Abstract
Low-level transcutaneous vagus nerve stimulation at the tragus (LLTS) is anti-adrenergic. We aimed to evaluate the acute effects of LLTS on left ventricular (LV) function and autonomic tone. Patients with diastolic dysfunction and preserved LV ejection fraction were enrolled in a prospective, randomized, double-blind, 2×2 cross-over study. Patients received 2 separate, 1hour sessions, at least 1 day apart, of active LLTS (20Hz, 1mA below the discomfort threshold) and sham stimulation. Echocardiography was performed after LLTS or sham stimulation to assess cardiac function. A 5-minute ECG was performed to assess heart rate variability (HRV). Twenty-four patients were enrolled. LV global longitudinal strain improved by 1.8±0.9% during active LLTS compared to sham stimulation (p=0.001). Relative to baseline, HRV frequency domain components (low frequency, high frequency and their ratio) were favorably altered after LLTS compared to sham stimulation (all p<0.05). We concluded that LLTS acutely ameliorates cardiac mechanics by modulating the autonomic tone.
Keywords: neuromodulation, transcutaneous vagus nerve stimulation, heart rate variability, diastolic dysfunction, left ventricular strain imaging
Introduction
Heart failure with preserved ejection fraction (HFpEF) has become a major public health concern. Epidemiological studies have shown that the prevalence and hospitalizations related to HFpEF are increasing [1, 2], and the growing elderly population is expected to further worsen these trends. Despite normal or near-normal left ventricular (LV) ejection fraction, the rates of morbidity and mortality among these patients are high and similar to those of patients with heart failure with reduced ejection fraction (HFrEF) [3, 4]. Unfortunately, no pharmacologic therapy has been shown to improve morbidity and mortality in patients with HFpEF [5]. Incomplete understanding of HFpEF pathophysiology and patient heterogeneity may account for the negative results of trials of pharmacologic therapy in HFpEF [6]. Recent animal and human studies suggest that a systemic pro-inflammatory state, produced by comorbidities, including aging, plays a central role in the development of HFpEF [7–9]. Importantly, patients with HFpEF have impaired LV function, as assessed by LV strain [10]. In addition, patients with HFpEF have marked autonomic dysfunction, characterized by increased activity of the sympathetic nervous system and decreased activity of the parasympathetic nervous system [11, 12]. Therefore, inflammation and/or autonomic dysfunction may be important targets for the treatment of HFpEF.
Vagus nerve stimulation (VNS) exerts prominent anti-adrenergic and anti-inflammatory effects [13–15] and can be accomplished transcutaneously by stimulating the auricular branch of the vagus nerve [16]. Using this approach, we and others, have shown that low-level transcutaneous VNS (LLTS), at levels not causing bradycardia, can restore autonomic imbalance and reduce inflammatory cytokine levels in patients with atrial fibrillation [17], myocardial infarction undergoing primary coronary intervention [18] and healthy volunteers [19]. In this study, we hypothesized that short-term LLTS may ameliorate cardiac mechanics and improve autonomic balance in patients with diastolic dysfunction and preserved LV ejection fraction. Notably, diastolic dysfunction is a dominant feature in the majority of patients with HFpEF and it has been argued that future trials should require echocardiographic evidence of diastolic dysfunction [6].
Methods
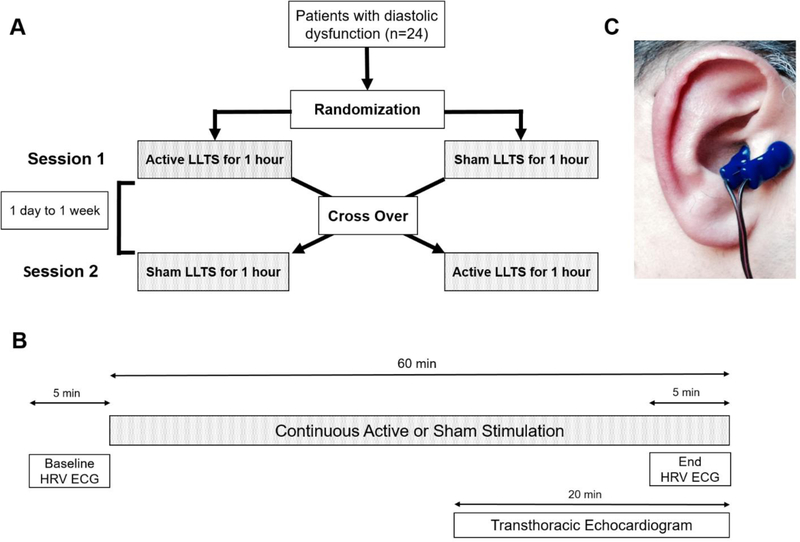
This was a prospective, randomized, double-blind, 2×2 cross over study. Patients diagnosed with diastolic dysfunction by echocardiogram, according to current guidelines [20] within 24 months of study enrollment were eligible for enrollment in the study. In addition, patients were required to be in sinus rhythm at the time of the study. Patients were excluded if they had any of the following: LV dysfunction (LV ejection fraction <40%), significant valvular disease (i.e., prosthetic valve or hemodynamically significant valvular diseases), recent (<6 months) myocardial infarction, severe heart failure (class IV), recurrent vasovagal syncope, unilateral or bilateral vagotomy, sick sinus syndrome (without a pacemaker), 2nd or 3rd degree AV block, bifascicular block or prolonged PR (>300ms) and pregnancy or nursing. All patients received 2 separate, 1-hour sessions, at least 1 day and up to 1 week apart, of active and sham LLTS, with the sequence of the sessions being randomized (Figure 1A). Stimulation was provided using a transcutaneous electrical nerve stimulation (TENS) unit, attached to an ear clip electrode (Parasym device, Parasym Health, Inc., London, UK). In the active group, the ear clip electrode was attached to tragus of the ear (Figure 1B), whereas in the sham group the electrode was placed on the ear lobe, which is devoid of vagal innervation [21]. The TENS unit was set at a pulse width of 200 μs and a pulse frequency of 20 Hz. The stimulation amplitude was individualized to 1mA below the discomfort threshold. The titration to the final stimulation amplitude occurred over 10 to 20 seconds and no appreciable effects on the heart rate were observed during this period. The patients were not aware which location corresponds to the active vs. sham treatment. The investigators assessing the outcomes were blinded to treatment assignment. The study was approved by the Institutional Review Board of the University of Oklahoma Health Sciences Center and all patients provided informed consent prior to enrollment in the study. The study design and timeline of events is summarized in Figure 1C.
Figure 1.
Schematic representation of the study design and timeline of events (A, B). Active low-level transcutaneous vagus nerve stimulation (LLTS) was accomplished by attaching an electrode clip at the tragus of the right ear (C).
Echocardiography
Echocardiography (Acuson SC2000, Siemens) was performed after 40 minutes of active or sham stimulation to assess LV function by a board-certified echocardiographer, who remained blinded to treatment assignment (Figure 1A). Two-dimensional parasternal long-axis, right ventricular inflow, parasternal short-axis, and apical four (A4C), three (A3C) and two chamber (A2C) views were obtained. Wall thickness and chamber dimensions, were measured in the parasternal long axis view. LV ejection fraction was calculated from A4C and A2C views using the Simpson’s method. Based on the 2016 update to the guidelines for assessment of left ventricular diastolic function, we obtained peak tricuspid regurgitant velocity, left atrial end-systolic volume index, mitral annular tissue Doppler velocities (e’) and average E/e’ ratio [20]. Tricuspid regurgitant velocity was assessed in the right ventricular inflow and right ventricular-focused A4C views and the overall peak tricuspid regurgitant velocity was reported. Left atrial end-systolic volume index was determined from atrially-focused A4C and A2C views. Pulse-wave Doppler was used to measure mitral inflow velocities (E and A waves) in the A4C view and the E/A ratio was calculated. Mitral annulus septal and lateral tissue Doppler velocities (e’) were measured in the A4C view, as previously described [20] and the E/e’ ratio was calculated. LV global longitudinal strain (GLS), a sensitive and specific marker of early impairment in LV long-axis function in HFpEF [10], was measured through analysis of A4C, A3C, and A2C views using the Siemens speckle-tracking algorithm (Acuson SC2000 eSie VVI ™). LV global circumferential strain was measured through analysis of the parasternal short-axis view at the mid-papillary level, using the same speckle-tracking algorithm. All echocardiographic measurements were obtained offline and the investigators performing the off-line analysis were blinded to treatment assignment.
Heart rate variability
At each visit, a 12-lead ECG was continuously monitored throughout the study. In addition, serial 5-minute ECGs at a sampling rate of 1,000 Hz were obtained for HRV analysis at baseline and after 1 hour of stimulation, using a PC-based ECG machine (Figure 1A). ECG was obtained in the supine position after resting for 15 minutes. Patients were instructed to abstain from coffee, smoking and exercise for at least 6 hours. Analysis and interpretation of the HRV data was performed in a blinded fashion using the Kubios software [22]. The following HRV parameters were obtained by time domain analysis: 1. SDNN [standard deviation of adjacent normal-to-normal (NN) intervals], 2. RMSSD (square root of the mean of the sum of the squares of difference between adjacent NN intervals) and 3. pNN50 (number of pairs of adjacent NN intervals differing by more than 50 ms), and by frequency domain analysis: 1. Low frequency (LF) power, 2. high frequency (HF) power and 3. the LF/HF ratio [23]. The autoregressive method, which is the preferred method for HF band calculation [24], was used for frequency domain analysis. According to current recommendations, both short (5 minutes) and long (24 hours) duration ECG recordings are acceptable options for measuring HRV; however, frequency domain analysis measures perform better than time domain measures when short duration recordings are examined [23]. Notably, the HF power overall reflects parasympathetic activity and the LF power is considered a measure of sympathetic activity, while the LF/HF ratio reflects sympathetic to parasympathetic balance [25].
Statistical analysis
Continuous variables are expressed as mean ± standard deviation. Logarithmic transformation was performed when applicable to achieve normality. Categorical variables are expressed as percentages. Echocardiographic and HRV parameters were compared between active and sham stimulation using a mixed linear model. Significant interactions were followed by time-stratified analyses to investigate group effects. For all pair-wise testing, we adjusted for multiple comparisons using Tukey’s method. Linear regression models were computed to assess the relationship between the change in GLS during active vs. sham stimulation and the GLS during sham stimulation, as well as the change in HRV parameters during active vs. sham stimulation. Statistical significance was declared at p<0.05.
The study was powered to detect a 20% relative change in GLS with LLTS, assuming a baseline GLS of −17.1±2.0% during sham stimulation, as seen in patients with hypertension without HFpEF [10]. Under these assumptions, 24 patients would provide at least 90% power to detect this difference in a 2×2 cross over design. Based on the observed baseline GLS of −21.2±3.0% during sham stimulation, a sample size of 24 patients provided 80% power to detect a difference of 1.8% between active and sham stimulation sequences.
Results
Thirty-five patients were screened for eligibility and eventually 24 patients were included in the study. The baseline characteristics of the patients included in the study are shown in Table 1. In summary, the majority of the patients (83%) were hypertensive, 42% were diabetic, 50% were obese (body mass index > 30kg/m2) and 46% had a diagnosis of paroxysmal atrial fibrillation. Notably, half of the patients had grade II or greater diastolic dysfunction and 38% had heart failure.
Table 1.
Baseline characteristics of the patients included in the study
| Variable | |
|---|---|
| Age (years) | 68.3±11.2 |
| Male gender, n (%) | 13 (54) |
| Race | |
| African American, n (%) | 2 (8) |
| Body mass index (kg/m2) | 31.6±6.3 |
| Diabetes, n (%) | 10 (42) |
| Hypertension, n (%) | 20 (83) |
| Sleep apnea, n (%) | 3 (13) |
| Obesity (body mass index > 30kg/m2), n (%) | 12 (50) |
| Paroxysmal atrial fibrillation, n (%) | 11 (46) |
| Hyperlipidemia, n (%) | 9 (38) |
| Coronary artery disease, n (%) | 3 (13) |
| Chronic kidney disease, n (%) | 1 (4) |
| Heart failure, n (%) | 9 (38) |
| III, n (%) | 1 (11) |
| Grade III, n (%) | 2 (8) |
| Statins, n (%) | 9 (38) |
| Systolic blood pressure (mmHg)* | 130.2±23.9 |
| Diastolic blood pressure (mmHg)* | 77.4±13.4 |
| Heart rate (bpm)* | 73.1±18.1 |
average of 2 visits
ACE = angiotensin converting enzyme
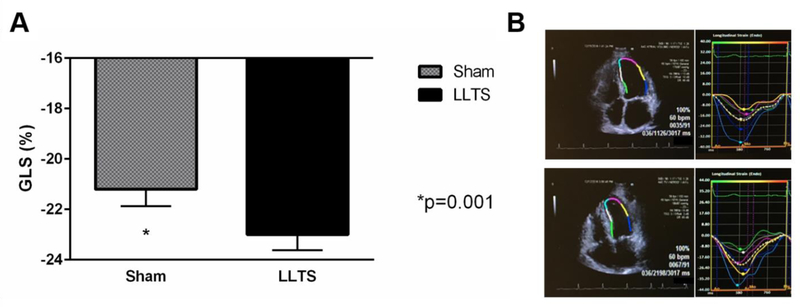
The average stimulation amplitude was 22.6 ± 5.8 mA and 21.8 ± 5.6 mA during sham and active LLTS, respectively (p=0.85). No change was seen in average heart rate during stimulation. When comparing heart rate during vs. post stimulation at baseline, no significant changes were observed in either sham or active stimulation (sham: 72.5±16.2 bpm vs. 72.5±13.8 bpm; p=0.91 and active: 70.1±12.3 bpm vs. 69.3±11.4 bpm; p=0.63). Likewise, QT remained stable over the same period of time, during both sham and active stimulation (sham: 400.9±29.4 ms vs. 399.1±29.1 ms; p=0.83 and active 417.5±26.1 ms vs. 421.5±28.7 ms; p=0.32). None of the patients reported any discomfort during stimulation and no adverse effects occurred during the stimulation period, or within a week after each session. GLS improved by 1.8 ± 0.9% during active LLTS compared to sham stimulation (−23.0±2.8% vs. −21.2±3.0%, respectively, p=0.001; Figure 2). Importantly, this improvement in GLS with active stimulation is similar in magnitude to the difference between patients with HFpEF compared to those with hypertensive heart disease [10, 26]. None of the other echocardiographic parameters differed significantly between active and sham LLTS (Table 2).
Figure 2.
Comparison of the effect of LLTS on global longitudinal strain (GLS) during active vs. sham stimulation. A. Active LLTS resulted in a significant improvement in GLS (p=0.001) compared to sham stimulation. B. Representative example of left ventricular strain analysis (apical 4-chamber view) showing the effect of LLTS (lower panel) compared to sham (upper panel) on the same patient. There was a decrease in GLS from −19.3% to −23.1%, which represents a favorable change.
Table 2.
Echocardiographic parameters
| Variable | Sham | LLTS | P value |
|---|---|---|---|
| Global longitudinal strain (%) | −21.2±3.0 | −23.0±2.8 | 0.001 |
| Global circumferential strain (%) | −31.3±5.6 | −30.9±5.7 | 0.82 |
| LV ejection fraction (%) | 66.9±5.7 | 65.46±5.08 | 0.35 |
| LV diameter (cm) | 4.5±0.6 | 4.51±0.52 | 0.91 |
| LV septum diameter (cm) | 1.2±0.3 | 1.2±0.4 | 0.80 |
| LV posterior wall diameter (cm) | l.l±0.2 | l.l±0.2 | 0.91 |
| E velocity (cm/s) | 74.1±19.0 | 75.2±20.0 | 0.52 |
| A velocity (m/s) | 79.3±18.1 | 81.0±22.1 | 0.74 |
| E/A ratio | 0.95±0.43 | 0.97±0.37 | 0.75 |
| Average e’ velocity (cm/s) | 7.9±2.0 | 8.5±2.0 | 0.56 |
| Average E/e’ ratio | 9.6±4.2 | 9.3±2.9 | 0.78 |
| Peak TR velocity (m/s) | 2.6±1.5 | 2.5±1.4 | 0.66 |
| LA diameter (cm) | 5.6±0.9 | 5.7±1.1 | 0.57 |
| LA volume index (ml/m2) | 28.6±10.4 | 31.2±12.9 | 0.29 |
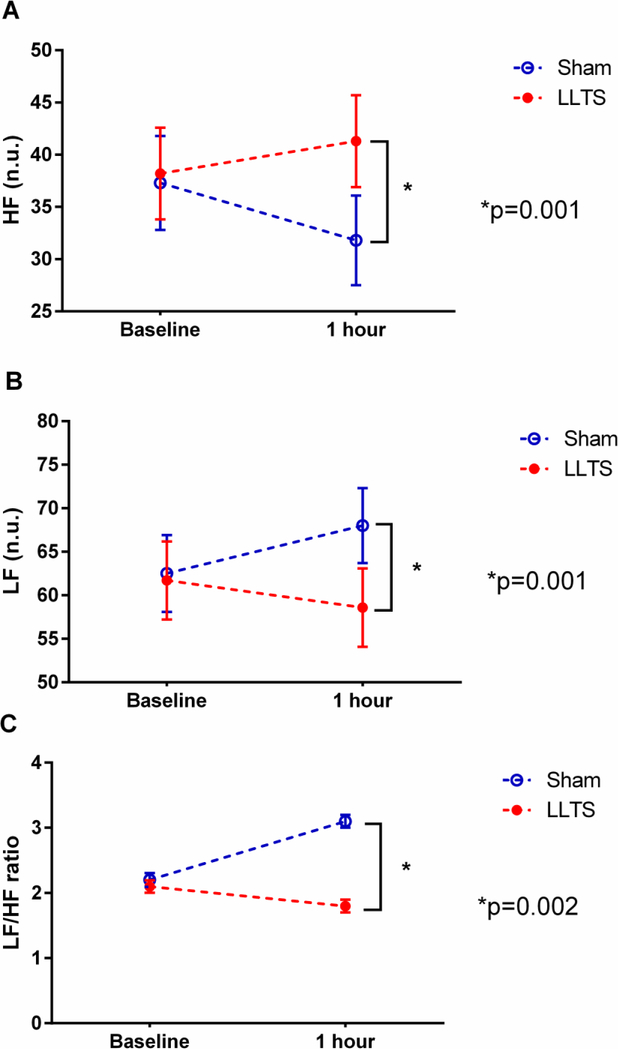
The results of the HRV analysis are summarized in Table 3. There was a significant time by treatment period interaction (p<0.001) for all 3 frequency domain HRV variables examined, indicating that these parameters changed differently over time between the 2 treatment periods (active vs. sham LLTS). The difference between sham stimulation and LLTS at the end of the respective treatment period in all the 3 frequency domain HRV parameters examined was statistically significant. Specifically, HF was significantly higher after 1 hour of active LLTS compared to sham stimulation (p=0.001; Figure 3A). Likewise, LF was significantly lower after 1 hour of active LLTS compared to sham stimulation (p=0.001; Figure 3B). Finally, the LF/HF ratio, which reflects sympathovagal balance [25], was favorably altered during LLTS compared to sham stimulation (p=0.002; Figure 3C). None of the time domain parameters differed significantly between active and sham LLTS.
Table 3.
Heart rate variability analysis
| Variable | Sham | LLTS | P value* | ||
|---|---|---|---|---|---|
| baseline | 1 hour | baseline | 1 hour | ||
| pNN50 (%) | 1.8±0.5 | 1.8±0.4 | 1.6±0.4 | 1.2±0.4 | 0.29 |
| LF/HF | 2.2±0.4 | 3.1±0.4 | 2.1±0.4 | 1.8±0.4 | 0.002 |
comparison between Sham and LLTS at 1 hour
log transformed values to achieve normality
n.u. = normalized units
Figure 3.
Effect of active vs sham LLTS on measures of heart rate variability. A. Low frequency (LF). B. High frequency (HF). C. Ratio of LF to HF (LF/HF ratio). All 3 parameters were favorably altered after 1 hour of active LLTS compared to sham stimulation.
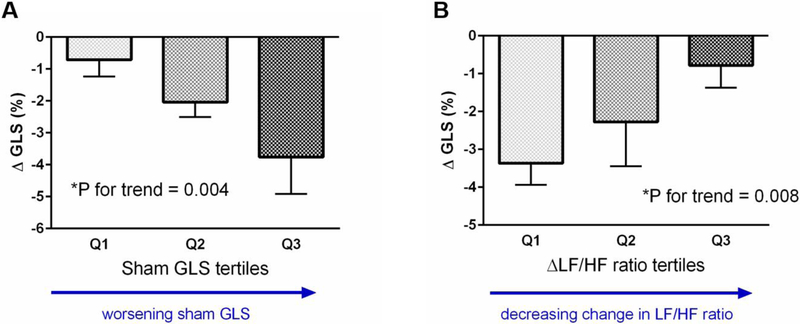
To understand the relationship of the improvement in GLS during active LLTS with baseline LV strain, we modeled the change in GLS during active vs. sham LLTS as a function of baseline GLS (sham stimulation). Worse GLS during sham stimulation, reflecting more advanced stage of LV longitudinal dysfunction, was associated with a larger improvement in GLS during active LLTS (p = 0.004; Figure 4A). These findings suggest that patients with worse GLS, at levels comparable to those seen in patients with HFpEF [10], would derive more benefit from LLTS. To correlate the change in strain with the change in autonomic function, we modeled the difference in GLS during active vs. sham stimulation as a function of the difference in the LF/HF ratio during active vs. sham stimulation. A larger change in LF/HF ratio during active vs. sham stimulation was correlated positively with a larger improvement in GLS during active vs. sham stimulation (p = 0.008; Figure 4B). These data suggest that improvement in autonomic function during active stimulation was associated with improvement in cardiac mechanics.
Figure 4.
Association of the difference in global longitudinal strain between active and sham stimulation (ΔGLS) with GLS during sham stimulation (tertiles) (A) and the difference in low frequency to high frequency ratio between active and sham stimulation ((ΔLF/HF; tertiles) (B).
Discussion
In this study, transcutaneous stimulation of the auricular branch of the right vagus nerve at the tragus for one hour resulted in an acute improvement in LV longitudinal mechanics in patients with diastolic dysfunction and preserved LV ejection fraction. This improvement was associated with a favorable change in sympathovagal balance. Importantly, the improvement in LV strain was greater in those who had lower baseline GLS (Figure 4A), suggesting that patients with worse longitudinal cardiac function, such as those with HFpEF [10], would derive even more benefit from this treatment modality. This proof-of-concept, first-in-human study suggests that non-invasive neuromodulation using LLTS may be useful in the treatment of HFpEF. These results are significant in light of the increasing number of patients with HFpEF [1, 2] and the failure of pharmacological therapies to improve clinical outcomes in this condition [5]. Although our study targeted patients with diastolic dysfunction rather than HFpEF, it has to be acknowledged that diastolic dysfunction is a dominant feature in the majority of patients with HFpEF [6]. This favorable effect in cardiac mechanics is possibly related to improvement in autonomic function. As shown in Figure 4B, the improvement in cardiac mechanics was proportionate to the improvement in autonomic function. The tragus of the ear is innervated by a purely sensory (afferent) nerve, the auricular branch of the vagus nerve [27]. Importantly, afferent vagal stimulation inhibits sympathetic activity [28]. In addition, functional magnetic resonance imaging studies indicated that stimulation of the auricular branch of the vagus nerve leads to activation of the ipsilateral nucleus tractus solitarius, which is the first central relay of vagal afferents, resulting in stimulation of higher order vagal projections in the brainstem and forebrain [29]. HFpEF, as well as its risk factors, including hypertension, diabetes and obesity, is associated with hyperactivity of the sympathetic nervous system and impaired autonomic reflexes [30, 31], which in turn lead to cardiac dysfunction [10]. In light of evidence suggesting that acute (within minutes) resensitization of adrenergic receptors occurs upon removal of the increased sympathetic stimulation [32], we hypothesize that LLTS-mediated, afferent vagal activation, which results in reflex inhibition of central sympathetic output, leads to acute resensitization of cardiac adrenergic receptors, which in turn manifests as improvement in cardiac mechanics. It has been recently shown that subthreshold VNS (not causing bradycardia) exerts a modest positive effect on both cardiac inotropy and lusitropy at low stimulation intensities, comparable to those used in our study [33]. Nonetheless, the exact mechanisms and the downstream mediators of this effect remain to be determined.
In this study, we added LV strain imaging to traditional echocardiographic parameters of LV function, as it has been shown to be a powerful predictor of clinical outcomes in patients with HFpEF [34]. In addition, GLS and its deterioration were associated with major adverse cardiac events in a population comparable to our study, such as asymptomatic patients with hypertensive heart disease, independent of the presence of traditional clinical parameters or LV hypertrophy [35]. Subendocardial myocardial fibers are oriented longitudinally and contribute primarily to longitudinal myocardial mechanics [36]. These fibers are also the most susceptible to ischemia and hypoperfusion. GLS is therefore ideal to screen for subclinical myocardial disease in diverse populations, including those with hypertensive heart disease, diabetes and obesity [34]. Identification of LV dysfunction before the onset of disease in at-risk populations, including those with hypertensive heart disease, diabetes and obesity, would allow implementation of therapies to halt the progression of disease. In our study, GLS was the only echocardiographic parameter which was significantly different when LLTS was applied compared to sham stimulation. Notably, acute changes in LV strain, but not other echocardiographic parameters, have been demonstrated after excessive alcohol ingestion [37] and during hypoxic breathing [38].
Autonomic imbalance, characterized by increased sympathetic nerve activity, is significantly associated with and may contribute to the development of diastolic dysfunction in humans [11, 30]. Importantly, VNS, even at subthreshold levels not causing bradycardia, exhibits antiadrenergic properties, by injuring the sympathetic neurons in the stellate ganglia [39, 40]. In addition, VNS attenuated cardiac remodeling and suppressed sympathoexcitation in a guinea-pig model of pressure overload [15]. In this study, we have shown that 1 hour of LLTS ameliorates cardiac mechanics and favorably alters the sympathovagal balance, by enhancing parasympathetic tone and decreasing sympathetic tone. These results are consistent with a previous study, in which LLTS delivered for 15 minutes improved autonomic balance in healthy volunteers [19]. In the same study, there was an inverse relationship between baseline autonomic dysfunction (assessed by the LF/HF ratio) and the effect of LLTS (assessed by the change in LLTS ratio), indicating that worse higher LF/HF ratios predict a greater decrease in LF/HF during LLTS, similar to our findings (Figure 4B). Notably, a significant association between cardiac function, as assessed by GLS, and autonomic function, as assessed by HRV parameters, has been previously shown in patients with hypertension [41] and scleroderma [42]. Frequency domain, but not time domain parameters changed significantly with LLTS. This is somewhat expected as we only used 5 min ECG recordings, given that time domain analysis has higher variability with shorter (5 min) durations and frequency domain analysis measures perform better than time domain measures when short duration recordings are examined [23].
Our results should be examined in the context of the recent trials of VNS for systolic heart failure [43–45]. Two of the studies (INNOVATE-HF [43] and NECTAR-HF [44]) failed to meet their clinical endpoints, whereas ANTHEM-HF [45] demonstrated efficacy. Notably, the 3 studies differed significantly in terms of stimulation protocols. Mechanistic studies have suggested that the optimal stimulation parameters for VNS are at the point at which afferent and efferent fibers are activated in a balanced manner (“neural fulcrum”). At the neural fulcrum, VNS results in a neutral heart rate response, because the afferent-driven decreases in central parasympathetic drive are counteracted by direct activation of the cardiac parasympathetic efferent projections to the intrinsic cardiac autonomic nervous system and the heart [33, 46]. Extrapolating the canine data to humans, Ardell et al. [46] indicated that the stimulation parameters of ANTHEM-HF were very close to the target therapeutic zone for optimal effects during VNS, thus explaining its favorable outcome, in contrast to the other 2 aforementioned studies, whose stimulation parameters were not optimized to achieve therapeutic effects. It is reasonable to speculate that our study engaged vagal fibers close to the target therapeutic zone. In light of the differential effects of different stimulation parameters on cardiac physiology [46], more research needs to be directed towards optimizing the stimulation parameters for neuromodulation therapy.
Limitations
This was a small, proof of concept, short-term study, designed to establish the first evidence of the acute effects of LLTS on LV function in humans and provide the basis for the design of human studies using this modality to target HFpEF. Longer term assessment is needed before translating this modality into therapy for HFpEF. In addition, we included patients with diastolic dysfunction on initial screening echocardiogram, both with and without clinical HFpEF. However, if anything, including low risk patients would be expected to diminish the magnitude of the effect seen, as suggested by the fact that the effect of LLTS was stronger in those with the lowest baseline GLS (Figure 4A); therefore we expect that our findings would apply to HFpEF patients. Although the primary endpoint of the study was met, it should be acknowledged that the magnitude of the effect was modest. Nonetheless, the change in GLS between LLTS and sham is comparable to the difference between patients with HFpEF compared to those with hypertensive heart disease[10, 26]. In addition, HRV analysis using the FFT method did not yield positive results. However, it has been previously shown that the autoregressive method used in our study is the preferred method for HF band calculation [24]. We only evaluated a fixed set of stimulation parameters for LLTS in our study (frequency 20Hz, pulse duration 200μs, amplitude 1mA below the discomfort threshold), which were selected empirically, based on the favorable response to simulation in our previous study in patients with atrial fibrillation [17]. These parameters likely activated vagal afferent fibers [33, 46]. As the selection of stimulation parameters is a critical factor for determining the efficacy of autonomic neuromodulation therapies [46], future studies should systematically evaluate the impact of different stimulation protocols on the observed outcomes. We did not make any more recordings after stopping stimulation. Therefore, we cannot comment on any memory effects of LLTS. However, based on other evidence suggesting that both the antiarrhythmic [47] and the anti-inflammatory [48] effects of VNS exhibit memory, it is reasonable to speculate that memory exists also for its effects on cardiac mechanics and HRV. Finally, we did not examine any biomarkers in this study, or measures of autonomic tone other than HRV. Nonetheless, a recent study has shown that sympathetic tone, as assessed by muscle sympathetic nerve activity, as well as the LF/HF ratio, were significantly decreased by LLTS (frequency 30Hz, pulse duration 200μs, just below the sensory threshold) in healthy volunteers [19].
Clinical implications
In this first-in-man, proof-of-concept study, we demonstrated that LLTS results in a significant improvement in myocardial longitudinal function as measured by GLS in patients with preserved LV ejection fraction. As myocardial longitudinal function measured by GLS has been shown to be a powerful and independent predictor of clinical outcomes in patients with diabetes [49], hypertension [35] and HFpEF [34], we propose that LLTS may be a potential promising treatment for HFpEF. This study forms the basis for the design of further studies to evaluate the efficacy of LLTS as a novel therapy for HFpEF. Notably, the stimulation voltage used to achieve LLTS was below patient discomfort threshold, and significantly below the cardiac threshold, suggesting that this therapy could be well-tolerated and safe in the ambulatory setting. Importantly, it has been previously demonstrated that vagal afferent fibers can be activated at approximately 20% of the bradycardia threshold [33]. In addition, we have recently shown in humans with atrial fibrillation that the discomfort threshold is approximately 60% of the bradycardia threshold, while stimulation at 50% of the bradycardia threshold resulted in a significant decrease in inflammatory cytokines and atrial fibrillation duration [17]. Further chronic studies in ambulatory patients with HFpEF are warranted to evaluate the efficacy of this treatment modality in this population.
Conclusions
In this study, we demonstrated for the first time in humans that LLTS acutely ameliorates LV longitudinal mechanics and favorably alters sympathovagal balance in patients with diastolic dysfunction and preserved LV ejection fraction. Our results support the use of LLTS as a possible therapy for patients with HFpEF. Further larger scale investigations are necessary to confirm our results.
Acknowledgments
Sources of funding: Funded by an Oklahoma Shared Clinical and Translational Resources pilot grant (NIGMS IDeA-CTR U54-GM104938) to Stavros Stavrakis
Abbreviations
- HFpEF
Heart failure with preserved ejection fraction
- LV
Left ventricle
- HFrEF
Heart failure with reduced ejection fraction
- VNS
Vagus nerve stimulation
- LLTS
Low-level transcutaneous vagus nerve stimulation
- TENS
Transcutaneous electrical nerve stimulation
- GLS
Global longitudinal strain
- HRV
Heart rate variability
- HF
high frequency
- LF
low frequency
Footnotes
Clinical trial registration: NCT02983448
Disclosures: None
Human Subjects/informed consent statement: All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000. Informed consent was obtained from all patients for being included in the study.
Animal studies: No animal studies were carried out by the authors for this article.
References:
- 1.Lam CS, Donal E, Kraigher-Krainer E, Vasan RS (2011). Epidemiology and clinical course of heart failure with preserved ejection fraction, Eur J Heart Fail 13(1) 18–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Owan TE, Hodge DO, Herges RM, Jacobsen SJ, Roger VL, Redfield MM (2006). Trends in prevalence and outcome of heart failure with preserved ejection fraction, N Engl J Med 355(3) 251–9. [DOI] [PubMed] [Google Scholar]
- 3.Fonarow GC, Stough WG, Abraham WT, Albert NM, Gheorghiade M, Greenberg BH, O’Connor CM, Sun JL, Yancy CW, Young JB (2007). Characteristics, treatments, and outcomes of patients with preserved systolic function hospitalized for heart failure: a report from the OPTIMIZE-HF Registry, J Am Coll Cardiol 50(8) 768–77. [DOI] [PubMed] [Google Scholar]
- 4.Tribouilloy C, Rusinaru D, Mahjoub H, Souliere V, Levy F, Peltier M, Slama M, Massy Z (2008). Prognosis of heart failure with preserved ejection fraction: a 5 year prospective population-based study, Eur Heart J 29(3) 339–47. [DOI] [PubMed] [Google Scholar]
- 5.Butler J, Fonarow GC, Zile MR, Lam CS, Roessig L, Schelbert EB, Shah SJ, Ahmed A, Bonow RO, Cleland JG, Cody RJ, Chioncel O, Collins SP, Dunnmon P, Filippatos G, Lefkowitz MP, Marti CN, McMurray JJ, Misselwitz F, Nodari S, O’Connor C, Pfeffer MA, Pieske B, Pitt B, Rosano G, Sabbah HN, Senni M, Solomon SD, Stockbridge N, Teerlink JR, Georgiopoulou VV, Gheorghiade M (2014). Developing therapies for heart failure with preserved ejection fraction: current state and future directions, JACC Heart Fail 2(2) 97–112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Senni M, Paulus WJ, Gavazzi A, Fraser AG, Diez J, Solomon SD, Smiseth OA, Guazzi M, Lam CS, Maggioni AP, Tschope C, Metra M, Hummel SL, Edelmann F, Ambrosio G, Stewart Coats AJ, Filippatos GS, Gheorghiade M, Anker SD, Levy D, Pfeffer MA, Stough WG, Pieske BM (2014). New strategies for heart failure with preserved ejection fraction: the importance of targeted therapies for heart failure phenotypes, Eur Heart J 35(40) 2797–815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Glezeva N, Baugh JA (2014). Role of inflammation in the pathogenesis of heart failure with preserved ejection fraction and its potential as a therapeutic target, Heart Fail Rev 19(5) 681–94. [DOI] [PubMed] [Google Scholar]
- 8.Gomberg-Maitland M, Shah SJ, Guazzi M (2016). Inflammation in Heart Failure With Preserved Ejection Fraction: Time to Put Out the Fire, JACC Heart Fail 4(4) 325–8. [DOI] [PubMed] [Google Scholar]
- 9.Paulus WJ, Tschope C (2013). A novel paradigm for heart failure with preserved ejection fraction: comorbidities drive myocardial dysfunction and remodeling through coronary microvascular endothelial inflammation, J Am Coll Cardiol 62(4) 263–71. [DOI] [PubMed] [Google Scholar]
- 10.Kraigher-Krainer E, Shah AM, Gupta DK, Santos A, Claggett B, Pieske B, Zile MR, Voors AA, Lefkowitz MP, Packer M, McMurray JJ, Solomon SD, Investigators P (2014). Impaired systolic function by strain imaging in heart failure with preserved ejection fraction, J Am Coll Cardiol 63(5) 447–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Aikawa T, Naya M, Obara M, Manabe O, Tomiyama Y, Magota K, Yamada S, Katoh C, Tamaki N, Tsutsui H (2017). Impaired Myocardial Sympathetic Innervation Is Associated with Diastolic Dysfunction in Heart Failure with Preserved Ejection Fraction: (11)C-Hydroxyephedrine PET Study, J Nucl Med 58(5) 784–790. [DOI] [PubMed] [Google Scholar]
- 12.Toledo C, Andrade DC, Lucero C, Arce-Alvarez A, Diaz HS, Aliaga V, Schultz HD, Marcus NJ, Manriquez M, Faundez M, Del Rio R (2017). Cardiac diastolic and autonomic dysfunction are aggravated by central chemoreflex activation in heart failure with preserved ejection fraction rats, J Physiol 595(8) 2479–2495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pavlov VA, Tracey KJ (2015). Neural circuitry and immunity, Immunol Res 63(1–3) 38–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tracey KJ (2009). Reflex control of immunity, Nat Rev Immunol 9(6) 418–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Beaumont E, Wright GL, Southerland EM, Li Y, Chui R, KenKnight BH, Armour JA, Ardell JL (2016). Vagus nerve stimulation mitigates intrinsic cardiac neuronal remodeling and cardiac hypertrophy induced by chronic pressure overload in guinea pig, Am J Physiol Heart Circ Physiol 310(10) H1349–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Fallgatter AJ, Neuhauser B, Herrmann MJ, Ehlis AC, Wagener A, Scheuerpflug P, Reiners K, Riederer P (2003). Far field potentials from the brain stem after transcutaneous vagus nerve stimulation, J Neural Transm 110(12) 1437–43. [DOI] [PubMed] [Google Scholar]
- 17.Stavrakis S, Humphrey MB, Scherlag BJ, Hu Y, Jackman WM, Nakagawa H, Lockwood D, Lazzara R, Po SS (2015). Low-level transcutaneous electrical vagus nerve stimulation suppresses atrial fibrillation, J Am Coll Cardiol 65(9) 867–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yu L, Huang B, Po SS, Tan T, Wang M, Zhou L, Meng G, Yuan S, Zhou X, Li X, Wang Z, Wang S, Jiang H (2017). Low-Level Tragus Stimulation for the Treatment of Ischemia and Reperfusion Injury in Patients With ST-Segment Elevation Myocardial Infarction: A Proof-of-Concept Study, JACC Cardiovasc Interv 10(15) 1511–1520. [DOI] [PubMed] [Google Scholar]
- 19.Clancy JA, Mary DA, Witte KK, Greenwood JP, Deuchars SA, Deuchars J (2014). Non-invasive Vagus Nerve Stimulation in Healthy Humans Reduces Sympathetic Nerve Activity, Brain Stimul 7(6) 871–7. [DOI] [PubMed] [Google Scholar]
- 20.Nagueh SF, Smiseth OA, Appleton CP, Byrd BF 3rd, Dokainish H, Edvardsen T, Flachskampf FA, Gillebert TC, Klein AL, Lancellotti P, Marino P, Oh JK, Alexandru Popescu B, Waggoner AD, Houston, T., Oslo, N., Phoenix, A., Nashville, T., Hamilton, O.C., Uppsala, S., Ghent, Liege, B., Cleveland, O., Novara, I., Rochester, M., Bucharest, R., St. Louis, M. (2016). Recommendations for the Evaluation of Left Ventricular Diastolic Function by Echocardiography: An Update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging, Eur Heart J Cardiovasc Imaging 17(12) 1321–1360. [DOI] [PubMed] [Google Scholar]
- 21.Peuker ET, Filler TJ (2002). The nerve supply of the human auricle, Clin Anat 15(1) 35–7. [DOI] [PubMed] [Google Scholar]
- 22.Tarvainen MP, Niskanen JP, Lipponen JA, Ranta-Aho PO, Karjalainen PA (2014). Kubios HRV--heart rate variability analysis software, Comput Methods Programs Biomed 113(1) 210–20. [DOI] [PubMed] [Google Scholar]
- 23.(1996). Heart rate variability: standards of measurement, physiological interpretation and clinical use. Task Force of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology, Circulation 93(5) 1043–65. [PubMed] [Google Scholar]
- 24.Laborde S, Mosley E, Thayer JF (2017). Heart Rate Variability and Cardiac Vagal Tone in Psychophysiological Research - Recommendations for Experiment Planning, Data Analysis, and Data Reporting, Front Psychol 8 213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Freeman R (2006). Assessment of cardiovascular autonomic function, Clin Neurophysiol 117(4) 716–30. [DOI] [PubMed] [Google Scholar]
- 26.Mordi IR, Singh S, Rudd A, Srinivasan J, Frenneaux M, Tzemos N, Dawson DK (2018). Comprehensive Echocardiographic and Cardiac Magnetic Resonance Evaluation Differentiates Among Heart Failure With Preserved Ejection Fraction Patients, Hypertensive Patients, and Healthy Control Subjects, JACC Cardiovasc Imaging 11(4) 577–585. [DOI] [PubMed] [Google Scholar]
- 27.Deuchars SA, Lall VK, Clancy J, Mahadi M, Murray A, Peers L, Deuchars J (2018). Mechanisms underpinning sympathetic nervous activity and its modulation using transcutaneous vagus nerve stimulation, Exp Physiol 103(3) 326–331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Schwartz PJ, Pagani M, Lombardi F, Malliani A, Brown AM (1973). A cardiocardiac sympathovagal reflex in the cat, Circ Res 32(2) 215–20. [DOI] [PubMed] [Google Scholar]
- 29.Frangos E, Ellrich J, Komisaruk BR (2015). Non-invasive Access to the Vagus Nerve Central Projections via Electrical Stimulation of the External Ear: fMRI Evidence in Humans, Brain Stimul 8(3) 624–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Grassi G, Seravalle G, Quarti-Trevano F, Dell’Oro R, Arenare F, Spaziani D, Mancia G (2009). Sympathetic and baroreflex cardiovascular control in hypertension-related left ventricular dysfunction, Hypertension 53(2) 205–9. [DOI] [PubMed] [Google Scholar]
- 31.Toschi-Dias E, Rondon M, Cogliati C, Paolocci N, Tobaldini E, Montano N (2017). Contribution of Autonomic Reflexes to the Hyperadrenergic State in Heart Failure, Front Neurosci 11 162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Vasudevan NT, Mohan ML, Goswami SK, Naga Prasad SV (2011). Regulation of beta-adrenergic receptor function: an emphasis on receptor resensitization, Cell Cycle 10(21) 3684–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ardell JL, Rajendran PS, Nier HA, KenKnight BH, Armour JA (2015). Central-peripheral neural network interactions evoked by vagus nerve stimulation: functional consequences on control of cardiac function, Am J Physiol Heart Circ Physiol 309(10) H1740–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Potter E, Marwick TH (2018). Assessment of Left Ventricular Function by Echocardiography: The Case for Routinely Adding Global Longitudinal Strain to Ejection Fraction, JACC Cardiovasc Imaging 11(2 Pt 1) 260–274. [DOI] [PubMed] [Google Scholar]
- 35.Saito M, Khan F, Stoklosa T, Iannaccone A, Negishi K, Marwick TH (2016). Prognostic Implications of LV Strain Risk Score in Asymptomatic Patients With Hypertensive Heart Disease, JACC Cardiovasc Imaging 9(8) 911–21. [DOI] [PubMed] [Google Scholar]
- 36.Ho SY (2009). Anatomy and myoarchitecture of the left ventricular wall in normal and in disease, Eur J Echocardiogr 10(8) iii3–7. [DOI] [PubMed] [Google Scholar]
- 37.Schroder J, Hamada S, Altiok E, Almalla M, Koutziampasi C, Napp A, Keszei A, Hein M, Becker M (2017). Detection of Acute Changes in Left Ventricular Function by Myocardial Deformation Analysis after Excessive Alcohol Ingestion, J Am Soc Echocardiogr 30(3) 235–243 e1. [DOI] [PubMed] [Google Scholar]
- 38.Dedobbeleer C, Hadefi A, Naeije R, Unger P (2013). Left ventricular adaptation to acute hypoxia: a speckle-tracking echocardiography study, J Am Soc Echocardiogr 26(7) 736–45. [DOI] [PubMed] [Google Scholar]
- 39.Sha Y, Scherlag BJ, Yu L, Sheng X, Jackman WM, Lazzara R, Po SS (2011). Low-level right vagal stimulation: anticholinergic and antiadrenergic effects, J Cardiovasc Electrophysiol 22(10) 1147–53. [DOI] [PubMed] [Google Scholar]
- 40.Chinda K, Tsai WC, Chan YH, Lin AY, Patel J, Zhao Y, Tan AY, Shen MJ, Lin H, Shen C, Chattipakorn N, Rubart-von der Lohe M, Chen LS, Fishbein MC, Lin SF, Chen Z, Chen PS (2016). Intermittent left cervical vagal nerve stimulation damages the stellate ganglia and reduces the ventricular rate during sustained atrial fibrillation in ambulatory dogs, Heart Rhythm 13(3) 771–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Tadic M, Cuspidi C, Pencic B, Pavlovic SU, Ivanovic B, Kocijancic V, Celic V (2015). Association between left ventricular mechanics and heart rate variability in untreated hypertensive patients, J Clin Hypertens (Greenwich) 17(2) 118–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Tadic M, Zlatanovic M, Cuspidi C, Ivanovic B, Stevanovic A, Damjanov N, Kocijancic V, Celic V (2017). The relationship between left ventricular deformation and heart rate variability in patients with systemic sclerosis: Two- and three-dimensional strain analysis, Int J Cardiol 236 145–150. [DOI] [PubMed] [Google Scholar]
- 43.Gold MR, Van Veldhuisen DJ, Hauptman PJ, Borggrefe M, Kubo SH, Lieberman RA, Milasinovic G, Berman BJ, Djordjevic S, Neelagaru S, Schwartz PJ, Starling RC, Mann DL (2016). Vagus Nerve Stimulation for the Treatment of Heart Failure: The INOVATE-HF Trial, J Am Coll Cardiol 68(2) 149–58. [DOI] [PubMed] [Google Scholar]
- 44.Zannad F, De Ferrari GM, Tuinenburg AE, Wright D, Brugada J, Butter C, Klein H, Stolen C, Meyer S, Stein KM, Ramuzat A, Schubert B, Daum D, Neuzil P, Botman C, Castel MA, D’Onofrio A, Solomon SD, Wold N, Ruble SB (2015). Chronic vagal stimulation for the treatment of low ejection fraction heart failure: results of the NEural Cardiac TherApy foR Heart Failure (NECTAR-HF) randomized controlled trial, Eur Heart J 36(7) 425–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Premchand RK, Sharma K, Mittal S, Monteiro R, Dixit S, Libbus I, DiCarlo LA, Ardell JL, Rector TS, Amurthur B, KenKnight BH, Anand IS (2014). Autonomic regulation therapy via left or right cervical vagus nerve stimulation in patients with chronic heart failure: results of the ANTHEM-HF trial, J Card Fail 20(11) 808–16. [DOI] [PubMed] [Google Scholar]
- 46.Ardell JL, Nier H, Hammer M, Southerland EM, Ardell CL, Beaumont E, KenKnight BH, Armour JA (2017). Defining the neural fulcrum for chronic vagus nerve stimulation: implications for integrated cardiac control, J Physiol 595(22) 6887–6903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Salavatian S, Beaumont E, Longpre JP, Armour JA, Vinet A, Jacquemet V, Shivkumar K, Ardell JL (2016). Vagal stimulation targets select populations of intrinsic cardiac neurons to control neurally induced atrial fibrillation, Am J Physiol Heart Circ Physiol 311(5) H1311–H1320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Koopman FA, Chavan SS, Miljko S, Grazio S, Sokolovic S, Schuurman PR, Mehta AD, Levine YA, Faltys M, Zitnik R, Tracey KJ, Tak PP (2016). Vagus nerve stimulation inhibits cytokine production and attenuates disease severity in rheumatoid arthritis, Proc Natl Acad Sci U S A 113(29) 8284–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Liu JH, Chen Y, Yuen M, Zhen Z, Chan CW, Lam KS, Tse HF, Yiu KH (2016). Incremental prognostic value of global longitudinal strain in patients with type 2 diabetes mellitus, Cardiovasc Diabetol 15 22. [DOI] [PMC free article] [PubMed] [Google Scholar]