Abstract
Background
We used population-level Australian data to estimate prevalence, age of onset and speed of transitions across stages of alcohol and cannabis use, abuse and dependence, and remission from disorder, and consider the potential impacts that an individual’s age cohort’s level of substance use predicted transitions into and out of substance use.
Methods
Data on use, DSM-IV use disorders, and remission from these disorders were collected from participants (n=8463) in the 2007 Australian National Survey of Mental Health and Wellbeing using the Composite International Diagnostic Interview.
Results
Lifetime prevalence (95% confidence interval) of alcohol use, regular use, abuse and dependence were 94.1% (93.3–94.8%), 64.5% (62.9–66.2%), 18.7% (17.4–19.9%) and 4.0% (3.4–4.6%). Lifetime prevalence (standard error) of cannabis use, abuse and dependence were 19.8% (18.6–20.9%), 4.4% (3.8–5.0%) and 1.9% (1.5–2.4%). Among those with the disorder, rates of remission from cannabis abuse, alcohol abuse, cannabis dependence and alcohol dependence were 90.5% (87.4–93.6%), 86.2% (83.8–88.7%), 79.6% (71.1–88.1%) and 53.8% (46.6–61.0%). Increases in the estimated proportion of people in the respondent’s age cohort who used alcohol/cannabis as of a given age were significantly associated with most transitions from use through to remission beginning at the same age.
Conclusions
Clear associations were documented between cohort-level prevalence of substance use and personal risk of subsequent transitions of from use to greater substance involvement. This relationship remained significant over and above associations involving the individual’s age of initiation. These findings have important implications for our understanding of the causal pathways into and out of problematic substance use.
Keywords: alcohol, cannabis, abuse, dependence, remission, cohort
Introduction
Increased understanding of the natural history of substance use disorders and transitions through the stages (initiation, transition to and remission from problems) is necessary to better identify prevention and treatment opportunities, targets, and optimal timing. Research on the trajectories of use has been carried out but has most often considered only the transition between use and dependence [e.g. 1,2] or focused on specific populations (e.g. young adults and people seeking treatment [3–5]).
The general population studies that have explored the natural history of substance use show that commonly-identified social contextual risk factors have a differential role according to transition stage [2,6–10]. For example, substance use is highly linked to social and peer-level variables [11] and there is evidence to suggest that the extent to which behaviour is normative may be associated with adverse outcomes [12,13].
Previous studies have consistently reported chronological age, historical period (“secular influences”) and birth cohort effects associated with differences in substance use and related problems [14–17]. Even the well-documented gender differences in substance use and disorders have been found to be associated with age, period and cohort effects [18–20]. Many studies have documented age related differences in substance use and related problems and these differences are usually attributed at least in part to developmental and maturational factors especially when cross-sectional comparisons are made across a sample comprised of a broad age range of a population [21–23]. However, individuals are also strongly influenced by the broader social contextual period effects.
Substance use-related period influences, including both risk and protective factors (e.g. substance use norms, enforcement of sanctions, substance availability, and perceptions of risk), have varied widely across geographical locations and in different time periods in history. Birth cohort effects more focally include the shared social and environmental influences on the individuals born at particular times as they mature as a group, experiencing the extant period effects including changes in the period effects over time. There are complex issues involved in distinguishing period and cohort effects [24,25], and while there is evidence of both influences, research has shown that substance use behaviours are especially related to cohort effects [17,20,26], which may filter or modify period effects and perhaps exert other social and peer influences. It may also be that cohort effects vary at different ages and stages of use.
Using data from a national study of Australian adults sampled across all cohorts in the population, the aims of the present study were to estimate the prevalence, age of onset and speed of transitioning across stages of alcohol and cannabis use, abuse and dependence, and remission from abuse and dependence in the Australian population, and to determine the impact that an individual’s age cohort’s level of substance use has on transitioning between these stages. We hypothesised that involvement in to, and out of, all stages of involvement with alcohol is largely impacted by the prevalence of its’ use among similarly aged peers such that risk of transitioning to all stages increases with prevalence of cohort use.
Method
Sample
Data from the Confidentialised Unit Record File of the 2007 National Survey of Mental Health and Well-Being (NSMHWB) were obtained from the Australian Bureau of Statistics. The 2007 NSMHWB was conducted by trained Australian Bureau of Statistics interviewers between August and December 2007. The aim of the survey was to provide reliable estimates of mental disorders at a national level. The 2007 NSMHWB sample of 17,352 dwellings was selected using a stratified, multistage area probability sample of people aged 16–85 years in private dwellings across all Australian states and territories excluding very remote areas. The area-based selection ensured that all sections of the population living in private dwellings within the geographical scope of the survey were represented. Non-private dwellings (hospitals, nursing homes, prisons, hotels) were not sampled. After removal of households with no in-scope respondents, and vacant, under construction or derelict dwellings, the effective sample size was reduced to 14,805 dwellings. All interviews were conducted in English, meaning that non-English speakers were excluded from the sample. However, those persons unable to answer themselves but who otherwise fell within the survey’s scope are represented in statistical outputs through inclusion in the population benchmarks used for weighting, a standard approach implemented by the Australian Bureau of Statistics [27]. Each interview was conducted in person using computer assisted interviewing and took approximately 90 minutes to complete.
There were 8841 participants aged 16 and over (8463 participants when limited to those aged 18 years and over, of which 50.4% (standard error = 0.8) were female), with a response rate of 60%. Due to the lower than expected response rate (it was expected that a 75% response rate would be achieved), extensive non-response analyses were undertaken to assess the reliability of the survey estimates. A purposive sample of fully non-responding households in two metropolitan areas, Sydney and Perth, was followed up with a short-form interview, to gain a qualitative assessment of non-response bias. The study indicated the impact of non-response to be small at the aggregate level, but possible underestimation of the prevalence of mental disorders may exist for men, young people and those residing in Perth. The final sample represented an estimated population count of 16,015,300 Australian adults. Further information about the procedure and instrument is published elsewhere [28].
The 2007 NSMHWB used the World Mental Health Survey Initiative version of the Composite International Diagnostic Interview Version 3.0 (WMH-CIDI 3.0) [29]. This interview has undergone extensive methodological development and testing and has been used in household surveys in at least 28 countries around the world. This instrument collects both diagnostic information on a broad range of mental disorders and information on risk factors, impacts, patterns and treatment of mental disorders. There were some modifications made to the WMH-CIDI to tailor the survey to the Australian context.
All analyses were based on weighted data, accounting for stratification and clustering. The application of the weights ensured the data were representative of the national population. Person weights and replicate weights generated by the Australian Bureau of Statistics were obtained from the Confidentialised Unit Record File [30].
Assessment of Alcohol and Cannabis Use Disorders
The WMH-CIDI produces diagnostic information according to the American Psychiatric Association’s Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM- IV) [31]. The WMH-CIDI uses a lifetime time frame. Diagnoses were derived using standard WMH-CIDI diagnostic algorithms and the lifetime DSM-IV diagnosis criteria are used in the current report.
In order to minimise unnecessary respondent burden, questions regarding alcohol use disorders were asked of all people who, in the year they drank most, drank alcohol at least three days per week or consumed at least three standard (10 g) alcoholic drinks per drinking day. Questions about cannabis use disorders were asked of those who had used cannabis at least five times in their lifetime. These questions were asked of 5522 alcohol and 1639 cannabis users (N=5444 for alcohol and N=1606 for cannabis when limited to 18 years or older).
Data Analysis
We looked at the age of onset and speed of transition between stages. For alcohol, these stages were use (first time drank a standard alcoholic drink), regular use (drank alcohol on at least three days per week; or at least three standard alcoholic drinks per drinking day in the year they drank most), DSM-IV abuse without dependence and DSM-IV dependence. For cannabis, they were age of onset among people who used more than five times in their life, DSM-IV abuse without dependence, and DSM-IV dependence. We also assessed remission from dependence and from abuse without dependence, where remission was defined as the absence of all disorder related symptoms for more than 12 months prior to the interview.
All analyses were carried out using SAS Version 9.4. Life-table (actuarial) estimates of the survival functions for age of onset and remission were produced using the SAS PROC LIFETEST procedure and are reported as weighted prevalence (95% confidence interval). The associations of cohort-level lifetime prevalence of use as of given ages controlling for basic socio-demographics with these transitions were assessed using discrete-time survival models in SAS PROC SURVEYLOGISTIC with person-year the unit of analysis and a logistic link function [32]. We defined a contextual variable to represent the level of alcohol/cannabis use in an individuals’ birth cohort to estimate the effect of changes in use over time. An individual’s birth cohort was based on their year of birth +/− 5 years, which created 11-year wide cohorts centred around each year of birth. The cohort widths were reduced for those aged between 18 and 22 years to, as close as possible, ensure symmetry around birth year; total band width was of size two for 18-year olds (18–19), three for 19-year olds (18–20), five for 20-year olds (18–22), seven for 21-year olds (18–24) and nine for 22-year olds (18–26). Cohorts were top-coded for those aged 65 or older. The predictor variable was the estimated proportion of people (/10) in the individual’s birth cohort who had used the specific substance (either alcohol or cannabis) by the prior person year. In order to capture only the most prominent changes in cohort use, cohort use prevalence was set to zero for person years below the age of 12 and top-coded for 30 years and over.
Predictor variables were sex, age of person year (<=14, 15–17, 18–20, 21–24, 25–29 and 30+ for all use/use disorder models and <=18, 19–20, 21–22, 23–24, 25–29, 30–39 and 40+ for remission from alcohol abuse or dependence), time-varying education level (student, low, low/medium, medium/high or high), age of commencing use (except for modelling commencement of use) defined as early youth, mid-teens or adulthood and speed of transition from use to abuse or dependence defined as early, mid or late tertiles (only for remission from alcohol abuse or dependence). Low education is defined as having completed 11 years or less, low/medium as completion of 12 years, medium/high as 13–15 years and high as 16 or more years.
Results
Prevalence of use, use disorders and remission
Lifetime prevalence estimates for alcohol and cannabis use and use disorders are shown in Table 1. Prevalence of alcohol use, regular use, abuse and dependence of alcohol were 94.1%, 64.5%, 18.7% and 4.0%, respectively. One in five (19.8%) had used cannabis more than five times during their lifetime; 1.9% had been dependent upon cannabis.
Table 1:
Prevalence of levels of involvement with alcohol and cannabis use, Australia
| Alcohol | Cannabis6 | |||||
|---|---|---|---|---|---|---|
| N | Weighted prevalence (%) | 95% CI | N | Weighted prevalence (%) | 95% CI | |
| Prevalence1,2 | ||||||
| Use | 8463 | 94.1 | 93.3–94.8 | 8,463 | 19.8 | 18.6–20.9 |
| Regular use4,5 | 8463 | 64.5 | 62.9–66.2 | |||
| Abuse | 8463 | 18.7 | 17.4–19.9 | 8,463 | 4.4 | 3.8–5.0 |
| Dependence | 8463 | 4.0 | 3.4–4.6 | 8,463 | 1.9 | 1.5–2.4 |
| Remission from abuse | 8463 | 16.1 | 14.9–17.3 | 8,463 | 4.0 | 3.4–4.6 |
| Remission from dependence | 8463 | 2.1 | 1.7–2.6 | 8,463 | 1.5 | 1.2–1.9 |
| Conditional prevalence3 | ||||||
| Regular use4 | use | 7945 | 68.6 | 66.9–70.3 | |||
| Abuse | use | 7945 | 19.9 | 18.5–21.2 | 1,606 | 22.2 | 19.3–25.0 |
| Dependence | use | 7945 | 4.2 | 3.7–4.8 | 1,606 | 9.8 | 7.5–12.2 |
| Remission from abuse| LT abuse W/O dependence | 1464 | 86.2 | 83.8–88.7 | 340 | 90.5 | 87.4–93.6 |
| Remission from dependence| LT dependence | 342 | 53.8 | 46.6–61.0 | 144 | 79.6 | 71.1–88.1 |
Lifetime.
Excludes people aged under 18 at the time of interview.
Inclusion in the denominator is conditional on persons having met a certain level of alcohol involvement e.g. ‘Regular use | use’ is regular use among persons who had ever used alcohol.
Regular use of cannabis was not assessed.
Prevalence of lifetime abuse with or without dependence was 22.1(0.6) for alcohol and 6.1(0.3) for cannabis.
Cannabis use defined as having used more than 5 times in lifetime.
CI, confidence interval; LT, lifetime; SE, standard error; W/O, without.
Once conditioned on use, a higher percentage of cannabis users compared to alcohol users developed abuse (22.2% versus 19.9%) and dependence (9.8% versus 4.2%). Those with cannabis use disorders also had a higher prevalence of remission than people with alcohol use disorders; for example, 79.6% of people with lifetime cannabis dependence had remitted by the time of interview, compared to just over half (53.8%) of people with alcohol dependence.
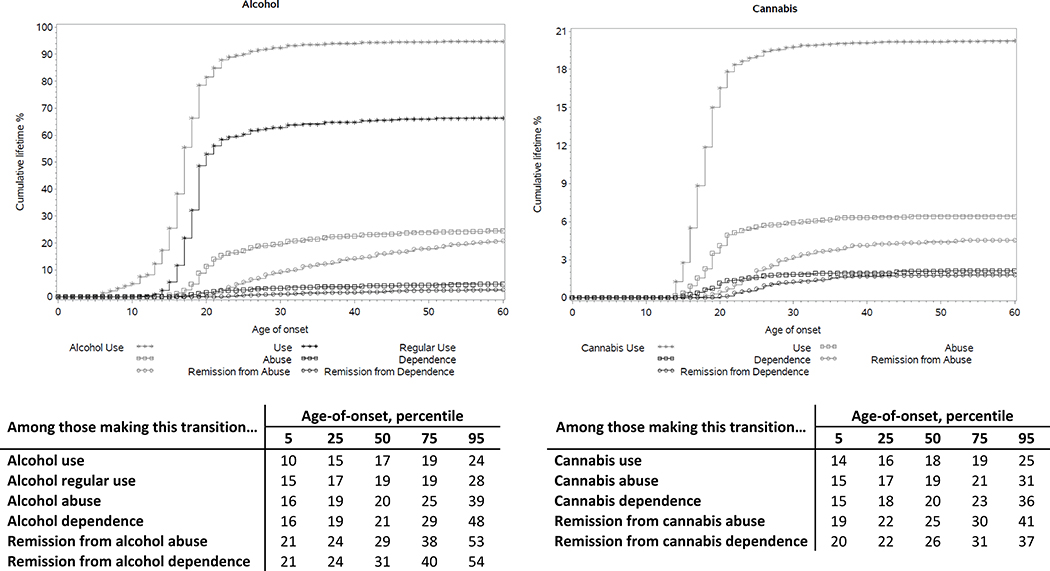
Age of onset distributions
Figure 1 shows the cumulative age of onset (AOO) curves for onset of alcohol and cannabis use, abuse, dependence, remission from abuse and remission from dependence. The onset of use for both alcohol and cannabis largely occurred by age 19 (75th percentile for both alcohol and cannabis). Onset of cannabis abuse and dependence typically occurred at earlier ages than for alcohol abuse and dependence; for example, the 75th percentile for cannabis abuse onset was 21 years, compared to 25 years for alcohol abuse.
Figure 1:
Age of onset of alcohol use, regular use, use disorder, and remission, and cannabis use, use disorder and remission, Australia; Y-axis scales range from 0–100% for alcohol and 0–21% for cannabis
Remission AOO curves also showed that remission from cannabis abuse and dependence occurred at earlier ages than for remission from alcohol use disorders. For example, the 75th percentile for remission of alcohol dependence was age 40, compared to 31 years for cannabis dependence. Cumulative AOO curves among those that reached each stage, and remission AOO curves among those with the disorder, are shown in the Appendix (Figure S1 and S2, respectively).
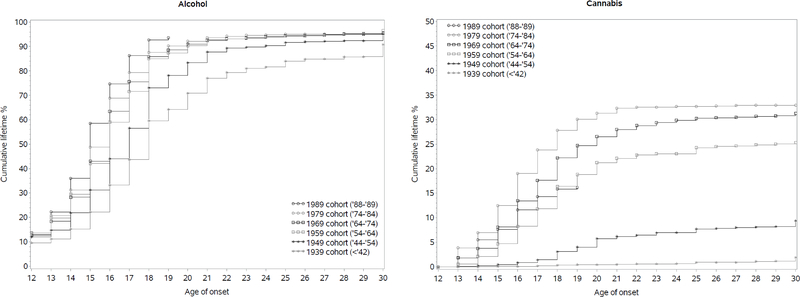
AOO curves for alcohol and cannabis use, in selected birth cohorts, are shown in Figure 2. The median age of onset of alcohol and cannabis use both decreased for alcohol and cannabis use in more recent cohorts, and particularly for cannabis use, overall levels of use reached much higher levels in more recent cohorts, with the exception that those in the 1989 cohort (which includes those born in ‘88 and ‘89) had lower levels of cannabis use compared to the 1979, 1969 and 1959 cohorts (all +/− 5 years) by the age of 19.
Figure 2:
Age of onset curve for alcohol and cannabis use among selected birth cohorts, Australia
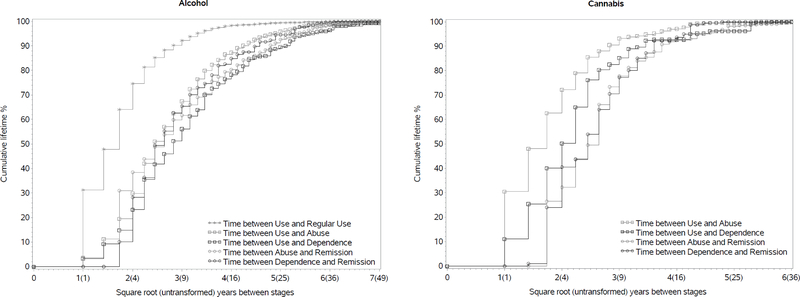
Time to transition across stages of involvement with alcohol and cannabis use
Figure 3 shows the cumulative curves for time between stages for alcohol and cannabis. For alcohol, the transition from initial use to regular use showed the fastest transition speed, with more than half of all individuals who become regular users doing so within three years of initial use. The time lag between onset of use to disorder was longer for alcohol than cannabis: for alcohol dependence for example, 75% of alcohol dependence cases had developed 15 years after onset of use; for cannabis dependence, 75% of cases had begun six years after onset of use.
Figure 3:
Transition times between alcohol use, regular use, use disorder and remission, and cannabis use, use disorder and remission, Australia
The time from onset to remission of either abuse or dependence was similar within alcohol and cannabis. For example, around 75% of cases of alcohol abuse and alcohol dependence had remitted by 13 years after onset of the disorder, and 75% of cannabis abuse and cannabis dependence had remitted by 9 years after onset of the disorder.
Predictors of transition between stages
Table 2 shows the results from multivariable discrete-time survival analyses investigating predictors of transitions between stages for both alcohol and cannabis, where the outcome modelled is the likelihood of transitioning to use or from use to use disorder in a given year. Men were more likely to start using alcohol and cannabis, and to transition to abuse and dependence of these substances after starting use. An individual’s AOO of alcohol use was also significantly associated with the onset of both abuse and dependence, while AOO of cannabis use was only significantly associated with risk of dependence.
Table 2:
Multivariate predictors of transitions to alcohol and cannabis use and use disorder, Australia
| Commencing use | Use to abuse (w/o prior dependence) | Use to dependence | ||||
|---|---|---|---|---|---|---|
| OR | (95% CI) | OR | (95% CI) | OR | (95% CI) | |
| Alcohol | N=8,463 | N=7,945 | N=7,945 | |||
| Individual’s age of commencing alcohol use3 | ||||||
| Early youth | - | - | 2.63* | (2.09–3.31) | 3.21* | (2.10–4.91) |
| Mid-teens | - | - | 1.37* | (1.07–1.76) | 1.71* | (1.06–2.75) |
| Adulthood | - | - | 1.00 | - | 1.00 | - |
| χ22 [p] | - | - | 79.55** | [<0.001] | 38.29** | [<0.001] |
| Male | 1.63* | (1.50–1.77) | 2.78* | (2.40–3.23) | 1.64* | (1.24–2.16) |
| χ21 [p] | 133.29** | [<0.001] | 187.69** | [<0.001] | 12.67** | [<0.001] |
| Percentage of individual’s age cohort already using5 | 1.34* | (1.30–1.39) | 1.37* | (1.30–1.45) | 1.76* | (1.51–2.05) |
| χ21 [p] | 328.90** | [<0.001] | 135.30** | [<0.001] | 53.95** | [<0.001] |
| Education6 | ||||||
| Student | 1.53 | (0.96–2.45) | 2.02* | (1.39–2.93) | 0.66 | (0.31–1.40) |
| Low | 1.25 | (0.81–1.90) | 1.88* | (1.39–2.56) | 0.76 | (0.38–1.52) |
| Low/Med | 0.69 | (0.46–1.06) | 1.52* | (1.03–2.24) | 0.65 | (0.33–1.29) |
| Med/High | 1.18 | (0.76–1.83) | 1.76* | (1.27–2.44) | 0.75 | (0.39–1.44) |
| High | 1.00 | - | 1.00 | - | 1.00 | - |
| χ24 [p] | 37.91** | [<0.001] | 18.07** | [0.001] | 2.07 | [0.723] |
| Cannabis | N=8,463 | N=1,5997 | N=1,6047 | |||
| Individual’s age of commencing cannabis use4 | ||||||
| Early youth | - | - | 0.61* | (0.37–1.00) | 1.06 | (0.58–1.95) |
| Mid-teens | - | - | 0.71 | (0.42–1.22) | 0.59 | (0.33–1.06) |
| Adulthood | - | - | 1.00 | - | 1.00 | - |
| χ22 [p] | - | - | 3.97 | [0.137] | 8.74** | [0.013] |
| Male | 1.94* | (1.70–2.21) | 1.55* | (1.20–2.00) | 1.69* | (1.03–2.78) |
| χ21 [p] | 102.81** | [<0.001] | 12.04** | [0.001] | 4.49** | [0.034] |
| Percentage of individual’s age cohort engaged in use5 | 2.09* | (1.88–2.33) | 1.17 | (0.95–1.44) | 2.57* | (1.60–4.13) |
| χ21[p] | 182.19** | [<0.001] | 2.25 | [0.134] | 15.75** | [<0.001] |
| Education6 | ||||||
| Student | 2.36* | (1.66–3.36) | 1.94 | (0.97–3.89) | 1.24 | (0.32–4.77) |
| Low | 1.42 | (0.95–2.10) | 2.20* | (1.19–4.08) | 1.43 | (0.42–4.86) |
| Low/Med | 1.35 | (0.87–2.08) | 0.84 | (0.37–1.91) | 1.44 | (0.39–5.37) |
| Med/High | 0.97 | (0.63–1.49) | 1.56 | (0.80–3.05) | 1.28 | (0.35–4.72) |
| High | 1.00 | - | 1.00 | - | 1.00 | - |
| χ24[p] | 61.09** | [<0.001] | 13.54** | [0.009] | 0.56 | [0.967] |
Person-years were defined from six years of age for alcohol and thirteen years of age for cannabis in modelling commencement of use.
N = The total unweighted number of respondents included in model, conditioning on initial stage.
Model also controlled for age person year (not shown in table) - groups were <= 14, 15–17, 18–20, 21–24, 25–29, and 30+.
Individual’s age of commencing alcohol use is split into tertiles among all those who ever used alcohol. The earliest (early youth) tertile is age <=15, the 2nd tertile (mid-teens) age 16–17 and the 3rd tertile (adulthood) aged 18+.
Individual’s age of commencing cannabis use is split into tertiles among those who ever used cannabis. The first tertile (early youth) is age <=16, the 2nd tertile (mid-teens) 17–18 and the last (adulthood) 19+.
%(/10) of +/−5-yr cohort used by prior person year. e.g. For an individual born in 1975 the cohort would be persons born between 1970 and 1980. An OR of 1.5 for commencement of use would be interpreted as an increase of 50% in the odds of commencing use with an increase of 10% of people in the age cohort who had commenced use by the previous person year (controlling for all other variables in the model).
Low education is defined as completed 11 or less years, low/med is completed 12 years, medium 13–15 years and high 16 or more years.
Individuals with a missing age of onset were excluded from the model (N=4 for cannabis abuse and N=2 for cannabis dependence).
- significant at the 0.05 level, two-sided test; CI, confidence interval; OR, odds ratio.
More consistent associations were observed between the percentage of an individual’s age cohort who had already started using alcohol or cannabis, and the likelihood of that individual transitioning to use and dependence for both alcohol and cannabis, as well as to abuse for alcohol. Most notable was the large cohort effect for transitioning to dependence, where each 10% increase of people in an individual’s age cohort having commenced use by the previous person year was associated with an increase of 76% and 157% in the adjusted odds of transitioning from use to dependence, for alcohol and cannabis, respectively.
Predictors of remission from abuse and dependence
Table 3 shows the results from multivariable discrete-time survival analyses investigating predictors of remission from alcohol and cannabis use disorders. The two variables related to risk of remitting in any given year were gender for cannabis, and levels of use in an individual’s age cohort for remission from abuse for cannabis and abuse and dependence for alcohol. Men were less likely than women to remit from abuse or dependence for cannabis. Interestingly, the higher the level of use in an individual’s age cohort, the higher the likelihood that a person who had developed alcohol abuse or dependence or cannabis abuse, was to remit from these disorders.
Table 3:
Multivariate predictors of remission from DSM-IV alcohol and cannabis use disorders, Australia
| Predictors of remission among people who had met criteria for DSM-IV alcohol… | Predictors of remission among people who had met criteria for DSM-IV cannabis… | |||||||
|---|---|---|---|---|---|---|---|---|
| …abuse1 | …dependence1 | …abuse1 | …dependence1 | |||||
| OR | (95% CI) | OR | (95% CI) | OR | (95% CI) | OR | (95% CI) | |
| Individual’s age of commencing use2 | ||||||||
| Early youth | 0.75* | (0.57–0.99) | 0.63 | (0.32–1.24) | 0.82 | (0.57–1.17) | 1.09 | (0.65–1.84) |
| Mid-teens | 0.86 | (0.66–1.12) | 0.69 | (0.34–1.43) | 1.15 | (0.80–1.66) | 1.29 | (0.63–2.63) |
| Adulthood | 1.00 | - | 1.00 | - | 1.00 | - | 1.00 | - |
| χ22 [p] | 4.78 | [0.091] | 1.89 | [0.389] | 5.03 | [0.081] | 0.52 | [0.772] |
| Male | 0.92 | (0.74–1.14) | 0.67 | (0.45–1.02) | 0.51* | (0.36–0.71) | 0.44* | (0.26–0.75) |
| χ21 [p] | 0.62 | [0.433] | 3.60 | [0.058] | 16.10** | [<0.001] | 9.54** | [0.002] |
| Individual’s speed to transition from use to disorder3 | ||||||||
| Early | 1.02 | (0.81–1.27) | 0.95 | (0.56–1.62) | 1.28 | (0.87–1.87) | 2.23* | (1.28–3.91) |
| Mid | 0.75 | (0.55–1.02) | 0.70 | (0.40–1.22) | 1.18 | (0.79–1.75) | 1.69 | (0.97–2.94) |
| Late | 1.00 | - | 1.00 | - | 1.00 | - | 1.00 | - |
| χ22 [p] | 5.23 | [0.073] | 2.09 | [0.351] | 1.68 | [0.432] | 9.70** | [0.008] |
| Percentage of individual’s age cohort already engaged in use4 | 2.88* | (2.08–4.00) | 9.02* | (1.96–41.44) | 1.72* | (1.26–2.34) | 1.53 | (0.99–2.37) |
| χ21 [p] | 41.90** | [<0.001] | 8.32** | [0.004] | 12.41** | [<0.001] | 3.8 | [0.051] |
| Education level5 | ||||||||
| Student | 0.58 | (0.31–1.07) | 2.21 | (0.42–11.77) | 0.59 | (0.24–1.50) | 1.15 | (0.30–4.49) |
| Low | 0.82 | (0.60–1.13) | 0.76 | (0.37–1.56) | 0.67 | (0.38–1.18) | 0.74 | (0.38–1.44) |
| Low/Med | 0.87 | (0.60–1.25) | 0.84 | (0.33–2.17) | 0.96 | (0.54–1.72) | 1.72 | (0.80–3.70) |
| Med/High | 0.85 | (0.61–1.18) | 0.78 | (0.39–1.58) | 0.85 | (0.52–1.40) | 1.42 | (0.69–2.91) |
| High | 1.00 | - | 1.00 | - | 1.00 | - | 1.00 | - |
| χ24 [p] | 3.58 | [0.465] | 2.85 | [0.584] | 3.26 | [0.516] | 6.88 | [0.143] |
Person-years were defined from six years of age for alcohol and thirteen years of age for cannabis in modelling commencement of use.
Models also controlled for age person year (not shown in table) with age groups <= 18, 19–20, 21–22, 23–24, 25–29, 30–39, and 40+.
Individual’s age of commencing alcohol use is split into tertiles among all those who ever used alcohol. The earliest (early youth) tertile is age <=15, the 2nd tertile (mid-teens) age 16–17 and the 3rd tertile (adulthood) aged 18+. Individual’s age of commencing cannabis use is split into tertiles among those who ever used cannabis. The first tertile (early youth) is age <=16, the 2nd tertile (mid-teens) 17–18 and the last (adulthood) 19+.
Individual’s speed of transition from alcohol use to disorder is split into tertiles. When predicting remission from abuse, tertiles were calculated for transition from use to abuse: the fastest at 0–4 years, the middle tertile 5–8 years and late transitions were 9+ years. Among those who transition from use to dependence when predicting remission from dependence the early tertile is 0–4 years from use to dependence, mid is 5–11 years and late is 12+ years. Individual’s speed of transition from cannabis use to disorder is split into tertiles. When predicting remission from abuse, tertiles were calculated for transition from use to abuse: the fastest at 0–1 years, the middle tertile 2–3 years and late transitions were 4+ years. Among those who transition from use to dependence when predicting remission from dependence the early tertile is 0–2 years from use to dependence, mid is 3–5 years and late is 6+ years.
%(/10) of +/−5-yr cohort used by prior person year. e.g. For an individual born in 1975 the cohort would be persons born between 1970 and 1980. An OR of 1.5 for commencement of use would be interpreted as an increase of 50% in the odds of commencing use with an increase of 10% of people in the age cohort who had commenced use by the previous person year (controlling for all other variables in the model).
Low education is defined as completed 11 or less years, low/med is completed 12 years, medium 13–15 years and high 16 or more years.
Where the reported time since last disorder problem was <2 years but the exact age of remission was not reported, age of remission could not be evaluated and these individuals were excluded from the models (N=86 remission from alcohol abuse, N=21 remission from alcohol dependence, N=19 remission from cannabis abuse and N=5 remission from cannabis dependence).
- significant at the 0.05 level, two-sided test; DSM-IV, Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition.
Discussion
The aim of the present study was to examine prevalence and transitions between alcohol and cannabis use, disorder, and remission in a nationally representative Australian sample, with a specific focus on the extent to which substance use of an individual’s age cohort predicted risk of these transitions.
Most Australian adults are estimated to engage in lifetime alcohol use, with two-thirds reporting a lifetime history of regular use, and over one-fifth meeting criteria for an alcohol use disorder. Lower rates of lifetime use and disorder were observed for cannabis, but among those using, the prevalence of use disorders was higher for cannabis, and the speed of transition to use disorders was faster for people using cannabis than it was for people using alcohol. Onset of use and use disorders typically occurred between mid-teens and early 20s and there was a trend for declining AOO in more recent birth cohorts consistent with recent reviews of this evidence [33,34].
In line with existing research [35], transition time from cannabis use to use disorder was generally half the time of that from alcohol use to use disorder. Also, people who transitioned to cannabis use disorders were more likely to later remit from these disorders, and to do so at an earlier age, than people with alcohol use disorders. These findings align with previous research showing higher rates of remission from lifetime cannabis dependence versus alcohol dependence, attributed to social pressures surrounding legality of cannabis, and greater environmental cues for consumption with alcohol, as well as other physical, psychological and social consequences of use [36].
The key focus of this paper was to consider whether there was any impact of the substance use context in an individual’s age peers. We found that there clearly is. The higher the level of use in an individual’s age cohort, the greater the likelihood of an individual starting use in the following year and, if use had begun, the greater the likelihood of transitioning to disorder, for both alcohol and cannabis. Further, this variable was a strong predictor of remission from alcohol and cannabis abuse and alcohol dependence, in that the more people in an individual’s age cohort who were using those substances, the greater the likelihood of remitting from use disorder.
These findings speak strongly to the social context in which substance use occurs. One of the most consistent findings around substance use is that substance use of one’s peers predicts a greater likelihood of involvement with substance use for an individual [37]. Here, we have further shown that this is a generalised pattern whereby it is not only substance use among one’s friends, but in one’s peer cohort more generally. This may be through multiple mechanisms, including impacts on perceived norms related to substance use [38], as well as increasing opportunities to use substances [39]. As substance use increases and the onset of disorder becomes more about the cohort as a whole, persons transitioning to disorders may be less problematic or use disorder prone at the individual level and, as a result, remit from those disorders at a higher rate. These findings also provide data that suggest that the level of risk for developing problems with substance use (and likelihood of remission of problems once they begin) is not static, but affected by other variables, in this case the extent to which substance use is occurring among one’s age peers.
This suggests that any intervention that reduced the overall level of substance use within a cohort would also reduce individual-level risk for transitioning into greater levels of involvement with substance use. Educational settings provide ready access and easy delivery of interventions to young people, but there are problems with the quality of studies of school-based prevention [11] and many studies only report on changes in attitudes and knowledge [40,41]; these also do not include young people who have left school, a group at higher risk of substance use [37]. There are structural-level interventions with good evidence of a much greater preventive impact upon substance use [42]. For example, limiting outlets where alcohol may be sold can reduce young people’s access to alcohol [43]; increasing alcohol taxation or alcohol price also reduces alcohol consumption [44,45]. Raising the age at which alcohol purchase is legal has also been shown to reduce alcohol-related motor vehicle accidents, alcohol-related hospitalisations and mortality [44,45].
While the current study identifies the effect of cohort involvement measures on risk of transitioning to higher stages of the same substance, it would also be of interest to investigate the impact of cross-substance use. Do disorders of difference substances tend to occur at the same ages or over time? Do cohort involvement measures predict across substances? Such findings would provide further insight of the patterns and influences of poly-substance use and use disorders.
Previous research has shown a differential role of sociodemographic risk factors in transitioning across the stages of alcohol use and use disorder [6–8,10]. These findings were reflected in the current study for both alcohol and cannabis to the extent that being male and lower educational attainment predicted onset of use, and transition from use to regular use and abuse. Men were also less likely to report lifetime remission from cannabis abuse and dependence; this has previously been suggested to reflect a higher likelihood of greater physical, psychological and social consequences of substance use among women and their faster progression to treatment [36,46]. Models for alcohol use transitions were run for the transitions of use to regular use, regular use to abuse without prior dependence, and regular use to dependence, similarly to those in Table 2 (see Appendix Table S1). Individuals’ age of onset was significantly associated with all transitions, lower education and being male were associated with increased risk of transitioning from use to regular use and regular use to abuse, and the prevalence of use among one’s peers was positively significantly associated with transitions from regular use to use disorders.
Although treatment provision was not factored into these analyses, separate analyses have suggested that treatment rates for substance use disorders were very low [47], and there is considerable scope to improve the reach of effective early intervention and continuing care throughout the journey to remission, and for targeted intervention within the comparably brief time window between onset of use and use disorder, particularly for cannabis.
Limitations
This study provided detail regarding the prevalence and timing of various stages across the full trajectory of both alcohol and cannabis use, with clinically valid diagnoses and inclusion of contextual predictors not previously accounted for within the literature. It should be noted that data on age of onset for each stage were obtained via retrospective self-report and may be subject to ‘forward telescoping’, whereby participants are more likely to report events as closer to the point of interview than is accurate [48,49]. Large upticks in the cohort curves presented in Figure 2, relative to surrounding years, are likely representative of such memory bias. However, this literature does not suggest that the order of recalled events will be altered.
The peer networks that individuals from the same birth cohort directly interact with will vary. It was not clear with the current dataset how to capture the prevalence of use among an individual’s true peer group. The estimates presented here are likely lower-bound estimates of the effect sizes that would have been obtained if we had completely accurate data on peer groups.
The illegality and potential stigmatism surrounding substance use may have meant respondents under-reported their true level of involvement with substances. While this may influence the overall prevalence levels, we have no reason to suspect this would vary by cohort or age. If the true level of substance use is in fact higher, cohort use may have an even larger effect on risk of transitioning than is observed here.
Due to the small counts in certain models, it was necessary to use large age-categories such as the person-year age grouping of 40+ years, which combines different age groups including middle-aged adults and seniors and may obscure putative specific effects in the elderly. Conditional relationships may also exist between the age-related variables (age of onset, person year and education) though interactive terms were not explicitly modelled.
Changes to the national schooling structure over time means there is likely variation in the education completion thresholds across cohort groups, as well as at the institution and geographic location levels. Information relating to schooling was not captured in enough detail that would allow for reliable cohort-specific education categories. Therefore, the significance of this variable may in part capture the age of an individual.
Conclusion
We documented clear associations between the substance use of an individual’s age cohort and an individual’s personal risk of transitioning to greater involvement with that substance. This relationship remained a significant predictor of transitioning into and out of problematic substance use, over and above that individual’s age of initiation and speed of transition into substance use. These findings have important implications for our understanding of the causal pathways into and out of problematic substance use.
Supplementary Material
Acknowledgements
The World Health Organization’s World Mental Health Survey are supported by the US National Institute of Mental Health (R01 MH070884), the MacArthur Foundation, the Pfizer Foundation, the US Public Health Service (R13-MH066849, R01-MH069864 and R01 DA016558), the Fogarty International Center (R03-TW006481), the Pan American Health Organization, Eli Lilly and Company, Ortho-McNeil Pharmaceutical Inc., GlaxoSmithKline, Bristol-Myers Squibb, and Shire. This work was supported by an Australian National Health and Medical Research Council (NHMRC) project grant (no. 1081984). LD is supported by an NHMRC Principal Research Fellowship and AP by an NHMRC Early Career Fellowship.
In the past three years, LD has received investigator-initiated untied educational grants for studies of opioid medications in Australia from Indivior, Mundipharma and Seqirus. AP has received investigator-initiated untied educational grants from Mundipharma and Seqirus. In the past 3 years, RK received support for his epidemiological studies from Sanofi Aventis; was a consultant for Johnson & Johnson Wellness and Prevention, Shire, Takeda; and served on an advisory board for the Johnson & Johnson Services Inc. Lake Nona Life Project. RK is a co-owner of DataStat, Inc., a market research firm that carries out healthcare research.
The views expressed in this report are those of the authors and should not be construed to represent the views or policies of the World Health Organization, other sponsoring organisations, agencies or governments, and do not necessarily represent the views, official policy, or position of the US. Department of Health and Human Services or any of its affiliated institutions or agencies. MG’s role on this study is through his involvement as a Science Officer on U01-MH60220. He had no involvement in the other cited grants.
References
- 1.Lopez-Quintero C, Cobos JP, Hasin DS, Okuda M, Wang S, Grant BF, et al. Probability and predictors of transition from first use to dependence on nicotine, alcohol, cannabis, and cocaine: Results of the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC). Drug Alcohol Depend 2011;115:120–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Butterworth P, Slade T, Degenhardt L. Factors associated with the timing and onset of cannabis use and cannabis use disorder: Results from the 2007 Australian National Survey of Mental Health and Well-Being. Drug Alcohol Rev 2014;33:555–64. [DOI] [PubMed] [Google Scholar]
- 3.Calabria B, Degenhardt L, Briegleb C, Vos T, Hall W, Lynskey M, et al. Systematic review of prospective studies investigating “remission” from amphetamine, cannabis, cocaine or opioid dependence. Addict Behav 2010;35:741–9. [DOI] [PubMed] [Google Scholar]
- 4.Behrendt S, Wittchen H-U, Höfler M, Lieb R, Beesdo K. Transitions from first substance use to substance use disorders in adolescence: is early onset associated with a rapid escalation? Drug Alcohol Depend 2009;99:68–78. [DOI] [PubMed] [Google Scholar]
- 5.Coffey C, Carlin JB, Lynskey M, Li N, Patton GC. Adolescent precursors of cannabis dependence: findings from the Victorian Adolescent Health Cohort Study. Br J Psychiatry 2003;182:330–6. [DOI] [PubMed] [Google Scholar]
- 6.Suliman S, Seedat S, Williams DR, Stein DJ. Predictors of transitions across stages of alcohol use and alcohol-use disorders in South Africa*. J Stud Alcohol Drugs 2010;71:695–703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kalaydjian A, Swendsen J, Chiu W-T, Dierker L, Degenhardt L, Glantz M, et al. Sociodemographic predictors of transitions across stages of alcohol use, disorders, and remission in the National Comorbidity Survey Replication. Compr Psychiatry 2009;50:299–306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Silveira CM, Viana MC, Siu ER, de Andrade AG, Anthony JC, Andrade LH. Sociodemographic correlates of transitions from alcohol use to disorders and remission in the Sao Paulo megacity mental health survey, Brazil. Alcohol Alcohol 2011;46:324–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Abdin E, Subramaniam M, Vaingankar JA, Chong SA. The role of sociodemographic factors in the risk of transition from alcohol use to disorders and remission in singapore. Alcohol Alcohol 2014;49:103–8. [DOI] [PubMed] [Google Scholar]
- 10.Lee S, Guo WJ, Tsang A, He YL, Huang YQ, Zhang MY, et al. Associations of cohort and socio-demographic correlates with transitions from alcohol use to disorders and remission in metropolitan China. Addiction 2009;104:1313–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hall WD, Patton G, Stockings E, Weier M, Lynskey M, Morley KI, et al. Why young people’s substance use matters for global health. Lancet Psychiatry 2016;3:265–79. [DOI] [PubMed] [Google Scholar]
- 12.Weiss RD, Mirin SM, Griffin ML, Michael JL. Psychopathology in cocaine abusers. Changing trends. J Nerv Ment Dis 1988;176:719–25. [DOI] [PubMed] [Google Scholar]
- 13.Breslau NN, Scott P; Kessler, Ronald C. Psychiatric disorders and stages of smoking. Biol Psychiatry 2004;55:69–76. [DOI] [PubMed] [Google Scholar]
- 14.O’Malley PM, Bachman JG, Johnston LD. Period, age, and cohort effects on substance use among young Americans: a decade of change, 1976–86. Am J Public Health 1988;78:1315–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Anthony JC, Warner L, Kessler R. Comparative epidemiology of dependence on tobacco, alcohol, controlled substances, and inhalants: Basic findings from the National Comorbidity Survey. Exp Clinical Psychopharmacol 1994;2:244–68. [Google Scholar]
- 16.Grant BF. Prevalence and correlates of drug use and DSM-IV drug dependence in the United States: results of the National Longitudinal Alcohol Epidemiologic Survey. J Subst Abuse 1996;8:195–210. [DOI] [PubMed] [Google Scholar]
- 17.Rice JP, Neuman RJ, Saccone NL, Corbett J, Rochberg N, Hesselbrock V, et al. Age and birth cohort effects on rates of alcohol dependence. Alcohol Clin Exp Res 2003;27:93–9. [DOI] [PubMed] [Google Scholar]
- 18.Holdcraft LC, Iacono WG. Cohort effects on gender differences in alcohol dependence. Addiction 2002;97:1025–36. [DOI] [PubMed] [Google Scholar]
- 19.Slade T, Chapman C, Swift W, Keyes K, Tonks Z, Teesson M. Birth cohort trends in the global epidemiology of alcohol use and alcohol-related harms in men and women: systematic review and metaregression. BMJ Open 2016;6:e011827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Grucza RA, Bucholz KK, Rice JP, Bierut LJ. Secular Trends in the Lifetime Prevalence of Alcohol Dependence in the United States: A Re-evaluation. Alcohol Clin Exp Res 2008;32:763–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Grant BF. Prevalence and correlates of alcohol use and DSM-IV alcohol dependence in the United States: results of the National Longitudinal Alcohol Epidemiologic Survey. J Stud Alc 1997;58:464–73. [DOI] [PubMed] [Google Scholar]
- 22.Hasin D, Grant B. The co-occurrence of DSM-IV alcohol abuse in DSM-IV alcohol dependence: NESARC results on heterogeneity that differs by population subgroup. Arch Gen Psychiatry 2004;61:891–6. [DOI] [PubMed] [Google Scholar]
- 23.Kessler RC, McGonagle KA, Zhao S, Nelson CB, Hughes M, Eshleman S, et al. Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States: results from the National Comorbidity Survey. Arch Gen Psychiatry 1994;51:8–19. [DOI] [PubMed] [Google Scholar]
- 24.Johnson RA, Gerstein DR. Age, period, and cohort effects in marijuana and alcohol incidence: United States females and males, 1961–1990. Subst Use Misuse 2000;35:925–48. [DOI] [PubMed] [Google Scholar]
- 25.Kerr WC, Greenfield TK, Bond J, Ye Y, Rehm J. Age–period–cohort modelling of alcohol volume and heavy drinking days in the US National Alcohol Surveys: divergence in younger and older adult trends. Addiction 2009;104:27–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Keyes KM, Schulenberg JE, O’malley PM, Johnston LD, Bachman JG, Li G, et al. The social norms of birth cohorts and adolescent marijuana use in the United States, 1976–2007. Addiction 2011;106:1790–800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Australian Bureau of Statistics. National Survey of Mental Health and Wellbeing: Summary of Results, 2007 (cat. No. 4362.0). Canberra: ABS; Available from: http://www.abs.gov.au/AUSSTATS/abs@.nsf/Lookup/4326.0Explanatory%20Notes12007?OpenDocument. Accessed 23 January 2018; 2008. [Google Scholar]
- 28.Australian Bureau of Statistics. National Survey of Mental Health and Wellbeing: Users’ Guide 2007 (Cat. No. 4326.0). 2009. [cited; Available from: http://www.abs.gov.au/ausstats/abs@.nsf/mf/4327.0
- 29.Kessler RC, Üstün TB. The World Mental Health (WMH) Survey Initiative version of the World Health Organization (WHO) Composite International Diagnostic Interview (CIDI). Int J Methods Psychiatr Res 2004;13:93–121. doi: 10.1002/mpr.168 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Australian Bureau of Statistics. Technical Manual: National Survey of Mental Health and Wellbeing, Confidentialised Unit Record Files (Cat. No.4326.0); 2009.
- 31.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (Fourth Edition - Technical Revision ). Washington, DC: American Psychiatric Association; 2000. [Google Scholar]
- 32.An A Performing Logistic Regression on Survey Data with the New SURVEYLOGISTIC Procedure. Paper 258–27. Proceedings of the 27th Annual SAS Users Group International Conference (SUGI 27); 2002; 2002. p. 14–7. [Google Scholar]
- 33.Keyes KM, Li G, Hasin DS. Birth cohort effects and gender differences in alcohol epidemiology: a review and synthesis. Alcohol Clin Exp Res 2011;35:2101–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Slade T, Chapman C, Swift W, Keyes K, Tonks Z, Teesson M. Birth cohort trends in the global epidemiology of alcohol use and alcohol-related harms in men and women: systematic review and metaregression. BMJ Open 2016;6: e011827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lopez-Quintero C, de los Cobos JP, Hasin DS, Okuda M, Wang S, Grant BF, et al. Probability and predictors of transition from first use to dependence on nicotine, alcohol, cannabis, and cocaine: Results of the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC). Drug Alcohol Depend 2011;115:120–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lopez-Quintero C, Hasin DS, de los Cobos JP, Pines A, Wang S, Grant BF, et al. Probability and predictors of remission from lifetime nicotine, alcohol, cannabis, or cocaine dependence: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. Addiction 2011;106:657–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Degenhardt L, Stockings E, Patton G, Hall WD, Lynskey M. The increasing global health priority of substance use in young people. Lancet Psychiatry 2016;3:251–64. [DOI] [PubMed] [Google Scholar]
- 38.Pollard JW, Freeman JE, Ziegler DA, Hersman MN, Goss CW. Predictions of normative drug use by college students. J College Stud Psychother 2000;14:5–12. [Google Scholar]
- 39.Wells JE, Maria Haro J, Karam E, Lee S, Lepine J-P, Elena Medina-Mora M, et al. Cross-national comparisons of sex differences in opportunities to use alcohol or drugs, and the transitions to use. Subst Use Misuse 2011;46:1169–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Wood E, Shakeshaft A, Gilmour S, Sanson-Fisher R. A systematic review of school-based studies involving alcohol and the community. Aust N Z J Public Health 2006;30:541–9. [DOI] [PubMed] [Google Scholar]
- 41.Foxcroft DR, Lister-Sharp D, Lowe G. Alcohol misuse prevention for young people: a systematic review reveals methodological concerns and lack of reliable evidence of effectiveness. Addiction 1997;92:531–7. [PubMed] [Google Scholar]
- 42.Stockings E, Hall WD, Lynskey M, Morley KI, Reavley N, Strang J, et al. Prevention, early intervention, harm reduction, and treatment of substance use in young people. Lancet Psychiatry 2016;3:280–96. [DOI] [PubMed] [Google Scholar]
- 43.Babor T, Caetano R, Casswell S, Edwards G, Giesbrecht N, Graham K, et al. Alcohol: No ordinary commodity. Research and Public Policy 2010. [Google Scholar]
- 44.Latimer J, Guillaume L, Goyder E, Chilcott J, Payne N. Interventions on control of alcohol price, promotion and availability for prevention of alcohol use disorders in adults and young people. ScHARR Public Health Evidence Report 2009; 23. [Google Scholar]
- 45.Martineau F, Tyner E, Lorenc T, Petticrew M, Lock K. Population-level interventions to reduce alcohol-related harm: An overview of systematic reviews. Prev Med 2013;57:278–96. [DOI] [PubMed] [Google Scholar]
- 46.Hernandez-Avila CA, Rounsaville BJ, Kranzler HR. Opioid-, cannabis-and alcohol-dependent women show more rapid progression to substance abuse treatment. Drug Alcohol Depend 2004;74:265–72. [DOI] [PubMed] [Google Scholar]
- 47.Degenhardt L, Glantz M, Evans-Lacko S, Sadikova E, Sampson N, Thornicroft G, et al. Estimating treatment coverage for people with substance use disorders: An analysis of data from the World Mental Health Survey. World Psychiatry 2017;16:299–307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Shillington AM, Woodruff SI, Clapp JD, Reed MB, Lemus H. Self-reported age of onset and telescoping for cigarettes, alcohol, and marijuana: across eight years of the National Longitudinal Survey of Youth. J Child Adolesc Subst Abuse 2012;21:333–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Johnson EO, Schultz L. Forward telescoping bias in reported age of onset: an example from cigarette smoking. Int J Methods Psychiatr Res 2005;14:119–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.