Abstract
Background:
The Government of Canada legalized nonmedical use of cannabis in October 2018. Our objectives were to determine the percentage of Canadians intending to try or increase their cannabis use following legalization and to explore characteristics associated with this intent.
Methods:
We used data from the 2018 National Cannabis Survey and constructed multivariable regression models. Respondents’ data were weighted and bootstrapped. We report relative measures of association as adjusted odds ratios (ORs) and absolute measures of association as adjusted risk increases (RIs).
Results:
Among the 39 000 households selected for recruitment for the survey, 17 089 respondents provided complete data (43.8%) and our weighted analysis represented 27 808 081 Canadians aged 15 years and older. An estimated 18.5% of respondents (95% confidence interval [CI] 17.6%–19.5%) indicated they intended to try or increase cannabis use following legalization. Being more likely to try or increase cannabis use was associated with younger age (15–24 yr v. ≥ 65 yr; adjusted OR 3.8, 95% CI 2.6–5.6; adjusted RI 20.1%, 95% CI 13.9%–26.2%), cannabis use in the past 3 months versus no use (adjusted OR 3.3, 95% CI 2.8–3.9; adjusted RI 20.4%, 95% CI 17.1%–23.6%), higher income (≥ $80 000 v. < $40 000; adjusted OR 1.5, 95% CI 1.3–1.9; adjusted RI 6.1%, 95% CI 3.2%–9.0%) and poor or fair mental health versus good to excellent mental health (adjusted OR 2.0, 95% CI 1.6–2.6; adjusted RI 11.5%, 95% CI 6.7%–16.2%).
Interpretation:
Nearly 1 in 5 respondents reported that they intended to try or increase cannabis use after legalization; however, intention may not translate into behaviour. Continued monitoring should help to establish rates and patterns of cannabis use among Canadians following legalization.
According to the 2017 Canadian Tobacco Alcohol and Drugs Survey, 15% of Canadians aged 15 years and older reported using cannabis in the past year, the same percentage as for current cigarette use.1 Approximately 78% of respondents reported consuming alcohol in the past year and 24% reported heavy drinking.1 Overall, substance use was highest among males aged 20–24 years.1 There is substantial evidence that cannabis use is associated with motor vehicle collisions, decreased birthweight (if consumed during pregnancy), chronic bronchitis episodes (if cannabis is inhaled), psychotic symptoms and disorders, and cannabis addiction.2–6 The lifetime risk of cannabis abuse (recurrent use) or dependence (symptoms of tolerance and withdrawal) among Canadians was 6.8% in 2012, and 1.3% of Canadians met criteria for cannabis abuse or dependence in the past year.6 Moreover, the potency of illicit cannabis increased from 4% in 1995 to 12% in 2014, with higher potency associated with increased risk of adverse health outcomes.7–11 In general, people who use cannabis more frequently and at a younger age are at higher risk for harm.11,12
In an effort to promote responsible use, deter criminal activity and protect public health and safety, the federal government legalized nonmedical use of cannabis on Oct. 17, 2018.13 Cannabis use for medical purposes has been legal in Canada since 2001.14 The evidence from the United States on the impact of legalization is mixed, with some studies showing increased rates of use and others showing no change.15–18 It is crucial to monitor the prevalence of cannabis use, patterns of use and modes of use to determine the impact of policy change.19 In 2018, Statistics Canada, the national statistics agency, developed and implemented the National Cannabis Survey (NCS), a cross-sectional survey designed to better understand the frequency of cannabis use and monitor changes in attitudes and behaviour as a result of legalization.20
Our study objectives were to (a) determine the percentage of Canadians (aged ≥ 15 yr) likely to try or increase cannabis use after legalization of use for nonmedical purposes and (b) explore characteristics associated with intent to try or increase cannabis use.
Methods
We followed the reporting standards outlined in the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines.21
Study design and respondents
This was a cross-sectional study involving analysis of the 2018 NCS master file.20,22 The NCS was developed by Statistics Canada in consultation with the Public Health Agency of Canada, the Department of Justice Canada and Public Safety Canada. Cognitive testing of questionnaire content was conducted and validation of estimates was done through cross-tabulations of other data and consultation with Statistics Canada stakeholders. The data used in this study were collected before legalization of nonmedical use of cannabis, from February to September 2018, in 3 waves. Participation in the NCS was voluntary and data were collected through an electronic questionnaire or computer-assisted telephone interview. The study population consisted of noninstitutionalized Canadians aged 15 years and older who resided in one of Canada’s 10 provinces or one of its 3 territory capital cities. The sampling method was a 2-stage simple random sample of dwellings and people stratified by province or territory, which aimed to represent the Canadian population.20 The authors of this paper have no relationship with the developers of the NCS and accessed data through the Statistics Canada Research Data Centre (RDC) at McMaster University.23
Measures
Our primary outcome measure was derived from an NCS question that asked respondents if they were likely to try cannabis or increase their consumption when it became legal to use it for nonmedical purposes.22 The response options were “Yes,” “Maybe” and “No.” We also summarized whether respondents indicated they would be more likely to try different types of cannabis products or acquire cannabis from another source, using pairwise deletion for missing data (i.e., reporting all cases for which we had data). Information on gender, age, cannabis use in the past 3 months, education level, income level, main activity during the previous week and self-reported mental health are also reported. As the NCS categories of male and female for gender are commonly understood as the sex of a person, we have interpreted them as such in our paper.24 Categories for age, education, income, main activity and self-reported mental health were collapsed to ensure adequate cell size and simplify analysis and interpretation. The full questionnaire is available elsewhere.22
Statistical analysis
Data from the 3 independent NCS waves were pooled for analysis. We used descriptive statistics to summarize the data, and we constructed univariable and multivariable logistic regression models to explore factors associated with the intent to try or increase cannabis use following legalization (“Yes” and “Maybe” were combined and compared with “No”). Among respondents likely to try or increase cannabis use after legalization, we considered those who had not used cannabis in the past 3 months to be those looking to try. Our independent variables were sex, age, cannabis use in the past 3 months, education, income, main activity and self-reported mental health. We adjusted our multivariable regression model for survey wave and province or territory of residence. Results are presented as odds ratios (ORs) with 95% confidence intervals (CIs). An OR greater than 1 indicates an increased association, meaning the odds of respondents endorsing the intent to try or increase cannabis use following legalization are greater in the comparison group than in the reference group. All analyses were 2-tailed and statistical significance was defined as p < 0.05. For all statistically significant associations in our adjusted model, we calculated adjusted risk increases (RIs) as the difference between the risk of the outcome in the reference group (e.g., Canadians aged ≥ 65 yr) and the risk in the comparison group (e.g., Canadians aged 15–24 yr), while holding all other variables constant.25
Before conducting our analysis, we reviewed unweighted cross-tabulations of independent variables and the outcome to ensure adequate cell sizes (≥ 10 events).26 Bootstrap weights provided by Statistics Canada were applied to convert unweighted frequencies to represent the Canadian population and adjust for nonresponse bias in the survey sampling design.27 Missing data were excluded from the regression analysis using listwise deletion (i.e., only complete cases were analyzed). The likelihood ratio test determined if the multivariable logistic regression model fit significantly better than a model with no predictors, and the Wald test indicated whether predictors in the model had significant associations at the p < 0.05 level compared with no association. We performed a Hosmer–Lemeshow test, which compares whether or not observed rates and associations match expected rates and associations in subgroup analyses in the model population, to assess the goodness of fit of our adjusted model.28 All data pooling, modification and statistical analyses were performed using Stata/SE 15 software (StataCorp LLC).
Ethics approval
As per Article 2.2(a) of the Tri-Council Policy Statement: Ethical Conduct for Research Involving Humans, research is exempt from research ethics board review if it relies exclusively on publicly available information that is legally accessible to the public and appropriately protected by law.29 Our results were reviewed by an analyst at the Statistics Canada Research Data Centre at McMaster University before release to ensure that the confidentiality of survey respondents’ information was respected.
Results
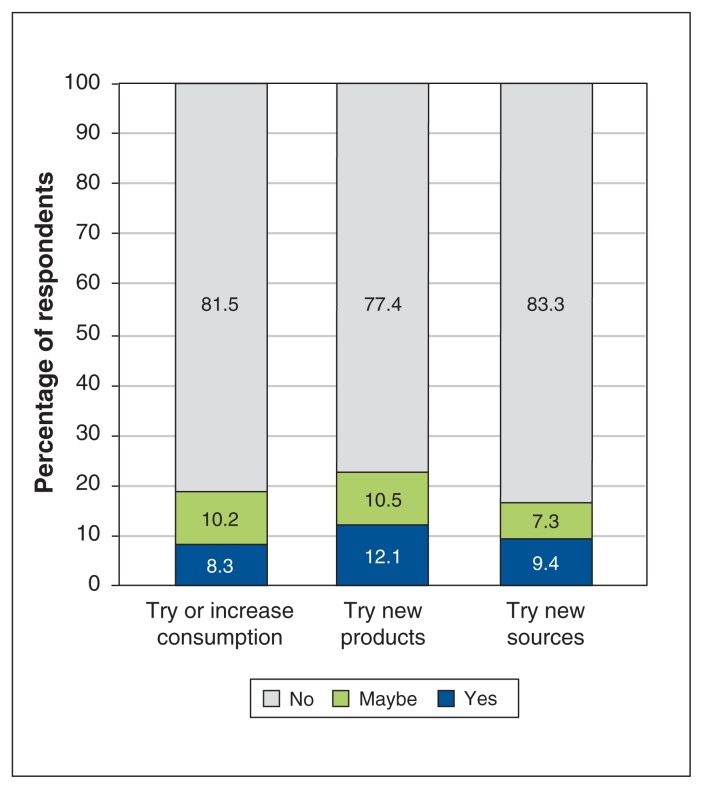
There were 39 000 households selected for recruitment for NCS Waves 1–3 and the response rates were 51.2% (Wave 1), 51.3% (Wave 2) and 51.6% (Wave 3). A total of 17 089 respondents provided complete data and were included in our multivariable logistic regression analysis (completion rate 43.8%). There was an equal distribution of males and females, most were employed (59.2%) and reported good to excellent mental health (93.8%), and 15.2% reported use of cannabis in the past 3 months (Table 1). The “please specify” category of sex was removed from analysis and reporting because of low response (n < 10). Overall, 18.5% (95% CI 17.6%–19.5%) of respondents reported they were likely to try or increase their cannabis use after legalization for nonmedical purposes; of these respondents, 66.5% reported not having used cannabis in the past 3 months. Almost a quarter (22.6%, 95% CI 21.7%–23.6%) reported they were likely to try different types of cannabis products and 16.7% (95% CI 15.8%–17.6%) reported they were likely to acquire cannabis from a new source after legalization (Figure 1).
Table 1:
Weighted table of respondent characteristics (n = 27 808 081)
| Characteristic | Percentage (95% CI) |
|---|---|
| Sex | |
| Female | 50.3 (50.0–50.6) |
| Male | 49.7 (49.4–50.0) |
| Age, yr | |
| ≥ 65 | 18.5 (18.2–18.7) |
| 45–64 | 32.6 (32.3–32.9) |
| 35–44 | 16.6 (16.4–16.8) |
| 25–34 | 19.5 (18.7–20.4) |
| 15–24 | 12.9 (12.0–13.7) |
| Cannabis use in past 3 mo | |
| No | 84.8 (84.0–85.7) |
| Yes | 15.2 (14.3–16.0) |
| Education level | |
| Bachelor’s degree or higher | 32.7 (31.7–33.8) |
| College or diploma | 33.7 (32.6–34.7) |
| Less than HS or HS only | 33.6 (32.6–34.7) |
| Income level, $ | |
| < 40 000 | 49.7 (48.7–50.8) |
| 40 000–79 999 | 32.0 (31.0–33.1) |
| ≥ 80 000 | 18.3 (17.5–19.0) |
| Main activity | |
| Employed | 59.2 (58.1–60.2) |
| Student | 6.8 (6.1–7.5) |
| Caregiving/housework | 8.4 (7.8–9.1) |
| Retired/LTI | 20.6 (20.0–21.2) |
| Other | 5.0 (4.4–5.6) |
| Mental health | |
| Good to excellent | 93.8 (93.2–94.4) |
| Fair or poor | 6.2 (5.6–6.8) |
| Province or territory capital city, grouped | |
| Ontario | 39.4 (39.1–39.7) |
| Quebec | 22.9 (22.7–23.2) |
| Atlantic provinces | 6.5 (6.4–6.6) |
| Manitoba | 3.4 (3.3–3.4) |
| Saskatchewan | 3.0 (2.9–3.0) |
| Alberta | 11.5 (11.3–11.6) |
| British Columbia | 13.3 (13.1–13.5) |
| Territory capital cities | 0.05 (0.049–0.051) |
| Survey wave | |
| 1 | 32.9 (32.6–33.2) |
| 2 | 33.5 (33.2–33.8) |
| 3 | 33.7 (33.4–34.0) |
Note: CI = confidence interval, HS = high school, LTI = long-term illness. Percentage totals for ages and provinces do not add up to exactly 100% because of bootstrapping and rounding. A weighted count (n) can be calculated by multiplying the proportion by the total population size.
Figure 1:
Percentages of respondents who reported they would try or increase their cannabis consumption (n = 29 928 424), try or consume different types of cannabis products (n = 29 607 064), and obtain or purchase cannabis from another source (n = 29 300 593), following legalization of cannabis use for nonmedical purposes.
In our adjusted model, younger age (15–24 yr; adjusted OR 3.8, 95% CI 2.6–5.6; adjusted RI 20.1%, 95% CI 13.9%–26.2%), cannabis use in past 3 months (adjusted OR 3.3, 95% CI 2.8–3.9; adjusted RI 20.4%, 95% CI 17.1%– 23.6%), higher income (≥ $80 000; adjusted OR 1.5, 95% CI 1.3–1.9; adjusted RI 6.1%, 95% CI 3.2%–9.0%) and poor or fair mental health (adjusted OR 2.0, 95% CI 1.6– 2.6; adjusted RI 11.5%, 95% CI 6.7%–16.2%) were associated with a greater likelihood of trying or increasing cannabis use following legalization compared with reference categories (Table 2). The Hosmer–Lemeshow (p = 0.5) and likelihood ratio (p < 0.05) tests suggested a good fit of our adjusted model.
Table 2:
Results of the multivariable logistic regression analysis with the outcome of interest being more likely to try or increase cannabis use after legalization (n = 27 808 081)
| Characteristic | Unadjusted OR (95% CI) | Adjusted OR (95% CI) | Adjusted risk increase percentage (95% CI) |
|---|---|---|---|
| Sex | |||
| Female | Ref. | Ref. | Ref. |
| Male | 1.3* (1.2–1.5) | 1.1 (1.0–1.3) | NR |
| Age, yr | |||
| ≥ 65 | Ref. | Ref. | Ref. |
| 45–64 | 1.7* (1.4–2.1) | 1.3 (1.0–1.6) | NR |
| 35–44 | 2.8* (2.3–3.3) | 1.8* (1.3–2.4) | 6.8 (3.5–10.1) |
| 25–34 | 4.2* (3.5–5.1) | 2.6* (1.9–3.4) | 12.6 (8.8–16.4) |
| 15–24 | 5.3* (4.2–6.8) | 3.8* (2.6–5.6) | 20.1 (13.9–26.2) |
| Cannabis use in past 3 mo | |||
| No | Ref. | Ref. | Ref. |
| Yes | 4.3* (3.7–5.0) | 3.3* (2.8–3.9) | 20.4 (17.1–23.6) |
| Education level | |||
| Bachelor’s degree or higher | Ref. | Ref. | Ref. |
| College or diploma | 0.8* (0.7–0.9) | 0.9 (0.7–1.0) | NR |
| Less than HS or HS only | 0.9 (0.8–1.1) | 0.9 (0.8–1.1) | NR |
| Income level, $ | |||
| < 40 000 | Ref. | Ref. | Ref. |
| 40 000–79 999 | 1.0 (0.8–1.1) | 1.2* (1.0–1.4) | 2.5 (0.3–4.7) |
| ≥ 80 000 | 1.2* (1.1–1.4) | 1.5* (1.3–1.9) | 6.1 (3.2–9.0) |
| Main activity | |||
| Employed | Ref. | Ref. | Ref. |
| Student | 1.4* (1.1–1.9) | 0.9 (0.6–1.3) | NR |
| Caregiving/housework | 0.8 (0.7–1.0) | 1.0 (0.8–1.3) | NR |
| Retired/LTI | 0.4* (0.4–0.5) | 0.9 (0.7–1.1) | NR |
| Other | 1.1 (0.8–1.4) | 0.8 (0.6–1.1) | NR |
| Mental health | |||
| Good to excellent | Ref. | Ref. | Ref. |
| Poor or fair | 2.6* (2.1–3.2) | 2.0* (1.6–2.6) | 11.5 (6.7–16.2) |
Note: CI = confidence interval, HS = high school, LTI = long-term illness, NR = not reported (for adjusted ORs that were not significant), OR = odds ratio, Ref. = reference category. The adjusted model includes province/territory and survey wave.
Wald test for predictors being significant in model at p < 0.05.
Interpretation
The NCS data collected before legalization suggest that nearly 1 in 5 Canadians were likely to try or increase cannabis use after it was legalized for nonmedical purposes, with the majority of these people not having used cannabis in the past 3 months. Respondents who were younger, had used cannabis in the past 3 months, reported having a higher income and reported worse mental health were significantly more likely to try or increase cannabis use following legalization. Nearly 1 in 4 respondents reported they were likely to try consuming different types of cannabis products, which will become legally available in October 2019.30 A 2017 survey of 1087 Canadians found that up to 46% were willing to try cannabis-infused food products.31 In addition, a 2018 Deloitte survey found that 58% of Canadians who use cannabis preferred edible products.32 We also found that 1 in 6 respondents would obtain cannabis from new sources after legalization, and the Deloitte survey reported that Canadians who use cannabis may shift up to 63% of their purchases toward legal channels.32
Complementing our findings, a 2014 survey of 3532 US adults aged 18–34 years found that 13.5% reported they would consume cannabis more frequently if use was legalized. 33 This is concerning as younger people are at a higher risk of experiencing harms associated with cannabis use than older people.11,12 However, previous studies have shown that the correlation between cannabis use intention and subsequent behaviour can range from 0.39 to 0.84, and it is affected by attitudes and subjective norms (perceived social pressure). 34–38 The 2014 US study also found that those who did not use cannabis but experienced anxiety were more interested in trying cannabis if use was legalized.33 Although some studies have reported an association between cannabis use and the development of schizophrenia, depressive disorders and increased suicidal ideation, attempts and completion, management of psychiatric disorders is also one of the top reasons cited for cannabis use.12,39–42 However, there is very limited evidence that cannabis use is effective for treating symptoms related to mental illnesses (e.g., anxiety and posttraumatic stress disorder).42–45
The public may underestimate the harms associated with cannabis use. A 2017 survey of 16 280 US adults found that 22.4% believe cannabis is not addictive and 9% believe there are no risks associated with cannabis use.46 A 2013 qualitative study of 76 Canadian youth (aged 14–19 yr) found that many were unaware of the potential harms associated with cannabis use.47 The Canadian Psychiatric Association released a position statement in 2018 highlighting concerns about the impact of increased access to cannabis on mental health, particularly for youth.48 The Canadian Medical Association has proposed developing educational interventions for youth considering the potential effects on brain development as well as advocating for a legal age of 21 years and restrictions for those under 25 years of age.49 NCS Wave 4 data (collected from November to December 2018) show that rates of self-reported cannabis use (15%) did not change in the 3 months immediately after legalization, although 19% of respondents indicated they intended to use cannabis in the next 3 months.50 Data for the first wave of NCS 2019 (collected from February to March 2019) indicate that 18% of respondents reported use in the past 3 months; the highest increases were seen among males aged 45–64 years and over 646 000 Canadians were estimated to be first-time cannabis users.51 Intentions may take time to translate into action and behaviour may continue to change as nonmedical use of cannabis becomes normalized.
Limitations
Self-reported use of cannabis and intention to try or increase use may be subject to measurement error and bias. It is possible that the prevalence of cannabis use may have been underreported, although a number of studies have found data on self-reported cannabis use to be as reliable as data on other self-reported behaviours.52–54 The NCS did not collect information on people in institutions and our findings may not be generalizable to this population. Furthermore, the NCS data we used for our study measured only intentions to use cannabis, not actual changes in behaviour.
Conclusion
Nearly 1 in 5 Canadians may try or increase cannabis use following legalization of use for nonmedical purposes, particularly those who are younger, who have used cannabis in the past 3 months, who have a higher income and who self-report their mental health as poor or fair. Clinicians, public health officials and policy-makers should pay special attention to these higher risk populations to ensure informed decision-making and responsible use. Continued monitoring through national-level surveys, such as the NCS, will be crucial in establishing rates and patterns of cannabis use among Canadians following legalization of use for nonmedical purposes.
Supplementary Material
Acknowledgements
The authors would like to thank Drs. Li Wang, Peter Kitchen, Mustafa Ornek (Statistics Canada Research Data Centre at McMaster University) and Behnam Sadeghi (Department of Health Research Methods, Evidence, and Impact, McMaster University) for statistical support. They also thank Dr. Emmanuel Guindon (Department of Health Research Methods, Evidence, and Impact, McMaster University) for reviewing our manuscript. This analysis was conducted at the Statistics Canada Research Data Centre at McMaster University, which is part of the Canadian Research Data Centre Network. The services and activities provided by the Statistics Canada Research Data Centre at McMaster University are made possible by the financial or in-kind support of the Social Sciences and Humanities Research Council, the Canadian Institutes of Health Research, Statistics Canada and McMaster University.
Footnotes
Competing interests: None declared.
This article has been peer reviewed.
Contributors: Each author contributed substantially to the conception and design of the article. Harman Sandhu analyzed the data and drafted the initial manuscript. Each author revised the manuscript critically for important intellectual content, gave final approval of the version to be published and agreed to be accountable for all aspects of the work.
Data sharing: The 2018 National Cannabis Survey master file can be accessed through a Research Data Centre. The analysis code can be accessed by contacting the corresponding author.
Supplemental information: For reviewer comments and the original submission of this manuscript, please see www.cmajopen.ca/content/7/2/E399/suppl/DC1.
References
- 1.Canadian Tobacco, Alcohol and Drugs Survey, 2017. Ottawa: Statistics Canada; 2018. [accessed 2019 Jan 29]. Available: www150.statcan.gc.ca/n1/daily-quotidien/181030/dq181030b-eng.htm. [Google Scholar]
- 2.Asbridge M, Hayden JA, Cartwright JL. Acute cannabis consumption and motor vehicle collision risk: systematic review of observational studies and meta-analysis. BMJ. 2012;344:e536. doi: 10.1136/bmj.e536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gunn JKL, Rosales CB, Center KE, et al. Prenatal exposure to cannabis and maternal and child health outcomes: a systematic review and meta-analysis. BMJ Open. 2016;6:e009986. doi: 10.1136/bmjopen-2015-009986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gurney J, Shaw C, Stanley J, et al. Cannabis exposure and risk of testicular cancer: a systematic review and meta-analysis. BMC Cancer. 2015;15:897. doi: 10.1186/s12885-015-1905-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Moore BA, Augustson EM, Moser RP, et al. Respiratory effects of marijuana and tobacco use in a U.S. sample. J Gen Intern Med. 2005;20:33–7. doi: 10.1111/j.1525-1497.2004.40081.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pearson C, Janz T, Ali J. Mental and substance use disorders in Canada. Ottawa: Statistics Canada; [accessed 2019 Jan 9]. modified 2015 Nov 27. Cat no 82-624-X. Available: www150.statcan.gc.ca/n1/pub/82-624-x/2013001/article/11855-eng.htm. [Google Scholar]
- 7.ElSohly MA, Mehmedic Z, Foster S, et al. Changes in cannabis potency over the last 2 decades (1995–2014): analysis of current data in the United States. Biol Psychiatry. 2016;79:613–9. doi: 10.1016/j.biopsych.2016.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Volkow ND, Baler RD, Compton WM, et al. Adverse health effects of marijuana use. N Engl J Med. 2014;370:2219–27. doi: 10.1056/NEJMra1402309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Di Forti M, Sallis H, Allegri F, et al. Daily use, especially of high-potency cannabis, drives the earlier onset of psychosis in cannabis users. Schizophr Bull. 2014;40:1509–17. doi: 10.1093/schbul/sbt181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Drug Abuse Warning Network 2011: national estimates of drug-related emergency department visits. Rockville (MD): Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration; 2013. (DAWN Series D-39). HHS Publication no (SMA) 13-4760. [PubMed] [Google Scholar]
- 11.Hall W. What has research over the past two decades revealed about the adverse health effects of recreational cannabis use? Addiction. 2015;110:19–35. doi: 10.1111/add.12703. [DOI] [PubMed] [Google Scholar]
- 12.Memedovich KA, Dowsett LE, Spackman E, et al. The adverse health effects and harms related to marijuana use: an overview review. CMAJ Open. 2018;6:E339–46. doi: 10.9778/cmajo.20180023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.An Act respecting cannabis and to amend the Controlled Drugs and Substances Act, the Criminal Code and other Acts. 42nd Parliament, 1st sess, 2018 June 21. [accessed 2019 Jan 9]. Available: www.parl.ca/DocumentViewer/en/42-1/bill/C-45/royal-assent.
- 14.Fischer B, Kuganesan S, Room R. Medical marijuana programs: implications for cannabis control policy — observations from Canada. Int J Drug Policy. 2015;26:15–9. doi: 10.1016/j.drugpo.2014.09.007. [DOI] [PubMed] [Google Scholar]
- 15.Cerdá M, Wall M, Feng T, et al. Association of state recreational marijuana laws with adolescent marijuana use. JAMA Pediatr. 2017;171:142–9. doi: 10.1001/jamapediatrics.2016.3624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kerr DCR, Bae H, Koval AL. Oregon recreational marijuana legalization: changes in undergraduates’ marijuana use rates from 2008 to 2016. Psychol Addict Behav. 2018;32:670–8. doi: 10.1037/adb0000385. [DOI] [PubMed] [Google Scholar]
- 17.Ghosh TS, Vigil DI, Maffey A, et al. Lessons learned after three years of legalized, recreational marijuana: the Colorado experience. Prev Med. 2017;104:4–6. doi: 10.1016/j.ypmed.2017.02.021. [DOI] [PubMed] [Google Scholar]
- 18.Estoup AC, Moise-Campbell C, Varma M, et al. The impact of marijuana legalization on adolescent use, consequences, and perceived risk. Subst Use Misuse. 2016;51:1881–7. doi: 10.1080/10826084.2016.1200623. [DOI] [PubMed] [Google Scholar]
- 19.Fischer B, Russell C, Rehm J, et al. Assessing the public health impact of cannabis legalization in Canada: core outcome indicators towards an ‘index’ for monitoring and evaluation. J Public Health (Oxf) 2018 May 30; doi: 10.1093/pubmed/fdy090. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.National Cannabis Survey (NCS) Ottawa: Statistics Canada; [accessed 2019 Jan 9]. modified 2019 May 14. Available: www23.statcan.gc.ca/imdb/p2SV.pl?Function=getSurvey&SDDS=5262. [Google Scholar]
- 21.von Elm E, Altman DG, Egger M, et al. STROBE Initiative. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. PLoS Med. 2007;4:e296. doi: 10.1371/journal.pmed.0040296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.National Cannabis Survey [questionnaire] Ottawa: Statistics Canada; [accessed 2019 Jan 9]. modified 2018 Oct. 25 Available: www23.statcan.gc.ca/imdb/p3Instr.pl?Function=assembleInstr&lang=en&Item_Id=1173861. [Google Scholar]
- 23.The Research Data Centres (RDC) program. Ottawa: Statistics Canada; [accessed 2019 Jan 9]. modified 2018 Dec 27. Available: www.statcan.gc.ca/eng/rdc/index. [Google Scholar]
- 24.How to integrate sex and gender into research. Ottawa: Canadian Institutes of Health Research; 2019. [accessed 2019 Jan 9]. Available: www.cihr-irsc.gc.ca/e/50836.html. [Google Scholar]
- 25.Norton EC, Miller MM, Kleinman LC. Computing adjusted risk ratios and risk differences in Stata. Stata J. 2013;13:492–509. doi: 10.1177/1536867X1301300304. [DOI] [Google Scholar]
- 26.Peduzzi P, Concato J, Kemper E, et al. A simulation study of the number of events per variable in logistic regression analysis. J Clin Epidemiol. 1996;49:1373–9. doi: 10.1016/s0895-4356(96)00236-3. [DOI] [PubMed] [Google Scholar]
- 27.Gagné C, Roberts G, Keown LA. Weighted estimation and bootstrap variance estimation for analyzing survey data: How to implement in selected software. Ottawa: Statistics Canada; 2014. Can no 12-002-X — no. 2014001. [Google Scholar]
- 28.Hosmer DW, Lemeshow S. Goodness of fit tests for the multiple logistic regression model. Commun Stat Theory Methods. 1980;9:1043–69. doi: 10.1080/03610928008827941. [DOI] [Google Scholar]
- 29.Canadian Institutes of Health Research; Natural Sciences and Engineering Research Council of Canada; Social Sciences and Humanities Research Council of Canada. Tri-Council policy statement: ethical conduct for research involving humans. Secretariat on Responsible Conduct of Research; 2014. pp. 1–10. [Google Scholar]
- 30.Hansen L. Cannabis edibles, drinks will mark “2nd wave” of legalization. CBC News. 2018. Nov 12, [accessed 2019 Jan 9]. Available: www.cbc.ca/news/canada/ottawa/cannabis-legalization-second-wave-edibles-1.4901297.
- 31.Charlebois S, Somogyi S. Marijuana-infused food and Canadian consumers’ willingness to consider recreational marijuana as a food ingredient. Halifax: Dalhousie University; 2017. [accessed 2019 Jan 9]. Available: https://cdn.dal.ca/content/dam/dalhousie/pdf/management/News/Preliminaryresultscannibis-infusedfoodsEN.pdf. [Google Scholar]
- 32.A society in transition, an industry ready to bloom: 2018 cannabis report. Toronto: Deloitte; 2018. [accessed 2019 Jan 9]. Available: www2.deloitte.com/content/dam/Deloitte/ca/Documents/consulting/ca-cannabis-2018-report-en.PDF. [Google Scholar]
- 33.Cohn AM, Johnson AL, Rose SW, et al. Support for marijuana legalization and predictors of intentions to use marijuana more often in response to;egalization among U.S. young adults. Subst Use Misuse. 2017;52:203–13. doi: 10.1080/10826084.2016.1223688. [DOI] [PubMed] [Google Scholar]
- 34.Morell-Gomis R, Moriano JA, Laguía A, et al. Adolescents cannabis use intention: validating a theory of planned behavior questionnaire in four European countries. J Subst Use. 2019;24:66–72. doi: 10.1080/14659891.2018.1510050. [DOI] [Google Scholar]
- 35.Ritter C. Resources, behavior intentions, and drug use: a ten-year national panel analysis. Soc Psychol Q. 1988;51:250–64. doi: 10.2307/2786923. [DOI] [Google Scholar]
- 36.Ito TA, Henry EA, Cordova KA, et al. Testing an expanded theory of planned behavior model to explain marijuana use among emerging adults in a promarijuana community. Psychol Addict Behav. 2015;29:576–89. doi: 10.1037/adb0000098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Conner M, McMillan B. Interaction effects in the theory of planned behaviour: studying cannabis use. Br J Soc Psychol. 1999;38:195–222. doi: 10.1348/014466699164121. [DOI] [PubMed] [Google Scholar]
- 38.Sniehotta FF, Scholz U, Schwarzer R. Bridging the intention-behaviour gap: planning, self-efficacy, and action control in the adoption and maintenance of physical exercise. Psychol Health. 2005;20:143–60. doi: 10.1080/08870440512331317670. [DOI] [Google Scholar]
- 39.Walsh Z, Gonzales R, Crosby K, et al. Medical cannabis and mental health: a systematic review. Clin Psychol Rev. 2017;51:15–29. doi: 10.1016/j.cpr.2016.10.002. [DOI] [PubMed] [Google Scholar]
- 40.Ogborne AC, Smart RG, Weber T, et al. Who is using cannabis as a medicine and why: an exploratory study. J Psychoactive Drugs. 2000;32:435–43. doi: 10.1080/02791072.2000.10400245. [DOI] [PubMed] [Google Scholar]
- 41.Walsh Z, Callaway R, Belle-Isle L, et al. Cannabis for therapeutic purposes: patient characteristics, access, and reasons for use. Int J Drug Policy. 2013;24:511–6. doi: 10.1016/j.drugpo.2013.08.010. [DOI] [PubMed] [Google Scholar]
- 42.National Academies of Sciences, Engineering, and Medicine. The health effects of cannabis and cannabinoids: the current state of evidence and recommendations for research. Washington (DC): National Academies Press; 2017. [accessed 2019 May 2]. Available: www.nap.edu/catalog/24625. [PubMed] [Google Scholar]
- 43.O’Neil ME, Nugent SM, Morasco BJ, et al. Benefits and harms of plant-based cannabis for posttraumatic stress disorder: a systematic review. Ann Intern Med. 2017;167:332–40. doi: 10.7326/M17-0477. [DOI] [PubMed] [Google Scholar]
- 44.Hoch E, Niemann D, von Keller R, et al. How effective and safe is medical cannabis as a treatment of mental disorders? A systematic review. Eur Arch Psychiatry Clin Neurosci. 2019;269:87–105. doi: 10.1007/s00406-019-00984-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Turna J, Patterson B, Van Ameringen M. Is cannabis treatment for anxiety, mood, and related disorders ready for prime time? Depress Anxiety. 2017;34:1006–17. doi: 10.1002/da.22664. [DOI] [PubMed] [Google Scholar]
- 46.Keyhani S, Steigerwald S, Ishida J, et al. Risks and benefits of marijuana use a national survey of U.S. adults. Ann Intern Med. 2018;169:282–90. doi: 10.7326/M18-0810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Porath-Waller AJ, Brown JE, Frigon AP, et al. What Canadian youth think about cannabis [technical report] Ottawa: Canadian Centre on Substance Abuse; 2013. [accessed 2019 Jan 9]. pp. 1–57. Available: www.ccsa.ca/sites/default/files/2019-05/CCSA-What-Canadian-Youth-Think-about-Cannabis-2013-en.pdf. [Google Scholar]
- 48.Tibbo P, Cracker CE, Lam RW, et al. Implications of cannabis legalization on youth and young adults. Can J Psychiatry. 2018;63:65–71. doi: 10.1177/0706743718759031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Bill C-45: The Cannabis Act [policy] Ottawa: Canadian Medical Association; 2018. [accessed 2019 Jan 9]. Available: https://policybase.cma.ca/en/permalink/policy13861. [Google Scholar]
- 50.National Cannabis Survey, fourth quarter 2018. Ottawa: Statistics Canada; [accessed 2019 Feb 21]. modified 2019 Feb 7. Available: www150.statcan.gc.ca/n1/daily-quotidien/190207/dq190207b-eng.htm?HPA=1. [Google Scholar]
- 51.National Cannabis Survey, first quarter 2019. Ottawa: Statistics Canada; [accessed 2019 May 19]. modified 2019 May 2. Available: www150.statcan.gc.ca/n1/daily-quotidien/190502/dq190502a-eng.htm. [Google Scholar]
- 52.Hall W, Pacula RL. Cannabis use and dependence: public health and public policy. Cambridge (UK): Cambridge University Press; 2003. pp. 1–298. [Google Scholar]
- 53.O’Malley PM, Bachman JG, Johnston LD. Reliability and consistency in self-reports of drug use. Int J Addict. 1983;18:805–24. doi: 10.3109/10826088309033049. [DOI] [PubMed] [Google Scholar]
- 54.Harrison ER, Haaga J, Richards T. Self-reported drug use data: What do they reveal? Am J Drug Alcohol Abuse. 1993;19:423–41. doi: 10.3109/00952999309001632. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.