Introduction
Post-acute care (PAC) services provided in skilled nursing facilities (SNFs) are vital to the success of patients with heart failure (HF) transition from hospital to home.1 The impetus to improve the quality of PAC is accelerated by changes in Medicare regulation that will apply penalties to PAC providers for hospital readmissions in 2017.2 Skilled nursing facilities provide transitional care services for many old and frail residents with multiple comorbidities. Notably, 25% of Medicare beneficiaries with HF are discharged to SNFs following a hospitalization.3 Clinical practice guidelines specifically for HF disease management in long-term care exists;4,5 however, these publications are based on clinical experience and HF guidelines developed for different settings. There is very little data indicating the best way to manage patients with HF in SNFs and subsequently how to improve patient outcomes, including a decrease in rehospitalizations.1
All-cause rehospitalizations from SNFs have increased from 18% to 24% over the past decade6 and have been reported as high as 58% for patients with HF.7 Reasons for rehospitalizations at the time of transfer are difficult to determine. SNF staff does not have the ability or resources to determine a medical diagnosis at the time of transfer to the hospital. Typically, when a patient demonstrates signs and symptoms that require hospitalization, a registered nurse or licensed practical nurse notifies the patient’s physician and coordinates an ambulance transfer to the hospital. The documentation from the nurse includes only the patients’ signs and symptoms. At the facility level, capturing this data and factors associated with rehospitalizations in a registry is important in order to understand patterns and opportunities for improvement. Although a patient registry seems obvious, there is no published literature describing the use of a patient registry to facilitate the reduction of the number of rehospitalizations from SNFs.
We previously reported on a SNF HF disease management program implemented in four SNFs in the greater Cleveland metropolitan area.8 The HF disease management program quality improvement (QI) project included staff education, identification of patients with HF, a baseline data collection form, a nursing standing order set, and an audit and feedback process. We reported that successful facilities adhered to HF disease management implementation protocols more often if they used a local coach and staff and physician champions.9 The purpose of this case report is to describe the lessons learned from one SNF that targeted the reduction of rehospitalizations for patients with HF.
Methods
The project was reviewed and approved by the local Institutional Review Board. One SNF described above received grant funding to increase efforts to reduce rehospitalizations during 2011. The SNF is a 160 bed long-term care facility with 60 beds dedicated to skilled nursing care. The SNF is located in the suburbs and the majority of patients are Caucasian. Because the QI prior work indicated that a coach was important to implementation success, a nurse practitioner was hired, with part of her duties being the HF coach. The physician from the original program served as a facilitator. Other members of the leadership team included the executive director, director of nursing, marketing executive, dietician, and a clinical nurse specialist.
The SNF leadership determined that the best way to streamline resources was to develop specialty beds for all patients with HF admitted to the SNF. These beds would be assigned to licensed practical nurses and registered nurses who were trained in the HF disease management program. This reduced the burden of training all staff in the SNF and provided a way to enhance accountability for the HF disease management protocols. Staff was specifically trained to rapidly identify patients’ signs and symptoms of a changing condition so that early treatment could be initiated. Education modules (e.g. identification of patients’ signs and symptoms, HF diet, daily weighing, and when to call the physician) were delivered to patients and families during the patient’s SNF stay. Specially trained staff recorded completion of the modules using a tracking tool. A trained dietician assisted patients with dietary choices while in the facility and nursing staff implemented a structured discharge plan for HF self-management at home.
The SNF leadership also developed a registry to collect and store data on all patients regarding the number and reasons for rehospitalization. It was the intent of the leadership team to use the registry to examine the number of rehospitalizations, the differences between patients with and without HF, and to identify factors related to rehospitalizations. The registry contained data on age category (<80, 80-89, <=90), day of transfer to the hospital (weekday or weekend),primary or secondary HF diagnosis, high and low risk for rehospitalization, and length of stay in the SNF. The high and low risk for rehospitalization was captured by a risk tool. The risk tool was a simple way for staff to categorize patients with HF at the time of admission to the SNF and is defined as follows:
High-risk category included any one of the following:
Hospitalized in the last 6 months for HF exacerbation
Primary hospital discharge diagnosis of HF or an active secondary diagnosis (signs and symptoms of HF)
New York Heart Association Classification III or IV
Hypertensive with blood pressure > 150/90
Low-risk category included both criteria present:
6 months or longer since last hospitalization
New York Heart Association Classification I or II
The inclusion of HF as a primary or secondary diagnosis was used to evaluate the value of this single factor on rehospitalizations. Primary and secondary hospital discharge diagnosis was assigned by the discharging hospital. A primary diagnosis was defined as the primary reason for the rehospitalization. A secondary diagnosis was defined as a history of HF as listed in the discharge diagnosis list.
Length of stay in the SNF was identified from the literature as an important factor to consider for patients with HF due to the high rehospitalization rates in community samples during the first 7 days after discharge.1 Facility leadership determined that analyzing SNF length of stay would inform whether hospital transfer early in the SNF stay may indicate patients were discharged from the hospital prematurely.
The registry was developed and maintained by the Director of Nursing, a registered nurse, because no electronic system existed to systematically or reliably collect and store the data. All rehospitalizations, for both patients with HF and non-HF, were included in the registry and the cause of rehospitalization was abstracted from nursing notes documented at the time of the transfer to the hospital. Nursing notes were descriptive and routinely described the reason for the transfer to the hospital as the symptoms a patient was experiencing or abnormal vital sign that prompted the hospital transfer. There was no standardization of choices for documentation of the reason for hospitalization; specifically SNF staff does not have a patient diagnosis at the time of hospital transfer. The rehospitalizations were categorized into seven different reasons: critical event (such as patient found agonal, severe chest pain, or sudden severe dyspnea), unexpected and concerning symptoms (a new symptom that was previously not occurring, such as shortness of breath in a patient who was not previously short of breath), lab or vital abnormality, tube failure (such as a pulled-out gastric tube), infection/fever, fall, or other. The unexpected symptoms category was further categorized into five types: cardiopulmonary, gastrointestinal, neurological, genitourinary, and other. All patients admitted to the SNF were included in the registry regardless of insurance. The registry data were used to explore reasons for rehospitalizations in order for the facility to initiate future quality improvement projects.
Analyses
Rates of rehospitalization were compared among patients with HF at the SNF pre- and post-HF (2008-2012) disease management program implementation. Next, within the data collected in the post HF disease management program implementation, we compared the reasons for rehospitalization and type of unexpected symptoms between patients with a primary or secondary HF diagnosis versus those without HF using Chi-square tests. Next, in the subset of patients with a HF diagnosis, we examined the association of rehospitalization with HF as a primary diagnosis, rehospitalization risk category, age group, day of transfer (weekend or weekday), and SNF length of stay using Chi-square tests.
Results
At this SNF, rehospitalization rates decreased during the 4 years of active QI work. In 2008, prior to the HF disease management program implementation, out of 79 patients with HF, 34 (43%) were rehospitalized.8 After implementation of specialty HF beds (July 2011 to June 2012), 35 out of 115 (30%) patients with HF were rehospitalized (p=0.07).
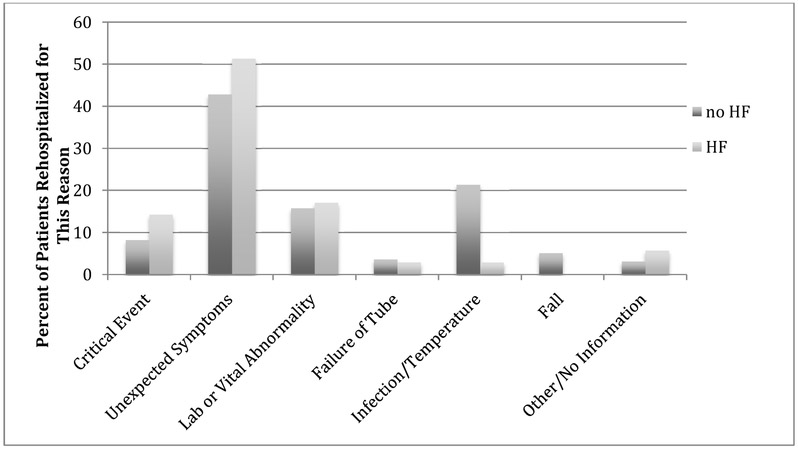
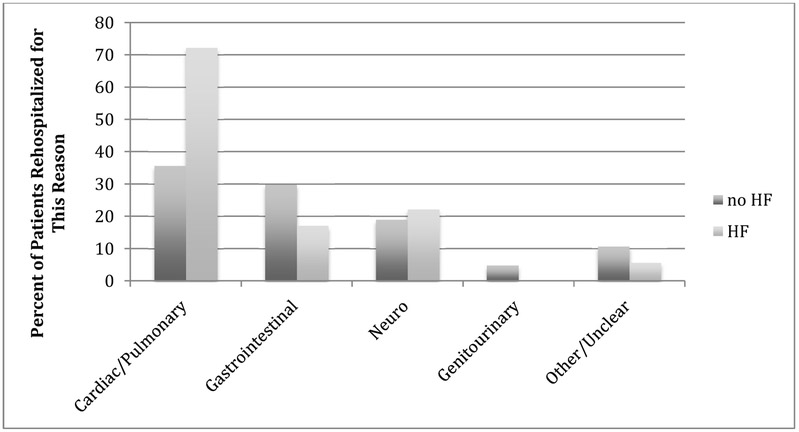
Figure 1 displays the number of patients (N=231) and reasons for rehospitalization of patients with (n=35) and without HF (n=196). Reasons for rehospitalization were relatively similar between patients with and without HF, with the exception of infection or fever. Among those without a HF diagnosis, 42 (21%) were rehospitalized due to infection or fever, while 1 (3%) patient with HF was rehospitalized for this reason (p=0.009). There were no differences identified among the other reasons for rehospitalization. Further, 102 patients (18 HF, 84 without HF) were rehospitalized due to unexpected symptoms, and the distribution of the types of unexpected symptoms by HF diagnosis is shown in Figure 2. Over 70% of patients with HF were rehospitalized for cardiac/pulmonary symptoms, whereas 36% of patients without HF were rehospitalized for cardiac/pulmonary reasons (p=0.004).
Figure 1:
Reasons for Rehospitalization of Skilled Nursing Facility Patients With (n= 35) and Without (n=196) Heart Failure
Figure 2:
Percent of Types of Unexpected Symptoms Related to Rehospitalizations Among Skilled Nursing Facility Patients With (n=18) and Without Heart Failure (n=84).
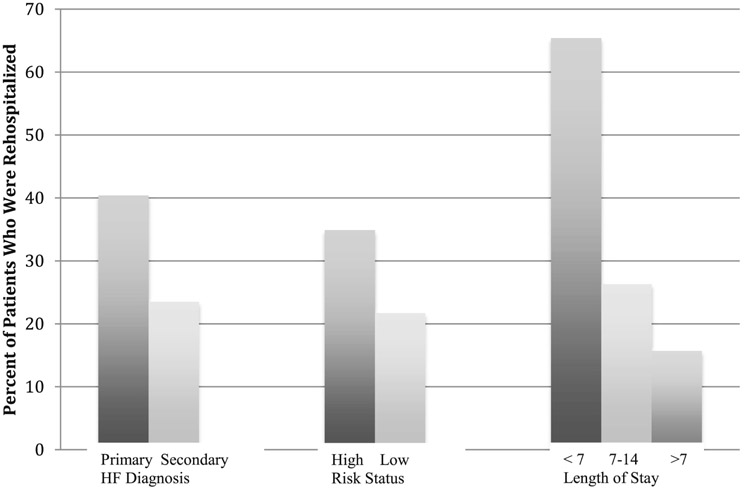
Factors related to rehospitalization in the 115 patients with HF are displayed in Figure 3. A higher percentage of patients with HF as their primary diagnosis (19/47, 40%) were rehospitalized compared to those who had HF as a secondary diagnosis (16/68, 24%) (p=0.05). Also, patients in the high-risk category had a higher rate of rehospitalization (29 /83, 35%) compared to those in the low-risk category (5/23, 22%) (p=0.08). Patients with HF with a SNF length of stay less than 7 days were more likely to be rehospitalized (17/ 26, 65%) than those with a longer stay (10/38, 26%) (p=.04). We did not observe significant differences in rates of rehospitalization among patients with HF by age groupings (<80, 80-89, >=90; 30.3%, 34% and 24.1% respectively, p=.65), or admission time during the weekend (11/40 or 27.5%) compared with those admitted during the. week (24/75, 32%) (p=.81).
Figure 3:
Factors Associated With Rehospitalization for Skilled Nursing Facility Patients With Heart Failure (N=115)
Discussion
We found that a registry aided in the tracking and understanding of factors related to rehospitalizations in one SNF. This facility demonstrated that the collection of data is possible and that learning from the data and making improvements can lead to better outcomes. The registry assisted the leadership in the identification of indicators of HF rehospitalization, including a hospital discharge primary diagnosis of HF, a high-risk category, and length of SNF stay less than 7 days. Although in community-dwelling elders the reduction of the 30-day HF rehospitalization rate is associated with a physician visit within the first 7days after hospital discharge, factors associated with rehospitalizations from SNF back to the hospital have not been clearly established.11
Although the registry was an important component in the continuation of the quality improvement initiative, it had limitations. The registry was created manually and required staff time to read nursing notes and record responses. Data capture was time consuming, reflective of clinical practice, and potentially inaccurate. The implementation of an electronic medical record is needed to support and sustain efforts in SNFs. In addition, data acquisition regarding reasons for patient rehospitalization was difficult due to lack of diagnostic capability at the time of hospital transfer and substandard reporting mechanisms. At the time of transfer to the hospital, symptom reports, and not a medical diagnosis, were the predominant reason for rehospitalizations. The lack of a medical diagnosis makes improvement challenging; however, this emphasizes the importance of competent symptom monitoring by SNF staff, especially early in the patient’s SNF stay. It also emphasizes the importance of bidirectional communication between hospital and SNF for quality improvement in both settings.
Differences in reasons for rehospitalizations between patients with and without HF were noted. Patients with HF were more often admitted due to critical events and unexpected cardiopulmonary symptoms. Patients without HF were more likely to be readmitted due to infection or fever. These reasons for rehospitalizations rely heavily on assessment of symptoms and vital signs. Front line, unlicensed assistive staff is responsible for the task of measuring vital signs and has the most contact with patients. Often, vital signs are taken using automatic electronic devices to check heart rate, blood pressure, and temperature. These devices may distract the unlicensed staff from observing the patients’ symptoms, specifically, monitoring respiratory rate and other subtle changes in symptoms that are critical assessments during a change of condition. Observation is especially important for patients who have difficulty identifying their own symptoms or communicating symptom changes. Leaders in SNFs can improve HF assessment by training unlicensed personnel about the importance of observation in addition to objective vital sign skills.
Over the 4 year implementation of the HF disease management program, rehospitalizations went from 45% in 2009 to 30% in 2012. The QI initiatives in this SNF were effective as leaders and staff focused on a common goal and implementation of incremental improvement through multiple plan-do-study-act cycles. The SNF in this case report demonstrated characteristics of a “learning” organization. Specifically, the staff collected data, identified gaps, and implemented improvement.10 Leadership took lessons learned from their implementation during 2009 -2011 (difficulty training all facility staff, the need to track data, and champions) and implemented changes that included designated HF beds, assigning a HF staff champion, a HF coach, and a patient registry.
In long-term care, QI initiatives are effective as has been demonstrated in the Interventions to Reduce Acute Care Transfers (INTERACT) project.12 The INTERACT project provides online tools and resources for long-term care facilities to implement evidence-based guidelines to manage acute changes in the patient’s condition in order to avoid hospitalization. INTERACT has 5 fundamental strategies: (1) incorporation of QI methods, (2) early identification and evaluation of changes in condition, (3) management of common changes in condition, (4) improved advance care planning, and (5) improved communication with and between the nursing home staff and hospital. Use of the INTERACT tools has been reported to improve outcomes in large, system wide long-term care implementation.13;14 Because patients with HF have one of the highest readmission rates, specific QI programs for this subset of patients may be of additional benefit.
A limitation was that the results were from only one institution and as such cannot be generalized. Research is needed to test whether or not these factors are related to rehospitalizations in multiple sites. Another limitation was that the project was funded by an outside source. Although the funding has ended, the administrators at the facility realized the benefit of the nurse practitioner hired for the project and retained her at the facility to continue the work of the QI initiative.
Clinical implications include the need to target vigilant assessment of a declining condition in patients with a primary HF diagnosis during the first 7 days of SNF care. The use of the HF rehospitalization risk tool may also provide insight in the identification of patients at high-risk for readmission. Leaders in SNFs can create a QI learning environment by educating their staff on QI methods. Resources for QI education are available at the Institute for Healthcare Improvement (IHI.org) and in a free online course.15
In this case, we have highlighted specific factors important for future research to reduce rehospitalizations of patients with HF. These factors include use of a patient registry to track data, distinguishing between patients with and without HF, and implementation of a rehospitalization risk tool. The changes in Medicare rules and impending financial penalties for rehospitalizations provide an opportunity for leaders in SNFs to adopt QI methods, driven by data to improve processes of patient care and outcomes.
Abbreviation List
- HF
heart failure
- SNF
skilled nursing facility
- PAC
post-acute care
- QI
quality improvement
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Mary A. Dolansky, Frances Payne Bolton School of Nursing.
Luann Capone, Cleveland Clinic, Connected Care Program.
Erin Leister, University of Colorado School of Public Health, Department of Biostatistics and Informatics.
Rebecca Boxer, University of Colorado School of Medicine.
References
- 1.Jurgens CY, Goodlin S, Dolansky MA, Ahmed A, Fonarow GC, Boxer R, Arena R, Blank L, Buck HG, Cranmer K, Fleg JL, Lampert RJ, Lennie TJ, Lindenfelf J, Pina IL, Semla T, Trebbien P, Rich MW (2015). Heart failure management in skilled nursing facilities. A scientific statement from the American Heart Association and the Heart Failure Society of America. Journal of Cardiac Failure, 21(4), 263–297. [DOI] [PubMed] [Google Scholar]
- 2.Slavitt AM, Burwell SM (2015) Medicare Program; Prospective Payment System and Consolidated Billing for Skilled Nursing Facilities (SNF’s) for FY 2017, SNF Value-Based Purchasing Program, SNF Quality Reporting Program, and Staffing Data Collection. Retrieved 5-1-2016 from https://www.federalregister.gov/articles/2016/04/25/2016-09399/medicare-program-prospective-payment-system-and-consolidated-billing-for-skilled-nursing-facilities.
- 3.Dolansky MA, Xu F, Zullo M, Shishehbor M, Moore SM, & Rimm AA (2010). Postacute care services received by older adults following a cardiac event: A population-based analysis. Journal of Cardiovascular Nursing, 25(4), 342–249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.American Medical Directors Association (2013). Heart Failure in the Long-Term Care Setting. CPGR2. Retrieved 5-1-2016 from http://www.paltc.org/product-store/heart-failure-cpg. [Google Scholar]
- 5.Harrington C (2006). Assessing heart failure in long term care facilities. Iowa City (IA): University of Iowa Gerontological Nursing Interventions Research Center, Research Translation and Dissemination Core; Retrieved 5-1-2016 from Agency for Healthcare Quality National Guideline Clearinghouse. https://www.guideline.gov/content.aspx?id=37694 [Google Scholar]
- 6.Centers for Medicare & Medicaid Services Initiative to reduce avoidable hospitalizations among nursing facility residents Retrieved 5-1-2016 from http://innovation.cms.gov/initiatives/rahnfr.
- 7.Hutt E, Ecord M, Ellertsen TB, Frederickson E, & Kramer AM (2002). Precipitants of emergency room visits and acute hospitalization in short0stay Medicare nursing home residents. Journal of the American Geriatrics Society, 50, 223–229. [DOI] [PubMed] [Google Scholar]
- 8.Boxer R, Dolansky MA, Frantz MA, Prosser R, Hitch J, & Pina I (2012). The bridge project improving heart failure care in skilled nursing facilities. Journal of the American Medical Directors Association, 13(1), 83–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dolansky MA, Hitch JA, Piña IL, & Boxer RS (2013). Improving heart failure disease management in skilled nursing facilities: Lessons learned. Clinical Nursing Research, 22(4), 432–47. [DOI] [PubMed] [Google Scholar]
- 10.Senge PM (2006). The Fifth Discipline: The Art and Practice of the Learning Organization. Double Day: New York. [Google Scholar]
- 11.Hernandez MB, Schwartz RS, Asher CR, Navas EV, Tolfalusi V, Buitrago I, Lahoti A, Novaro GM (2013). Predictors of 30-day readmissions in patients hospitalized with decompensated heart failure. Clinical Cardiology, 36(9), 542–547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ouslander JB, Bonner A, Herndon L and Shutes J (2014). The interventions to reduce acute care transfers (INTERACT) quality improvement program: an overview for medical directors and primary care clinicians in long-term care. Journal of the American Medical Directors Association, 15(3) 162–170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tena-Nelson R, Santos K, Weingast E, Amrhein S, Ouslander J, Boockvar K (2012). Reducing potentially preventable hospital transfers: results from thirty nursing home collaborative. Journal of the American Medical Directors Association, 13(7), 651–656. [DOI] [PubMed] [Google Scholar]
- 14.Rantz MJ, FLesner MK, Franklin J, Galambos C, Pudlowski J, Pritchett A, Alexander G, Lueckenotte A (2015). Better care, better quality: Reducing avoidable hospitalizations of nursing home residents. Journal of Nursing Care Quality, 30(4), 290–297. [DOI] [PubMed] [Google Scholar]
- 15.Dolansky MA, Moore SM, Singh MK (2014). Take the lead on Healthcare quality. Massive open online course. Retrieved 5-1-2016 from https://www.coursera.org/course/hcqualityimprovement. [Google Scholar]