Abstract
OBJECTIVES:
Growing evidence shows that cardiovascular health (CVH) is associated with brain health. Little is known about this topic among older adults in Latin America, where the number of people living with dementia is rising. This study aimed to assess the longitudinal association between cardiovascular health and dementia in six Latin American countries.
METHODS:
We analyzed longitudinal data from the 10/66 study which included non-demented residents at baseline aged 65+ in six Latin American countries (n=6447) and were followed up for three years. An index of modifiable CVH factors (ranging from 0 to 14) was calculated. Incident dementia was modeled using competing risks regression to adjust for risk of death.
RESULTS:
The sample included 6.2% participants with poor (0–5), 81.0% with moderate (6–10) and 12.8% with ideal CVH (11–14). At follow-up, 9.4% had developed dementia and 13.1% had died. Compared to poor CVH, participants with moderate and ideal levels of CVH had a significantly lower risk of dementia both in the unadjusted (subhazard ratio for moderate: 0.77; ideal: 0.59) and adjusted models (moderate: 0.73; ideal: 0.66).
CONCLUSION:
Moderate and ideal levels of CVH in old age may protect against dementia incidence. These findings may inform health promotion efforts within dementia national plans adopted recently in some Latin American countries.
Keywords: Dementia, Latin America, Cardiovascular health, Competing risks, Survival analysis
Introduction
Dementia is a growing public health concern in Latin America. Life expectancy in Latin America has increased ~9 years in the last 30 years and the population 65 and older is projected to increase from 7.6% in 2015 to 19.4% in 2050. 1,2 Latin America has one of the highest dementia prevalence worldwide and the number of dementia cases is projected to result in a 346% increase from 2013 to 2050. 3–5 This increase will have serious consequences at multiple levels. At the individual level, mortality and disability will increase significantly. In fact, in Latin American countries, mortality rates among people with dementia are up to six times higher than for healthy older adults. 6 In addition, dementia disability burden has exponentially grown in Latin America compared to other health conditions in the last decades. 7 In these countries more so than most high-income countries, patients with dementia are mainly cared for by families and to a much lesser extent by public institutions. 3 Thus at the family level, dementia care will place a great burden on relatives, impacting the health of informal family caregivers. 8,9 At the social level in Latin America, costs for elder patients with dementia are seven times higher than for elder patients without dementia and are mainly accounted for by informal care. 3,10,11 In fact, in these countries the directly attributable cost of dementia exceeds that of depression, hypertension, diabetes, ischaemic heart disease and stroke. 5 Understanding factors that increase dementia risk among older adults in Latin America is paramount to develop effective public policies and prevention strategies in these countries.
Cardiovascular health (CVH) might play an important role in reducing dementia incidence in Latin America. Dementia incidence has declined in some high-income countries, which might be partly explained by CVH improvements in these countries. 12 However in Latin America, there is an increasing transition to urban settings and adaptation of lifestyles associated with cardiovascular and metabolic disease. 13,14 Abundant evidence from high-income countries and some from Latin America shows that single cardiovascular risk factors and indices are associated with cognition and dementia. 12,14–16 A growing body of research is focusing on the cumulative impact of modifiable cardiovascular risk factors on brain health. 17 For example, the American Heart Association Life’s Simple 7 CVH guidelines are based on four modifiable health behaviors: nonsmoking, healthy diet, physical activity, and body mass index (BMI); and three modifiable biological factors: blood pressure (BP), total cholesterol, and fasting glucose. 18 CVH indices such as the Life’s Simple 7 represent an improvement over the assessment of single cardiovascular risk factors as these factors often coexist and affect the brain through common pathways. 18 These CVH indices also overcome limitations of other indices such as the Framingham index as it only focuses on modifiable risk factors and include different levels of severity within each factor. 18 While studies have shown that an index of modifiable CVH factors is associated with stroke, brain integrity and cognitive functioning and decline, 19–27 to our knowledge only two studies (the Framingham study and the INVADE-trial) have assessed its association with dementia incidence. 21,28 However, the sample in the Framingham study was highly educated, both studies were from high-income countries (USA and Germany) and their models did not account for competing risk of death, which may have biased associations as individuals with lower CVH have a higher mortality rate. 29
The present study aimed to explore the longitudinal association between an index of modifiable CVH factors and dementia incidence among Latin American older adults using data from the 10/66 study. We hypothesized that higher levels of CVH would be associated with a lower incidence of dementia. We accounted for mortality by using competing risks survival analysis. Given the region’s history of wealth inequalities, 30 we explored whether associations differed by wealth. Determining the association between CVH and dementia among older adults in Latin America will inform dementia prevention policies and practice in these countries.
Methods
Study design
Two publications have described the 10/66 study in detail previously. 31,32 In short, this is an observational cohort study recruiting all resident adults 65 and older from 11 specific rural and urban catchment areas in eight low- and middle-income countries in Latin America, Africa and Asia. The present secondary analysis included only Latino American countries: Cuba, Dominican Republic, Venezuela, Mexico, Peru and Puerto Rico. Literate participants gave written informed consent and illiterate participants gave verbal consent with an independent witness. The 10/66 study followed the ethical guidelines of the 1975 Declaration of Helsinki and Institutional Review Boards of the local sites and King’s College London approved the study protocol. Study procedures for the secondary analysis were determined by the University of Kansas Medical Center’s Institutional Review Board as not involving human subjects research.
Sample and procedure
Centers conducted the baseline survey between 2004 and 2010 and included a clinical participant and informant interview, and a physical examination, which gathered information about dementia and risk factors, mental and physical health, anthropometrics, disability and use of services. 31,32 Phlebotomists took fasting blood samples at baseline from participants. Each full assessment lasted an average of 2–3 hours and centers translated, back-translated and adapted materials to the different languages as needed.
Centers conducted the follow-up assessments between 2007 and 2013 and aimed to re-interview all participants from baseline using the same measurements. 6,31,32 Interviewers attempted to locate participants up to four times at their household and if they were no longer present, contacted up to three non-cohabiting friends or relatives about their vital status and new location. Interviewers contacted relocated participants in person or by telephone irrespective of whether their new location was outside the catchment area or conducted a verbal autopsy with an informant if they had died, including the date of death and evidence of dementia-related cognitive decline and functioning impairment.
Measures
CVH index
We calculated a CVH index at baseline based on the Life’s Simple 7 index with few modifications given data availability (Appendix 1). 18 Participants were asked whether they had ever smoked, if they were still smoking regularly and at what age they quit smoking. The average of two sitting blood pressure assessments were used to define blood pressure. Participants who had been told they had hypertension and were currently receiving treatment for it were considered to be under hypertension treatment. Phlebotomists collected fasting glucose and interviewers asked whether participants were being treated for diabetes and the type of treatment. Only participants who currently used insulin or oral hypoglycemics were considered as being treated for diabetes. Cholesterol values were obtained from fasting blood samples but they did not include questions on treatment for hypercholesteremia. Given the lack of data on participants’ weight, obesity was defined using waist circumference and the World Health Organization cut-off points for risk of metabolic complications. 33 Participants were asked if they had gone for walks of half kilometer (10–15 minutes) or more and the number of times they had gone for walks of half a kilometer during the last month. A cutoff of 20 walks per month (5 walks per week) was used as a proxy indicator for 150 minutes of moderate physical activity per week. Only dietary intake of meat, fish and fruits and vegetables and frequency of intake were collected. Therefore, diet was calculated by adding points (0: inappropriate or 1: appropriate) using these three measures. The frequency of meat and fish consumption was measured with a four point Likert scale (never, some days, most days and every day). We considered meat consumption appropriate for values of never and some days. We considered fish consumption appropriate for values of some days, most days and every day. The survey also asked about the amount of servings of fruits and vegetables in the last 3 days. We considered values of 13.5 or more servings in the last 3 days (4.5 per day) appropriate. We scored the seven criteria individually as either 0 (poor), 1 (intermediate) or 2 (ideal). For the present analyses, the total score was the sum of all criteria ranging from 0 to 14, which we also categorized into three groups based on data distribution (0–5, 6–10, and 11–14) since studies show associations may not be linear. 23,26,34
Covariates
To adjust for potential confounding, we selected baseline socio-demographic covariates that could be determinants of dementia and CVH. 8 These covariates included age (65–69; 70–75; 75–79; 80+), sex, educational level (did not complete primary, completed primary, completed secondary), wealth (top; bottom 50% out of a summary score of assets owned: motor vehicles, television, refrigerator and/or freezer, water utilities, electricity utilities, telephone, plumbed toilet, and plumbed bathroom) and country. The term sex was used to be coherent with the term used in the data collection method. However, we acknowledge that any effect of this variable might be related to either genetic (sex) or social (gender) factors. 35
Dementia diagnosis
Dementia cases were defined using either 10/66 or DSM-IV criteria for which algorithms have been previously published and validated. 36–39 10/66 dementia cases scored above a cut-point of predicted probability for dementia, calculated with coefficients derived from a logistic regression equation based on cognitive test, informant report scores and diagnostic output from clinical interviews. 36 DSM-IV dementia cases needed to have cognitive impairment, impairment in social or occupational functioning and cognitive deficits that did not occur exclusively during the course of delirium and that were not better explained by another mental disorder. 38
We obtained information for dementia diagnosis from culturally and linguistically adapted cognitive tests (CSI’D’, COGSCORE scale with CERAD’s animal-naming verbal fluency, and modified CERAD ten word list learning task with delayed recall), 40,41 participant interview (Geriatric Mental State), 42 informant interview (CSI’D’, RELSCORE scale and HAS-DDS) and neurological examination (including the Luria three step motor sequencing fist-edge-palm test). 40,43 Participants who died after baseline and had a score higher than two on RELSCORE from the post-mortem informant interview, with endorsement of either “deterioration in memory” or “a general deterioration in mental functioning”, or both; an increase in RELSCORE higher than two points from baseline; and the onset of these signs being 6 months before death or later were diagnosed as probable incident dementia.
Cohort for analysis
Participants were included if 1) they were from countries in Latin America, including urban and rural sites in Mexico and Peru and urban sites in Cuba, Dominican Republic, Venezuela, and Puerto Rico, 2) had available blood test data, 3) did not have dementia at baseline using 10/66 and DSM-IV criteria and 4) had an existing value in either 10/66 or DSM-IV dementia diagnosis at follow-up.
Statistical analysis
Descriptive analyses of baseline characteristics are presented as frequencies and percentages. We calculated person-years at risk as the interval between baseline and follow-up assessment, or the estimated time of onset of dementia, or the time of death, whichever occurred first. Competing risks regression was used to model the impact of CVH on 10/66 and DSM-IV dementia incidence, 44 where competing events that occur prior to or instead of the event of interest cannot be treated as censored. The model estimates a cumulative incidence function, the probability of observing an event before a given time, for the failure event of interest (dementia) while acknowledging the possibility of the competing event (death). We estimated subhazard ratios and their 95% confidence intervals for participants’ CVH scores, which we modelled as both a discrete score and categorized based on data distribution (0–5, 6–10, and 11–14). Models adjusted for age, sex, level of education, wealth and country. Secondary analyses explored associations stratified by age, sex, education, asset ownership. We performed all analyses using Stata version 13 with statistical significance at p< 0.05. 45
Results
Table 1 summarizes the baseline characteristics for all participants by CVH levels, dementia and deceased status. The final analytic sample consisted of 6,447 participants and included 400 (6.2%) participants with poor (0–5), 5,222 (81.0%) with moderate (6–10) and 825 (12.8%) with ideal CVH (11–14). There were 605 (9.4%) incident dementia and 846 (13.1%) participants died during follow-up. Those with poor baseline CVH levels were younger (65–69 years old: 30.8%), had not completed primary education (39.9%), and were in the bottom 50% of wealth (55.0%). Those with dementia at follow-up tended to be older (80+ years old: 40.5%), women (69.4%), and had not completed primary education (46.1%). Mortality was higher among individuals who were older (i.e. 80+: 26.2% vs 65–69: 7.0%), male (17.0% vs 11.1%), less educated (incomplete primary: 16.7% vs completed secondary: 6.1%), and less wealthy (14.6% vs 11.6%).
Table 1:
Baseline characteristics of 10/66 participants by categories of cardiovascular health (CVH) and dementia status (N=6447)
| Cardiovascular Health (CVH) Status | Dementia Status | |||||
|---|---|---|---|---|---|---|
| Poor CVH (0–5) n=400 | Moderate CVH (6–10) n=5222 | Ideal CVH (11–14) n=825 | No Dementia n=4996 | Dementia n=605 | Deceased n=846 | |
| Age group | ||||||
| 65–69 | 123, 30.8% | 1490, 25.6% | 298, 36.1% | 1712, 34.3% | 65, 10.8% | 134, 15.8% |
| 70–74 | 101, 25.3% | 1473, 28.2% | 224, 27.2% | 1481, 29.7% | 137, 22.7% | 180, 21.3% |
| 75–79 | 84, 21.1% | 1150, 22.0% | 176, 21.3% | 1067, 21.4% | 157, 26.0% | 186, 22.0% |
| 80+ | 91, 22.8% | 1105, 21.2% | 127, 15.4% | 733, 14.7% | 244, 40.5% | 346, 40.9% |
| Sex | ||||||
| Female | 204, 51.0% | 3385, 64.8% | 667, 80.9% | 3362, 67.3% | 420, 69.4% | 474, 56.0% |
| Male | 196, 49.0% | 1837, 35.2% | 158, 19.2% | 1634, 32.7% | 185, 30.6% | 372, 44.0% |
| Education | ||||||
| Incomplete Primary | 159, 39.9% | 2009, 38.5% | 297, 36.0% | 1774, 35.5% | 279, 43.1% | 412, 48.8% |
| Completed Primary | 126, 31.6% | 1440, 27.6% | 205, 24.9% | 1375, 27.6% | 178, 29.4% | 218, 25.8% |
| Completed Secondary | 114, 28.6% | 1767, 33.9% | 322, 39.1% | 1841, 36.9% | 1448, 24.5% | 214, 25.4% |
| Wealth | ||||||
| Bottom 50% | 180, 45.0% | 2607, 49.9% | 455, 55.1% | 2456, 49.2% | 312, 51.6% | 474, 56.0% |
| Top 50% | 220, 55.0% | 2613, 50.1% | 370, 44.9% | 2538, 50.8% | 293, 48.4% | 372, 44.0% |
| Country | ||||||
| Cuba | 141, 35.3% | 1476, 28.3% | 194, 23.5% | 1319, 26.4% | 157, 25.9% | 335, 39.6% |
| Dominican Republic | 64, 16.0% | 859, 16.5% | 110, 13.3% | 711, 14.2% | 113, 18.7% | 209, 24.7% |
| Peru | 13, 3.3% | 395, 7.6% | 102, 12.4% | 465, 9.3% | 21, 3.5% | 24, 2.8% |
| Venezuela | 52, 13.0% | 572, 10.9% | 99, 12.0% | 572, 11.5% | 90, 14.9% | 61, 7.2% |
| Mexico | 57, 14.3% | 1007, 19.3% | 221, 26.8% | 1056, 21.1% | 108, 17.8% | 121, 14.3% |
| Puerto Rico | 73, 18.3% | 913, 17.5% | 99, 12.0% | 873, 17.5% | 116, 19.2% | 96, 11.4% |
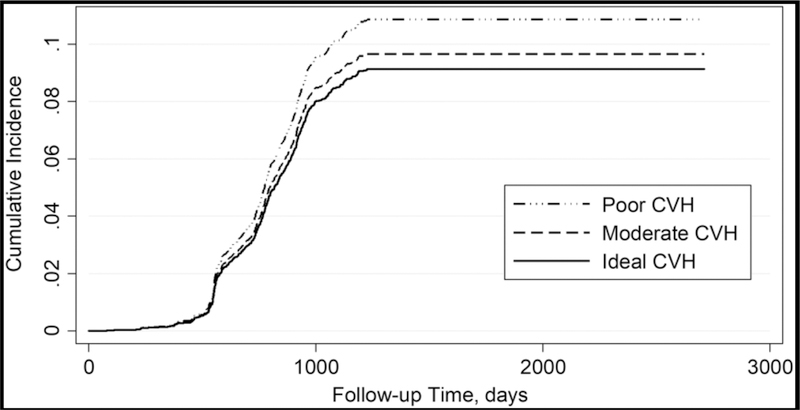
Figure 1 shows the cummulative incidence function of dementia by the three levels of CVH. Those with poor CVH levels had a higher cumulative incidence of dementia that those with moderate and ideal levels, which had a similar dementia incidence. Table 2 shows the unadjusted and adjusted subhazard ratios of dementia by baseline CVH and stratified by wealth levels. The risk of dementia was 4% lower with each additional point of the 0–14 continuous score of CVH in the unadjusted associations (p=0.04). However, this association attenuated slightly and was not statistically significant after adjusting for age, gender, education, assets and country. Compared to poor CVH, participants with moderate and ideal levels of CVH had a significantly lower risk of dementia both in the adjusted and unadjusted models. Maintaining moderate CVH conveyed a 27% (Adj. SHR: 0.73, 95% Confidence Interval [CI]: 0.54, 0.97) lower risk of dementia compare poor CVH. As well, participants with ideal CVH had a 34% (Adj. SHR: 0.66, 95% CI: 0.46, 0.96) lower risk of dementia than those with poor CVH.
Figure 1.
Cumulative incidence function for dementia by cardiovascular health (CVH) score categories.
Table 2:
Unadjusted and adjusted subhazard ratios of dementia by baseline categories of cardiovascular health (CVH), total and stratified by level of wealth
| Unadjusted SHR | p-value | Adjusted SHR* | p-value | |
|---|---|---|---|---|
| Total (n=6447) | ||||
| Total CVH | 0.96 (0.92, 0.997) | 0.040 | 0.97 (0.93, 1.02) | 0.189 |
| CVH Category | ||||
| Poor | Reference | Reference | ||
| Moderate | 0.72 (0.54, 0.95) | 0.022 | 0.73 (0.54, 0.97) | 0.030 |
| Ideal | 0.59 (0.41, 0.85) | 0.004 | 0.66 (0.46, 0.96) | 0.031 |
| Top 50% Wealth (n=3203) | ||||
| CVH Category | ||||
| Poor | Reference | Reference | ||
| Moderate | 0.88 (0.58, 1.33) | 0.545 | 0.93 (0.61, 1.42) | 0.725 |
| Ideal | 0.49 (0.27, 0.89) | 0.019 | 0.60 (0.33, 1.1) | 0.098 |
| Bottom 50% Wealth (n=3242) | ||||
| CVH Category | ||||
| Poor | Reference | Reference | ||
| Moderate | 0.58 (0.39, 0.86) | 0.006 | 0.57 (0.39, 0.85) | 0.005 |
| Ideal | 0.61 (0.68, 0.97) | 0.038 | 0.65 (0.40, 1.1) | 0.082 |
Adjusted for age (4 categories), sex, education (3 categories), wealth, country
In secondary analysis stratified by wealth, participants in the top 50% of wealth with ideal CVH had lower risk of dementa (Adj. SHR: 0.60, p=0.098) than those with poor CVH, after adjusting for covariates. Among those in the bottom 50% of wealth, unadjusted associations were statistically significant for both moderate and ideal CVH levels and the strength of the association remained after adjustment (Adj. SHRs: 0.57 & 0.65), although ideal CVH was only marginally significant (p=0.085). Those with moderate and ideal levels of CVH had 54–75% lower risk of dementia than those with poor levels.
Discussion
To our knowledge, this is the first study to explore the longitudinal association between an index of modifiable CVH risk factors and dementia incidence among Latin American older adults. This is also one of the first studies worldwide to study such associations. Our analyses build upon the Framingham study by assessing these associations among individuals in a wide spectrum of socioeconomic positions from low- and middle-income countries, which increases the external validity of our results. Another strength compared to previous research is that this study also accounts for competing risk of death, decreasing bias related to the associations between CVH, dementia and mortality. 29 Our findings suggest that CVH is inversely associated with dementia incidence in this population. These associations were mostly present among individuals in the bottom 50% of wealth.
We hypothesized that higher levels of CVH would be inversely associated with dementia incidence. In line with our hypothesis, we found that moderate and ideal levels of CVH were associated with a lower dementia incidence than poor levels. These findings are in line with a growing literature showing that cumulative indices of modifiable CVH factors are associated with stroke, cognitive functioning, decline, brain integrity and dementia. 19–27,34 Findings are consistent with the Framingham study in that the 0–14 continuous CVH index was not associated with dementia incidence. 21 Results are also similar to those in the REGARDS study, which found a lower cognitive impairment incidence among an ethnically diverse American middle age adult sample with moderate and ideal CVH levels in a diverse sample of middle agers. 26 In addition, the risk of dementia was similar among those with moderate and ideal CVH levels and the effect sizes were comparable to the ones found in this study.
Similar to findings from individual risk factors, 12 most studies exploring the association between indices of modifiable CVH factors and brain health have found associations among young or middle-aged individuals. 19,20,22–26,34 However, in the present study we found that such associations exist among individuals aged 65 and over. Whereas the earlier findings reinforce the importance of maintaining ideal levels of CVH decades before a potential dementia onset, our findings offer a rather optimistic picture for individuals and policy-makers in that even moderate levels of CVH are sufficient to reduce dementia risk.
This study shows that the association between CVH and dementia was mostly present among participants at the bottom 50% of wealth. The Study of Latinos in the USA had similar findings in which CVH was cross-sectionally associated with verbal learning scores among those with low levels of education. 19 However, the Study of Latinos found an interaction of education adjusted for income whereas in our analyses, we have found a differential association by wealth adjusted for education. These different findings might shed light into independent mechanisms interacting with CVH. CVH plays an important role in β-amyloid and other neurodegenerative protein deposition and clearance as well as vascular pathology development, which might interact with neurodegeneration. 46,47 The moderating effect of education found in the Study of Latinos might be related to cognitive reserve buffering the effects of poor CVH among those with higher levels of education. 48 However, since we adjusted for education in our study, an alternative explanation to our findings is that the effect of poor CVH on the brain is aggravated by the well-established chronic stress driven by lower social standing. 49 Recent findings support this idea as comorbid depression and diabetes significantly increased risk for mild cognitive impairment and Alzheimer’s disease among Mexican-Americans. 50
These results are the first attempt to examine the longitudinal association between a Life’s Simple 7-like index of modifiable CVH factors and dementia in the Latin American population. Our previous study found that a similar four-component index was associated with cognitive functioning cross-sectionally in a representative sample of Mexicans 50 and older. 34 Our study extends findings from the USA by demonstrating that an index of modifiable CVH risk factors is associated with dementia incidence in a diverse sample of Latin American older adults. This diverse sample reflects the population of catchment areas from six countries in Latin America, men and women, with different ancestries and varying levels of wealth. Besides the implications for Latin America, findings may also apply to some extent to the Latino population in the USA, where 17% of the population identify as Hispanic or Latino, mostly from Puerto Rico, Mexico and Cuba. 51 In fact the Study of Latinos found CVH to be associated with cognitive function among middle-aged Latinos of different origins. 19 However, generizability might be compromised by acculturation effects and the Hispanic paradox in which there is a positive selection of immigrants from Latin America to the USA. 52,53
Study limitations
There are limitations to this study. First, the operationalization of CVH did not replicate the Life’s Simple 7 index fully. 18 Differences in the operationalization might compromise the comparability between our study and others. Second, the CVH index has not been previously validated in Latin America although the individual CVH criteria used in the USA and Latin America are comparable. Third, the assessment of a CVH index gives the same weight to the different domains, which might not represent their real contribution to CVH.
Public health implications and future research recommendations
Regarding potential public health implications, this study highlights the importance of maintaining ideal or moderate levels of CVH to reduce the risk of dementia. Our findings convey a positive and important public health message that even moderate levels of CVH are enough to reduce dementia risk. Given that 94% of the study population of Latin Americans 65 and older have moderate or ideal levels of CVH, policy-makers should put a great effort in promoting maintenance of CVH. These policies may include media and educational campaigns, labeling and consumer information, taxation, subsidies, and other economic incentives, local environmental changes, direct restrictions, and mandates. 54 Strengthening the countries’ welfare state might also diminish the differential association between CVH and dementia by wealth. Our findings may help inform a holistic CVH promotion at the primary care level in Latin American countries with an existing dementia national plan (i.e. Cuba, Mexico or Puerto Rico). 55 In Cuba for example, there are protocols in place to promote physical activity, smoking cessation and prevent hypertension and diabetes among older adults. However, Cuba’s dementia risk-reduction program is not being implemented equally in all regions and was approved without additional budget allocation, which may hinder the execution of some of the proposed measures. 56
Further research is needed to better understand the differential association between CVH and dementia incidence by wealth. Potential effect modifiers such as social participation, social contact and loneliness should also be explored. 57 Further research should also aim to understand the effect of CVH maintenance across the lifespan in reducing dementia risk rather than studying CVH at a single point in time. Also, dementia risk-reduction clinical trials should aim to improve CVH among those with poor CVH levels.
Conclusion
These findings add to the growing evidence that CVH is important for optimal brain health 17 and is the first study in Latin America to address the association between CVH and dementia incidence using an index of modifiable levels of CVH. We found that moderate and ideal levels of CVH were associated with a lower incidence of dementia among older adults from six countries in Latin America. These results suggest that dementia-related policies in Latin America need to focus on reaching and maintaining at least moderate CVH levels in older age.
Supplementary Material
Key points:
Few studies have explored the link between modifiable cardiovascular health indices and dementia risk
Research linking heart and brain health is scarce in Latino America
Dementia risk is lower among Latin American elders with moderate/ideal cardiovascular health
The association between cardiovascular health and dementia risk differs by wealth
Acknowledgements
This is a secondary analysis of data collected by the 10/66 Dementia Research Group (www.alz.co.uk/1066). The 10/66 DRG is led by Martin Prince at the Institute of Psychiatry, Psychology and Neuroscience, King’s College London. The other principal investigators, data custodians and responsible for research governance in each site are Juan Llibre Rodriguez (Cuba), Daisy Acosta (Dominican Republic), Mariella Guerra (Peru), Aquiles Salas (Venezuela), Ana Luisa Sosa (Mexico), KS Jacob (Vellore, India), Joseph D Williams (Chennai, India), Ivonne Jimenez (Puerto Rico) and Yueqin Huang (China). The 10/66 Dementia Research Group’s research has been funded by the Wellcome Trust Health Consequences of Population Change Programme (GR066133 – Prevalence phase in Cuba and Brazil; GR080002-Incidence phase in Peru, Mexico, Argentina, Cuba, Dominican Republic, Venezuela and China), the World Health Organization (India, Dominican Republic and China), the US Alzheimer’s Association (IIRG – 04 – 1286 - Peru, Mexico and Argentina), the Puerto Rico State Legislature (Puerto Rico), and FONACIT/ CDCH/ UCV (Venezuela). The authors are thankful to 10/66 researchers, staff and participants for making such important data available.
Funding
Research reported in this publication was supported by the National Institute on Aging of the National Institutes of Health under Award Number P30AG035982. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Conflicts of interest: none
Contributor Information
Jaime Perales-Puchalt, University of Kansas Alzheimer’s Disease Center, MS6002, Fairway, KS, 66205, USA.
Michelle L Vidoni, The University of Texas Health Science Center at Houston; Center for Clinical and Translational Sciences (CCTS); Biostatistics, Epidemiology, and Research Design (BERD) core; 6410 Fannin; Houston, TX 77030, USA.
Juan Llibre Rodríguez, Facultad de Medicina Finley-Albarrán, Universidad de Ciencias Médicas de la Habana, Habana, 11500, Cuba.
Eric D Vidoni, University of Kansas Alzheimer’s Disease Center, MS6002, Fairway, KS 66205, USA.
Sandra Billinger, Department of Physical Therapy and Rehabilitation Science, University of Kansas Medical Center, Kansas City, KS 66160, USA.
Jeffrey Burns, University of Kansas Alzheimer’s Disease Center, MS6002, Fairway, KS 66205, USA.
Maëlenn Guerchet, King’s College London, Centre for Global Mental Health, Health Services and Population Research Department, Institute of Psychiatry, Psychology and Neuroscience, London, SE5 8AF, United Kingdom.
MinJae Lee, The University of Texas Health Science Center at Houston, McGovern Medical School; Houston, TX 77030, USA.
References
- 1.United Nations. World Population Prospects: The 2017 Revision, custom data acquired via website https://population.un.org/wpp/DataQuery/: Department of Economic and Social Affairs, Population Division;2017.
- 2.Barreto SM, Miranda JJ, Figueroa JP, et al. Epidemiology in Latin America and the Caribbean: current situation and challenges. International journal of epidemiology 2012;41(2):557–571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Custodio N, Wheelock A, Thumala D, Slachevsky A. Dementia in latin america: epidemiological evidence and implications for public policy. Frontiers in aging neuroscience 2017;9:221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Baez S, Ibáñez A. Dementia in Latin America: An emergent silent tsunami. Frontiers in aging neuroscience 2016;8:253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Prince M, Wimo A, Guerchet M, Ali G-C, Wu Y-T, Prina M. The global impact of dementia: an analysis of prevalence, incidence, cost and trends London, UK: August, 2015. 2015. [Google Scholar]
- 6.Prince M, Acosta D, Ferri CP, et al. Dementia incidence and mortality in middle-income countries, and associations with indicators of cognitive reserve: a 10/66 Dementia Research Group population-based cohort study. The Lancet 2012;380(9836):50–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Murray CJ, Vos T, Lozano R, et al. Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. The lancet 2012;380(9859):2197–2223. [DOI] [PubMed] [Google Scholar]
- 8.World Health Organization. Dementia: a public health priority World Health Organization; 2012. [Google Scholar]
- 9.Schulz R, O’Brien AT, Bookwala J, Fleissner K. Psychiatric and physical morbidity effects of dementia caregiving: prevalence, correlates, and causes. The gerontologist 1995;35(6):771–791. [DOI] [PubMed] [Google Scholar]
- 10.Veras RP, Caldas CP, Dantas SB, Sancho LG, Sicsu B, Motta LB. Demented elderly people living at home in Rio de Janeiro, Brazil: Evaluation of expenditure on care. Psychogeriatrics 2008;8(2):88–95. [Google Scholar]
- 11.Wimo A, Guerchet M, Ali G-C, et al. The worldwide costs of dementia 2015 and comparisons with 2010. Alzheimer’s & dementia: the journal of the Alzheimer’s Association 2017;13(1):1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pase MP, Satizabal CL, Seshadri S. Role of improved vascular health in the declining incidence of dementia. Stroke 2017;48(7):2013–2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yusuf S, Reddy S, Ôunpuu S, Anand S. Global burden of cardiovascular diseases: part I: general considerations, the epidemiologic transition, risk factors, and impact of urbanization. Circulation 2001;104(22):2746–2753. [DOI] [PubMed] [Google Scholar]
- 14.Schargrodsky H, Hernández-Hernández R, Champagne BM, et al. CARMELA: assessment of cardiovascular risk in seven Latin American cities. The American journal of medicine 2008;121(1):58–65. [DOI] [PubMed] [Google Scholar]
- 15.Levin BE, Llabre MM, Dong C, et al. Modeling metabolic syndrome and its association with cognition: the Northern Manhattan study. Journal of the International Neuropsychological Society 2014;20(10):951–960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Albanese E, Dangour AD, Uauy R, et al. Dietary fish and meat intake and dementia in Latin America, China, and India: a 10/66 Dementia Research Group population-based study–. The American journal of clinical nutrition 2009;90(2):392–400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gorelick PB, Furie KL, Iadecola C, et al. Defining optimal brain health in adults: a presidential advisory from the American Heart Association/American Stroke Association. Stroke 2017;48(10):e284–e303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lloyd-Jones DM, Hong Y, Labarthe D, et al. Defining and setting national goals for cardiovascular health promotion and disease reduction. Circulation 2010;121(4):586–613. [DOI] [PubMed] [Google Scholar]
- 19.González HM, Tarraf W, Gouskova N, et al. Life’s Simple 7’s Cardiovascular Health Metrics are Associated with Hispanic/Latino Neurocognitive Function: HCHS/SOL Results. Journal of Alzheimer’s Disease 2016;53(3):955–965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.González HM, Tarraf W, Harrison K, et al. Midlife cardiovascular health and 20-year cognitive decline: Atherosclerosis Risk in Communities Study results. Alzheimer’s & Dementia 2017. [DOI] [PMC free article] [PubMed]
- 21.Pase MP, Beiser A, Enserro D, et al. Association of ideal cardiovascular health with vascular brain injury and incident dementia. Stroke 2016:STROKEAHA. 115.012608. [DOI] [PMC free article] [PubMed]
- 22.Bancks MP, Allen NB, Dubey P, et al. Cardiovascular health in young adulthood and structural brain MRI in midlife The CARDIA study. Neurology 2017;89(7):680–686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lutski M, Weinstein G, Goldbourt U, Tanne D. Cardiovascular Health and Cognitive Decline 2 Decades Later in Men with Preexisting Coronary Artery Disease. The American journal of cardiology 2017. [DOI] [PubMed]
- 24.Reis JP, Loria CM, Launer LJ, et al. Cardiovascular health through young adulthood and cognitive functioning in midlife. Annals of neurology 2013;73(2):170–179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Crichton GE, Elias MF, Davey A, Alkerwi Aa. Cardiovascular health and cognitive function: the Maine-Syracuse Longitudinal Study. PLoS One 2014;9(3):e89317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Thacker EL, Gillett SR, Wadley VG, et al. The American Heart Association Life’s Simple 7 and incident cognitive impairment: the REasons for Geographic And Racial Differences in Stroke (REGARDS) study. Journal of the American Heart Association 2014;3(3):e000635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gardener H, Wright CB, Dong C, et al. Ideal cardiovascular health and cognitive aging in the Northern Manhattan Study. Journal of the American Heart Association 2016;5(3):e002731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hessler JB, Ander K-H, Brönner M, et al. Predicting dementia in primary care patients with a cardiovascular health metric: a prospective population-based study. BMC neurology 2016;16(1):116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Muntner P, Judd SE, Gao L, et al. Cardiovascular risk factors in CKD associate with both ESRD and mortality. Journal of the American Society of Nephrology 2013:ASN. 2012070642. [DOI] [PMC free article] [PubMed]
- 30.Messina J, Silva J. Wage inequality in Latin America: Understanding the past to prepare nthe future Washington DC, USA: 2018. [Google Scholar]
- 31.Prince M, Ferri CP, Acosta D, et al. The protocols for the 10/66 dementia research group population-based research programme. BMC public health 2007;7(1):165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Prina AM, Acosta D, Acosta I, et al. Cohort profile: the 10/66 study. International journal of epidemiology 2016;46(2):406–406i. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.World Health Organization. Waist circumference and waist-hip ratio: report of a WHO expert consultation, Geneva, 8–11 December 2008 2011. [Google Scholar]
- 34.Perales J, Hinton L, Burns J, Vidoni ED. Cardiovascular health and cognitive function among Mexican older adults: cross-sectional results from the WHO Study on Global Ageing and Adult Health. International psychogeriatrics 2018:1–10. [DOI] [PMC free article] [PubMed]
- 35.Unger RK. Toward a redefinition of sex and gender. American Psychologist 1979;34(11):1085. [Google Scholar]
- 36.Prince M, Acosta D, Chiu H, Scazufca M, Varghese M, Group DR. Dementia diagnosis in developing countries: a cross-cultural validation study. The Lancet 2003;361(9361):909–917. [DOI] [PubMed] [Google Scholar]
- 37.Prince MJ, De Rodriguez JL, Noriega L, et al. The 10/66 Dementia Research Group’s fully operationalised DSM-IV dementia computerized diagnostic algorithm, compared with the 10/66 dementia algorithm and a clinician diagnosis: a population validation study. BMC public health 2008;8(1):219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. Am. Psychiatr. Assoc Washington, DC; 1994. [Google Scholar]
- 39.Jotheeswaran A, Williams JD, Prince MJ. The predictive validity of the 10/66 Dementia diagnosis in Chennai, India–a three year follow-up study of cases identified at baseline. Alzheimer disease and associated disorders 2010;24(3):296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hall K, Hendrie H, Brittain H, et al. The development of a dementia screening interview in 2 distinct languages. International Journal of Methods in Psychiatric Research 1993;3(1):1–28. [Google Scholar]
- 41.Ganguli M, Chandra V, Gilby JE, et al. Cognitive test performance in a community-based nondemented elderly sample in rural India: the Indo-US Cross-National Dementia Epidemiology Study. International Psychogeriatrics 1996;8(4):507–524. [DOI] [PubMed] [Google Scholar]
- 42.Copeland J, Dewey ME, Griffiths-Jones H. A computerized psychiatric diagnostic system and case nomenclature for elderly subjects: GMS and AGECAT. Psychological medicine 1986;16(1):89–99. [DOI] [PubMed] [Google Scholar]
- 43.Dewey ME, Copeland JR. Diagnosis of dementia from the history and aetiology schedule. International journal of geriatric psychiatry 2001;16(9):912–917. [DOI] [PubMed] [Google Scholar]
- 44.Fine JP, Gray RJ. A proportional hazards model for the subdistribution of a competing risk. Journal of the American statistical association 1999;94(446):496–509. [Google Scholar]
- 45.StataCorp. Stata Statistical Software: Release 13 College Station, TX: 2013. [Google Scholar]
- 46.Gottesman RF, Schneider AL, Zhou Y, et al. Association between midlife vascular risk factors and estimated brain amyloid deposition. Jama 2017;317(14):1443–1450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Boyle PA, Yu L, Wilson RS, Leurgans SE, Schneider JA, Bennett DA. Person-specific contribution of neuropathologies to cognitive loss in old age. Annals of neurology 2018;83(1):74–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Tucker AM, Stern Y. Cognitive reserve and the aging brain. Geriatric neurology 2014:118–125.
- 49.Marmot M The status syndrome: how social standing affects our health and longevity 2004. London: Bloomsbury. [Google Scholar]
- 50.Johnson LA, Gamboa A, Vintimilla R, et al. Comorbid depression and diabetes as a risk for mild cognitive impairment and Alzheimer’s disease in elderly Mexican Americans. Journal of Alzheimer’s Disease 2015;47(1):129–136. [DOI] [PubMed] [Google Scholar]
- 51.Flores A How the U.S. Hispanic population is changing Washington, DC: Pew Research Center;2017. [Google Scholar]
- 52.Markides KS, Eschbach K. Aging, migration, and mortality: current status of research on the Hispanic paradox. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences 2005;60(Special_Issue_2):S68–S75. [DOI] [PubMed] [Google Scholar]
- 53.Kondo KK, Rossi JS, Schwartz SJ, Zamboanga BL, Scalf CD. Acculturation and cigarette smoking in Hispanic women: A meta-analysis. J Ethn Subst Abuse 2016;15(1):46–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Mozaffarian D, Afshin A, Benowitz NL, et al. Population approaches to improve diet, physical activity, and smoking habits: a scientific statement from the American Heart Association. Circulation 2012:CIR. 0b013e318260a318220b. [DOI] [PMC free article] [PubMed]
- 55.Alzheimer’s Disease International. From plan to impact: Progress towards targets of the Global action plan on dementia London, UK: 2018. [Google Scholar]
- 56.Bosch-Bayard RI, Llibre-Rodríguez JJ, Fernández-Seco A, et al. Cuba’s strategy for Alzheimer disease and dementia syndromes. MEDICC review 2016;18:9–13. [DOI] [PubMed] [Google Scholar]
- 57.Kuiper JS, Zuidersma M, Voshaar RCO, et al. Social relationships and risk of dementia: a systematic review and meta-analysis of longitudinal cohort studies. Ageing research reviews 2015;22:39–57. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.