Abstract
TPMT activity exhibits a monogenic co-dominant inheritance and catabolizes thiopurines. TPMT variant alleles are associated with low enzyme activity and pronounced pharmalogic effecs of thiopurines. Loss-of-function alleles in the NUDT15 gene are common in Asians and Hispanics and reduces the degradation of active thiopurine nucleotide metabolites, also predisposing to myelosuppression. We provide recommendations for adjusting starting dosesof azathioprine, mercaptopurine, and thioguanine based on TPMT and NUDT15 genotypes (updates on www.cpicpgx.org).
Keywords: thiopurine, TPMT, pharmacogenetics, azathioprine, mercaptopurine, thioguanine, genetic testing, NUDT15, CPIC
INTRODUCTION
This document is an update to the Clinical Implementation Consorium (CPIC) Guidelines for Thiopurine Methyltransferease Genotype and Thiopurine guideline updated last in April 2013. The guideline text, evidence table and recommendations have been updated to reflect any new evidence. Specifically, this guideline adds a recommendation for NUDT15 genotype with minor changes to the TPMT recommendation. Although most of the dosing recommendations have been generated from clinical studies in just a few diseases, we have extrapolated recommended doses to all conditions, given the pharmacokinetic nature of the genotype/phenotype associations. CPIC guidelines are published and periodically updated on www.cpicpgx.org. Detailed guidelines for use of phenotypic tests (e.g. TPMT activity and thiopurine metabolite levels), as well as analyses of cost effectiveness, are beyond the scope of this document.
FOCUSED LITERATURE REVIEW
A systematic literature review focused on TPMT and NUDT15 genotypes and thiopurine use was conducted (details in Supplement). Definitive reviews (1–4) were relied upon to summarize much of the earlier literature.
DRUGS: THIOPURINES
Background
Three thiopurines are used clinically: azathioprine (a prodrug for mercaptopurine), mercaptopurine, and thioguanine. Although all three medications share many of the same pharmacologic effects, mercaptopurine and azathioprine are generally used for non-malignant immunologic disorders, mercaptopurine for lymphoid malignancies, and thioguanine for myeloid leukemias. Because azathioprine is a prodrug for mercaptopurine, the two drugs can be considered to have identical interactions with TPMT and NUDT15. Recommendations for individuals with variants in one or both of these genes will be addressed in detail in the following sections.
GENES: TPMT AND NUDT15
Background
TPMT.
TPMT activity is inherited as a monogenic, autosomal co-dominant trait (Supplement, Figure S1). Three TPMT single nucleotide polymorphisms (SNPs), which result in unstable proteins and enhanced TPMT protein degradation (2, 3), account for over 90% of low activity phenotypes and are the most common inactivating alleles, and so genotyping tests including these three variants have a high likelihood of being informative for TPMT phenotype (5, 6). Complementary phenotype laboratory tests can be helpful adjuncts to genotyping tests (Supplement, Other Considerations) (7).
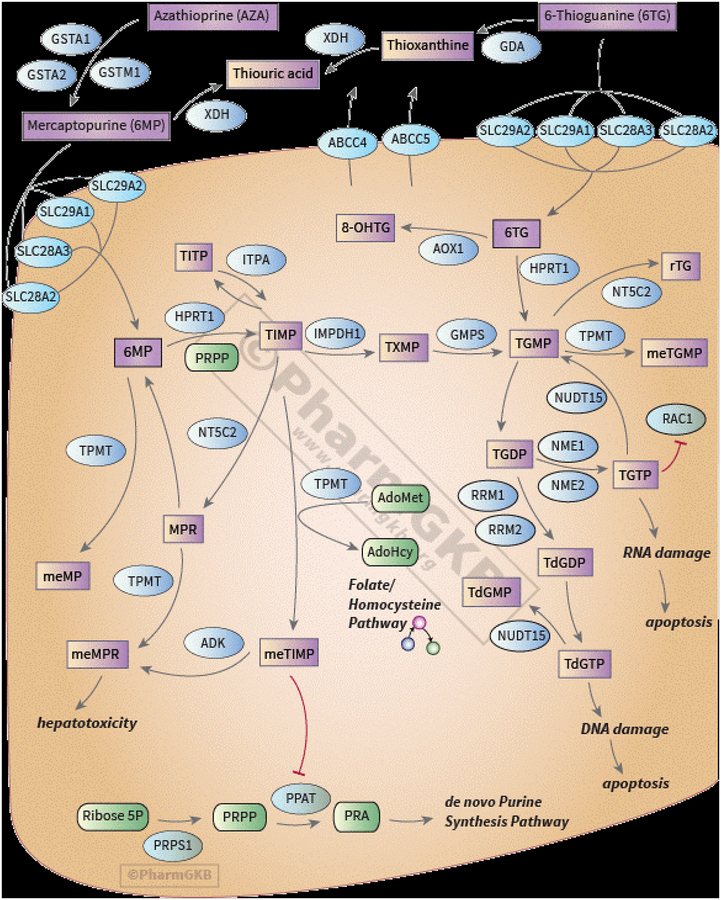
TPMT catabolizes mercaptopurine to an inactive methylmercaptopurine base, leaving less parent drug available for eventual anabolism to active thioguanine nucleotides (TGNs, Figure 1). The secondary metabolite of mercaptopurine, thioinosine monophosphate (TIMP), is also a substrate for TPMT, and methylTIMP (and its further phosphorylated metabolites, methylmercaptopurine nucleotides or MeMPN) have pharmacologic activity (mostly immunosuppressive and hepatotoxic), inhibit de novo purine synthesis, and may contribute to some of the adverse effects of mercaptopurine, generally hepatotoxicity (2, 8, 9). Individuals who inherit two loss-of-function TPMT alleles (homozygous or compound heterozygous TPMT deficient individuals) are at very high risk for life-threatening myelosuppression, due to very high TGNs, if given conventional doses of mercaptopurine (or azathioprine). Despite having higher TGNs than wild-type patients, only about 30–60% of TPMT heterozygotes cannot tolerate full doses of mercaptopurine or azathioprine (8, 10, 11). Good thiopurine tolerance in some heterozygotes may be because although they have higher TGNs than homozygous wild-type patients, they have lower concentrations (and thus fewer toxic effects) of the MeMPNs than do normal metabolizers, which may offset the toxic effects of having higher TGNs. Thus, there is less of a consensus over how to dose azathioprine and mercaptopurine in patients who are heterozygous for TPMT compared to those that are homozygous, although they are at a higher risk for toxicity compared to patients carrying two normal function alleles (12).
Figure 1:
Metabolism of azathioprine, thioguanine, and mercaptopurine (41). Permission has been given by PharmGKB and Stanford to use figure (https://www.pharmgkb.org/pathway/PA2040). Pathway images and data are available under a Creative Commons BY-SA 4.0 license.
Although there is lower affinity between thioguanine and TPMT than between mercaptopurine and TPMT, TPMT significantly affects thioguanine pharmacokinetics and its cytotoxic effects (12–16). Thioguanine is directly metabolized by TPMT to inactive methylthioguanine base, leaving less drug available for anabolism by HPRT and other enzymes to active TGN metabolites. There is not an analogous secondary metabolite of thioguanine to undergo activation via TPMT (i.e. there are no methylTIMP or methylmercaptopurine nucleotides). As a result, patients receiving thioguanine are able to tolerate substantially higher TGN concentrations than do those receiving mercaptopurine or azathioprine (15). Within each TPMT phenotypic group, the initial recommended relative dosage decreases are similar for thioguanine, mercaptopurine, and azathioprine (Table 2).
Table 2.
Recommended Dosing of Thiopurines by TPMT phenotype
| Mercaptopurine | Azathioprine | Thioguanine | ||||||
|---|---|---|---|---|---|---|---|---|
| Phenotype | Implications for mercaptopurine and azathioprine phenotypic measures | Dosing recommendations for mercaptopurine |
Classification of
recommendations |
Dosing recommendations for azathioprine |
Classification of
recommendations |
Implications for thioguanine phenotypic measures | Dosing recommendations for thioguanine |
Classification of
recommendations |
| TPMT Normal metabolizer | Lower concentrations of TGN metabolites,
higher MeTIMP, this is the ‘normal’
pattern Normal risk of thiopurine-related leukopenia, neutropenia, myelosuppression |
Start with normal starting dosea (e.g. 75 mg/m2/day or 1.5 mg/kg/day) and adjust doses of mercaptopurine (and of any other myelosuppressive therapy) without any special emphasis on mercaptopurine compared to other agents. Allow at least 2 weeks to reach steady-state after each dose adjustment (4, 27, 30). | Strong | Start with normal starting dosea (e.g. 2–3 mg/kg/day) and adjust doses of azathioprine based on disease-specific guidelines. Allow 2 weeks to reach steady-state after each dose adjustment (4, 30, 37). | Strong | Lower concentrations of TGN metabolites, but
note that TGN after thioguanine are 5–10× higher than TGN
after mercaptopurine or azathioprine Normal risk of thiopurine-related leukopenia, neutropenia, myelosuppression |
Start with normal starting dosea (e.g. 40–60 mg/m2/day) and adjust doses of thioguanine and of other myelosuppressive therapy without any special emphasis on thioguanine. Allow 2 weeks to reach steady-state after each dose adjustment (4, 16). | Strong |
|
TPMT Intermediate
metabolizer OR TPMT Possible intermediate metabolizer |
Moderate to high concentrations of TGN
metabolites; low concentrations of MeTIMP Increased risk of thiopurine-related leukopenia, neutropenia, myelosuppression |
Start with reduced starting doses
(30%−80% of normal dose) if normal starting dosea is ≥75
mg/m2/day or ≥ 1.5 mg/kg/day (e.g. start at
25–60 mg/m2/day or 0.45–1.2 mg/kg/day) and
adjust doses of mercaptopurine based on degree of myelosuppression and
disease-specific guidelines. Allow 2–4 weeks to reach
steady-state after each dose adjustment. If myelosuppression occurs, and
depending on other therapy, emphasis should be on reducing
mercaptopurine over other agents (4, 11, 15, 24, 25, 27, 30, 38, 39). If normal starting dose is already <75mg/m2/day or < 1.5mg/kg/day, dose reduction may not be recommended. |
Strong | Start with reduced starting doses (30%−80% of normal dose) if normal starting dosea is 2–3 mg/kg/day, (e.g. 0.6 – 2.4 mg/kg/day), and adjust doses of azathioprine based on degree of myelosuppression and disease-specific guidelines. Allow 2–4 weeks to reach steady-state after each dose adjustment (4, 30, 37, 38). | Strong | Moderate to high concentrations of TGN
metabolites; but note that TGN after thioguanine are 5–10×
higher than TGN after mercaptopurine or
azathioprine Increased risk of thiopurine-related leukopenia, neutropenia, myelosuppression |
Start with reduced doses (50% to 80% of normal dose) if normal starting dosea is ≥40–60 mg/m2/day (e.g. 20–48 mg/m2/day) and adjust doses of thioguanine based on degree of myelosuppression and disease-specific guidelines. Allow 2–4 weeks to reach steady-state after each dose adjustment. If myelosuppression occurs, and depending on other therapy, emphasis should be on reducing thioguanine over other agents (4, 16). | Moderate |
| TPMT Poor metabolizer | Extremely high concentrations of TGN
metabolites; fatal toxicity possible without dose decrease; no MeTIMP
metabolites Greatly increased risk of thiopurine-related leukopenia, neutropenia, myelosuppression |
For malignancy, start with drastically reduced doses (reduce daily dosea by 10-fold and reduce frequency to thrice weekly instead of daily, e.g. 10 mg/m2/day given just 3 days/week) and adjust doses of mercaptopurine based on degree of myelosuppression and disease-specific guidelines. Allow 4–6 weeks to reach steady-state after each dose adjustment. If myelosuppression occurs, emphasis should be on reducing mercaptopurine over other agents. For non-malignant conditions, consider alternative non-thiopurine immunosuppressant therapy (4, 26, 30, 38). | Strong | For non-malignant conditions, consider
alternative non-thiopurine immunosuppressant therapy. For malignancy, start with drastically reduced doses (reduce daily dosea by 10-fold and dose thrice weekly instead of daily) and adjust doses of azathioprine based on degree of myelosuppression and disease-specific guidelines. Allow 4–6 weeks to reach steady-state after each dose adjustment (28, 30, 37, 38, 40). |
Strong | Extremely high concentrations of TGN
metabolites; fatal toxicity possible without dose
decrease Greatly increased risk of thiopurine-related leukopenia, neutropenia, myelosuppression |
Start with drastically reduced doses (16) (reduce daily dosea by 10-fold and dose thrice weekly instead of daily) and adjust doses of thioguanine based on degree of myelosuppression and disease-specific guidelines. Allow 4–6 weeks to reach steady-state after each dose adjustment. If myelosuppression occurs, emphasis should be on reducing thioguanine over other agents. For non-malignant conditions, consider alternative non-thiopurine immunosuppressant therapy (4). | Strong |
Normal starting doses vary by race/ethnicity and treatment regimens. If standard dose is below normal recommended dose, dose reduction might not be recommended for intermediate metabolizers.
NUDT15.
Through agnostic genome-wide association studies, variants in NUDT15 have been identified that strongly influence thiopurine tolerance in patients with acute lymphoblastic leukemia (ALL) (17) and those with inflammatory bowel diseases (18). As a nucleoside diphosphatase, NUDT15, catalyzes the conversion of cytotoxic thioguanine triphosphate (TGTP) metabolites to the non-toxic thioguanine monophosphate (TGMP). Defects in NUDT15-mediated degradation of TGTP results in more TGTP available for incorporation into DNA (DNA-TG, the primary antileukemic metabolite (19)), thus allowing for DNA damage and apoptosis. The SNP (rs 116855232; c.415C>T) causing p.R139C was the first NUDT15 variant linked to thiopurine toxicity. It was shown that this amino acid change results in a nearly complete loss of enzymatic activity and protein stability in vitro. Patients carrying this allele showed excessive DNA-TG and severe myelosuppression (20). In children with ALL, patients homozygous for the p.R139C variant allele tolerated only 8% of the standard dose of mercaptopurine, whereas tolerated dose intensity was 63% and 83.5% for those heterozygous and wildtype for this SNP, respectively (17). While most clinical studies focused on mercaptopurine, in vitro experiments using laboratory models indicated similar influence of NUDT15 on the cytotoxicity of azathioprine and thioguanine (20). Additional variant alleles have been identified with varying prevalence among differing ancestral groups and varying degrees of functional effects (NUDT15 Allele Functionality Table and Frequency Table). The variant p.R139C has been studied most extensively in patients receiving thiopurine therapy, thus, providing the strongest evidence for clinical implementation. Subsequent studies reported additional variants, most of which are rare, and their associations with clinical thiopurine toxicity do not rise to clinical actionability at this point, even though some showed decreased NUDT15 activity in in vitro. For this reason, these variants (*4 to *9) are designated as unclear function but may be clarified as more data emerge.
Inherited TPMT deficiency is the primary genetic cause of thiopurine intolerance in Europeans and Africans, whereas risk alleles in NUDT15 explain the majority of thiopurine-related myelosuppression in Asians and have been found in Hispanics.
Genetic Test Interpretation
Genetic testing analyzes the DNA sequence at specific SNP locations in the TPMT and NUDT15 genes (Supplement). Each named star (*) allele is defined by the genotype at one or more specific loci (TPMT Allele Definition Table (21, 22) and NUDT15 Allele Definition Table (21, 23)) and is associated with a level of enzyme activity (TPMT Allele Functionality Table (21, 22) and NUDT15 Allele Functionality Table (21, 23)). Table 1 summarizes the assignment of the likely TPMT and NUDT15 phenotypes, based on the most common * allele diplotypes, and these assignments are used to link genotypes with thiopurine prescribing recommendations. Of note, the phenotype of “possible intermediate metabolizer” has been introduced to the this guideline to describe an individual carrying one uncertain/unknown function allele PLUS one known no function allele, as this individual should be treated with “at least” the same precautions as would apply to an intermediate metabolizer. Although inactivating TPMT and NUDT15 alleles have been identified in multiple populations (TPMT Frequency Table (21, 22) and NUDT15 Frequency Table (21, 23)), one of the limitations inherent in a commercial genotype-only test is that rare or previously undiscovered variants may not be included.
Table 1.
Assignment of likely TPMT and NUDT15 phenotypes based on genotypes
| Assignment of likely TPMT phenotypes based on genotypes | ||
|---|---|---|
| Likely Phenotype | Genotypes | Examples of diplotypes |
| Normal metabolizer | an individual carrying normal function alleles | *1/*1 |
| Intermediate metabolizer | an individual carrying one normal function allele PLUS one no function allele | *1/*2, *1/*3A, *1/*3B, *1/*3C, *1/*4 |
| Possible Intermediate metabolizer | an individual carrying one uncertain/unknown function allele PLUS one no function allele | *2/*8, *3A/*7 |
| Poor metabolizer | an individual carrying two no function alleles | *3A/*3A, *2/*3A, *3A/*3C, *3C/*4, *2/*3C, *3A/*4 |
| Indeterminate | An individual carrying two uncertain/unknown
function alleles OR one normal function allele plus one uncertain allele function allele |
*6/*8 *1/*8 |
| Assignment of likely NUDT15 phenotypes based on genotypes | ||
| Normal metabolizer | an individual carrying two normal function alleles | *1/*1 |
| Intermediate metabolizer | an individual carrying one normal function allele PLUS one no function allele | *1/*2, *1/*3 |
| Possible Intermediate metabolizer | an individual carrying one uncertain function allele PLUS one no function allele | *2/*5, *3/*6 |
| Poor metabolizer | an individual carrying two no function alleles | *2/*2, *2/*3, *3/*3 |
| Indeterminate | one normal function allele PLUS one uncertain
function allele OR two uncertain function alleles |
*1/*4,
*1/*5 *4/*5, *5/*6 |
Available Genetic Test Options
See Supplementary material and the Genetic Testing Registry (https://www.ncbi.nlm.nih.gov/gtr/) for more information on commercially available clinical testing options.
Incidental findings
There are no diseases or phenotypic traits that have been linked to variation in TPMT or NUDT15 in the absence of thiopurine treatment (2).
Linking genetic variability to variability in drug-related phenotypes
There is substantial evidence linking TPMT and NUDT15 genotype with phenotypic variability (see Table S1). Pre-emptive dose adjustments based on TPMT genotype have reduced thiopurine-induced adverse effects without compromising desired antitumor and immunosuppressive therapeutic effects in several clinical settings (Table S1). Similarly, retrospective studies strongly indicate that patients with loss-of-function NUDT15 alleles are at excessive risk of thiopurine toxicity if the standard dose is administered. This body of evidence, rather than randomized clinical trials, provides the basis for most of the dosing recommendations in Tables 2 and 3.
Table 3.
Recommended Dosing of Thiopurines by NUDT15 phenotype
| Mercaptopurine | Azathioprine | Thioguanine | |||||
|---|---|---|---|---|---|---|---|
| Phenotype | Implications for thiopurine phenotypic measures | Dosing recommendations for mercaptopurine |
Classification of
strong |
Dosing recommendations for azathioprine |
Classification of
recommendations |
Dosing recommendations for thioguanine |
Classification of
recommendations |
| NUDT15 Normal metabolizer | Normal risk of thiopurine-related leukopenia, neutropenia, myelosuppression | Start with normal starting dosea (e.g., 75mg/m2/day or 1.5mg/kg/day) and adjust doses of mercaptopurine (and of any other myelosuppressive therapy) without any special emphasis on mercaptopurine compared to other agents. Allow at least 2 weeks to reach steady-state after each dose adjustment (4, 27, 30). | Strong | Start with normal starting dosea (e.g., 2–3 mg/kg/day) and adjust doses of azathioprine based on disease-specific guidelines. Allow 2 weeks to reach steady-state after each dose adjustment (4, 30, 37). | Strong | Start with normal starting dosea (40–60 mg/day). Adjust doses of thioguanine and of other myelosuppressive therapy without any special emphasis on thioguanine. Allow 2 weeks to reach steady-state after each dose adjustment (4, 16). | Strong |
|
NUDT15 Intermediate
metabolizer OR Possible NUDT15 Intermediate metabolizer |
Increased risk of thiopurine-related leukopenia, neutropenia, myelosuppression | Start with reduced starting doses
(30%−80% of normal dose) if normal starting dosea is ≥75
mg/m2/day or ≥ 1.5 mg/kg/day (e.g. start at
25–60 mg/m2/day or 0.45–1.2 mg/kg/day) and
adjust doses of mercaptopurine based on degree of myelosuppression and
disease-specific guidelines. Allow 2–4 weeks to reach
steady-state after each dose adjustment. If myelosuppression occurs, and
depending on other therapy, emphasis should be on reducing
mercaptopurine over other agents (4, 11, 15, 24, 25, 27, 30, 38, 39). If normal starting dose is already <75mg/m2/day or < 1.5mg/kg/day, dose reduction may not be recommended. |
Strong | Start with reduced starting doses (30%−80% of normal dose) if normal starting dosea is 2–3 mg/kg/day, (e.g. 0.6 – 2.4 mg/kg/day), and adjust doses of azathioprine based on degree of myelosuppression and disease-specific guidelines. Allow 2–4 weeks to reach steady-state after each dose adjustment (4, 30, 37, 38). | Strong | Start with reduced doses (50% to 80% of normal dose) if normal starting dosea is ≥40–60 mg/m2/day (e.g. 20–48 mg/m2/day) and adjust doses of thioguanine based on degree of myelosuppression and disease-specific guidelines. Allow 2–4 weeks to reach steady-state after each dose adjustment. If myelosuppression occurs, and depending on other therapy, emphasis should be on reducing thioguanine over other agents (4, 16). | Moderate |
| NUDT15 Poor metabolizer | Greatly increased risk of thiopurine-related leukopenia, neutropenia, myelosuppression | For malignancy, initiate dose at 10
mg/m2/day and adjust dose based on myelosuppression and
disease-specific guidelines. Allow 4–6 weeks to reach steady
state after each dose adjustment. If myelosuppression occurs, emphasis
should be on reducing mercaptopurine over other
agents. For non-malignant conditions, consider alternative non-thiopurine immunosuppressant therapy (4, 26, 30, 38). |
Strong | For non-malignant conditions, consider
alternative non-thiopurine immunosuppressant therapy. For malignant conditions, start with drastically reduced normal daily dosesa (reduce daily dose by 10-fold) and adjust doses of azathioprine based on degree of myelosuppression and disease-specific guidelines. Allow 4–6 weeks to reach steady-state after each dose adjustment (28, 30, 37, 38, 40). |
Strong | Reduce doses to 25% of normal dosea and adjust doses of thioguanine based on degree of myelosuppression and disease-specific guidelines. Allow 4–6 weeks to reach steady-state after each dose adjustment. In setting of myelosuppression, emphasis should be on reducing thioguanine over other agents. For non-malignant conditions, consider alternative non-thiopurine immunosuppressant therapy (4). | Strong |
Normal starting doses vary by race/ethnicity and treatment regimens. If standard dose is below normal recommended dose, dose reduction might not be recommended for intermediate metabolizers.
Therapeutic Recommendations
Thiopurines are used to treat malignant and non-malignant conditions, and thus the approach to dosing adjustments and the propensity to initiate therapy at higher vs. lower starting doses based on TPMT/NUDT15 status may differ depending on the clinical indication.. Thiopurines have a unique role in the treatment of many malignancies. The “normal” starting doses of thiopurines are generally “high” because they have been derived from trials which have been heavily weighted by the ~90% of the population who are wild-type for TPMT and NUDT15 and receive maximal tolerable doses by the standards of anticancer treatment (hence, full doses should be given to those who are normal metabolizers for TPMT and NUDT15, Tables 2 and 3). Because the level of thiopurine tolerance is highly correlated with genetic ancestry (17), the “normal” starting doses can also vary by geographic regions and clinical practice.
TPMT recommendation.
If starting doses are already high (e.g., 75 mg/m2 of mercaptopurine), as is true in some ALL treatment regimens, lower than normal starting doses should be considered in TPMT intermediate metabolizers (11, 15, 24, 25) and markedly reduced doses (10-fold reduction) should be used in TPMT poor metabolizers (26) (Table 2). This approach has decreased the risk of acute toxicity without compromising relapse rate in ALL (27). Even at these markedly reduced dosages, erythrocyte TGN concentrations in TPMT poor metabolizers remain well above those tolerated and achieved by the majority of patients (who are TPMT normal metabolizers) (4, 26).
In some nonmalignant conditions, alternative agents may be chosen for TPMT intermediate or poor metabolizers rather than reduced doses of thiopurines; if thiopurines are used, full starting doses are recommended for TPMT normal metabolizers, reduced doses (30–80% of target dose) in TPMT intermediate metabolizers (28, 29), and substantially reduced doses (or use of an alternative agent) in TPMT poor metabolizers (Table 2) (4, 30).
Some of the clinical data upon which dosing recommendations are based (Table 2) rely on measures of TPMT phenotype rather than genotype; however, because TPMT genotype is strongly linked to TPMT phenotype (5–7, 31), these recommendations apply regardless of the method used to assess TPMT status.
NUDT15 recommendation.
Similar to TPMT, tolerated mercaptopurine dosage is also correlated with the number of non-functional alleles of the NUDT15 gene (17, 18). In fact, the degree of thiopurine intolerance (e.g., for mercaptopurine) is also largely comparable between carriers of TPMT vs. NUDT15 decreased function alleles (17), although there remains a paucity of multi-ethnic studies examining both TPMT and NUDT15 variants. Therefore, our NUDT15 recommendations parallel those for TPMT. For NUDT15 normal metabolizers (NUDT15*1/*1), starting doses do not need to be altered. For NUDT15 intermediate metabolizers (e.g., NUDT15*1/*3, Table 2), reduced starting doses should be considered to minimize toxicity, particularly if the starting doses is high (e.g., 75 mg/m2/day for mercaptopurine). For NUDT15 poor metabolizers (e.g., *3/*3), substantially reduced doses (e.g., 10 mg/m2/day of mercaptopurine) or the use of an alternative agent should be used (Table 2) (20).
As for TPMT, there has been some variability in the tolerated thiopurine dosages within NUDT15 intermediate metabolizers, with a minority of individuals who do not seem to require significant dose reduction (17, 20). Therefore, genotype-guided prescribing recommendations apply primarily to starting doses; subsequent dosing adjustments should be made based on close monitoring of clinical myelosuppression (or disease-specific guidelines). In contrast, a full dose of mercaptopurine poses a severe risk of prolonged hematopoietic toxicity in NUDT15 poor metabolizers and preemptive dose reductions are strongly recommended (32, 33).
The NUDT15 poor metabolizer phenotype is observed at a frequency of about one in every 50 patients of East Asian descent, which is more common than the TPMT poor metabolizer phenotype in Europeans, and thus genotyping NUDT15 in the Asian populations may be of particular clinical importance. NUDT15 deficiency is also more prevalent in individuals of Hispanic ethnicity, particularly those with high levels of Native American genetic ancestry (17).
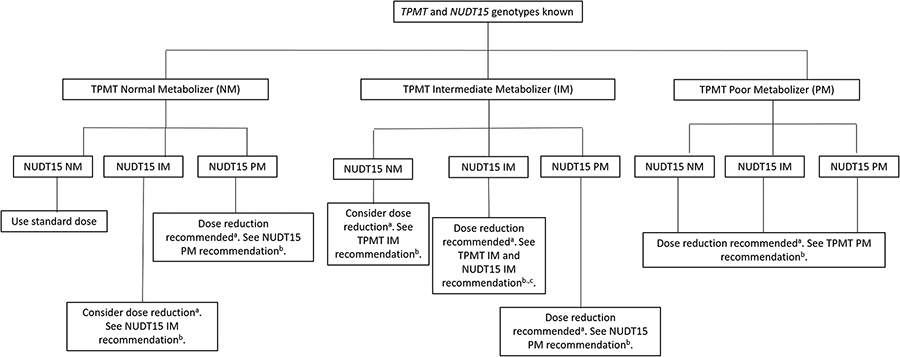
TPMT and NUDT15 recommendation.
Figure 2 outlines the recommended course of action if both TPMT and NUDT15 genotypes are known. There have been reports of patients with intermediate metabolizer status for both TPMT and NUDT15 (i.e., compound intermediate metabolizers), and there was a trend for a lower thiopurine tolerance in these individuals compared to intermediate metabolizers for only TPMT or NUDT15. The two genes are independent: the likelihood of an individual being an intermediate metabolizer for both genes depends upon the population frequencies for variant alleles. For example, given estimates of no function alleles for NUDT15 of 11% and of no function alleles for TPMT of 2%, the frequency of the compound intermediate phenotype is estimated at 0.2%. However, the evidence for a different starting dosage recommendation for the compound intermediate metabolizers remains limited.
Figure 2.
Recommended Starting Doses of Thiopurines by TPMT and NUDT15 phenotype
aWhether a dose reduction is recommended from the starting dose depends on the level of the standard starting dose; for example, if the standard starting dose of mercaptopurine is 75 mg/m2/day or higher, then a lower starting dose may be considered in intermediate metabolizers and would be recommended in poor metabolizers, whereas if the starting dose is 50 mg/m2/day or lower, a reduced starting dose may not be necessary in intermediate metabolizers.
bSee Table 2 for recommendation.
cFor patients who are IM for both TPMT and NUDT15, further dose reduction might be needed compared to those who are only IM with respect to one gene (TPMT or NUDT15).
Recommendations for Incidental Findings
Not applicable.
Other considerations
If test results are available for only one gene (TPMT or NUDT15, but not both), prescribing recommendations based on that gene’s results may be implemented, with the caveat that the other gene’s results are missing and may have important implications. The higher frequency of decreased function NUDT15 variants among individuals of Asian and Hispanic backgrounds and of TPMT variants in those with European and African backgrounds should be considered. In addition, there may be other reasons underlying poor tolerance to thiopurines that are not related to TPMT or to NUDT15 genetic variation.
Complementary clinical laboratory tests are available to measure thiopurine metabolites in erythrocytes: TGNs (for mercaptopurine, azathioprine, and thioguanine) and MeMPNs (or MeTIMP) for those on mercaptopurine or azathioprine (see Supplement for details on associations with TPMT). Erythrocyte TGNs or MeMPNs are not related to NUDT15 genotypes (34–36) because clinical assays do not distinguish among the mono-, di-, and tri-phosphate forms of active TGNs, but there is evidence that intermediate and poor metabolizers for NUDT15 accumulate higher level of DNA-TG than normal metabolizers given the same mercaptopurine dosage (20). Thus, currently available erythrocyte therapeutic drug monitoring tests do not distinguish NUDT15 metabolizer phenotypes.
Implementation of this guideline.
The guideline supplement contains resources that can be used within electronic health records (EHRs) to assist clinicians in applying genetic information to patient care for the purpose of drug therapy optimization (see Resources to incorporate pharmacogenetics into an electronic health record with clinical decision support sections of supplement).
POTENTIAL BENEFITS AND RISKS FOR THE PATIENT
The benefits of pre-emptive TPMT testing are that doses that are customized based on TPMT status reduce the likelihood of acute myelosuppression without compromising disease control (4, 8, 24, 25). The risks would be that a proportion of TPMT intermediate metabolizers may spend a period of time at lower thiopurine doses than they can eventually tolerate, because only ~30–60% of TPMT heterozygous patients receiving conventional thiopurine doses experience severe myelosuppression (4, 8, 11). However, because steady state is reached in 2–4 weeks, any period of “under-dosing” should be short, and using this approach, at least in ALL and in inflammatory bowel disease, outcomes were not compromised (4, 8, 24, 25, 28).
Similar benefits are expected with pre-emptive NUDT15 genotyping, especially for Asian patients, given that these variants have comparable effects as risk alleles in TPMT. At least in ALL, leukemia cells with loss-of-function NUDT15 alleles are also more sensitive to mercaptopurine (20) and thus in theory NUDT15 genotyped guided dosing would not compromise anti-leukemic efficacy of this drug.
A possible risk to the patient is an error in genotyping (4). Some TPMT and/or NUDT15 variants may not be included in the genotype test used and patients with these variants may be assigned a “wild-type” (*1) genotype by default. Thus, an assigned “wild-type” allele could potentially harbor a no or decreased function variant. Because genotypes are life-long test results, any such error could stay in the medical record for the life of the patient.
CAVEATS: APPROPRIATE USE AND/OR POTENTIAL MISUSE OF GENETIC TESTS
Most of the time, thiopurines are given orally daily for a period of at least several months. Genotype-based starting doses are just that—starting doses, and in most diseases, titration to the desired degree (or lack thereof) of myelosuppression is required. Thus, clinicians must continue to evaluate markers of disease progression and/or of myelosuppression to adjust thiopurine doses up or down from the genotype-directed starting doses. One caveat is that some serious long-term adverse effects (secondary tumors) have been associated with defective TPMT activity without necessarily causing serious acute myelosuppression; whether capping doses of thiopurines in those with a TPMT defect will decrease the risk of the late effect of secondary cancer is not known. Some adverse reactions to thiopurines, such as pancreatitis and hepatotoxicity, are not related to low TPMT activity.
The discovery and clinical implementation of NUDT15 variants in thiopurine dosing is relatively recent and the exact impact of NUDT15 genotype-guided dose adjustments on toxicity and efficacy are less clear compared to TPMT.
Supplementary Material
Clinical Pharmacogenetics Implementation Consortium (CPIC) guideline for thiopurine dosing based on TPMT and NUDT15 genotypes: 2018 update
CPIC Thiopurine Supplemental Tables
ACKNOWLEDGEMENTS
We acknowledge the critical input of members of the Clinical Pharmacogenetics Implementation Consortium (CPIC) of the Pharmacogenomics Research Network (PGRN), funded by the National Institutes of Health (CPIC (R24GM115264) and PharmGKB (R24GM61374)) and the PharmVar TPMT and NUDT15 expert panels especially Andrea Gaedigk, Ph.D. This work is also supported by the Robert Bosch Foundation, Stuttgart, Germany.
FUNDING
This guideline is funded by the National Institutes of Health (CPIC (R24GM115264) and PharmGKB (R24GM61374)).
Footnotes
Disclaimer
Clinical Pharmacogenetics Implementation Consortium (CPIC) guidelines reflect expert consensus based on clinical evidence and peer-reviewed literature available at the time they are written and are intended only to assist clinicians in decision-making, as well as to identify questions for further research. New evidence may have emerged since the time a guideline was submitted for publication. Guidelines are updated periodically on https://cpicpgx.org/guidelines/ and it is the responsibility of the guideline user to consult this website for updates. Guidelines are limited in scope and are not applicable to interventions or diseases not specifically identified. Guidelines do not account for all individual variation among patients and cannot be considered inclusive of all proper methods of care or exclusive of other treatments. It remains the responsibility of the health care provider to determine the best course of treatment for the patient. Adherence to any guideline is voluntary, with the ultimate determination regarding its application to be solely made by the clinician and the patient. CPIC assumes no responsibility for any injury to persons or damage to property related to any use of CPIC’s guidelines, or for any errors or omissions.
CONFLICT OF INTEREST
The authors declared no competing interests for this work.
REFERENCES
- (1).Sandborn WJ Pharmacogenomics and IBD: TPMT and thiopurines. Inflamm Bowel Dis 10 Suppl 1, S35–7 (2004). [DOI] [PubMed] [Google Scholar]
- (2).Evans WE Pharmacogenetics of thiopurine S-methyltransferase and thiopurine therapy. Ther Drug Monit 26, 186–91 (2004). [DOI] [PubMed] [Google Scholar]
- (3).Weinshilboum R Inheritance and drug response. N Engl J Med 348, 529–37 (2003). [DOI] [PubMed] [Google Scholar]
- (4).Ford LT & Berg JD Thiopurine S-methyltransferase (TPMT) assessment prior to starting thiopurine drug treatment; a pharmacogenomic test whose time has come. J Clin Pathol 63, 288–95 (2010). [DOI] [PubMed] [Google Scholar]
- (5).Schaeffeler E et al. Comprehensive analysis of thiopurine S-methyltransferase phenotype-genotype correlation in a large population of German-Caucasians and identification of novel TPMT variants. Pharmacogenetics 14, 407–17 (2004). [DOI] [PubMed] [Google Scholar]
- (6).Yates CR et al. Molecular diagnosis of thiopurine S-methyltransferase deficiency: genetic basis for azathioprine and mercaptopurine intolerance. Ann Intern Med 126, 608–14 (1997). [DOI] [PubMed] [Google Scholar]
- (7).Liu C et al. Genomewide Approach Validates Thiopurine Methyltransferase Activity Is a Monogenic Pharmacogenomic Trait. Clin Pharmacol Ther 101, 373–81 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- (8).Relling MV et al. Mercaptopurine therapy intolerance and heterozygosity at the thiopurine S-methyltransferase gene locus. J Natl Cancer Inst 91, 2001–8 (1999). [DOI] [PubMed] [Google Scholar]
- (9).Nygaard U, Toft N & Schmiegelow K Methylated metabolites of 6-mercaptopurine are associated with hepatotoxicity. Clin Pharmacol Ther 75, 274–81 (2004). [DOI] [PubMed] [Google Scholar]
- (10).Evans WE et al. Preponderance of thiopurine S-methyltransferase deficiency and heterozygosity among patients intolerant to mercaptopurine or azathioprine. J Clin Oncol 19, 2293–301 (2001). [DOI] [PubMed] [Google Scholar]
- (11).Stocco G et al. Genetic polymorphism of inosine triphosphate pyrophosphatase is a determinant of mercaptopurine metabolism and toxicity during treatment for acute lymphoblastic leukemia. Clin Pharmacol Ther 85, 164–72 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- (12).Higgs JE, Payne K, Roberts C & Newman WG Are patients with intermediate TPMT activity at increased risk of myelosuppression when taking thiopurine medications? Pharmacogenomics 11, 177–88. [DOI] [PubMed] [Google Scholar]
- (13).Hartford C et al. Differential effects of targeted disruption of thiopurine methyltransferase on mercaptopurine and thioguanine pharmacodynamics. Cancer Res 67, 4965–72 (2007). [DOI] [PubMed] [Google Scholar]
- (14).Hosni-Ahmed A, Barnes JD, Wan J & Jones TS Thiopurine methyltransferase predicts the extent of cytotoxicty and DNA damage in astroglial cells after thioguanine exposure. PLoS One 6, e29163 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- (15).Lennard L & Lilleyman JS Individualizing therapy with 6-mercaptopurine and 6-thioguanine related to the thiopurine methyltransferase genetic polymorphism. Ther Drug Monit 18, 328–34 (1996). [DOI] [PubMed] [Google Scholar]
- (16).McBride KL, Gilchrist GS, Smithson WA, Weinshilboum RM & Szumlanski CL Severe 6-thioguanine-induced marrow aplasia in a child with acute lymphoblastic leukemia and inhibited thiopurine methyltransferase deficiency. J Pediatr Hematol Oncol 22, 441–5 (2000). [DOI] [PubMed] [Google Scholar]
- (17).Yang JJ et al. Inherited NUDT15 variant is a genetic determinant of mercaptopurine intolerance in children with acute lymphoblastic leukemia. J Clin Oncol 33, 1235–42 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- (18).Yang SK et al. A common missense variant in NUDT15 confers susceptibility to thiopurine-induced leukopenia. Nat Genet 46, 1017–20 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- (19).Nielsen SN et al. DNA-thioguanine nucleotide concentration and relapse-free survival during maintenance therapy of childhood acute lymphoblastic leukaemia (NOPHO ALL2008): a prospective substudy of a phase 3 trial. Lancet Oncol 18, 515–24 (2017). [DOI] [PubMed] [Google Scholar]
- (20).Moriyama T et al. NUDT15 polymorphisms alter thiopurine metabolism and hematopoietic toxicity. Nat Genet 48, 367–73 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- (21).CPIC. CPIC Guideline for Thiopurines and TPMT and NUDT15. <https://cpicpgx.org/guidelines/guideline-for-thiopurines-and-tpmt/>.
- (22).PharmGKB. Gene Reference Materials for TPMT. <https://www.pharmgkb.org/page/tpmtRefMaterials>. Accessed January 1 2018.
- (23).PharmGKB. Gene Reference Materials for NUDT15. <https://www.pharmgkb.org/page/nudt15RefMaterials>.
- (24).Schmiegelow K et al. Thiopurine methyltransferase activity is related to the risk of relapse of childhood acute lymphoblastic leukemia: results from the NOPHO ALL-92 study. Leukemia 23, 557–64 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- (25).Schmiegelow K et al. Long-term results of NOPHO ALL-92 and ALL-2000 studies of childhood acute lymphoblastic leukemia. Leukemia 24, 345–54 (2010). [DOI] [PubMed] [Google Scholar]
- (26).Evans WE, Horner M, Chu YQ, Kalwinsky D & Roberts WM Altered mercaptopurine metabolism, toxic effects, and dosage requirement in a thiopurine methyltransferase-deficient child with acute lymphocytic leukemia. J Pediatr 119, 985–9 (1991). [DOI] [PubMed] [Google Scholar]
- (27).Relling MV, Pui CH, Cheng C & Evans WE Thiopurine methyltransferase in acute lymphoblastic leukemia. Blood 107, 843–4 (2006). [DOI] [PubMed] [Google Scholar]
- (28).Meggitt SJ, Gray JC & Reynolds NJ Azathioprine dosed by thiopurine methyltransferase activity for moderate-to-severe atopic eczema: a double-blind, randomised controlled trial. Lancet 367, 839–46 (2006). [DOI] [PubMed] [Google Scholar]
- (29).Coenen MJ et al. Identification of Patients With Variants in TPMT and Dose Reduction Reduces Hematologic Events During Thiopurine Treatment of Inflammatory Bowel Disease. Gastroenterology 149, 907–17e7 (2015). [DOI] [PubMed] [Google Scholar]
- (30).Sandborn WJ Rational dosing of azathioprine and 6-mercaptopurine. Gut 48, 591–2 (2001). [DOI] [PMC free article] [PubMed] [Google Scholar]
- (31).Tamm R et al. Polymorphic variation in TPMT is the principal determinant of TPMT phenotype: A meta-analysis of three genome-wide association studies. Clin Pharmacol Ther 101, 684–95 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- (32).Zhu Y et al. Combination of common and novel rare NUDT15 variants improves predictive sensitivity of thiopurine-induced leukopenia in children with acute lymphoblastic leukemia. Haematologica, (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- (33).Ailing Z, Jing Y, Jingli L, Yun X & Xiaojian Z Further evidence that a variant of the gene NUDT15 may be an important predictor of azathioprine-induced toxicity in Chinese subjects: a case report. J Clin Pharm Ther 41, 572–4 (2016). [DOI] [PubMed] [Google Scholar]
- (34).Moriyama T et al. The effects of inherited NUDT15 polymorphisms on thiopurine active metabolites in Japanese children with acute lymphoblastic leukemia. Pharmacogenet Genomics 27, 236–9 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- (35).Lee JH et al. Measurements of 6-thioguanine nucleotide levels with TPMT and NUDT15 genotyping in patients with Crohn’s disease. PLoS One 12, e0188925 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- (36).Asada A et al. NUDT15 R139C-related thiopurine leukocytopenia is mediated by 6-thioguanine nucleotide-independent mechanism in Japanese patients with inflammatory bowel disease. J Gastroenterol 51, 22–9 (2016). [DOI] [PubMed] [Google Scholar]
- (37).Anstey AV, Wakelin S, Reynolds NJ, British Association of Dermatologists Therapy, G. & Audit, S. Guidelines for prescribing azathioprine in dermatology. Br J Dermatol 151, 1123–32 (2004). [DOI] [PubMed] [Google Scholar]
- (38).Lichtenstein GR, Abreu MT, Cohen R, Tremaine W & American Gastroenterological A. American Gastroenterological Association Institute technical review on corticosteroids, immunomodulators, and infliximab in inflammatory bowel disease. Gastroenterology 130, 940–87 (2006). [DOI] [PubMed] [Google Scholar]
- (39).Krynetski EY & Evans WE Pharmacogenetics of cancer therapy: getting personal. Am J Hum Genet 63, 11–6 (1998). [DOI] [PMC free article] [PubMed] [Google Scholar]
- (40).Kaskas BA et al. Safe treatment of thiopurine S-methyltransferase deficient Crohn’s disease patients with azathioprine. Gut 52, 140–2 (2003). [DOI] [PMC free article] [PubMed] [Google Scholar]
- (41).Zaza G et al. Thiopurine pathway. Pharmacogenet Genomics 20, 573–4 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.