Abstract
Carotid endarterectomy (CEA) is widely used for cervical artery stenosis. In Japan, primary closure after endarterectomy has been a standard technique. Recently, the patch closure has been shown to be superior to the primary suture for the prevention of restenosis and ipsilateral stroke. This study evaluated the 5- and 10-year outcomes following CEA with patch graft closure in our institution. Between January 2000 and March 2013, 134 patients, who underwent CEA with patch graft closure were investigated in the current retrospective study. Among these patients, 102 CEAs in 97 patients were followed up for 5 years and 66 CEAs in 61 patients were for 10 years after the procedure. Restenosis was defined as >50% recurrent luminal narrowing at the endarterectomy site. In 5 years, symptomatic restenosis exhibited minor stroke in one patient at 58 months after CEA (restenosis rate 1.0%). The ipsilateral minor stroke occurred in three patients including the above case (2.9%). In 10 years, asymptomatic restenosis occurred in three patients in addition to the above symptomatic case (restenosis rate 6.1%), and the ipsilateral minor stroke occurred in four patients (6.1%). Carotid endarterectomy with patch graft exerted a high protective effect from restenosis up to 5 and 10 years in our institution. The number of carotid artery stenting is increasing all over the world but we speculated that the established surgical procedure of patched CEA prevented restenosis and ipsilateral stroke.
Keywords: carotid endarterectomy, patch graft closure, long term results, restenosis
Introduction
Atherosclerotic carotid artery stenosis causes transient ischemic attack and stroke. The endovascular treatment of carotid artery stenosis by percutaneous transluminal insertion of a stent is less invasive and an alternative to endarterectomy. However, whether carotid artery stenting (CAS) is superior to endarterectomy at the points of perioperative complications, prevention of stroke, restenosis, and death is yet controversial. Therefore, endarterectomy remains an established surgical option of stroke prevention in symptomatic and selected asymptomatic patients with carotid artery stenosis. The North American Symptomatic Carotid Endarterectomy (NASCET) Trial and The Asymptomatic Carotid Atherosclerosis Study provide Class 1 evidence of superior outcomes with endarterectomy as compared to the medical therapy for the prevention of stroke.1–4) The rate of restenosis after carotid endarterectomy (CEA) was 5–15% as reported previously5–7) and less frequent with CEA than CAS.8) Some studies emphasized that patch graft closure and eversion CEA are superior to conventional primary closure CEA at the point of restenosis, although this is yet controversial.9–12) Moreover, only a few studies reported the long-term outcome, while a majority reported the outcome after CEA with a follow-up period 30 days to 5 years.4,5,13,14) In Japan, primary closure after endarterectomy has been recognized as a standard closure technique; however, patch angioplasty with hemashield patch has been performed in Tokushima university since 2000.
In this retrospective study, we reported the incidence of restenosis and ipsilateral stroke in a 5- and 10-year follow-up of our patients who underwent CEA with patch graft closure for symptomatic and asymptomatic carotid artery stenosis.
Materials and Methods
Between January 2000 and March 2013, 175 CEAs were performed in 166 patients with internal carotid artery (ICA) occlusive disease in our institution; 157 patients underwent unilateral CEAs, and the remaining nine patients underwent bilateral CEAs and 134 patched CEAs and 130 CASs were performed between January 2000 and March 2013. CEA was performed as a first line procedure, and CAS was primarily applied for patients >75 years of age or those with heart disease or with high position bifurcation of ICA. Magnetic resonance imaging (MRI) was performed within 7 days after CEA.
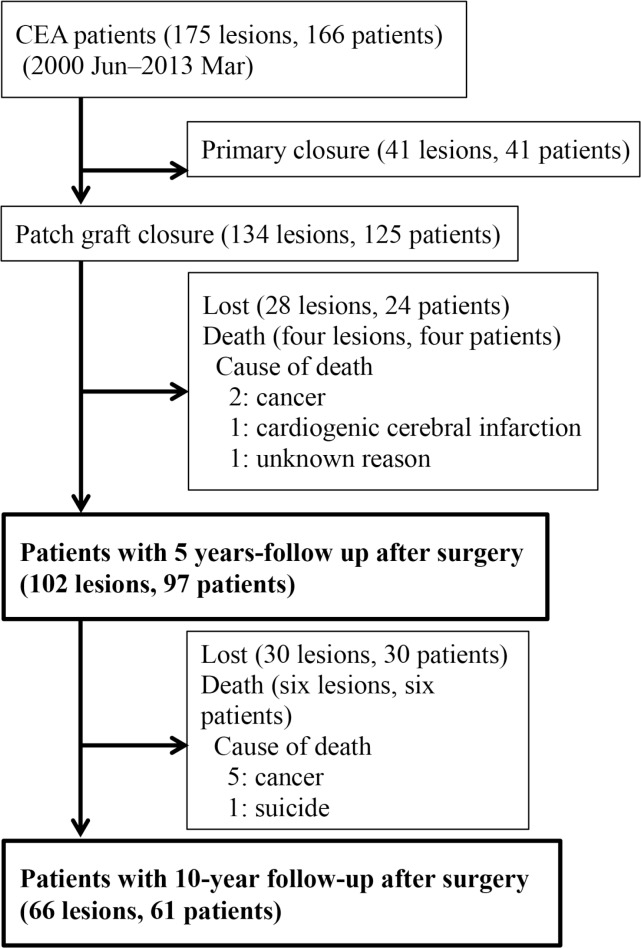
A total of 41 CEAs in four patients received primary closure between 2001 and 2003 because the Hemashield woven Double Velour Finesse (Intervascular SAS, La Ciotat, France) could not be supplied in Japan. Thus, a total of 125 patients with 134 CEA received patch graft closure, while 20 patients with unilateral CEA and four patients with bilateral CEAs were lost during the 5-year follow-up. A cohort of 98 patients with 102 CEAs received patch graft closure that was analyzed during the 5-year follow-up and 66 CEAs in 61 patients were in a 10-year follow-up (Fig. 1). Routinely, MRI, magnetic resonance angiography (MRA) was performed each year and Doppler ultrasonography was sometimes performed. Restenosis was defined as such when >50% recurrent luminal narrowing was observed at the endarterectomy site on MRA or Doppler ultrasonography using NASCET method. However, European Carotid Surgery Trial method was used in unusual cases that could not assessed by NASCET method. Stroke was defined as ipsilateral ischemic cerebral infarction. The medical records of the patients were reviewed to collect the data regarding patient characteristics, stroke, mortality, restenosis, and other surgical complications. From their hospital records, preoperative atherosclerotic risk factors were accessed.
Fig. 1.
Baseline characteristics of patients who underwent carotid endarterectomy with patch graft closure in 5- and 10-year follow-up. CEA, carotid endarterectomy.
Protocol of preoperative and intraoperative management
Antiplatelet medications were routinely administered preoperatively, ceased 3 days before the procedure, and re-administered 1 day after the procedure. Coronary angiography was performed preoperatively to avoid intra and postoperative coronary artery events. The coronary artery stenting or bypass graft was performed preoperatively if necessary. The surgical procedures were performed under general anesthesia. The surgical techniques and methods of intraoperative neurofunctional monitoring were reported in 2007.15) The patch angioplasty with Hemashield woven Double Velour Finesse was performed with 6-0 Prolene (Ethicon Inc., Bridgewater, NJ, USA) after standard endarterectomy. Direct angiography or indocyanine green video angiography was performed after patch angioplasty. The hyperperfusion state was determined based on the increase in transcranial Doppler or regional saturation of oxygen. Moreover, sedation was accomplished by intravenous anesthesia to decrease and stabilize the intracranial and blood pressure.
Statistical analysis
Statistical analysis was performed using JMP 13.2 (SAS Institute Inc., Cary, NC, USA). Univariate and multivariate logistic regression analysis was performed to identify the risk factors that affected restenosis. The stepwise forward selection method was used to select the factors for multivariate analysis. The P-value threshold for entry was set at 0.05, and P <0.05 was considered as statistically significant.
Results
About 106/134 (79.1%) CEAs were monitored for >5 years post-surgery. The baseline characteristics of the patients, excluding the dead cases, are shown in Table 1. The average age of the patients at the time of surgery was 68 ± 7.3 years, and 85.3% were males. Symptomatic carotid artery stenosis was observed in 62/102 (63.4%) patients; of these, 83/102 (81.4%) had hypertension, and approximately half had a smoking history and hyperlipidemia. Moreover, 39/102 (38.2%) had diabetes, and 16/102 (15.7%) had prior coronary disease. Four patients died after operation and two because of cancer, while one patient died of cardiogenic cerebral infarction and one more patient died due to unknown reason within 5 years.
Table 1.
Baseline characteristics of the patients excluding dead cases who underwent carotid endarterectomy with patch graft closure in 5-year follow-up
| No. (%) | N = 102 |
|---|---|
| Age (years), mean ± SD | 68 ± 7.3 |
| Gender (Male) | 87 (85.3) |
| Symptomatic | 64 (62.8) |
| Atherosclerotic risk factors | |
| Smoking | 49 (48.0) |
| Hyperlipidemia | 51 (50.0) |
| Hypertension | 83 (81.4) |
| Diabetes | 39 (38.2) |
| Past coronary artery disease | 16 (15.7) |
Symptomatic restenosis, which induced minor stroke on parietal cortex, occurred in one patient (restenosis rate 1.0%) at 58 months after CEA, while non-symptomatic restenosis was not observed in any patient. Ipsilateral stroke occurred in three patients including the above case (2.9%) and minor stroke occurred in all cases. The causes of minor stroke were diagnosed as perforating branch infarctions unrelated to the procedure without the above symptomatic case. In the above case with symptomatic restenosis, MRA showed no restenosis 1 year before. Additional CAS was performed in the above case.
Among the 102 CEAs, asymptomatic high signals were detected on postoperative diffusion-weighted image (DWI) in six patients, while one was symptomatic. This symptomatic patient presented contralateral hemiparesis 2 days after the surgery due to the occlusion of the ipsilateral internal carotid artery on MRA that was treated by revascularization. In addition, the hemiparesis was almost recovered. Furthermore, five cases were in the hyperperfusion state without neurological deterioration although stringent blood pressure control was essential. Neither death nor acute myocardial infarction was observed within 30 days after surgery. There were two cases of transient cranial nerve injury, one of subcutaneous hematoma that needed reoperation, one of transient C5 palsy, one of interstitial pneumonia in 1, one of heart failure that recovered fully (Table 2).
Table 2.
Major and minor mortality in 102 patched CEAs
| Number of patients | ||
|---|---|---|
| Symptomatic | Asymptomatic | |
| Major morbidity/mortality (Stroke, death) | ||
| Postoperative DWI-positive | 1 | 6 |
| Hyperperfusion syndrome | 0 | 5 |
| Stroke | 1 | |
| Death | 0 | |
| Acute myocardial infarction | 0 | |
| Minor morbidity | ||
| Local complication | ||
| Cranial nerve injury | Permanent | Transient |
| Laryngeal nerve | 0 | 1 |
| Hypoglossal nerve | 0 | 1 |
| C5 palsy | 0 | 1 |
| Neurological deterioration | 0 | 2 |
| Bleeding, hematoma | 1 | |
| Retinal artery thrombosis | 1 | |
| Systemic complication | ||
| Operation related | None | |
| Operation non-related | ||
| Severe pneumoniae | 1 | |
| Heart failure | 1 | |
| Acute myocardial infarction | 0 | |
CEA: carotid endarterectomy, DWI: diffusion-weighted image.
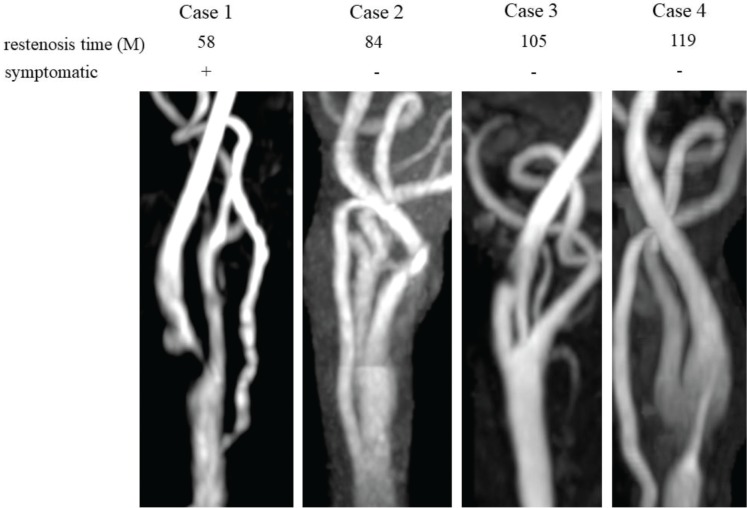
Between January 2000 and March 2008, 104 patched CEAs were performed in 95 patients. These 95 patients received unilateral CEAs, while the remaining nine patients received bilateral CEAs. Among the 104 CEAs, 76 CEAs in 71 patients were followed up for 10 years post-surgery. We found that 10 patients died after operation and seven because of cancer, while one patient died of cardiogenic cerebral infarction and one patient died due to suicide and one more patient died due to unknown reason within 10 years. The tracking rate was 73.1% (76/104). Symptomatic restenosis occurred in one patient at 58 months after CEA, and non-symptomatic restenosis was observed in three patients (symptomatic restenosis rate 1.5%, all restenosis rate 6.1%). Ipsilateral stroke occurred in four patients including the above symptomatic restenosis case (6.1%), and minor stroke occurred in all cases. The causes of minor stroke were diagnosed as perforating branch infarctions unrelated to the procedure without the symptomatic restenosis case. The restenosis time and risk factors of symptomatic and asymptomatic restenosis in all cases are listed in Table 3, and cervical MRA at restenosis were shown in Fig. 2. Rapid restenosis within 1 year was occurred in Case 1 at the 58 months and in Case 2 at the 84 months, respectively. On the other hand, slow restenosis within 3 years was occurred in Case 3 at the 105 months and in Case 4 at the 119 months, respectively. All the restenosis cases were smokers before the procedure, although whether they were current smokers at the time of restenosis could not be deduced. Furthermore, the univariate and multivariate analysis demonstrated that the restenosis risk was significantly higher in smokers compared with the patients without smoking history (P = 0.0362, 0.0342, respectively). As shown in Fig. 2, a part of restenosis was variable. Consequently, no symptomatic restenosis was observed between 5 and 10 years post-surgery. However, in Case 3, additional CAS was needed because amaurosis fugax occurred in 11 years post-surgery.
Table 3.
Restenosis time and the risk factors of the patients with restenosis after patched CEA
| Case | Restenosis time (M) | Symptomatic | Age | Sex | Smoking | Hyperlipidemia | Hypertension | Diabetes | Past coronary artery disease |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 58 | + | 72 | M | + | − | − | − | + |
| 2 | 84 | − | 57 | M | + | + | + | + | − |
| 3 | 105 | − | 59 | M | + | − | − | − | − |
| 4 | 119 | − | 71 | F | + | − | + | − | − |
CEA: carotid endarterectomy.
Fig. 2.
Cervical MRA when restenosis was pointed out in all cases of restenosis. Case 1 only showed symptomatic restenosis 58 months after patched CEA and other three cases showed asymptomatic restenosis 84, 105, 119 months after CEA, respectively. Case 3 showed amaurosis fugax in 11 years after surgery and CAS was performed. CEA, carotid endarterectomy.
Discussion
A prolonged lifespan of more than a decade and improved long-term outcomes of the surgical procedures are required. In this study, we reported long-term outcomes after CEA in our institution. Literature suggested that patched CEA could reduce the combined perioperative and long-term risk of stroke and the risk of restenosis as compared with the primary closure; however, large prospective studies are essential to prove the superiority of patched CEA.11,16,17) Paraskevas et al.12) reported a systematic review and meta-analysis of outcomes following eversion vs. conventional endarterectomy in randomized controlled trials and observational studies. In this meta-analysis, eversion and patched CEA was superior to the conventional CEA with respect to the perioperative outcomes (death, stroke, death/stroke) and late stenosis (>50%). Although the duration of late stenosis was not clearly defined, the follow-up period in a majority of the studies was within 5 years. Interestingly, >5-year follow-up data of patched CEA were limited.5,13)
As shown in Table 2, the rate of permanent perioperative complications was low (1.0%) in our cohort although transient complications were observed in five patients (4.9%). Compared with that described in previous studies,18–20) the current results were acceptable. First, the neurosurgeons performed endarterectomy and patch graft closure using a microscope and under general anesthesia. Second, postoperative management with intra and postoperative monitors were presumed to decrease the incidence of postoperative wound hemorrhage and prevent the intracranial hemorrhage and hyperperfusion syndrome. This might also explain the need for CAS in high-risk patients for CEA.
In the current series, restenosis rate and ipsilateral stroke rate were 1.0% and 2.9% in 5 years and 6.1% and 6.1% in 10 years after patched CEA, respectively. Avgerinos et al.9) reported that 5- and 10-year restenosis rate of >50% and ipsilateral stroke were 15.4% and 24.3% and 4.5% and 8.5%, respectively. On the other hand, Lamba et al.14) reported the long-term outcomes after primary closure CEA of an average-volume neurosurgeon and demonstrated that 5- and 10-year restenosis rate of >70% and ipsilateral stroke were 2.1% and 3.2% and 1.6% and 2.1%, respectively. As shown in Fig. 2, 5- and 10-year restenosis rate of >70% in 2 cases (Cases 1 and 4) was 1.0% and 3.0%, respectively, and these results were comparable to the outcomes of the study by Lamba et al. Although the definition of restenosis by Lamba et al. was different from the current study, the results were surprisingly excellent; however, the risk factors of restenosis were not discussed. Chan et al. reported that a low restenosis rate was associated with never smokers in both univariate and multivariate analysis (median follow-up time: 40 months). Garzon-Muvdi et al.21) reported that restenosis-free survival was influenced by the presence of hyperlipidemia, age, and family history of stroke. As shown in Table 3, all the four patients, who showed restenosis within 10 years after patched CEA, were smokers. In the current cohort, a high restenosis rate was found to be associated with smokers before the procedure in both univariate and multivariate analysis (P = 0.0362, 0.0342, respectively). The other atherosclerotic risk factors were not significantly associated with restenosis. In our series, appropriate medical treatment to risk factors was performed after procedure, but we could not access that smokers before procedure could quit smoking after procedure. In past, various factors such as female and intimal hyperplasia were pointed out expect the above atherosclerotic risk factors.22–25) In this series, we could not access the factors because there were few females and none of female showed restenosis in 5 years and one showed restenosis among 11 female patients in 10 years. Concerning to intimal hyperplasia, we reviewed the reports of Doppler ultrasonography, because we could not access with conventional MRA. Slight or mild intimal hyperplasia was not detected in 1 year after procedure in almost cases and detected in 3 years approximately in half, but there was no lesion where intimal hyperplasia caused significant stenosis. It was considered that patch could thicken the diameter of ICA and did not cause significant stenosis even if intimal hyperplasia happened.
Till now no past reports on the site and pattern of restenosis was debated. However, in our series, there was no tendency and it had various forms such as proximal side, distal side, bifurcation part, and dissection like appearance hence it is clear that restenosis is very uncertain pattern.
Restenosis rates after CEA are less frequent with CEA than CAS.8) In 2017, Kumar et al.26) reviewed restenosis and recurrent ipsilateral stroke after CEA and CAS. The weighted incidence of restenosis >70% was 4.1% after patched CEA with median 32 months and 10% after CAS with median 62 months. Heo et al.27) reported early outcomes and restenosis rates between CEA and CAS using the propensity score matching analysis on 1184 patients at a single institution (654 CEA and 530 CAS). To compare with the CEA group, the CAS group showed a relatively high 30-day incidence of major adverse clinical events (2.4% vs. 7.5%) but a low incidence of procedure-related complications (5.3% vs. 1.5%). During a mean follow-up of 49.1 months, restenosis rates were higher after CAS than after CEA (1.5% vs. 1.0% at 12 months and 5.4% vs. 1.2% at 24 months, respectively). Herein, we did not assess the CAS group in our institution and presumed that our results were acceptable at the points of procedure-related complications, early and late restenosis rate, and ipsilateral stroke rate.
Limitations
This study has some limitations. First, this study was not prospective. Second, 28/134 CEAs (20.1%) during the 5-year follow-up and 28/104 patients (26.9%) during the 10-year follow-up were lost. Third, we did not compare with the simultaneous our CAS group in our institution. Nevertheless, this study represented one of the longest-duration studies of CEA with patch graft from a single institution.
Conclusion
We demonstrated that CEA with patch graft closure is an established procedure for preventing ipsilateral stroke and restenosis with carotid artery stenosis. Symptomatic restenosis occurred in only one case at 58 months after patched CEA, and the frequency in 5- and 10-year follow-up was 1.0% and 1.5%, respectively. Despite limitations, the pre, intra, and postoperative management and surgical skill provided satisfactory long-term outcomes for patched CEA.
Footnotes
Author Contributions
All authors accept equal responsibility for the content of this report. None has any financial interests concerning this manuscript.
Conflicts of Interest Disclosure
The authors report no conflict of interest concerning the materials or methods used in this study or the findings reported. All authors have completed the online self-reported COI disclosure statement on the website of The Japan Neurosurgical Society.
References
- 1).North American Symptomatic Carotid Endarterectomy Trial. Methods, patient characteristics, and progress. Stroke 22: 711–720, 1991 [DOI] [PubMed] [Google Scholar]
- 2).Endarterectomy for asymptomatic carotid artery stenosis. Executive Committee for the Asymptomatic Carotid Atherosclerosis Study. JAMA 273: 1421–1428, 1995 [PubMed] [Google Scholar]
- 3).Randomised trial of endarterectomy for recently symptomatic carotid stenosis: final results of the MRC European Carotid Surgery Trial (ECST) Lancet 351: 1379–1387, 1998 [PubMed] [Google Scholar]
- 4).Halliday A, Harrison M, Hayter E, et al. : 10-year stroke prevention after successful carotid endarterectomy for asymptomatic stenosis (ACST-1): a multicentre randomised trial. Lancet 376: 1074–1084, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5).Chan RC, Chan YC, Cheung GC, Cheng SW: Predictors of restenosis after carotid endarterectomy: 17-year experience in a tertiary referral vascular center. Vasc Endovascular Surg 48: 201–206, 2014 [DOI] [PubMed] [Google Scholar]
- 6).LaMuraglia GM, Stoner MC, Brewster DC, et al. : Determinants of carotid endarterectomy anatomic durability: effects of serum lipids and lipid-lowering drugs. J Vasc Surg 41: 762–768, 2005 [DOI] [PubMed] [Google Scholar]
- 7).Lattimer CR, Burnand KG: Recurrent carotid stenosis after carotid endarterectomy. Br J Surg 84: 1206–1219, 1997 [PubMed] [Google Scholar]
- 8).Arquizan C, Trinquart L, Touboul PJ, et al. : Restenosis is more frequent after carotid stenting than after endarterectomy: the EVA-3S study. Stroke 42: 1015–1020, 2011 [DOI] [PubMed] [Google Scholar]
- 9).Avgerinos ED, Chaer RA, Naddaf A, El-Shazly OM, Marone L, Makaroun MS: Primary closure after carotid endarterectomy is not inferior to other closure techniques. J Vasc Surg 64: 678–683.e1, 2016 [DOI] [PubMed] [Google Scholar]
- 10).Bonati LH, Ederle J, McCabe DJ, et al. : Long-term risk of carotid restenosis in patients randomly assigned to endovascular treatment or endarterectomy in the Carotid and Vertebral Artery Transluminal Angioplasty Study (CAVATAS): long-term follow-up of a randomised trial. Lancet Neurol 8: 908–917, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11).Malas M, Glebova NO, Hughes SE, et al. : Effect of patching on reducing restenosis in the carotid revascularization endarterectomy versus stenting trial. Stroke 46: 757–761, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12).Paraskevas KI, Robertson V, Saratzis AN, Naylor AR: Editor’s choice - an updated systematic review and meta-analysis of outcomes following Eversion vs. conventional carotid endarterectomy in randomised controlled trials and observational studies. Eur J Vasc Endovasc Surg 55: 465–473, 2018 [DOI] [PubMed] [Google Scholar]
- 13).Park H, Kwon TW, Kwon SU, et al. : A retrospective 10-year, single-institution study of carotid endarterectomy with a focus on elderly patients. J Clin Neurol 12: 49–56, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14).Lamba N, Zenonos GA, Igami Nakassa AC, Du R, Friedlander RM: Long-term outcomes after carotid endarterectomy: the experience of an average-volume surgeon. World Neurosurg 118: e52–e58, 2018 [DOI] [PubMed] [Google Scholar]
- 15).Uno M, Suzue A, Nishi K, Nagahiro S: Hemodynamic cerebral ischemia during carotid endarterectomy evaluated by intraoperative monitoring and post-operative diffusion-weighted imaging. Neurol Res 29: 70–77, 2007 [DOI] [PubMed] [Google Scholar]
- 16).Babu MA, Meissner I, Meyer FB: The durability of carotid endarterectomy: long-term results for restenosis and stroke. Neurosurgery 72: 835–838; discussion 838–839; quiz 839, 2013 [DOI] [PubMed] [Google Scholar]
- 17).Rerkasem K, Rothwell PM: Systematic review of randomized controlled trials of patch angioplasty versus primary closure and different types of patch materials during carotid endarterectomy. Asian J Surg 34: 32–40, 2011 [DOI] [PubMed] [Google Scholar]
- 18).Al-Rawi PG, Turner CL, Waran V, Ng I, Kirkpatrick PJ: A randomized trial of synthetic patch versus direct primary closure in carotid endarterectomy. Neurosurgery 59: 822–828; discussion 828–829, 2006 [DOI] [PubMed] [Google Scholar]
- 19).Katz D, Snyder SO, Gandhi RH, et al. : Long-term follow-up for recurrent stenosis: a prospective randomized study of expanded polytetrafluoroethylene patch angioplasty versus primary closure after carotid endarterectomy. J Vasc Surg 19: 198–203; discussion 204–205, 1994 [DOI] [PubMed] [Google Scholar]
- 20).Mannheim D, Weller B, Vahadim E, Karmeli R: Carotid endarterectomy with a polyurethane patch versus primary closure: a prospective randomized study. J Vasc Surg 41: 403–407; discussion 407–408, 2005 [DOI] [PubMed] [Google Scholar]
- 21).Garzon-Muvdi T, Yang W, Rong X, et al. : Restenosis after carotid endarterectomy: insight into risk factors and modification of postoperative management. World Neurosurg 89: 159–167, 2016 [DOI] [PubMed] [Google Scholar]
- 22).Johnson CA, Tollefson DF, Olsen SB, Andersen CA, McKee-Johnson J: The natural history of early recurrent carotid artery stenosis. Am J Surg 177: 433–436, 1999 [DOI] [PubMed] [Google Scholar]
- 23).Bond R, Rerkasem K, Cuffe R, Rothwell PM: A systematic review of the associations between age and sex and the operative risks of carotid endarterectomy. Cerebrovasc Dis 20: 69–77, 2005 [DOI] [PubMed] [Google Scholar]
- 24).Reina-Gutiérrez T, Serrano-Hernando FJ, Sánchez-Hervás L, Ponce A, Vega de Ceniga M, Martín A: Recurrent carotid artery stenosis following endarterectomy: natural history and risk factors. Eur J Vasc Endovasc Surg 29: 334–341, 2005 [DOI] [PubMed] [Google Scholar]
- 25).Hugl B, Oldenburg WA, Neuhauser B, Hakaim AG: Effect of age and gender on restenosis after carotid endarterectomy. Ann Vasc Surg 20: 602–608, 2006 [DOI] [PubMed] [Google Scholar]
- 26).Kumar R, Batchelder A, Saratzis A, et al. : Restenosis after carotid interventions and its relationship with recurrent ipsilateral stroke: a systematic review and meta-analysis. Eur J Vasc Endovasc Surg 53: 766–775, 2017 [DOI] [PubMed] [Google Scholar]
- 27).Heo SH, Yoon KW, Woo SY, et al. : Editor’s choice - comparison of early outcomes and restenosis rate between carotid endarterectomy and carotid artery stenting using propensity score matching analysis. Eur J Vasc Endovasc Surg 54: 573–578, 2017 [DOI] [PubMed] [Google Scholar]