Abstract
Background: The gut microbiota play an essential role in protecting the host against pathogenic microorganisms by modulating immunity and regulating metabolic processes. In response to environmental factors, microbes can hugely alter their metabolism. These factors can substantially impact the host and have potential pathologic implications. Particularly pathogenic microorganisms colonizing pancreas and biliary tract tissues may be involved in chronic inflammation and cancer evolution.
Purpose: To evaluate the effect of bile microbiota on survival in patients with pancreas and biliary tract disease (PBD).
Patients and Methods: We investigated 152 Italian patients with cholelithiasis (CHL), cholangitis (CHA), cholangiocarcinoma (CCA), gallbladder carcinoma (GBC), pancreas head carcinoma (PHC), ampullary carcinoma (ACA), and chronic pancreatitis (CHP). Demographics, bile cultures, therapy, and survival rates were analyzed in cohorts (T1 death <6 months; T2 death <12 months; T3 death <18 months, T3S alive at 18 months).
Results: The most common bacteria in T1 were E. coli, K. pneumoniae, and P. aeruginosa. In T2, the most common bacteria were E. coli and P. aeruginosa. In T3, there were no significant bacteria isolated, while in T3S the most common bacteria were like those found in T1. E. coli and K. pneumoniae were positive predictors of survival for PHC and ACA, respectively. E. coli, K. pneumoniae, and P. aeruginosa showed a high percentage of resistant bacteria to 3CGS, aminoglycosides class, and quinolone group especially at T1 and T2 in cancer patients.
Conclusions: An unprecedented increase of E. coli in bile leads to a decrease in survival. We suggest that some strains isolated in bile samples may be considered within the group of risk factors in carcinogenesis and/or progression of hepato-biliary malignancy. A better understanding of bile microbiota in patients with PBD should lead to a multifaceted approach to rapidly detect and treat pathogens before patients enter the surgical setting in tandem with the implementation of the infection control policy.
Keywords: human bile microorganisms; survival; pancreatic and biliary tract disease, E. coli
Introduction
The gut microbiota plays an indispensable role in protecting the host against pathogenic microorganisms by modulating immunity and regulating metabolic processes.1 In response to environmental factors, microbes can hugely alter their metabolism. These factors can substantially impact the host and have potential pathologic implications. In 1989, Wells published a work in which he demonstrated that the post-surgical infections were more often to be found in patients with non-sterile bile.2 Since then, there is increasing interest in the bile microbiome of the hepatobiliary system. There is an increasing interest to investigate cohorts of patients according to the STROBE guidelines. STROBE stands for international collaboration of epidemiologists, methodologists, statisticians, researchers, and editors involved in the conduct and diffusion of observational studies, with the common aim of STrengthening the Reporting of OBservational studies in Epidemiology.3 The importance to target the bile microbiota may suggest avenues for future studies of biomarkers and therapeutic interventions in hepatobiliary disease.4–8
The primary malignancies of the biliary tract, ie, cholangiocellular carcinoma (CCA) and gallbladder carcinoma (GBC), have been traditionally diagnosed at an advanced stage and harbor a low sensitivity to radiation and chemotherapy.9 In the last decade, both the diagnostic and therapeutic approaches of these patients have started to change because of the improvement of imaging and the introduction of new chemical compounds addressing specific signaling pathways of carcinogenesis.9–12 On the other hand, the mortality in some groups of malignancies of the pancreatic-biliary system remains obscurely high with low survival rates.13–15 Our research question was to address the potential clinical impact of the bile microbiota in these patients and if Enterobacteriaceae are significantly associated with neoplasms of the pancreas and biliary tract.
Accumulating evidence indicates that a multidisciplinary approach to surgical and non-surgical treatment strategies for patients with complex pancreatic and biliary disease is crucial.16 Thus, a series of interdisciplinary meetings occurred in our institution with occasional foreign visitors with expertise in clinical pathology and public health. Preoperative biliary drainage (POBD) is often performed by endoscopic placement of an endo-biliary stent into the common bile duct (CBD) or via percutaneous transhepatic drainage of the biliary tract or after decompression of the biliary duct. Previous studies showed a favorable effect of POBD on postoperative morbidity and mortality, although a stent may be a significant risk factor for bacterial contamination of the biliary system. Subjects with microbiota that is resistant to antibiotics are at an increased risk of postoperative infection as also shown in previous research work from us and others.17–20 Moreover, oncologic patients may be affected by malnutrition or cachexia and exhibit a low quality of life, increased morbidity and mortality, prolonged hospital stays, and a reduced response to treatment.21–23 Postoperative complications may also influence biliary microbiota.24–26 In line with this research, we hypothesized that certain kinds of bacterial and/or fungal microorganisms isolated in bile might be associated with specific pancreas and biliary tract diseases (PBDs) especially in surgical patients undergoing surgery due to PBD. A particular strain might be responsible for a decrease in survival other than the neoplastic disease. We retrospectively investigated the microbiota in the bile of surgical patients with PBD for a correlation between dead/survived patients considering bacterial strains collected from the bile, the underlying disease, and the anti-infective therapy.
Materials and methods
Study design and patients
This study is a single-center cohort investigation that was performed in a quality assurance (QA)-certified academic setting.27 We retrieved the files of patients with a diagnosis of cholelithiasis (CHL), cholangitis (CHA), CCA, GBC, carcinoma of the head of the pancreas (PHC), ampullary carcinoma (ACA), and chronic pancreatitis (CHP). The patients were hospitalized at the Department of General and Emergency Surgery, University Hospital of Palermo, Italy, between June 2010 and June 2014, with follow-up until December 2016. The study population consisted of patients with positive culture of bile samples collected during endoscopic retrograde cholangiopancreatography (ERCP) from patients harboring hepatobiliary disease at an external quality assurance-certified General Surgery and Emergency Academic Unit by the same operator (FD) as previously published.28,29
Routine Antibiotic prophylaxis was not administrated in unselected patients underwent to ERCP for bile sampling as reported in the literature (Performance measures for ERCP and endoscopic ultrasound: a European Society of Gastrointestinal Endoscopy (ESGE) Quality Improvement Initiative).30 The operational guidelines for anti-infective prophylaxis used in the study period were previously reported31 and also available on the website of the University Hospital “P. Giaccone” of Palermo, Italy (http://www.policlinico.pa.it/portal/pdf/news/CIO/LineeGuidaAntibioticoProfilassiLast.pdf)
The patient population included hospitalized patients at the first surgery (58%) and patients readmitted at our unit (12%). Our surgical emergency reference admitted outpatients are also coming from several surgical groups (30%). All outpatients (30%) were emergency cases and showed a history of surgery. Moreover, half of the patients had a history of previous antibiotic treatment. The incidence of comorbidities such as diabetes and cardiovascular disease mirrored those reported in the general population according to age and sex during the study period.32
Data about kind of surgical intervention applied at the Department of General and Emergency Surgery of the Policlinic of Palermo and experience about revision, re-exploration, and solution of complications of surgical procedures performed both in the open and in a laparoscopic way have previously been reported.33 In general, in resettable pancreatic cancer and periampullary neoplasms, pre-operative biliary drainage was done with ERCP if the serum bilirubin was more than 20 mg/dl or if the patient had a fever because of acute CHA.33 In gallstones disease and acute cholecystitis, a laparoscopic approach was preferred in elderly patients.34 According to European guidelines, a biliary stent was placed in cases of malignant obstruction and if the tumor was unresectable (about 18% of enrolled patients).
Ethics procedures and adherence to STROBE guidelines
All the patients gave written informed consent for surgical procedures and collection and storage of research data set including their anonymous publication according to ethical guidelines of the Declaration of Helsinki for clinical studies. Moreover, a written informed consent, also including the potential release of the patient’s details, was obtained from each patient’s next of kin by the principles of the Declaration of Helsinki as previously reported. Our study was inserted in the surveillance program for multidrug-resistant Gram-negative bacilli, including active surveillance cultures, that has been carried out in the Surgical Emergency Unit since January 2010 as previously reported.35,36 The study protocol was fully approved by the Ethics Committee of the Azienda Ospedaliero-Universitaria Policlinic “P. Giaccone”, University of Palermo, Palermo, Italy (IRB n.10_8/2013). This work follows the STROBE guidelines for retrospective cohort studies.3
The cyto- and/or histopathological examination was performed in a Quality Assurance (QA)-certified hospital only setting using protocols and standard operative procedures.37
Microbiota identification
Bacterial identification with antimicrobial susceptibility testing was carried out by collecting laboratory data using either the Phoenix Automated Microbiology System (Becton Dickinson Diagnostic Systems, Sparks, United States) or the Vitek-2 System (Bio-Mérieux, Marcy l’Etoile, France).38,39 Antibiotic susceptibility testing and detection of the Extended-spectrum beta-Lactamase (ESBL) were first performed by disk diffusion and double disk synergy test and then confirmed by Etest (BioMerieux, Marcy l’Etoile, France) methods according to the guidelines of the European Committee specialized on Antimicrobial Susceptibility Testing (EUCAST).40
All isolates were confirmed to be non-susceptible to imipenem and/or meropenem according to the EUCAST breakpoints as previously reported.40 As previously reported,37 a multidisciplinary team meeting approved the introduction of a specific antibiotic therapy in patients who presented with at least one of the following specimens positive for pathogens – peritoneal fluid, peritoneal fluid cultures, drainage fluid/blood or bile or tissue – during surgical procedures according to the Infectious Diseases Society of America and the American Society for Microbiology.41
Candida spp. were also identified by both conventional morphological and biochemical methods as previously reported.37
Statistical analysis
The statistical analysis was performed using the Matrix Laboratory (MATLAB) analytical toolbox version 2008 (MathWorks, Natick, MA, USA). Data are explicitly presented as number and percentage for categorical variables. Continuous data expressed as the mean ± standard deviation (SD) unless otherwise specified. The multiple comparison chi-square tests were used to define significant differences among percentages. If the chi-square test was significant (p<0.05), the residual analysis with the Z-test was performed. In the case of paired data, the multiple comparison Cochran’s Q tests were used to compare the differences among percentages under the consideration of the null hypothesis that there are no differences between the variables. When the Cochran’s Q test was positive (p<0.05), then a minimum required difference for a significant difference between two proportions was calculated using the Minimum Required Differences method with Bonferroni p-value corrected for multiple comparisons according to Sheskin (2004). Multi-comparison tests on continuous data were performed with one-way ANOVA test to evaluate significant differences among means. If the ANOVA test was positive, the Scheffé’s method, a technique for adjusting levels of significance in a linear regression analysis to justify multiple comparisons, was performed for pairwise comparison of subgroups. Also, univariate and multivariate linear correlation analysis was performed, where the test on Pearson’s linear correlation coefficient R was performed with the t-Student test, under the null hypothesis of Pearson’s linear correlation coefficient of R equals to zero. At this step, we defined an experimental probability distribution for the patients’ survival, therapy, disease, bacteria type, and gender. We assigned a score 1 in the case of survival after 18 months else zero, 1 to male and zeroed to female, 1 to therapy-sensitive and zero with therapy resistance, 1 for positive bacterial culture, and zero for sterile culture, and 1 for a pancreaticobiliary disease and zero for no-disease.
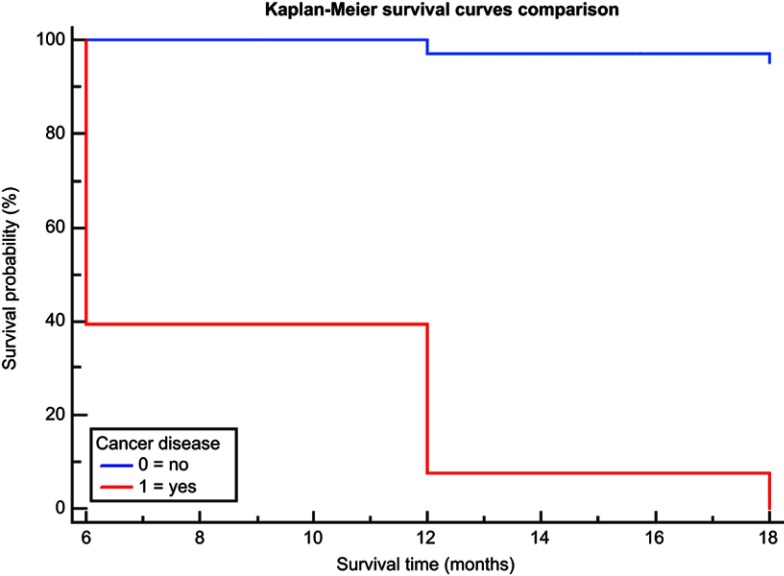
To analyze the overall survival time, we categorized the patients in four cohorts: T1, patients with death within six months; T2, death within 12 months; T3, death within 18 months, and T3S patients alive at 18 months. Finally, we analyzed the effect of several risk factors on survival. For this scope, we defined the dichotomous variables: Cancer_disease (1= yes cancer: CCA, GBC, PHC, or ACA and 0 = no cancer, ie, inflammatory disease: CHL, CHA, or CHP) and Frequent_bacteria (1= most frequent: K. pneumoniae, Pseudomonas spp or E. coli and 0 = Others). Particularly, the Kaplan–Meier survival curves were showed for no cancer and cancer group in Figure 2 and compared with the log-rank test; instead, the Cox proportional-hazards regression results are shown in Table 4 and Figure 3. All tests with p-value (p) <0.05 were considered significant.
Figure 2.
The Kaplan–Meier curves comparison with log-rank test, considering the dichotomous variable: Cancer_disease, used to define two groups: group with cancer and group without cancer.
Table 4.
Cox proportional-hazards regression
| Covariates | Percentages or mean ± SD | HR | 95% CI | p-value |
|---|---|---|---|---|
| Age | 72.3±12.6 | 1.0 | 0.99–1.03 | 0.48 |
Gender
|
53.3 (81/152) 46.7 (71/152) |
1.0 |
0.67–1.40 |
0.87 |
Therapy
|
94.7 (144/152) 5.3 (8/152) |
0.6 |
0.26–1.37 |
0.22 |
Frequent bacteria
|
57.9 (88/152) 42.1 (64/152) |
1.1 |
0.74–1.53 |
0.74 |
Disease type
|
78.3 (119/152) 21.7 (33/152) |
73.6 |
10.1–537.5 |
<0.0001 * |
Note: *Significant test.
Abbreviations: HR, hazard ratio(s); CCA, Cholangiocarcinoma; PHC, carcinoma of the head of the pancreas; ACA, ampullary carcinoma; GBC, gallbladder carcinoma; CHL, cholelithiasis; CHA, cholangitis; CHP, chronic pancreatitis HR, hazards ratio; CI, confidence interval; SD, standard deviation.
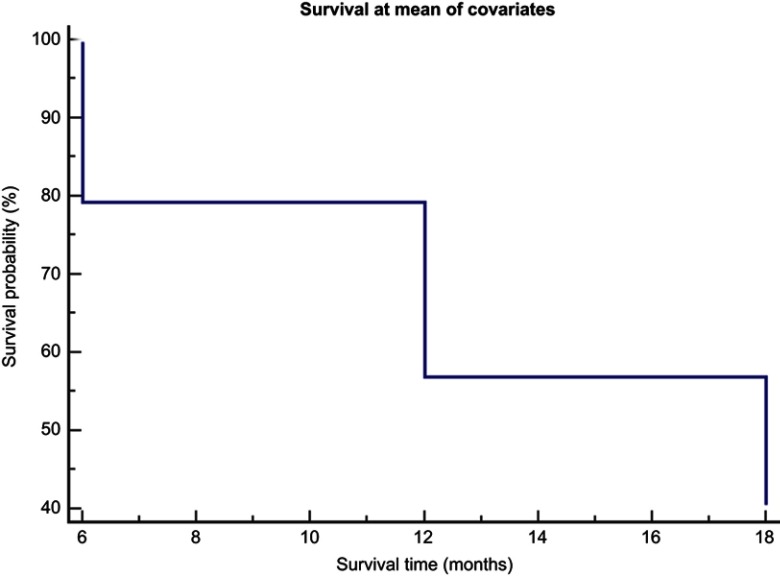
Figure 3.
Cox proportional – hazard regression analysis. In the graph, a single survival curve at a mean of all covariates in the model is shown. The survival curve represents the probability (Y-axis) of surviving a given length of time (X-axis).
Results
Patients and grouping
A total of 152 consecutive patients met our eligibility criteria and were enrolled in the study: 53.29% males and 46.71% females with age range of 26–93 (72±13; mean ± SD). Table 1 shows mean age, percentages by sex and isolates, pancreatic and biliary tract diseases, and anti-infective therapy administered in the enrolled patients divided by their follow-up control points (T1, T2, T3, and T3S). Also, we reported the antimicrobials used according to antimicrobial test against bacteria isolated. The statistical analysis among groups defined at T1, T2, T3, and T3S is presented in the last column of Table 1. A multivariate analysis was performed, among all control points for every variable considered and where the multivariate analysis was positive (p<0.05) a post hoc test with pairwise comparison was completed. In this case, only significant results are reported. By contrast of mean age, we found a significant difference (p<0.0001, one-way ANOVA); notably, there was a significant difference between T1 patients and T3S patients (75.56>65.15, p<0.005), ie, the dead patients within 6 months had an age significantly greater in comparison to survival patients at 18 months.
Table 1.
Characteristic of 152 studied patients divided in different groups by time of overall survival and significant multicomparison tests among groups: T1 death within 6 months; T2 death within 12 months; T3 death within 18 months and T3S alive at 18 months
| Parameters | T1 | T2 | T3 | T3S | p-value |
|---|---|---|---|---|---|
| Patients % | 47.36% (72/152) | 25.65% (39/152) | 5.26% (8/152) | 21.71% (33/152) | – |
| <0.0001* (A) | |||||
| Age (mean ± SD) | 75.6±10.4 | 71.5±8.8 | 77.1±6.5 | 65.2±17.5 | T1 vs T3S: <0.005*(Sc) |
| Female | 43.1% (31/72) | 51.3% (20/39) | 25.0% (2/8) | 54.5% (18/33) | 0.385 (C) |
| Disease | |||||
| <0.0001* (C) | |||||
| T1: <0.0001** (Z) | |||||
| T2: <0.0001*** (Z) | |||||
| T3: 0.0090*** (Z) | |||||
| PHC (72) | 100% (72/72) | 0.0% | 0.0% | 0.0% | T3S: <0.0001*** (Z) |
| <0.0001* (C) | |||||
| T1: 0.0001*** (Z) | |||||
| T2: <0.0001** (Z) | |||||
| CCA (42) | 0.0% | 100% (39/39) | 0.0% | 9.1% (3/33) | T3S: 0.0351*** (Z) |
| <0.0001* (C) | |||||
| GBC (5) | 0.0% | 0.0% | 62.5%(5/8) | 0.0% | T3: <0.0001** (Z) |
| <0.0001* (C) | |||||
| ACA (4) | 0.0% | 0.0% | 37.5% (3/8) | 3.0% (1/33) | T3: <0.0001** (Z) |
| <0.0001* (C) | |||||
| T1: 0.0042*** (Z) | |||||
| T2: 0.0123*** (Z) | |||||
| CHL (27) | 0.0% | 0.0% | 0.0% | 81.8% (27/33) | T3S: <0.0001** (Z) |
| CHA (1) | 0.0% | 0.0% | 0.0% | 3.0% (1/33) | 0.304 (C) |
| CHP (1) | 0.0% | 0.0% | 0.0% | 3.0% (1/33) | 0.304 (C) |
| % of patients with presence of specific pathogens isolated in bile samples | |||||
| Escherichia coli | 20.8% (15/72) | 28.2% (11/39) | 12.5% (1/8) | 24.2% (8/33) | 0.726 (C) |
| Klebsiella pneumonia | 12.5% (9/72) | 2.6% (1/39) | 12.5% (1/8) | 15.2% (5/33) | 0.295 (C) |
| Enterococcus spp. | 0.0% | 2.6% (1/39) | 0.0% | 3.0% (1/33) | 0.516 (C) |
| Enterobacter spp. | 1.4% (1/72) | 7.7% (3/39) | 0.0% | 6.1% (2/33) | 0.334 (C) |
| Citrobacter spp. | 5.6% (4/72) | 5.1% (2/39) | 12.5% (1/8) | 6.1% (2/33) | 0.877 (C) |
| Serratia spp. | 0.0% | 0.0% | 0.0% | 3.0% (1/33) | 0.304 (C) |
| Aeromonas spp. | 1.4% (1/72) | 0.0% | 0.0% | 0.0% | 0.304 (C) |
| Pseudomonas aeruginosa | 23.6% (17/72) | 20.5% (8/39) | 25.0% (2/8) | 30.3% (10/33) | 0.809 (C) |
| Stenotrophomonas spp. | 5.5% (4/72) | 2.6% (1/39) | 0.0% | 0.0% | 0.454 (C) |
| 0.0339 * (C) | |||||
| Alcaligenes spp. | 0.0% | 10.3% (4/39) | 0.0% | 3.0% (1/33) | T2: 0.0354 ** (Z) |
| Acinetobacter spp. | 9.7% (7/72) | 0.0% | 0.0% | 3.0% (1/33) | 0.121 (C) |
| Achromobacter spp. | 4.2% (3/72) | 7.7% (3/39) | 12.5% (1/8) | 3.0% (1/33) | 0.614 (C) |
| Brevundimonas spp. | 1.4% (1/72) | 5.1% (2/39) | 0.0% | 3.0% (1/33) | 0.655 (C) |
| Delftia spp. | 2.8% (2/72) | 2.6% (1/39) | 0.0% | 0.0% | 0.768 (C) |
| Elizabethkingia spp. | 1.4% (1/72) | 2.6% (1/39) | 0.0% | 0.0% | 0.797 (C) |
| 0.0122* (C) | |||||
| GNBNI | 4.2% (3/72) | 2.6% (1/39) | 25.0% (2/8) | 0.0% | T3: 0.0029** (Z) |
| Candida albicans | 5.6% (4/72) | 0.0% | 0.0% | 0.0% | 0.207 (C) |
| % of Patients where the pathogens isolated in bile were sensible (S) to the specific therapy | |||||
| Meropenem | 79.2% (57/72) | 74.4% (29/39) | 75.0% (6/8) | 75.8% (25/33) | 0.98 (C) |
| Imipenem | 80.6% (58/72) | 71.8% (28/39) | 62.5% (5/8) | 72.7% (24/33) | 0.54 (C) |
| Ertapenem | 75.0% (54/72) | 76.9% (30/39) | 75.0% (6/8) | 72.7% (24/33) | 0.98 (C) |
| 3GCs plus MT | 63.9% (46/72) | 51.3% (20/39) | 50.0% (4/8) | 42.4% (14/33) | 0.20 (C) |
| Aminoglycosides | 47.2% (34/72) | 38.5% (15/39) | 50.0% (4/8) | 36.4% (12/33) | 0.66 (C) |
| Ciprofloxacin | 58.3% (42/72) | 35.9% (14/39) | 37.5% (3/8) | 39.4% (13/33) | 0.08 (C) |
| Levofloxacin | 37.5% (27/72) | 18.0% (7/39) | 37.5% (3/8) | 33.3% (11/33) | 0.20 (C) |
| 3GCs | 43.1% (31/72) | 25.6% (10/39) | 25.0% (2/8) | 30.3% (10/33) | 0.24 (C) |
| Total survival rate | 52.6% (80/152) | 51.3% (41/80) | 80.5% (33/41) | 33 | 0.0033 * (C) |
| T3: 0.0042 *** (Z) | |||||
| Survival rate in cancer group only (CCA, GBC, PHC or ACA) | 39.50% (47/119) | (9/47)19.15% | (1/9) 11.11% | 1 | 0.0154 * (C) |
| No localized significant results at significant level α =0.05 | |||||
| Survival rate in no cancer group only(CHL, CHA or CHP) | (33/33)100% | (32/33) 96.97% | (32/32)100% | 32 | 0.37 (C) |
Notes: T1 = death within 6 months, T2 = death within 12 months; T3 = death within 18 months; T3S = patients survival at T3. *Significant test; **Significant more frequent; ***Significant less frequent.
Abbreviations: GNBNI, gram negative bacilli not identified; N, no response; R, resistant; S, sensible; 3GCs, 3rd generation cephalosporin; MT, metronidazole; CCA, cholangiocarcinoma; PHC, carcinoma of the head of the pancreas; ACA, ampullary carcinoma; GBC, gallbladder carcinoma; CHL, cholelithiasis; CHA, cholangitis; CHP, chronic pancreatitis; A, one way ANOVA test; Sc, Schaffè test for pairwise comparison; C, multicomparison chi-square test; Z, Z-test.
Microbiota identification
For bacteria, among T1, T2, T3, and T3S, there was a significant difference for Alcaligenes spp (p=0.0339), the highest frequency was localized at T2 (p=0.0354) and for Gram-negative bacilli not identified (GNBNI) (p=0.0122) the highest frequency was localized at T3 (p=0.0029).
In examining the pancreatic and biliary tract diseases, PHC was mostly observed in dead patients at T1 (p<0.0001), CCA in deceased patients at T2 (p<0.0001), GBC and ACA in deceased patients at T3 (both p<0.0001), and CHL, in survival patients at T3S (p<0.0001, p=0.0093). Regarding the therapy, there were no significant differences among patients who underwent to susceptibility to antibiotics at T1, T2, T3, and T3S.
Survival graphics, disease, and microbiota
Finally, we reported the survival rates among T1 (80/152, 52.65%), T2 (41/80, 51.25%), and T3 (33/41, 80.49%). The survival rate was significantly higher in patients belonging to the T3 cohort (p=0.0042). Particularly, the survival rates for patients with cancer only (CCA, GBC, PHC, or ACA) among T1 (47/119, 39.50%), T2 (9/47, 19.15%), and T3 (1/9, 11.11%) and the survival rate for patients with no cancer (CHL, CHA, or CHP) among T1 (33/33, 100%), T2 (32/33, 96.97%), and T3 (32/32, 100%). In these cases, we observed for cancer group a significant differences of survival rate among T1, T2 and T3 (p=0.0154), but at significant level equal to 0.05 there were no significant survival rate higher/lower in comparison to others, even though at T1 the survival rate was of 39.50% greater in comparison to others. Instead, for patients with no cancer, no significant differences there were among T1, T2, and T3 (p=0.37). Table 2 shows the results of the statistical test into groups (ie, T1 death within six months; T2 death within 12 months; T3 death within 18 months, and T3S alive at 18 months). We observed that the most common bacteria in T1 were E. coli (p<0.0001), K. pneumoniae (p=0.0215), and P. aeruginosa (p<0.0001), while the less frequently isolated strains included: Alcaligenes spp. (p=0.0396), Serratia spp. (p=0.0396), and Enterococcus spp. (p=0.0396). In T2, the most common bacteria were E. coli (p<0.0001) and P. aeruginosa (p<0.0001), but no one was significantly less frequently seen in comparison to others. In T3, there were no bacteria isolated in comparison to others. In T3S, the most common bacteria were similar to those found in T1, while there were no bacteria significantly less frequent in comparison to others.
Table 2.
Multicomparison tests among percentages into groups: T1 death within 6 months; T2 death within 12 months; T3 death within 18 months and T3S alive at 18 months
| Parameters | T1 | T2 | T3 | T3S |
|---|---|---|---|---|
| Bacteria | <0.0001 * (C) | <0.0001 * (C) | 0.34 (C) | <0.0001 * (C) |
| Escherichia coli | <0.0001 ** (Z) | <0.0001 ** (Z) | − | <0.0001 ** (Z) |
| Klebsiella pneumoniae | 0.0215 ** (Z) | − | − | 0.0408 ** (Z) |
| Enterococcus spp | 0.0396 *** (Z) | − | − | − |
| Enterobacter spp | − | − | − | − |
| Citrobacter spp | − | − | − | − |
| Serratia spp | 0.0396 *** (Z) | − | − | − |
| Aeromonas spp | − | − | − | − |
| Pseudomonas aeruginosa | <0.0001 ** (Z) | <0.0001 ** (Z) | − | − |
| Stenotrophomonas spp | − | − | − | <0.0001 ** (Z) |
| Alcaligenes spp | 0.0396 *** (Z) | − | − | − |
| Acinetobacter spp | − | − | − | − |
| Achromobacter spp | − | − | − | − |
| Brevundimonas spp | − | − | − | − |
| Delftia spp | − | − | − | − |
| Elizabethkingia spp | − | − | − | − |
| GNBNI | − | − | − | − |
| Disease | <0.0001 * (C) | <0.0001 * (C) | <0.0001 * (C) | <0.0001 * (C) |
| PHC | <0.0001 ** (Z) | 0.0165 *** (Z) | − | 0.0299 *** (Z) |
| CCA | 0.0073 *** (Z) | <0.0001 ** (Z) | − | − |
| GBC | 0.0073 *** (Z) | 0.0165 *** (Z) | <0.0001 ** (Z) | 0.0299 *** (Z) |
| ACA | 0.0073 *** (Z) | 0.0165 *** (Z) | 0.0139 ** (Z) | − |
| CHL | 0.0073 *** (Z) | 0.0165 *** (Z) | − | <0.0001 ** (Z) |
| CHA | 0.0073 *** (Z) | 0.0165 *** (Z) | − | − |
| CHP | 0.0073 *** (Z) | 0.0165 *** (Z) | − | − |
| The most and less frequent therapy used in patients with bile disease | <0.0001 * (Q) test | <0.0001 * (Q) | 0.10 (Q) | <0.0001 * (Q) |
| Meropenem | <0.005 ** (Sh) | <0.005 ** (Sh) | − | <0.005 ** (Sh) |
| Imipenem | <0.005 ** (Sh) | − | − | − |
| Ertapenem | − | <0.005 ** (Sh) | − | − |
| 3GCs plus MT | − | − | − | − |
| Aminoglycosides | − | − | − | <0.005 *** (Sh) |
| Ciprofloxacin | − | <0.005 *** (Sh) | − | − |
| Levofloxacin | <0.005 *** (Sh) | <0.005 *** (Sh) | − | <0.005 *** (Sh) |
| 3GCs | − | <0.005 *** (Sh) | − | <0.005 *** (Sh) |
Notes: *Significant test; **Significant more frequent; ***Significant less frequent; T1 =6 months, T2 =12 months, and T3 =18 months; T3S = patients survival at T3.
Abbreviations: Q, multicomparison Cochran’s Q test; (Sh) Sheskin’s procedure for significant difference between two proportions; C, multicomparison chi-square test; Z, Z-test; GNBNI, Gram negative bacilli not identified; N, no response; R, resistant; S, Bacteria sensible to the therapy; NT, no therapy; 3GCs, 3rd generation cephalosporin; MT, metronidazole; CCA, cholangiocarcinoma; PHC, carcinoma of the head of the pancreas; ACA, ampullary carcinoma; GBC, gallbladder carcinoma; CHL, cholelithiasis; CHA, cholangitis; CHP, chronic pancreatitis.
Therapy and general drug resistance
We observed that E. coli, K. pneumoniae, and P. aeruginosa showed a high percentage of resistance to third-generation cephalosporins (3GCs), aminoglycosides class, and quinolone group, especially to levofloxacin in cohort one and two were the several numbers of enrolled pts are enrolled presented and/or alive.
On the other hand, the analysis of susceptibility test showed that E. coli, K. pneumoniae, and P. aeruginosa had a percentage of sensibility to adopted carbapenem of about 70%.
Pancreatic/biliary tract diseases, microbiota, drugs, and correlation analysis
Regarding the pancreatic and biliary tract diseases, PHC was the most frequent disease in T1 (p<0.0001), CCA in T2 (p<0.0001), while GBC (p<0.0001) and ACA (p=0.0139) were more often seen in T3. At T3S, the most frequent pancreatic and biliary tract disease was CHL (p<0.0001), while less frequent diseases included PHC and GBC (p=0.0299). In other words, the PHC had the highest impact on dead patients within six months. About the antibiotic therapy, we observed that the most frequent treatments in T1 were meropenem (p<0.005) and imipenem (p<0.005), while the less commonly occurring therapy was levofloxacin (p<0.005). In T2, we more often encountered meropenem (p<0.005) and ertapenem (p<0.005), while the fewer common antibiotics were ciprofloxacin, levofloxacin, and 3CGs. In T3, there was no therapy, which was significant in any category. Conversely, in T3S, meropenem was the most frequent therapy identified (p<0.005). Fewer standard treatments used in T3S were aminoglycosides, levofloxacin, and 3GCs (p<0.005).
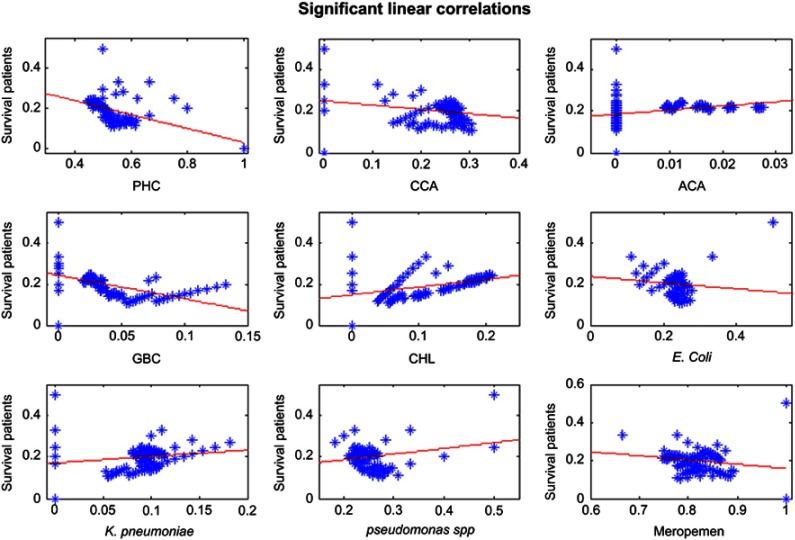
Table 3 shows univariate and multivariate linear correlation analysis considering as dependence variable: survival patients and independence variables: age, gender, most frequently: isolated strains (E coli, K pnumoniae, P. aeruginosa), underlying diseases (PHC, CCA, ACA, GBC, and CHL), and carbapenem class (meropenem, imipenem, and ertapenem).
Table 3.
Univariate and multivariate linear correlation analysis on the most frequent bacteria and disease, age, gender, and survival patients
| Linear correlation analysis | Univariate analysis | Multivariate analysis |
|---|---|---|
| Parameters | R (p-value) | Rpartial; p-value |
| Multiple linear correlation coefficient =1.0 | ||
| Survival patients/PHC | −0.45 (<0.0001) * | Rpartial= −0.99; p-value <0.0001 * |
| Survival patients/CCA | −0.22 (0.0062) * | Rpartial = −0.98; p-value <0.0001 * |
| Survival patients/ACA | 0.33 (<0.0001) * | Rpartial = −0.90; p-value <0.0001 * |
| Survival patients/GBC | −0.55 (<0.0001) * | Rpartial = −0.98; p-value <0.0001 * |
| Survival patients/CHL | 0.43 (<0.0001) * | Rpartial = −0.24; p-value =0.0040 * |
| Survival patients/E. coli | −0.21 (0.0088) * | Rpartial = 0.04; p-value =0.68 |
| Survival patients/K. pneumoniae | 0.16 (0.0495) * | Rpartial = 0.05; p-value =0.58 |
| Survival patients/Pseudomonas aeruginosa | 0.23 (0.0038) * | Rpartial = −0.07; p-value =0.45 |
| Survival patients/Meropenem | −0.20 (0.0157) * | Rpartial = 0.05; p-value =0.59 |
| Survival patients/Imipenem | 0.08 (0.31) | Rpartial = −0.02; p-value =0.84 |
| Survival patients/Ertapenem | −0.13 (0.11) | Rpartial = −0.08; p-value =0.38 |
| Survival patients/Age | −0.10 (0.20) | Rpartial = −0.16; p-value =0.06 |
| Survival patients/Gender | −0.09 (0.25) | Rpartial = −0.11; p-value =0.10 |
| Multiple linear correlation coefficient =0.63 | ||
| PHC/E. coli | 0.52 (<0.0001) * | Rpartial =0.29; p-value =0.0003 * |
| PHC/K. pneumoniae | −0.46 (<0.0001) * | Rpartial =−0.27; p-value =0.0008 * |
| PHC/Pseudomonas aeruginosa | 0.13 (0.12) | Rpartial =0.058; p-value =0.48 |
| Multiple linear correlation coefficient =0.59 | ||
| CCA/E. coli | −0.35 (<0.0001) * | Rpartial =−0.42; p-value <0.0001 * |
| CCA/K. pneumoniae | 0.42 (<0.0001) * | Rpartial =−0.09; p-value =0.26 |
| CCA/Pseudomonas aeruginosa | −0.36 (<0.0001) * | Rpartial =−0.43; p-value <0.0001 * |
| Multiple linear correlation coefficient =0.16 | ||
| GBC/E. coli | −0.12 (0.16) | Rpartial =0.01; p-value =0.93 |
| GBC/K. pneumoniae | 0.13 (0.11) | Rpartial =0.12; p-value =0.16 |
| GBC/Pseudomonas aeruginosa | 0.03 (0.70) | Rpartial =0.08; p-value =0.32 |
| Multiple linear correlation coefficient =0.16 | ||
| ACA/E. coli | −0.08 (0.31) | Rpartial =0.06; p-value =0.44 |
| ACA/K. pneumoniae | 0.25 (0.0017) * | Rpartial =0.20; p-value =0.0131 * |
| ACA/Pseudomonas aeruginosa | −0.12 (0.15) | Rpartial =0.04; p-value =0.65 |
| Multiple linear correlation coefficient =0.52 | ||
| CHL/E. coli | −0.21 (0.0099) * | Rpartial =−0.22; p-value =0.0083 * |
| CHL/K. pneumoniae | 0.43 (<0.0001) * | Rpartial =0.06; p-value =0.45 |
| CHL/Pseudomonas aeruginosa | −0.40 (<0.0001) * | Rpartial =−0.33; p-value <0.0001 * |
| Multiple linear correlation coefficient =0.59 | ||
| E coli/Meropenem | 0.36 (<0.0001) * | Rpartial =0.32; p-value =0.0001 * |
| E coli/Imipenem | 0.51 (<0.0001) * | Rpartial =0.49; p-value <0.0001 * |
| E coli/Ertapenem | 0.15 (0.06) | Rpartial = −0.30; p-value =0.0002 * |
| Multiple linear correlation coefficient =0.76 | ||
| K. pneumoniae/Meropenem | −0.24 (0.0027) * | Rpartial =0.10; p-value =0.24 |
| K. pneumoniae/Imipenem | −0.75 (<0.0001) * | Rpartial =−0.72; p-value <0.0001 * |
| K. pneumoniae/Ertapenem | −0.33 (<0.0001) * | Rpartial =0.02; p-value =0.65 |
| Multiple linear correlation coefficient =0.56 | ||
| Pseudomonas aeruginosa/Meropenem | 0.029 (0.72) | Rpartial =−0.35; p-value <0.0001 * |
| Pseudomonas aeruginosa/Imipenem | 0.45 (<0.0001) * | Rpartial =0.40; p-value <0.0001 * |
| Pseudomonas aeruginosa/Ertapenem | 0.35 (<0.0001) * | Rpartial =0.33; p-value <0.0001 * |
Notes: *significant test; R = Pearson’s linear correlation coefficient; Rpartial= the partial correlation coefficient is the coefficient of correlation of the variable with the dependent variable, adjusted for the effect of the other variables in the mode
Abbreviations: CCA, cholangiocarcinoma; PHC, carcinoma of the head of the pancreas; ACA, ampullary carcinoma; GBC, gallbladder carcinoma; CHL, cholelithiasis.
By multivariate analysis, the negative significant predictors of survival were: PHC (p<0.0001), CCA (p<0.0001), ACA (p<0.0001), GBC (p<0.0001), and CHL (p=0.0040). There were no significant positive predictors. In other words, the presence of PHC, CCA, ACA, GBC, and CHL implicated a decreasing of survival.
In univariate analysis, the survival was negatively correlated to PHC (p<0.0001), CCA (p<0.0001), GBC (p<0.0001), E. coli (p=0.0088), and meropenem (p=0.0157). Conversely, the survival was positively correlated to ACA (p<0.0001), CHL (p<0.0001), K. pneumoniae (p=0.0495), and P. aeruginosa (p=0.0038). Considering each variable individually, we found that the presence of PHC, CCA, GBC, E. Coli, and meropenem was connected to patients with low survival. On the other hand, ACA, CHL, K. pneumoniae, and P. aeruginosa were connected with patients who survived more in comparison to others.
Considering additional analyses, we observed that in univariate and multivariate analysis E. coli was a significant positive predictor of PHC, ie, the presence of E. coli is associated with PHC. In both univariate and multivariate analysis, K. pneumoniae was a significant negative predictor of PHC, ie, the presence of K. pneumoniae does not implicate the presence of PHC.
In the univariate and multivariate analysis, E. coli and P. aeruginosa were significant negative predictors of CCA. In other words, E. coli or P. aeruginosa. suggests the absence of CCA. Moreover, only in univariate analysis K. pneumoniae was positively correlated to CCA, and K. pneumoniae implicates CCA. About GBC, there were no significant correlations with E. coli, K. pneumoniae, and P. aeruginosa.
In the univariate and multivariate analysis, K. pneumoniae was a significant positive predictor of ACA, ie, the presence of K. pneumoniae implicates the diagnosis of ACA. In the univariate and multivariate analysis, E. coli and P. aeruginosa were significant negative predictors of gallstone disease, ie, the presence of E. coli or P. aeruginosa may implicate the absence of CHL.
In univariate analysis alone, K. pneumoniae was positively correlated to CHL, ie, the presence of K. pneumoniae would suggest CHL.
Figure 1 summarizes all significant linear correlations described in Table 3. Particularly in Figure 1, the dependence variable: survival patients was associated with the vertical axis. The independent variables: PHC, CCA, ACA, GBC, CHL, E coli, K. pneumoniae, P. aeruginosa, meropenem, were located on the horizontal axis. Regarding bacteria, the scatter plot showed a negative correlation between E. coli and survival variable. Moreover, the scatter plot showed a negative association between CCA and PHC and survival.
Figure 1.
Significant Linear correlations between independent variables: pancreas head carcinoma, cholangiocellular carcinoma, ampullary carcinoma, gallbladder carcinoma, gallbladder stone disease, E. coli, K pneumoniae, Pseudomonas spp., Meropenem and the dependent variable of survival of the patients. Also, the asterisks represented a pair of values (independence variable, dependence variable) and the red line indicated the best linear correlation model of the scatter plot points.
Abbreviations: CCA, cholangiocarcinoma; PHC, carcinoma of the head of the pancreas; ACA, ampullary carcinoma; GBC, gallbladder carcinoma; CHL, cholelithiasis.
By Kaplan–Meier survival curves comparison, among patients with cancer (CCA, GBC, PHC, or ACA) and no cancer (CHL, CHA, or CHP), we confirmed a significant difference (p-value <0.0001, log-rank test, Figure 2).
Finally, we considered the Cox proportional hazard regression to evaluate the effect of several risk factors on survival. The risk factors or covariates studied were represented by Age, Gender, Bacteria, and Disease variables. For this scope, two models were considered – the null model: −2ln(L0), where L0 is the likelihood to obtain the observations if the independent variables did not affect the outcome, and the full model: −2ln(L0), where L0 is the likelihood of achieving the views with all independent variables incorporated in the model. The difference between these two yields was estimated with the chi-square test, to define how well the independent variables may affect the outcome or dependent variable. By chi-square test, the p-value <0.0001, ie, there was evidence that at least one of the independent variables or covariates contributes to the prediction of the outcome. By this investigation, it results that only the presence of cancer provides a significant contribution to survival time in comparison to other covariates considered, as shown by Cox proportional hazard regression analysis (Figure 3 and Table 4).
Discussion
Bacteria and candida colonizing pancreatic and biliary tract tissues may be involved in chronic inflammation and cancer evolution.37 In the twenty-first century, scientists started hypothesizing that chronic inflammation caused by persistent bacterial infections might lead to carcinogenesis and bacterial toxins and secondary metabolites produced by the chronic bacterial infection might induce carcinogenesis, and some mechanisms of cholangiocarcinogenesis have been delineated.9,10,42
Emerging studies on pancreatic, biliary tract, and gallbladder disease have been identified as the significant pathogens implicated in inflammatory and tumor microenvironment (TME).43,44
In comparison to these studies, our study analyzed two proper further investigations: we analyzed both the survival rate of different cohorts of pats about pathogens identified during bile culture after the first diagnosis of BPS, and we examined the survival rate regarding anti-infective therapy according to results of antimicrobial tests.
Regarding the first point, we found that E. coli, P. aeruginosa, and K. pneumoniae are the leading bacteria isolated.
When we analyze these three Gram-negative pathogens each examined individually about the following variables: survival time (T1, T2, T3) and pathology of the biliopancreatic tract, the results obtained are different:
E. coli, P. aeruginosa, and K. pneumoniae were the most significant pathogens isolated in patients’ death within six months from diagnosis of PBD and again E. coli and P. aeruginosa were prevalent in patients’ death within the first year. Regarding underlying diseases, in general, the presence of E. coli, P. aeruginosa, and K. pneumoniae was statistically significant identified in the cancer population, and their presence reduces survival time.
In particular, E. coli seems to be the bacterium that most correlates with a reduction in survival and in univariate and multivariate analysis E. coli was a significant positive predictor of PHC.
These findings are in harmony with Costi et al who reported E. coli in the bile being significantly related to poor outcome in pancreaticoduodenectomies.45 A few years ago, we described an outbreak of colonization by ESBL-producing E. coli (ESBL-E. coli) in intensive care units.35,39,46–48 A variety of E. coli, called as ESBL-producing E. coli (ESBLEC), is currently considered a significant cause of bacteremia in cancer patients.49,50 These strains showed some microbiological determinants, including virulence factors, involving adhesion to and invasion of host cells, iron availability, toxic effects on host cells, or protecting factors against the host’s immune system.39,51 They are recognized as the etiologic agents of hospital infections mainly through the urinary tract. Moreover, they are playing a tremendous role in the field of transmission through the food chain, and therefore they can colonize healthy subjects and could be responsible for severe infections as soon as the decay of the immune system of elderly patients.52
Recently, in our geographical area, we have investigated the presence of E. coli ST131 in food animals.53,54 E. coli ST131 is increasing rapidly worldwide and shows resistance to fluoroquinolones. By antimicrobial susceptibility analysis, the percentage of sensibility to a fluoroquinolone was low, while most of our E. coli strains were susceptible only to carbapenem class. Moreover, analyzing the correlations described in Table 3 where E coli compared to K. pneumoniae and P. aeruginosa has a significant negative association with survival, this means that an increase of E. coli in bile leads to a decrease in survival, while this is not found for K. pneumoniae and P. aeruginosa. This result could be helpful in the management of pancreatic tract disorders. For example, knowing that E. coli is more incisive on the reduction of survival, other antibiotics could be used, especially in patients with PHC where the probability of E. coli was present in bile was higher than other bacteria.
Among the relationship between microorganisms and cancer of pancreatic and biliary system, we found that K. pneumoniae is the bacterium with a reduction in survival in CCA patients.
The isolation of pathogens has not always shown a negative correlation with the survival because in non-carcinomatous pathologies especially gallstone disease the findings of above-mentioned gram-negative bacilli as E. coli, P. aeruginosa, and K. pneumoniae had a negative predictor of the biliary calculi.
Therefore, we could confirm that it is the TME that influences the significance of the finding of some microorganisms. In the future, it would be interesting to investigate the protective role of Alcaligenes spp. in the gut microbiome.
Regarding the survival and anti-infective treatment, we found that E. coli, K. pneumoniae, and P. aeruginosa showed a high percentage of resistant to 3CGS, aminoglycosides class, and quinolone group, especially to levofloxacin. On the other hand, the analysis of susceptibility test showed that E. coli, K. pneumoniae, and P. aeruginosa had a percentage of sensibility to adopted carbapenem (meropenem, imipenem, and ertapenem) more than 70% of all isolated strains.
In fact, the prescription of meropenem due to the isolation of pathogens resistant to other class of antibiotics seems to be associated with a decrease in survival. The scatter plot for meropenem shows a negative linear correlation between survival and antibiotic, ie, if meropenem use/dosage increases, the survival decreases. On the other hand, the isolation of pathogens sensible to carbapenem class alone may be contributing to the emerging of particular multi-drug-resistant microbiota.
Moreover, in our study, K. pneumoniae was negatively associated with meropenem, imipenem, and ertapenem showing a decrease of sensitivity to the carbapenem class confirming two previously described cases.36
Resistant pathogens are increasingly reported in cancer patients and may be associated with cancer screening tests. The widespread use of these drugs can lead to the emergence of metallo-beta-lactamase strains as the authors have previously reported in NICU setting.55 Infectious disease consultants in an emergency setting often must prescribe an immediate antimicrobial therapy, which is based on co-morbidities such as type 2 diabetes mellitus, obesity, chronic liver disease, alcoholism. Mono- or combined antimicrobial therapy needs to be chosen considering the most favorable pharmacokinetic/pharmacodynamic profiles, and tissue penetration against the isolated bacteria, as well as the acquisition and interpretation of the hospital ecology.33,34
The Cox proportional-hazard regression indicates that only the presence of cancer disease per se provides a significant contribution to survival time in comparison to other covariates.
In conclusions, our study suggests that some strains isolate in bile samples may be considered within the group of risk factors in carcinogenesis and/or progression of hepato-biliary malignancy.
Moreover, the knowledge of bile microbiota and susceptibility test results highlight the necessity to consider the multidisciplinary management of patients with inflammation and cancer of pancreatic and biliary tract disease PBD. The finding that pathogens isolated in gut microbiota belong to the same class of pathogens responsible for sepsis in cancer patients may indicate that dysbiosis favors the production of genotoxins and metabolites inducing the dysregulation of the immune response, which may favor carcinogenesis.
The primary limitation may entail the local event (single-center). A multicentric investigation involving several geographic areas may be warranted to address public health policies. This aspect may be important because the colonization by resistant germs could significantly influence the future medical approach.56 The development of inflammatory bowel disease that may be associated with biliary diseases highlights the qualitative and quantitative disorders of the microbiota of the intestine (dysbiosis). Increasing evidence indicates that dysbiosis favors indeed the production of genotoxins and metabolites that induce dysregulation of the immune response of the most closely associated with carcinogenesis.57 Some microorganisms occur in specific pancreatic and biliary diseases, and our data may be vital in addressing the anti-infective therapy in patients harboring PBD neoplasms.
Acknowledgments
We thank the patients and their families for supporting this study. This study has been supported by the University of Palermo (intramural grant).
Author contributions
All authors contributed to data analysis, drafting and revising the article, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Disclosure
Dr. C. Sergi has received research funding from the Women and Children’s Health Research Institute Hair Massacure, WCHRI Grant Application ID #2096. Dr. C. Sergi has also received fees for serving as a grant reviewer for the Women’s and Children Health Research Institute, Canada, Health and Medical Research Fund (HMRF), Hong Kong Special Administrative Region, Polish National Health Center, and as a consultant for Guidepoint Global LLC. The authors report no other conflicts of interest in this work.
References
- 1.Wang WL, Xu SY, Ren ZG, Tao L, Jiang JW, Zheng SS. Application of metagenomics in the human gut microbiome. World J Gastroenterol. 2015;21(3):803–814. doi: 10.3748/wjg.v21.i3.803 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wells GR, Taylor EW, Lindsay G, Morton L; West of Scotland Surgical Infection Study Group. Relationship between bile colonization, high-risk factors and postoperative sepsis in patients undergoing biliary tract operations while receiving a prophylactic antibiotic. Br J Surg. 1989;76(4):374–377. [DOI] [PubMed] [Google Scholar]
- 3.von Elm E, Altman DG, Egger M, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet. 2007;370(9596):1453–1457. doi: 10.1016/S0140-6736(07)61602-X [DOI] [PubMed] [Google Scholar]
- 4.Verdier J, Luedde T, Sellge G. Biliary mucosal barrier and microbiome. Viszeralmedizin. 2015;31(3):156–161. doi: 10.1159/000431071 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tabibian JH, O’Hara SP, Trussoni CE, et al. Absence of the intestinal microbiota exacerbates hepatobiliary disease in a murine model of primary sclerosing cholangitis. Hepatology. 2016;63(1):185–196. doi: 10.1002/hep.27927 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tabibian JH, Varghese C, LaRusso NF, O’Hara SP. The enteric microbiome in hepatobiliary health and disease. Liver Int. 2016;36(4):480–487. doi: 10.1111/liv.13009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kummen M, Holm K, Anmarkrud JA, et al. The gut microbial profile in patients with primary sclerosing cholangitis is distinct from patients with ulcerative colitis without biliary disease and healthy controls. Gut. 2017;66(4):611–619. doi: 10.1136/gutjnl-2015-310500 [DOI] [PubMed] [Google Scholar]
- 8.Shen H, Ye F, Xie L, et al. Metagenomic sequencing of bile from gallstone patients to identify different microbial community patterns and novel biliary bacteria. Sci Rep. 2015;5:17450. doi: 10.1038/srep17450 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Al-Bahrani R, Abuetabh Y, Zeitouni N, Sergi C. Cholangiocarcinoma: risk factors, environmental influences and oncogenesis. Ann Clin Lab Sci. 2013;43(2):195–210. [PubMed] [Google Scholar]
- 10.Al-Bahrani R, Nagamori S, Leng R, Petryk A, Sergi C. Differential expression of sonic hedgehog protein in human hepatocellular carcinoma and intrahepatic cholangiocarcinoma. Pathol Oncol Res. 2015;21(4):901–908. doi: 10.1007/s12253-015-9918-7 [DOI] [PubMed] [Google Scholar]
- 11.Bahitham W, Liao X, Peng F, et al. Mitochondriome and cholangiocellular carcinoma. PLoS One. 2014;9(8):e104694. doi: 10.1371/journal.pone.0104694 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Callea F, Sergi C, Fabbretti G, Brisigotti M, Cozzutto C, Medicina D. Precancerous lesions of the biliary tree. J Surg Oncol Suppl. 1993;3:131–133. [DOI] [PubMed] [Google Scholar]
- 13.Bridgewater JA, Goodman KA, Kalyan A, Mulcahy MF. Biliary tract cancer: epidemiology, radiotherapy, and molecular profiling. Am Soc Clin Oncol Educ Book. 2016;35:e194–e203. doi: 10.1200/EDBK_160831 [DOI] [PubMed] [Google Scholar]
- 14.Ebata T, Ercolani G, Alvaro D, Ribero D, Di Tommaso L, Valle JW. Current status on cholangiocarcinoma and gallbladder cancer. Liver Cancer. 2016;6(1):59–65. doi: 10.1159/000449493 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ilic M, Ilic I. Epidemiology of pancreatic cancer. World J Gastroenterol. 2016;22(44):9694–9705. doi: 10.3748/wjg.v22.i44.9694 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pomakova D, Segal BH. Prevention of infection in cancer patients. Cancer Treat Res. 2014;161:485–511. doi: 10.1007/978-3-319-04220-6_16 [DOI] [PubMed] [Google Scholar]
- 17.Bonnetain F, Bonsing B, Conroy T, et al. Guidelines for time-to-event end-point definitions in trials for pancreatic cancer. Results of the DATECAN initiative (Definition for the Assessment of Time-to-event End-points in CANcer trials). Eur J Cancer. 2014;50(17):2983–2993. doi: 10.1016/j.ejca.2014.07.011 [DOI] [PubMed] [Google Scholar]
- 18.Sudo T, Murakami Y, Uemura K, et al. Specific antibiotic prophylaxis based on bile cultures is required to prevent postoperative infectious complications in pancreatoduodenectomy patients who have undergone preoperative biliary drainage. World J Surg. 2007;31(11):2230–2235. doi: 10.1007/s00268-007-9210-4 [DOI] [PubMed] [Google Scholar]
- 19.Serra N, Di Carlo P, Gulotta G, et al. Bactibilia in women affected with diseases of the biliary tract and pancreas. A STROBE guidelines-adherent cross-sectional study in southern Italy. J Med Microbiol. 2018;67(8):1090–1095. doi: 10.1099/jmm.0.000787 [DOI] [PubMed] [Google Scholar]
- 20.Di Carlo P, Serra N, Gulotta G, et al. Bactibilia in diseases of the biliary tract and pancreatic gland in patients older than 80 years: a STROBE-retrospective cohort study in a teaching hospital in Italy. Eur J Clin Microbiol Infect Dis. 2018;37(5):953–958. doi: 10.1007/s10096-018-3213-y [DOI] [PubMed] [Google Scholar]
- 21.Herzog T, Belyaev O, Hessam S, et al. Bacteribilia with resistant microorganisms after preoperative biliary drainage – the influence of bacteria on postoperative outcome. Scand J Gastroenterol. 2012;47(7):827–835. doi: 10.3109/00365521.2012.679684 [DOI] [PubMed] [Google Scholar]
- 22.Gartner S, Kruger J, Aghdassi AA, et al. Nutrition in pancreatic cancer: a review. Gastrointest Tumors. 2016;2(4):195–202. doi: 10.1159/000442873 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mueller TC, Burmeister MA, Bachmann J, Martignoni ME. Cachexia and pancreatic cancer: are there treatment options? World J Gastroenterol. 2014;20(28):9361–9373. doi: 10.3748/wjg.v20.i28.9361 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Iovene MR, Bombace F, Maresca R, et al. Intestinal dysbiosis and yeast isolation in stool of subjects with autism spectrum disorders. Mycopathologia. 2017;182(3–4):349–363. doi: 10.1007/s11046-016-0068-6 [DOI] [PubMed] [Google Scholar]
- 25.Scheufele F, Aichinger L, Jager C, et al. Effect of preoperative biliary drainage on bacterial flora in bile of patients with periampullary cancer. Br J Surg. 2017;104(2):e182–e188. doi: 10.1002/bjs.10450 [DOI] [PubMed] [Google Scholar]
- 26.Hinchliffe RJ, Earnshaw JJ. Surgical infection. Br J Surg. 2017;104(2):e8–e10. doi: 10.1002/bjs.10468 [DOI] [PubMed] [Google Scholar]
- 27.Rodolico V, Di Carlo P, Gulotta G, et al. Intra-abdominal Candida spp infection in acute abdomen in a quality assurance (QA)-certified academic setting. J Clin Pathol 2016;70(77):579–583. doi: 10.1136/jclinpath-2016-203936 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.D‘Arpa F, Tutino R, Battaglia EO, et al. Post-ERCP pancreatitis. A single center experience and an update on prevention strategies. Ann Ital Chir. 2015;86(3):234–238. [PubMed] [Google Scholar]
- 29.Di Carlo P, Di Vita G, Guadagnino G, et al. Surgical pathology and the diagnosis of invasive visceral yeast infection: two case reports and literature review. World J Emerg Surg. 2013;8(1):38. doi: 10.1186/1749-7922-8-38 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Domagk D, Oppong KW, Aabakken L, et al. Performance measures for ERCP and endoscopic ultrasound: a European Society of Gastrointestinal Endoscopy (ESGE) quality improvement initiative. Endoscopy. 2018;50(11):1116–1127. doi: 10.1055/a-0749-8767 [DOI] [PubMed] [Google Scholar]
- 31.Sinatra I, Carubia L, Marchese V, et al. Prevalence survey of healthcare-associated infections and antimicrobial use at the University Hospital “Paolo Giaccone”, Palermo, Italy. J Prev Med Hyg. 2013;54(4):200–204. [PMC free article] [PubMed] [Google Scholar]
- 32.Grosso G, Pajak A, Mistretta A, et al. Protective role of the Mediterranean diet on several cardiovascular risk factors: evidence from Sicily, southern Italy. Nutr Metab Cardiovasc Dis. 2014;24(4):370–377. doi: 10.1016/j.numecd.2013.09.020 [DOI] [PubMed] [Google Scholar]
- 33.Agrusa A, Frazzetta G, Chianetta D, et al. “Relaparoscopic” management of surgical complications: the experience of an Emergency Center. Surg Endosc. 2016;30(7):2804–2810. doi: 10.1007/s00464-015-4558-2 [DOI] [PubMed] [Google Scholar]
- 34.Agrusa A, Romano G, Frazzetta G, et al. Role and outcomes of laparoscopic cholecystectomy in the elderly. Int J Surg. 2014;12 Suppl 2:S37–S39. doi: 10.1016/j.ijsu.2014.08.385 [DOI] [PubMed] [Google Scholar]
- 35.Di Carlo P, Gulotta G, Casuccio A, et al. KPC-3 Klebsiella pneumoniae ST258 clone infection in postoperative abdominal surgery patients in an intensive care setting: analysis of a case series of 30 patients. BMC Anesthesiol. 2013;13(1):13. doi: 10.1186/1471-2253-13-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Di Carlo P, Pantuso G, Cusimano A, et al. Two cases of monomicrobial intraabdominal abscesses due to KPC–3 Klebsiella pneumoniae ST258 clone. BMC Gastroenterol. 2011;11:103. doi: 10.1186/1471-230X-11-93 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Rodolico V, Di Carlo P, Gulotta G, et al. Intra-abdominal Candida spp infection in acute abdomen in a quality assurance (QA)-certified academic setting. J Clin Pathol. 2017;70(7):579–583. doi: 10.1136/jclinpath-2016-203936 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bonura C, Giuffre M, Aleo A, et al. An update of the evolving epidemic of blaKPC Carrying Klebsiella pneumoniae in Sicily, Italy, 2014: emergence of multiple non-ST258 clones. PLoS One. 2015;10(7):e0132936. doi: 10.1371/journal.pone.0132936 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Giuffre M, Geraci DM, Bonura C, et al. The increasing challenge of multidrug-resistant gram-negative bacilli: results of a 5-year active surveillance program in a neonatal intensive care unit. Medicine (Baltimore). 2016;95(10):e3016. doi: 10.1097/MD.0000000000004864 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Brown DF, Wootton M, Howe RA. Antimicrobial susceptibility testing breakpoints and methods from BSAC to EUCAST. J Antimicrob Chemother. 2016;71(1):3–5. doi: 10.1093/jac/dkv287 [DOI] [PubMed] [Google Scholar]
- 41.Baron EJ, Miller JM, Weinstein MP, et al. A guide to utilization of the microbiology laboratory for diagnosis of infectious diseases: 2013 recommendations by the Infectious Diseases Society of America (IDSA) and the American Society for Microbiology (ASM) (a). Clin Infect Dis. 2013;57(4):e22–e121. doi: 10.1093/cid/cit278 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Abuetabh Y, Garcia E, Persad S, Sergi C. Molecular events of cholangiocarcinogenesis. Ann Clin Lab Sci. 2010;40(2):189. [Google Scholar]
- 43.Wang M, Zhao J, Zhang L, et al. Role of tumor microenvironment in tumorigenesis. J Cancer. 2017;8(5):761–773. doi: 10.7150/jca.17648 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Maekawa T, Fukaya R, Takamatsu S, et al. Possible involvement of Enterococcus infection in the pathogenesis of chronic pancreatitis and cancer. Biochem Biophys Res Commun. 2018;506(4):962–969. doi: 10.1016/j.bbrc.2018.10.169 [DOI] [PubMed] [Google Scholar]
- 45.Costi R, De Pastena M, Malleo G, et al. Poor results of pancreatoduodenectomy in high-risk patients with endoscopic stent and bile colonization are associated with E. coli, diabetes and advanced age. J Gastrointest Surg. 2016;20(7):1359–1367. doi: 10.1007/s11605-016-3158-3 [DOI] [PubMed] [Google Scholar]
- 46.Mammina C, Cala C, Bonura C, et al. Polyclonal non multiresistant methicillin resistant Staphylococcus aureus isolates from clinical cases of infection occurring in Palermo, Italy, during a one-year surveillance period. Ann Clin Microbiol Antimicrob. 2012;11:17. doi: 10.1186/1476-0711-11-17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Mammina C, Aleo A, Bonura C, et al. Multiclonal emergence of carbapenem-resistant Klebsiella pneumoniae in Tuscany, Italy. Int J Antimicrob Agents. 2010;36(6):576–578. doi: 10.1016/j.ijantimicag.2010.08.004 [DOI] [PubMed] [Google Scholar]
- 48.Mammina C, Palma DM, Bonura C, et al. Outbreak of infection with Klebsiella pneumoniae sequence type 258 producing Klebsiella pneumoniae Carbapenemase 3 in an intensive care unit in Italy. J Clin Microbiol. 2010;48(4):1506–1507. doi: 10.1128/JCM.00315-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Cornejo-Juarez P, Suarez-Cuenca JA, Volkow-Fernandez P, et al. Fecal ESBL Escherichia coli carriage as a risk factor for bacteremia in patients with hematological malignancies. Support Care Cancer. 2016;24(1):253–259. doi: 10.1007/s00520-015-2772-z [DOI] [PubMed] [Google Scholar]
- 50.Medboua-Benbalagh C, Touati A, Kermas R, et al. Fecal carriage of extended-spectrum beta-lactamase-producing enterobacteriaceae strains is associated with worse outcome in patients hospitalized in the pediatric oncology unit of beni-messous hospital in Algiers, Algeria. Microb Drug Resist. 2017. doi: 10.1089/mdr.2016.0153 [DOI] [PubMed] [Google Scholar]
- 51.Greve AS, Skals M, Fagerberg SK, et al. P2X1, P2X4, and P2X7 receptor knock out mice expose differential outcome of sepsis induced by alpha-haemolysin producing escherichia coli. Front Cell Infect Microbiol. 2017;7:113. doi: 10.3389/fcimb.2017.00517 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Ghodousi A, Bonura C, Di Carlo P, van Leeuwen WB, Mammina C. Extraintestinal pathogenic Escherichia coli sequence type 131 H30-R and H30-Rx subclones in retail chicken meat, Italy. Int J Food Microbiol. 2016;228:10–13. doi: 10.1016/j.ijfoodmicro.2016.04.004 [DOI] [PubMed] [Google Scholar]
- 53.Caruso G, Giammanco A, Cardamone C, et al. Extra-intestinal fluoroquinolone-resistant escherichia coli strains isolated from meat. Biomed Res Int. 2018;2018:8714975. doi: 10.1155/2018/8714975 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Nicolas-Chanoine MH, Bertrand X, Madec JY. Escherichia coli ST131, an intriguing clonal group. Clin Microbiol Rev. 2014;27(3):543–574. doi: 10.1128/CMR.00125-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Mazzariol A, Mammina C, Koncan R, et al. A novel VIM-type metallo-beta-lactamase (VIM-14) in a Pseudomonas aeruginosa clinical isolate from a neonatal intensive care unit. Clin Microbiol Infect. 2011;17(5):722–724. doi: 10.1111/j.1469-0691.2010.03424.x [DOI] [PubMed] [Google Scholar]
- 56.Zitvogel L, Galluzzi L, Viaud S, et al. Cancer and the gut microbiota: an unexpected link. Sci Transl Med. 2015;7(271):271ps271. doi: 10.1126/scitranslmed.aad3106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Tomasello G, Tralongo P, Damiani P, et al. Dismicrobism in inflammatory bowel disease and colorectal cancer: changes in response of colocytes. World J Gastroenterol. 2014;20(48):18121–18130. doi: 10.3748/wjg.v20.i48.18121 [DOI] [PMC free article] [PubMed] [Google Scholar]