1. Introduction
The task of researching and developing novel therapeutic agents, especially in the therapeutic area of central nervous system (CNS) drugs, remains an expensive, uncertain, time-consuming, competitive, and inefficient enterprise (Safavi et al., 2016). These challenges result in a very high failure rate of CNS drug development programs and pose continuous challenges for all stakeholders involved in drug discovery, including regulators and payers alike.
One of the key issues facing current regulatory processes for CNS therapies is the complete or partial lack of tractability among current paradigms. Such disagreement is likely due to a lack of understanding in several areas: disease pathophysiology; disparities, or low informative value, between animal models and the target disease; lack of translatability of results from healthy individuals to patients; heterogeneous patient populations and complex diagnostic entities; and complications (e.g. treatment discontinuation, death) that may occur during clinical trials. Heterogeneity between patients may result in differences in response, tolerability and/or adherence to a particular treatment, both in clinical trials and real-world settings. These factors subsequently impact upon the design of clinical trials that represent the real-life population of patients (with their inclusion and exclusion criteria), the choice of informative comparators, the use of validated endpoints, tools and scales, and therefore the ability of regulators to properly evaluate novel therapies to the point of approval.
Regulatory decisions are currently based upon the results of randomized controlled trials (RCTs), within which treatment conditions are highly optimized and the patient population is strictly controlled. Consequently, RCTs may lack external validity, thus creating an efficacy-effectiveness gap, whereby drugs perform well in clinical trials (efficacy) but fail to do so in clinical practice (effectiveness) (Eichler et al., 2011). Although they will never be relevant to all patients and clinical settings, RCTs should be designed and reported in such a way that the target population is clearly identified (Rothwell, 2006; Thorpe et al., 2009). Some approaches, with the potential to reduce attrition rates, have recently been proposed; furthermore, the judicious use of clinically qualified predictive biomarkers holds great promise for further development of therapeutic targets, improved survival, and ultimately personalized medicine (Safavi et al., 2016). These biomarkers may help to identify specific populations that could benefit from a treatment within an RCT and clinical practice. For instance, measures such as attenuated mismatch negativity (Koola, 2018; Naatanen et al., 2016), brain intrinsic functional networks (Du et al., 2018), and structural network alterations (Padula et al., 2017) all hold promise for tracking individual patient progress, disease progression or modification, and pharmacological mechanisms of action. Biomarkers that can justify label claims for both registration and reimbursement are being pursued with particular vigor.
This article aims to provide an overview of the regulatory and policy issues relating to the treatment of CNS disorders, with a focus on attenuated psychosis syndrome (APS) and schizophrenia.
2. Emerging regulatory trends
“Evidence versus access,” a conundrum often faced by drug regulators, refers to the delicate balance between encouraging rapid patient access to promising therapies, whilst ensuring that there is adequate evidence regarding the benefits and harms of the therapy at the time of market authorization (Eichler et al., 2015; Woodcock, 2012). Increasingly well informed and better organized patient advocacy groups have been a driving force behind calls for drug development and market access to benefit patients in the here and now (Eichler et al., 2015). To facilitate such rapid access, however, payers (and sometimes patients) must first consider any uncertainties regarding net benefit alongside potential financial costs and the availability of alternate treatment options (Eichler et al., 2015). In response, a number of flexible licensing pathways, including accelerated approval (USA) and conditional marketing authorization/approval (EU and Japan), have been implemented or are being explored by legislators and regulatory agencies (Baird et al., 2014; Eichler et al., 2015). Such approaches are pertinent for situations whereby immediate availability of the therapy would generate public health benefits that outweigh the inherent risks of the time required for additional data to be collected (Commission Regulation, 2006). Healthcare payers have responded by adopting a range of innovative reimbursement approaches, termed “managed entry agreements (MEAs)”. MEAs help ensure rapid access to novel health technologies, whilst maintaining value and developing real-world effectiveness and valued outcomes, such as avoided costs, which can provide additional information on the relative effectiveness assessment of new products (Henshall and Schuller, 2013; Klemp et al., 2011; Pavlovic et al., 2014; Stafinski et al., 2011). Considering the increased pressure to facilitate rapid access to potentially beneficial new therapies, regulators now seem to be more open to the discussion and implementation of revisions that would aid improvement of current regulatory processes. For example, discussions leading to a better understanding of patient subgroup stratification within complex multifactorial diseases could enhance study design and outcomes during late-stage drug development. Furthermore, choice of endpoints and how they are reported have a major impact on the relative effectiveness assessment (REA) of pharmaceuticals, a component of health technology assessment (HTA) (Pavlovic et al., 2014). The EUnetHTA guidelines on endpoints for REA state that the choice of all endpoints should depend upon the particular disease, population, treatment, and decision context (Pavlovic et al., 2014). Long-term endpoints are preferred wherever adequate and feasible; however, short-term endpoints are acceptable for acute conditions; surrogate endpoints can also be used when validated against the final outcome of interest (Pavlovic et al., 2014).
There is also an emerging trend for early and ongoing dialogue between regulators and payers to avoid the issues seen with anti-hepatitis C (HCV) (AASLD-IDSA, 2017) and anti-low-density lipoprotein (LDL) monoclonal antibodies (Baum, 2017; Baum et al., 2017), in which restrictive criteria for reimbursement have limited their use in clinical practice, despite approval in a broad patient population. Dissonance between the development of novel therapies and the lack of creativity demonstrated during manufacturer-payer negotiations, may contribute to regulators authorizing a much larger patient population to be treated than payers are accepting for reimbursement. For instance, sofosbuvir, indicated for the treatment of chronic HCV mono-infection and HCV/human immunodeficiency virus-1 coinfection as part of a combination regimen, was limited to patients with advanced fibrosis or cirrhosis by the majority of payers worldwide (Barua et al., 2015).
Further interesting examples include the anti-proprotein convertase subtilisin/kexin type 9 (PCSK9) monoclonal antibodies evolocumab and alirocumab, which had US Food and Drug Administration (FDA) fast-track approval (Toklu et al., 2016). These drugs were approved as adjuncts to diet and maximally tolerated statin therapy for patients with familial hypercholesterolemia or clinical atherosclerotic cardiovascular disease, who required a greater reduction in LDL cholesterol levels. Despite the study of PCSK9 inhibitors for use in other patient subgroups, such as statin-intolerant patients in the Goal Achievement After Utilizing an Anti-PCSK9 Antibody in Statin Intolerant Subjects-3 (GAUSS-3) trial, these agents are not currently approved worldwide for other indications (Nissen et al., 2016), mainly for reimbursement reasons. These examples illustrate that even successful therapies with previously unattainable clinical effectiveness and statistically significant efficacy versus comparator, fail to achieve reimbursement for all patients due to sustainability and lack of satisfactory negotiation models. In other cases, regulators appear to have been obliged to approve drugs for use in much less well-defined populations than those in clinical trials, leading to increased variability in drug response and decreased real-world effectiveness (Eichler et al., 2011). The Massachusetts Institute of Technology's NEW Drug ParadlGmS (NEWDIGS) initiative is a multi-stakeholder collaboration, within a neutral “safe haven” environment, that aims to define what an adaptive development and licensing program to enable timely availability of innovative medicines might look like (Baird, 2013). Importantly, the initiative suggests that regulatory change will not be achieved by regulators alone, and that a safe environment for such discussions will be required for stakeholders to align regarding benefit-risk tradeoffs. For some treatments, such as gene therapy, there may also be some uncertainty about long-term durability of response, even at the time of approval, because this cannot be fully assessed in a clinical trial (Gottlieb, 2018). Indeed, the NEWDIGS FoCUS (Financing and Reimbursement of Cures in the USA) consortium suggest that precision financing approaches may be required for such durable, perhaps lifetime, therapies that incur high upfront reimbursement costs (MIT NEWDIGS FoCUS Project, 2017).
Regulators are also becoming more amenable to discussions regarding the approval of potential new target populations and indications. Patient populations in RCTs could be enriched according to the presence of biomarkers (genetic and/or phenotypic), improving the ability of regulators to license drugs for specific populations and potentially leading to improved efficacy and/or safety (Arneric et al., 2018; Eichler et al., 2011; EMA, 2010). Indeed, regulatory (FDA, 2018c) and clinical (Mobasheri et al., 2019) perspectives from other heterogeneous, multifaceted diseases with multiple causes concur that biomarkers may be employed as tools for patient stratification in clinical trials, and for more rational and targeted drug development.
Such treatments have the considerable benefit of potentially being able to modify disease progression. However, these unique approaches require researchers to apply new methodologies, such as novel biomarker strategies and unique clinical trial designs, and to consider the application of data collected from trial designs that are new to them. The key example for the purpose of this article is the prevention of first-episode psychosis in patients with APS via early intervention. This strategy is currently being investigated with the novel phosphodiesterase 9 inhibitor BI 409306 (Keefe et al., 2017). These preventative strategies are also being applied to Alzheimer's disease (AD), where research has identified the APOE and TOMM40 genetic loci as associated with the age of AD onset (Crenshaw et al., 2013). While Takeda and Zinfandel discontinued the pioglitazone program using the TOMM40 biomarker as a treatment criterion, putatively due to inadequate treatment effect (Takeda, 2018), other preventative trials are underway. Meanwhile, Biogen has initiated Phase I studies for the use of aducanumab in patients with prodromal or mild AD (NCT01677572). Moreover, regulators have proposed the use of biomarkers as tools to improve the diagnosis specificity of AD and to predict conversion from a specific amnestic disorder to full dementia status over a relatively short time period (≤2 years) (Isaac et al., 2011). Current prospective data consistently demonstrate that for patients with mild cognitive impairment, per the Peterson Criteria (less specific for AD than the Dubois Criteria), a positive cerebral spinal fluid (CSF) tau/Aβ1–42 biomarker ratio is predictive of conversion to dementia within the next 2–3 years. The relative risk for dementia is still uncertain; nevertheless, it is known to be more frequent in patients with a positive CSF biomarker ratio than those with a negative CSF biomarker ratio (Isaac et al., 2011).
These strategies are likely to open debate on the differences between disease modification and progression, and whether demonstrating disease-modifying activity is truly a requirement. Discussion around these paradigms should also consider the correlation between improvement in symptoms/functioning, normalization of the underlying biological mechanism of disease, and choice of biomarkers and trial design while considering differences between European, US, and Asian regulatory requirements. Challenges associated with disease modification must also be considered, such as trial duration, sample/effect size, the non-inferiority margin, patient withdrawal, and the subsequent effects on randomization and missing data.
3. Continuum versus spectrum disorders
AD, Parkinson's disease (PD), and many other neuropsychiatric disorders can be considered as progressive, or continuum, neurological disorders that follow a pattern of increasing severity over time (EMA, 2012; EMA, 2018). The shift toward a desire for early treatment of PD, for instance, has triggered a vast amount of research into the use of biomarkers with high positive predictive value for early population identification (EMA, 2012; Noyce et al., 2016). Regarding AD, EMA representatives consider pharmacological interventions directed to suspected pathophysiological mechanisms underlying AD at a pre-symptomatic stage to be a reasonable strategy for prevention (EMA, 2018). Similarly, FDA representatives consider patients with Stage 1 AD (no symptoms) a valid target, because in their view intervention should start as early as possible (FDA, 2018b). As such, biomarkers are gaining increasing interest as a potential basis for the accelerated assessment of such conditions.
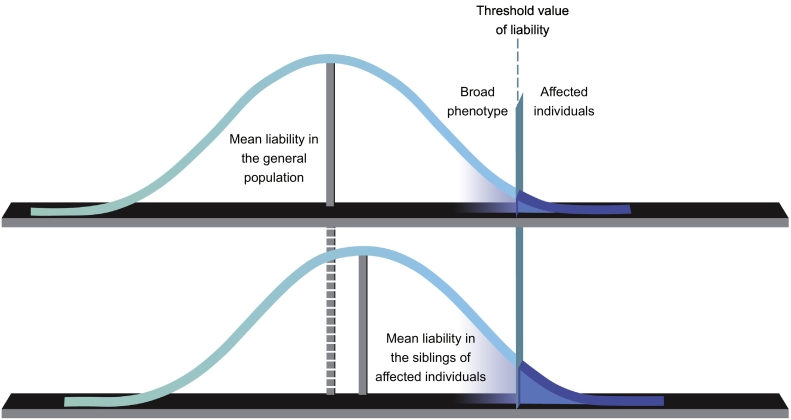
Psychiatric illnesses are also being reconceptualized, but as trans-diagnostic entities such as with the Research Domain Criteria approach (Cuthbert and Insel, 2013) that focuses on the underlying biology that manifests as specific behavior and experience. Classic diagnostic entities are also under re-examination as more genetic and biological data come to light. For example, recent opinion suggests that schizophrenia should undergo a reconceptualization of breadth to become part of the psychotic spectrum (Fig. 1) (Guloksuz and Van Os, 2018), similar to what has been established for autism spectrum disorder. This perspective would consider the clinical manifestations of schizophrenia, schizoaffective disorder, and bipolar disorder, including affective and non-affective symptoms and the five symptom dimensions (positive and negative symptoms, mania, depression and disorganization) as part of the same spectrum of illness (Guloksuz and Van Os, 2018). We agree with this approach, which will pave the way for future conceptualization (Guloksuz and Van Os, 2018) and identification of the key trans-diagnostic factors that limit function and produce suffering.
Fig. 1.
The psychotic spectrum
S. Guloksuz and J. van Os. The slow death of the concept of schizophrenia and the painful birth of the psychosis spectrum. Psychological Medicine, 2018, 48, 2, 229–244, reproduced with permission.
4. Regulatory issues: schizophrenia and APS
The reconceptualization of schizophrenia as a part of a spectrum of psychosis that includes APS raises further regulatory and reimbursement issues. APS could represent an early manifestation of schizophrenia or other psychotic disorders, with 26% of such individuals converting to psychosis within 38 months (Fusar-Poli et al., 2015). APS symptoms may also remit in ~50% of non-converters (Cannon, in press; Lam et al., 2018). Following remission, these participants may not be distinguishable from the general population. The APS population poses two challenges: (1) from a clinical perspective, it may be unethical and unjustifiable to treat these individuals and (2) payers may not reimburse treatment for such individuals. Additionally, transitory, enduring, and progressing forms of APS are difficult to differentiate from one another based solely on clinical observation. The development of new biomarkers could contribute to a more accurate differentiation and prediction of how APS will progress over time.
As the focus on prodromal conditions in regulated trials burgeons, new methods have been developed to understand the novel emergent data. When it comes to APS, the possibility of intercurrent clinical events that occur after treatment randomization is of particular relevance. These events include the occurrence of an index psychotic episode that would call for the use of a rescue medication, use of a medication prohibited by the protocol or subsequent line of therapy, discontinuation of treatment, treatment switching, or a terminal event such as death. These events will either preclude observation of the variable or affect its interpretation.
One approach for regulators trying to address these issues is the use and definition of estimands in clinical trials. This is reflected by the development of an addendum of the International Council for Harmonization of Technical Requirements for Pharmaceuticals for Human Use (ICH) E9, which covers estimands and sensitivity analyses in clinical trials (ICH R9[R1]) (ICH, 2017). ICH R9 (R1) attempts to better define what is perhaps the most important question for drug development and licensing, which seems to be of relevance in the case of APS: the quantification of treatment effects. In other terms, the use of estimands that define how a treatment outcome compares with the outcome that would have occurred in the same patients under different treatment conditions. An estimand considers whether values of the variable after an intercurrent event (that occurs after treatment initiation and precludes the observation or affects the interpretation of the variable of interest) are relevant. It also considers how to account for the (possibly treatment-related) occurrence or non-occurrence of the event itself. More formally, an estimand provides a detailed definition of what needs to be estimated in order to answer a specific trial objective. Estimations within clinical trials include: the population of interest (the patients who are eligible for inclusion); the endpoint of interest (measurements taken and the timepoint or period of interest); the specification of how to account for intercurrent events and whether these are of interest to the endpoint (early discontinuation, rescue medication, death); and the population-level summary measure (how are comparisons between treatment conditions summarized) (ICH, 2017).
These regulatory guidelines may provide great benefit to clinical trials testing the safety and efficacy of treatments for prodromal conditions. According to the guidelines, a stratum of the target population may be of interest, defined in terms of a potential intercurrent event; for example, the stratum of patients who would adhere to the treatment. With regards to APS specifically, it could be argued that because patients have high rates of spontaneous remission and non-conversion, they may be poorly adherent. On the other hand, patients may be suffering and would therefore derive value from a relieving treatment to manage any symptoms and possibly assist their daily functioning. In any case, these patients are highly deserving of treatment, and the key outcome measures for APS may consist of quantities related to clinical outcomes (e.g. time to first episode, hospitalization required, duration of hospitalization). These variables may also incorporate intercurrent events such as discontinuation of treatment, treatment taken prior to discontinuation and treatment based on composites (e.g. treatment failure defined as non-response or treatment discontinuation due to lack of efficacy and/or safety issues). Since intercurrent events can present in multiple forms, and thus affect interpretation of the variable of interest, it will be necessary to specify how to account for potential intercurrent events in a way that reflects the particular scientific question. For example, if a patient takes rescue medication in addition to the treatment of interest, the scores for the selected endpoints will reflect the combined effect of the treatment and the rescue medication. If a patient discontinues treatment because of toxicity, again the scores for the selected endpoints will reflect the lack of effect of the treatment when it is not taken.
Currently, there are no approved medications for APS, and there is no established regulatory standard for the conduct of clinical trials in this area. Research into the accurate and sensitive inclusion of individuals within clinical trials, and the conduct of such trials within the global regulatory environment, requires further consideration. Indeed, during the design of novel drug trials that will enroll patients at high risk of conversion to psychosis, several factors must be carefully considered. Firstly, treatment response should be monitored according to positive, negative, and cognitive symptom scales that have regulatory approval. The measurement of such symptoms should continue for a sufficient number of months/years, dictated by the natural history of the disorder under study, in a sufficient number of patients, to enable significant changes in a number of predetermined measurable variables (i.e. time to first episode, hospitalization required, duration of hospitalization) to be observed. For instance, should hospitalization be considered as an outcome for a study, the sample size should be large enough to support the claim that hospitalization slows (or even modifies) the progression to psychosis. Secondly, it should be considered that, although the scientific question of interest (treatment versus placebo) may be best addressed via an RCT, such trials are not always free from confounding and selection bias. Of course, RCTs are expected to be free from baseline confounding bias; however, not necessarily from post-randomization confounding and selection bias. Finally, it must also be considered that high-risk patients may not be able to adhere to treatment over an extended period of time.
5. Future considerations for APS trials and treatment
One of the most important regulatory issues in the evolution of medicine toward treatment of a prodromal state is precise patient identification. The early detection of subtle changes based on APS symptoms such as unusual perception, thought and suspiciousness, cognitive performance on symbol coding and verbal memory, changes in global functioning, and digital speech analytics may help to limit the number of false positive cases included in trials (Bedi et al., 2015; Cannon et al., 2016). Importantly, some patients with high-risk symptoms may never convert to psychosis; however, they may still experience attenuated psychotic symptoms for many years, if not decades. This group of non-remitters who do not convert comprises a large proportion of all patients with APS, and they have considerable morbidity. Moreover, high risk for psychosis has been shown to be high risk for other psychiatric issues; therefore, identification of this patient population is very important. Criteria to identify this group of patients remain poorly defined, but should aim to describe a specific time period after which non-conversion is confirmed (this time period may be of considerable duration). It may be a legitimate strategy to treat patients with these APS symptoms using a similar approach to that used in the treatment of negative symptoms or cognitive deficits in people with schizophrenia (but without the need to manage psychosis). The aim would be to reduce their suffering and to act on specific treatment targets, such as non-remission, negative symptoms, cognitive deficits, functional capacity, and social competence. Thus, a simple dichotomy of conversion to psychosis versus non-conversion may not account for the benefits of symptom reduction to these patients.
Biomarkers are emerging as potentially being of particular interest for the identification of patients with prodromal disorders who would benefit from specific interventions; however, this strategy is hampered by the complexity of schizophrenia and the diverse range of genetic and environmental factors that are associated with the condition (Goff et al., 2016). Ideally, to guide treatment, regulators would prefer biomarkers linked to a drug mechanism of action and disease neurobiology to allow a disease-modifying claim within the product label. Furthermore, the EMA has recently highlighted a need for the co-development of biomarkers alongside corresponding assays that can be successfully transitioned into clinical practice (EMA, 2017). Additional regulatory hurdles associated with prodromal states may include the measurement of positive and negative predictive values for biomarkers, the sustainability of time to event analyses and clinical meaningfulness of the event, and the use of surrogate endpoints if patients are not followed for long enough.
Digital medicine and bio-behavioral markers have the potential to identify and track patients (Dagum, 2018; Insel, 2017), and hold great promise for individuals with prodromal psychosis. For example, Bedi et al., describe a novel combination of automated semantic and syntactic speech analyses able to accurately predict conversion to psychosis in a clinical high-risk cohort; substantial additional validation is, however, required (Bedi et al., 2015). Digital tools that can be used on smartphones or tablets are of particular interest (FDA, 2018a). Such applications would allow the active measurement of cognitive function (i.e. symbol coding test) (Atkins et al., 2017) and functional capacity (Keefe et al., 2016), with the possibility of an integrated reward system to promote adherence, in addition to the more passive measurement of movement and social functioning via global positioning system (GPS). As is true for any measure, several basic psychometric and testing considerations must also be applied to digital biomarkers, including reliability, validity, practicality, and translatability. Validation and certification of digital measures will be a necessity for regulators and payers, and they will value the ability of such tools to transition from clinical trials into clinical practice. The resulting strength of such evidence could be used to direct reimbursement criteria. Of note, three areas of technology currently in development will be valuable for the detection and medium/long-term follow-up of patients with APS: (1) wearable sensors for activity monitoring (broadly speaking); (2) pattern recognition (speech, movement, behavioral); and (3) human machine interfaces capable of handling interactions between humans and devices, such as smartphones.
However, there are several challenges associated with the use of these new technologies. In particular: selecting the appropriate device for a particular endpoint; choice of device features; choice of metrics to assess sensitivity, reliability, and clinical relevance; applicability to different populations/countries; requirement for internet connectivity via Wi-Fi or Bluetooth; patient privacy, experience, training, and adherence; usability of the technology; and specific data challenges, such as volume and continuous data flow, making it difficult to determine a defined variable or endpoint. Furthermore, when capturing data from such digital devices there are the additional challenges of missing and/or unrealistic values, and the need to prepare the data for regulatory submission. Importantly, the Clinical Trials Transformation Initiative recommendations for the use of mobile technologies state that: “Any test, tool, or instrument used for data collection in a clinical trial should meet acceptable feasibility and performance characteristics such as accuracy, precision, and consistency of measurements over time, and uniformity of measurements across mobile technologies. When mobile technologies are used for data capture, they should also meet relevant technical performance specifications that relate to their ability to reliably capture, process, store, and transfer the valid data to satisfy the needs of the trial. Sponsors should have access to data quantifying the accuracy, precision, consistency, and uniformity of the technologies. This information would reasonably be provided by the mobile technology manufacturer.”
6. Conclusions
The evolving reconceptualization of schizophrenia as a psychotic spectrum disorder, along with increased focus on the prodromal stages of the disease, is placing increasing pressure on the regulatory system. APS represents one of the earliest manifestations of the psychosis spectrum, and regulators are now realizing the importance of therapies that target these initial stages. The subsequent interest in biomarkers for the identification of patients with prodromal CNS disease is extremely challenging due to the various molecular and environmental complexities involved. Moving forward, translational science should be applied to regulatory concepts and measures, with regulatory guidelines followed for the certification of such measures. Finally, digital technologies that enable active measurement of key endpoints in both clinical trials and real-world settings will shortly be available, paving the way for a new era in patient identification and monitoring.
Funding
Funding for this article was provided by Boehringer Ingelheim International GmbH. The sponsor was given the opportunity to review the manuscript for medical and scientific accuracy as well as intellectual property considerations. No financial support of any kind was given to the authors.
Disclaimer
The opinions expressed in this manuscript are the personal views of the Authors and may not be understood or quoted as being made on behalf of or reflecting the position of any of the Institutions or Companies for which they work, have worked or have collaborated with. The mention of commercial products, their sources, or their use in connection with material reported herein is not to be construed as either an actual or implied endorsement of such products to any Public Department or Health and/or Payer Services.
Disclosures
LP is a part-time employee of the Universities of Modena and Reggio Emilia, Italy and Miami, USA and acts as Chief Scientific Officer for the EDRA-LSWR Publishing Company and the Inpeco SA Total Lab Automation Company; he is also VP for Regulatory Strategy and Market Access Innovation at VeraSci and has acted as a scientific consultant for Acadia USA, Ferrer Spain, Johnson & Johnson USA, NeuroCog Trials USA, Otsuka USA, Pfizer Global USA, and PharmaMar Spain. RSEK is an employee of Duke University and in the past 3 years has received research funding from the National Institute of Mental Health and Boehringer-Ingelheim; in the past 3 years he has also received honoraria, served as a consultant, speaker, or advisory board member for AbbVie, Acadia, Aeglea, Akebia, Akili, Alkermes, Allergan, ArmaGen, Astellas, Avanir, AviNeuro/ChemRar, Axovant, Biogen, Boehringer-Ingelheim, Cerecor, CoMentis, Critical Path Institute, FORUM, Gammon Howard & Zeszotarski, Global Medical Education (GME), GW Pharmaceuticals, Intracellular Therapeutics, Janssen, Kempharm, Lundbeck, Lysogene, MedScape, Mentis Cura, Merck, Merrakris Therapetics, Minerva Neurosciences Inc., Mitsubishi, Montana State University, Monteris, Moscow Research Institute of Psychiatry, Neuralstem, Neuronix, Novartis, NY State Office of Mental Health, Orygen, Otsuka, Paradigm Testing, Percept Solutions, Pfizer, Pharm-Olam, Regenix Bio, Reviva, Roche, Sangamo, Sanofi, SOBI, Six Degrees Medical, Sunovion, Takeda, Targacept, Teague Rotenstreich Stanaland Fox & Holt, Thrombosis Research Institute, University of Moscow, University of Southern California, University of Texas Southwest Medical Center, WebMD, and Wilson Therapeutics. He receives royalties from versions of the BAC testing battery, the MATRICS Battery (BACS Symbol Coding), and the Virtual Reality Functional Capacity Assessment Tool (VRFCAT) and is a shareholder in VeraSci and Sengenix.
Acknowledgments
Editorial support in the form of initial preparation of the outline based on input from all authors, and collation and incorporation of author feedback to develop subsequent drafts, assembling figures, copy-editing and referencing was provided by Sam Halliwell, PhD of Fishawack Communications Ltd., which was funded by Boehringer Ingelheim International GmbH.
References
- AASLD-IDSA Recommendations for testing, managing, and treating hepatitis C. 2017. https://www.hcvguidelines.org/evaluate/cost [Online]. Available. (Accessed September 2018)
- Arneric S.P., Kern V.D., Stephenson D.T. Regulatory-accepted drug development tools are needed to accelerate innovative CNS disease treatments. Biochem. Pharmacol. 2018;151:291–306. doi: 10.1016/j.bcp.2018.01.043. [DOI] [PubMed] [Google Scholar]
- Atkins A.S., Tseng T., Vaughan A., Twamley E.W., Harvey P., Patterson T., Narasimhan M., Keefe R.S. Validation of the tablet-administered Brief Assessment of Cognition (BAC app) Schizophr. Res. 2017;181:100–106. doi: 10.1016/j.schres.2016.10.010. [DOI] [PubMed] [Google Scholar]
- Baird L.G.A.H.,.G. Adaptive licensing: creating a safe haven for discussions. 2013. https://newdigs.mit.edu/sites/default/files/SRA%20Sept%202013_Adaptive%20licensing_NEWDIGS%20Safe%20Haven.pdf [Online]. Available. (Accessed January 2019 2018)
- Baird L.G., Banken R., Eichler H.G., Kristensen F.B., Lee D.K., Lim J.C., Lim R., Longson C., Pezalla E., Salmonson T., Samaha D., Tunis S., Woodcock J., Hirsch G. Accelerated access to innovative medicines for patients in need. Clin. Pharmacol. Ther. 2014;96:559–571. doi: 10.1038/clpt.2014.145. [DOI] [PubMed] [Google Scholar]
- Barua S., Greenwald R., Grebely J., Dore G.J., Swan T., Taylor L.E. Restrictions for Medicaid reimbursement of sofosbuvir for the treatment of hepatitis C virus infection in the United States. Ann. Intern. Med. 2015;163:215–223. doi: 10.7326/M15-0406. [DOI] [PubMed] [Google Scholar]
- Baum S.J. PCSK9 inhibitors: a revolution in lipid lowering therapy-breaking down barriers to access. 2017. https://www.acc.org/latest-in-cardiology/articles/2017/07/20/13/30/pcsk9-inhibitors-a-revolution-in-lipid-lowering-therapy [Online]. Available. (Accessed January 2019 2018)
- Baum S.J., Toth P.P., Underberg J.A., Jellinger P., Ross J., Wilemon K.J.C.C. PCSK9 inhibitor access barriers—issues and recommendations: improving the access process for patients, clinicians and payers. 2017;40:243–254. doi: 10.1002/clc.22713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bedi G., Carrillo F., Cecchi G.A., Slezak D.F., Sigman M., Mota N.B., Ribeiro S., Javitt D.C., Copelli M., Corcoran C.M. Automated analysis of free speech predicts psychosis onset in high-risk youths. NPJ Schizophr. 2015;1 doi: 10.1038/npjschz.2015.30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cannon T.D. 2019. Delivering on the Public Health Promise of the Psychosis Risk Paradigm. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cannon T.D., Yu C., Addington J., Bearden C.E., Cadenhead K.S., Cornblatt B.A., Heinssen R., Jeffries C.D., Mathalon D.H., T.H.J.A.J.O.P., Mcglashan An individualized risk calculator for research in prodromal psychosis. 2016;173:980–988. doi: 10.1176/appi.ajp.2016.15070890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- COMMISSION REGULATION . (EC) No 507/2006. Official Journal of the European Union. European Commission; 2006. Commission regulation (EC) no 507/2006 of 29 march 2006 on the conditional marketing authorisation for medicinal products for human use falling within the scope of regulation (EC) no 726/2004 of the European Parliament and of the council. [Google Scholar]
- Crenshaw D.G., Gottschalk W.K., Lutz M.W., Grossman I., Saunders A.M., Burke J.R., Welsh-Bohmer K.A., Brannan S.K., Burns D.K., Roses A.D. Using genetics to enable studies on the prevention of Alzheimer's disease. Clin. Pharmacol. Ther. 2013;93:177–185. doi: 10.1038/clpt.2012.222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cuthbert B.N., Insel T.R. Toward the future of psychiatric diagnosis: the seven pillars of RDoC. BMC Med. 2013;11:126. doi: 10.1186/1741-7015-11-126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dagum P. Digital biomarkers of cognitive function. npj Digital Medicine. 2018;1:10. doi: 10.1038/s41746-018-0018-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Du Y., Fryer S.L., Lin D., Sui J., Yu Q., Chen J., Stuart B., Loewy R.L., Calhoun V.D., Mathalon D.H. Identifying functional network changing patterns in individuals at clinical high-risk for psychosis and patients with early illness schizophrenia: a group ICA study. Neuroimage Clin. 2018;17:335–346. doi: 10.1016/j.nicl.2017.10.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eichler H.-G., Abadie E., Breckenridge A., Flamion B., Gustafsson L.L., Leufkens H., Rowland M., Schneider C.K., Bloechl-Daum B. Bridging the efficacy–effectiveness gap: a regulator's perspective on addressing variability of drug response. Nat. Rev. Drug Discov. 2011;10:495. doi: 10.1038/nrd3501. [DOI] [PubMed] [Google Scholar]
- Eichler H.G., Baird L.G., Barker R., Bloechl-Daum B., Borlum-Kristensen F., Brown J., Chua R., Del Signore S., Dugan U., Ferguson J., Garner S., Goettsch W., Haigh J., Honig P., Hoos A., Huckle P., Kondo T., Le Cam Y., Leufkens H., Lim R., Longson C., Lumpkin M., Maraganore J., O'rourke B., Oye K., Pezalla E., Pignatti F., Raine J., Rasi G., Salmonson T., Samaha D., Schneeweiss S., Siviero P.D., Skinner M., Teagarden J.R., Tominaga T., Trusheim M.R., Tunis S., Unger T.F., Vamvakas S., Hirsch G. From adaptive licensing to adaptive pathways: delivering a flexible life-span approach to bring new drugs to patients. Clin. Pharmacol. Ther. 2015;97:234–246. doi: 10.1002/cpt.59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- EMA Reflection paper on co-development of pharmacogenomic biomarkers and assays in the context of drug development. 2010. http://www.ema.europa.eu/docs/en_GB/document_library/Scientific_guideline/2010/07/WC500094445.pdf [Online]. Available. (Accessed January 2019)
- EMA Guideline on clinical investigation of medicinal products in the treatment of Parkinson's disease. 2012. http://www.ema.europa.eu/docs/en_GB/document_library/Scientific_guideline/2012/07/WC500129601.pdf [Online]. Available. (Accessed January 2019)
- EMA Concept paper on predictive biomarker-based assay 4 development in the context of drug development and 5 lifecycle. 2017. http://www.ema.europa.eu/docs/en_GB/document_library/Scientific_guideline/2017/07/WC500232420.pdf [Online]. Available. (Accessed January 2019)
- EMA Guideline on the clinical investigation of medicines for the treatment of Alzheimer's disease. 2018. http://www.quotidianosanita.it/allegati/allegato3574949.pdf [Online]. Available. (Accessed January 2019)
- FDA Digital health. 2018. https://www.fda.gov/medicaldevices/digitalhealth/ [Online]. Available. (Accessed January 2019)
- FDA Early Alzheimer's disease: developing drugs for treatment guidance for industry. 2018. https://www.fda.gov/downloads/Drugs/GuidanceComplianceRegulatoryInformation/Guidances/UCM596728.pdf [Online]. Available. (Accessed January 2019) [DOI] [PMC free article] [PubMed]
- FDA Osteoarthritis: structural endpoints for the development of drugs, devices, and biological products for treatment guidance for industry. 2018. https://www.fda.gov/downloads/drugs/guidancecomplianceregulatoryinformation/guidances/ucm071577.pdf [Online]. Available. (Accessed January 2019)
- Fusar-Poli P., Cappucciati M., Rutigliano G., Schultze-Lutter F., Bonoldi I., Borgwardt S., Riecher-Rössler A., Addington J., Perkins D., Woods S.W. At risk or not at risk? A meta-analysis of the prognostic accuracy of psychometric interviews for psychosis prediction. World Psychiatry. 2015;14:322–332. doi: 10.1002/wps.20250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goff D.C., Romero K., Paul J., Perez-Rodriguez M.M., Crandall D., Potkin S.G. Biomarkers for drug development in early psychosis: current issues and promising directions. Eur. Neuropsychopharmacol. 2016;26:923–937. doi: 10.1016/j.euroneuro.2016.01.009. [DOI] [PubMed] [Google Scholar]
- Gottlieb S. 2018. Remarks by Commissioner Gottlieb to the Alliance for Regenerative Medicine's Annual Board Meeting. [Online]. (Accessed January 2019) [Google Scholar]
- Guloksuz S., Van Os J. The slow death of the concept of schizophrenia and the painful birth of the psychosis spectrum. Psychol. Med. 2018;48:229–244. doi: 10.1017/S0033291717001775. [DOI] [PubMed] [Google Scholar]
- Henshall C., Schuller T. Health technology assessment, value-based decision making, and innovation. Int. J. Technol. Assess. Health Care. 2013;29:353–359. doi: 10.1017/S0266462313000378. [DOI] [PubMed] [Google Scholar]
- ICH International council for harmonisation of technical requirements for pharmaceuticals for human use ICH harmonised guideline: estimands and sensitivity analysis in clinical trials E9(R1) 2017. http://www.ich.org/fileadmin/Public_Web_Site/ICH_Products/Guidelines/Efficacy/E9/E9-R1EWG_Step2_Guideline_2017_0616.pdf [Online]. Available. (Accessed January 2019)
- Insel T.R. Digital phenotyping: technology for a new science of behavior. JAMA. 2017;318:1215–1216. doi: 10.1001/jama.2017.11295. [DOI] [PubMed] [Google Scholar]
- Isaac M., Vamvakas S., Abadie E., Jonsson B., Gispen C., Pani L. Qualification opinion of novel methodologies in the predementia stage of Alzheimer's disease: cerebro-spinal-fluid related biomarkers for drugs affecting amyloid burden—regulatory considerations by European Medicines Agency focusing in improving benefit/risk in regulatory trials. Eur. Neuropsychopharmacol. 2011;21:781–788. doi: 10.1016/j.euroneuro.2011.08.003. [DOI] [PubMed] [Google Scholar]
- Keefe R.S.E., Davis V.G., Atkins A.S., Vaughan A., Patterson T., Narasimhan M., Harvey P.D. Validation of a computerized test of functional capacity. Schizophr. Res. 2016;175:90–96. doi: 10.1016/j.schres.2016.03.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keefe R., Woods S., Cannon T., Ruhrmann S., Mathalon D., Mcguire P., Fillon G., Rosenbrock H., Sand M.J.S.B. M15. Early intervention in attenuated psychosis syndrome: a phase II study evaluating efficacy, safety, and tolerability of oral BI 409306. 2017;43:S216. doi: 10.1111/eip.13083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klemp M., Fronsdal K.B., Facey K. What principles should govern the use of managed entry agreements? Int. J. Technol. Assess. Health Care. 2011;27:77–83. doi: 10.1017/S0266462310001297. [DOI] [PubMed] [Google Scholar]
- Koola M.M. Attenuated mismatch negativity in attenuated psychosis syndrome predicts psychosis: can galantamine-memantine combination prevent psychosis? Mol. Neuropsychiatry. 2018;4:71–74. doi: 10.1159/000488797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lam M., Lee J., Rapisarda A., See Y.M., Yang Z., Lee S.-A., Abdul-Rashid N.A., Kraus M., Subramaniam M., Chong S.-A.J.J.P. 2018. Longitudinal Cognitive Changes in Young Individuals at Ultrahigh Risk for Psychosis. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MIT NEWDIGS FOCUS PROJECT Existing gene therapy pipeline likely to yield dozens of approved products within five years. 2017. https://newdigs.mit.edu/sites/default/files/FoCUS_Research_Brief_2017F211v011.pdf [Online]. Available. (Accessed January 2019)
- Mobasheri A., Van Spil W.E., Budd E., Uzieliene I., Bernotiene E., Bay-Jensen A.C., Larkin J., Levesque M.C., Gualillo O., Henrotin Y. Molecular taxonomy of osteoarthritis for patient stratification, disease management and drug development: biochemical markers associated with emerging clinical phenotypes and molecular endotypes. Curr. Opin. Rheumatol. 2019;31:80–89. doi: 10.1097/BOR.0000000000000567. [DOI] [PubMed] [Google Scholar]
- Naatanen R., Todd J., Schall U. Mismatch negativity (MMN) as biomarker predicting psychosis in clinically at-risk individuals. Biol. Psychol. 2016;116:36–40. doi: 10.1016/j.biopsycho.2015.10.010. [DOI] [PubMed] [Google Scholar]
- Nissen S.E., Stroes E., Dent-Acosta R.E., Rosenson R.S., Lehman S.J., Sattar N., Preiss D., Bruckert E., Ceska R., Lepor N., Ballantyne C.M., Gouni-Berthold I., Elliott M., Brennan D.M., Wasserman S.M., Somaratne R., Scott R., Stein E.A. Efficacy and tolerability of evolocumab vs ezetimibe in patients with muscle-related statin intolerance: the GAUSS-3 randomized clinical trial. JAMA. 2016;315:1580–1590. doi: 10.1001/jama.2016.3608. [DOI] [PubMed] [Google Scholar]
- Noyce A.J., Lees A.J., Schrag A.-E. The prediagnostic phase of Parkinson's disease. J. Neurol. Neurosurg. Psychiatry. 2016;87:871–878. doi: 10.1136/jnnp-2015-311890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Padula M.C., Scariati E., Schaer M., Sandini C., Ottet M.C., Schneider M., Van De Ville D., Eliez S. Altered structural network architecture is predictive of the presence of psychotic symptoms in patients with 22q11.2 deletion syndrome. Neuroimage Clin. 2017;16:142–150. doi: 10.1016/j.nicl.2017.07.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pavlovic M., Teljeur C., Wieseler B., Klemp M., Cleemput I., Neyt M. Endpoints for relative effectiveness assessment (REA) of pharmaceuticals. Int. J. Technol. Assess. Health Care. 2014;30:508–513. doi: 10.1017/S0266462314000592. [DOI] [PubMed] [Google Scholar]
- Rothwell P.M. Factors that can affect the external validity of randomised controlled trials. PLoS Clin. Trials. 2006;1:e9. doi: 10.1371/journal.pctr.0010009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Safavi M., Sabourian R., Abdollahi M. The development of biomarkers to reduce attrition rate in drug discovery focused on oncology and central nervous system. Expert Opin. Drug Discovery. 2016;11:939–956. doi: 10.1080/17460441.2016.1217196. [DOI] [PubMed] [Google Scholar]
- Stafinski T., Menon D., Mccabe C., Philippon D.J. To fund or not to fund: development of a decision-making framework for the coverage of new health technologies. Pharmacoeconomics. 2011;29:771–780. doi: 10.2165/11539840-000000000-00000. [DOI] [PubMed] [Google Scholar]
- TAKEDA Takeda and zinfandel pharmaceuticals discontinue TOMMORROW trial following planned futility analysis. 2018. https://www.takeda.com/newsroom/newsreleases/2018/takeda-tommorrow-trial/ [Online]. Available. (Accessed January 2019)
- Thorpe K.E., Zwarenstein M., Oxman A.D., Treweek S., Furberg C.D., Altman D.G., Tunis S., Bergel E., Harvey I., Magid D.J., Chalkidou K. A pragmatic-explanatory continuum indicator summary (PRECIS): a tool to help trial designers. J. Clin. Epidemiol. 2009;62:464–475. doi: 10.1016/j.jclinepi.2008.12.011. [DOI] [PubMed] [Google Scholar]
- Toklu B., Jossed A., Giugliano Robert P. American College of Cardiology: American College of Cardiology; 2016. Current Indications, Cost, and Clinical Use of Anti-PCSK9 Monoclonal Antibodies.https://www.acc.org/latest-in-cardiology/articles/2016/05/18/14/34/current-indications-cost-and-clinical-use-of-anti-pcsk9-monoclonal-antibodies Online. Available. (Accessed January 2019) [Google Scholar]
- Woodcock J. Evidence vs. access: can twenty-first-century drug regulation refine the tradeoffs? Clin. Pharmacol. Ther. 2012;91:378–380. doi: 10.1038/clpt.2011.337. [DOI] [PubMed] [Google Scholar]