity over a similar time course.
Therefore, bilateral infusions of pentagastrin into various subdivisions of the amygdala (including the central nucleus, basolateral nucleus, and lateral nuclei) resulted in potentiation of startle responses. Consistent with this, CCKB receptors are found throughout the amygdala and, in particular, are highly concentrated in the lateral, basolateral, and cortical nuclei of the amygdala (Larssen and Rehfeld, 1979; McDonald, 1985; Vanderhaeghen, 1985; Ingram et al., 1989; Schiffmann and Vanderhaeghen, 1991; Pu et al., 1994). In contrast, when both injection cannulae were located dorsal, ventral, medial, or lateral to the amygdala, infusions of pentagastrin had no effect on startle responses. In these cases, postinfusion startle amplitudes were indistinguishable from those after intra-amygdala vehicle infusions. Therefore, these results show that infusions of pentagastrin into the amygdala, but not neighboring nuclei, potentiate startle responses and demonstrate a degree of anatomical specificity.
Infusions of similar doses of pentagastrin into the striatum or nucleus accumbens did not potentiate startle responses. Indeed, there was a strong trend for intrastriatal infusions of the highest dose of pentagastrin to attenuate startle. Together, these data suggest that CCKB receptors in the amygdala, but not in the striatum or nucleus accumbens, are important for the potentiation of startle, again suggesting some anatomical specificity for the potentiating effects of centrally administered pentagastrin on startle. This conclusion, however, does not rule out the possibility that CCKBreceptors in the striatum, or other regions, are important for the expression of behavioral changes (other than the potentiation of startle) that are associated with increases in “anxiety.”
Previously, we found that systemic administration of the CCKB antagonist L-365,260 attenuates fear-potentiated startle without affecting baseline startle responses (Josselyn et al., 1995a). Similarly, systemic administration of the CCKBantagonist LY288513 attenuates potentiated startle induced by diazepam withdrawal (Rasmussen et al., 1993). Here we show that pretreatment with L-365,260 weakly attenuates potentiation of startle induced by intra-amygdala infusions of pentagastrin. Therefore, systemic injections of CCKB antagonists block the potentiation of startle induced (1) pharmacologically by intra-amygdala administration of the CCKB agonist pentagastrin, (2) by “anxiety”-evoking stimuli such as cues previously paired with shock, and (3) by withdrawal from the anxiolytic diazepam. The present results suggest that systemic injections of L-365,260 result in a blockade of CCKB receptors in the amygdala. They further suggest that antagonism of amygdala CCKB receptor sites is at least one possible mechanism via which L-365,260 attenuates fear-potentiated startle (Josselyn et al., 1995a).
It is notable that systemically injected L-365,260 only weakly (and nonsignificantly) attenuated potentiation of startle induced by intra-amygdala infusions of pentagastrin in the present study. This is consistent with the partial blockade of fear-potentiated startle produced by systemically injected L-365,260 (Josselyn et al., 1995a). A likely reason for this is the poor aqueous solubility, absorption, and limited bioavailability of L-365,260 (Chen et al., 1992; Lin et al., 1996).
Fendt et al. (1995) reported that infusions of CCK-8S, the octapeptide form of CCK that selectively activates CCKA receptors, into the caudal pontine reticular formation (PnC) increase the number of acoustically activated spikes recorded from PnC single units. Because PnC giant neurons form an obligatory relay in the circuit-mediating acoustic startle responses (Davis et al., 1982; Koch et al., 1992; Lingenhöhl and Fraiuf, 1992, 1994; Frankland et al., 1995; Lee et al., 1996; Yeomans and Frankland, 1996), these data suggested that one locus of modulation of startle by CCK may be within the startle circuit. Largely consistent with this, Fendt et al. (1995)showed that infusions of CCK-8S into the PnC produced modest increases in startle (30–40%) at some doses (5 ng/μl) but not others (2.5 and 10 ng/μl). Therefore, CCK receptor activation may also modulate startle within the startle circuit at the level of the PnC.
In Experiment 5, we found that intra-amygdala infusions of the CCKB antagonist PD-135158 almost completely blocked the potentiation of startle induced by i.c.v. infusions of pentagastrin. Similar injections had no effect on baseline startle levels, however. Therefore, either systemic (Josselyn et al., 1995a) or intra-amygdala injections of CCKB antagonists block potentiation of startle but do not affect baseline startle responses. The present findings support the conclusion that antagonism of amygdala CCKB receptors results in a blockade of fear-potentiated startle. Therefore, although modulation of startle responses may be dependent on CCK receptor activation at the level of the PnC, the present data suggest that modulation of startle via amygdala CCKB receptors is also important. The potentiation of startle responses is then presumably mediated by direct (Hitchcock and Davis, 1991; Rosen et al., 1991) and indirect (Yeomans and Pollard, 1993; Fendt et al., 1994b, 1996; Krase et al., 1994; Kungel et al., 1994; Frankland and Yeomans, 1995) pathways from the amygdala to the brainstem startle circuit.
The finding that the potentiation of startle is mediated, at least in part, by CCKB receptors in the amygdala is consistent with a large body of data showing that the amygdala is critical for the expression of behavioral and autonomic responses to “fear”- and “anxiety”-evoking stimuli (Davis, 1992). For example, lesions of the amygdala block increases in freezing (LeDoux et al., 1988; Kim et al., 1993) and changes in heart rate and blood pressure (Kapp et al.,1979) that are elicited in the presence of a conditioned stimulus previously paired with shock.
These present results suggest that CCKB receptors may be one class of receptor in the amygdala that participate in the processing of “fear”- or “anxiety”-inducing stimuli. Because systemically and i.c.v. administered CCKB agonists produce a broad range of autonomic and behavioral changes associated with “anxiety” (Singh et al., 1991; Harro et al., 1993; Belcheva et al., 1994), it is possible that the activation of amygdala CCKBreceptors may result in the expression of a large number of behavioral and autonomic changes associated with “anxiety” or “fear.” Consistent with this proposal is the finding that endogenous CCK-4 levels are elevated in the amygdala in rats after exposure to a predator-scented cloth (Pavlasevic et al., 1993). Similarly, mRNA levels for CCK are elevated in the basolateral amygdala in rats after pretreatment with the anxiogenic drug FG7142 (Pratt and Brett, 1995). Furthermore, in humans intravenous administration of the same doses of CCK-4 that evoke panic-like attacks also increases cerebral blood flow in the amygdala (Benkelfat et al., 1995).
Potentiation of startle is not exclusively dependent on CCKB receptor activation, however. For example, startle amplitudes are increased after intra-amygdala infusions of the glutamate agonist trans-ACPD (Koch, 1993) or the α2-adrenergic antagonist yohimbine (Fendt et al., 1994a). In addition, infusions of corticotropin-releasing hormone into the bed nucleus of the stria terminalis (Lee and Davis, 1996), but not the amygdala (Liang et al., 1992), potentiate startle responses. Therefore, different neurotransmitter systems and anatomical substrates may contribute to the potentiation of startle. It is possible that this complex anatomical and neurochemical coding reflects functionally distinct psychological processes underlying “anxiety” and “fear.”
Footnotes
This work was supported by an NSERCC grant to J.S.Y. and a Medical Research Council grant to F.J.V. PD-135158 was a generous gift from Parke Davis (Cambridge, UK). L-365,260 was a generous gift from Merck Sharp and Dohme Laboratories (Harlow, UK). We thank Veronica Franco, Marlene Taube, and Toni De Cristofaro for help on parts of these experiments.
Correspondence should be addressed to Paul W. Frankland, Beckman Neuroscience Center, Cold Spring Harbor Laboratory, Cold Spring Harbor, NY 11724.
REFERENCES
- 1.Belcheva I, Belcheva S, Petkov VV, Petkov VD. Asymmetry in behavioral responses to cholecystokinin microinjected into rat nucleus accumbens and amygdala. Neuropharmacology. 1994;33:995–1002. doi: 10.1016/0028-3908(94)90158-9. [DOI] [PubMed] [Google Scholar]
- 2.Benkelfat C, Bradwejn J, Meyer E, Ellenbogen M, Milot S, Gjedde A, Evans A. Functional neuroanatomy of CCK4-induced anxiety in normal healthy volunteers. Am J Psychiatry. 1995;152:1180–1184. doi: 10.1176/ajp.152.8.1180. [DOI] [PubMed] [Google Scholar]
- 3.Cassella JV, Davis M. The design and calibration of a startle measurement system. Physiol Behav. 1986;36:377–383. doi: 10.1016/0031-9384(86)90032-6. [DOI] [PubMed] [Google Scholar]
- 4.Chen I-W, Dorley JM, Ramjit HG, Pitzenberger SM, Lin JH. Physiological disposition and metabolism of L-365,260, a potent antagonist of brain cholecystokinin receptor, in laboratory animals. Drug Metab Dispos. 1992;20:390–395. [PubMed] [Google Scholar]
- 5.Davis M. Diazepam and flurazepam: Effects on conditioned fear as measured with potentiated startle paradigm. Psychopharmacology. 1979;62:1–7. doi: 10.1007/BF00426027. [DOI] [PubMed] [Google Scholar]
- 6.Davis M. The role of the amygdala in fear and anxiety. Annu Rev Neurosci. 1992;15:353–375. doi: 10.1146/annurev.ne.15.030192.002033. [DOI] [PubMed] [Google Scholar]
- 7.Davis M, Gendelman DS, Tischler M, Gendelman PM. A primary acoustic startle circuit: lesion and stimulation studies. J Neurosci. 1982;2:791–805. doi: 10.1523/JNEUROSCI.02-06-00791.1982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Davis M, Falls WA, Campeau S, Kim M. Fear-potentiated startle: a neural and pharmacological analysis. Behav Brain Res. 1993;58:175–198. doi: 10.1016/0166-4328(93)90102-v. [DOI] [PubMed] [Google Scholar]
- 9.Emson PC, Rehfeld JF, Rossor MN. Distribution of cholecystokinin-like peptides in the human-brain. J Neurochem. 1982;38:1177–1179. doi: 10.1111/j.1471-4159.1982.tb05369.x. [DOI] [PubMed] [Google Scholar]
- 10.Fendt M, Koch M, Schnitzler H-U. Amygdaloid noradrenaline is involved in the sensitization of the acoustic startle response in rats. Pharmacol Biochem Behav. 1994a;48:307–314. doi: 10.1016/0091-3057(94)90532-0. [DOI] [PubMed] [Google Scholar]
- 11.Fendt M, Koch M, Schnitzler H-U. Lesions of the central gray block the sensitization of the acoustic startle response in rats. Brain Res. 1994b;661:163–173. doi: 10.1016/0006-8993(94)91193-2. [DOI] [PubMed] [Google Scholar]
- 12.Fendt M, Koch M, Kungel M, Schnitzler H-U. Cholecystokinin enhances the acoustic startle response in rats. NeuroReport. 1995;6:2081–2084. doi: 10.1097/00001756-199510010-00030. [DOI] [PubMed] [Google Scholar]
- 13.Fendt M, Koch M, Schnitzler H-U. Lesions of the central gray block conditioned fear as measured with the potentiated startle paradigm. Behav Brain Res. 1996;74:127–134. doi: 10.1016/0166-4328(96)82984-6. [DOI] [PubMed] [Google Scholar]
- 14.Frankland PW, Yeomans JS. Fear-potentiated startle and electrically evoked startle mediated by synapses in the rostrolateral midbrain. Behav Neurosci. 1995;109:669–680. doi: 10.1037//0735-7044.109.4.669. [DOI] [PubMed] [Google Scholar]
- 15.Frankland PW, Scott BS, Yeomans JS. Axons and synapses mediating electrically evoked startle: collision tests and latency analysis. Brain Res. 1995;670:97–111. doi: 10.1016/0006-8993(94)01220-c. [DOI] [PubMed] [Google Scholar]
- 16.Frankland PW, Josselyn SA, Bradwejn J, Vaccarino FJ, Yeomans JS. Intracerebroventricular infusion of the CCKB receptor agonist, pentagastrin, potentiates acoustic startle. Brain Res. 1996;733:129–132. doi: 10.1016/0006-8993(96)00756-1. [DOI] [PubMed] [Google Scholar]
- 17.Gaudreau P, Quiron R, St Pierre S, Pert CB. Characterization and visualization of cholecystokinin receptors in rat brain using [3H]pentagastrin. Peptides. 1983;4:755–762. doi: 10.1016/0196-9781(83)90032-3. [DOI] [PubMed] [Google Scholar]
- 18.Grillon C, Ameli R, Goddard A, Woods SW, Davis M. Baseline and fear-potentiated startle in panic disorder patients. Biol Psychiatry. 1994;35:431–439. doi: 10.1016/0006-3223(94)90040-x. [DOI] [PubMed] [Google Scholar]
- 19.Harro J, Vasar E, Bradwejn J. ) CCK in animal and human research on anxiety. Trends Pharmacol Sci. 1993;14:244–249. doi: 10.1016/0165-6147(93)90020-k. [DOI] [PubMed] [Google Scholar]
- 20.Harro J, Vasar E. Cholecystokinin-induced anxiety. How is it reflected in studies on exploratory behavior? Neurosci Biobehav Rev. 1991;15:473–477. doi: 10.1016/s0149-7634(05)80134-4. [DOI] [PubMed] [Google Scholar]
- 21.Hitchcock J, Davis M. The efferent pathway of the amygdala involved in conditioned fear as measured with the fear-potentiated startle paradigm. Behav Neurosci. 1991;105:826–842. doi: 10.1037//0735-7044.105.6.826. [DOI] [PubMed] [Google Scholar]
- 22.Hughes J, Boden P, Costall B, Domeney A, Kelly E, Horwell DC, Hunter JC, Pinnock RD, Woodruff GN. Development of a class of selective cholecystokinin type-B receptor antagonists having potent anxiolytic activity. Proc Natl Acad Sci USA. 1990;87:6728–6732. doi: 10.1073/pnas.87.17.6728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ingram SM, Krause RG, II, Baldino F, Jr, Skeen LC, Lewis ME. Neuronal localization of cholecystokinin mRNA in the rat brain by using in situ hybridization histochemistry. J Comp Neurol. 1989;287:260–272. doi: 10.1002/cne.902870209. [DOI] [PubMed] [Google Scholar]
- 24.Innis RB, Snyder SN. Cholecystokinin receptor binding in brain and pancreas: regulation of pancreatic binding by cyclic and acyclic guanine nucleotides. Eur J Pharmacol. 1980;65:123–124. doi: 10.1016/0014-2999(80)90221-6. [DOI] [PubMed] [Google Scholar]
- 25.Josselyn SA, Frankland PW, Petrisano S, Bush DEA, Yeomans JS, Vaccarino FJ. The CCKB antagonist, L-365,260, attenuates fear-potentiated startle. Peptides. 1995a;7:1313–1315. doi: 10.1016/0196-9781(95)02013-m. [DOI] [PubMed] [Google Scholar]
- 26.Josselyn SA, Frankland PW, Yeomans JS, Vaccarino FJ. Intra-amygdala infusion of the CCKB agonist, pentagastrin, produces a facilitation of the acoustic startle reflex. Soc Neurosci Abstr. 1995b;21:1697. [Google Scholar]
- 27.Kapp BS, Frysinger RC, Gallagher M, Haselton JR. Amygdala central nucleus lesions: effects on heart rate conditioning in the rabbit. Physiol Behav. 1979;23:1109–1117. doi: 10.1016/0031-9384(79)90304-4. [DOI] [PubMed] [Google Scholar]
- 28.Kehne JH, Cassella JV, Davis M. Anxiolytic effects of buspirone and gepirone in the fear-potentiated startle paradigm. Psychopharmacology (Berl) 1988;94:8–13. doi: 10.1007/BF00735872. [DOI] [PubMed] [Google Scholar]
- 29.Kim JJ, Rison RA, Fanselow MS. Effects of amygdala, hippocampus, and periaqueductal gray lesions on short- and long-term contextual fear. Behav Neurosci. 1993;107:1093–1098. doi: 10.1037//0735-7044.107.6.1093. [DOI] [PubMed] [Google Scholar]
- 30.Koch M. Microinjections of the metabotropic glutamate receptor agonist, trans-(±)-1-amino-cyclopentane-1,3-dicarboxylate (trans-ACPD), into the amygdala increase the acoustic startle response of rats. Brain Res. 1993;629:176–179. doi: 10.1016/0006-8993(93)90500-m. [DOI] [PubMed] [Google Scholar]
- 31.Koch M, Lingenhöhl K, Pilz PKD. Loss of the acoustic startle response after neurotoxic lesions of the caudal pontine reticular formation: possible role of giant neurons. Neuroscience. 1992;49:617–625. doi: 10.1016/0306-4522(92)90231-p. [DOI] [PubMed] [Google Scholar]
- 32.Krase W, Koch M, Schnitzler H-U. Substance P is involved in the sensitization of the acoustic startle response by footshocks in rats. Behav Brain Res. 1994;63:81–88. doi: 10.1016/0166-4328(94)90053-1. [DOI] [PubMed] [Google Scholar]
- 33.Kungel M, Ebert U, Herbert H, Ostwald J. Substance P and other putative transmitters modulate the activity of reticular pontine neurons: an electrophysiological and immunohistochemical study. Brain Res. 1994;643:29–39. doi: 10.1016/0006-8993(94)90005-1. [DOI] [PubMed] [Google Scholar]
- 34.Larssen LI, Rehfeld JF. Localization of molecular and heterogeneity of cholecystokinin in the central and peripheral nervous system. Brain Res. 1979;165:201–218. doi: 10.1016/0006-8993(79)90554-7. [DOI] [PubMed] [Google Scholar]
- 35.LeDoux JE, Iwata J, Cicchetti P, Reis DJ. Different projections of the central amygdaloid nucleus mediate autonomic and behavioral correlates of conditioned fear. J Neurosci. 1988;8:2517–2529. doi: 10.1523/JNEUROSCI.08-07-02517.1988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lee Y, Davis M. The role of the bed nucleus of the stria terminalis in CRH-enhanced startle: an animal model of anxiety. Soc Neurosci Abstr. 1996;22:465. [Google Scholar]
- 37.Lee Y, López DE, Meloni EG, Davis M. A primary acoustic startle pathway: obligatory role of cochlear root neurons and the nucleus reticularis pontis caudalis. J Neurosci. 1996;16:3775–3789. doi: 10.1523/JNEUROSCI.16-11-03775.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Liang KC, Melia KR, Miserendino MJD, Falls WA, Campeau S, Davis M. Corticotropin-releasing factor: long-lasting facilitation of the acoustic startle reflex. J Neurosci. 1992;12:2303–2312. doi: 10.1523/JNEUROSCI.12-06-02303.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lin JH, Storey DE, Chen I-W, Xu X. Improved oral absorption of L-365,260, a poorly soluble drug. Biopharmacol Drug Dispos. 1996;17:1–15. doi: 10.1002/(SICI)1099-081X(199601)17:1<1::AID-BDD934>3.0.CO;2-G. [DOI] [PubMed] [Google Scholar]
- 40.Lingenhöhl K, Friauf E. Giant neurons in the caudal pontine reticular formation receive short latency acoustic input: an intracellular recording and HRP-study in the rat. J Comp Neurol. 1992;325:473–492. doi: 10.1002/cne.903250403. [DOI] [PubMed] [Google Scholar]
- 41.Lingenhöhl K, Friauf E. Giant neurons in the rat reticular formation: a sensorimotor interface in the elementary acoustic startle circuit? J Neurosci. 1994;14:1176–1194. doi: 10.1523/JNEUROSCI.14-03-01176.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Männistö PT, Lang A, Harro J, Peuranen E, Bradwejn J, Vasar E. Opposite effects mediated by CCKA and CCKB receptors in behavioral and hormonal studies in rats. Naunyn Schmiedebergs Arch Pharmacol. 1994;349:478–484. doi: 10.1007/BF00169136. [DOI] [PubMed] [Google Scholar]
- 43.McDonald AJ. Morphology of peptide-containing neurons in the rat basolateral amygdaloid nucleus. Brain Res. 1985;338:186–191. doi: 10.1016/0006-8993(85)90266-5. [DOI] [PubMed] [Google Scholar]
- 44.Moran TH, Robinson PH, Goldrich MS, McHugh PR. Two brain cholecystokinin receptors: implications for behavioral actions. Brain Res. 1986;362:175–179. doi: 10.1016/0006-8993(86)91413-7. [DOI] [PubMed] [Google Scholar]
- 45.Patrick CJ, Berthot BD, Moore JD. Diazepam blocks fear-potentiated startle in humans. J Abnorm Psychol. 1996;105:89–96. doi: 10.1037//0021-843x.105.1.89. [DOI] [PubMed] [Google Scholar]
- 46.Pavlasevic S, Bednar I, Qureshi GA, Soderste P. Brain cholecystokinin tetrapeptide levels are increased in a rat model of anxiety. NeuroReport. 1993;5:225–228. doi: 10.1097/00001756-199312000-00009. [DOI] [PubMed] [Google Scholar]
- 47.Paxinos G, Watson C. The rat brain in stereotaxic coordinates, 2nd Ed. Academic; San Diego: 1986. [Google Scholar]
- 48.Plappert CF, Pilz PK, Schnitzler H-U. Acoustic startle response and habituation in freezing and nonfreezing rats. Behav Neurosci. 1993;107:981–987. doi: 10.1037//0735-7044.107.6.981. [DOI] [PubMed] [Google Scholar]
- 49.Pu S, Zhuang H, Lu Z, Wu X, Han J. Cholecystokinin gene expression in rat amygdaloid neurons: normal distribution and effect of morphine tolerance. Brain Res Mol Brain Res. 1994;21:183–189. doi: 10.1016/0169-328x(94)90249-6. [DOI] [PubMed] [Google Scholar]
- 50.Pratt JA, Brett RR. The benzodiazepine receptor inverse agonist FG7142 induces cholecystokinin gene expression in the rat brain. Neurosci Lett. 1995;184:197–200. doi: 10.1016/0304-3940(94)11205-w. [DOI] [PubMed] [Google Scholar]
- 51.Rasmussen K, Helton DR, Berger JE, Scearce E. The CCKB antagonist LY288513 blocks effects of diazepam withdrawal on auditory startle. NeuroReport. 1993;5:154–156. doi: 10.1097/00001756-199311180-00015. [DOI] [PubMed] [Google Scholar]
- 52.Rataud J, Darche F, Piot O, Stutzmann J-M, Böhme GA, Blanchard J-C. “Anxiolytic” effect of CCK-antagonists on plus maze behavior in mice. Brain Res. 1991;548:315–317. doi: 10.1016/0006-8993(91)91139-r. [DOI] [PubMed] [Google Scholar]
- 53.Rex A, Barth T, Voigt J-P, Domeney AM, Fink H. Effects of cholecystokinin tetrapeptide and sulfated cholecystokinin octapeptide in rat models of anxiety. Neurosci Lett. 1994;172:139–142. doi: 10.1016/0304-3940(94)90681-5. [DOI] [PubMed] [Google Scholar]
- 54.Rosen JB, Hitchcock JM, Sananes CB, Miserendino MJD, Davis M. A direct projection from the central nucleus of the amygdala to the acoustic startle pathway: anterograde and retrograde tracing studies. Behav Neurosci. 1991;105:817–825. doi: 10.1037/0735-7044.105.6.817. [DOI] [PubMed] [Google Scholar]
- 55.Saito A, Goldfine ID, Williams JA. Characterization of receptors for cholecystokinin and related peptides in mouse cerebral cortex. J Neurochem. 1980;37:433–490. doi: 10.1111/j.1471-4159.1981.tb00481.x. [DOI] [PubMed] [Google Scholar]
- 56.Schiffmann SN, Vanderhaeghen JJ. Distribution of cells containing mRNA encoding cholecystokinin in the rat central nervous system. J Comp Neurol. 1991;304:219–233. doi: 10.1002/cne.903040206. [DOI] [PubMed] [Google Scholar]
- 57.Singh L, Field MJ, Hughes J, Vass CA, Woodruff GN. The behavioral properties of CI-988, a selective cholecystokinin-B receptor antagonist. Br J Pharmacol. 1991;104:239–245. doi: 10.1111/j.1476-5381.1991.tb12413.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Vanderhaeghen JJ. Neuronal cholecystokinin. In: Björklund A, Hökfelt T, editors. Handbook of chemical neuroanatomy, Vol 4, GABA and neuropeptides in the CNS. Elsevier; Amsterdam: 1985. pp. 406–435. [Google Scholar]
- 59.Vanderhaeghen JJ, Signeau JC, Gepts W. New peptide in the vertebrate CNS reacting with anti-gastrin antibodies. Nature. 1975;257:604–605. doi: 10.1038/257604a0. [DOI] [PubMed] [Google Scholar]
- 60.Wecker JR, Ison JR. Effects of motor activity on the elicitation and modification of the startle reflex in rats. Anim Learn Behav. 1986;14:287–292. [Google Scholar]
- 61.Yeomans JS, Frankland PW. The acoustic startle reflex: neurons and connections. Brain Res Rev. 1996;21:301–314. doi: 10.1016/0165-0173(96)00004-5. [DOI] [PubMed] [Google Scholar]
- 62.Yeomans JS, Pollard BA. Amygdala efferents mediating electrically evoked startle-like responses and fear potentiation of acoustic startle. Behav Neurosci. 1993;107:596–610. doi: 10.1037//0735-7044.107.4.596. [DOI] [PubMed] [Google Scholar]
- 63.Zhou Y, Arifuzzaman AI, Josselyn SA, Frankland PW, Bradwejn J, Vaccarino FJ. Effects of intraperitoneal administration of CCK agonist and antagonist on acoustical startle response, an anxiety model, in rats. Soc Neurosci Abstr. 1996;22:1153. [Google Scholar]