Abstract
STUDY DESIGN:
Laboratory study, case-control design.
OBJECTIVES:
Investigate if individuals with femoroacetabular impingement (FAI) syndrome have different hip and pelvic motion during gait, at their preferred speed and a prescribed speed, compared to individuals of the same sex without pain.
BACKGROUND:
FAI syndrome may affect gait kinematics differently between males and females.
METHODS:
Eleven males and 10 females with FAI syndrome and 19 males and 22 females without hip pain participated. Groups were not different in age, body mass index, or activity score. Kinematic data for all participants were collected while walking at a preferred speed and at 1.25 m/s. For each sex and walking speed, linear regression analyses examined the effect of group and the interaction of group-by-limb.
RESULTS:
At both speeds, males with FAI syndrome walked with more than 6° less peak hip extension (P ≤ .018), 5° greater anterior pelvic tilt (P ≤ .020), and 5° less posterior pelvic tilt (P ≤ .018) compared to males without hip pain. Females with FAI syndrome walked with 2° less hip extension (P ≤ .012) and at least 3° more hip adduction (P < .001) in the more painful hip than in the less painful hip at both speeds.
CONCLUSION:
Males and females with FAI syndrome have different gait alterations when compared to a same sex comparison group. In males, differences were between groups. In females with FAI syndrome, differences were between the more painful and less painful limb.
Keywords: FAIS, biomechanics, hip pain, gait, movement system
INTRODUCTION
Femoroacetabular impingement (FAI) syndrome is an increasingly recognized clinical diagnosis for hip pain in young and middle-aged adults. FAI syndrome classifies individuals who present with hip pain in combination with structural hip morphology thought to contribute to premature contact between the proximal femur and acetabulum.17 While there is agreement that movement contributes to FAI syndrome,17 a very small percentage of the current research evaluates factors beyond available hip joint range of motion. Among the few studies that examine functional movement, gait has been evaluated more than any other task;5, 13, 18, 22, 24, 36 yet the picture of how gait is altered in the presence of FAI syndrome remains unclear. Some of the variability in findings for hip and pelvic kinematics among studies could be due to individual differences in walking speeds as studies to date have used a self-selected speed for testing.
A substantial limitation of the current gait studies in individuals with FAI syndrome is that the majority of the participants in these studies are males despite females comprising an equal or greater percentage of the surgical population.9 Additionally, the current studies report only on the involved or painful limb during gait despite the structural morphology consistent with FAI syndrome being often present bilaterally.
Given these limitations, a study that contributes to the understanding of gait in both males and females with FAI syndrome is warranted. Therefore, the purpose of this study was to evaluate sex-specific differences in individuals with FAI syndrome compared to individuals without hip pain walking at both their preferred speed as well as a prescribed speed. We anticipated that some gait alterations would be consistent across the sexes, and that some differences would be unilateral (limb-specific) while others would be bilateral (person-specific).
METHODS
Participants
We performed our a priori power analysis on peak hip extension. We anticipated a 4.8° group difference (3.2° standard deviation) in hip extension angles21 during natural treadmill walking at 1.25 m/s.27 Accordingly, to achieve statistical power of .80 with an alpha of 0.05, a minimum of 8 participants of each sex for the FAI syndrome group and for the healthy comparison group was needed.
To be a participant in either group, individuals had to be between 14 and 50 years of age and report being able to walk safely for at least 10 minutes without an assistive device. Individuals with a history of neurological disorder or back surgery, or current back, knee, or ankle pain were excluded from participation in either group.
We recruited individuals with FAI syndrome through area orthopaedic and rehabilitation clinics between January 2011 and December 2016. To be included in the FAI syndrome group, individuals had to have been diagnosed with cam, pincer, or mixed FAI syndrome by a physician and had to have their pain reproduced by at least 1 of 3 provocative tests performed during the study visit. The 3 provocative tests included: 1) flexion, adduction, internal rotation (FADIR) test; 2) flexion, abduction, external rotation (FABER) test; and 3) resisted straight leg raise. For the FADIR test, the hip was passively flexed to 90°, and then adducted and internally rotated.16 For the FABER test, the hip was passively positioned in flexion, abduction, and external rotation with the foot of the tested leg on top of the contralateral knee.38 For the resisted straight leg raise, the leg was passively positioned in 30° of hip flexion with the knee extended.32 The participant was then asked to keep the leg in that position without assistance, and continue to hold the position as resistance was applied at the distal leg. If the test reproduced the individual’s pain, the test was considered positive. While these tests are highly sensitive for intra-articular hip pathology, they have low specificity.32, 34 Therefore, they were used as screening tests to eliminate individuals in the hip pain group when all the tests were negative (suggesting that there was not hip involvement) and to eliminate individuals in the comparison group when a test was positive (suggesting that there might be hip involvement despite the lack of self-reported symptoms). Exclusion criteria included current or recent (within the last 2 months) lower extremity injury, history of lower extremity orthopaedic surgery, history of hip pain, and hip or groin pain or discomfort during any of the provocative tests.
This study was approved by the Institutional Review Boards of Boston University and Boston Children’s Hospital and all individuals provided written informed consent prior to participation. Data from some of the participants included in this study have been published elsewhere.26
Instrumentation
As this was part of a larger study for multiple functional tasks, we recorded whole body kinematic data of the trunk, pelvis, and lower extremity using a 10-camera motion capture system (Vicon Motion Systems Ltd. Cenntennial, CO, USA) sampling at 100 Hz. Participants walked on an instrumented split-belt treadmill (Bertec Corp, Columbus, OH, USA) sampling at 1000 Hz. Retro-reflective markers were placed over 30 bony landmarks on the trunk and pelvis and bilaterally on the lower extremities, along with rigid clusters of markers on the thighs and shanks as previously described.28
Questionnaires
All participants completed self-report questionnaires including the UCLA activity score,3 the modified Harris Hip Score (mHHS),6 and the hip disability and osteoarthritis outcome score (HOOS).23 The Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) was scored from the HOOS.33 The UCLA activity score is from 1 to 10 with 10 being most active. All other questionnaires were scored from 0% to 100% with 100% corresponding to excellent or no limitations.
Experimental Protocol
For testing, all participants wore a tight-fitting shirt, spandex shorts, and their own exercise shoes. Prior to data collection, the 3 provocative hip tests were performed on each participant. Preferred walking speed was determined by taking the average time of five 5-meter trials as participants walked laps around the lab. We placed reflective markers on the participant, and then collected a static calibration trial with the participant standing in a neutral posture with feet shoulder width apart and shoulders in approximately 90° of abduction. Joint centers for the hips and knees were created using this trial, but were not normalized in this position. We removed the medial knee and ankle markers after this trial.
Participants walked on the treadmill at their preferred speed and at a prescribed speed of 1.25 m/s. After the treadmill achieved the set speed and the participant acclimated, data were recorded for up to 120 seconds of continuous walking. At least 50 strides were used for analysis at each speed, with a median of 90 strides. Strides were excluded from analysis if there were missing marker data. The preferred speed was collected first to capture the individual’s natural pattern before enforcing the speed constraint. As walking speed affects gait kinematics,8, 25 the prescribed speed was used to obtain kinematics at a standard walking speed. Every 30 seconds, each participant was asked to verbally rate his or her pain on an 11-point (0: no pain-10: extreme pain) numeric rating scale.14
Data Analysis
Motion capture data were processed as previously described.28 Briefly, marker trajectories were labeled and gaps were filled using Vicon Nexus (Vicon Motion Systems Ltd, Centennial, CO, USA). Marker and ground reaction force data were filtered using a low-pass fourth-order Butterworth filter with a cutoff frequency of 6 Hz and 10 Hz, respectively. A participant-specific 8-segment hybrid model was created in Visual3D (C-Motion, Inc., Germantown, MD, USA) using the CODA pelvis model to define the pelvis and the hip joint centers. Kinematics of the hip, pelvis, and thigh were calculated. Pelvic and thigh segment angles were defined with respect to the laboratory coordinate system. Hip joint angles were defined as the angle between the thigh and pelvis segments. Ground reaction force data were used to determine heel strike.
For each stride, hip, pelvic, and thigh angles were normalized to the gait cycle (heel strike to ipsilateral heel strike). We extracted the dependent variables of interest, which included peak hip, pelvic, and thigh angles in the sagittal and frontal planes. The peak angle for each stride were then averaged together for each limb, and the average was used for statistical analysis.
Statistical Analysis
As there are well documented differences in hip and pelvis kinematics during gait due to speed8, 25 and sex,29 we performed separate analyses for each speed as well as for males and females. We used a linear regression analysis with one between participants factor (group: FAI syndrome versus comparison) and one within participants factor (limb: more painful versus less painful). For participants with FAI syndrome, the limb with worse self-reported symptoms was the more painful limb. For participants without hip pain, the more painful limb was randomly assigned to have a similar distribution between left and right as the FAI syndrome group. As each limb was included in the analysis and group sizes were uneven, a generalized estimating equation (GEE) correction was applied to the linear regression model.31 To understand the effects of group and limb, we analyzed the main effect of group (FAI syndrome versus comparison), and the interaction of group-by-limb. A separate GEE was performed for each dependent variable. If the group-by-limb interaction was significant, we performed 2 subsequent analyses. First, we used least significant difference (LSD) pairwise comparisons to analyze the difference between the more painful limb and less painful limb in individuals with FAI syndrome. Second, we calculated the average of the 2 limbs for each dependent variable for the comparison group, and used pairwise comparisons to analyze the difference between the more painful limb of individuals with FAI syndrome and the average of the 2 limbs for the individuals without hip pain. For each significant pairwise comparisons, Cohen’s d was used to compute the effect size (ES) and interpreted as small (0.2), medium (0.5), and large (0.8) effects.11 Differences less than 1.4° were not interpreted, as this has been reported as the minimal detectable change (MDC) for hip kinematics in a single testing session.39 All analyses were run in IBM SPSS Statistics version 20 (IBM Corporation, Armonk, NY).
RESULTS
Eleven males and 10 females with FAI syndrome and 19 males and 22 females without hip pain participated in the study (TABLE 1). The groups were not different in terms of height, mass, BMI, activity score, or preferred walking speed. The majority of the individuals with FAI syndrome had cam morphology. Seven of the 11 males with FAI syndrome reported symptoms on 1 limb only, while 7 of 10 females with FAI syndrome reported symptoms bilaterally. For both males and females, the FADIR test was positive in most individuals (TABLE 2). Of those in the FAI syndrome group who reported pain during walking, the average (SD) pain ratings for males and females were 1.8 (0.5) and 2.8 (1.3) at the preferred speed and 2.5 (1.3) and 1.7 (0.8) at the prescribed speed. The individuals with FAI syndrome generally scored lower on the self-report questionnaires than the individuals without hip pain (TABLE 3).
TABLE 1.
Demographic data.*
| Males | Females | ||||
|---|---|---|---|---|---|
| FAI Syndrome | Comparison | FAI Syndrome | Comparison | ||
| N | 11 | 19 | 10 | 22 | |
| Age (years) | 25.3 ± 8.0 | 25.1 ± 6.2 | 20.7 ± 6.8 | 22.5 ± 2.8 | |
| Height (m) | 1.80 ± 0.08 | 1.79 ± 0.07 | 1.67 ± 0.06 | 1.64 ± 0.07 | |
| Mass (kg) | 82.0 ± 9.1 | 77.4 ± 12.2 | 62.5 ± 7.2 | 59.9 ± 8.3 | |
| BMI (kg/m2) | 25.4 ± 1.6 | 24.2 ± 3.1 | 22.4 ± 2.2 | 22.4 ± 2.6 | |
| UCLA Activity Score | 9.5 (5−10) | 9 (5−10) | 8 (4−10) | 9 (4−10) | |
| Preferred walking speed (m/s) | 1.26 ± 0.17 | 1.27 ± 0.18 | 1.31 ± 0.14 | 1.28 ± 0.16 | |
Data are mean ± SD analyzed with independent-samples t-test, except for UCLA Activity Score which is median (range) and was analyzed with Mann-Whitney U test. Data for UCLA Activity Score were missing for 1 male with FAI syndrome and 1 female without hip pain. There was no significant difference between groups for all variables, P > .05.
Abbreviations: BMI, body mass index; FAI, femoroacetabular impingement.
TABLE 2.
Number of individuals with FAI syndrome who had pain with provocative tests and during gait.*
| Males (N = 11) | Females (N = 10) | ||||
|---|---|---|---|---|---|
| More Painful Limb N (%) |
Less Painful Limb N (%) |
More Painful Limb N (%) |
Less Painful Limb N (%) |
||
| Provocative Test | |||||
| FADIR | 10 (91%) | 5 (45%) | 10 (100%) | 8 (80%) | |
| FABER | 5 (45%) | 1 (9%) | 4 (40%) | 1 (10%) | |
| SLR | 5 (45%) | 3 (27%) | 6 (60%) | 4 (40%) | |
| Gait | |||||
| Preferred | 4 (36%) | 2 (18%) | 5 (50%) | 2 (20%) | |
| Prescribed | 4 (36%) | 2 (18%) | 6 (60%) | 2 (20%) | |
Individuals in the comparison group did not have any positive (painful) tests.
Abbreviations: FABER, flexion, adduction, external rotation test; FADIR, flexion, adduction, internal rotation test; FAI, femoroacetabular impingement; SLR, straight leg raise resisted at 30°.
TABLE 3.
Data from self-report questionnaire scores.*
| FAI Syndrome | Comparison | |||||||
|---|---|---|---|---|---|---|---|---|
| Males (N = 10) |
Females (N = 10) |
Males (N = 19) |
Females (N = 21) |
|||||
| Questionnaire† | More Painful Limb | Less Painful Limb | More Painful Limb | Less Painful Limb | ||||
| mHHS | 76.9 ± 12.7 | 94.1 ± 9.4 | 71.1 ± 20.4 | 84.9 ± 16.9 | 100.0 ± 0.0 | 99.8 ± 1.2 | ||
| HOOS Subscales | ||||||||
| Pain | 70.5 ± 18.2 | 92.8 ± 13.9 | 68.3 ± 16.9 | 91.5 ± 8.4 | 100.0 ± 0.0 | 100.0 ± 0.0 | ||
| Symptoms | 63.0 ± 13.2 | 88.5 ± 13.6 | 68.5 ± 14.2 | 87.0 ± 12.5 | 99.0 ± 2.1 | 97.3 ± 4.4 | ||
| Functional Activities | 84.4 ± 12.3 | 95.9 ± 8.3 | 84.9 ± 12.3 | 97.1 ± 5.3 | 99.9 ± 0.3 | 100.0 ± 0.0 | ||
| Recreation/Sport Activities | 68.8 ± 20.8 | 86.9 ± 15.4 | 66.3 ± 21.3 | 90.6 ± 13.9 | 100.0 ± 0.0 | 99.7 ± 1.3 | ||
| Quality of Life | 49.4 ± 19.4 | 82.5 ± 19.5 | 43.8 ± 25.3 | 81.3 ± 17.7 | 100.0 ± 0.0 | 99.7 ± 1.3 | ||
| WOMAC | 81.7 ± 13.4 | 95.6 ± 9.1 | 81.5 ± 10.9 | 96.1 ± 5.6 | 99.9 ± 0.2 | 100.0 ± 0.0 | ||
Data are mean ± SD; data were missing for 1 male with FAI syndrome and 1 control female.
Questionnaire scores range from 0% to 100%, with 100% corresponding to excellent or no limitations.
Abbreviations: FAI, femoroacetabular impingement; HOOS, hip disability and osteoarthritis outcome score; mHHS, modified Harris Hip Score; WOMAC, Western Ontario and McMaster Universities Osteoarthritis Index.
Sex-specific analyses: males
There were significant group differences at the hip and pelvis, but not at the thigh (TABLE 4, 5, and 6). There were only 2 significant group-by-limb interactions at the pelvis (TABLE 5). No other interactions were significant.
TABLE 4:
Peak hip angles* in the sagittal and frontal planes of the more painful limb and less painful limb for the FAI syndrome group and of the averaged left and right limbs for the comparison group walking at the preferred and prescribed speeds.
| FAI Syndrome | Comparison Group | ||||
|---|---|---|---|---|---|
| Angle (°) | Speed | More Painful Limb | Less Painful Limb | Average of Limbs | |
| Males | |||||
| Hip Flexion | Prf † | 32.7 ± 6.5 | 31.8 ± 7.2 | 26.3 ± 9.2 | |
| Prsc | 30.0 ± 5.8 | 30.4 ± 6.7 | 25.9 ± 8.7 | ||
| Hip Extension | Prf † | −6.8 ± 8.1 | −7.7 ± 5.5 | −15.4 ± 8.8 | |
| Prsc † | −9.0 ± 8.7 | −8.9 ± 6.9 | −15.8 ± 8.8 | ||
| Hip Adduction | Prf | 2.5 ± 3.6 | 2.1 ± 3.7 | 4.1 ± 2.8 | |
| Prsc | 3.2 ± 3.3 | 3.7 ± 3.1 | 4.2 ± 2.8 | ||
| Hip Abduction | Prf | −7.5 ± 2.8 | −7.5 ± 3.4 | −8.3 ± 1.7 | |
| Prsc † | −7.4 ± 1.9 | −7.0 ± 3.0 | −8.5 ± 1.8 | ||
| Females | |||||
| Hip Flexion | Prf | 32.1 ± 10.0 | 31.7 ± 8.1 | 32.6 ± 7.1 | |
| Prsc | 32.2 ± 9.2 | 31.0 ± 8.4 | 32.3 ± 8.2 | ||
| Hip Extension | Prf ‡§ | −10.4 ± 9.5 | −12.2 ± 9.2 | −9.9 ± 7.4 | |
| Prsc ‡§ | −10.6 ± 10.4 | −12.7 ± 10.5 | −10.2 ± 7.7 | ||
| Hip Adduction | Prf ‡§ | 8.1 ± 3.3 | 4.4 ± 1.9 | 7.1 ± 2.4 | |
| Prsc ‡§ | 8.7 ± 4.0 | 4.8 ± 2.2 | 7.1 ± 2.3 | ||
| Hip Abduction | Prf ‡§ | −6.4 ± 2.0 | −9.2 ± 2.6 | −6.8 ± 1.9 | |
| Prsc ‡§ | −6.0 ± 1.9 | −9.6 ± 2.8 | −6.9 ± 1.9 | ||
Data are mean ± SD. Hip flexion and hip adduction are positive.
Significant main effects of group, P < .05.
Significant interaction effects of group-by-limb, P < .05.
Significant within FAI syndrome group effects of limb, P < .05.
Abbreviations: FAI, femoroacetabular impingement; Prf, preferred; Prsc, prescribed.
TABLE 5:
Peak pelvic segment angles* in the sagittal and frontal planes of the more painful limb and less painful limb for the FAI syndrome group and of the averaged left and right limbs for the comparison group walking at the preferred and prescribed speeds.
| FAI Syndrome | Comparison Group | ||||
|---|---|---|---|---|---|
| Angle (°) | Speed | More Painful Limb | Less Painful Limb | Average of Limbs | |
| Males | |||||
| Pelvic Posterior Tilt | Prf † | −4.8 ± 5.5 | −4.8 ± 5.5 | 0.5 ± 7.1 | |
| Prsc † | −4.8 ± 5.5 | −4.8 ± 5.5 | 0.7 ± 7.0 | ||
| Pelvic Anterior Tilt | Prf † | −9.4 ± 5.7 | −9.4 ± 5.9 | −4.0 ± 6.9 | |
| Prsc † | −9.3 ± 5.8 | −9.3 ± 5.9 | −4.0 ± 6.9 | ||
| Pelvic Hike | Prf | 2.6 ± 1.8 | 2.8 ± 1.7 | 3.1 ± 1.2 | |
| Prsc ‡ | 3.1 ± 1.9 | 2.7 ± 1.8 | 3.2 ± 1.2 | ||
| Pelvic Drop | Prf | −2.8 ± 1.7 | −2.6 ± 1.7 | −3.1 ± 1.2 | |
| Prsc ‡ | −2.7 ± 1.8 | −3.2 ± 1.8 | −3.2 ± 1.2 | ||
| Females | |||||
| Pelvic Posterior Tilt | Prf ‡ | −3.4 ± 7.0 | −3.5 ± 7.0 | −3.2 ± 6.0 | |
| Prsc ‡ | −3.6 ± 6.8 | −3.7 ± 6.8 | −3.2 ± 6.5 | ||
| Pelvic Anterior Tilt | Prf ‡ | −7.5 ± 7.1 | −7.5 ± 7.1 | −7.1 ± 5.6 | |
| Prsc ‡ | −7.6 ± 6.9 | −7.6 ± 6.8 | −7.2 ± 6.0 | ||
| Pelvic Hike | Prf | 3.5 ± 1.3 | 5.3 ± 2.5 | 4.1 ± 1.2 | |
| Prsc | 3.5 ± 1.6 | 5.7 ± 2.5 | 4.3 ± 1.3 | ||
| Pelvic Drop | Prf | −5.3 ± 2.5 | −3.5 ± 1.3 | −4.1 ± 1.2 | |
| Prsc | −5.7 ± 2.5 | −3.5 ± 1.6 | −4.3 ± 1.3 | ||
Data are mean ± SD. Pelvic posterior tilt and pelvic hike of the contralateral side are positive.
Significant main effects of group, P < .05.
Significant interaction effects of group-by-limb, P < .05.
Abbreviations: FAI, femoroacetabular impingement; Prf, preferred; Prsc, prescribed.
TABLE 6:
Peak thigh segment angles* in the sagittal and frontal planes of the more painful limb and less painful limb for the FAI syndrome group and of the averaged left and right limbs for the comparison group walking at the preferred and prescribed speeds.
| FAI Syndrome | Comparison Group | ||||
|---|---|---|---|---|---|
| Angle (°) | Speed | More Painful Limb | Less Painful Limb | Average of Limbs | |
| Males | |||||
| Thigh Flexion | Prf | 25.2 ± 4.9 | 24.1 ± 5.7 | 24.5 ± 3.4 | |
| Prsc | 23.1 ± 2.3 | 23.1 ± 3.8 | 24.3 ± 3.2 | ||
| Thigh Extension | Prf | −15.1 ± 4.8 | −15.6 ± 4.4 | −17.9 ± 3.0 | |
| Prsc | −17.3 ± 4.5 | −16.7 ± 3.8 | −18.3 ± 2.9 | ||
| Thigh Adduction | Prf | 1.4 ± 2.7 | 1.7 ± 2.3 | 3.0 ± 2.0 | |
| Prsc | 2.0 ± 2.2 | 2.2 ± 1.8 | 2.9 ± 2.1 | ||
| Thigh Abduction | Prf | −6.4 ± 2.8 | −6.1 ± 2.5 | −6.6 ± 2.4 | |
| Prsc | −5.5 ± 2.1 | −5.7 ± 2.3 | −6.8 ± 2.0 | ||
| Females | |||||
| Thigh Flexion | Prf | 26.4 ± 3.1 | 25.4 ± 3.5 | 27.4 ± 2.7 | |
| Prsc | 26.3 ± 2.6 | 24.7 ± 3.1 | 27.1 ± 3.2 | ||
| Thigh Extension | Prf | −16.4 ± 3.3 | −17.7 ± 3.1 | −15.7 ± 3.0 | |
| Prsc ‡§ | −16.5 ± 3.9 | −18.3 ± 3.7 | −16.0 ± 3.1 | ||
| Thigh Adduction | Prf ‡ | 4.4 ± 1.9 | 3.3 ± 1.3 | 4.6 ± 1.8 | |
| Prsc | 4.5 ± 2.5 | 3.4 ± 1.5 | 4.5 ± 1.6 | ||
| Thigh Abduction | Prf | −4.1 ± 2.2 | −4.8 ± 1.9 | −3.3 ± 1.6 | |
| Prsc | −3.8 ± 2.3 | −4.9 ± 2.2 | −3.4 ± 1.6 | ||
Data are mean ± SD. Flexion and adduction of the thigh segment are positive.
Significant interaction effects of group-by-limb, P < .05.
Significant within FAI syndrome group effects of limb, P < .05.
Abbreviations: FAI, femoroacetabular impingement; Prf, preferred; Prsc, prescribed.
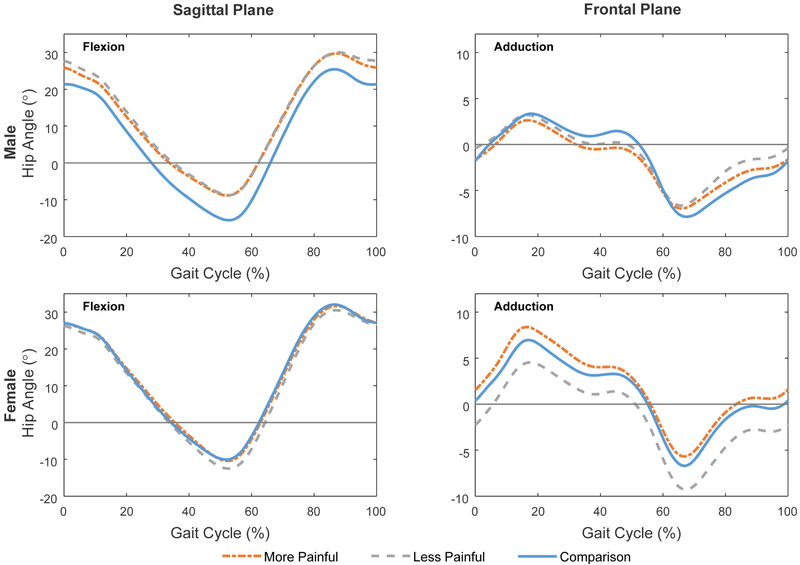
Hip:
Males with FAI syndrome had 6.0° more peak hip flexion than the comparison group when walking at the preferred speed (95% Confidence Interval (CI): 0.4, 11.5; P = .035; ES = 0.71) (TABLE 4, FIGURE 1). Males with FAI syndrome also walked with 8.2° less peak hip extension than males without hip pain at the preferred walking speed (95% CI: 2.8, 13.5; P = .003; ES = 1.01), and 6.9° less peak hip extension at the prescribed walking speed (95% CI: 1.2, 12.6; P = .018; ES = 0.83). Males with FAI syndrome had 1.4° less peak hip abduction than males without hip pain at the prescribed speed (95% CI: 0.02, 2.7; P = .047; ES = 0.74).
FIGURE 1.
Average hip angles in the sagittal and frontal planes of the more and less painful limbs for the femoroacetabular impingement syndrome group and of the averaged left and right limbs for the comparison group walking at the prescribed speed. Hip flexion and hip adduction are positive. Data are from heel strike to ipsilateral heel strike.
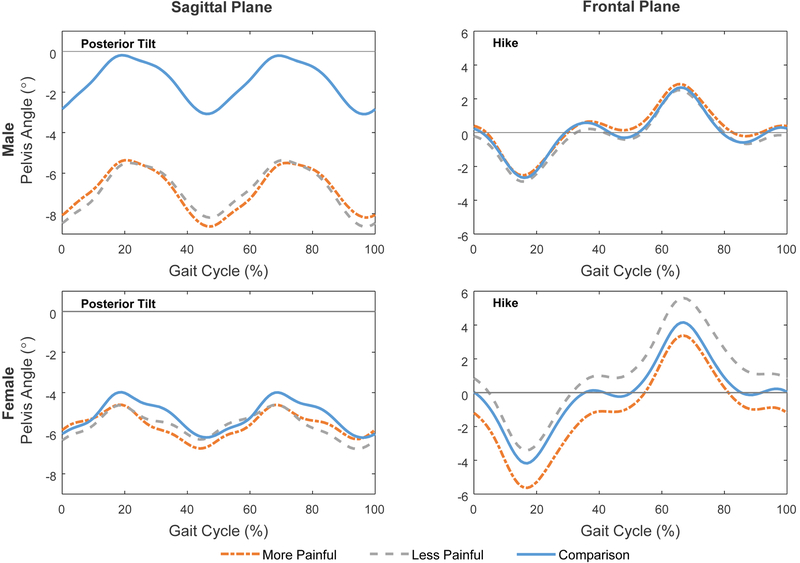
Pelvis:
At the pelvis, there were group differences in peak posterior pelvic tilt and peak anterior pelvic tilt in males at both speeds (TABLE 5, FIGURE 2). Males with FAI syndrome walked with 5.3° less peak posterior pelvic tilt than males without hip pain at the preferred speed (95% CI: 0.9, 9.7; P = .018; ES = 0.80), and 5.4° less peak posterior pelvic tilt at the prescribed speed (95% CI: 1.1, 9.8; P = .015; ES = 0.83). Males with FAI syndrome also walked with 5.4° more peak anterior pelvic tilt than males without hip pain at the preferred speed (95% CI: 1.0, 9.9; P = .017; ES = 0.83), and 5.3° more peak anterior pelvic tilt at the prescribed speed (95% CI: 0.8, 9.8; P = .020; ES = 0.81). There were significant group-by-limb interactions for peak pelvic hike (P = .033) and drop (P = .033) at the prescribed speed; no differences were noted in the subsequent pairwise analyses.
FIGURE 2.
Average pelvic segment angles in the sagittal and frontal planes of the more and less painful limbs for the femoroacetabular impingement syndrome group and of the averaged left and right limbs for the comparison group walking at the prescribed speed. Pelvic posterior tilt and pelvic hike of the contralateral side are positive. Data are from heel strike to ipsilateral heel strike.
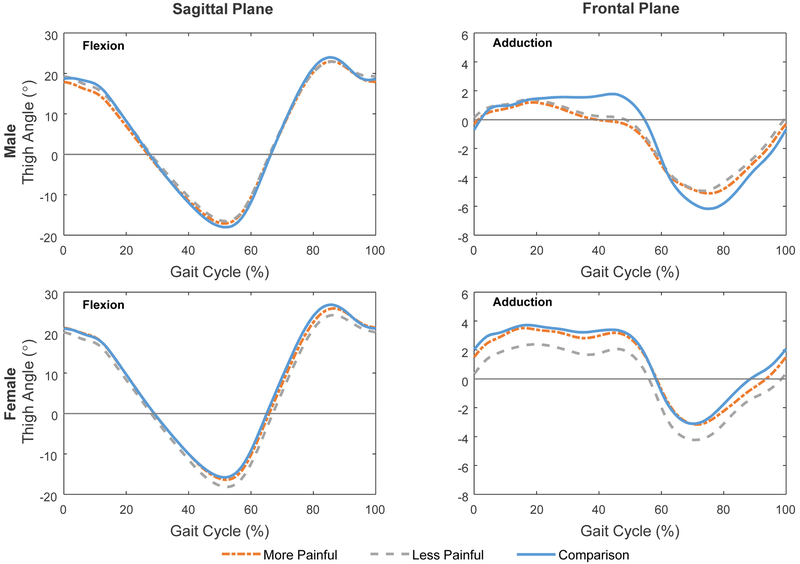
Thigh:
There were no significant group differences or group-by-limb interactions for the thigh in either plane at either speed (TABLE 6, FIGURE 3).
FIGURE 3.
Average thigh segment angles in the sagittal and frontal planes of the more painful limb and less painful limb for the femoroacetabular impingement syndrome group and of the averaged left and right limbs for the comparison group walking at the prescribed speed. Flexion and adduction of the thigh segment are positive. Data are from heel strike to ipsilateral heel strike.
Sex-specific analyses: Females
There were no significant group effects (P ≥ .069) for any of the variables in females, but were significant group-by-limb interactions at the hip, pelvis, and thigh (TABLES 4, 5, and 6).
Hip:
At the hip, there were significant group-by-limb interactions for peak hip extension (P = .033, P = .010 for the preferred and prescribed speeds, respectively), peak hip adduction (P < .001, P < .001), and peak hip abduction (P = .014, P = .004) (TABLE 4, FIGURE 1). In the subsequent pairwise analyses, there were differences between the more painful limb and the less painful limb in females with FAI syndrome. In the FAI syndrome group, individuals walked with 1.8° less peak hip extension on the more painful limb than on the less painful limb at the preferred speed (95% CI: 0.4, 3.2; P = .012; ES = 0.75), and 2.1° less peak hip extension on the more painful limb at the prescribed speed (95% CI: 0.7, 3.4; P = .004; ES = 0.87). In the frontal plane, females with FAI syndrome walked with 3.8° more peak hip adduction on the more painful limb than on the less painful limb at the preferred speed (95% CI: 2.2, 5.3; P < .001; ES = 1.46), and 3.9° more peak hip adduction at the prescribed speed (95% CI: 1.8, 5.9; P < .001; ES = 1.11). Additionally, females with FAI syndrome walked with 2.8° less peak hip abduction on the more painful limb than on the less painful limb at the preferred speed (95% CI: 0.8, 4.8; P = .006; ES = 0.82) and 3.6° less peak hip abduction at the prescribed speed (95% CI: 1.4, 5.8; P = .002; ES = 0.95).
Pelvis:
There were significant group-by-limb interactions for peak posterior pelvic tilt (P = .012, P = .043 for the preferred and prescribed speeds, respectively) and peak anterior pelvic tilt (P = .047, P < .001) (TABLE 5, FIGURE 2). In the subsequent pairwise analysis, there were no differences between the FAI syndrome group and the comparison group (P ≥ .867). While peak posterior pelvic tilt at the preferred speed was different between limbs (P = .044), it was less than the MDC, and therefore, was not interpreted.
Thigh:
There was a significant group-by-limb interaction for peak thigh extension position in the sagittal plane at the prescribed speed (P = .017, TABLE 6, FIGURE 3). Within the FAI syndrome group, the thigh of the more painful limb was in 1.7° less of an extended position compared to the less painful limb (95% CI: 0.5, 2.9; P = .004; ES = 0.86) at the prescribed speed. In the frontal plane, the group-by-limb interaction for peak thigh adduction position was significant at the preferred speed (P = .028, FIGURE 3); no differences were noted in the subsequent pairwise analyses.
DISCUSSION
The results of this study indicate that there are sex-specific differences in the gait alterations observed in individuals with FAI syndrome compared to individuals without hip pain. In males, there were primarily group effects suggesting person-specific alterations. Whereas, in females, there were group-by-limb interactions suggesting limb-specific alterations. These findings indicate that FAI syndrome may contribute to gait alterations differently in males than in females.
Males with FAI syndrome had decreased peak hip extension compared to males without hip pain, a difference that was slightly larger than noted by Hunt et al.21 While we had expected a unilateral alteration, we found a group difference for males, suggesting a bilateral alteration. This may be due to the increased anterior pelvic tilt in the FAI syndrome group, a group effect for males as well. The anterior pelvic tilt could produce an offset in the hip angle curve, especially as the sagittal plane thigh angle was not different. In a secondary analysis of standing posture, males with FAI syndrome were in more anterior pelvic tilt than males without hip pain, highlighting the importance of not normalizing data to a position. Increased anterior pelvic tilt (or decreased posterior tilt) has been reported in individuals with FAI syndrome during bilateral squatting4 and stair climbing.36 In females, however, we did not note a difference in pelvic tilt, and the reduction in hip extension was on the more painful limb compared to the less painful limb.
We also found sex-specific alterations in the frontal plane. This is in partial agreement with previous studies which noted decreased abduction of the more painful hip compared to healthy comparison participants walking at a preferred speed.18, 22, 36 However, we found that this was a person-specific alteration for males and a limb-specific alteration for females. Females with FAI syndrome also had increased peak hip adduction on the more painful limb compared to the less painful limb. The increased hip adduction may be due to weakness which has been noted in the hip abductor muscles in this patient population,7 or may be an adaptation to reduce compressive forces on the hip due to muscle activation.30 However, reliance on the hip ligaments for stability may increase hip contact force.12 Alternatively, the increased hip adduction, which is closer to the impingement position,16 may contribute to symptoms and explain why females experience symptoms with less severe cam morphology than do males.19
A consistent pattern throughout our findings was that there were primarily group differences for males, but only group-by-limb interactions for females. The group effects in the males could imply that males with FAI syndrome displayed the movement alterations bilaterally. However, there was significant variability as to which hip was affected more, raising questions on how to best interpret the alterations. For example, the morphology itself is unlikely to produce a reduction in hip extension. Instead, the reduction could be a result of shortened or overactive hip flexor muscles, or could be an adaptation to reduce anteriorly directed hip joint forces30 or to reduce tension on anterior hip joint structures (eg, the iliofemoral ligament).20 As cam morphology, and not pincer morphology,1, 37 has been linked to an increased risk for hip OA,2, 37 it could also be an early indicator of OA. Based on these arguments, it should follow that hip extension would be limited to a greater extent in the more painful hip than in the less painful. While this was true in females with FAI syndrome, it was not true in males. Additionally, the group effect versus group-by-limb interaction effect findings may indicate that FAI syndrome is more likely to manifest itself bilaterally in males and unilaterally in females. However, in our study, we had more females with bilateral symptoms than males with bilateral symptoms. Thus, we expected group effects in females and limb effects in males.
It remains unclear how the gait alterations noted in individuals with FAI syndrome contribute to or result from the morphology or symptoms of FAI syndrome. Although anterior pelvic tilt35 and hip adduction16 could cause impingement, the hip does not reach the point of impingement during gait. Nonetheless, individuals with FAI syndrome report pain with prolonged walking.10 The alterations may be a compensation for pain. The alterations were slightly larger in individuals who reported pain during gait compared to individuals with FAI syndrome who did not. It may also be that individuals with FAI syndrome display these same movement alterations in tasks that are closer to end range motions when impingement is more likely.
The present study does have limitations. Our groups were small and we did not have the power to detect small differences in movement that might be present (type II error). Also because of the small numbers, we used a statistical approach which might increase the likelihood of detecting a difference when there was not one (type I error). Multi-center studies are necessary to produce larger datasets. For the individuals with FAI syndrome, the type of bony morphology was reported by the orthopaedic clinic or participant, not measured as part of the study. We did not image our comparison group to evaluate hip morphology. Our healthy comparison group was comprised of individuals without hip pain, and therefore without FAI syndrome,17 but may have had cam or pincer morphology which is often present in asymptomatic individuals, especially athletes.15 As a cross-sectional study, it was impossible to determine the cause of the altered movement patterns. The alterations may have contributed to the development of FAI syndrome or be a compensation. Longitudinal studies are needed to disentangle cause and compensation. Similarly, we did not test if modifying the walking patterns would change the symptoms.
CONCLUSIONS
The results of this study suggest that males with FAI syndrome have different gait alterations than females with FAI syndrome when compared to sex-matched individuals without hip pain. In males, the differences were primarily between groups. In females with FAI syndrome, the differences were between the more and less painful limbs. These findings suggest that altered movement may be a contributing factor to FAI syndrome and may be modifiable through neuromuscular training.
KEY POINTS.
Findings:
Gait alterations in individuals with FAI syndrome were sex-specific. Males with FAI syndrome displayed a bilateral reduction in peak hip extension and abduction, and an increase in peak anterior pelvic tilt compared to males without hip pain. Females with FAI syndrome displayed a reduction in peak hip extension and hip abduction and an increase in peak hip adduction on the more painful limb compared to the less painful limb.
Implications:
These differences may indicate different etiology and the need for sex-specific movement interventions for individuals with FAI syndrome.
Caution:
This cross-sectional study does not address the question of cause versus compensation. Future studies are warranted to determine if these movement alterations are present in more challenging tasks, and if modifying these patterns affects symptoms.
Acknowledgments
Research reported in this manuscript was supported by the Peter Paul Career Development Professorship and the National Institute of Arthritis and Musculoskeletal and Skin Diseases of the National Institutes of Health under Award Numbers R21 AR061690, K23 AR063235, and P60 AR047785.
Footnotes
This study was approved by Institutional Review Boards of Boston University and Boston Children’s Hospital and all individuals provided written informed consent prior to participation.
References
- 1.Agricola R, Heijboer M, Roze R, et al. Pincer deformity does not lead to osteoarthritis of the hip whereas acetabular dysplasia does: Acetabular coverage and development of osteoarthritis in a nationwide prospective cohort study (CHECK). Osteoarthr Cartil 2013;21(10):1514–21. [DOI] [PubMed] [Google Scholar]
- 2.Agricola R, Heijboer MP, Bierma-Zeinstra SM, Verhaar JA, Weinans H, Waarsing JH. Cam impingement causes osteoarthritis of the hip: A nationwide prospective cohort study (CHECK). Ann Rheum Dis. 2013;72(6):918–23. 10.1136/annrheumdis-2012-201643. [DOI] [PubMed] [Google Scholar]
- 3.Amstutz HC, Thomas BJ, Jinnah R, Kim W, Grogan T, Yale C. Treatment of primary osteoarthritis of the hip. A comparison of total joint and surface replacement arthroplasty. J Bone Joint Surg Am. 1984;66(2):228–41. [PubMed] [Google Scholar]
- 4.Bagwell JJ, Snibbe J, Gerhardt M, Powers CM. Hip kinematics and kinetics in persons with and without cam femoroacetabular impingement during a deep squat task. Clin Biomech. 2016;31:87–92. [DOI] [PubMed] [Google Scholar]
- 5.Brisson N, Lamontagne M, Kennedy MJ, Beaule PE. The effects of cam femoroacetabular impingement corrective surgery on lower-extremity gait biomechanics. Gait Posture. 2013;37(2):258–63. 10.1016/j.gaitpost.2012.07.016. [DOI] [PubMed] [Google Scholar]
- 6.Byrd JW, Jones KS. Prospective analysis of hip arthroscopy with 2-year follow-up. Arthroscopy. 2000;16(1526–3231; 6):578–87. [DOI] [PubMed] [Google Scholar]
- 7.Casartelli NC, Maffiuletti NA, Item-Glatthorn JF, et al. Hip muscle weakness in patients with symptomatic femoroacetabular impingement. Osteoarthritis Cartilage. 2011;19(7):816–21. 10.1016/j.joca.2011.04.001. [DOI] [PubMed] [Google Scholar]
- 8.Chung M, Wang MJ. The change of gait parameters during walking at different percentage of preferred walking speed for healthy adults aged 20–60 years. Gait Posture. 2010;31(1):131–5. [DOI] [PubMed] [Google Scholar]
- 9.Clohisy JC, Baca G, Beaulé PE, et al. Descriptive epidemiology of femoroacetabular impingement: A North American cohort of patients undergoing surgery. Am J Sports Med. 2013;41(6):1348–56. [DOI] [PubMed] [Google Scholar]
- 10.Clohisy JC, Knaus ER, Hunt DM, Lesher JM, Harris-Hayes M, Prather H. Clinical presentation of patients with symptomatic anterior hip impingement. Clin Orthop Relat Res. 2009;467(3):638–44. 10.1007/s11999-008-0680-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cohen J Statistical power analysis for the behavioral sciences. 2nd ed Hillsdale, NJ: Lawrence Erlbaum Associates, Inc; 1988. [Google Scholar]
- 12.Crowninshield RD, Johnston RC, Brand RA, Pedersen DR. Pathologic ligamentous constraint of the hip. Clinical Orthopaedics and Related Research. 1983;181:291–7. [PubMed] [Google Scholar]
- 13.Diamond LE, Wrigley TV, Bennell KL, Hinman RS, O’Donnell J, Hodges PW. Hip joint biomechanics during gait in people with and without symptomatic femoroacetabular impingement. Gait Posture. 2016;43:198–203. [DOI] [PubMed] [Google Scholar]
- 14.Downie WW, Leatham PA, Rhind VM, Wright V, Branco JA, Anderson JA. Studies with pain rating scales. Ann Rheum Dis. 1978;37(4):378–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Frank JM, Harris JD, Erickson BJ, et al. Prevalence of femoroacetabular impingement imaging findings in asymptomatic volunteers: A systematic review. Arthroscopy. 2015;31(6):1199–204. [DOI] [PubMed] [Google Scholar]
- 16.Ganz R, Parvizi J, Beck M, Leunig M, Notzli H, Siebenrock KA. Femoroacetabular impingement: A cause for osteoarthritis of the hip. Clin Orthop. 2003(417):112–20. [DOI] [PubMed] [Google Scholar]
- 17.Griffin DR, Dickenson EJ, O’Donnell J, et al. The Warwick Agreement on femoroacetabular impingement syndrome (FAI syndrome): An international consensus statement. Br J Sports Med. 2016;50(19):1169–76. 10.1136/bjsports-2016-096743. [DOI] [PubMed] [Google Scholar]
- 18.Hetsroni I, Funk S, Ben-Sira D, Nyska M, Palmanovich E, Ayalon M. Femoroacetabular impingement syndrome is associated with alterations in hindfoot mechanics: A three-dimensional gait analysis study. Clin Biomech. 2015;30(10):1189–93. 10.1016/j.clinbiomech.2015.08.005. [DOI] [PubMed] [Google Scholar]
- 19.Hetsroni I, Dela Torre K, Duke G, Lyman S, Kelly BT. Sex differences of hip morphology in young adults with hip pain and labral tears. Arthroscopy. 2013;29(1):54–63. 10.1016/j.arthro.2012.07.008. [DOI] [PubMed] [Google Scholar]
- 20.Hidaka E, Aoki M, Izumi T, Suzuki D, Fujimiya M. Ligament strain on the iliofemoral, pubofemoral, and ischiofemoral ligaments in cadaver specimens: Biomechanical measurement and anatomical observation. Clin Anat. 2014;27(7):1068–75. 10.1002/ca.22425. [DOI] [PubMed] [Google Scholar]
- 21.Hunt MA, Gunether JR, Gilbart MK. Kinematic and kinetic differences during walking in patients with and without symptomatic femoroacetabular impingement. Clin Biomech. 2013;28(5):519–23. [DOI] [PubMed] [Google Scholar]
- 22.Kennedy MJ, Lamontagne M, Beaule PE. Femoroacetabular impingement alters hip and pelvic biomechanics during gait walking biomechanics of FAI. Gait Posture. 2009;30(1):41–4. 10.1016/j.gaitpost.2009.02.008. [DOI] [PubMed] [Google Scholar]
- 23.Klässbo M, Larsson E, Mannevik E. Hip disability and osteoarthritis outcome score an extension of the Western Ontario and McMaster universities osteoarthritis index. Scand J Rheumatol. 2003;32(1):46–51. [DOI] [PubMed] [Google Scholar]
- 24.Kumar D, Dillon A, Nardo L, Link TM, Majumdar S, Souza RB. Differences in the association of hip cartilage lesions and cam-type femoroacetabular impingement with movement patterns: A preliminary study. PM R. 2014;6(8):681–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lelas JL, Merriman GJ, Riley PO, Kerrigan DC. Predicting peak kinematic and kinetic parameters from gait speed. Gait Posture. 2003;17(2):106–12. [DOI] [PubMed] [Google Scholar]
- 26.Lewis CL, Loverro KL, Khuu A. Kinematic differences during single leg stepdown between individuals with femoroacetabular impingement syndrome and individuals without hip pain. J Orthop Sports Phys Ther. 2018. (Accepted). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lewis CL, Ferris DP. Walking with increased ankle pushoff decreases hip muscle moments. J Biomech. 2008;41(10):2082–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lewis CL, Foch E, Luko MM, Loverro KL, Khuu A. Differences in lower extremity and trunk kinematics between single leg squat and step down tasks. PLoS One. 2015;10(5):e0126258 10.1371/journal.pone.0126258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lewis CL, Laudicina NM, Khuu A, Loverro KL. The human pelvis: Variation in structure and function during gait. Anat Rec (Hoboken). 2017;300(4):633–42. 10.1002/ar.23552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lewis CL, Sahrmann SA, Moran DW. Effect of hip angle on anterior hip joint force during gait. Gait Posture. 2010;32(4):603–7. 10.1016/j.gaitpost.2010.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ma Y, Mazumdar M, Memtsoudis SG. Beyond repeated-measures analysis of variance: Advanced statistical methods for the analysis of longitudinal data in anesthesia research. Reg Anesth Pain Med. 2012;37(1):99–105. 10.1097/AAP.0b013e31823ebc74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Maslowski E, Sullivan W, Forster Harwood J, et al. The diagnostic validity of hip provocation maneuvers to detect intra-articular hip pathology. PM R. 2010;2(3):174–81. 10.1016/j.pmrj.2010.01.014. [DOI] [PubMed] [Google Scholar]
- 33.Nilsdotter AK, Lohmander LS, Klassbo M, Roos EM. Hip disability and osteoarthritis outcome score (HOOS)--validity and responsiveness in total hip replacement. BMC Musculoskelet Disord. 2003;4:10 10.1186/1471-2474-4-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Reiman MP, Goode AP, Cook CE, Holmich P, Thorborg K. Diagnostic accuracy of clinical tests for the diagnosis of hip femoroacetabular impingement/labral tear: A systematic review with meta-analysis. Br J Sports Med. 2015;49(12):811,2014–094302. Epub 2014 Dec 16. 10.1136/bjsports-2014-094302. [DOI] [PubMed] [Google Scholar]
- 35.Ross JR, Nepple JJ, Philippon MJ, Kelly BT, Larson CM, Bedi A. Effect of changes in pelvic tilt on range of motion to impingement and radiographic parameters of acetabular morphologic characteristics. Am J Sports Med. 2014;42(10):2402–9. [DOI] [PubMed] [Google Scholar]
- 36.Rylander J, Shu B, Favre J, Safran M, Andriacchi T. Functional testing provides unique insights into the pathomechanics of femoroacetabular impingement and an objective basis for evaluating treatment outcome. J Orthop Res. 2013;31(9):1461–8. 10.1002/jor.22375. [DOI] [PubMed] [Google Scholar]
- 37.Saberi Hosnijeh F, Zuiderwijk ME, Versteeg M, et al. Cam deformity and acetabular dysplasia as risk factors for hip osteoarthritis. Arthritis Rheumatol. 2017;69(1):86–93. [DOI] [PubMed] [Google Scholar]
- 38.Troelsen A, Mechlenburg I, Gelineck J, Bolvig L, Jacobsen S, Soballe K. What is the role of clinical tests and ultrasound in acetabular labral tear diagnostics? Acta Orthop. 2009;80(3):314–8. 10.3109/17453670902988402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Wilken JM, Rodriguez KM, Brawner M, Darter BJ. Reliability and minimal detectible change values for gait kinematics and kinetics in healthy adults. Gait Posture. 2012;35(2):301–7. 10.1016/j.gaitpost.2011.09.105. [DOI] [PubMed] [Google Scholar]