The hospital’s physical environment plays an important role in patient acquisition of healthcare-associated pathogens. Multiple different pathogenic organisms have been cultured from surfaces within patient rooms and many (e.g. vancomycin resistant enterococcus, multidrug resistant (MDR) Acinetobacter and Clostridium difficile) can persist on dry surfaces for weeks to months. Patients admitted to a room where the previous occupant was colonized or infected with a MDR Organism (MDRO) are, independent of other factors, more likely to acquire the same MDRO, highlighting the essential role of adequate room cleaning and disinfection.1 Healthcare workers’ (HCW) hands also can be a vehicle for transmission of pathogens from environmental surfaces near the patient. Pathogen contamination of HCW’s gown and gloves at room exit is related to the number of surfaces touched.2 Despite this risk of pathogen transmission, studies have found that less than half of hospital room surfaces are adequately cleaned and disinfected.3,4
Adequate microbiologic disinfection of surfaces can be achieved with appropriate cleaning procedures5; however, implementation and adoption of these practices in real-world settings has been difficult and incomplete. While considerable efforts have been made to improve education and training on patient room cleaning and to develop strategies for monitoring and providing feedback on cleaning performance, 6 there remains considerable variability in cleaning practices by environmental services (EVS) staff. A large multi-intensive care unit trial to enhance environmental cleaning via educational and programmatic interventions found between six and 30% of surfaces were still potentially contaminated in the post intervention period.3 Given the complexity of the patient room cleaning process, the associated work system, and the barriers to effective implementation, an approach guided by human factors engineering (HFE) principles may be helpful to design and implement effective and sustainable interventions for improving patient room cleaning and disinfection. Development of a HFE approach to patient room cleaning could then be adapted for cleaning and disinfection of other high risk hospital environments, such as the operating room.
HFE is “the scientific discipline concerned with the understanding of interactions among humans and other elements of a system, and the profession that applies theory, principles, data, and methods to design in order to optimize human wellbeing and overall system performance.” 7 Evidence has shown the effectiveness of HFE in improving healthcare quality and safety with issues such as medication errors, readmissions after complex surgery, and safe implementation of the electronic health records.8 Several researchers proposed the application of HFE to infection prevention, such as improving central line care.9,10 Yanke et al have used this methodology to evaluate a C. difficile prevention bundle.10 In this paper, we describe a HFE approach to hospital room cleaning which emphasizes the three core characteristics of HFE: (1) using a systems approach, (2) being design-driven, and (3) focusing on both system performance and human well-being.
A HFE approach to patient room cleaning highlights interactions among work system elements and levels, the dynamic impact of individual work system elements on the whole system, and links between work system, care processes, and system outcomes.11 According to the Systems Engineering Initiative for Patient Safety (SEIPS) 2.0 model,12 a systems engineering model anchored within HFE, patient room cleaning is collaborative work of EVS associates, healthcare providers (e.g., nurses), and patients and their families, who perform different tasks (e.g., cleaning high touch surfaces, communication), with various tools and technologies (e.g., cleaning tools and supplies, checklists), under certain organizational conditions (e.g., safety culture, work schedule), in an internal (e.g., patient room and bathroom) and external (e.g., social attitude, regulations) environment. A combination of these interrelated work system elements influences the patient room cleaning process and other care processes, which further influence patient (e.g., healthcare associated infections, patient satisfaction), employee (e.g., employee satisfaction, motivation) and organization (e.g. reputation and reimbursement based on healthcare associated infection rates) outcomes (see Figure).
Figure 1.
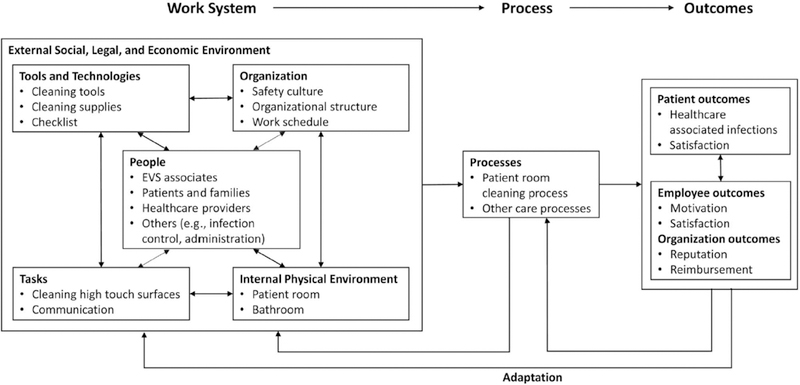
Systems Engineering Initiative for Patient Safety model for patient room cleaning. EVS, environmental secvices.
EVS associates, in the center of the work system, face a number of challenges associated with different work system elements (see Table). The knowledge and skills of EVS associates are important work system elements. Training EVS associates to improve their knowledge and skills, however, is not sufficient to ensure high-quality patient room cleaning. Other work system elements also need to be well-designed for optimal performance. For example, a well-trained EVS associate may need support from peers (teamwork) to clean a large unit with many patient rooms. Some work system elements are difficult to change and may be addressed by improving other work system elements. For example, well-designed cleaning tools may facilitate the work of EVS associates who are not able to reach certain surfaces due to their physical limitations (e.g., height, musculoskeletal disorder).The Table provides examples of potential intervention ideas for improving patient room cleaning.
Table 1.
Challenges to patient room cleaning and HFE-informed intervention ideas for improving patient room cleaning.
| Work system elements | Challenges to patient room cleaning | HFE-Informed intervention ideas |
|---|---|---|
| People | ○ EVS associates ○ Education, literacy and language barriers that are not addressed with current education tools ○ Physical limitations (e.g., height, back pain) that hinder the cleaning of certain surfaces ○ Lack of practical relevant information (e.g., when to change cleaning cloths, mop heads) ○ Personal concerns about working in close proximity to bacteria ○ Lack of skills to communicate with patients and families, particularly in areas such as psychiatry, labor and delivery, and intensive care ○ Patients and Families ○ Lack of recognition of the role of EVS associates in keeping the near patient environment clean and their role in infection prevention |
○ Training of EVS associates ○ Redesigning training materials for patient room cleaning based on HFE analysis (e.g., physical ergonomic assessment, task analysis) ○ Simulation-based communication training with role-plays and observations of EVS associate-patient interactions ○ Creating a forum for EVS associates to ask questions and discuss anxieties ○ Specific, easy to understand teaching about contact precaution rooms, droplet and airborne precautions, with a questions and answers forum ○ Patient and family education ○ Developing education materials to enhance patient and family awareness as to the essential role of the EVS associates |
| Tasks | ○ Patient Room Cleaning ○ High workload with time pressure and interruptions ○ Repetitive nature of patient room cleaning tasks intensifying feelings of boredom and fatigue ○ Ambiguity about responsibility for patient room cleaning and medical equipment cleaning |
○ Job redesign ○ Redefining responsibilities and tasks of EVS associates using principles of job enrichment, job enlargement, and job rotation ○ Balancing individual work and teamwork of EVS associates ○ Task redesign ○ Redesigning patient room cleaning tasks based on physical ergonomics principles (e.g., work in neutral postures, reduce excessive force) and sociotechnical system principles (e.g., responsible autonomy, adaptability) |
| Tools and technologies | ○ Cleaning tools and supplies ○ Cleaning tools and supplies not supporting patient room cleaning tasks ○ Complex instructions for using cleaning tools and supplies (e.g., mixing or dilution of solutions) ○ Distributed storage of cleaning tools and supplies ○ Cleaning checklist ○ Poorly designed, ineffective cleaning checklists ○ Cleaning checklist not fitting with the workflow of EVS associates ○ Medical equipment ○ Complex medical equipment (e.g., patient bed) that is difficult to clean |
○ Redesign and rearrangement of cleaning tools and supplies ○ Redesigning cleaning tools and supplies based on usability evaluation (e.g., heuristic evaluation, user testing) ○ Redesigning instructions, labels and warnings using HFE principles (e.g. HFE principles for labeling) ○ Limiting the number of cleaning tools and supplies used and centralizing the their storage ○ Redesign of cleaning checklist ○ Using a participatory, user-centered design approach to redesign the cleaning checklist ○ Selection of medical equipment ○ HFE and infection prevention professionals assessing medical equipment before making purchasing decisions to ensure adequate cleaning is feasible |
| Organization | ○ Organizational culture ○ Lack of appreciation that EVS associates contribute to patient safety ○ Organizational structure ○ Hierarchy with power difference between frontline workers and leadership and between EVS associates and other healthcare professionals ○ Performance evaluation and promotion ○ No long term recognition of good work of EVS associates ○ No promotion pathway for EVS associates ○ Staffing and work schedule ○ Conflicting pressures such as minding a child, who is sick and cannot go to school, or school is closed, that may prevent an EVS associate from coming to work. |
○ Creation of safety culture ○ Building a culture of safety by highlighting the importance of EVS associates in infection prevention ○ Involving EVS associates in a unit-based forum for addressing safety-related issues ○ Change of organizational structure ○ Building teams between EVS associates and other healthcare professionals ○ Change of evaluation and promotion system ○ Providing certification programs with testing and qualifications to EVS associates ○ Developing clear promotion pathway for EVS associates ○ Staffing and work schedule ○ Flexibility of hours ○ Inexpensive daycare options ○ Backup system whereby if an EVS associate is unable to come to work their tasks are covered. |
| Internal environment | ○ Patient Room ○ Patient room cluttered with patient belongings ○ Patient room with dim light |
○ Patient room layout ○ Providing specific areas (e.g., labeled shelving and closet space) for patients and families to hold their belongings ○ Color-coding high touch surfaces to alert EVS associates |
EVS Environmental Services
HFE Human Factors Engineering
Various HFE methods (e.g., proactive risk analysis, task analysis, usability evaluation)13 and principles (e.g., HFE principles for checklist design, HFE implementation principles)14 can be used to facilitate the redesign process. This includes analysis of the existing system, design and implementation of interventions, and evaluation of the impact of the interventions. In addition, a HFE approach emphasizes the participation of different stakeholders who can affect, or are affected by, patient room cleaning in the redesign process. This is known as participatory ergonomics.15 Patient room cleaning involves multiple stakeholders, including front line EVS associates, healthcare providers (e.g., nurses, physicians), EVS managers, and hospital leaders. These different stakeholder groups have varied values, norms, responsibilities, experience, tasks, skills, and priorities. They possess heterogeneous perspectives regarding patient room cleaning; these different perspectives are invaluable and need to be considered and integrated in the redesign process.
Finally, a HFE approach to patient room cleaning aims to improve both system performance and human well-being. The ultimate goal of patient room cleaning is to improve quality of care and patient safety by decreasing pathogen burden in the near patient environment. Quality of care and patient safety can be assessed with measures of cleaning processes and patient outcomes. The cleaning process can be measured by use of fluorescent markers; invisible fluorescent gel markers are placed on high touch surfaces prior to cleaning and assessed for removal post-cleaning with a black light. Measures of patient outcomes include rates of healthcare-associated infections and patient experience scores. In addition to quality of care and patient safety, a HFE approach to patient room cleaning should enhance well-being of EVS associates (e.g., job satisfaction, motivation), since poor employee outcomes are likely to be related to poor patient outcomes. This also impacts organizational outcomes as enhanced EVS associate well-being should result in improved staff retention. In addition to impacting patient safety outcomes, enhanced patient room cleaning affects organizational reputation and finances as well. Public reports of rates of healthcare-associated infections and patient satisfaction scores and these metrics’ impact on reimbursement are further incentives for healthcare facilities to seek improvement of environmental cleaning and disinfection.
Using a HFE approach, we highlight several challenges and potential interventions to enhance patient room cleaning. The integration of a HFE approach into infection prevention challenges is likely to lead to improved interventions that are effective and sustainable. This is a much needed step towards creating a cleaner and safer patient environment. This paper demonstrates the complex system of patient room cleaning though the lens of the SEIPS 2.0 model. However, implementation of a HFE approach is not without challenges including budgetary constraints, insufficient manpower, and resistance to change. There are likely additional barriers to be uncovered, and different institutions may have a different hierarchy of challenges, which may require different strategies.16 Further work needs to be done in this area, but this paper proposes one framework for understanding and addressing the role of the EVS work system in the transmission of pathogens in the healthcare environment.
Acknowledgements
We wish to thank the Environmental Care Facilities Department and Department of Hospital Epidemiology and Infection Control at The Johns Hopkins Hospital.
Financial support: Financial support for this work was provided by CDC Prevention Epicenters Program.
CR, SC, HEG, NS, LLM, APG, and AX are supported by CDC Prevention Epicenters Program. SK is supported by the National Center for Advancing Translational Sciences KL2 Award KL2TR001077.
Footnotes
Conflict of interest: All authors have no potential conflicts of interest to report.
References
- 1.Drees M, Snydman DR, Schmid CH, et al. Prior environmental contaminations increases the risk of acquisition of vancomycin-resistant enterococci. Clin Infect Dis 2008;46:678–685. [DOI] [PubMed] [Google Scholar]
- 2.Rock C, Thom KA, Masnick M, Johnson JK, Harris AD, Morgan DJ. Frequency of Klebsiella pneumoniae carbapenemase (KPC)–producing and non-KPC-producing Klebsiella species contamination of healthcare workers and the environment. Infect Control Hosp Epidemiol 2014;35:426–429. doi: 10.1086/675598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Carling PC, Parry F, von Beheren M. Identifying opportunities to enhance environmental cleaning in 23 acute care hospitals. Infect Control Hosp Epidemiol 2008;29:1–7. [DOI] [PubMed] [Google Scholar]
- 4.Goodman ER, Platt R, Bass R, et al. Impact of environmental cleaning intervention on the presence of methicillin-resistant Staphylococcus aureus and vancomycin-resistant enterococci on surfaces in intensive care unit rooms. Infect Control Hosp Epidemiol 2008;29:593–599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Carling PC, Parry MM, Rupp ME, et al. Improving cleaning of the environment surrounding patients in 35 acute care hospitals. Infect Control Hosp Epidemiol 2008;11:1035–1041. [DOI] [PubMed] [Google Scholar]
- 6.Han JH, Sullivan N, Leas BF, Pegues DA, Kaczmarek JL, Umscheid CA. Cleaning hospital room surfaces to prevent health care-associated infections. A technical brief. Ann Intern Med 2015;163:598–607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Definition and Domains of Ergonomics. International Ergonomics Association website. http://www.iea.cc/whats/index.html. Published 2016. Accessed March 21, 2016.
- 8.Xie A, Carayon P. A systematic review of human factors and ergonomics (HFE)-based healthcare system redesign for quality of care and patient safety. Ergonomics 2015;58:33–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gurses AP, Seidl K, Vaidya V, et al. Systems ambiguity and guideline compliance: A qualitative study of how intensive care units follow evidence-based guidelines to reduce healthcare-associated infections. BMJ Qual Saf 2008;17:351–359. [DOI] [PubMed] [Google Scholar]
- 10.Yanke E, Carayon P, Safdar N. Translating evidence into practice using a systems engineering framework for infection prevention. Infect Control Hosp Epidemiol 2014;35:1176–1182. [DOI] [PubMed] [Google Scholar]
- 11.Waterson P A critical review of the systems approach within patient safety research. Ergonomics 2009;52:1185–1195. [DOI] [PubMed] [Google Scholar]
- 12.Holden RJ, Carayon P, Gurses AP, Hoonakker P, Hundt AS, Ozok AA, Rivera-Rodriguez AJ. SEIPS 2.0: A human factors framework for studying and improving the work of healthcare professionals and patients. Ergonomics 2013;56:1669–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Stanton NA, Salmon PM, Walker GH, Baber C, Jenkins DP. Human Factors Methods: A Practical Guide for Engineering and Design. Aldershot, UK: Ashgate; 2005. [Google Scholar]
- 14.Carayon P, Alyousef B, Xie A. Human factors and ergonomics in health care In: Salvendy G, ed. Handbook of Human Factors and Ergonomics. 4th ed New York: John Wiley and Sons; 2012:1574–1595. [Google Scholar]
- 15.Wilson JR, Haines H, Morris W. Participatory ergonomics In: Wilson JR, Corlett EN, eds. Evaluation of Human Work. 3rd ed Boca Raton, FL: Taylor & Francis; 2005:933–962. [Google Scholar]
- 16.Carayon P Human factors in patient safety as an innovation. Applied Ergonomics 2010;41:657–665. [DOI] [PMC free article] [PubMed] [Google Scholar]


