Abstract
Background
Significant increases in the prevalence of obesity have been observed among patients with peritoneal dialysis (PD). The impact of body mass index (BMI) on survival remains unknown in Korean PD patients.
Methods
Among data of 80,674 patients on PD acquired from the Insan Memorial ESRD Registry database for the years 1985 to 2014, 6,071 cases were analyzed. Subjects were classified by baseline BMI; < 21.19 kg/m2 (quartile 1, n = 1,518), 21.19 to 23.18 kg/m2 (quartile 2, reference; n = 1,453), 23.19 to 25.71 kg/m2 (quartile 3, n = 1,583), and > 25.71 kg/m2 (quartile 4, n = 1,517).
Results
Mean age was 65.8 years, and baseline BMI was 23.57 kg/m2. Numbers of male and diabetic patients were 3,492 (57.5%) and 2,192 (36.1%), respectively. Among 6,071 cases, 2,229 (36.7%) all-cause deaths occurred. As a whole, Kaplan–Meier survival curves according to BMI quartiles was significantly different (P = 0.001). All-cause mortality was significantly higher in quartile 4 than in the reference (hazard ratio [HR] = 1.154, 95% confidence interval [CI], 1.025–1.300; P = 0.018). There was no statistical difference in all-cause mortality among BMI quartiles in diabetic patients on PD. In non-diabetic patients, all-cause mortality of quartiles 1 and 3 was not different from the reference, but the HR was 1.176 times higher in quartile 4 (95% CI, 1.024–1.350; P = 0.022).
Conclusion
Baseline BMI > 25.71 kg/m2 seems to be an important risk factor for all-cause mortality in Korean PD patients.
Keywords: Body mass index, Diabetes mellitus, Mortality, Peritoneal dialysis
Introduction
Peritoneal dialysis (PD) is a maintenance renal replacement therapy for patients with end-stage renal disease (ESRD) [1]. Unlike hemodialysis (HD), there is no need to visit the hospital frequently, there is no pain due to needle puncture, and residual renal function is maintained for a long time on PD. However, PD-related complications such as peritonitis or metabolic syndrome can occur [2].
Significant increases in the prevalence of obesity have been observed among patients with ESRD [3,4]. Very low body mass index (BMI) and high BMI in the general population are associated with increased mortality [5]. In patients with HD, the reverse pattern is seen [6]. However, it is controversial whether this trend is the same in PD as it is in HD [7], and it has not been well investigated in Korean ESRD patients on PD [8].
The Insan Memorial ESRD Registry (ImESRDR-KSN) is the largest Korean ESRD registry and has been collecting data since 1985. To evaluate the impact of BMI at the initiation of PD on mortality in Korean PD patients, we analyzed ImESRDR-KSN data from 1985 to 2014.
Methods
Study participants and data collection
ImESRDR-KSN is a nationwide database of patients with ESRD, which was launched in 1985 by the ESRD registry committee of the Korean Society of Nephrology (KSN). The registry data is updated yearly. For each patient on HD, PD, or who had undergone kidney transplantation, the start date of renal replacement therapy and new information from the past 1 year, such as the date of HD or PD initiation, newly developed comorbid diseases, adequacy data, laboratory data, and outcome (alive, dead, transferred to another modality or hospital) are updated. As registry enrollment is voluntarily updated by members of the KSN, the ESRD registry covers about two-thirds of all patients on dialysis in Korea [9,10]. Among 80,674 patients on PD in the ImESRDR-KSN registry, inclusion criteria for our study were as follows: 1) age ≥ 18 years; 2) patients on PD between 1985 and 2014, and 3) patients whose first registered record had at minimum data about height, weight, PD date, and primary kidney disease and whose final record had at least outcome (alive or dead) and where applicable, date of death. Among possible cases identified (10,495), 4,424 cases with insufficient data or no BMI data were excluded. Finally, 6,071 cases were included (Supplementary Fig. 1; available online).
Baseline BMI was calculated as weight (kg)/height2 (m2) of the first registered data. Age, sex, presence or absence of diabetes mellitus (DM), systolic blood pressure (SBP), diastolic blood pressure (DBP), presence of residual renal function, duration of dialysis, normalized protein catabolic rate, total body water (TBW), protein equivalent of total nitrogen appearance (PNA), weekly total Kt/Vurea and creatinine clearance (CCr) were recorded. In addition, laboratory findings such as hemoglobin (Hb), alkaline phosphatase, albumin, calcium, phosphorus, aspartate aminotransferase, parathyroid hormone (PTH), and total cholesterol were recorded. TBW, PNA, weekly total Kt/Vurea, and CCr were calculated using the following equations:
Male TBW (L) = 2.447 − (0.09516 × age [year]) + (0.1074 × height [cm]) + (0.3362 × weight [kg])
Female TBW (L) = −2.097 + (0.1069 × height [cm]) + (0.2466 × weight [kg]) [11]
PNA (g/day) = 10.76 × (0.69 × 0.00001 × ((amount of urine × 24/time of corrected urine) × (urine urea + dialysate volume × dialysate urea) + 1.46) + dialysate protein × dialysate volume × 0.00001
Weekly total Kt/V = (dialysate urea × 24-hour dialysate volume × 7)/(blood urea nitrogen × TBW × 1,000), and
Weekly total CCr (L/wk) = 7 × {(dialysate creatinine × 24-hour dialysate volume) + (urine creatinine × urine volume × 24 / time of corrected urine)}/(serum creatinine × 1,000)
Subjects were classified into four groups according to the quartile of baseline BMI: quartile 1, < 21.19 kg/m2; quartile 2, 21.19–23.18 kg/m2; quartile 3, 23.19–25.71 kg/m2; and quartile 4 > 25.71 kg/m2. Quartile 2 was used as the reference quartile.
Statistical analysis
Continuous variables are presented as means ± standard deviations or medians with interquartile ranges, as appropriate. Categorical variables are expressed as numbers and percentages. Demographic characteristics and covariates of the four groups were compared using the Pearson chi-square test for categorical variables and one-way analysis of variance for continuous variables. Kaplan–Meier analysis was used to evaluate the change in survival among BMI groups, and Kaplan–Meier curves were compared using the log-rank test. Cox proportional hazard analysis was performed to evaluate independent associations among BMI quartiles and the long-term risk of death among patients on PD; data are presented as hazard ratios (HRs) and 95% confidence intervals (CIs). The proportional hazard assumption for the Cox model was tested using log-minus-log plots. Model 1 used the crude model and model 2 used only age and sex. We adjusted the regression model with available parameters known to be related to mortality. We also used the Bonferroni adjustment for multiple comparisons due to subgroup analyses. However, some parameters had too few patients (e.g., only 100 patients), so we excluded parameters that were not statistically significant when the data were adjusted. Therefore, among the independent variables, parameters related to mortality were included from among the parameters for which the number of patients was close to that of the dependent variable [12–16]. Finally, the following variables were adjusted in model 3: model 2 + primary disease, presence of DM, serum albumin level, serum Hb level, total cholesterol level, phosphorus level, SBP, DBP, HbA1c level, TBW, PNA, and weekly total Kt/Vurea and CCr. Analyses were performed using the Statistical Package for Social Sciences (SPSS®) software, version 18.0 (IBM Corp., Armonk, USA). All statistical tests were two-tailed, and P < 0.05 was considered significant.
Results
Baseline demographic, clinical, and laboratory characteristics
Among 6,071 cases, mean age was 65.8 ± 13.7 years, and BMI was 23.57 ± 3.63 kg/m2 (Table 1). Numbers of male and diabetic patients were 3,492 (57.5%) and 2,192 (36.1%), respectively. Fifty-three patients had peritonitis. The number of patients who were converted to kidney transplants was 43 (0.7%). The number of patients who were converted to HD was 1,774. Of these, 393 patients (22.2%) had diabetes, and 1,381 (77.8%) did not have diabetes. The numbers of patients converted to HD were 431 (24.3%) in quartile 1, 422 (23.8%) in quartile 2, 459 (25.9%) in quartile 3, and 462 (26.0%) in quartile 4; these differences were not statistically significant. Age was advanced in quartile 3 compared to the reference quartile, but there was no difference in age between the other quartiles. Serum phosphorus values were the lowest in quartile 1 (P = 0.033). Serum cholesterol levels were highest in quartile 1, and quartile 1 showed significantly higher cholesterol level than quartile 4 (P = 0.009). In diabetic patients on PD, there were no significant differences in SBP, DBP, Hb level, albumin level, calcium level, phosphorus level, uric acid level, PNA, weekly CCr, or intact PTH level among the four quartiles.
Table 1.
Baseline characteristics of patients according to quartile of baseline body mass index
| Variable | Total patients | Quartile 1 (< 21.19 kg/m2) | Quartile 2 (21.19–23.18 kg/m2) | Quartile 3 (23.19–25.71 kg/m2) | Quartile 4 (> 25.71 kg/m2) | P value |
|---|---|---|---|---|---|---|
| Number of patients | 6,071 (100) | 1,518 (25.0) | 1,453 (24.0) | 1,583 (26.0) | 1,517 (25.0) | |
| Age (yr) | 65.8 ± 13.7 | 66.1 ± 13.3 | 64.9 ± 13.9 | 66.3 ± 13.9 | 65.8 ± 13.5 | 0.043 |
| Sex, male | 3,489 (57.5) | 870 (57.3) | 806 (55.5) | 923 (58.3) | 890 (58.7) | 0.302 |
| Comorbidity, DM | 2,190 (36.1) | 554 (36.5) | 520 (35.8) | 582 (36.8) | 534 (35.2) | 0.792 |
| Systolic BP (mmHg) | 136.8 ± 20.2 (4,378) | 136.0 ± 20.4 (1,073) | 137.2 ± 20.1 (1,055) | 137.5 ± 19.9 (1,129) | 136.6 ± 20.3 (1,121) | 0.332 |
| Diastolic BP (mmHg) | 82.2 ± 12.2 (4,376) | 82.7 ± 12.9 (1,072) | 82.3 ± 12.2 (1,055) | 82.1 ± 12.2 (1,129) | 81.8 ± 11.9 (1,120) | 0.425 |
| Hemoglobin (g/dL) | 9.3 ± 2.8 (4,807) | 9.2 ± 2.8 (1,185) | 9.3 ± 2.9 (1,159) | 9.4 ± 2.8 (1,241) | 9.4 ± 2.7 (1,223) | 0.429 |
| Albumin (g/dL) | 3.5 ± 1.0 (4,809) | 3.5 ± 0.5 (1,074) | 3.5 ± 0.5 (1,055) | 3.5 ± 0.5 (1,131) | 3.5 ± 0.5 (1,122) | 0.660 |
| Calcium (mg/dL) | 8.5 ± 0.9 (455) | 8.7 ± 0.9 (104) | 8.6 ± 1.2 (107) | 8.56 ± 0.8 (111) | 8.4 ± 0.8 (133) | 0.277 |
| Phosphorus (mg/dL) | 4.9 ± 1.6 (455) | 4.7 ± 1.4 (85) | 4.8 ± 1.6 (121) | 4.9 ± 1.8 (136) | 5.0 ± 1.7 (113) | 0.324 |
| TC (mg/dL) | 160.0 ± 48.1 (425) | 172.6 ± 47.5 (95) | 158.2 ± 48.1 (100) | 159.2 ± 47.1 (107) | 151.9 ± 47.9 (123) | 0.017 |
| Uric acid (mg/dL) | 6.7 ± 1.8 (421) | 6.5 ± 1.7 (99) | 6.8 ± 1.6 (99) | 6.7 ± 1.9 (104) | 7.0 ± 2.0 (119) | 0.157 |
| HbA1c (%) | 6.17 ± 2.68 (224) | 5.9 ± 2.9 (43) | 5.8 ± 3.0 (50) | 5.6 ± 1.9 (55) | 6.9 ± 2.4 (74) | 0.025 |
| PNA (g/d) | 59.1 ± 117.2 (5,667) | 56.5 ± 177.8 (1,435) | 59.6 ± 94.2 (1,364) | 57.7 ± 89.7 (1,464) | 62.9 ± 78.4 (1,404) | 0.487 |
| Kt/Vurea week total | 2.23 ± 7.71 (5,173) | 2.3 ± 5.1 (1,217) | 2.0 ± 2.1 (1,240) | 2.0 ± 5.2 (1,365) | 2.0 ± 2.4 (1,347) | 0.032 |
| CCr weekly (L) | 94.40 ± 255.09 (5,162) | 94.07 ± 322.19 (1,242) | 87.14 ± 188.50 (1,234) | 83.60 ± 195.16 (1,356) | 104.68 ± 289.38 (1,330) | 0.153 |
| Intact PTH (pg/mL) | 242.9 ± 213.2 (350) | 269.9 ± 262.7 (84) | 225.3 ± 205.9 (82) | 241.3 ± 185.6 (87) | 236.1 ± 194.7 (97) | 0.574 |
Data are presented as number (%) for categorical variables, and mean ± standard deviation (number) for continuous variables.
BP, blood pressure; CCr, creatinine clearance; DM, diabetes mellitus; Hb, hemoglobin; NPNA, normalized protein equivalent of total nitrogen appearance (PNA) = PNA/(total body water/0.58); PTH, parathyroid hormone; TC, total cholesterol.
Effect of baseline BMI on all-cause mortality
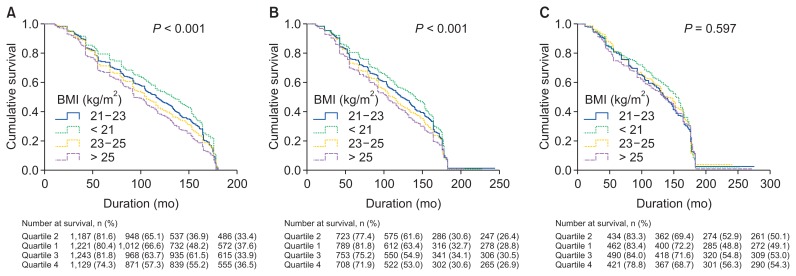
Among 6,071 cases, 2,229 (36.7%) all-cause deaths were recorded over the follow-up period. Mean follow-up period was 90.96 ± 54.34 months. Kaplan–Meier survival curves were reanalyzed for all-cause mortality according to BMI quartiles (Supplementary Fig. 2; available online). Log rank of the Kaplan–Meier survival curves of all patients according to BMI quartiles was 27.44, and the P value was < 0.001 (Fig. 1A).
Figure 1. Kaplan–Meier survival curves of patients according to body mass index (BMI) quartiles.
(A) All patients, (B) patients without diabetes mellitus (DM), and (C) patients with DM.
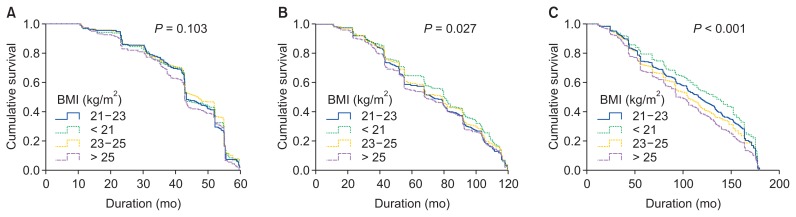
Survival curves of patients without DM were analyzed for differences in mortality at 5, 10, and 15 years (Fig. 2). There was no difference at 5 years (P = 0.103; log rank, 6.18). The 10-year survival analysis showed a significant difference among BMI quartiles (P = 0.027; log rank, 9.19). In comparison analysis, mortality was increased in quartile 4 compared to quartile 1 (P = 0.008; log rank, 6.966). Fifteen-year mortality was also significantly higher in quartile 4 than quartile 1 by about 30% (log rank, 55.56; HR = 1.309; 95% CI, 1.136–1.509; P < 0.001).
Figure 2. Kaplan–Meier survival curves in patients without diabetes mellitus according to body mass index (BMI) quartiles.
(A) At 5 years’ follow-up, (B) at 10 years’ follow-up, and (C) at 15 years’ follow-up.
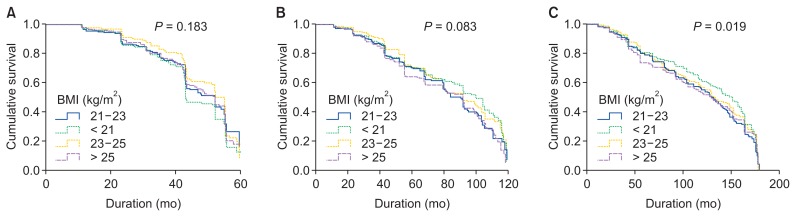
Next, we analyzed survival curves of patients with DM for differences in mortality at 5, 10, and 15 years (Fig. 3). At 5 and 10 years, there were no significant differences in survival in quartiles other than quartile 2. However, at 15 years, patients in quartile 1 showed a significant decrease in mortality compared to those in quartile 2 (P = 0.019; log rank, 5.457). A decreased BMI in diabetic patients was associated with decreased mortality.
Figure 3. Kaplan–Meier survival curves in patients with diabetes mellitus according to body mass index (BMI) quartiles.
(A) At 5 years’ follow-up, (B) at 10 years’ follow-up, and (C) at 15 years’ follow-up.
In Cox proportional hazard analysis, compared to the reference, all-cause mortality of all patients was reduced by about 10% in quartile 1 (HR = 0.91; 95% CI, 0.832–0.995; P = 0.039; Table 2). An increase in mortality of about 14% was seen in quartile 4 compared to the reference (HR = 1.140; 95% CI, 1.042–1.247; P = 0.004). Adjusting several parameters resulted in a significant increase in mortality in quartile 4 compared to the reference (HR = 1.154; 95% CI, 1.025–1.300; P = 0.018). The results of multivariate analysis showed that there were no statistically significant differences in all-cause mortality among BMI quartiles in the DM group. However, in the non-DM group, mortality was approximately 18% higher in quartile 4 than the reference (HR = 1.176; 95% CI, 1.024–1.350; P = 0.022).
Table 2.
Univariate and multivariate Cox regression analyses of mortality according to body mass index quartile
| Mortality | Crude model | Model 1 | Model 2 | ||||||
|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|||||||
| HR | 95% CI | P | HR | 95% CI | P | HR | 95% CI | P | |
| All-cause mortality | |||||||||
| Quartile 2 | Reference | Reference | Reference | ||||||
| Quartile 1 | 0.910 | 0.832–0.995 | 0.039 | 0.931 | 0.851–1.018 | 0.118 | 0.965 | 0.856–1.088 | 0.557 |
| Quartile 3 | 1.048 | 0.958–1.146 | 0.309 | 1.061 | 0.970–1.161 | 0.195 | 1.040 | 0.923–1.171 | 0.521 |
| Quartile 4 | 1.140 | 1.042–1.247 | 0.004 | 1.145 | 1.047–1.253 | 0.003 | 1.154 | 1.025–1.300 | 0.018 |
| All-cause mortality in DM patients | |||||||||
| Quartile 2 | Reference | Reference | Reference | ||||||
| Quartile 1 | 0.931 | 0.787–1.103 | 0.410 | 0.940 | 0.794–1.113 | 0.472 | 0.979 | 0.781–1.226 | 0.852 |
| Quartile 3 | 0.957 | 0.807–1.134 | 0.611 | 0.936 | 0.790–1.110 | 0.449 | 0.866 | 0.692–1.084 | 0.209 |
| Quartile 4 | 1.041 | 0.874–1.239 | 0.656 | 1.017 | 0.854–1.211 | 0.851 | 0.930 | 0.734–1.179 | 0.550 |
| All-cause mortality in non-DM patients | |||||||||
| Quartile 2 | Reference | Reference | Reference | ||||||
| Quartile 1 | 0.903 | 0.812–1.004 | 0.059 | 0.922 | 0.830–1.025 | 0.135 | 0.944 | 0.819–1.087 | 0.423 |
| Quartile 3 | 1.096 | 0.986–1.218 | 0.088 | 1.110 | 0.999–1.234 | 0.053 | 1.072 | 0.932–1.232 | 0.332 |
| Quartile 4 | 1.175 | 1.058–1.305 | 0.003 | 1.190 | 1.072–1.322 | 0.001 | 1.176 | 1.024–1.350 | 0.022 |
CI, confidence interval; DM, diabetes mellitus; HR, hazard ratio.
Model 1, multivariate model including age and gender; Model 2, multivariate model including model 1 + DM, serum albumin level, serum hemoglobin, total cholesterol, systolic blood pressure, diastolic blood pressure, HbA1c, total body water (TBW), protein equivalent of total nitrogen appearance (PNA), normalized PNA (PNA/[TBW/0.58]), urine duration, Kt/Vurea week total, and creatinine clearance weekly.
Discussion
In this study, all-cause mortality was significantly higher in Korean patients on PD in the highest baseline BMI quartile, but it was similar among patients in the other three baseline BMI quartiles. Compared to quartile 2, mortality was increased by approximately 14% in quartile 4. In particular, the impact of baseline BMI on all-cause mortality differed according to the presence or absence of DM. Multivariate analysis revealed no significant differences in all-cause mortality among BMI quartiles in patients with DM. However, in patients without DM, mortality was approximately 18% higher in quartile 4 than the reference quartile.
It remains controversial whether obesity or a high BMI in patients on PD is associated with higher mortality [17]. Several reports have suggested that obesity is associated with mortality in patients on PD. McDonald et al [18] reported that obesity at the start of PD was associated with mortality. Kiran et al [13] reported that the relative risk for mortality (adjusted for age, diabetes status, and cardiovascular disease [CVD]) was similar for normal and overweight groups, but higher for underweight and obese groups. Increased mortality in obese patients was more prominent in patients with DM than in those without DM [10]. Xiong et al [19] reported that obesity was a risk factor for CVD mortality, but not all-cause mortality.
Other studies have suggested that obesity is not associated with an increased risk of mortality in patients on PD. Snyder et al [20] reported that the association between BMI and outcome was dependent on the time interval elapsed from the initiation of PD, but that obese subjects had better survival than those with a lower BMI. Abbott et al [21] reported that patients on PD in the lowest quartile of BMI had an increased risk of dying, whereas those in the second to fourth quartiles of BMI had a virtually identical risk of death over time. de Mutsert et al [22] reported that obese patients on PD at the initiation of dialysis did not have a worse survival rate than those with a normal BMI. Fernandes et al [23] reported that being overweight or obese did not increase mortality in patients with incident PD. In Korean patients on PD, the lowest quartile of BMI was associated with higher mortality, but a higher BMI quartile was not associated with mortality when quartile 2 (21.4–23.5 kg/m2) was the reference [8]. One study reported that obesity was a risk factor for death in a subgroup of patients on PD, but not all patients on PD. In more detail, Hoogeveen et al [24] reported that obesity was not associated with increased mortality in older (≥ 65 years) dialysis patients, but younger patients with a low or very high BMI had an increased risk of dying.
In a meta-analysis, Ahmadi et al [25] reported that being underweight was associated with higher first-year mortality, and being overweight or obese was associated with lower first-year mortality; however, the association between BMI and mortality was not significant over the long-term. Liu et al [12] reported that being underweight or obese (BMI = 25.0–29.9 kg/m2) was associated with a higher risk of all-cause and CVD mortality in a meta-analysis of Asian patients undergoing PD.
The inconsistent results from these obesity studies regarding the risk of mortality are likely due to differences in study subjects and study design. There were anthropometric differences in the study subjects, such as age distribution, sex, race, and/or BMI. There were also differences in comorbidities among study subjects. In addition, classifications of BMI varied among studies, and included the WHO classification and WHO classification for Asians, or quartiles of BMI. In McDonald and colleagues’ study of 9,679 incident PD patients in the Australia and New Zealand Dialysis and Transplant Registry [18], patients were classified into one of four categories based on BMI: obese, ≥ 25.71 kg/m2; overweight, 23.19–25.71 kg/m2; normal weight, 21.19–23.18 kg/m2; and underweight, < 21.19 kg/m2 according to the Australian classification [8,21,26]. Abbott et al [21] performed a study to retrospectively analyze the survival data of 1,662 patients on PD in the USRDS Dialysis Morbidity and Mortality Study Wave II cohort for 5 years (from 1996 to 2001); in that study, mean age was 56.3 ± 15.7 years and mean BMI was 26.4 ± 5.5 kg/m2. Obese and diabetic patients comprised 22% and 49.7% of the study subjects, respectively. In de Mutsert et al’s study [22], 688 incident PD patients were selected from the Netherlands Cooperative Study on the Adequacy of Dialysis-2 cohort and followed-up for 5 years. Mean age and BMI were 53 years and 34.6 kg/m2, and obese patients accounted for 8.4% of all patients. In Fernandes et al’s retrospective observational study of data from the Brazilian Peritoneal Dialysis Multicenter Cohort Study from 2004 to 2007 [23], 1,911 patients on PD were analyzed; their mean age was 59 years and their mean BMI was 21.58 ± 3.13 kg/m2. The median follow-up duration was 34 months, and 38% of patients had DM nephropathy. BMI was classified according to the WHO classification, and obese patients accounted for 12% of the study population. Kim et al’s prospective cohort study in Korea [8] included 900 Korean patients on PD. Their mean age was 56 ± 12 years, mean BMI was 23.6 ± 3.2 kg/m2, incidence of DM was 32%, and mean follow-up duration was 24 months. These authors classified BMI by quartiles, not by the WHO classification. Kiran et al’s 8-year single-center study in Hong Kong [13] included 274 patients on PD; their mean age and BMI were 63 years and 21.97 kg/m2, respectively, 35 (12.8%) patients were obese, and the incidence of DM was 50.4%. In Xiong et al’s study of 1,263 patients on PD [19], mean age and BMI were 47.8 ± 15.0 years and 21.58 ± 3.13 kg/m2, respectively, 12.9% of patients were obese, the median follow-up duration was 25.3 months, and BMI was classified according to the WHO classification for Asian populations. Liu et al’s study [12] was a meta-analysis of seven studies that used the WHO classification for BMI in Asians. However, results were reported only for the underweight, normal, overweight, and obese I groups (25.0–29.9 kg/m2), and no data about the obese II group (BMI ≥ 30 kg/m2) were reported. Hoogeveen et al’s study [24] included 1,749 ESRD patients on HD or PD in the Netherlands from 1997 to 2004. They used the WHO classification for BMI classification, and about 10% of patients were obese.
Our results support the finding that high BMI is associated with increased mortality in patients on PD. However, some of the findings of this study are novel. PD was initiated around the early 1980s in Korea [27]. Therefore, almost all Korean patients on PD were included in the study for the following reasons: 1) ImESRDR-KSN has been active for 30 years, 2) most patients with PD were enrolled and followed in a university hospital setting, and 3) the registration rate of patients on PD from these university hospitals was high. Differences in results between our study and the previous study of Korean patients on PD [8] may be due to differences in study design, data quality, and prevalence of DM and CVD. ImESRDR-KSN data are based on annual retrospective voluntary submissions. However, complete data are lacking. Thus, among 80,674 patients on PD, data from only 6,071 patients were available for statistical analysis, despite the long study period (30 years). In Kim et al’s study [8], all data were collected prospectively. Thus, data collection was sufficient, but the follow-up duration was relatively short (24 months). Patients in our study were older than those in Kim et al’s study (mean age, 66 ± 14 years vs. 56 ± 12 years). However, mean BMI (23.57 ± 3.63 kg/m2 vs. 23.6 ± 3.2 kg/m2) and incidence of DM (36.1% vs. 32%) were similar between the two studies. Both studies classified BMI by quartiles, not by the WHO classification.
Interestingly, compared to patients with DM, obese patients (BMI > 25.7 kg/m2) without DM had a higher mortality rate than non-obese patients without DM. The mortality rate was significantly different between obese and non-obese patients without DM at approximately 10 years or more since initiation of PD. However, during the 15-year follow-up period, obese patients with DM did not have a significantly different all-cause mortality rate than non-obese patients without DM. Rather, patients with DM in quartile 1 showed a significant decrease in mortality compared to the reference group (patients with DM in quartile 2). Results are inconsistent between our study and other studies in terms of the relationship between DM status and mortality risk in Asians according to BMI. In a prospective study of 328 incident PD patients [28], underweight (BMI < 18.5 kg/m2) diabetic patients showed significantly greater mortality than normal diabetic patients. However, the HRs for mortality in overweight and obese diabetic patients were not different from that of normal diabetic patients. In non-diabetic patients on PD, there were no differences in mortality among BMI groups [29]. The lowest quartile of BMI showed higher mortality than quartile 2 (reference group) in both DM and non-DM patients, but higher quartiles of BMI (quartiles 3 and 4) did not have a significantly different mortality than the reference group. However, Zhou et al [30] reported a higher mortality risk in PD patients with BMI > 25 kg/m2, irrespective of their DM status. Kiran et al [13] showed that the relationship between BMI and mortality was U-shaped, with higher mortality in underweight and obese patients, and reported that the negative impact of obesity was more prominent in diabetic patients on PD than non-diabetic patients on PD.
The reasons for these aforementioned findings may be related to differences in subject characteristics, study duration, prevalence of DM and CVD, classification of BMI, body composition, hydration status, and patient selection bias. BMI cannot be used to differentiate the contribution of muscle mass or fat mass to body weight or differentiate central obesity from generalized obesity; thus, it may also reflect hydration status [31]. Furthermore, the mortality rate of diabetic patients on PD is worse than that of non-diabetic patients on PD [32], but recent studies showed that similar outcomes could be achieved in diabetic patients as non-diabetics if inflammation, protein energy wasting, and/or cardiovascular morbidity were controlled [33,34].
Obesity has been associated with a shorter time to transfer to HD therapy [20], higher risk for peritonitis [35], and faster decline in residual kidney function [36]. This may explain the increased mortality rate of obese patients on PD. Obesity has a negative effect on survival in patients on PD due to an increased peritonitis rate, secretion of proinflammatory cytokines by adipose tissue, and a more rapid decline in residual renal function than is seen in non-obese patients [28,31,37,38]. In addition, a glucose-based dialysis solution and polymorphisms in uncoupling protein 2 may aggravate obesity in patients undergoing PD [39,40]. Patients undergoing PD are exposed to a large amount of glucose in the PD solution, which leads to increased exposure to metabolic syndrome [41]. In diabetic patients, PD can aggravate glycemic control, and poor glycemic control is associated with increased mortality [42,43]. However, we could not evaluate the degree of glycemic control because these data were not available in the ImESRDR-KSN.
As mentioned above, a glucose-based dialysis solution may aggravate obesity in patients on PD. Indeed, 80% of patients undergoing PD showed an increase in body weight of more than 3% after 1 year in one study [23], most of which was likely due to an increase in fat mass [44]. However, patients who gained weight were not at increased risk of mortality compared to those with stable weight, regardless of their DM status [23]. Furthermore, the increase in BMI was not persistent in patients undergoing PD. During the follow-up period, there was a nonlinear increase in BMI for the first 3 years, followed by a gradual decrease in BMI over time [45].
This study had several limitations. First, all-cause mortality was analyzed rather than specific causes of mortality because of inadequate records regarding the cause of death. Accurate information on cardiovascular mortality cannot be obtained from ImESRDR-KSN data because of the lack of information on the cause of death. Second, the number of patients with a BMI ≤ 18 kg/m2, which is associated with the highest mortality rate, was very small. Third, because screening of body composition was not performed in this study, body composition related to fat, lean body mass, and overhydration could not be measured. Fourth, BMI at the single point (initiation of PD) was used for the analysis. Some may argue that a single measurement of BMI at the initiation of PD does not reflect a patient’s real BMI because most patients experience an increase in BMI after PD. However, most previous studies have used a single BMI value at baseline. Additionally, there was a non-linear increase in BMI for the first 3 years, and then there was a gradual decrease of BMI over time; the change of yearly BMI was 0.4 kg/m2 in patients undergoing PD [34], which was not a large increase compared to the change in BMI classification. Finally, as shown in Supplementary Fig. 2, the authors used available data, and of those about 80,000 initially enrolled patients, duplication and death cases and data without BMI were excluded from the study. As a result, the possibility of selection bias may be suspected.
In conclusion, baseline BMI > 25.7 kg/m2 at the initiation of PD might be a risk factor for all-cause mortality in Korean patients undergoing PD, especially non-diabetic patients.
Supplementary Information
Acknowledgments
The current study was supported by an Inha University Hospital Research Grant. This study was also supported by a grant from the Basic Science Research Program through the National Research Foundation of Korea funded by the Ministry of Education, Science, and Technology (SDH: NRF-2017R1D1A1B03030691).
Footnotes
Conflicts of interest
All authors have no conflicts of interest to declare.
Authors’ contributions
Seun Deuk Hwang, Jin Ho Lee, and Seoung Woo Lee participated in the data collection and wrote the manuscript. Seun Deuk Hwang, Jin Ho Lee, and Seoung Woo Lee participated in the study design and performed the statistical analysis. Seun Deuk Hwang, Jin Ho Lee, and Seoung Woo Lee participated in the conception, analysis, and interpretation of data. Seun Deuk Hwang, Jin Ho Lee, Jong Hyun Jhee, Joon Ho Song, Joong Kyung Kim, and Seoung Woo Lee provided intellectual content of critical importance to the work and technical support. Seun Deuk Hwang, Jin Ho Lee, and Seoung Woo Lee participated in the study design and coordination and helped to draft the manuscript. All authors read and approved the final manuscript.
References
- 1.Dimkovic N, Oreopoulos DG. Chronic peritoneal dialysis in the elderly: a review. Perit Dial Int. 2000;20:276–283. [PubMed] [Google Scholar]
- 2.Jiang N, Qian J, Lin A, Lindholm B, Axelsson J, Yao Q. Initiation of glucose-based peritoneal dialysis is associated with increased prevalence of metabolic syndrome in non-diabetic patients with end-stage renal disease. Blood Purif. 2008;26:423–428. doi: 10.1159/000153248. [DOI] [PubMed] [Google Scholar]
- 3.Kovesdy CP, Furth SL, Zoccali C World Kidney Day Steering Committee. Obesity and kidney disease: hidden consequences of the epidemic. Can J Kidney Health Dis. 2017;4 doi: 10.1177/2054358117698669. 2054358117698669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Park J, Ahmadi SF, Streja E, et al. Obesity paradox in end-stage kidney disease patients. Prog Cardiovasc Dis. 2014;56:415–425. doi: 10.1016/j.pcad.2013.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Naidu AN, Rao NP. Body mass index: a measure of the nutritional status in Indian populations. Eur J Clin Nutr. 1994;48(Suppl 3):S131–S140. [PubMed] [Google Scholar]
- 6.Kalantar-Zadeh K, Block G, Humphreys MH, Kopple JD. Reverse epidemiology of cardiovascular risk factors in maintenance dialysis patients. Kidney Int. 2003;63:793–808. doi: 10.1046/j.1523-1755.2003.00803.x. [DOI] [PubMed] [Google Scholar]
- 7.Pliakogiannis T, Trpeski L, Taskapan H, et al. Reverse epidemiology in peritoneal dialysis patients: the Canadian experience and review of the literature. Int Urol Nephrol. 2007;39:281–288. doi: 10.1007/s11255-006-9142-1. [DOI] [PubMed] [Google Scholar]
- 8.Kim YK, Kim SH, Kim HW, et al. The association between body mass index and mortality on peritoneal dialysis: a prospective cohort study. Perit Dial Int. 2014;34:383–389. doi: 10.3747/pdi.2013.00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jin DC, Yun SR, Lee SW, Han SW, Kim W, Park J. Current characteristics of dialysis therapy in Korea: 2015 registry data focusing on elderly patients. Kidney Res Clin Pract. 2016;35:204–211. doi: 10.1016/j.krcp.2016.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kim CS, Jin DC, Yun YC, Bae EH, Ma SK, Kim SW. Relationship between serum uric acid and mortality among hemodialysis patients: retrospective analysis of Korean end-stage renal disease registry data. Kidney Res Clin Pract. 2017;36:368–376. doi: 10.23876/j.krcp.2017.36.4.368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Brown EA, Davies SJ, Rutherford P, et al. EAPOS Group. Survival of functionally anuric patients on automated peritoneal dialysis: the European APD Outcome Study. J Am Soc Nephrol. 2003;14:2948–2957. doi: 10.1097/01.ASN.0000092146.67909.E2. [DOI] [PubMed] [Google Scholar]
- 12.Liu J, Zeng X, Hong HG, Li Y, Fu P. The association between body mass index and mortality among Asian peritoneal dialysis patients: a meta-analysis. PLoS One. 2017;12:e0172369. doi: 10.1371/journal.pone.0172369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kiran VR, Zhu TY, Yip T, Lui SL, Lo WK. Body mass index and mortality risk in Asian peritoneal dialysis patients in Hong Kong-impact of diabetes and cardiovascular disease status. Perit Dial Int. 2014;34:390–398. doi: 10.3747/pdi.2013.00055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ravel VA, Molnar MZ, Streja E, et al. Low protein nitrogen appearance as a surrogate of low dietary protein intake is associated with higher all-cause mortality in maintenance hemodialysis patients. J Nutr. 2013;143:1084–1092. doi: 10.3945/jn.112.169722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rocco MV, Frankenfield DL, Prowant B, Frederick P, Flanigan MJ Centers for Medicare & Medicaid Services Peritoneal Dialysis Core Indicators Study Group. Risk factors for early mortality in U.S. peritoneal dialysis patients: impact of residual renal function. Perit Dial Int. 2002;22:371–379. [PubMed] [Google Scholar]
- 16.Jotterand Drepper V, Kihm LP, Kälble F, et al. Overhydration is a strong predictor of mortality in peritoneal dialysis patients - independently of cardiac failure. PLoS One. 2016;11:e0158741. doi: 10.1371/journal.pone.0158741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ekart R, Hojs R. Obese and diabetic patients with end-stage renal disease: peritoneal dialysis or hemodialysis? Eur J Intern Med. 2016;32:1–6. doi: 10.1016/j.ejim.2016.03.016. [DOI] [PubMed] [Google Scholar]
- 18.McDonald SP, Collins JF, Johnson DW. Obesity is associated with worse peritoneal dialysis outcomes in the Australia and New Zealand patient populations. J Am Soc Nephrol. 2003;14:2894–2901. doi: 10.1097/01.ASN.0000091587.55159.5F. [DOI] [PubMed] [Google Scholar]
- 19.Xiong L, Cao S, Xu F, et al. Association of body mass index and body mass index change with mortality in incident peritoneal dialysis patients. Nutrients. 2015;7:8444–8455. doi: 10.3390/nu7105405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Snyder JJ, Foley RN, Gilbertson DT, Vonesh EF, Collins AJ. Body size and outcomes on peritoneal dialysis in the United States. Kidney Int. 2003;64:1838–1844. doi: 10.1046/j.1523-1755.2003.00287.x. [DOI] [PubMed] [Google Scholar]
- 21.Abbott KC, Glanton CW, Trespalacios FC, et al. Body mass index, dialysis modality, and survival: analysis of the United States Renal Data System Dialysis Morbidity and Mortality Wave II Study. Kidney Int. 2004;65:597–605. doi: 10.1111/j.1523-1755.2004.00385.x. [DOI] [PubMed] [Google Scholar]
- 22.de Mutsert R, Grootendorst DC, Boeschoten EW, Dekker FW, Krediet RT. Is obesity associated with a survival advantage in patients starting peritoneal dialysis? Contrib Nephrol. 2009;163:124–131. doi: 10.1159/000223790. [DOI] [PubMed] [Google Scholar]
- 23.Fernandes NM, Bastos MG, Franco MR, et al. Brazilian Peritoneal Dialysis Multicenter Study (BRAZPD) Group. Body size and longitudinal body weight changes do not increase mortality in incident peritoneal dialysis patients of the Brazilian peritoneal dialysis multicenter study. Clinics (Sao Paulo) 2013;68:51–58. doi: 10.6061/clinics/2013(01)OA08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hoogeveen EK, Halbesma N, Rothman KJ, et al. Netherlands Cooperative Study on the Adequacy of Dialysis-2 (NECOSAD) Study Group. Obesity and mortality risk among younger dialysis patients. Clin J Am Soc Nephrol. 2012;7:280–288. doi: 10.2215/CJN.05700611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ahmadi SF, Zahmatkesh G, Streja E, et al. Association of body mass index with mortality in peritoneal dialysis patients: a systematic review and meta-analysis. Perit Dial Int. 2016;36:315–325. doi: 10.3747/pdi.2015.00052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Byers T. Body weight and mortality. N Engl J Med. 1995;333:723–724. doi: 10.1056/NEJM199509143331109. [DOI] [PubMed] [Google Scholar]
- 27.Jin DC. Current status of dialysis therapy in Korea. Korean J Intern Med. 2011;26:123–131. doi: 10.3904/kjim.2011.26.2.123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Prasad N, Sinha A, Gupta A, et al. Effect of body mass index on outcomes of peritoneal dialysis patients in India. Perit Dial Int. 2014;34:399–408. doi: 10.3747/pdi.2013.00056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Tobias DK, Manson JE. The obesity paradox in type 2 diabetes and mortality. Am J Lifestyle Med. 2016;12:244–251. doi: 10.1177/1559827616650415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Zhou H, Cui L, Zhu G, et al. Survival advantage of normal weight in peritoneal dialysis patients. Ren Fail. 2011;33:964–968. doi: 10.3109/0886022X.2011.615968. [DOI] [PubMed] [Google Scholar]
- 31.Lo WK. Metabolic syndrome and obesity in peritoneal dialysis. Kidney Res Clin Pract. 2016;35:10–14. doi: 10.1016/j.krcp.2015.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Passadakis PS, Oreopoulos DG. Diabetic patients on peritoneal dialysis. Semin Dial. 2010;23:191–197. doi: 10.1111/j.1525-139X.2010.00707.x. [DOI] [PubMed] [Google Scholar]
- 33.Xu R, Han Q, Zhu T, et al. Diabetic patients could do as well as non-diabetic patients without inflammation on peritoneal dialysis. PLoS One. 2013;8:e80486. doi: 10.1371/journal.pone.0080486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Chung SH, Han DC, Noh H, et al. Risk factors for mortality in diabetic peritoneal dialysis patients. Nephrol Dial Transplant. 2010;25:3742–3748. doi: 10.1093/ndt/gfq233. [DOI] [PubMed] [Google Scholar]
- 35.Piraino B, Bernardini J, Centa PK, Johnston JR, Sorkin MI. The effect of body weight on CAPD related infections and catheter loss. Perit Dial Int. 1991;11:64–68. [PubMed] [Google Scholar]
- 36.Johnson DW, Mudge DW, Sturtevant JM, et al. Predictors of decline of residual renal function in new peritoneal dialysis patients. Perit Dial Int. 2003;23:276–283. [PubMed] [Google Scholar]
- 37.Johnson DW. What is the optimal fat mass in peritoneal dialysis patients? Perit Dial Int. 2007;27(Suppl 2):S250–S254. [PubMed] [Google Scholar]
- 38.Guilherme A, Virbasius JV, Puri V, Czech MP. Adipocyte dysfunctions linking obesity to insulin resistance and type 2 diabetes. Nat Rev Mol Cell Biol. 2008;9:367–377. doi: 10.1038/nrm2391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Postorino M, Marino C, Tripepi G, Zoccali C CREDIT (Calabria Registry of Dialysis and Transplantation) Working Group. Abdominal obesity and all-cause and cardiovascular mortality in end-stage renal disease. J Am Coll Cardiol. 2009;53:1265–1272. doi: 10.1016/j.jacc.2008.12.040. [DOI] [PubMed] [Google Scholar]
- 40.Nordfors L, Heimbürger O, Lönnqvist F, et al. Fat tissue accumulation during peritoneal dialysis is associated with a polymorphism in uncoupling protein 2. Kidney Int. 2000;57:1713–1719. doi: 10.1046/j.1523-1755.2000.00016.x. [DOI] [PubMed] [Google Scholar]
- 41.Li PK, Kwan BC, Ko GT, Chow KM, Leung CB, Szeto CC. Treatment of metabolic syndrome in peritoneal dialysis patients. Perit Dial Int. 2009;29(Suppl 2):S149–S152. [PubMed] [Google Scholar]
- 42.Duong U, Mehrotra R, Molnar MZ, et al. Glycemic control and survival in peritoneal dialysis patients with diabetes mellitus. Clin J Am Soc Nephrol. 2011;6:1041–1048. doi: 10.2215/CJN.08921010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Lee MJ, Kwon YE, Park KS, et al. Glycemic control modifies difference in mortality risk between hemodialysis and peritoneal dialysis in incident dialysis patients with diabetes: results from a nationwide prospective cohort in Korea. Medicine (Baltimore) 2016;95:e3118. doi: 10.1097/MD.0000000000003118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Choi SJ, Kim NR, Hong SA, et al. Changes in body fat mass in patients after starting peritoneal dialysis. Perit Dial Int. 2011;31:67–73. doi: 10.3747/pdi.2009.00131. [DOI] [PubMed] [Google Scholar]
- 45.Badve SV, Paul SK, Klein K, et al. The association between body mass index and mortality in incident dialysis patients. PLoS One. 2014;9:e114897. doi: 10.1371/journal.pone.0114897. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.