Abstract
A 20-year-old woman recently married presented to the outpatient department of the hospital, with primary amenorrhea and difficulty in having coitus. Her height was 155 cm, breast development was normal for age, and other secondary sexual characters seemed normal. On local examination, external genitalia was normal looking, and there was no vaginal discharge. She had a blind vagina of 2 cm length. The ultrasound showed a normal-sized uterus and ovaries seemingly normal. Hormonal profile comprising serum follicle-stimulating hormone, luteinising hormone, prolactin and thyroid stimulating hormone were all within normal limits. Karyotyping was done, which showed a 46,XX pattern. The patient underwent vaginal surgery during which septum resection was done, and amnion grafting was performed to prevent stricture formation. The patient resumed successful coitus 3 months after surgery. There was no discomfort on coitus. She conceived 7 months later. Following this, the patient delivered a healthy baby boy through caesarean section at term.
Keywords: pregnancy, plastic and reconstructive surgery
Background
The transition from childhood to adolescence is one of the most dynamic transformations that occur during the life of a woman. These include physical, emotional, psychological, behavioural and sexual transformations. All these changes result in a young girl developing and maturing into a young adult with full reproductive potential. In a low- and middle-income country (LMIC) such as Pakistan, puberty is acknowledged with the start of menstruation. Absence of menses in girls on reaching pubertal age has a stigma attached to it along with many superstitious myths and doubts regarding her gender. The management of primary amenorrhoea requires detailed investigations before a diagnosis is established, and then in some patients, there is a need for surgery. Müllerian abnormalities are one of the most common causes of primary amenorrhea, with transverse vaginal septum having an incidence of 1 in 2100 to 1 in 72 000. The modern surgical methods are very expensive and available in only a few centres in Pakistan. In our unit, we have developed an inexpensive technique with easily available contraption for this highly specialised procedure of vaginoplasty.
Case presentation
A 20-year-old woman married for the last 6 months presented with the complaint of dyspareunia. On history, she disclosed that she never had menstruation and experienced cyclical lower abdominal pain for the last 3 years. She took some medication for initiation of her menstruation but never experienced any withdrawal bleeding. However, her pain aggravated after taking medication. She had well-developed secondary sexual characters. Her mother considered this amenorrhoea as a temporary menstrual delay and planned her marriage. She experienced dyspareunia on first coitus, and full penetration was not possible. She subsequently felt the same on repeated attempts at coitus and experienced verbal and physical abuse by her husband. Due to the stigma, she was sent back to her parents' home to be treated for the condition. On examination, there was a blind-ending vagina of 2 cm length with hymenal remnants. The diagnosis of vaginal septum was made based on the examination findings. The patient and her family were counselled in detail about her diagnosis and need for surgery. The family and patient agreed for surgery after much consideration.
Investigations
A complete workup including hormonal profile (follicle-stimulating hormone, luteinising hormone, prolactin, thyroid stimulating hormone), ultrasonography and karyotyping was done. All investigations were within normal limits.
Treatment
An incision was made at the dome of the vagina. It was extended upwards by blunt and sharp dissection with guidance of urinary catheter anteriorly and a finger along anterior wall of the rectum. This resulted in a small opening through which a probe was passed, and about 200 cc of thick, dark-coloured blood was drained. A thick septum is seen in the lower half of the vagina. The septum was resected. The approximation of distance between upper and lower end of vagina was not possible, so an amnion mould was placed (figures 1–3). The mould was kept in the vagina for 7 days. Afterwards, it was replaced by a silicon solid mould that was specially designed. It was 8 cm long and 4 cm wide, easily washable and costed only 600 Pakistani rupees (around US $5). The mould was kept in the vagina for 3 weeks (figures 4–7).
Figure 1.

Space created between bladder and urethra anteriorly and rectum posteriorly. Blunt dissection performed with finger.
Figure 2.

Amnion membranes to line the neovagina were obtained from elective caesarean delivery. Mother screened for hepatitis B and C as well as HIV.
Figure 3.

Cavity size of depth 8 cm in length and 4 cm in width achieved.
Figure 4.
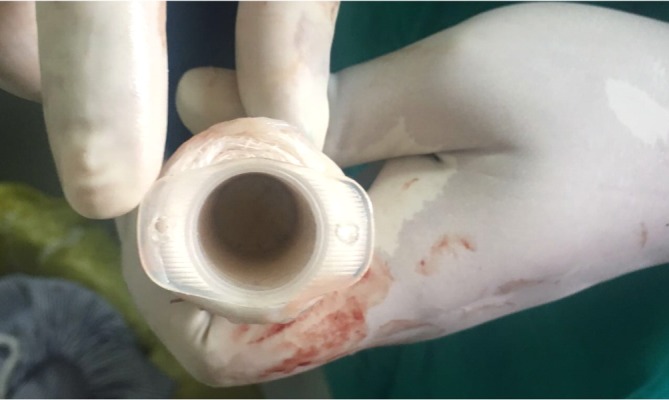
Vaginal mould was made with 50 mL syringe wrapped in sterile gauze.
Figure 5.
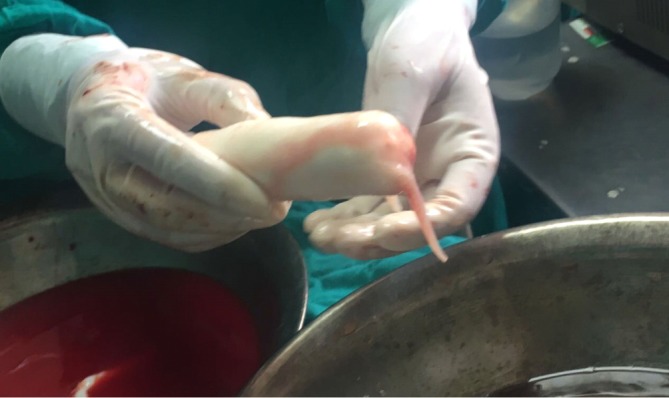
Mould was then wrapped in amnion.
Figure 6.

Mould was covered with latex condom.
Figure 7.

Mould was then placed in the constructed cavity.
Outcome and follow-up
Patient was advised about maintaining meticulous vaginal hygiene, especially during menstruation. In the second month, she was advised to keep the mould only at night, and in the third month, she had to keep mould four times a week. After that, she was allowed to resume intercourse. No postoperative complications were noted. She came for regular follow-ups. The patient conceived 7 months after surgery and delivered a healthy baby boy by caesarean section at term.
Discussion
Uterovaginal anomalies are divided into four groups—vertical fusion disorders, müllerian duct dysgenesis, disorders of lateral fusion and unusual configurations and combinations of defects. In these disorders, at the time of development, certain dysplastic changes take place at the level of müllerian ducts and urogenital sinus, which result in a range of anomalies of the uterus and vagina. In some cases, uterus or part of the vagina may be absent. Faults in the junction between the downgrowing müllerian ducts and the upgrowing derivative of the urogenital sinus are a result of vertical fusion disorders. Failure of lateral fusion of the two müllerian ducts may result in lateral fusion disorders.1
Mostly, lateral fusion disorders lead to unilateral vaginal obstruction. Moreover, unilateral obstruction can be accompanied by the absence of ipsilateral kidney. Bilateral renal agenesis is accompanied with bilateral obstruction. This can be associated with subsequent nonviability of the developing embryo. Cases of complete vaginal obstruction at the time of menarche or following menarche need urgent attention to prevent harm to the reproductive system. The damage occurs due to retrograde tubal reflux and subsequent development of endometriosis. However, there is no emergency for correction in case of non-obstructive malformation. Hence, a complete evaluation is necessary to determine whether these müllerian disorders are a cause of reproductive problems or not.2
Management of developmental anomalies of the müllerian duct is difficult to correct and needs training with precise and meticulous surgical technique and is associated with poor success rates. Investigators are now searching for alternative surgical techniques and materials to obtain better postoperative results. One of the solutions is the use of amnion graft to reduce the risk of postoperative complications. Amniotic membrane is used as a graft to cover the inner surface of the vagina.
Amniotic membrane has low antigenicity (incomplete human leukocyte antigen A, B, C and DR antigens), and the risk of rejection is very low. When the membrane is used as a vaginal graft, it draws fibrinogen and collagen into the local fascia, thus strengthening the weak local fascia.3 4
Fresh amnion is a prerequisite as a graft for this surgery. It can be obtained from delivery suites and used immediately. This is a simple and cost-effective graft, which demonstrates good results for the transvaginal repair.5
Success of treatment in a case of transverse vaginal septum is dependent on the size of septum and severity of symptoms. Small transverse vaginal septa <1 cm in thickness can be managed by excision with a simple end-to-end anastomosis of the vaginal epithelium or a Z-plasty.6–8 In case of septum thickness >1 cm), preoperative vaginal dilation can be used, followed by a longitudinal Z-plasty technique. This can reduce the incidence of stenosis and scarring at the site of graft.7 8
Postoperative dilatation of the vagina is needed, failing which stricture might form leading to dyspareunia. In patients with small septa, vaginal dilators are the first-line treatment for management. Dilation can also be done as a preoperative measure to improve the success rates resulting in decreasing the probability of strictures, scarring, or stenosis.8
These patients should be counselled for long-term follow-up in order to watch for adverse postoperative outcomes. Dyspareunia, fertility issues and preterm labour are some of the complications.6 8 9
Many techniques of vaginoplasty have evolved over the years such as laparoscopic approach along with different materials for graft purposes. In LMIC facilities, affordability and expertise of newer techniques are issues. Therefore, vaginoplasty using amnion graft is still an inexpensive, safe and effective procedure to treat patients of müllerian abnormalities. All such treated cases should be monitored for complications and record maintained.
Patient’s perspective.
This surgery has given me a new life in true sense. I had to suffer a lot of verbal, physical and emotional abuse from my own family and my in-laws. People told my family that I was not a female but a trans gender that I can never be sexually active nor could I ever conceive. My self-esteem was lost and I could not face anyone out of this guilt.
This treatment blessed me with happy marital relations, self-confidence and a healthy baby.
Learning points.
Early diagnosis and referral for such cases are needed.
Vaginoplasty by procedure using amnion graft is still a safe, inexpensive, easily available and effective procedure
Low-cost surgical procedures can be alternative in a low-resource setting.
Footnotes
Contributors: RS and SK wrote the manuscript. AM and AA contributed to case management.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Patient consent for publication: Obtained.
References
- 1. Rock JA, Breech LL. Surgical Correction of Uterovaginal Anomalies Chapter 70 Lippincott Williams & Wilkins Publications CD Rom. 1-6, 2004. [Google Scholar]
- 2. Rock JA. Surgery for anomalies of the müllerian ducts : Thompson JD, Rock JA, Telinde’s Operative Gynecology, p 688. Philadelphia: JB Lippincott, 1997. [Google Scholar]
- 3. Seifeldin A. Vaginal wall repair – using amniotic membrane graft. Obstet Gynecol Int J 2015;2:00056 10.15406/ogij.2015.02.00056 [DOI] [Google Scholar]
- 4. Choolani M, Chan J, Fisk NM. Fetal therapy: 2020 and beyond. Prenat Diagn 2010;30:699–701. 10.1002/pd.2527 [DOI] [PubMed] [Google Scholar]
- 5. Mi S, David AL, Chowdhury B, et al. . Tissue engineering a fetal membrane. Tissue Eng Part A 2012;18(3-4):373–81. 10.1089/ten.tea.2011.0194 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Deligeoroglou E, Iavazzo C, Sofoudis C, et al. . Management of hematocolpos in adolescents with transverse vaginal septum. Arch Gynecol Obstet 2012;285:1083–7. 10.1007/s00404-011-2114-4 [DOI] [PubMed] [Google Scholar]
- 7. Wierrani F, Bodner K, Spängler B, et al. . “Z”-plasty of the transverse vaginal septum using Garcia’s procedure and the Grünberger modification. Fertil Steril 2003;79:608–12. 10.1016/S0015-0282(02)04803-3 [DOI] [PubMed] [Google Scholar]
- 8. Lankford JC, Mancuso P, Appel R. Congenital reproductive abnormalities. J Midwifery Womens Health 2013;58:546–51. 10.1111/jmwh.12020 [DOI] [PubMed] [Google Scholar]
- 9. Rock JA, Zacur HA, Dlugi AM, et al. . Pregnancy success following surgical correction of imperforate hymen and complete transverse vaginal septum. Obstet Gynecol 1982;59:448–51. [PubMed] [Google Scholar]


