Abstract
There are many systematic reviews on social capital (SC) and various health outcomes, but each of these reviews shows one piece of the larger SC and health puzzle. The aim of this research was to systematically review systematic reviews on SC and health, in order to provide an overview of existing evidence and to identify strategies for future research. Nine databases were searched for key words that could fall under the broad umbrella of SC and health outcomes. We screened 4941 titles and abstracts and read 187 reviews before retaining 20 of them. A critical appraisal of each review was conducted. The reviews show there is good evidence to suggest that SC predicts better mental and physical health, and indicators of SC are protective against mortality. At the same time, many reviews also found numerous non-significant and negative relationships that are important to consider. It was unclear whether SC interventions for health were really improving SC, or other aspects of the social environment. Overall, this research shows that evidence on how various aspects of SC affect different health outcomes for different actors remains unclear. Intergroup and lifecourse perspectives could help clarify this link. Future research could benefit from conceptualizing the link between SC and health in a what, who, where, when, why and how framework.
Keywords: Social capital, Social cohesion, Social networks, Social identity, Lifecourse, Health, Systematic review
Highlights
-
•
Social capital predicts better health.
-
•
Other aspects of social capital should also be considered in health research.
-
•
Recommendations on how to improve social capital and health research are made.
1. Introduction
Social capital (SC) and health has been approached from various perspectives. Having more SC can be associated with better health outcomes (Moore & Kawachi, 2017; Villalonga-Olives & Kawachi, 2015), but SC can also have negative relationships with health (Villalonga-Olives & Kawachi, 2017). Various systematic reviews have synthesized empirical data concerning SC and health outcomes, but individually, these reviews show us fragments of the SC and health puzzle. A literature review recently pointed out that there is a need to reconceptualise how we approach SC and health, and used examples of existing systematic reviews to point out some gaps in the literature (Shiell, Hawe, & Kavanagh, 2018). We argue that a systematic review of systematic reviews (herein referred to as a meta-review) is necessary to have an overview of the current trends in SC and health research. This meta-review will use comprehensive search strategies tailored to understanding the different approaches to SC and health research. It will comprehensively summarize, compare, and discuss the strength of the evidence from existing systematic reviews. It will critically appraise each review, with the goal of informing the design, planning, and implementation of future SC and health research.
Contemporary SC and health research considers social cohesion and social network approaches to health (Moore & Kawachi, 2017). These approaches provide us with broad theoretical lenses through which we can conceptualize SC, though the distinction between the two is nuanced. The cohesion approach stems from Coleman (1990), who considered SC to be the level of trust and reciprocity amongst community members. He suggested that SC can exist both horizontally (on the same level) and vertically (between individuals, groups, and institutions), and that SC affects social structures. Putnam (2000) built on Coleman's perspective and showed that social trust and civic engagement were highly correlated with the success of local governments, though Putnam more emphasis on the importance of social networks and how their presence facilitated cohesion and overall cooperation between individuals and groups (Carlson & Chamberlain, 2003; Putnam, 2000; Putnam, Leonardi, & Nanetti, 1994). One of the first studies on SC and health also fell in line with the cohesion approach: Kawachi, Kennedy, Lochner, and Prothrow-Stith (1997) understood SC as the features of social organization (such as trust in others, norms of reciprocity, and civic participation) that can facilitate coordination and cooperation in a mutually beneficial way. Since then, a large proportion of public health research has focused largely on the cohesion approach (Carpiano, 2006).
Carpiano (2006) argued that sociological network approaches to SC could help understand health outcomes. The network approach stems from Bourdieu's work, which showed that individual group members could draw on their network's collective resources. For Bourdieu (1986), SC could be quantified in terms of the size of one's social network and the volume of the different capitals that belongs to each member in that network. Lin (2002, 2017) also did a considerable amount of work concerning the network approach, and stressed that SC is defined as resources that are embedded within social networks.
Contemporary SC and health research goes beyond cohesion and network approaches, and can be viewed through three complimentary lenses: dimensions, settings, and levels of SC. First, there are different dimensions of SC that fall within both cohesion and network approaches to health: cognitive, structural, bonding, bridging, and linking SC. Cognitive SC refers to the perception of trust, reciprocity, norms, and values within a community. Structural SC refers to the quantity of relationships and membership in institutions that can bring individuals and groups together (McKenzie & Harpham, 2006). Bonding SC refers to social resources that an individual can get through close networks or groups with similar socio-demographic characteristics. Bridging SC refers to resources that can be accessed from networks or groups with different characteristics. Finally, linking SC connects individuals and groups within hierarchies of power and authority (Moore & Kawachi, 2017).
Second, SC tends to take place in different settings. Three common settings for looking at SC and health are within families, in the workplace, in various neighborhood (community) contexts (Moore & Kawachi, 2017), or larger geographic areas. For example, neighborhood contexts can include a variety of institutions and organizations that are locally available, and may include a range of activities, such as neighborhood clubs, fitness groups, or religious organizations. SC can take place in more or less formalized settings (e.g., work; community), and can consist of more or less formal ties (e.g., employer-employee; friends and acquaintances) within the same settings. Virtual settings may also contribute to creating and maintaining SC, though there has been debate as to whether the internet creates conditions that truly replicate conditions for SC in real life (Best & Krueger, 2006). The setting of SC can result in different resources, thereby contributing to whether and how SC can influence health.
Third, SC has been conceptually defined and measured at the individual and group (aggregate or ecological) levels (Islam, Merlo, Kawachi, Lindström, & Gerdtham, 2006; McKenzie & Harpham, 2006). Portes (1998) argued that SC is an individual attribute (Islam et al., 2006; Portes, 1998), whereas Kawachi and Berkman (2014) argued that the distinctive feature of SC is that it is external to individuals, or an ecological characteristic. The cohesion approach views SC as more of a group property, whereas the network approach tends to view SC as something that belongs to both individuals and groups (Porta, 2015). However, the conceptualization and measurement of SC is more complex than individual and group level dichotomies. SC has been understood and measured at various levels: macro (e.g., countries), meso (e.g., neighborhoods, groups), and micro (e.g., smaller groups and individuals) (Islam et al., 2006; Macinko & Starfield, 2001). Indicators used to measure SC at each of these levels can focus on perceptions or more objective measures, and can aggregate individual responses to group levels (McKenzie & Harpham, 2006). Overall, there is a complex relationship between the dimension, setting, and level of SC, as well as the indicators chosen to measure and represent them.
This meta-review aims to give a large overview of the existing evidence concerning different types of SC and health outcomes. More specifically, the objectives of this meta-review are to: (1) systematically map and synthesize systematic reviews on SC and any health outcome; (2) differentiate between various approaches to SC and how they are mobilized in health literature; (3) identify whether some health outcomes benefit more from SC; (4) identify trends and current gaps in SC and health research; and (5) make recommendations for future research.
2. Methods
This meta-review was written in accordance with the PRISMA guidelines (Moher, Liberati, Tetzlaff, Altman, & Group, 2009). A protocol for this meta-review was registered in the PROPERO database, ID: CRD42018095243.
This meta-review included all published review articles (scoping reviews, systematic reviews, meta-analyses) concerning SC and any health outcome. Our definition of health outcomes included physical, mental, and self-rated health, as well as mortality. We included reviews that approached SC from a social network or social cohesion perspective.
We excluded overall quality of life and general wellbeing, except when measured by health indicators (e.g., health-related quality of life). We excluded reviews that focused on how SC was measured in health settings (as opposed to how SC influenced health outcomes). We also excluded dyadic social support, peer mentorship, and peer support, as they focus more on the provision of individual support and do not fall under the network or cohesion definitions in this article. We chose to exclude reviews on virtual social networks and social media, as online participation did not reflect our conceptualization of SC. The full list of inclusion and exclusion criteria is available in Supplementary Materials, Appendix A.
We searched nine databases to include a range of health related and social scientific disciplines: Medline, PsycINFO, EMBASE, PubMed, Cochrane, CINAHL, SocIndex, ERIC, and Web of Science. References from all relevant reviews were checked to find any other potential reviews to include. We contacted authors for full text when they were unavailable online. We regularly checked Google Scholar over the course of the review for other relevant articles to include, and included one review published after the search date (Villalonga-Olives, Wind, & Kawachi, 2018). An example search strategy is included in Supplementary Materials Appendix B. Search results for each database are in Appendix C.
The first author conducted the search strategy, and screened titles and abstracts against the inclusion criteria. The first, second, and third authors evaluated full text articles against the inclusion criteria, and extracted key information from 10% of the reviews into a pre-tested data extraction spreadsheet. Data extracted included information on the type of review conducted, the search strategy of the review, which databases were searched, the objectives of review, the target SC type and definition, the target health-related outcome, the review population, the total number of participants in the review, any outcome or summary measures, key results, any suggested mechanisms involved, key sources of bias, conclusions, and recommendations. The three reviewing authors established an inter-rater reliability of over 90%, and resolved any disagreements with the last author.
The analysis conducted in meta-reviews is mostly descriptive (French, Cameron, Benton, Deaton, & Harvie, 2017; Smith, Devane, Begley, & Clarke, 2011). The first and second authors used content analysis (Elo & Kyngäs, 2008) to code each column of the data extraction sheet in order to synthesize the evidence. In case of disagreement, the first two authors went back to the original sources to verify that all information was correctly interpreted, and discussed the conclusions and implications of each review. The first two authors summarized key findings and any take away messages concerning our understanding of SC and its relationship to health, and noted gaps that future research could address.
To give the reader a sense of the quality of each review, the third author did a critical appraisal of each review using the AMSTAR tool (Shea et al., 2007, 2009), as recommended by Smith et al. (2011) when conducting a meta-systematic review. The AMSTAR is for the critical appraisal of systematic reviews and meta-analyses of interventions, so the full version was used for systematic reviews of intervention studies, and an adapted version (omitting items that concerned interventions only) for systematic reviews of non-intervention studies. The full AMSTAR criteria are in the Supplementary Materials, Appendix D.
3. Results
3.1. Review characteristics
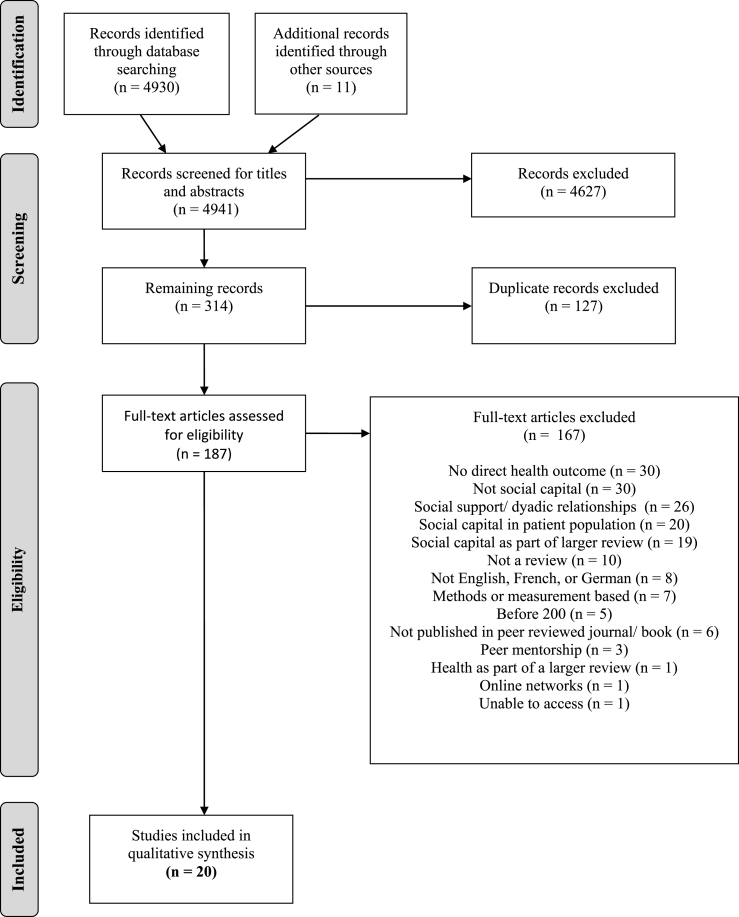
4941 titles and abstracts were screened, and 187 articles were screened for full text. Overall, 20 reviews met our inclusion criteria. A flow diagram of included reviews and the selection process is presented in Fig. 1. Almost all of the included reviews were systematic reviews, but we also included what authors self-described as a scoping review (Ransome et al., 2018) and an interdisciplinary review (Almedom, 2005), as they had comprehensive search strategies and met our inclusion criteria. Three different reviews conducted a meta-analysis in addition to their systematic review (Choi et al., 2014; Gilbert, Quinn, Goodman, Butler, & Wallace, 2013; Nyqvist, Pape, Pellfolk, Forsman, & Wahlbeck, 2014), and three of the systematic reviews focused on SC interventions (Coll-Planas et al., 2017; Flores et al., 2018; Villalonga-Olives et al., 2018). The characteristics and objectives of each review are listed in Table 1.
Fig. 1.
Flow diagram of included studies.
Table 1.
Review characteristics.
| Reference | Aim of review | Target population | Date range of included studies | Type of review | Search sources | Type of studies | Included studies |
|---|---|---|---|---|---|---|---|
| Almedom (2005) | Investigate the associations between SC and mental health | Any | Up to Dec 2003 | Interdisciplinary review | CINAHL, HealthSTAR, MEDLINE, PsycINFO, Web of Science/Knowledge | Longitudinal, cross-sectional | 12 |
| Alvarez et al. (2017) | Examine the use and measurement of family SC in the health literature | Families | Up to Sept 2015 | SR | PubMed, Sociological Abstracts, Web of Science/Knowledge | Any quantitative | 30 |
| Carlson and Chamberlain (2003) | Synthesize the empirical evidence that links SC to population health | Any | Jan 1990 to June 2002 | SR | CINAHL, PubMed, | Quantitative and qualitative | 19 |
| Choi et al. (2014) | Evaluate the effect of SC on three specific health outcomes: all-cause mortality, cardiovascular disease (CVD) and cancer | Adults | Up to Oct 2018 | Meta-analysis | EMBASE, MEDLINE, PsycINFO, | Longitudinal | 14 |
| Coll-Planas et al. (2017) | Assess the impact on health outcomes and use of health-related resources of interventions that promote SC or its components among older people | Elderly (60+) | January 1980 to July 2015 | SR | CINAHL, Cochrane Central Register of Controlled Trials, EMBASE, MedLine, PsycINFO, Web of Science/Knowledge | RCT | 73 |
| De Silva et al. (2005) | Systematically review quantitative studies examining the association between SC and mental illness | Any | Up to March 2003 | SR | CAB abstracts, Cochrane Library, C2-SPECTR, Eldis, EMBASE, HMIC, IBSS, ID21, Inter-American initiative on SC, ethics and development – document library, Lilacs, National Research register, Popline, PsychINFO, PubMed, Science and Social Science Citation Index, SERFile, SIGLE4, TRIP Database, World Bank SC document library, Zetoc | Any quantitative | 21 |
| Ehsan and De Silva (2015) | Systematically review all published quantitative studies examining the direct association between SC and common mental disorders (CMD) | Adults | Up to July 2014 | SR | Central Cochrane Database (Cochrane Database of Systematic Reviews, Cochrane Central Register of Controlled Trials) EMBASE, Global Health, IBSS, MEDLINE, PsycINFO, PubMed, SocIndex, Social Sciences, TRIP database | Longitudinal, cross-sectional | 39 |
| Flores et al. (2018) | Identify controlled studies that assess the effects of SC interventions on mental health outcomes in an adult population in any setting | Adults | Up to July 2017 | SR | CAB Abstracts, Clinical Trials Registry Platform, CENTRAL, EMBASE, EU Clinical Trials Registry, Global Health, Health Management Information Consortium, IBSS, LILACS, PsycINFO, Social Science Citation Index, Sociofile, US Clinical Trials Register, WHO International, World Bank e-library | RCT, quasi-experimental | 7 |
| Gilbert et al. (2013) | Compile the SC literature to determine whether SC has a positive relationship with health | Any | Not mentioned | Meta-analysis | Cochrane Database of Systematic Reviews, Cochrane Library, MEDLINE, PsycINFO, Sociological Abstracts, Web of Science/Knowledge | Any quantitative | 39 |
| Hu et al. (2014) | Analyze the quantitative studies that have investigated the association between SC and NCDs, and explore the role of SC in NCD prevention and control | Any | Up to July 2014 | SR | Biosis Previews, EBSCO, ELSEVIER ScienceDirect, JCR, PubMed, SCIE, Wiley Online Library | Longitudinal, cross-sectional | 17 |
| Islam et al. (2006) | Critically review the origins and different forms and dimensions of SC as it has been operationalized in the empirical literature, systematically review the empirical studies that have examined the health impact of individual and area level SC for different countries, and explore some analytical and interpretational issues that may be pertinent when assessing the health impact of area level SC | Any | Jan 1995 to June 2005 | SR | EconLit, IBSS, MEDLINE, Sociological Abstracts | Any quantitative | 42 |
| Khazaeian, Kariman, Ebadi, and Nasiri (2017) | Systematically review the impact of SC and social support on the health of female heads of households | Women- head of household | 2000 to 2015 | SR | Google Scholar, Irandoc, Iranmedex, Magiran, Scientific Information Database, PubMed, Scopus, Science Direct | Any quantative | 15 |
| McPherson et al. (2014) | Identify, analyze and synthesize primary evidence on the association between SC and mental health and behavioral problems in children and adolescents | Children and adolescents (0–18) | Jan 1990 to Apr 2012 | SR | ASSIA, CINAHL, Cochrane Database of Systematic Reviews, Cochrane Central Register of Controlled Trials, Database of Abstracts of Reviews Effects, EMBASE, MEDLINE, PsycINFO, Sociological Abstracts" | Quantitative and qualitative | 55 |
| McPherson et al. (2013) | Systematically review of the literature on the role and impact of SC on the health and wellbeing of children and adolescents | Children and adolescents (0–18) | Jan 1990 to Mar 2012 | SR | ASSIA, CINAHL, Cochrane Library, EMBASE, MEDLINE, PsycINFO, Sociological Abstracts | Longitudinal, cross-sectional, RCT, quasi-experimental | 102 |
| Murayama et al. (2012) | Review prospective multilevel analytic studies of the association between SC and health | Any | Up until Aug 2011 | SR | PubMed | Longitudinal | 13 |
| Nyqvist et al. (2014) | Clarify the link between SC and mortality by deconstructing the umbrella concept of SC into its different key aspects | Adults | Up to Sept 2009 | Meta-analysis | ASSIA, CINAHL, MEDLINE, PubMed, SocINDEX, Social Services Abstracts, SocAbst | Longitudinal | 20 |
| Ransome et al. (2018) | Identify the state of the evidence of SC and it's relationship with prevention, transmission, and treatment of HIV/AIDS outcomes in the United States | USA | 2003 to 2017 | Scoping review | EMBASE, PubMed, PsycInfo, Sociological Abstracts, Web of Science/Knowledge | Quantitative and qualitative | 13 |
| Uphoff et al. (2013) | Clarify the relationship between SC and health inequalities | Any | Up to July 2012 | SR | Cochrane library, CINAHL, EMBASE, Medline | Quantitative and qualitative | 60 |
| Villalonga-Olives and Kawachi (2017) | Search for empirical studies that have identified an association between SC and negative health outcomes | Any | Up to 2017 | SR | EMBASE, PubMed, PsycINFO | Longitudinal, cross-sectional | 44 |
| Villalonga-Olives et al. (2018) | Perform a systematic review of studies that claim to have fostered SC interventions in public health | Any | up to Jan 2018 | SR | PubMed, PsycINFO | Longitudinal, cross-sectional, RCT, quasi-experimental | 17 |
Notes: SR = Systematic Review, RCT = Randomized Control Trials.
All 20 reviews conducted searches within allied health and medically oriented databases (such as PubMed, PsycINFO, MEDLINE, EMBASE, CINAHL), and only 11 also searched in social-scientific databases (such as IBSS, Social Sciences Abstracts) (see Table 1 for detailed references). Of these, three consulted more than one social-scientific database, whereas most reviews consulted multiple medical databases. Six reviews searched within very broad databases (such Web of Science/Knowledge, Google Scholar) that included literature targeted at broad audiences. We note that the search designs were clearly geared towards medical literature, and it is possible that some of these reviews missed publications from other disciplines that were not catalogued in the medical sciences. This is particularly true for reviews that only searched one or two databases.
Every review focused on quantitative methods, though four reviews also allowed for qualitative designs in their inclusion criteria (see Table 1 for detailed references). Three reviews looked exclusively at longitudinal research and two included only experimental or quasi-experimental designs. Two reviews focused on multilevel designs. Specific inclusion criteria are useful when comparing individual studies and help establish a direction of causality, as well as the relationship between SC and specific health outcomes. However, we see that there was a preference towards quantitative methodologies, showing that it has been valorized much more than qualitative research in the SC and health literature.
Most reviews included very broad target populations, or did not specify the target population (see Table 1 for detailed references). Some reviews focused on specific ages, such as adults, children and adolescents, or older adults (60+). Reviews with more specific target populations focused on families, women who are the head of their household, or individual studies conducted in the USA. Most of the reviews included studies came from predominantly higher income countries, and were often based in the USA, the UK, or Scandinavian countries.
3.2. Social capital and health characteristics
3.2.1. Social capital characteristics
All of the reviews acknowledged the complexity in working with a heterogeneous concept such as SC (see Table 2 for detailed references). They often included everything under the umbrella of SC, ranging from scales to measure SC, to specific indicators of SC (e.g., trust). Reviews usually chose to use one or two conceptualizations of SC for their final analysis and interpretation. This generally fell in terms of dimensions (cognitive/structural, or bonding/bridging), though some studies chose to focus on levels or settings: One review looked at the measurement level of SC (individual, individual aggregated, or ecological), and three reviews looked at SC in different settings (family SC or SC in the community). It was difficult to disentangle the approaches within the studies, as there was already a large synthesis done in each review, and reviews chose to synthesize the studies differently. For example, one review took anything that could be considered SC and synthesized them under individual or group dimensions of structural or cognitive SC, based on how SC was measured. These measurements reflected how SC was operationalized as opposed to how individual studies conceptualized SC (Ehsan & De Silva, 2015).
Table 2.
Social capital conceptualizations and health outcomes.
| Reference | SC approach used to synthesize the results | SC indicators used to describe the results and show how the approach to SC is operationalized | Offered precise information on how SC was measured in each study | Key results | Overall relationship between SC and health (++, +, n.s., -) |
|---|---|---|---|---|---|
| Almedom (2005) | Cognitive and structural components of both bonding and bridging SC, on micro-(e.g. family SC) and macro-levels (e.g. community or neighborhood SC). | A broad variety of indicators used by the reviewed studies are reported. These are not grouped into SC dimensions. | Some precise information | There is consistent evidence that SC is linked to better mental health outcomes, but there are also negative relationships. The effects vary according to subgroups (low SES, minority groups, excluded groups, gender, life course) and contexts (e.g., SC can be harmful for health in disadvantaged neighborhoods). | +/− |
| Alvarez et al. (2017) | Family SC as conceptualized by cohesion and network approaches. SC dimensions are described as they are used in the reviewed studies; the authors did not re-group studies and indicators according to SC dimensions. |
Cohesion approach: Indicators for family cohesion: Collective efficacy, informal control, social interaction, sense of belonging Network approach: Indicators for family support: emotional support, instrumental support, family conflict; family network: network structure, quality of family ties. |
Precise information | There is consistent evidence that indicators of family SC in both the cohesion and network approaches were related to better health. Also, the mechanisms social influence/social control, social engagement and the exchange of social support can be related to better health. Yet, there was also evidence for non-significant relationships and the (so far still underexplored) negative impact of SC via mechanisms such as family conflict (e.g., conflicting goals or excessive demands), negative social support, and social influence. | ++/n.s./- |
| Carlson and Chamberlain (2003) | Broad category of community-level SC as conceptualized by Coleman and Putman; individual or geographic attributes, single or multi-level. | A variety of indicators are taken into account. The focus lies on perceptions of trust and social participation. | Some precise information | Most of the reviewed studies point to an association of SC and health, but the authors state that interpretation of the results is problematic due to a lack of conceptual and methodological development in the reviewed studies. There is also evidence for variations in the relationship between SC and health due to subgroups (black/white) and low/high income regions, but the mechanisms remain unclear. | + |
| Choi et al. (2014) | Seven dimensions of SC that are assessed at an individual- or area-level. These were adapted from the UK National Office for Statistics. | Seven dimensions of SC: Social participation, social network, civic participation, social support, trust, norm of reciprocity, sense of community. | Precise information | Looking at all levels, the results indicate lower mortality rates for higher levels of trust, social participation and civic participation. There were non-significant relations for social support, norm of reciprocity, sense of community and social networks. | I–S: +/n.s. I–C: +/n.s. |
| Coll-Planas et al. (2017) | Cognitive and structural components of SC at individual and community levels, bonding, bridging, linking SC, existing SC (relationships), and new SC (new relationships). | A broad variety of different indicators are assessed and are linked to SC dimensions. Indicators belong to the following categories: Social support, social participation, social network, trust and social cohesion. |
Some precise information | Although the majority of intervention studies failed to show a significant improvement of health outcomes, there is evidence for positive effects when considering low-risk-of bias studies and specific populations. | +/n.s./- |
| De Silva et al. (2005) | Cognitive and structural SC at both individual and ecological levels. | A broad variety of indicators that are used by the reviewed studies are reported. These are classified into either cognitive or structural SCs that can be assessed on either an individual or ecological level. Examples for cognitive indicators: Trust, social cohesion, sense of community. Examples for structural indicators: Group-membership, social participation. |
Some precise information | There is evidence that both cognitive and structural SCs are protective against the development of mental disorders at the individual level, but evidence is lacking or inconsistent on an ecological level. | I–C: ++ I–S: + I-mixed: + E-C: n.s. E-S: n.s./- E-mixed: +/n.s./- |
| Ehsan and De Silva (2015) | Cognitive and structural SC at both individual and ecological levels. | A broad variety of indicators that are used by the reviewed studies are reported. These are classified into either cognitive or structural SCs that can be assessed on either an individual or ecological level. Cognitive indicators: Trust, social cohesion, perceived social support, sense of community. Structural indicators: Group-membership, engagement in public affairs, actual social support, community networks |
Some precise information | Cognitive indicators of SC seem to be protective against the development of common mental disorder both on an individual and ecological level, whereas structural indicators point to no or mixed associations, with some evidence of negative associations in low resource settings. | I–C: ++ I–S: n.s./- E-C: ++; E-S: +/n.s./- |
| Flores et al. (2018) | Cognitive and structural SC or proxy indicators for these dimensions, both on an individual and ecological level. | A broad range of indicators are reported. Results are reported in an aggregated way according to the broader SC dimensions. Examples for structural indicators as given by the authors: group-memberships, social participation, social networks. Examples for cognitive indicators: group identification, social connectedness, and sense of community. | Precise information | Although most interventions improved health outcomes, evidence is inconsistent as to whether or not SC is improved. There is not enough evidence showing that an improvement in health outcomes is due to improvements in SC through the interventions. | I–C: +/n.s. I–S: +/n.s. E-mixed: + |
| Gilbert et al. (2013) | Different constructs of SC at either the individual level, the group/ecological level, or multi-level. | 102 measures were classified into constructs of SC: Participation, trust, efficacy, sense of community, social support, social networks, bonding (e.g., participation, trust, reciprocity), bridging (e.g. social networks, political or electoral participation), linking (e.g., voting and trust in legal, political, or government institutions), or combined (SC indices). | No precise information | The relationship between SC and health is on average positive; a one unit increase in SC is related to a 27% increase to be in good health (OR = 1.27; self-reported health: OR = 1.29, survival: OR = 1.17). Yet, there is significant heterogeneity that points to numerous negative and non-significant relationships. Results seem to vary due to the different constructs of SC, levels and countries, however, none of these heterogeneity tests reached significance. | ++/n.s./- |
| Hu et al. (2014) | Cognitive and structural SC on an individual or ecological level. | A broad range of indicators were assessed. Example indicators for cognitive SC given by the authors: trust, fairness, help, support, reciprocity; for structural SC: membership, participation, voting or election, homeownership, and crime rates. | Some precise information | There was good evidence that both cognitive and structural indicators (mixed levels) and individual- and ecological-level indicators (mixed dimensions of SC) were associated with less illness. However, there were also numerous non-significant relationships. There was consistent good evidence for SC as a protective factor against CVD (most strongly at the ecological level and for structural SC), diabetes (especially for cognitive SC), cancer (especially for structural SC) and no evidence in the few studies that investigated COPD. | I-mixed: +/n.s./- (CVD, diabetes) E-mixed: +/n.s. (CVD:++; cancer, diabetes: +; COPD: n.s.) C: +/n.s./- (CVD, diabetes) S: ++/n.s. (CVD, cancer; diabetes: n.s.) CVD: + Diabetes: + COPD: n.s. |
| Islam et al. (2006) | Individual level SC, aggregated SC (individual responses aggregated), or contextual SC, including multi-level. | A broad range of individual indicators and contextual indicators are taken into consideration when results are reported. These are grouped according to levels and study designs. The authors state, however, that most of their reviewed studies operationalized SC as a combination of both cognitive (particularly, trust and reciprocity) and structural (informal participation or civic engagement) dimensions, and at an area level, most studies used aggregated responses. | Precise information | There is strong evidence for a positive relationship between SC and health or survival at both individual and ecological levels. The positive association between SC and health varies between countries and is stronger in less egalitarian countries. Cross-level interactions indicate that living in an area with high SC is more strongly associated with health in less egalitarian countries. | Single-level mixed: ++ Multi-level mixed: ++ With moderators: ++/n.s./- |
| Khazaeian et al. (2017) | SC as one whole concept | Indicators for SC are not exhaustively listed. In the description of the results, the authors report results for three indicators: Trust, sense of belonging and social participation. | Some precise information | There is evidence for a positive relationship between the SC and the health of female heads of households. | I–C: + I–S: + |
| McPherson et al. (2014) | Family and community SC. | Indicators of family SC: Family structure, quality of parent-child relations, adult interest in the child, parent's monitoring of the child, extended family support and exchange. social support networks Indicators of community SC: civic engagement in local institutions, trust and safety, religiosity, quality of the school, quality of the neighborhood. Other indicators were classified as “other family or community SC” or “composite SC”. | Some precise information | Family SC (most consistent evidence for parent-child relationships and extended family relationships) and community SC (most consistent evidence for both children's and parent's quality and quantity of social support networks, quality of school and neighborhood) is related to better mental health and fewer behavioral problems. However, there were also a number of non-significant and negative relationships. There is evidence that this association is stronger in affluent and low-violence neighborhoods and for children at schools in urban compared to rural communities. | I-mixed: +, n.s., - E-mixed: +, n.s., - |
| McPherson et al. (2013) | Family and community SC | Indicators of family SC: Family structure, quality of parent-child relations, adult interest in the child, parent's monitoring of the child, extended family support and exchange. social support networks Indicators of community SC: civic engagement in local institutions, trust and safety, religiosity, quality of the school, quality of the neighborhood. Other indicators were classified as “other family or community SC” or “composite SC”. | Some precise information | There was good evidence that family (most consistent evidence for parent-child-relations and relations with other family members) and community SC (most consistent evidence for quality and quantity of social support networks of children and their families, civic engagement, group activities, quality of school and neighborhood) is related to better mental health and fewer behavioral problems. Yet, here were also a number of non-significant and negative relationships. Variations are observed due to e.g. ineffective coping- networks or increase health-risk-behaviour in support networks, living in urban compared to rural regions, belonging to minority groups, living in one compared to two-parents-households, being female and younger versus older adolescents. | I-mixed: +, n.s., - E-mixed: +, n.s., - |
| Murayama et al. (2012) | Multi-level SC comprising community, workplace (ecological level, aggregated or contextual indices), and individual-level SC. SC dimensions or indicators are described as they are used in the reviewed studies, but the authors did not group the reviewed studies according to SC dimensions. | A broad range of indicators were assessed. Frequently used indicators for community- or workplace level SC: Trust and civic participation (aggregated variables); voter turnout (contextual indicator) |
Some precise information | Evidence from prospective multilevel studies indicates that both individual and ecological level (community and workplace) SC can have positive effects on different health outcomes, although there were also a number of non-significant relationships. | All cause-mortality: +/n.s./- Suicide: +/n.s. Alcohol-related mortality: + Cancer-related mortality: + Hospitalization: for CHD, psychosis: +, for depression: n.s. Depression: +/n.s. Self-rated-health: + |
| Nyqvist et al. (2014) | Cognitive and structural SC. |
Indicators of cognitive SC: social support, trust. Indicators of structural SC: social participation, social networks. |
Some precise information | Longitudinal studies provide evidence for a positive relationship between higher individual-level-structural SC and length of life. This was most pronounced regarding the structural SC indicator social participation, followed by social networks. There was some evidence regarding the cognitive SC indicators of trust, and no evidence regarding social support. | I–C: + I–S: ++ With moderators (age and gender): attenuated |
| Ransome et al. (2018) | SC as one whole on individual or ecological levels. | Indicators of SC: Social/civic participation, social trust, social cohesion, social support, collective efficacy, social control; or composite indices. | Some precise information | A protective effect of SC against HIV could be found in 58% of the studies, whereas there were also numerous associations pointing to a negative impact of SC on HIV or no relationships. Different indicators of SC were either associated with higher or lower diagnoses rates or HIV care, which might be explained by confounding variables such as social segregation and social conditions. | +/n.s./- |
| Uphoff et al. (2013) | Cognitive, structural, bonding, bridging, and linking SC as individual or contextual SC (area-/community-level), including multi-level. Results are further grouped according to functions that SC can have in the relationship between socioeconomic status and health. | A broad variety of indicators that are used by the reviewed studies are reported, but it is not clear how the authors grouped specific indicators into the dimensions. Example indicators: friendship, trust, religious participation. | No precise information | There was a general positive relationship between SC, socioeconomic status and health, when SC was measured on an individual level. When SC was measured on the contextual level, this relationship was non-significant. Regarding bonding SC, there was consistent (individual level) and some (ecological level) evidence that the positive relationship with health was more pronounced in low-SES- and minority groups (buffer effect). For bridging and linking SC, there was some evidence that the positive relationship with health was more pronounced in high-SES compared to low-SES and minority groups (dependency effect). Also, these SCs were negatively related to health for low-SES and minority groups, especially if the latter lived in areas with high bridging and linking contextual SC. | I: ++ E: n.s. With moderators: I–C, I–S: +/n.s./- E-C, E-S: +/n.s./- |
| Villalonga-Olives and Kawachi (2017) | SC as a broad category that includes individual, community and multiple levels. SC dimensions or indicators are described as they are used in the reviewed studies. The authors group studies according to the negative functions of SC. In the discussion they summarize results for community, bonding, and bridging SC. | A broad variety of indicators used by the reviewed studies are reported. These indicators present both specific items, scales, and constructs (e.g., trust, community participation), as well as broader dimensions of SC (e.g., cognitive, structural, bonding, bridging, linking). | Some precise information | There is evidence that high bonding SC (especially in the presence of low bridging SC) can be related to lower health outcomes. Community SC can be positively or negatively related to health depending on specific subgroups or contexts (e.g., gender, young age, negative relationship for low-trusting individuals in regions with high community SC). Mechanisms explaining the negative relationships might be related to exclusion of outsiders, excess claims on group members, restrictions on individual freedoms, downward leveling norms, social contagion and cross-level interactions between social cohesion and individual characteristics. | C: S: −/+ |
| Villalonga-Olives et al. (2018) | SC as a broad category that includes individual, community and multiple levels. SC dimensions or indicators are described as they are used in the reviewed studies. The authors did not group the reviewed studies according to SC dimensions. Instead, they focus on the level and the function of SC (as a target and/or channel, or segmentation variable in interventions). |
A broad variety of indicators used by the reviewed studies are reported. These indicators present both specific items, scales, and constructs (e.g., trust, community participation), as well as broader dimensions of SC (e.g., cognitive, structural, bonding, bridging, linking). | Some precise information | 8 out of 9 manuscripts show a positive effect on SC and/or the health outcomes evaluated after the intervention. Yet, it is often not tested whether an improvement in health is due to an improvement in SC. | + |
Notes: When only indicators of SC were presented in the results (e.g., trust), we re-classified these into “cognitive” or “structural” dimensions at either the individual or ecological level in order to more easily compare results across reviews.I–C (individual level cognitive); I–S (individual structural); I-mixed (individual mixed SC); E-C (ecological cognitive); E-S (ecological structural); E-mixed (ecological mixed SC); no indication = mixed SC.
++ → strong evidence that SC is associated with better health/less illness; + → some evidence that SC is associated with better health/less illness; - → evidence that SC is associated with worse health outcomes/more illness; n.s. → non-significant findings.
3.3.2. Health characteristics
Many reviews included broad health outcomes (see Table 3 for detailed references). Eight reviews included a range of both physical and mental health indicators, six reviews focused on mental health (e.g., depression or anxiety disorders), and six reviews focused on physical health. The outcome variables of the reviews ranged from: general health indicators (general health-indices or self-rated health), mental health, and physical health, which included cardiovascular diseases, hypertension, obesity, diabetes, chronic respiratory diseases, all-cause mortality, cancer, HIV/AIDS, and sexually transmitted infections.
Table 3.
Target health outcomes.
| Reference | Target health outcomes | Documented reliable and valid health measures? | Mental (M) and/or Physical (P) health | Subjective (S) and/or more objective (O) health measures |
|---|---|---|---|---|
| Almedom (2005) | Mental disorders and mental ill-health | Yes | M | S & O |
| Alvarez et al. (2017) | Self-rated health, psychosomatic health, mental health, depression, global health ratings, drug use, developmental skills, robust mental health | No | M & P | S |
| Carlson and Chamberlain (2003) | Self-rated health, mortality | No | P | S & O |
| Choi et al. (2014) | All-cause mortality, cardio-vascular disease, cancer | No | P | O |
| Coll-Planas et al. (2017) | Self-perceived health, depression, anxiety, mortality General health, physical health, mental health | Yes | M & P | S & O |
| De Silva et al. (2005) | Mental disorder | Yes | M | S |
| Ehsan and De Silva (2015) | Common mental disorder | Yes | M | S & O |
| Flores et al., (2018) | Mental or behavioral disorder, depressive and anxiety symptoms, mental wellbeing, self-rated mental health | Yes | M | S |
| Gilbert et al. (2013) | Self-rated health, all-cause mortality | No | P | S & O |
| Hu et al. (2014) | Cardiovascular diseases (CVD), cancers, chronic respiratory diseases (COPD), diabetes | Yes | P | O |
| Islam et al. (2006) | Mortality, any health status: self-rated health, chronic health conditions, STDs, HIV/AIDS, BMI, psychiatric morbidity, psychological distress, CHD | No | M & P | S & O |
| Khazaeian et al. (2017) | Mental and physical health (e.g., general health, depression, social health) | Yes | M & P | S |
| McPherson et al. (2014) | Mental and behavioral health (self esteem, internalizing behaviors, e.g., depression/anxiety, externalizing behaviors, e.g., aggression) | No | M | S |
| McPherson et al. (2013) | Mental health and wellbeing (e.g., depression, anxiety, stress, developmental and behavioral problems, psychological and social wellbeing) | No | M | S |
| Murayama et al. (2012) | Mortality, self-rated health, depression, hospitalizations | No | M & P | S & O |
| Nyqvist et al. (2014) | All-cause mortality | No | P | O |
| Ransome et al. (2018) | HIV/AIDS (diagnosis, treatment, incident in population, perceived risk mediators) | Yes | P | S & O |
| Uphoff et al. (2013) | Self-rated health (most frequently), premature mortality, hypertension, obesity, symptoms of mental illness, mental disorders, smoking and substance abuse, longstanding illness | No | M & P | S & O |
| Villalonga-Olives and Kawachi (2017) | Broad range of health outcomes (e.g., self-rated health, mental health, depression, drug use, health-care use, use of psychiatric medication, physical health) | No | M & P | S & O |
| Villalonga-Olives et al. (2018) | Broad range of health outcomes (e.g., self-rated health, health-related quality of life, depressive, anxiety and posttraumatic symptoms, depressive or anxiolytic treatment, use of health services, physical and psychological functioning, bone densitometry) | No | M & P | S & O |
Notes: I–C (individual level cognitive); I–S (individual structural); I-mixed (individual mixed SC); E-C (ecological cognitive); E-S (ecological structural); E-mixed (ecological mixed SC); no indication = mixed SC.
++ → strong evidence that SC is associated with better health/less illness; + → some evidence that SC is associated with better health/less illness; - → evidence that SC is associated with worse health outcomes/more illness; n.s. → non-significant findings.
Most of the reviews mixed both subjective (e.g., self-rated health) and more objective measures (e.g., mortality) of health (see Table 3 for detailed references). Many also used measures of both health (positive orientation) and illness (negative orientation). Eight of the studies provided exact information on the scales that were used to measure different health outcomes, and whether these scales were reliable and validated.
3.3. The relationship between social capital and health
There is good evidence that on average, the relationship between SC and health is positive (see Table 2 for detailed references). Based on the type of SC, nine reviews provided strong, and 16 provided weak to moderate evidence that SC is positively related to health. The evidence for positive relationships outweighed the negative and non-significant relationships, but 14 reviews did show that individual studies also found non-significant relationships, and 13 reviews found some evidence of negative relationships between SC and health. One review focused on studies with a negative relationship between SC and health. Even though many reviews pointed to strong or moderate relationships between SC and health, we found that few studies were able to convincingly disentangle how SC affected different types of health outcomes. Table 2 summarizes how SC was approached in each review, and the relationship found between SC and health.
3.3.1. Dimensions of social capital
Some reviews showed that the dimension of SC makes a difference for health, but evidence was mixed. This was true for all dimensions of SC. For example, one review showed that for disadvantaged individuals, bonding SC improved health, whereas bridging and structural SCs were associated with worse health outcomes (Uphoff, Pickett, Cabieses, Small, & Wright, 2013). On the other hand, another review showed that bonding SC predicted worse health, whereas bridging SC predicted better health (Villalonga-Olives & Kawachi, 2017). Two reviews examining the relationship between SC and mental health found stronger evidence for the protective attributes of cognitive compared to structural SC (De Silva, McKenzie, Harpham, & Huttly, 2005; Ehsan & De Silva, 2015), whereas another review provided evidence that structural SC was more protective against mortality and cardiovascular diseases than cognitive SC (Hu et al., 2014).
It is important to consider the indicators used to measure different dimensions of SC, as they could affect the findings concerning SC and health. A summary of indicators used in the individual studies considered in each review is noted in Table 2. Some reviews reported a variation of findings based on different measures of structural SC (Choi et al., 2014; Gilbert et al., 2013; Nyqvist et al., 2014; Ransome et al., 2018) and cognitive SC (Choi et al., 2014; Gilbert et al., 2013). Three of the reviews conducted a meta-analysis that looked at precise indicators of SC and either mortality and/or self-rated health. All three found some evidence that indicators of SC were protective against mortality (Choi et al., 2014; Gilbert et al., 2013; Nyqvist et al., 2014). For example, a meta-analysis found that there were slightly positive effects for indicators of trust (mainly measured at the individual level) and social and civic participation (mainly measured at the ecological level), but they did not find any effects for other indicators of SC (i.e., perceived social support, norm of reciprocity, sense of community, or social networks) (Choi et al., 2014). Another meta-analysis found that social participation was protective against mortality, and that the link between social participation and health did not vary by gender or age. They also found that social networks predicted mortality, but this effect was less strong and did vary by age: it was not significant for older adults (Nyqvist et al., 2014). A third meta-analysis found an association between SC and mortality, and an even stronger positive relationship between SC and self-rated health. They noted that trust and reciprocity increased the likelihood of reporting good health more strongly than some structural or network approach indicators such as social participation, bridging, or linking SC (Gilbert et al., 2013).
3.3.2. Settings for social capital
The setting and larger context (including specific populations) are also important factors to consider in the relationship between SC and health. A review of multilevel studies found that the relationship between SC and a variety of physical and mental health indicators was higher in studies that were conducted in the USA and most European countries, but weaker in Canada, Australia, and Finland. The same review showed that living in a neighborhood with high SC was more strongly related to better health outcomes in less egalitarian countries (such as the USA) compared to more egalitarian countries (such as Canada) (Islam et al., 2006). Another review observed that the relationship between SC and self-rated health was more prominent in studies conducted in the USA, and that this relationship tended to diminish when comparing multiple countries (Gilbert et al., 2013). SC might act as a buffer in contexts with more inequality, and country-level effects could be important to consider in the relationship between SC and health.
Additionally, different actors (individuals and groups) may experience settings, and subsequently SC, differently from one another. One review showed that bonding SC functioned as a buffer for socially disadvantaged groups, whereas bridging and linking SC were only associated with better health for more advantaged groups. Higher group-level bridging SC seemed to promote exclusion and worse health outcomes for minorities (Uphoff et al., 2013). In this line, two reviews on the relationship between children and adolescents' SC and their mental health provided evidence that children and their mother's social support networks were only beneficial for children living in affluent and non-violent neighborhoods (compared to children living in poor neighborhoods with high degrees of violence) (McPherson et al., 2013, 2014). These differences show us that the relationship between SC and health can vary based on which groups individuals belong to, and whether these groups are marginalized or not.
3.3.3. Levels of social capital
The level at which SC is measured should be taken into account. Some of the reviews distinguished between individual and group levels of SC (De Silva et al., 2005; Ehsan & De Silva, 2015; Flores et al., 2018; Hu et al., 2014; Islam et al., 2006). Some found strong relationships at the individual level (De Silva et al., 2005; Ehsan & De Silva, 2015; Uphoff et al., 2013) and mixed evidence for group level SC and mental health (De Silva et al., 2005; Ehsan & De Silva, 2015). A meta-analysis provided some evidence that the relationship between SC and self-rated health was weakest in studies that used multi-level modeling (accounting for individuals nested within group level units), higher in studies that only looked at the individual level, and highest studies that only looked at the group level (Gilbert et al., 2013). Another review looking at cardiovascular diseases, cancer, chronic respiratory diseases, and diabetes found mixed evidence on both levels (Hu et al., 2014). Cross-level interactions also seem to be important: one review noted that individuals who have low trust might have detrimental health consequences in contexts with high-community or country-level trust. (Villalonga-Olives & Kawachi, 2017). The degree of egalitarianism and where individuals live within a country also interacts with how important SC is for health (Islam et al., 2006).
This evidence shows that it is important to simultaneously account for individuals and the larger groups to which they belong. However, based on the scale taken, these groups can refer to neighborhoods, towns, states, countries, or others. All of these settings and levels occur in concurrence but were rarely acknowledged as such in the reviews. Findings concerning SC and health can paint very different pictures based on where geographic or group lines are drawn. Therefore, the reference area or group should be carefully considered when conducting research and interpreting findings. This is particularly true for studies that use aggregated data to measure SC at the group level.
3.4. Social capital interventions for health
Three of the reviews focused on intervention studies only (Coll-Planas et al., 2017; Flores et al., 2018; Villalonga-Olives et al., 2018). One review focused on randomized control trials looking at a range of mental and physical health outcomes in older adults (Coll-Planas et al., 2017). Another looked at randomized and quasi-experimental designs for mental health in any population (Flores et al., 2018), and the most recent looked at a range of designs (quasi-experimental, cross-sectional, and qualitative studies) targeting both mental and physical health outcomes for any population (Villalonga-Olives et al., 2018). What constituted a SC intervention varied in each review: one aimed at increasing cognitive and structural components of individual SC (Flores et al., 2018), one looked at cognitive and bonding SC (Coll-Planas et al., 2017), and one included various dimensions of SC (cognitive, structural, bridging, bonding, and linking) (Villalonga-Olives et al., 2018). Target populations within intervention reviews were broad, and intervention components of the selected studies varied greatly. Moreover, most of the reviewed interventions were conducted in individual or group settings. Few interventions were community-based, and only some looked at outcomes on multiple levels (Villalonga-Olives et al., 2018). The SC components and health outcomes were mostly measured at the individual level rather than the group or community level. The majority of interventions on SC for health have targeted individuals rather than groups or larger communities.
Two reviews on any population found moderate to strong evidence of a positive effect on the inventions and health (Flores et al., 2018; Villalonga-Olives et al., 2018), and the one focused on elderly individuals found the results were mixed and sometimes worse for health (Coll-Planas et al., 2017). This review reported that SC interventions were more effective in vulnerable populations (e.g., elderly individuals in nursing homes). The same review observed evidence for possible mediators between SC and health, such as the improvement of physical functions, psychological variables, and slight indications for behavioral and instrumental changes (Coll-Planas et al., 2017). Another review distinguished between interventions that directly and indirectly targeted SC, for example through the introduction of specific activities (SC as a mediator), or that targeted SC for specific groups or populations (SC as a moderator). They identified a significant gap regarding studies that look at SC as a moderator (Villalonga-Olives et al., 2018).
It was unclear whether the interventions themselves increased SC: Two reviews found mixed evidence (Coll-Planas et al., 2017; Flores et al., 2018), and another one found little evidence (Villalonga-Olives et al., 2018) that the included interventions also increased SC components. It was difficult to assess whether an increase in health outcomes was due to an increase in SC, which is necessary to understand whether and how SC interventions can improve health (Coll-Planas et al., 2017; Flores et al., 2018; Villalonga-Olives et al., 2018). Two reviews noted that unintended consequences of these interventions, as well as the possibility that they occur in specific population sub-groups, were understudied (Coll-Planas et al., 2017; Villalonga-Olives et al., 2018).
3.5. Critical appraisal of included reviews
We conducted a critical appraisal of included reviews based on the AMSTAR criteria (Shea et al., 2007, 2009) in order to give readers more information on the transparency of each review. We noted that certain criteria were met systematically more or less often in the reviews. For example, no reviews reported sources of funding for included studies (item 10), but only one review did not meet the minimum criteria for a comprehensive literature search strategy, because they only searched one database (item 4) (Murayama, Fujiwara, & Kawachi, 2012). Overall, we see that most of the reviews fulfill most of the necessary AMSTAR criteria, but that some reviews documented more information than others in their manuscripts. In many cases, not meeting the criteria was due to the fact that there was no mention of the element in the review, or it was not stated explicitly enough for the reader to understand. This occurred several times for whether data extraction was conducted in duplicate (item 6), and reporting conflicts of interest (item 16). These differences may be due to the subject (e.g., reporting on sources of funding of individual studies may be less important for reviews on SC and health than for reviews of pharmaceutical intervention studies). They could also be due to guidelines for publishing systematic reviews when the review was published, word limitations, or different standards of reporting in different journals. Table 4 shows the critical appraisal of the systematic reviews according to relevant items (omitting items that were only relevant to intervention studies), and Table 5 shows the results of the systematic reviews of intervention studies in relation to all of the AMSTAR criteria.
Table 4.
Critical appraisal of systematic reviews of non-intervention studies based off AMSTAR (Shea et al., 2007).
| 2 | 4 | 5 | 6 | 7 | 10 | 14 | 15 | 16 | |
|---|---|---|---|---|---|---|---|---|---|
| Alvarez et al. (2017) | – | + | – | – | – | – | ++ | – | |
| Almedom (2005) | – | + | ++ | ++ | – | – | ++ | – | |
| Carlson and Chamberlain (2003) | – | + | – | – | – | – | – | – | |
| Choi et al. (2014) | + | + | ++ | – | ++ | – | ++ | ++ | ++ |
| De Silva et al. (2005) | + | + | ++ | ++ | ++ | – | ++ | ++ | |
| Ehsan and De Silva (2015) | + | + | ++ | – | ++ | – | ++ | ++ | |
| Gilbert et al. (2013) | + | + | ++ | – | – | – | ++ | ++ | – |
| Hu et al. (2014) | + | + | ++ | ++ | + | – | ++ | – | |
| Islam et al. (2006) | – | + | – | ++ | – | – | – | – | |
| Khazaeian et al. (2017) | – | + | ++ | ++ | + | – | ++ | ++ | |
| McPherson et al. (2014) | + | + | ++ | ++ | + | – | ++ | ++ | |
| McPherson et al. (2013) | + | + | ++ | ++ | + | – | ++ | ++ | |
| Murayama et al. (2012) | – | – | – | ++ | – | – | – | ++ | |
| Nyqvist et al. (2014) | + | + | ++ | – | + | – | ++ | ++ | ++ |
| Ransome et al. (2018) | – | + | ++ | ++ | ++ | – | ++ | – | |
| Uphoff et al. (2013) | ++ | ++ | ++ | ++ | ++ | – | ++ | ++ | |
| Villalonga-Olives and Kawachi (2017) | – | + | ++ | ++ | + | – | – | – |
Notes: ++ yes; + partial yes; - no; empty space is not applicable. AMSTAR questions are listed in supplementary materials, Appendix D.
Table 5.
Critical appraisal of systematic reviews of interventions based off AMSTAR (Shea et al., 2007).
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Coll-Planas et al. (2017) | ++ | ++ | ++ | ++ | ++ | ++ | + | ++ | ++ | – | ++ | ++ | ++ | |||
| Flores et al. (2018) | ++ | + | – | ++ | ++ | – | + | + | + | – | ++ | ++ | ++ | |||
| Villalonga-Olives et al. (2018) | ++ | – | – | + | ++ | – | + | + | – | – | ++ | – | – |
Notes: ++ yes; + partial yes; - no; empty space is not applicable. AMSTAR questions are listed in supplementary materials, Appendix D.
3.6. Sources of bias from reviews
The reviews on SC and health were subject to biases that should be taken into consideration. We identified two sources of bias from the reviews as a whole: bias from SC conceptualizations and bias from health conceptualizations.
3.6.1. Sources of bias from social capital conceptualizations
Every review noted that a key source of bias was the heterogeneous definition of SC. This resulted in the authors making different decisions in how to analyze SC and choosing various conceptualizations. Based on the approach authors took, SC was sometimes measured by validated scales (such as the A-SCAT or the SASCAT) (Almedom, 2005; Ransome et al., 2018; Villalonga-Olives et al., 2018) and sometimes measured by single indicators (such as social participation and trust) (Choi et al., 2014; Ehsan & De Silva, 2015; Hu et al., 2014; Nyqvist et al., 2014). Depending on the conceptualization of SC, measurements or indicators used could mean different things. For example, two reviews on family SC considered parental monitoring, parent-child communication, and parental interest in the child to be indicators of family SC (McPherson et al., 2013, 2014). SC is a multidimensional construct and single indicators of SC may be inappropriate.
3.6.2. Sources of bias from health conceptualizations
Another source of bias from the reviews was how differently they treated various health outcomes (see Table 3 for detailed references). Some reviews explicitly measured a single and specific health outcome (such as HIV/AIDS) whereas others measured health very broadly. A range of reviews included behaviors in their conceptualization of health: certain reviews looked at health-promoting behaviors, risk-taking behaviors such as smoking, assisted living, or general wellbeing in addition to the health outcomes that we had defined by our inclusion criteria (i.e., only outcomes directly related to health). These health-related behaviors and knowledge were sometimes included as health outcomes in the analysis (Alvarez, Kawachi, & Romani, 2017; Villalonga-Olives et al., 2018), though health related behaviors are known to mediate or moderate the relationship between SC and health (Nieminen et al., 2013; Poortinga, 2006).
While certain behaviors can indicate poor health (Murayama et al., 2012), human behavior is governed by social elements. Health behaviors can simultaneously indicate health and an individual's social environment. Individuals with higher SC may be more encouraged to seek help if their networks notice that they need help. At the same time, individuals with higher support networks may not need to seek formal help, as they already have support available to them. The health outcomes in this review have very social consequences that can affect SC as well. For example, individuals with mental illness or HIV/AIDS may face more stigmatization due to their illness, and therefore have reduced SC (Ransome et al., 2018). The relationship between SC and health is not unidirectional and can fluctuate over time.
Subjective wellbeing and loneliness were sometimes considered to be health outcomes among others (Alvarez et al., 2017; Coll-Planas et al., 2017; Flores et al., 2018; McPherson et al., 2013), though we excluded reviews that looked at subjective wellbeing as the main dependent variable (Nyqvist, Forsman, Giuntoli, & Cattan, 2013). These constructs are simultaneously social and health-related, and should not be considered solely as health outcomes. Well-being is a complex construct with heterogeneous conceptualizations. A global way to understand wellbeing is having enough psychological, social, and physical resources to meet a particular challenge (Dodge, Daly, Huyton, & Sanders, 2012). Even though subjective wellbeing can be an aspect of health, having enough resources to meet health challenges does not guarantee good health and vice versa. Furthermore, this definition of wellbeing clearly includes social resources, which could include SC. Loneliness was subject to the same bias as wellbeing, and it was included as a health outcome in some studies (Coll-Planas et al., 2017; Villalonga-Olives et al., 2018). Loneliness is a subjective feeling that can occur when there is a perceived mismatch between the relationships a person would like to have and the ones that they have (Heinrich & Gullone, 2006). In this way, loneliness can simultaneously indicate a lack of SC and be a symptom of certain health outcomes (APA, 2013), but is not equivocal to health. Including it as a health outcome could be a source of bias in the findings.
4. Discussion
This meta-review found that there is a good amount of evidence to indicate that SC is associated with better health. Most reviews showed positive or non-significant findings, and came to the conclusion that SC is beneficial to health outcomes. However, as indicated in one review (and supported by the results of others), negative findings are also important to consider (Villalonga-Olives & Kawachi, 2017). The reviews found that cognitive and structural aspects of SC often predicted good health, though the latter seemed to vary more depending on context. Bonding and bridging SC also predicted good health in general, but could predict worse health depending on the context and the groups that individuals belong to. There was evidence from the meta-analyses that showed that some indicators of SC are protective against mortality. This is in line with another meta-analyses that showed that social relationships are protective against mortality (Holt-Lunstad, Smith, & Layton, 2010). We also found that SC interventions for health seem promising but leave much to be desired, particularly when it comes to how a SC intervention is defined. Many of the interventions cited in the reviews were targeted at the individual level only. There was little evidence to show that the interventions themselves built SC, and that this in turn leads to better health outcomes.
4.1. Limitations and strengths
This meta-review was subject to limitations. First, this meta-review had a certain level of abstraction, as there was already a large amount of synthesis conducted in each review. Publication bias was a risk for both the systematic reviews and the overarching meta-review conducted here as well. Individual studies with inconclusive results may not have been published, and all areas of research may not be represented, as systematic reviews select specific topics. In addition, some reviews had similar aims, so it is possible that the same individual studies were included in multiple reviews. For example, one of the reviews by McPherson et al. (2014) analyzed a subgroup of the other review by McPherson et al. (2013), and was therefore subject to overlap. The reviews by De Silva et al. (2005) and Almedom (2003) both focused on mental health outcomes, and had three overlapping individual studies (Steptoe & Feldman, 2001; Drukker, Kaplan, Feron, & Van Os, 2003; Rosenheck, Morrissey, Lam, et al., 2001). On the other hand, the reviews by Ehsan and De Silva (2015) and De Silva et al. (2005) also had similar aims, but none of the included studies overlapped. We acknowledge this as a source of bias, but as our goal was to describe current trends in published systematic reviews, we included these studies regardless of the individual repetition within studies that had similar aims.
Our inclusion criteria were another source of limitations. We only included texts that were written in a language that at least one of the authors could read at an advanced level. Therefore, we had to exclude studies that seemed pertinent but were not in English, French, or German (Firouzbakht & Tirgar, 2017; Kripper & Sapag, 2009). We suggest that readers also consider reading these reviews if they are able to, as we could have missed important information due to the linguistic barrier in writing and publication. We did not consider online SC, but note that online communities can also create and maintain SC (Naseri, 2017), and are important to consider in future research. Finally, this meta-review focuses on the already large body of literature looking at the relationship between SC and health outcomes. It does not look at SC in groups of individuals with pre-existing health conditions, which should be researched in the future.
Despite these limitations, this research is the first meta-review of SC and health research. This work gives readers a comprehensive idea of what does and does not exist in the SC and health literature, and provides a stepping-stone for further reflection. This review was able to map and synthesize systematic reviews on SC and health (objective 1), and showed different approaches to SC and health that have been mobilized in the literature (objective 2). We tried to identify whether certain health outcomes benefitted more from SC than others, though we did not find enough evidence to draw conclusions (objective 3), and we identified trends and current gaps in SC and health research (objective 4). A key strength of this research is that it is conducted from a critical perspective that helps shed light on how SC and health research can be improved. Most importantly, this meta-review serves as a basis to make clear recommendations for improving SC and health research. These recommendations are discussed in the next section (objective 5).
4.2. Overcoming gaps in social capital and health research
SC should not be oversimplified in an attempt to understand how it relates to health. In this next section, we present possible solutions to questions concerning the “what, who, where, when, why, and how” that should be addressed in future SC and health research.
4.2.1. What?
To really understand what SC is, it is important to look beyond dimensions, settings, and levels for SC. SC is a multidimensional construct that is more than the sum of its parts. Looking at one piece of the SC puzzle at a time is a double edged sword: It can help simplify the mammoth task ahead of SC and health research, but we noted that the reviews allowed for broad criteria (and proxy indicators for SC) that did not necessarily reflect the multidimensionality of the subject. This may be due to the fact that many surveys do not ask enough questions to fully capture the various aspects of SC. For example, in many Canadian surveys, ‘sense of community belonging’ is used as an indicator of SC. As one study empirically showed, this question was unable to really point to SC (Carpiano & Hystad, 2011). Using validated scales can help overcome these problems (Agampodi, Agampodi, Glozier, & Siribaddana, 2015; Harpham, 2008), though these scales are often lengthy and difficult to find in existing surveys.
Moreover, certain dimensions of SC are utilized more than others in health research. Some underrepresented dimensions could be useful in further conceptualizing and understanding SC. For example, bonding, bridging, and linking SC were commonly mentioned, but none of the reviews discussed binding SC. Binding SC refers to long lasting and highly emotional relationships (Widmer, 2007). Many reviews differentiated between structural and cognitive dimensions of SC, but relational SC was not considered. Relational SC refers to individual relationships and shared identities (Nahapiet & Ghoshal, 1998). Future research should be careful about how they operationalize SC, and systematically distinguish between the different dimensions of SC and their particular relationship with health. We note that operationalizing SC can benefit from both quantitative and qualitative approaches, and that qualitative approaches to SC could be particularly useful in understanding what SC means to individuals.
4.2.2. Who?
In order to clearly respond to who benefits from SC in health research, it is important to show how actors (both individuals and various types of groups) interact with one another within different contexts, as well as how this influences the types of SC that they are privy to. Here, we suggest that SC and health research could benefit from looking more deeply into intergroup and intragroup dynamics. While Portes (1998) discussed the importance of intergroup relationships, this discourse has been somewhat forgotten in SC and health research. One of the reviews did highlight that coming back to Portes’ conceptualizations could be useful for understanding why SC is not always beneficial (Villalonga-Olives & Kawachi, 2017), and we recommend that future research follow this example. Coming back to this perspective could have important implications for how we interpret SC for different actors in general. For example, bonding SC might be beneficial for those that are part of an in-group (regardless of social status), but it might be exclusive and have negative effects on the health status of the out-group (Portes, 1998), especially when the social position of the out-group is lower. Bridging SC might only be beneficial for individuals who do not perceive social devaluation and discrimination through social exchanges that transcend different social categories and groups. Similarly, an individual can mistrust their larger community or neighborhood, but have high trust in their in-group, nuancing our understanding of cognitive SC. Relative deprivation can play a role in the development and maintenance of SC, and can reinforce inequalities or marginalize certain actors (Wilkinson & Pickett, 2007). This can influence intergroup dynamics, and help explain why SC exists for some and not others.
4.2.3. When?
SC and its relationship with health outcomes can develop and change over time: It is important to consider when SC is measured over an individual's lifecourse. Some reviews focused explicitly on longitudinal data or pre/post evaluations and some reviews observed age differences in their results (De Silva et al., 2005; Murayama et al., 2012; Nyqvist et al., 2014). One review considered a lifecourse perspective to help explain why SC could operate differently at different life stages (Almedom, 2005). Fluctuations in SC along life events and transitions that occur in different settings or life-domains (such as family or work) can influence health. SC can simultaneously change during these periods, and can alter the resources available during life transitions (such as marriage or the loss of a job) (Spini, Jopp, Pin, & Stringhini, 2016).
A life course approach can be useful for future research concerning SC and health. Lives develop over a long period of time, can be analyzed from different angles or dimensions, and unfold within different levels of social structures (Spini, Bernardi, & Oris, 2017; Spini et al., 2016). Specific social configurations and overarching institutions could lead to the accumulation or loss of SC along the life course. The way a life unfolds within a social context can affect the types of SC that are activated or lost during life events and transitions, which in turn impacts health outcomes. Indeed, research has proposed to look at SC as a type of reserve that can be accumulated over the lifecourse (Cullati, Kliegel, & Widmer, 2018). The importance of the life-course in social determinants of health research has been long discussed (Blane, 1995), and should be more carefully considered in SC and health research.
4.2.4. Where?
It is widely understood that SC is tied to contexts, but where SC takes place within contexts and why certain contexts have more SC than others remains obscure. Researchers have differentiated between individual and group levels of SC, but there was little differentiation in terms of how a group or geographic area was defined, if there was overlap with other possible groups, and where they fell within larger socio-geographic structures. Multilevel studies tried to address these issues, but the scales at which the context is considered can vary greatly (e.g., neighborhoods, countries). Additionally, an individual's own position within these contexts may alter how they perceive their environment and the SC that they are able to access. More attention should be given to clearly identifying the socio-geographic boundaries in which SC takes place.
4.2.5. Why?
The process of identifying with contexts, groups, and other actors are important to understand why SC is built. The social identification approach (Jetten et al., 2017) helps explain why SC exists for certain actors, and how it can influence health and/or reinforce inequalities. The SC literature has considered some social-psychological mechanisms that occur within individuals (e.g. perceptions of social trust), but has overlooked other aspects that may be equally important, such as social identification. Social identity lies at the intersection between psychological and sociological explanations of individual and group behaviour. It illustrates how belonging to groups can be become part of an individual, and how an individual can feel and act as a member within broader social structures. Identifying with a group makes that group an important part of an individual's self-definition. If an individual strongly identifies with a group that is associated with positive attributes, this can relate to feelings of belonging, trust, and support, which can improve health for those who identify with the group (Jetten et al., 2017). Social psychological research has shown that individuals who identify with multiple groups have better mental and physical health outcomes (Cruwys et al., 2013; Jones & Jetten, 2011) and adjust better to critical life events (Haslam et al., 2008; Iyer, Jetten, Tsivrikos, Postmes, & Haslam, 2009).
The social identity approach complements network and cohesion approaches to SC. Network approaches to SC measure the strength of ties between individuals, but they do not ask individuals whether or not they identify with these networks or groups as a whole. Cohesion approaches measure potential consequences of social identification (e.g., trust, social support), but do not consider identification as a mechanism. The link between cognitive SC and neighborhood identification is apparent: if individuals strongly identify with their neighborhood, and their neighborhood is associated with positive attributes such as social trust, they may perceive that their neighborhood has higher levels of cognitive SC (Fong, Cruwys, Haslam, & Haslam, 2019). Based on these reflections, we propose a table of approaches to SC that can be useful for future health research and that expands and complements previous cohesion and network approaches to SC by an identity perspective (Table 6).
Table 6.
Proposed conceptualization of social capital and health
| Approach | Approach definition | Dimension | Definition |
|---|---|---|---|
| Network | Patterns of social ties that exist within a set of actors (individuals, groups, organisations, etc.). Social ties refer to the links that bring different actors together, and can be formal or informal. | Binding | Long lasting, multiplex, and highly emotional relationships |
| Bonding | Resources that are accessed within networks or groups having generally similar characteristics | ||
| Bridging | Social resources that may be accessed across different groups (usually with different socio-demographic and socio-economic positions) | ||
| Linking | Networks of trust that connect individuals and groups across different structures (often in relation to institutionalized authority/ power) | ||
| Cohesion | The presence of strong social bonds that bridge divisions in society, and the lack of conflict in a society | Structural | Formal opportunities in which individual actors might develop social ties or social networks |
| Cognitive | Perceptions of trust, reciprocity, and support, shared values | ||
| Relational | Nature of relationships and identification with others | ||
| Identification | An individual’s socio-cognitive identification with one or several social category/ies or with one or several concrete groups | Cognitive | Self-categorization of belonging to a group, or group membership |
| Affective | Emotional evaluation of group membership | ||
| In-group ties | Perceptions of similarity and bonds with group members |
4.2.6. How?
Many of the reviews noted that SC and health research should continue to investigate how SC influences health. In order to do so, assumptions that SC has a linear relationship with health should be contested. Some of the reviews suggested that mixed and negative health outcomes from structural components of SC might be due to stress caused from an overburden of responsibilities. Indeed, a recent study found that there is a curvilinear relationship between group membership and mental health: moderate participation was ideal, whereas too much or too little could have negative consequences (Gallagher et al., 2018). Research on SC interventions for health should recognize that too little and too much SC might have undesirable consequences. One way to gain deeper insight on how SC can influence health could be to systematically review qualitative data that seeks to investigate this. A synthesis of qualitative evidence could be useful to developing and implementing these interventions (Langlois, Tunçalp, Norris, Askew, & Ghaffar, 2018).
5. Conclusion
It is difficult to disentangle every component of SC and assess whether a certain dimension, setting, or level for SC is linked with better health outcomes than others. Even though many of the reviews chose a theoretical lens to help synthesize the evidence, it is impossible to fully understand how SC influences health without understanding the interaction between what, who, when, where, and why. The interactions between the multi-dimensionality of SC, dynamics between actors, time, contexts, and underlying psychological mechanisms are useful to consider in the relationship between SC and health. Future research on SC and health can benefit from a what, who, when, where, why, and how framework.
Acknowledgements
This publication benefited from the support of the Swiss National Centre of Competence in Research LIVES—Overcoming vulnerability: Life course perspectives (NCCR LIVES), financed by the Swiss National Science Foundation. We thank Dr. Felicity Turner-Zwinkels for her guidance and Dr. Nicolas Sommet for his comments on the manuscript. We would also like to thank the two anonymous reviewers for their helpful comments.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ssmph.2019.100425.
Contributor Information
Annahita Ehsan, Email: annahita.ehsan@unil.ch.
Hannah Sophie Klaas, Email: hannah.klaas@unil.ch.
Alexander Bastianen, Email: alex.bastianen@gmail.com.
Dario Spini, Email: dario.spini@unil.ch.
Conflicts of interest
The authors have no conflict of interest to declare.
Funding
The authors are funded by the Institute of Social Sciences at the University of Lausanne and the Swiss National Centre of Competence in Research LIVES—Overcoming vulnerability: Life course perspectives (NCCR LIVES), which is financed by the Swiss National Science Foundation.
Ethics statement
This systematic review of systematic reviews did not use human subjects. It reviewed data that was already published online, and therefore did not require ethnical approval from a research ethics board.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- Agampodi T.C., Agampodi S.B., Glozier N., Siribaddana S. Measurement of social capital in relation to health in low and middle income countries (LMIC): A systematic review. Social Science & Medicine. 2015;128:95–104. doi: 10.1016/j.socscimed.2015.01.005. [DOI] [PubMed] [Google Scholar]
- Almedom A.M. Social capital and mental health: An interdisciplinary review of primary evidence. Social Science & Medicine. 2005;61(5):943–964. doi: 10.1016/j.socscimed.2004.12.025. [DOI] [PubMed] [Google Scholar]
- Alvarez E.C., Kawachi I., Romani J.R. Family social capital and health–a systematic review and redirection. Sociology of Health & Illness. 2017;39(1):5–29. doi: 10.1111/1467-9566.12506. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association . American Psychiatric Pub; 2013. Diagnostic and statistical manual of mental disorders (DSM-5®) [Google Scholar]
- Best S.J., Krueger B.S. Online interactions and social capital: Distinguishing between new and existing ties. Social Science Computer Review. 2006;24(4):395–410. [Google Scholar]
- Blane D. Social determinants of health--socioeconomic status, social class, and ethnicity. American Journal of Public Health. 1995;85(7):903–905. doi: 10.2105/ajph.85.7.903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bourdieu P. The forms of capital. Handbook of theory and research for the sociology of education. JG Richardson. New York, Greenwood. 1986;241(258):19. [Google Scholar]
- Cameron J.E. A three-factor model of social identity. Self and Identity. 2004;3(3):239–262. [Google Scholar]
- Carlson E.D., Chamberlain R.M. Social capital, health, and health disparities. Journal of Nursing Scholarship. 2003;35(4):325–331. doi: 10.1111/j.1547-5069.2003.00325.x. [DOI] [PubMed] [Google Scholar]
- Carpiano R.M. Toward a neighborhood resource-based theory of social capital for health: Can Bourdieu and sociology help? Social Science & Medicine. 2006;62(1):165–175. doi: 10.1016/j.socscimed.2005.05.020. [DOI] [PubMed] [Google Scholar]
- Carpiano R.M., Hystad P.W. “Sense of community belonging” in health surveys: What social capital is it measuring? Health & Place. 2011;17(2):606–617. doi: 10.1016/j.healthplace.2010.12.018. [DOI] [PubMed] [Google Scholar]
- Choi M., Mesa-Frias M., Nüesch E., Hargreaves J., Prieto-Merino D., Bowling A. Social capital, mortality, cardiovascular events and cancer: A systematic review of prospective studies. International Journal of Epidemiology. 2014;43(6):1895–1920. doi: 10.1093/ije/dyu212. [DOI] [PubMed] [Google Scholar]
- Coleman J. Foundations of social theory. Coleman, James (comp) The Belknap Press of Harvard University Press. Links; Cambridge, Massachusetts: 1990. Social capital. [Google Scholar]
- Coll-Planas L., Nyqvist F., Puig T., Urrutia G., Sola I., Monteserin R. Social capital interventions targeting older people and their impact on health: A systematic review. Journal of Epidemiology & Community Health. 2017;71(7):663–672. doi: 10.1136/jech-2016-208131. [DOI] [PubMed] [Google Scholar]
- Cruwys T., Dingle G.A., Haslam C., Haslam S.A., Jetten J., Morton T.A. Social group memberships protect against future depression, alleviate depression symptoms and prevent depression relapse. Social Science & Medicine. 2013;98:179–186. doi: 10.1016/j.socscimed.2013.09.013. [DOI] [PubMed] [Google Scholar]
- Cullati S., Kliegel M., Widmer E. Development of reserves over the life course and onset of vulnerability in later life. Nature Human Behaviour. 2018;1 doi: 10.1038/s41562-018-0395-3. [DOI] [PubMed] [Google Scholar]
- De Silva M.J., McKenzie K., Harpham T., Huttly S.R.A. Social capital and mental illness: A systematic review. Journal of Epidemiology & Community Health. 2005;59(8):619–627. doi: 10.1136/jech.2004.029678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deaux K. Social identification. In: Higgins E.T., Kruglanski A.W., editors. Social psychology: Handbook of basic principles. Guilford Press; New York, NY, US: 1996. pp. 777–798. [Google Scholar]
- Dodge R., Daly A.P., Huyton J., Sanders L.D. The challenge of defining wellbeing. International Journal of Wellbeing. 2012;2(3):222–235. [Google Scholar]
- Drukker M., Kaplan C., Feron F., Van Os J. Children's health-related quality of life, neighborhood socio-economic deprivation and social capital. A contextual analysis. Social Science & Medicine. 2003;57(5):825–841. doi: 10.1016/s0277-9536(02)00453-7. [DOI] [PubMed] [Google Scholar]
- Ehsan A.M., De Silva M.J. Social capital and common mental disorder: A systematic review. Journal of Epidemiology & Community Health. 2015;69(10):1021–1028. doi: 10.1136/jech-2015-205868. [DOI] [PubMed] [Google Scholar]
- Elo S., Kyngäs H. The qualitative content analysis process. Journal of Advanced Nursing. 2008;62(1):107–115. doi: 10.1111/j.1365-2648.2007.04569.x. [DOI] [PubMed] [Google Scholar]
- Firouzbakht M., Tirgar A. Workplace social capital and employee health: A systematic review study. Journal of Ergonomics. 2017;5(1):18–25. [Google Scholar]
- Flores E.C., Fuhr D.C., Bayer A.M., Lescano A.G., Thorogood N., Simms V. Mental health impact of social capital interventions: A systematic review. Social Psychiatry and Psychiatric Epidemiology. 2018;53(2):107–119. doi: 10.1007/s00127-017-1469-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fong P., Cruwys T., Haslam C., Haslam S.A. Neighbourhood identification and mental health: How social identification moderates the relationship between socioeconomic disadvantage and health. Journal of Environmental Psychology. 2019;61(2019):101–114. [Google Scholar]
- French D.P., Cameron E., Benton J.S., Deaton C., Harvie M. Can communicating personalised disease risk promote healthy behaviour change? A systematic review of systematic reviews. Annals of Behavioral Medicine. 2017;51(5):718–729. doi: 10.1007/s12160-017-9895-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gallagher H.C., Block K., Gibbs L., Forbes D., Lusher D., Molyneaux R. The effect of group involvement on post-disaster mental health: A longitudinal multilevel analysis. Social Science & Medicine. 2018;220(2018):161–175. doi: 10.1016/j.socscimed.2018.11.006. [DOI] [PubMed] [Google Scholar]
- Gilbert K.L., Quinn S.C., Goodman R.M., Butler J., Wallace J. A meta-analysis of social capital and health: A case for needed research. Journal of Health Psychology. 2013;18(11):1385–1399. doi: 10.1177/1359105311435983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harpham T. Social capital and health. Springer; New York, NY: 2008. The measurement of community social capital through surveys; pp. 51–62. [Google Scholar]
- Haslam C., Holme A., Haslam S.A., Iyer A., Jetten J., Williams W.H. Maintaining group memberships: Social identity continuity predicts well-being after stroke. Neuropsychological Rehabilitation. 2008;18(5–6):671–691. doi: 10.1080/09602010701643449. [DOI] [PubMed] [Google Scholar]
- Heinrich L.M., Gullone E. The clinical significance of loneliness: A literature review. Clinical Psychology Review. 2006;26(6):695–718. doi: 10.1016/j.cpr.2006.04.002. [DOI] [PubMed] [Google Scholar]
- Holt-Lunstad J., Smith T.B., Layton J.B. Social relationships and mortality risk: A meta-analytic review. PLoS Medicine. 2010;7(7) doi: 10.1371/journal.pmed.1000316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu F., Hu B., Chen R., Ma Y., Niu L., Qin X. A systematic review of social capital and chronic non-communicable diseases. Bioscience trends. 2014;8(6):290–296. doi: 10.5582/bst.2014.01138. [DOI] [PubMed] [Google Scholar]
- Islam M.K., Merlo J., Kawachi I., Lindström M., Gerdtham U.-G. Social capital and health: Does egalitarianism matter? A literature review. International Journal for Equity in Health. 2006;5(1):3. doi: 10.1186/1475-9276-5-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iyer A., Jetten J., Tsivrikos D., Postmes T., Haslam S.A. The more (and the more compatible) the merrier: Multiple group memberships and identity compatibility as predictors of adjustment after life transitions. British Journal of Social Psychology. 2009;48(4):707–733. doi: 10.1348/014466608X397628. [DOI] [PubMed] [Google Scholar]
- Jetten J., Haslam S.A., Cruwys T., Greenaway K.H., Haslam C., Steffens N.K. Advancing the social identity approach to health and well-being: Progressing the social cure research agenda. European Journal of Social Psychology. 2017;47(7):789–802. [Google Scholar]
- Jones J.M., Jetten J. Recovering from strain and enduring pain: Multiple group memberships promote resilience in the face of physical challenges. Social Psychological and Personality Science. 2011;2(3):239–244. [Google Scholar]
- Kawachi I., Berkman L.F. Social capital, social cohesion, and health. Social epidemiology. 2014;2:290–319. [Google Scholar]
- Kawachi I., Kennedy B.P., Lochner K., Prothrow-Stith D. Social capital, income inequality, and mortality. American journal of public health. 1997;87(9):1491–1498. doi: 10.2105/ajph.87.9.1491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khazaeian S., Kariman N., Ebadi A., Nasiri M. The impact of social capital and social support on the health of female-headed households: A systematic review. Electronic Physician. 2017;9(12):6027–6034. doi: 10.19082/6027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kripper C.E., Sapag J.C. Social capital and health in Latin America and the caribbean: A systematic review. Revista panamericana de salud publica= Pan American journal of public health. 2009;25(2):162–170. doi: 10.1590/s1020-49892009000200010. [DOI] [PubMed] [Google Scholar]
- Langlois E.V., Tunçalp Ö., Norris S.L., Askew I., Ghaffar A. Qualitative evidence to improve guidelines and health decision-making. Bulletin of the World Health Organization. 2018;96(2):79. doi: 10.2471/BLT.17.206540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin N. Vol. 19. Cambridge university press; 2002. (Social capital: A theory of social structure and action). [Google Scholar]
- Lin N. Social capital. Routledge; 2017. Building a network theory of social capital; pp. 3–28. [Google Scholar]
- Macinko J., Starfield B. The utility of social capital in research on health determinants. The Milbank Quarterly. 2001;79(3):387–427. doi: 10.1111/1468-0009.00213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKenzie K., Harpham T. Jessica Kingsley Publishers; 2006. Social capital and mental health. [Google Scholar]
- McPherson K., Kerr S., Cheater F., Morgan A. Glasgow Centre for population health. Glasgow Caledonian University; Glasgow: 2013. The role and impact of social capital on the health and wellbeing of children and adolescents: A systematic review. [Google Scholar]
- McPherson K., Kerr S., McGee E., Morgan A., Cheater F.M., McLean J. The association between social capital and mental health and behavioural problems in children and adolescents: An integrative systematic review. BMC Psychology. 2014;2(1):7. doi: 10.1186/2050-7283-2-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moher D., Liberati A., Tetzlaff J., Altman D.G., Group P. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Medicine. 2009;6(7) doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moore S., Kawachi I. Twenty years of social capital and health research: A glossary. Journal of Epidemiology & Community Health. 2017;71(5):513–517. doi: 10.1136/jech-2016-208313. [DOI] [PubMed] [Google Scholar]
- Murayama H., Fujiwara Y., Kawachi I. Social capital and health: A review of prospective multilevel studies. Journal of Epidemiology. 2012;22(3):179–187. doi: 10.2188/jea.JE20110128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nahapiet J., Ghoshal S. Social capital, intellectual capital, and the organizational advantage. Academy of Management Review. 1998;23(2):242–266. [Google Scholar]
- Naseri S. Online social network sites and SC: A case of facebook. International Journal of Applied Sociology. 2017;7(1) [Google Scholar]
- Nieminen T., Prättälä R., Martelin T., Härkänen T., Hyyppä M.T., Alanen E. Social capital, health behaviours and health: A population-based associational study. BMC Public Health. 2013;13(1):613. doi: 10.1186/1471-2458-13-613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nyqvist F., Forsman A.K., Giuntoli G., Cattan M. Social capital as a resource for mental well-being in older people: A systematic review. Aging & Mental Health. 2013;17(4):394–410. doi: 10.1080/13607863.2012.742490. [DOI] [PubMed] [Google Scholar]
- Nyqvist F., Pape B., Pellfolk T., Forsman A.K., Wahlbeck K. Structural and cognitive aspects of social capital and all-cause mortality: A meta-analysis of cohort studies. Social Indicators Research. 2014;116(2):545–566. [Google Scholar]
- Obst P., White K. Three-dimensional strength of identification across group memberships: A confirmatory factor analysis. Self and Identity. 2005;4(1):69–80. [Google Scholar]
- Poortinga W. Do health behaviors mediate the association between social capital and health? Preventive Medicine. 2006;43(6):488–493. doi: 10.1016/j.ypmed.2006.06.004. [DOI] [PubMed] [Google Scholar]
- Porta M., Greenland S., Hernán M., Dos Santos Silva I., Last J.M. 6th ed. Oxford University Press; New York: 2015. A dictionary of epidemiology. [Google Scholar]
- Portes A. Social capital: Its origins and applications in modern sociology. Annual Review of Sociology. 1998;24(1):1–24. [Google Scholar]
- Putnam R.D. Culture and politics. Palgrave Macmillan; 2000. Bowling alone: America's declining social capital; pp. 223–234. [Google Scholar]
- Putnam R.D., Leonardi R., Nanetti R.Y. Princeton university press; 1994. Making democracy work: Civic traditions in modern Italy. [Google Scholar]
- Ransome Y., Thurber K.A., Swen M., Crawford N.D., German D., Dean L.T. Social capital and HIV/AIDS in the United States: Knowledge, gaps, & future directions. SSM-Population Health. 2018;5:73–85. doi: 10.1016/j.ssmph.2018.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenheck R., Morrissey J., Lam J., Calloway M., Stolar M., Johnsen M. Service delivery and community: SC, service systems integration, and outcomes among homeless persons with severe mental illness. Health Services Research. 2001;36(4):691. [PMC free article] [PubMed] [Google Scholar]
- Shea B.J., Grimshaw J.M., Wells G.A., Boers M., Andersson N., Hamel C. Development of AMSTAR: A measurement tool to assess the methodological quality of systematic reviews. BMC Medical Research Methodology. 2007;7(1):10. doi: 10.1186/1471-2288-7-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shea B.J., Hamel C., Wells G.A., Bouter L.M., Kristjansson E., Grimshaw J. AMSTAR is a reliable and valid measurement tool to assess the methodological quality of systematic reviews. Journal of Clinical Epidemiology. 2009;62(10):1013–1020. doi: 10.1016/j.jclinepi.2008.10.009. [DOI] [PubMed] [Google Scholar]
- Shiell A., Hawe P., Kavanagh S. Evidence suggests a need to rethink social capital and social capital interventions. Social Science & Medicine. 2018 doi: 10.1016/j.socscimed.2018.09.006. [DOI] [PubMed] [Google Scholar]
- Smith V., Devane D., Begley C.M., Clarke M. Methodology in conducting a systematic review of systematic reviews of healthcare interventions. BMC Medical Research Methodology. 2011;11(1):15. doi: 10.1186/1471-2288-11-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spini D., Bernardi L., Oris M. Toward a life course framework for studying vulnerability. Research in Human Development. 2017;14(1):5–25. [Google Scholar]
- Spini D., Jopp D.S., Pin S., Stringhini S. 2016. The multiplicity of aging: Lessons for theory and conceptual development from longitudinal studies. Handbook of theories of aging; pp. 669–690. [Google Scholar]
- Steptoe A., Feldman P.J. Neighborhood problems as sources of chronic stress: Development of a measure of neighborhood problems, and associations with socioeconomic status and health. Annals of Behavioral Medicine. 2001;23(3):177–185. doi: 10.1207/S15324796ABM2303_5. [DOI] [PubMed] [Google Scholar]
- Uphoff E.P., Pickett K.E., Cabieses B., Small N., Wright J. A systematic review of the relationships between social capital and socioeconomic inequalities in health: A contribution to understanding the psychosocial pathway of health inequalities. International Journal for Equity in Health. 2013;12:54. doi: 10.1186/1475-9276-12-54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Villalonga-Olives E., Kawachi I. The measurement of social capital. Gaceta Sanitaria. 2015;29(1):62–64. doi: 10.1016/j.gaceta.2014.09.006. [DOI] [PubMed] [Google Scholar]
- Villalonga-Olives E., Kawachi I. The dark side of social capital: A systematic review of the negative health effects of social capital. Social Science & Medicine. 2017;194:105–127. doi: 10.1016/j.socscimed.2017.10.020. [DOI] [PubMed] [Google Scholar]
- Villalonga-Olives E., Wind T.R., Kawachi I. Social capital interventions in public health: A systematic review. Social Science & Medicine. 2018;212:203–218. doi: 10.1016/j.socscimed.2018.07.022. [DOI] [PubMed] [Google Scholar]
- Widmer E.D. Social capital in wide family contexts: An empirical assessment using social network methods. International Review of Sociology—Revue Internationale de Sociologie. 2007;17(2):225–238. [Google Scholar]
- Wilkinson R.G., Pickett K.E. The problems of relative deprivation: Why some societies do better than others. Social Science & Medicine. 2007;65(9):1965–1978. doi: 10.1016/j.socscimed.2007.05.041. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.