Abstract
Introduction
Pyoderma gangrenosum (PG) in pregnant women is rare and resembles surgical site infection (SSI). Here we present two cases of PG after caesarean section.
Case 1
A 29-year-old woman, who had a history of recurrent wound dehiscence after surgery, exhibited wound ulceration and exudate 6 days after caesarean section. Antibiotics were ineffective and multiple wound cultures were negative. Skin biopsy indicated PG and oral steroid administration resulted in wound improvement.
Case 2
A 27-year-old woman, who had a history of PG, exhibited wound ulceration and exudate 5 days after caesarean section. The lesion developed despite antibiotic administration, and multiple wound cultures were negative. Skin biopsy indicated PG and the wound improved after oral steroid administration.
Discussion
Definitive diagnosis of PG is essential because its treatment differs from that of SSI. PG after caesarean section can be misdiagnosed as SSI, even when there is a history of wound dehiscence or PG.
Keywords: Pyoderma gangrenosum, Caesarean section
Highlights
-
•
Pyoderma gangrenosum is rare in pregnancy and resembles surgical site infection.
-
•
Treatment of pyoderma gangrenosum differs from that of surgical site infection.
-
•
Pyoderma gangrenosum after caesarean section can be misdiagnosed as surgical site infection.
1. Introduction
Pyoderma gangrenosum (PG) is an inflammatory dermatosis with a tender nodule or pustule; it is a chronic, non-infectious condition caused by neutrophil infiltration [1]. PG is likely to develop in patients aged between 20 and 50 years and is more common in women than men [2]. However, PG rarely occurs in pregnant women, and since PG after caesarean section has similar symptoms as surgical site infection (SSI), obstetricians can misdiagnose PG in this setting. Because the treatment of PG differs from that of SSI, definitive diagnosis is essential. Here we present two cases in which PG after caesarean section was initially diagnosed as SSI.
2. Case Presentation
2.1. Case 1
A healthy, multiparous, 29-year-old woman was referred to an obstetric unit at 32 weeks' gestation because of previous recurrent wound dehiscence after caesarean section. Clinical examination showed no evidence of collagen diseases. An elective repeat caesarean section was performed at 37 weeks' gestation, and a female newborn was delivered (2464 g, Apgar scores at 1 and 5 min 8 and 8). After surgery, exudate developed in the wound. Six days after the caesarean section, the patient demonstrated wound ulceration (see Fig. 1), and computed tomography (CT) showed inflammation under the wound. The initial diagnosis was SSI, but several days of antibiotics were ineffective and multiple wound cultures were negative. A non-infective, inflammatory condition was suspected, and a skin biopsy showed neutrophilic infiltration and a necrotic lesion (see Fig. 2), leading to the diagnosis of PG. The administration of an oral steroid (started as prednisolone 40 mg/day, gradually decreasing the dose for 14 weeks) resulted in wound improvement. Seventeen weeks after the treatment, the wound had healed to a fine scar.
Fig. 1.
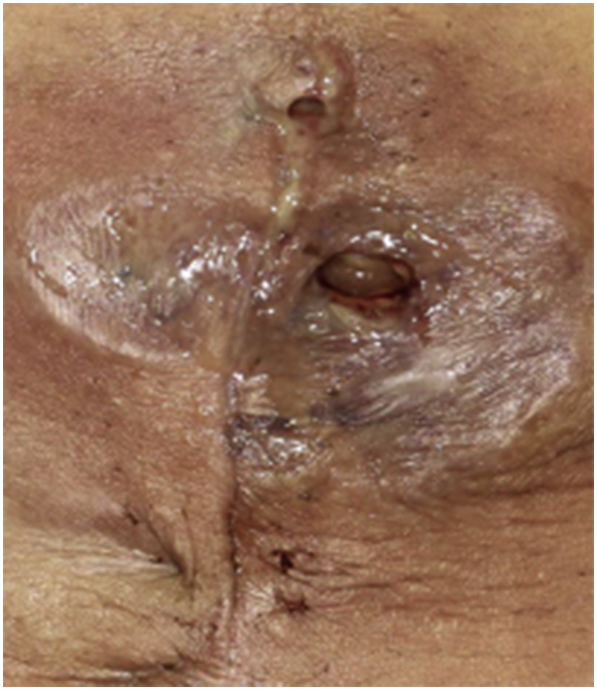
In case 1, the patient exhibited wound exudate and ulceration 6 days after caesarean section (HE stain, ×200).
Fig. 2.
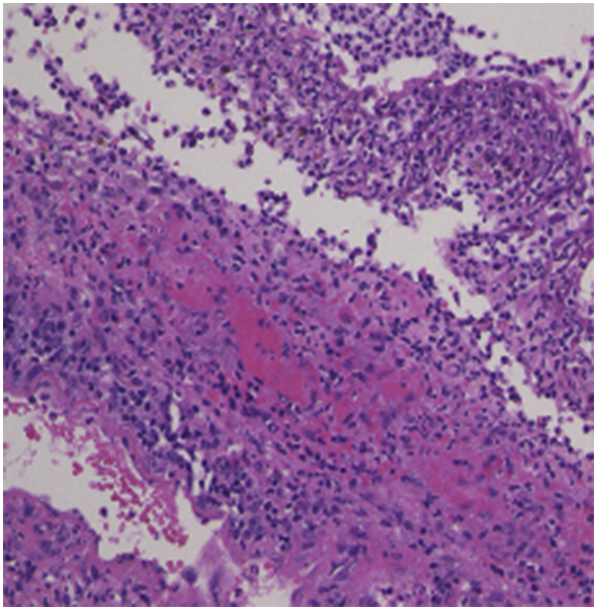
The skin biopsy showed neutrophilic infiltration and a necrotic lesion.
2.2. Case 2
A healthy, nulliparous, 27-year-old woman was referred to a facility at 32 weeks' gestation because of a history of PG and risk of preterm birth. Clinical chorioamnionitis occurred and an emergency caesarean section was performed at 33 weeks' gestation. A male newborn was delivered (2034 g, Apgar scores at 1 and 5 min 7 and 9, respectively). After surgery, exudate developed in the wound. Five days after the caesarean section, wound ulceration occurred (see Fig. 3), and CT showed inflammation under the wound. While the condition clinically resembled SSI, antibiotics were ineffective and wound cultures were negative. A skin biopsy revealed neutrophilic infiltration (see Fig. 4), indicating PG. Administration of an oral steroid (started as prednisolone 40 mg/day, gradually decreasing the dose for 19 weeks) resulted in wound improvement. Eighteen weeks after the treatment, the wound had healed to a fine scar.
Fig. 3.

In case 2, wound exudate and ulceration developed 5 days after caesarean section (HE stain, ×100).
Fig. 4.
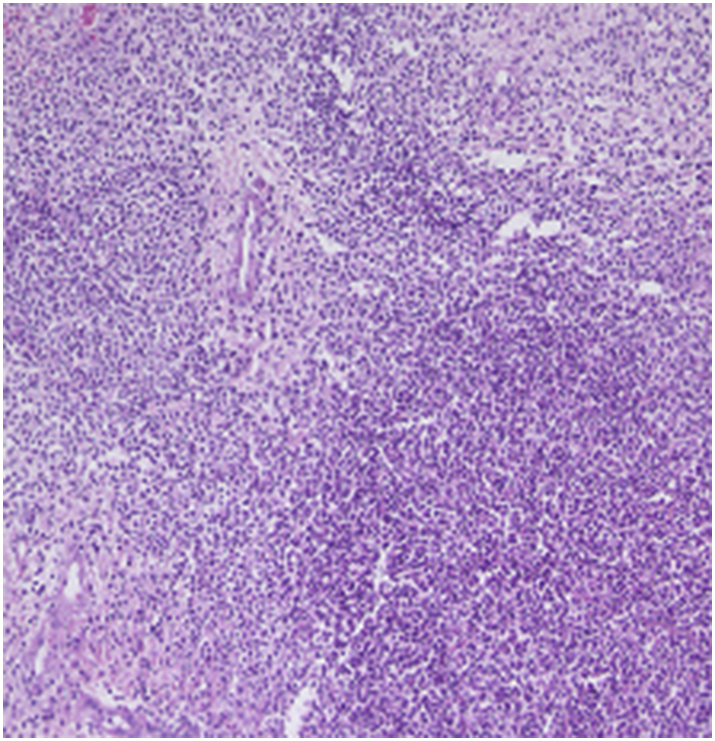
The skin biopsy showed neutrophilic infiltration.
3. Discussion
Obstetricians rarely encounter PG in pregnant women [3], and the lesions of PG after caesarean section mimic SSI, demonstrating wound ulceration and exudate. Therefore, PG after caesarean section can be incorrectly diagnosed due to its rarity and resemblance to SSI. The two patients presented above were initially misdiagnosed with SSI, despite their history of wound dehiscence or PG.
Definitive diagnosis of PG is essential because its treatment differs from that of SSI. In patients with PG, steroid therapy or immunosuppressive therapy results in dramatic wound improvement [1]. In patients misdiagnosed with SSI and in whom systemic antibiotics are ineffective, wound deterioration often leads surgeons to choose aggressive debridement, which only aggravates the wound due to pathergy [4]. Thus, misdiagnosis can have devastating outcomes.
A common clinical sign of PG after caesarean section is a lesion that fails to improve despite antibiotic administration [4]. Careful observation of the clinical course increases the likelihood that obstetric care providers will suspect PG. Of note, postoperative PG in obstetric and gynaecological patients was found to appear earlier than in other types of patients, at a mean of 5.2 days vs. 7.0 days, respectively [4]. Therefore, antibiotic ineffectiveness may be more common in PG after caesarean section than after other surgeries.
Negative bacterial cultures can help confirm a non-infectious condition, but can also be misleading because antibiotics are routinely administered postoperatively. In addition, contamination and secondary infections can occur in patients with PG. Repeat bacterial cultures are needed and the results require careful interpretation.
A skin biopsy can identify neutrophilic infiltration of the lesion in PG [5]. In some cases, necrosis or signs of vasculitis are observed [6]. A skin biopsy is also useful to exclude malignancies and systemic vasculitis. However, the finding of neutrophilic infiltration is not specific, and skin biopsies are also sometimes inaccurate, failing to reveal any histological findings [6].
In conclusion, PG after caesarean section can be misdiagnosed as SSI, even when there is a history of wound dehiscence or PG, as in the cases above. The diagnosis of PG after caesarean section is still challenging. Of note, in PG cases, steroids are dramatically effective.
Contributors
All authors were involved in the clinical care of the patient and contributed to the conception, drafting, review and revision of the manuscript. All authors saw and approved the final version of the paper and take full responsibility for the work.
Funding
This work did not receive any specific grant from funding agencies.
Patient Consent
Informed consent was obtained from the patients for publication of this work.
Provenance and Peer Review
This case report was peer reviewed.
Declaration of Competing Interest
The authors have no potential conflict of interest to declare.
References
- 1.Blitz N.M., Rudikoff D. Pyoderma gangrenosum. Mt Sinai J. Med. 2001;68:287–297. [PubMed] [Google Scholar]
- 2.Weizman A., Huang B., Berel D., Targan S.R., Dubinsky M., Fleshner P., Ippoliti A., Kaur M., Panikkath D., Brant S., Oikonomou I., Duerr R., Rioux J., Silverberg M., Rotter J.I., Vasiliauskas E., Haritunians T., Shih D., Li D., Melmed G.Y., McGovern D.P. Clinical, serologic, and genetic factors associated with pyoderma gangrenosum and erythema nodosum in inflammatory bowel disease patients. Inflamm. Bowel Dis. 2014;20:525–533. doi: 10.1097/01.MIB.0000442011.60285.68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Park J.Y., Lee J., Park J.S., Jun J.K. Successful vaginal birth after prior cesarean section in a patient with pyoderma gangrenosum. Obst. Gynecol. Sci. 2016;59:62–65. doi: 10.5468/ogs.2016.59.1.62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zuo K.J., Fung E., Tredget E.E., Lin A.N. A systematic review of post-surgical pyoderma gangrenosum: identification of risk factors and proposed management strategy. J. Plast. Reconstr. Aesthet. Surg. 2015;68:295–303. doi: 10.1016/j.bjps.2014.12.036. [DOI] [PubMed] [Google Scholar]
- 5.Crowson A.N., Mihm M.C., Jr., Magro C. Pyoderma gangrenosum: a review. J. Cutan. Pathol. 2003;30:97–107. doi: 10.1034/j.1600-0560.2003.00024.x. [DOI] [PubMed] [Google Scholar]
- 6.Steele R.B., Nugent W.H., Braswell S.F., Frisch S., Ferrell J., Ortega-Loayza A.G. Pyoderma gangrenosum and pregnancy: an example of abnormal inflammation and challenging treatment. Br. J. Dermatol. 2016;174:77–87. doi: 10.1111/bjd.14230. [DOI] [PubMed] [Google Scholar]


